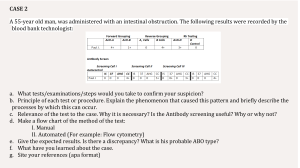
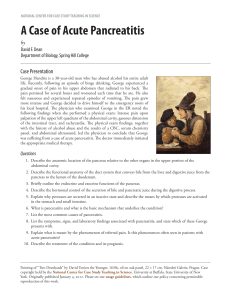
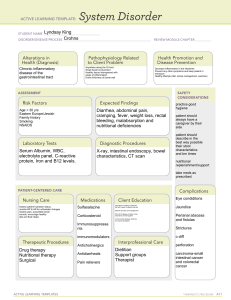
TEST 5 Acute and Chronic Cholecystitis and Acute Pancreatitis Ch 54 iggy 1. Apply knowledge of pathophysiology when planning care of patients with pancreatitis and cholecystitis, including signs, symptoms, risk factors, and complications a. Cholecystitis: inflammation of the gallbladder. Can be chronic or acute. Inflammatory process often affects the client’s nutrition status. i. Acute cholecystitis: 1. Calculous cholecystitis: chemical irritation and inflammation result from gallstones or calculi (cholelithiasis), that obstruct the cystic duct (most often), gallbladder neck, or common bile duct (choledocholithiasis). When the gallbladder is inflamed, trapped bile is reabsorbed and acts as a chemical irritant to the gallbladder wall. 2. Acalculous cholecystitis: inflammation occurring without gallstones. Typically associated with biliary stasis caused by any condition that affects the regular filling and emptying of the gallbladder. a. Can occur with sepsis, severe burns/trauma, long-term TPN, multiple organ dysfunction syndrome (MODS), major abdominal surgery, and hypovolemia ii. Chronic cholecystitis: repeated episodes of cystic duct obstruction cause chronic inflammation. Calculi are almost always present. Gallbladder becomes fibrotic and atrophied. iii. Risk factors for cholecystitis: women of all ages, American Indian, Mexican American, Caucasian, obesity, rapid weight loss or prolonged fasting; low-fat diet, increased cholesterol and lipids, women on HRT, cholesterol-lowering drugs, family hx of gallstones, Crohn’s disease, gastric bypass surgery, sickle cell disease, glucose intolerance/DM II, pregnancy, genetic factors. iv. S/S: abdominal pain- pain can be vague in chronic cases, discomfort that radiates to the right shoulder, pain triggered by high fat or high-volume meal, anorexia, nausea/vomiting, dyspepsia, eructation, flatulence, feeling of abdominal fullness, rebound tenderness (Blumberg sign), fever, jaundice, clay-colored stools, dark urine, steatorrhea (most common with chronic cholecystitis) b. Acute pancreatitis: inflammatory process caused by a premature activation of excessive pancreatic enzymes that destroy ductal tissue and pancreatic cells, resulting in autodigestion and fibrosis of the pancreas. i. Complications: pancreatic infection (causes septic shock), hemorrhage (necrotizing hemorrhagic pancreatitis), acute kidney failure, paralytic ileus, hypovolemic shock, pleural effusion, acute respiratory distress syndrome, atelectasis, pneumonia, multiorgan system failure, disseminated intravascular coagulation, type 2 DM ii. Causes: trauma- external (blunt, stab wounds, GSWs), metabolic problems (hyperlipidemia, hyperparathyroidism, or hypercalcemia), renal involvement (failure or transplantation), familial, inherited pancreatitis, penetrating gastric or duodenal ulcers (resulting in peritonitis), viral infections such as coxsackievirus B and HIV, alcoholism, toxicities of drugs (opiates, sulfonamides, thiazides, steroids, and oral contraceptives), cigarette smoking and tobacco use, cystic fibrosis, gallstones iii. S/S: pain (mid-epigastric or LUQ), jaundice, gray-blue discoloration of the abdomen and periumbilical area, gray-blue discoloration of the flank, caused by pancreatitis enzyme leakage to cutaneous tissue from the peritoneal cavity, ascites might be present, abdominal tenderness, guarding, tachycardia, fever iv. Labs: increased amylase, elevated lipase, elevated trypsin, elevated elastase, elevated glucose, decreased Ca and Mag, elevated bilirubin, elevated ALT, elevated AST, elevated leukocyte count, and presence of Creactive protein. v. Imaging: abdominal ultrasound (most sensitive test to diagnose causes of pancreatitis), contrast-enhanced CT is the most reliable image and diagnosis of acute pancreatitis. c. Chronic pancreatitis: progressive, destructive disease of the pancreas that has remissions and exacerbations. Inflammation and fibrosis of the tissue contribute to pancreatic insufficiency and diminished function of the organ. 1. Calcifying pancreatitis (CCP)- most caused by alcoholism and most common type. Found predominantly in men. 2. Chronic obstructive pancreatitis- develops from inflammation, spasm, and obstruction of the sphincter of Oddi, often from cholelithiasis (gallstones). 3. Autoimmune pancreatitis- chronic inflammatory process in which immunoglobulins invade the pancreas. 4. Idiopathic and hereditary chronic pancreatitis- associated with SPINK1 and CFTR gene mutations. People with hereditary pancreatitis are 53 x more likely to get pancreatic cancer. ii. Key features: intense abdominal pain (major symptom) that is continuous and gnawing, abdominal tenderness, ascites, possible LUQ mass, respiratory compromise manifesting with adventitious or diminished breath sounds, dyspnea, or orthopnea, steatorrhea; clay-colored stools, weight loss, jaundice, dark urine, polyuria, polydipsia, polyphagia (DM) 2. Develop a plan of care for patients with pancreatitis and cholecystitis a. Pancreatitis: severe acute pain d/t pancreatic inflammation and enzyme leakage. Weight loss due to inability to ingest food and absorb nutrients. b. Cholecystitis: acute or persistent pain due to gallbladder inflammation and/or gallstones. Weight loss due to decreased intake because of pain, nausea, and anorexia. 3. Identify assessment priorities for patients with pancreatitis and cholecystitis 4. Analyze the teaching needs of patients with pancreatitis and cholecystitis. a. Pancreatitis: avoid things that make your symptoms worse such as drinking caffeinated beverages. Avoid ingestion; refer to self-help group for assistance. Avoid nicotine. Eat bland, low-fat, high-protein, and moderate-carbohydrate meals; avoid gastric stimulants such as spices. Eat small meals and snacks high in calories. Take pancreatic enzymes that have been prescribed for you with meals. Rest frequently; restrict your activity to one floor until you regain your strength. b. Cholecystitis: report any repeated abdominal or epigastric pain with vomiting and/or diarrhea that may occur several weeks to several months after surgery (postcholecystecomy syndrome). Teach to eat nutritious foods and avoid fatty foods, especially fried food, butter, and fast food. 5. Prioritize care for patients undergoing a cholecystectomy a. Laparoscopic cholecystectomy- MIS, the gold standard. Advantages: complications are not common, death rate is low, bile duct injuries are rare, patient recovery is quicker, and postop pain is less severe. Assess patient’s O2 sat frequently until the effects of anesthesia have passed. Remind patient to perform deep-breathing exercises every hour. IBD and Intestinal Obstruction Ch 51 and 52 iggy 1. Apply knowledge of pathophysiology when planning care of patients with ulcerative colitis, Crohn’s, or intestinal obstruction, including signs, symptoms, risk factors, and complications. Differentiate between a mechanical and non-mechanical intestinal obstruction a. Intestinal obstructions: Mechanical obstruction: the bowel is physically blocked by problems outside the intestine (ex. adhesions), in the bowel wall (ex. Crohn’s disease), or in the intestinal lumen (ex. Tumors). Nonmechanical obstructions (paralytic ileus or functional obstruction): peristalsis is decreased or absent because of neuromuscular imbalance, resulting in slowing of the movement or a backup of intestinal contents. i. Complications: fluid and electrolyte balance and acid-base balance can be affected. Obstructions high in the small intestines cause loss of gastric hydrochloric acid which can lead to metabolic alkalosis. Obstruction below duodenum but above large bowel results in a loss of acids and bases (acid-base balance usually not compromised). Obstruction at the end of small intestine and lower in the intestinal tract causes loss of alkaline fluids which can lead to metabolic acidosis. Hypovolemia can cause AKI or even death. Bacterial peritonitis with or without actual perforation can result. Strangulated obstruction (obstruction with compromised blood flow that can be life threatening). ii. S/S: Small bowel obstruction: 1. Abdominal pain/discomfort possibly accompanied by visible peristaltic waves in the upper and middle abdomen, upper or epigastric abdominal distention, nausea and early, profuse vomiting (may contain fecal matter), obstipation, severe fluid and electrolyte imbalances, metabolic alkalosis (not always present). iii. S/S: Large bowel obstruction: 1. Intermittent lower abdominal cramping, lower abdominal distention, minimal or no vomiting, obstipation or ribbon-like stool, no major fluid or electrolyte imbalances, metabolic acidosis (not always present). b. Identify patients at risk for intestinal obstruction. i. Risk factors: prevalence and incidence are not well known. More commonly occurs in patients with bowel surgery hx, intestinal tumors, and older adults. c. Ulcerative colitis: widespread chronic inflammation of the rectum and rectosigmoid colon but can extend to entire colon when the disease is extensive. UC is associated with periodic remissions and exacerbations. The intestinal mucosa becomes hyperemic (increased blood flow), edematous, and reddened. In more severe inflammation, the lining can bleed, and ulcers can occur. i. Risk factors: Genetic (found in twins and families), immunologic causes (autoimmune dysfunction- IgG has been found in some patients with UC). UC increases risk for colon cancer. ii. S/S: vitals are usually WNL, PA can be normal in mild cases. Abdominal distension along the colon may occur. Tenesmus (an unpleasant and urgent sensation to defecate), lower abdominal colicky pain relieved with defecation, malaise, anxiety, anemia, dehydration, fever, and weight loss are common. iii. Labs: hct/hgb may be low; increased WNC, c-reactive protein, and or ESR; Na, Cl, K+ can be low because of diarrhea and malabsorption; decreased albumin is found in patients with extensive disease from losing protein in the stool. d. Crohn’s disease: chronic inflammatory disease of the small intestine, the colon, or both. It can affect the GI tract from the mouth to the anus but most commonly affects the terminal ileum. CD presents with inflammation that causes a thickened bowel wall. Strictures and deep ulcerations also occur which puts the patient at risk for developing a bowel fistula. i. Complications (similar to UC): hemorrhage/perforation, abscess formation, toxic megacolon, intestinal malabsorption, nonmechanical bowel obstruction, fistulas, colorectal cancer, extraintestinal 2. 3. 4. 5. 6. complications (arthritis, hepatic, and biliary disease (cholelithiasis), oral and skin lesions, and ocular disorders, such as iritis), osteoporosis. ii. S/S: abdominal pain that is constant (RLQ), pain around umbilicus before and after bowel movements, weight loss, diarrhea, low-grade fever, steatorrhea, stools may contain bright red blood. iii. Risk factors: exact cause of CD is unknown. Genetic, immune and environmental factors may contribute. Develop a plan of care for patients with ulcerative colitis, Crohn’s, or intestinal obstruction. Identify assessment priorities for patients with ulcerative colitis, Crohn’s, or intestinal obstruction Analyze the teaching needs of patients with ulcerative colitis, Crohn’s, or intestinal obstruction, including education related to medications. Compare and contrast ulcerative colitis and Crohn’s disease KNOW WBC, HEMOGLOBIN, HEMATOCRIT LEVELS.