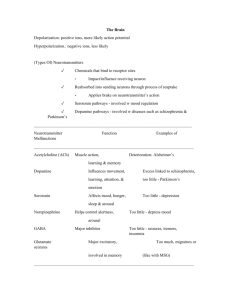
Chapter 11 – Psychotropic Drugs Biopsychiatry “The biological approach” a theoretical approach to understanding MH disorder as biological malfunctions of nervous system o Brain function is related to several factors: genetics, neurodevelopmental factors, drugs, infection, psychosocial experience, or combinations of all of these factors. o Changes (in behaviour/emotional/mental) are a result of brain damage Ex. When the brain is damaged, the way it produces/responds to NMT is changed also, resulting in symptoms of depression, anxiety, ptsd or any other combination of behavioral, emotional or mental symptoms. o Medication is used to augment effectiveness of NMT, and to restore balance to brain. o Lots of theories with drug therapies like dopamine theory of schizophrenia, but full understanding of how all these drugs improve symptoms are not well understood. STRUCTURE AND FUNCTION OF THE BRAIN Functions and Activities of the Brain Monitor changes in the external world Monitor the composition of body fluids Regulate the contractions of skeletal muscles Regulate the internal organs Initiate and regulate the basic drives: hunger, thirst, sex, aggressive self-protection Mediate conscious sensation Store and retrieve memories Regulate mood (affect) and emotions Think and perform intellectual functions Regulate the sleep cycle Produce and interpret language Process visual and auditory data mental health disturbances are often associated with alterations in other brain functions, and the drugs used to treat mental disturbances can interfere with other activities of the brain. Maintenance of Homeostasis - - - - - brain is coordinator of body’s response to internal/external changes, requires constant monitoring of environment, and control over appropriate organs of response, the goal of these responses are to maintain homeostasis. Peripheral nerves receive information about external world, sensations like light, sound, touch. A component of major psychiatric disturbance is alteration of sensory experience. o Pt experiences sensations that don’t originate in the external world. To respond to external changes brain has control over skeletal muscle, both for contraction, and contraction coordination for fine tuning. o Both psychiatric disease (PD) and treatment of PD with psychotropics are associated w movement disturbances Skeletal muscles controlled by the brain include the diaphragm (breathing) and muscles of the throat, tongue, and mouth (speech) Can lead to changes like stimulation/depression of respiration or slurred speech Brain not only monitors external world but also close watch on internal function – brain monitors constantly BP, temp, Blood gases, and chemical composition of body fluids received by the brain that command responses by the brain to maintain homeostasis. Adjustments to changes within body require the brain to exert control over various internal organs Regulation of the Autonomic Nervous System and Hormones - ANS and endocrine system are communication links b/w the brain and cardiac muscle, smooth mm and glands of which internal organs are composed. o If brain needs to stimulate heart -> activates sympathetic nerves to SA node and ventricular myocardium o If brain needs to vasoconstrict, it activates sympathetic nerves to smooth mm of arterioles. - - - This linkage b/w organs also translates mental health disturbances like anxiety into alteration in internal function o Ex. Anxiety for some people causes activation of parasympathetic nerves to digestive tract leading to hypermotility and diarrhea. Brain also exerts influence over internal organs via hormonal secretions of pituitary gland which regulates other glands. Hypothalamus secretes releasing factors, hormones that act on the pituitary gland to stimulate or inhibit synthesis and release of pituitary hormones, and once in the circulation these hormones in turn influence various internal activities o Ex. GNRH secreted by hypothalamus @ puberty stimulates release of FSH and LH, activating ovaries or testes. Hypothalamus secretes CRH – corticotropin releasing hormone – stimulating pituitary to release corticotropin, which stimulates cortex of each adrenal gland to secrete cortisol – a part of the normal response to mental and physical stresses o All 3 of those hormones influence functions of nerve cells of the brain, there is good evidence that this system is overactive in both anxiety and depression and doesn’t respond properly to negative feedback. Control of Biological Drives and Behaviour - Disturbances in basic drives like over/undereating or loss of sexual interest can be indication of underlying mental health disorders like depression. Cycle of sleep and wakefulness - Cycle of sleep and wakefulness (also intensity of alertness when person is awake) is under control of brain. Assessment of sleep patterns is part of what is required to determine a diagnosis of a MHD. Many drugs used to treat MHD interfere with normal regulation of sleep and alertness. Circadian rhythms - Cycle of sleep and wakefulness is one aspect of circadian rhythms – the fluctuations of physiological and behavioral parameters over a 24h cycle. Other variations: changes in body temp, secretion of hormones like corticotropin and cortisol and NMT like norepinephrine and serotonin. Both NE and ST are believed to be involved in mood – daily fluctuations of mood are related in part to circadian rhythm of NMT secretion (which is altered in MHD, esp those that involve mood) Conscious Mental Activity - conscious mental experience + sense of self originates from neurophysiological activity of brain. Conscious mental activity can be a basic random stream, or complex problem solving and interpretation of environment, and can be distorted in MHDs o Eg. schizophrenia may have chaotic and incoherent speech and thought patterns ((word salad) or unconnected phrases/topics “looseness of association”) and delusional interpretations of personal interactions Memory - Ability to retain and recall past experience. Some MHD like dementia, memory is affected. Social Skills - - Social skills make interpersonal relationships possible, its often a neglected aspect of brain functioning. All kinds of MHD, interpersonal relationships are important characteristics of the disorder and improvements in relationships are gauges of progress. Positive reward-based experiential learning and negative avoidance learning may involve different areas of the brain. Cellular Composition of the Brain - Brain made of billions of neurons which carry out same 3 types of physiological actions: o Respond to stimuli o Conduct electrical impulses o Release chemicals called neurotransmitters - Electrical impulse conduction results in change of membrane permeability allowing inward flow of sodium and outward flow of potassium -> changes polarity. - Electrical charges are self-propagating, a change on one end of a cell is conducted along the membrane until it reaches the other end. o The significance of this is that electrical impulses serve as a means of communication b/w parts of the body. - Once an impulse reaches the end of a neuron, an NMT is released, from the axon terminal @ the presynaptic neuron. It then diffuses across a space or “synapse” to an adjacent postsynaptic neuron, attaching to receptors. - It’s the interaction b/w neurotransmitters and receptors that is the major target of drugs used to treat MHDs. - After the NMT binds to a receptor, exerts its influence on the postsynaptic cell, it separates from the receptor and is destroyed. There are two mechanisms in which neurotransmitters are destroyed. o Enzymes (like acetylcholine enzyme destroyed by acetylcholinesterase) o Reuptake – back into presynaptic cell like norepinephrine. Upon return they are either reused or destroyed - MAO – monoamine oxidase is the enzyme that destroys monoamine NMT, like norepinephrine, dopamine, serotonin. o Once concentration of NMT is strong enough, to regulate concentration @ postsynaptic receptors, many NMT attach to presynaptic receptors @ the synapse to inhibit further release of NMT. In many cases, neurons release more than 1 chemical at a time – neuropeptides that can initiate long term changes on postsynaptic cells – like basic cell functions – gene expression and lead to modification of cell shape and responsiveness to stimuli. – this means that action of one neuron on another not only has the immediate response, but also affects its sensitivity to future influence. Communication b/w neurons @ a synapse is not unidirectional o Neurotrophic factors (proteins and gases) are released by postsynaptic cells, influencing growth, shape, and activity of presynaptic cells – important in fetal brain development guiding the brain to form proper neuronal connections Internal and external influences can alter the synaptic network of the brain. Neuronal development and responsiveness isn’t dependent only on chemicals released by other neurons (neurotrophic factors) but also on chemicals STEROID HORMONES – estrogen, testosterone, cortisol, they can bind to neurons causing long and short term changes in neuronal activity o Example of this: hypersecretion of cortisol from Cushing’s disease, or from use of high dose prednisone to treat chronic inflammatory disease. Organization of the Brain Brain Stem Responsible for vital functions: regulation of blood bases, internal organs, blood pressure Psychosomatic link b/w higher brain activities (thought and emotion) Functions as initial processing center for sensory information – RAS (reticular activation system) Brain stem involved in sleep/wakefulness, and ability of cerebrum to carry out conscious mental activity. Ascending pathways (mesolimbic, mesocortical) o Play strong roles modulating emotional value of sensory material – project onto those areas of the cerebrum – hypothalamus, amygdala, hippocampus (collectively: LIMBIC SYSTEM) Important for emotional status and psychological function Hypothalamus: - part of brain stem o Very important for basic drives – hunger, thirst, sex – Cerebellum Posterior to brain stem, mostly involved in skeletal mm coordination and contraction and maintenance of equilibrium Coordination of contraction for smooth movement Cerebrum (cerebral cortex + basal ganglia) - - Its distinguishes humans from the rest of the animal kingdom, sits on top of and surrounds the brain stem, responsible for mental activities, conscious sense of being, Perception of external world, our body, emotional status, memory, control of skeletal mm for willful direction of movement. Language and ability to communicate. Cerebral cortex is responsible for conscious sensation and initiation of movement. o Specific areas of the cortex are responsible for specific sensations: the parietal cortex for touch, the temporal cortex for sound, the occipital cortex for vision, and so on. The initiation of skeletal muscle contraction is controlled by a specific area of the frontal cortex. o Language in both sensory and motor aspects Sensory: ability to read, understand spoken language, know names of objects perceived by senses Motor: physical ability to use mm properly for speech and writing Basal Ganglia o Deep within grey matter of cerebrum – regulation of movement. Amygdala and hippocampus o Emotions, learning, memory, basic drives Visualizing the Brain (2 types) Structural imaging techniques o identify gross anatomical changes in the brain o CT & MRI Functional Imaging Techniques o PET & SPECT o Reveal physiological activity of brain – physiological and biochemical changes as they occur in living tissue with radioactive tag tracing glucose. With schizophrenia, PET can show decreased use of glucose in frontal lobes. People with OCD show increased brain metabolism in certain areas in frontal cortex. Disturbances of Mental Function - Most occurrence of mental health dysfunction are of unknown origin - Known causes are drugs, (LSD), long-term use of prednisone, excess levels of hormones (thyroxine, cortisol), infection (encephalitis), AIDS, and physical trauma. - Evidence suggests many people with psychiatric disorders are genetically predisposed to them (thought and mood disorders prevalence higher in relatives than in general pop) o Concordance – how one twin will be affected by the same illness as the other - Psychosocial stress is another factor increasing likelihood - Genetics and environment interact in complex ways, some people are better able to cope with stress than others - altered activity of neurons is another possible cause o current focus is on limbic system neurons: norepinephrine, dopamine, serotonin, GABA, glutamate o its thought a deficiency of norepinephrine or serotonin = biological basis for depression can be related to deficient release by presynaptic cell, or loss of ability of postsynaptic to respond to NMT. Or reduction in receptors. - Schizophrenia and other thought disorders are associated physiologically with excess transmission of NMT dopamine – excess release of NMT or increase in rct responsiveness. - GABA – plays role in modulating neuronal excitability and anxiety o Anxiolytics increase effectiveness of GABA by increasing receptor responsiveness. - Take home: Alterations in mental status whatever the cause, are often accompanied by changes in basic drives, sleep patterns, body movement and autonomic functions. MECHANISMS OF ACTION OF PSYCHOTROPIC DRUGS - Pharmacodynamics – biochemical and physiological effects of drugs on body (includes MA + effect) Pharmacokinetics – actions of body on the drug (absorption, distribution) pharmacokinetics determines the blood level of a drug and guides dosage schedule. Pharmacogenetics - takes into consideration individual genetic differences when considering how much and which medication to prescribe. Liver transforms drugs into active metabolites. Close to 40% of pts fail to achieve clinical response with initial drug treatment, and 63% experience at least one adverse event during course of treatment. 10-15% pts discontinue due to this adverse event. Most psychotropics act by increasing or decreasing activity of certain NMT-RCT systems. Antianxiety and Hypnotic Drugs - GABA is the main inhibitory NMT – there are 3 types GABAA, GABAB, GABAC receptors. o The subtypes of GABA-A (α1, α2, α3) are targets of benzos, barbiturates and alcohol. - GABA enhancers exert a sedative-hypnotic action on brain function - Most commonly used antianxiety are benzos, and antidepressants; SSRI, and SNRI Benzodiazepines - Promote activity of GABA by binding to a specific GABA-A receptor, inhibiting cellular excitation by blocking release of neurotransmitters. – has a calming effect These GABA-A RCT are commonly found in the limbic system, the brain’s emotional center. Higher doses = sedation, most administered in Canada have a predominantly hypnotic (sleep inducing) effect, but loser doses of lorazepam and alprazolam (Ativan and Xanax) reduce anxiety without being as soporific (sleep producing) - They are great anticonvulsants – ability to reduce neuronal overexcitement from alcohol withdrawal Even at high doses, they rarely inhibit the brain to degree respiratory depression, coma and death result, but when combined with others (TCA, alcohol, or other CNS depressants) they are life threatening. - Benzos interfere with motor ability, attention, and judgement – caution with engaging in certain activities. Ataxia is a common adverse effect from abundance of GABA rct in cerebellum. Short-Acting Sedative–Hypnotic Sleep Drugs - - Zopiclone – “Z-Drug” its unrelated to existing (structurally) to hypnotics, but it promotes GABA and inhibits release of NMT. As a result Zopiclone effects are: o Sedative, hypnotic, anxiolytic, anticonvulsant, and muscle relaxant. Onset faster than most benzos (short acting). Also has short ahlf life – peak plasma 2 hrs. Unique adverse effect: bitter taste upon awakening. Drug intolerance/overdose: severe drowsiness or impaired coordination Potential for misuse, so never to be taken for more than 7-10 day straight and cautioned in those who misuse alcohol or other substances. All benzos are schedule IV – controlled. Zopiclone is a schedule F drug – meaning prescription is required for use. Buspirone Hydrochloride - - anxiolytic drug for the short-term relief of excessive anxiety without strong sedative-hypnotic properties, better tolerated than benzos its not a CNS depressant and doesn’t have as great danger for interaction with other CNS depressants, and also lacks potential for dependence (unlike benzos) MA is not well understood, but seems to moderately enhance effects of serotonin Its therefore classified as a partial serotonin agonist o Also an antagonist – binds to dopamine 2 rct, stimulating dopamine release and inhibits its destruction – so it bocks the effects of the neurotransmitter – (its an agonist and antagonist) Adverse effects: headache dizziness, lightheadedness, nausea, decreased concentration, insomnia. Treating Anxiety Disorders With Antidepressants - symptoms, neurotransmitters, and circuits of anxiety disorders overlap with depressive disorders and many antidepressants have effectively treated anxiety disorders. - SSRI - increase both serotonin and norepinephrine o Treat OCD, SAD (social anxiety disorder), generalized anxiety disorder, panic disorder, ant PTSD. Antidepressant Drugs - SSRI – increase serotonin @ synapse - SNRI – block reuptake of serotonin in norepinephrine back into nerve cells - TCA – no longer first choice – block reuptake of serotonin and norepinephrine - MAOI – prevent breakdown of monoamines and increase availability of NMT in presynaptic nerve terminal - NMT norepinephrine and serotonin play huge role in mood regulation There are 3 hypotheses of antidepressant meahcnism of action o Monoamine hypothesis of depression Suggests a deficiency of 1 or more of 3 NMT – serotonin, norepinephrine, or dopamine, increasing these, alleviated depression. o Monoamine Receptor hypothesis of depression Suggests low lvls of NMT cause postsynaptic RCT to be up-regulated (increased in sensitivity and #) increasing of NMT by antidepressants result in downregulation (desensitization) Delayed length of time for down-regulation may explain why it takes so long for antidepressants work, esp if they rapidly increase NMT. o They increase production of neurotrophic factors w prolonged use Factors that regulate survival of nrueons and enhance sprouting of axons to form new synaptic connections. Tricyclic Antidepressants - Widely used before SSRI, no longer first line Take longer to reach optimal dose, far more lethal in overdose Work by bocking reuptake of norepinephrine for secondary amines and both (norepi and serotonin) for the tertiary amines. This blockage prevents norepinephrine from coming onto contact with MAO – a degrading enzyme, therefore increasing levels of norepinephrine @ synapse. Similarly with serotonin – preventing destruction of serotonin. These drugs also block muscarinic RCT the normally bind acetylcholine, leading to typical anticholinergic effects o Blurred vision, dry mouth, tachycardia, urinary retention, constipation. They can also cause drowsiness and sedation (block histamine-1 receptors in the brain) Selective Serotonin Reuptake Inhibitors - preferentially block the reuptake and, therefore, the destruction of serotonin Zoloft also inhibits neuronal reuptake of serotonin and has weak effects on norepinephrine and dopamine neuronal reuptake. Don’t block muscarinic and histamine-1 RCT like TCA More selective action, without anticholinergic or sedation effects and allow better adherence. SSRI have other adverse effects though: stimulation of various serotonin RCT may inhibit spinal reflexes of orgasm, lead to apathy and low libido, and cause N+V. Serotonin–Norepinephrine Reuptake Inhibitors - increase both serotonin and norepinephrine Hypertension, induced in about 5% of patients, is a dose-dependent effect based on norepinephrine reuptake blockade SNRIs also have therapeutic effects on neuropathic pain (like TCA) o Works by limiting pain signals ascending to the brain Serotonin and Norepinephrine Disinhibitors - Its just one drug mirtazapine (Remeron) Unique drug that increases norepinephrine, dopamine, and serotonin (5-HT) transmission by blocking central presynaptic α2 adrenergic inhibitory receptors antianxiety and antidepressant effects it’s a potent H1 rct antagonist = drowsiness and increased appetite resulting in weight gain. Also anticholinergic adverse effects, also suicide risk (shouldn’t be used under 18) Advantages: lower incidence of sexual dysfunction and antiemetic effects. Monoamine Oxidase Inhibitors - - - prevent the destruction of monoamines by inhibiting the action of monoamine oxidase MAO, which is located in neurons and in the liver, which is a problem, because liver destroys monoamine substances that enter the body via food or drugs, one really important is tyramine – present in many food substances like aged cheese, pickled or smoked fish, chocolate, beans, beer and wine. Tyramine poses a threat of HYPERTENSIVE CRISIS. In severe cases – Adrenergic Crisis can occur – esp in presence of MAOI because tyramine isn’t destroyed by the liver – extreme tachycardia and hypertension. – there is also a large number of drugs that are monoamines, and their dose is determined by the livers ability to destroy them. MAOI are contraindicated with any other antidepressant or sympathomimetic drugs Other Antidepressants - Bupropion hydrochloride - Great as antidepressant and for smoking cessation (zyban) Acts as a dopamine–norepinephrine reuptake inhibitor, and inhibits nicotinic acetylcholine receptors to reduce addictive action of nicotine. It has no serotonin action – doesn’t cause adverse sexual effects Adverse effects: insomnia, tremor, anorexia, weight loss Trazodone hydrochloride – boner drug o a serotonin antagonist and reuptake inhibitor (SARI) o not first choice antidreprrand, often given w others because of sedative effects, helps combat insomnia. o Antidrpressant effects are seen only at high therapeutic levels, common adverse effects are sedation and orthostatic hypotension. o Sedative effect from histamine-1 blickade with minimal anticholinergic effects. o Can lead to rare adverse effect – (potent α1 blockade) - priapism (painful prolonged penile erection). Mood Stabilizers Lithium Carbonate