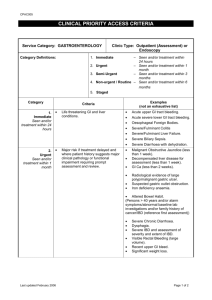
Anatomy of the Jejunum and Ileum General • Jejunum + ileum = 6-7 m long Jejunum • • • Second part of the small intestine, the jejunum, begins at the duodenojejunal flexure where the digestive tract resumes an intra-peritoneal course. Jejunum constituting approximately 2/5 Most of the jejunum lies in the left upper quadrant Ileum • • • • Third part of the small intestine, the ileum, ends at the ileocecal junction, the union of the terminal ileum and the cecum Ileum approximately 3/5 Most of the ileum lies in the right lower quadrant (RLQ) The terminal ileum usually lies in the pelvis from which it ascends, ending in the medial aspect of the cecum. Differentiation between the jejunum and ileum • Although no clear line of demarcation between the jejunum and ileum exists, they have distinctive characteristics that are surgically important Characteristics Caliber Wall Colour Vascularity Vasa recta Arcades Fat in mesentry Circular folds/ plicae circulares Lymphoid nodules (Peyer’s patches) Proximal Jejunum 2-4cm Thick & heavy Deeper red Greater Long Few large loops less Large, tall, & closely packed Few Distal Ileum 2-3cm Thin & light Paler pink Less Short Many short loops More Low & sparse, absent in distal part Many Mesentery • • • • • The mesentery is a fan-shaped fold of peritoneum that attaches the jejunum and ileum to the posterior abdominal wall The origin or root of the mesentery (approximately 15 cm long) is directed obliquely, inferiorly, and to the right It extends from the duodenojejunal junction on the left side of vertebra L2 to the right sacroiliac joint (ileocolic junction) The average length of the mesentery from its root to the intestinal border is 20 cm. The root of the mesentery crosses (successively): o The ascending and inferior parts of the duodenum o Abdominal aorta o IVC o Right ureter o Right psoas major o Right testicular or ovarian vessels Between the two layers of the mesentery are the superior mesenteric vessels, lymph nodes, a variable amount of fat, and autonomic nerves. Blood supply • • • • • Superior mesenteric artery (SMA) supplies the jejunum and ileum via jejunal & ileal arteries The SMA usually arises from the abdominal aorta at the level of the L1 vertebra, approximately 1 cm inferior to the celiac trunk Runs between the layers of the mesentery, sending 15-18 branches to the jejunum and ileum The arteries unite to form loops or arches, called arterial arcades These give rise to straight arteries, called vasa recta Venous drainage • • • The superior mesenteric vein drains the jejunum and ileum It lies anterior and to the right of the SMA in the root of the mesentery The SMV ends posterior to the neck of the pancreas, where it unites with the splenic vein to form the hepatic portal vein Lymphatics • • • • • • Specialized lymphatic vessels (lacteal) in the intestinal villi that absorb fat are called lacteals. They empty their milk-like fluid into the lymphatic plexuses in the walls of the jejunum and ileum. The lacteals drain in turn into lymphatic vessels between the layers of the mesentery. Within the mesentery, the lymph passes sequentially through three groups of lymph nodes: o Juxta-intestinal lymph nodes: located close to the intestinal wall. o Mesenteric lymph nodes: scattered among the arterial arcades. o Superior central nodes: located along the proximal part of the SMA. Efferent lymphatic vessels from the mesenteric lymph nodes drain to the superior mesenteric lymph nodes. Lymphatic vessels from the terminal ileum drain to the ileocolic lymph nodes Innervation Sympathetic inputs from T8-T10 o Reach the superior mesenteric nerve plexus through the sympathetic trunks and thoracic abdominopelvic (greater, lesser, and least) splanchnic nerves. o Sympathetic stimulation: ↓ peristaltic and secretory activity of the intestine Acts as a vasoconstrictor, reducing or stopping digestion and making blood (and energy) available for “fleeing or fighting.” Parasympathetic from posterior vagal trunk o Parasympathetic stimulation : ↑peristaltic and secretory activity of the intestine Restoring the digestion process following a sympathetic reaction. The small intestine also has sensory (visceral afferent) fibers o nsensitive to most pain stimuli, including cutting and burning o Sensitive to distension that is perceived as colic (spasmodic abdominal pains or “intestinal cramps”). Ileo-caecal junction The terminal ileum enters the cecum obliquely and partly invaginates into it. The ileal orifice enters the cecum between ileocolic lips The folds that meet laterally forming ridges called the frenula of the ileal orifice The orifice is usually closed by tonic contraction, however, appearing as an ileal papilla on the cecal side The papilla probably serves as a relatively passive flap valve, preventing reflux from the cecum into the ileum as contractions occur to propel contents up the ascending colon and into the transverse colon Blood supply SMA gives off the ileocolic branch ileal branch supply the junction Venous drainage Veins follow the arteries Histology of the Jejunum & Ileum Consists of: Duodenum Jejunum Ileum Digestion and absorption is enhanced by: • • • • Length (4-6m) Circular folds of mucosa and submucosa=plica circulares Fingerlike projections =villi Invaginations of mucosa between villi= Crypts of Liberkühn Intestinal villi Mucosa • Epithelium (four types of cells): o Absorption cells/Enterocytes: (90%) Simple columnar epithelium -microvilli (absorption) o Goblet cells (10%) Mucin secretion o Enteroendocrine/ Paneth cells: (0,5%) Secretes antimicrobial substances o Endocrine cells (similar to stomach) and stem cells Lamina propria • • • • • Central part of villus “Makes the villi stand up” Loose connective tissue: collagen + elastic fibers Vascular + lymphatic network: (Lacteal-blind ending lymphatic capillary) Smooth muscle fibers: from muscularis mucosae (intermittent contraction) Lymphocyte infiltration: o Individual cells (plasma, eosinophils + lymphocytes) o Peyer’s patches=lymphoid aggregates (ileum) o GALT structures Layers of crypts of Lieberkühn 1. Epithelial layer • • Columnar epithelial cells Stem cells o Base of gland • • • Paneth cells o Base of gland o Appear acidophilic o Produce lysozyme (bactericidal/controls intestinal flora) Goblet cells Enteroendocrine cells 2. Muscularis mucosae • Inner circular + outer longitudinal smooth muscle 3. Submucosa • • Loose connective tissue Brunner’s glands-open into the bottom of the crypts of Lieberkühn-zymogen and mucous secretion 4. Muscularis externa • Inner circular and an outer longitudinal smooth muscle 5. Serosa A very low magnification of the duodenum demonstrating the layers. 1. Mucosa 2. Submucosa 3. Muscularis externa 4. Brunner's glands 5. Muscularis mucosae 6. Plica circularis A higher magnification of the structures of the mucosa and submucosa. 1. Mucosa 2. Surface of duodenum 3. Submucosa 4. Mucinous glands of Brunner 5. Crypts of Lieberkuhn that invaginate from surface 6. Villi that extend from surface A high magnification of the structures of the duodenum. 1. Villus 2. Simple columnar epithelium (enterocytes) 3. Surface of duodenum 4. Muscilaris mucosae 5. Lumen of Crypt 6. Crypts of Lieberkuhn that invaginate from surface 7. Lamina propria A very high magnification of a part of a villus demonstating the structures. 1. Villus 2. Goblet cells 3. Connective tissue of the lamina propria 4. Simple columnar epithelium A high magnification of the secretory ducts of Brunner's gland. 1. Villi 2. Crypts of Lieberkuhn 3. Secretory units of Brunner's gland 4. Secretory duct of Brunner's gland opening into the bottom of a crypt of Lieberkuhn 5. Muscularis mucosae that are interrupted by secretory ducts 6. Surface of duodenum A high magnification of the secretory units of Brunner's gland. 1. Crypts of Lieberkuhn 2. Muscularis mucosae 3. Mucinous secretory units 4. Submucosa A very low magnification of a section through the ileum demonstrating the different layers and structures. 1. Mucosa 2. Villus 3. Muscularis externa 4. Submucosa 5. Ileum surface A higher magnification of the ileum demonstrating structures of the mucosa. 1. Mucosa 2. Lamina propria 3. Simple columnar epithelium 4. Surface of ileum 5. Submucosa 6. Muscularis externa 7. Crypt of Lierberkuhn 8. Muscularis mucosae A very high magnification of the ileum epithelium. 1. Lamina propria 2. Simple columnar epithelium 3. Microvilli 4. Goblet cell 5. Enterocyte 6. Basement membrane A very high magnification of the outer layers of the ileum. 1. Submucosa 2. Mucosa 3. Muscularis mucosae 4. Serosa 5. Longitudinal smooth muscle layer 6. Sirkulêrverlopende gladdespierlaag 7. Mesothelium A high magnification of a Peyer's patch in the ileum. 1. Submucosa of a plica circulares 2. Peyer's patch 3. Germinal center Physiology - Small Intestine Length of small intestine ~ 300 cm Length of colon ~ 80 cm However, the effective functional surface area of the small intestine is ~ 600 fold greater as a result of villi and microvilli. The small intestine and colon are anatomically and functionally distinct: o Villi are present in the small intestine, but absent in the colon. o Nutrient digestion and absorption take place in the small intestine, but not the colon. Functions of small intestinal epithelium: NB!!!! Nutrient digestion o Small intestine has enzymes (lactase) to digests disaccharides monosaccharides Nutrient absorption Fluid and electrolyte absorption and secretion: o The small intestine absorbs ~ 7-8 L of fluid per day o Dietary intake=1-2L per day o Salivary, gastric, pancreatic, biliary and intestinal fluid= 6-7 L per day Barrier and immune defence: synthesizes and secretes IgA Synthesis and secretion of proteins: Apolipoproteins Hormone production of several bioactive amines and peptides. o The intestine is a large endocrine organ—produces several amines and peptides that serve as paracrine and endocrine mediators of intestinal function. No precise anatomic characteristics separate the duodenum, jejunum and ileum. However, certain nutrients are absorbed exclusively in specific areas of the small intestine: o VitB12 and bile acids in terminal ileum NB! Disorders of Absorption From a clinical point of view Absorption can be increased or decreased. NOTE: Ulcerative colitis prevented by smoking Chron’s if you smoke you automatically get an another attack Increased Only 2 clinical conditions lead to increased absorption NB! o Hemochromatosis: Increased absorption of iron o Wilson`s disease: Increased absorption of copper Decreased Specific malabsorption syndromes: Example is decreased vitamin B12 absorption in the terminal ileum due to absence of intrinsic factor or ileal disease. Most NB localised malabsorption syndrome: NOTE: NB!! Local syndrome specific presentation General syndrome general presentation Terminal ileum: Crohn`s disease Resection: o Decreased absorption of vitamin B12 o Decreased absorption of bile acids. Decrease in bile acid pool. o Need bile acids for fat absorption o No bile acids, no fat absorption o No fat absorption, no absorption of fat soluble vitamins: A, D, E, K VitA deficiency: Blindness VitD deficiency: Osteopenia, fractures VitE deficiency: Neurological disease VitK deficiency: Bleeding tendency Generalised malabsorption Usually associated with steatorrhea–an increase in stool fat excretion > 6 % of dietary intake. This can be due to pancreatic or small intestinal disease Pancreatic causes Hereditary (atrophic, agenesis) Cystic fibrosis Chronic pancreatitis Resection After severe acute pancreatitis Small intestinal causes Crohn`s disease Celiac`s disease Whipple`s disease Amyloidosis Lymphoma Scleroderma Vascular insufficiency Radiation Blind loop syndrome Bypass surgery Resection How to you distinguish between the two D-Xylose absorption test to assess the integrity of the small intestinal mechanism of absorption. Fecal elastase, fats to assess efficacy of digestion (pancreatic) Physiological presentation of malabsorption: Chronic diarrhea (usually with steatorrhea) Weight loss Osteoporosis (vitD) Bleeding tendency (vitK) Blindness (VitA) Neurological / peripheral neuropathy (vitE) VitB12 malabsorption o True pernicious anemia (pernicious = destructive) o Ileal disease o Anaemia o Posterolateral sclerosis of spinal cord o Dementia o Jaundice due to haemolysis Physiology - Colon The colon prepares waste material for controlled evacuation. Colonic mucosa dehydrates the stool. This decreases daily fecal volume from 1000 to 1500 ml delivered from the ileum to 100 to 200 ml expelled from the rectum. Dense bacterial colonization in the colon: o This ferments undigested carbohydrates and short chain fatty acids. Small bowel obstruction Normal motility: electrical activity Slow waves – pacesetter potentials Spike discharges – contractile potentials Small bowel contractions o Ring contractions o Peristaltic contractions Ileocaecal junction NOTE: Dysentery blood in stools (only Colon) Introduction Most common surgical disorder Barrier to aborel progress Mechanical/dynamic o Simple: lumen only o Complicated (strangulated): compromised blood supply Non-mechanical/adynamic (ileus) o Neurogenic failure o No barrier to progress of contents o Poor peristalsis o Gas throughout the bowel o Non-operative management Causes Mechanical obstruction A BIG CHAV Annular pancreas Bezoars Intussusception very common in children Gall stone ileus Carcinomatosis Hernia Adhesions o Tough fibrous connective tissue o Constricting bands o Congenital or acquired Previous surgery Inflammation Infection o Accounts for most cases (50-70%) Volvulus Adynamic obstruction Peritonitis Mesenteric (vascular) occlusion Pelvic fracture Retroperitoneal haematoma Metabolic disorder o DKA o Hyponatraemia o Hypokalaemia o Uraemia PM PRM Bezoars Accumulation of hair or vegetable matter or a combination of the 2 which reduces nutritional absorption Can form a complete cast of the stomach and leads to malnutrition Usually seen in females who eat their hair and it remains undigested Dx through barium examination Tx with surgical removal through gastrostomy “Repunzel syndrome” Pathophysiology Reactive hyperperistalsis bowel sounds increase Luminal distention o Gas o Fluid from GIT Bacterial fermentation Oedema & mural transudation Volume contraction Clinical features Pain Distension Vomiting Constipation/obstipation X-ray features Bowel sounds Tenderness Temperature Management Nasogastric suction IV fluids Correction of electrolytes Monitoring o Hydration o Electrolytes o Blood gas – pH & HCO3 o Pain & tenderness o WBC o Free intra-peritoneal gas Removal of cause Surgery o Metabolic derangements o Evidence of strangulation/ischaemia o Peritonitis o Non-resolution o Hernia o Cancer Infective and malabsorptive diarrhoea Diarrhoea The means the stool has: Increased frequency, volume of stool Decreased consistency Children Numerous episodes first 5 years of life Most infectious and self limiting Can be associated significant complications and mortality Other o Acquired or inherited disorders of digestion and absorption o Motility disturbances o Drugs o Food intolerances Divided into: Chronic and acute ACUTE GASTROENTERITIS Denotes infections GIT caused by bacterial, viral or paracytic infections Many food-borne illnesses Most common manifestation vomiting and diarrhoea Associated systemic features abdominal pain, fever The problem Diarrheal disorders 18% childhood deaths Global mortality declining, overall incidence of diarrhoea remains the same 3-19% acute diarrhoea – persistent Up to 50% of diarrhoea deaths due to persistent diarrhoea Causes of Acute Diarrhoea CANCER Bacteria Salmonella Shigella Staphylococcus Aureus Vibrio cholera Yersinia enterocolitica Campylobacter jejuni E coli Clostridium Difficile Viruses Parasitic infections Protozoa Cryptosporidium Entamoeba Hystolytica Giardia Lamblia Microsporidium Isospora Helminths Strongyloides stercoralis Trichuris trichura Schistosoma Trichinella Caliciviruses Astroviruses Noroviruses CMV Enteric adenoviruses Rotavirus HSV HIV Differences in clinical presentation? Viral Bacterial Example Season Rotavirus Winter months Shigella BUT Multiple pathogens isolated stool Summer – bacterial contamination Age Presentation 6-24 months of age Preceding respiratory symptoms and profuse vomiting before onset diarrhoea Small intestinal mucosa damage o Invade mucosal cells tips vili o Shedding o disaccharidase deficiency ↓carbohydrate digestion (osmotic diarrhoea) o ↓reabsorption fluid and electrolytes < 6 months of age Abrupt onset diarrhoea, prominent CNS symptoms, high fever, no vomiting, blood and mucous in stools Adherence mucosal cell, damage Enterotoxin production o stimulate secretion large amounts fluid and electrolytes o Toxigenic E.coli, Vibrio cholera Cytotoxin production o Mucosal damage decreased absorptive surface Secondary inflammatory response ↑fluid secretion o Shigella dysentery type 1, campylobacter, enteroinvasive E.coli Mechanism Presentation: Dehydration The loss of body water leads to compensatory mechanisms: o Thirst o Antidiuresis o Catecholamine release of stress response Continuing water loss will result in failure of compensation, at which stage the patient enters a state of circulatory insufficiency. The clinical features of dehydration evolve in a continuous spectrum Features of dehydration Dry mouth and mucosa Reduced urine, sweat and tears Sunken eyes and fontanel Reduced skin turgor Acidotic breathing Restlessness to irritability Prolonged capillary filling time > 3 seconds Hypotension and shock, tachycardia Apathy to coma, convulsions What advice regarding dehydration? Prevent Replace amount that is lost in each vomit stool, +/- 15-30ml/kg additional to each feed ORS small frequent quantities, teaspoon Give as much as the child wants, 15-30 ml/kg/h Once stronger, alert, pass urine, want food : offer small feed Ongoing losses How to prepare home-made solution? - WRITE IT DOWN FOR MOM 8 teaspoons cane sugar ½ teaspoon salt 1 L cleanest water Presentation: Vomiting Why do you get vomiting in gastroenteritis? Impaired gastric emptying Starvation ketosis Local irritation and stimulation CNX Toxins – stimulation chemoreceptors vomiting center What do we do when we have child? Resuscitation: Shock medical emergency: IV fluids IV access : IV line, interosseus line Ringer’s / 0.9% Saline: isotonic fluids 20ml /kg bolus Reassess : another 10 – 20ml/kg bolus ½ Darrows 10-15ml/kg/h What are the complications Diarrhoea? Dehydration Shock o ARF o cerebral complications(hypoxic ischemia, cerebral vascular thrombosis), o NEC part of the intestine dies o Shock lung Acidosis and electrolyte disturbance Additional features o Fever o Convulsions o Ileus o Protein losing enteropathy o Necrotizing enterocolitis Dysfunction gut o ↓ digestion and absorption nutrients Complication: Convulsions Cerebral venous thrombosis Fever Hypoglycemia, hypo/hypernatremia Meningitis, encephalitis Cerebral edema rapid infusion hypotonic fluid Toxins Shigella etc Management of convulsion Prevent dehydration, continue feeds to allow maximal digestion and absorption Which electrolytes lost in diarrhoeal stool? NB! Sodium Potassium Chloride Bicarbonate Clinical features electrolyte disturbance? Hypokalemia: Weakness, hypotonia, paralysis, areflexia Cardiac arythmias Ileus Older child inability to hold up head Prolonged: renal tubular defects, reduced concentrating ability, interstitial nephritis Hyponatremia < 125 mmol/l : Nausea, vomiting, muscle twitching, lethargy < 115 mmol/l :Seizures and coma Hypernatremia Osmotic gradient water from intracellular to extracellular compartment- masked clinical signs dehydration Symptoms of intracellular water loss from brain cells depressed sensorium, irritability, convulsions Severity depends on degree and rate of rise of plasma osmolality Management and Advice Constituents Oral Rehydration Solution (ORS)? Advice regarding feeding? Maintaining nutrient intake important recovery Continue milk feeds Select solids easily digestable, bland and soft – starchy porridge, mashed banana Small quantities at a time, as frequently as tolerated Aim to restore normal intake 2nd-3rd day Additional therapies Zinc beneficial Antimotility agents like loperamide are contraindicated in children Similarly, due to the potentially serious side effects (lethargy, dystonia, malignant hyperpyrexia) of anti-emetics such as the phenothiazines they are of little value Careful oral rehydration is usually sufficient Ondansetron o Selective serotoninergic 5HT3 receptor antagonist o No sedative effect or extrapyramidal reactions Effective against placebo in relieving vomiting, reducing the need for intravenous fluids and decreasing hospitalization Antibiotic therapy If there is Dysentery Ciprobay 15 mg/kg/dose bd po x 3 days How to prevent gastroenteritis Hygiene and sanitation Exclusive breastfeeding 6 months Prevent malnutrition, early intervention Immunizations – Measles, Rotarix Chronic diarrhoea Passage of abnormal, unformed stools for 14 days or longer Developing countries most common following acute episode Other o Inherited abnormalities intestinal mucosa o Protein sensitisation o Anatomic abnormalities o Motility disturbances o Immune deficiencies o Chronic inflammatory disorders Definitions Most cases acute diarrhoea self-limiting Persisting diarrhoea > 7-14 days o Risk factors: formula feeding, < 3/12 at onset, malnutrition, immune suppression, associated illness, choice feeds during acute diarrhoea Chronic diarrhoea o 2-4 weeks without improvement o Related acute infective onset: persisting diarrhoea spectrum o Other cases: longstanding intestinal dysfunction, maldigestion and malabsorption Disorders associated chronic childhood diarrhoea Congenital Congenital Chloride diarrhoea Microvillus inclusion disease Epithelial displasia or Tufting enteropathy Auto-immune enteropathy Mucosal Damage and abnormalities Infections (viral, bacterial, protozoal) Post-enteritis enteropathy Celiac disease Protein-sensitive enteropathy Eosinophilic gastro-enteropathy Intestinal lymphangiectasia Immune deficiency HIV Primary immune deficiency Endocrine disorders VIP secreting tumours Zollinger-Ellison syndrome Carcinoid tumours Thyrotoxicosis Pancreatic disorders Cystic fibrosis Schwachman-Diamond Syndrome Congenital lipase deficiency Anatomic abnormalities Short bowel syndrome Stagnant loop syndrome Malrotation Metabolic and endocrine abnormalities Acrodermatitis enterohepatica Abetalipoproteinaemia Wolman’s disease Hypoparathyroidism Hyperparathyroidism Enzyme deficiencies Secondary disaccharidase deficiencies Adult-type lactase deficiency Congental disaccharidase deficiency Enterokinase deficiency Other Small bowel bacterial overgrowth 4. 1. 3. 2. 1. NB!! Persistence dehydrating diarrhoea and FTT after acute onset Risk factors Immune deficiency Onset of diarrhoea at less than 3 months Measles Malnutrition, Vit A and Zinc deficiency Lack of breastfeeding Environmental contamination with increased exposure to enteropathogens. Cases of persistent diarrhoea (episodes that began acutely but last for at least 14 days) account for 3-20% of all diarrhoeal episodes in children less than 5 years of age and up to 50% of all diarrhoeal deaths. Why post enteritis persisting diarrhoea? Persisting or new infection Malnutrition / HIV fail to clear infection Nosocomial infection overcrowded hospitals More than one pathogen o Specific pathogens associated o Cryptosporidium o Giardia Lamblia o EAggEC Small intestinal bacterial overgrowth o Unknown reasons o Damage mucosa o Deconjugation bile acids Small intestinal mucosal damage o Destruction villus mucosal cells disaccharidase deficiency carbohydrate malabsorption (as cannot absorb as o Osmotic agents bacterial action colon – aggrevate stool water losses o Damaged mucosal surfaces absorption intact foreign proteins 2 immunological reaction host further damage o Decreased intestinal absorptive surface nutrients and fluids Nutritional deterioration o Nutrient loss related severity diarrhoea and cumulative o >30g/kg/d nitrogen and energy loss too great for growth and tissue repair enterally alone o Vicious cycle diarrhoea progressive malnutrition aggrevates diarrhoea o Post enteritis enteropathy 2. Celiac disease (not done in class) Genetically determined autoimmune enteropathy Triggered exposure gluten Manifest at any age Wide range manifestations of variable severity Gluten Endosperm wheat, barley, rye High content glutamine and proline Resistant proteolytic enzymes GIT Gluten-derived gliadin peptides Clinical manifestations Classical celiac disease: intestinal symptoms o Diarrhoea +/- steatorrhea o Constipation o Anorexia o Vomiting o Abdominal pain o Abdominal distention o Weight loss o Failure to thrive Atypical Symptoms Iron deficiency anemia Rachitis, osteoporosis, dental enamel hypoplasia Peripheral neuropathy, epilepsy, irritability Short stature, delayed puberty, secondary hypoparathyroidism Dermatitis herpetiformis, aloplecia areata, erythema nodosum Ideopathic pulmonary hemosiderosis Infertility, adverse pregnancy outcome, menstrual abnormalities Diagnosis Intestinal biopsy gold standard Stepwise approach o High degree clinical suspicion o Age appropriate serological testing Screening o Symptoms o First degree relative o Associated diseases All testing on gluten containing diet GFD as diagnostic tool inappropriate Which antibodies are celiac specific? Endomysial antibody (EMA) Transglutaminase 2- specific antibody (anti-TG2) Deaminated gliadin-specific antibody (anti-DPG) 3. Non-dehydrating diarrhoea, FTT, appetite maintained (not done in class) Exocrine pancreatic disorders Good/increased appetite, bloated abdomen, foul smelling diarrhoea, undigested food Cystic fibrosis most common disorder F-elastase Sweat test Other: Schwachman, Diamond syndrome 4. Diarrhoea with normal hydration and nutrition (not done in class) Motility disturbances, normal digestion and absorption Toddler’s diarrhoea – Healthy child – 6m-4y – Episodically – Never at night, progressively more loose stools later day – Family history bowel disturbance Normal growth, physical exam, u+stool MCS, ESR, FBC Reassurance Diarrhoea in adults Definition 3 or more bowel movements per day are considered to be abnormal o Weight - above 200g/day o Consistency - loose/watery OR A CHANGE FROM USUAL PATTERN Secretion is abnormal, not absorption Pathophysiology and mechanism Is usually but not always a protective response to intestinal conditions Usually is due to excess of stool water rather than a decrease in the water-holding capacity of faecal solids o Implying an abnormality in water transport within the gut o Normally, the small intestine and colon absorb 99% of total water in transit Types of diarrhoea Osmotic water Disappears with fasting Cessation of ingestion of the offending substance solves NOTE: electrolyte absorption is not impaired in osmotic diarrhoea; thus, electrolyte concentrations in stool water may be quite low Ingestion of poorly absorbed account for most osmotic diarrhoeas: o cations and anions Magnesium sulfate Magnesium phosphate o absorbed sugars or sugar alcohols Mannitol Sorbitol (chewing gum!) Secretory Has many causes, the driving force for this is always: o either net secretion of chloride or bicarbonate o inhibition of net sodium absorption Most common causes by far is infection Enterotoxins from a host of infectious agent o Primarily bacteria but also parasites and virus o Interact with receptors modulating intestinal transport and lead to increased anion secretion Other peptides o Produced by endocrine tumours VIP Calcitonin o Released from subepithelial neurons and inflammatory cells cause secretory diarrhoea by stimulating secretion by epithelial cells Complex diarrhoea Cases of pure secretory or pure osmotic diarrhoea are uncommon Complex pathophysiology also may be observed in malabsorption syndromes and functional disorders Clinical Classification Time course (acute vs. chronic) Acute diarrhoea (<4 weeks) usually are due to infectionsmost self-limiting/ easily treated Chronic (>4weeks) Volume (large vs. small) Pathophysiology (secretory vs. osmotic) Epidemiology Stool characteristics (watery vs. fatty vs. inflammatory) Chronic watery diarrhoea o Infrequently due to ingestion of osmotically active substances that are poorly absorbed by the intestine (osmotic diarrhoea) o more commonly due to conditions causing secretory diarrhea Chronic inflammatory diarrhoeas o comprise a diverse group of infectious bacterial infections, such as: o Tuberculosis, yersinosis o Clostridium difficile– associated colitis viral infections that ulcerate such as; o cytomegalovirus ,herpes simplex invasive parasitic such as strongyloidiasis idiopathic inflammatory neoplastic processes. o Stools are characterized by the presence of mucus and pus associated with ulceration of the mucosa. Such as in ulcerative colitis and Crohn's disease Fatty diarrhoea o Malabsorption due to mucosal diseases celiac sprue Whipple's disease , typically produce fatty diarrhea. Short bowel syndrome or post resection Mesenteric ischemia may impair absorption of fat, but weight loss is often attributed to sitophobia ("fear of eating") due to postprandial pain o Maldigestion due to pancreatic exocrine insufficiency inadequate duodenal bile acid concentration produces steatorrhea. Management Dehydration Nutrition Fine tuned to The cause o History - travel o Physical examination o Laboratory investigations Chem Path - Lab evaluation of diarrhoea Laboratory evaluation Acute diarrhoea = production of loose stools +/- increased stool frequency for <2 weeks (chronic if >4 weeks) Lab evaluation unnecessary for mild acute diarrhoea Indicated for severe diarrhoea with fever, dysentery or if diarrheal illness is prolonged (>14 days) Tests may include UEC, FBC, stool M,C+S and investigation for parasites Lab tests for chronic diarrhoea FBC, ESR, UEC, Ca2+, Mg, PO4, albumin, TP Folate, vit B12, iron, LFT’s Stool analysis o MC+S for ova/parasites/leucocytes o Faecal occult blood Positive result suggests IBD, or neoplasm o Faecal fat Excessive fat excretion suggests malabsorption or maldigestion o Faecal osmolality, Na+, K+ to calculate osmotic gap OG = Osmolality – 2([Na+] + [K+]) >125 suggests osmotic diarrhoea <50 suggests secretory diarrhoea o Faecal pH <5.6 suggests carbohydrate malabsorption o Faecal laxative screening Magnesium, phenolphthalein Chronic secretory diarrhoea o Exclude bacterial/parasitic infection o Gastrin, VIP, 5HIAA, metanephrine, histamine, TSH o Test for bacterial overgrowth only in selected patients Chronic osmotic diarrhoea o Most osmotic diarrhoea without steatorrhoea is due to poorly absorbable CHO or Mg salts o In suspected lactose intolerance do hydrogen breath test or measure lactase in a mucosal biopsy o Investigate possibility of sorbitol or fructose ingestion Chronic inflammatory diarrhoea o Small bowel follow-through and sigmoidoscopy/colonoscopy with biopsies for evaluation of IBD o Stool culture to identify infectious causes of inflammation Chronic fatty diarrhoea o Assess pancreatic exocrine function by faecal elastase o Small bowel biopsy and aspirate of contents for culture Special tests – CHO malabsorption Hydrogen breath tests o Bacterial overgrowth, CHO malabsorption o Hydrogen measured in exhaled air in fasting pt o Hydrogen measured in exhaled air after giving test sugar D-Xylose Absorption Test o Xylose is a five-C sugar that is absorbed in the small intestine and does not require intraluminal digestion o Used to differentiate between mucosal disease (in which absorption will be decreased) and pancreatic disease Special tests – fat malabsorption Faecal elastase o Random stool sample o No need to discontinue enzymes o Good sensitivity for moderate/severe pancreatic insufficiency Faecal fat measurement o Diet containing 50-150g fat per day for 3d prior to and during collection of stool for 72h into weighed container o Sample homogenised, fats extracted and measured 14C-triolein breath test o Indirectly assesses pancreatic lipase activity in intestine o 14C-labelled triglyceride triolein is ingested by fasting patient o 14C-labelled CO2 is measured in exhaled air hourly for 6 hours thereafter Special tests – Coeliac disease Sensitivity to gluten (gliadin) in wheat/other cereals Inflammation of SI with malabsorption Measure antibodies while on gluten-containing diet o IgA endomysial antibody (IgA EMA) o IgA tissue transglutaminase antibody (IgA tTG) o Anti-gliadin antibodies no longer advised With selective IgA deficiency, do IgG tTG or EMA At least 3 duodenal biopsies to confirm diagnosis >99 % of pts have HLA DQ2 and/or DQ8 Special tests – Schilling test Stage 1: o o Stage 2: o Stage 3: o Stage 4: o o Labelled B12 p.o. and unlabelled B12 IM as flushing dose Measure labelled vit B12 in 24h urine collection Give IF with vit B12 – will normalise in pernicious anaemia Give pancreas extract with vit B12 – will normalise in pancreatic insufficiency Repeat stage 1 after course of antibiotics – will normalise in bacterial overgrowth If all 4 stages abnormal – ileal disease Virology Introduction 5 billion episodes of diarrhoeal disease globally every year Improved public health infrastructure has led to ↓ frequency of bacterial & parasitic causes of gastroenteritis BUT viral causes have not declined in an equal fashion Etiologic agents Viral gastroenteritis pathogens all infect the intestine & induce gastrointestinal symptoms → shared ability NOT to be confused with enteric viruses (which infect the intestine but predominantly produce manifestations at extraintestinal sites) e.g. enteroviruses, echoviruses, coxsackieviruses, polioviruses, Hepatitis A and E The medically important causes of viral gastroenteritis are: o Rotavirus o Astrovirus o Norovirus o Enteric Adenovirus Epidemiology Transmission Faecal-oral Person-to-person Contaminated food and water Risk groups Increased exposure to virus Increased susceptibility e.g. younger age or immunocompromised individuals Clinical manifestations Disease manifestations are clinically similar: o Watery diarrhea → usually without blood/mucus Diarrhoea ranges from mild to severe o Nausea & vomiting o Abdominal cramps o May be complicated by dehydration Major differences are in onset and duration of symptoms Gastroenteritis viruses ROTAVIRUS Family Genus Virus Transmission Incubation Duration Prevention General Season Outbreak At risk Vaccines Who should get the rotavirus vaccine? Efficacy Reoviridae Rotavirus Rotavirus – faecal-oral – ?respiratory droplets short: 2 - 3 days 4-7 days – Hygiene – Vaccine Most common cause of viral infantile diarrhoea in developing countries Highly infectious – 1012 per g faeces – Resistant Autumn → winter – nosocomial – child care centres – homes for elderly Children 6months 2years – Rotarix - Attenuated human rotavirus vaccine derived from a G1P[8] strain • Provides partial cross-protection against most other serotypes • Included in South African EPI schedule – RotaTeq - Pentavalent human-bovine rotavirus reassortant vaccine, contains only one G-type or Ptype protein from human strains—G1, G2, G3, G4, and P[8] – WHO recommends universal immunisation of infants – RotaTeq: 3 oral doses at 2, 4 & 6 months of age • Catch-up: vaccination not to be initiated after 15 weeks of age • Give last dose before 8 months of age in USA, 32 weeks in SA – Rotarix: 2 oral doses at 2 & 4 months (6 and 14 weeks in SA) • Catch-up: Initiate between 6 and 14 weeks of age, complete by 24 weeks – HIV infected children? • Rotarix found to be safe & immunogenic when administered to HIV+ infants • If symptomatic, weigh risks & benefits – Both vaccines protect (NOT 100%) against severe rotavirus gastroenteritis & hospitalisation for rotavirus gastroenteritis – Some cross-protection demonstrated against types not included in vaccine ADENOVIRUS Family Genus Virus Adenoviridae Mastadenovirus Human adenovirus Transmission Incubation Duration Season Outbreak At risk Vaccines – 1011 per gram faeces – Faecal-oral – Person-to-person 7-8 days - 6-7 days - Prolong excretion Midsummer peak – Nosocomial – Child care centres Children <2years NONE ASTROVIRUS Family Genus Virus Transmission Incubation Duration Season Outbreak At risk Vaccines Astroviridae Astrovirus Human astrovirus – 1011 per gram faeces – Faecal-oral – Person-to-person – Faecally contaminated food and water 2 - 3 days – 12 h – 3-4 days – Prolonged excretion Winter – Nosocomial – Child care centres – Schools/old age homes – 5 - 7% South Africa – Children < 7 yrs – Usually less severe than rotavirus NONE CALICIVIRUSES Family Genus Virus Epidemiology Transmission Incubation Duration Season Outbreak Caliciviridae Norovirus Sapovirus limited/no cross protection within genera USA: Norovirus now most common cause of gastroenteritis among young children following rotavirus immunisation – Most common cause of epidemic viral gastroenteritis among all ages – Extremely stable virus • Resist heating to 60ᵒC • Resist chlorine disinfection – 106 per gram faeces – Faecal-oral – Person-to-person – Aerosols of vomitus: high rate of secondary spread – Faecally contaminated food and water 1-3 days 1-4 days – None – Temperate climates: winter peak? – Common source (e.g. shellfish) – All age groups affected – Nosocomial – Child care centers – Schools/old age homes – Cruise ships – Vomiting more prominent, more likely to be the sole presenting symptom compared to other types of viral gastroenteritis NONE Clinical pic Vaccines Lab Diagnosis Viral isolation o Isolation difficult: NOT used for routine diagnosis Serology o Available for some viruses: NOT used for routine diagnosis Management Supportive care o Rehydration o Anti-motility drugs not recommended Isolation or patient cohorting Preventative measures o Hand washing o Appropriate diaper disposal Physiologic complications of chronic vomiting Face Subconjunctival hemorrhage Epistaxis Due to chronic retching Dental Dental erosion Cheilitis Mucositis of hard palate and throat (long term can cause pre-malignancy) Parotid gland Parotid gland hypertrophy (Known as sialadenosis) Exact cause unclear Larynx Hoarseness Oedema Telangiectasia Polyp formation Lower Oesophageal Sphincter Chronic GORD o Due to laxity of LES due to chronic retching Heartburn Odynophagia Stricture formation o Mucosal tears—Mallory Weiss syndrome Perforation of oesophagus—Boerhaave`s syndrome Barrett`s oesophagus adenocarcinoma Elevated amylase levels Hyperamylasemia Secreted by salivary glands Renal Volume depletion Resultant hyperaldosteronism (zona granulosum) o Secondary vs primary (tumour) hyperaldosteronism o Oedema Formation Oedema formation can result from chronic vomiting due to continued up regulation of aldosterone levels This leads to hypokalaemia and alkalosis o Also potassium and acid loss in vomitus o Effects of hypokalaemia Muscle weakness Cardiac arrhythmia Vomiting and Gastric Outlet Obstruction Vomiting and regurgitation Vomiting = active process where stomach content is actively expelled Regurgitation associated with o Achalasia o Pouches o Hiatus hernia Gastric outlet obstruction Caused by PUD most common Acute: edema in pyloric region o Treat conservatively (Give nasogastric tube and treat with IV fluids) Chronic: fibrosis o May need surgery Other: o Hypertrophic pyloric stenosis (infants) o Gastritis o Antral stenosis (Acid ingestion) o Gastric cancer Pathophysiology Stomach secreted acid (HCl) which is lost by vomiting Develops alkalosis (increased pH) Metabolic cause (loss of acid) Dehydration (loss of volume) Cells compensate (Potassium, hypokalemia) Results in: hypochloremic, hypokalaemic metabolic alkalosis Normal pH: 7.35-7.45 Henderson Hasselbach equation is used to determine pH o Mortality Alkalosis: pH>7.55 = 45% pH >7.65 = 80% Acidosis: pH <7 = 60% pH <6.9 = 100% Compensatory mechanisms Body compensates for acidosis (metabolic processes produce acids) …?? Commpensatory mechanisms o Buffers Bloodstream has HCO3, PO4 and albumin that can bind H+ (acidosis) H + HCO£ = H2CO3 = H20 + CO2 o o H + HPO4 = H2PO4 Respiratory Hypoventilation, increases CO2 pCO2 + H20 = H2CO3 = H+ HCO3 Increased HCO3 Renal Exchange H+ in tubule for K+, with increased K+ excretion (Hypokalemia) Reabsorb fluids for hypovolemia oliguria Vomiting or nasogastric suction Loss of HCL Generation of HCO3 Excretion of NaHCO3 in urine ECF contraction Renin will increase angiotensin II and aldosterone Excretion of K+: Kaliuresis Symptoms Non-specific Low K+ weakness, myalgia, ECG changes, hypoventilation Medical management PUD: o Reduced acid secretion: PPI, H2A o Empty stomach: nasogastric tube for drainage o Allow endoscopy and barium studies to confirm diagnosis] Endoscopy To establish Dx Identify specific cause Therapeutic …? Endoscopic balloon dilatation Safe and effective alternative in management..? Truncal vagotomy o Need drainage procedure because with paralyse pylorus! Finneys pyroplasty Heineke-mikulicz pyloroplasty Selective vagotomy Highly selective vagotomy o Only affects acid secreting parts of stomach o Does not affect pylorus o Recurrence rate quite high for PUD Problems with gastric outlet obstruction Chronic malnutrition Need food Give enterally (if feeding tube can be passed beyond obstruction) or paraenterally (TPN) Increased complications (Adverse effects) Surgical options Bilroth I: o Gastro-duodenostomy Bilroth II o Gastrojejunostomy o Attach stomach to jejunum (bypass duodenum) Roux – en-Y o Gastrojejunostomy o Attach jejunum to stomach and reattach duodenum to junum distally TUMORS OF THE SMALL BOWEL Benign and malignant tumours Benign Benign gist Adenoma Lipoma Hamartomas Hemangioma Malignant Adenocarcinoma Carcinoid tumor Malignant gist Lymphoma Introduction Small bowel neoplasms are rare. Only 5% of the all gastrointestinal tumors. Small bowel has rapid transit of luminal content and high turnover rate of epithelial cells which may minimize carcinogenic exposure. The content is alkaline, the level of IgA is high in the intestinal wall and the bacterial count is low. Epidemiology The mean age of the presentation is 62 years. The highest incidence of the cancer in the Maori of New Zealand and ethnic Hawaiians. AIDS CONTRIBUTED TO THE INCREASE OF LYMPHOMAS! (RSA) Duodenal tumours are the most common per unit area. Benign lesions are asymptomatic and identified at autopsy. 75% of symptomatic lesions that lead to surgery are malignant Aetiology Patients with Crohn’s disease and familial adenomatous polyposis are at higher risk for small bowel neoplasms. Mutations of the K-ras gene are commonly found. Risk factors include hereditary nonpolyposis colorectal cancer, Peutz-Jeghers syndrome, gluten sensitive enteropathyand biliary diversion (e.g. previous cholecystectomy). Smoking, heavy alcohol consumption and consumption of red meat or salt-cured foods may contribute to small bowel cancers. Pathology Benign lesions (polyps) are 10 times as common as malignant ones. Lymphoma is now the most common primary malignant tumor of the small bowel. Diagnosis Correct preoperative diagnosis is made in only 20%. CT enteroclysis has accuracy of about 90%. Flexible endoscopy is useful for the duodenum and terminal ileum. Push enteroscopy may take up to 8 hours to perform. Capsule endoscopy –swallowed radiotelemetry capsule that transmit images of the bowel is now more widely available. Plain films ( X-Ray ) may confirm the presence of an obstruction. It doesn’t tell us the nature of lesion. ( useless ) Angiography of value for vascular lesions. CT abdomen useful for GIST and staging of malignant cancers. Despite the sophisticated imaging and fancy diagnostic modalities, diagnosis often made at laparotomy done as an elective or as an emergency procedure. (? diagnostic laparotomy ) BENIGN TUMORS Types GIST Benign GIST is the most common tumor that produce symptoms. GIST-Gastrointestinal stromal tumors arise from the interstitial cell of Cajal, an intestinal pacemaker cell. On the microscopy: well-differentiated smooth muscle cells. GIST may grow intraluminal, intramural and extramural. These stromal tumors can cause bowel obstruction and bleed. If mitotic count low (<2) imply benign disease. If mitotic count > 5 per 50 HPF or size > 5cm imply malignancy. Adenoma Adenoma is the most common tumor on autopsy (asymptomatic) Adenomas are benign polyps and may be true , villous and Brunner gland adenomas. Adenomas are usually solitary polyps and may cause symptoms by intussusception or bleeding. Familial adenomatous polyposis is characterized by multiple intestinal and colonic polyps, osteomas and subcutaneous fibromas. The polyps are true neoplasms and there is a potential for periampullary duodenal cancer and colonic cancer. Lipoma Hamartomas Hamartoma may be solitary in patients who are free of associated anomalies. They are multiple in 50% of the cases. 10% of Hamartomas take part in Peutz-Jeghers syndrome a familial disorder characterised by diffuse gastrointestinal polyposis and mucocutaneous pigmentation. The classic pigmented lesions are small, 1 to 2-mm, brown or black spots located in the circumoral region of the face, buccal mucosa, forearms, palms, soles, digits and perianal area Hemangioma Hemangiomas are developmental malformations consisting of submucosal proliferation of blood vessels. They can occur at any level of the gastrointestinal tract. Patients with Turner’s syndrome are likely to have hemangiomas of the intestine. The most common symptom is intestinal bleeding. Angiography and Tc-red blood cell scanning are useful for the diagnosis. Resection is recommended. Endometriosis can implant on the small bowel Clinical findings Symptoms are often vague and nonspecific, dyspepsia, anorexia, malaise and dull abdominal pain (often intermittent and colicky). Most are asymptomatic. Benign small bowel tumors are the most common cause of the intussusception in adults. Haemorrhage is the next most common symptom. Usually occult bleeding. Rarely hematemesis and hematochezia. Treatment Surgical treatment is almost always indicated as the diagnosis cannot be made without microscopic examination of the specimen. Also segmental resection and primary anastomosis is needed to prevent complications. Small lesions may be resected by enterotomy. The search should be done for other lesions as they could be multiple. MALIGNANT TUMORS Types Adenocarcinoma Often asymptomatic or causes only minimal symptoms. They may produce the typical constricting apple-core lesions. Later may present with pain, weight loss, bleeding, anaemia and obstruction Metastases are present in 80% of cases at the time of operation. Wide segmental resection of bowel and adjacent mesentery is done when possible. 5 year survival is 25%. Carcinoid tumor They arise from enterochromaffin cells and may be associated with multiple endocrine neoplasia (MEN) type1 and 2. it produce serotonin, substance P, neurotensin, gastrin, Somatostatin, motilin, secretin and pancreatic polypeptide. 80% of those larger than 2 cm have metastatic spread. It presents with obstruction, pain, bleeding or the carcinoid syndrome. 10% of patients presents with carcinoid syndrome and others develop it later. Carcinoid syndrome It consists of cutaneous flushing, diarrhoea, bronchoconstriction and right sided cardiac valvular disease due to collagen deposition. Biologically active substances secreted by carcinoids are usually inactivated in the liver, so there are no above mentioned symptoms. Hepatic metastases or ovarian or bronchial carcinoids release these compounds directly into the systemic circulation, where they produce symptoms. Serotonin production is causing diarrhoea. Asthmatic attacks are usually observed during the flushing symptom. Bradykinin and serotonin are implicated. Serotonin is metabolised in the liver to the inactive 5-hydroxyindoleacetiacid (5-HIAA). Elevated urinary levels of 5-HIAA is the diagnostic hallmark of carcinoid syndrome. Chromogranin A is elevated in plasma and it is very useful in making the diagnosis. CT scan and Somatostatin receptor scintigraphy are useful localisation studies. Octreotide/ Somatostatin inhibit release of gastrointestinal hormones. It relieves flushing, wheezing and diarrhoea. Carcinoid tumor is regarded as a “malignant neoplasm in slow motion” and it should be resected aggressively. Isolated hepatic metastases should be resected. 5-year survival after resection is 70%. Median survival from the histologic diagnosis is 14 years. Malignant GIST GIST mostly arise from muscularis propria and grow extramurally. It is greater than 5 cm usually. Indications for surgery are bleeding and obstruction. GIST spread hematogenously and into adjacent tissues. Segmental bowel resection is indicated. Tyrosine kinase inhibitor imatinib mesylate gives a lot of hope in treatment of GIST. Lymphoma It may involve small bowel primarily or as a manifestation of systemic disease. They are most commonly found in the ileum, where is the greatest concentration of lymphoid tissue. AIDS patients have increased risk of getting it. Symptoms are pain, weight loss, nausea, vomiting and change in bowel habits. Perforation occur in 25% of patients. Treatment is wide resection including regional lymph nodes, radiation and chemotherapy. INFLAMMATORY BOWEL DISEASE Crohn’s disease Definition Inflammatory condition of unknown etiology o Any portion of the GIT, mouth to the perianal area. o Transmural Distribution Oral Gastroduodenal ileum Colon Perianal Epidemiology of IBD Crohn’s Disease Ulcerative Colitis Incidence per 100 000 1-10 3-15 Prevalence per 100 000 20-100 50-80 Peak age of onset 15-30 2nd peak 50-80 15-30 Gender M=F Race Whites > Blacks Ethnic Jewish>Non-Jewish Smoking + CD & -UC Appendectomy Protective in UC Genetics Chromosome 16 (CD), 3,5,7,12,19 Presentation Fatigue Prolonged diarrhoea (NO BLOOD) Abdominal pain Fever Weight loss Physical signs o Failure to thrive in children and young adults o And others to discuss) Laboratory Full blood count U&E CRP LFT Serum B12 and schilling test Imaging investigations Structural Cause Patterns Could be normal Straight abdominal X rays Barium studies Endoscopy CT scans Histology in Crohn’s Granulomas – they tend to be deep so that an ordinary biopsy may be too superficial to expose them – NON CASEATING Complications and extraintestinal manifestations Local o Strictures o Fistulae o Abscesses o Ulceration No part of the body is spared! Extra- intestinal o Crohn’s uveitis o Crohn’s abscess CT o Crohn’s fistula o Episceleritis in IBD o Erythema Nodosum in IBD o Early Pyoderma gangrenosum o Pyoderma gangrenosum Management of Crohn’s Acute Severe - Steroids o IV steroids o Oral steroids o ASA Complications o Minimal surgery Ulcerative colitis Definition Inflammation of unknown origin limited to the mucosa layer of the colon. o Invariably involves the rectum. o Continuous. Terms in colitis Ulcerative proctitis Distal colitis or proctosigmoiditis Left sided colitis – not beyond splenic flexure Extensive colitis – not as far as cecum Pancolitis extends to cecum Presentation Rectal bleeding Fever Pallor Imaging Radiography Endoscopy What will be seen: o Ulceration o Lead pipe colon o Endoscopic evolution of ulcerative colitis o Contiguos ulceration Management - Acute Severe Inform surgeon on call High dose IV steroids for 5 to 7 days Monitor severity o Number of stools, fever, wbc, platelets Day 5 Cyclosporin No response or getting worse do not hesitate to involve surgery o In theory the condition is curable Usual Management Depends on severity Area of Involvement Patient response to different treatments and side effects Dealing with complications Management of left sided colitis Toxic mega colon Transverse colon 8-10cm High fever Pallor Dehydration MEDICAL/SURGICAL EMERGENCY Intensive therapy Management of severe pancolitis Complications Uveitis and episcleritis Erythema nodosum and pyoderma gangrenosum Arthritis large joints and ankylosing spondylitis (B27) Sclerosing cholangitis Lung disease, DVT Autoimmune hemolytic anemia Neoplasia in UC Pancolitis More than 8-10 years Crohn’s vs Ulcerative colitis CD involvement of small bowel Sparing of the rectum by Crohn’s Absence of gross bleeding in Crohn’s Presence of bothersome perianal disease in Crohn’s CD panmural with granuloma Drugs Steroid spairing drugs ASA Azathioprine Methotrexate Immunomodulatory drugs Antibody to TNF Other approaches Antibiotics o Metronidazole o Quinolones Probiotics Conclusion Long history of abdominal pain – think of Crohn’s Long history of bloody diarrhea – think of Ulcerative colitis Nuclear Medicine GIT Bleeding Massive haemorrhage in the lower GIT is defined as bleeding distal to the lig of trietz in excess of 30ml/hr Causes Diverticular disease Angiodysplasia Neoplasm Trauma Role of NM Diagnosis Localization Prognosis Radiopharmaceuticals SC Rapid clearance Good target-tobackground Liver and spleen mask bleed Bleeding rate 0.050.1ml/min Limited imaging time Labelling not a problem Technetium Tc-99m RBC Tc-99m Sulfur colloid (SC) Other - Tc-99m albumin, In111 RBC RBC In Intravascular space 2448hrs Poor target-to-background Less liver and spleen 0.1-0.5ml/min Intermittent bleeds - up to 24hrs Problem of labelling Technique -in vivo -Modified in vitro -in vitro Interventions Glucagon - smooth muscle relaxation thus the tracer moves as slow as possible Interpretation NOTE: true bleed it moves Focal uptake and changes shape Change position - anterograde. Retrograde motion Changes intensity Severity o Low - bleed seen after 1h , less intense density than the liver o High - early appearance, equal to or more dense than the liver False positive o Vascular neoplasm o Horse-shoes kidney o Varices o Accessory spleen o Vascular grafts o Ischemic bowel o Dilated abdominal aorta o Inflammation o AV malformation False negative o Barium enema o Small bleeds o Intermittent bleeding o Liver and spleen activity Merckel’s diverticulum Congenital remnant of omphalomesentric duct of the embryo In terminal ileum 25%-40% asymptomatic 50% bleed by 2years 60% with gastric mucosa - histology parietal cells Imaging Tc-99m pertechnectate - localizes in gastric mucosal cells Patient prep Fasting No Barium studies for 2 days Interpretation Focal uptake Increases with time of intensity False negative o Ba enema o Upper GI exam o Small Merkel’s diverticulum o o Ischemia or necrosis Obscured by urinary activity o o Strictures Death GE reflux Common by 2 months Complications o FTT o Pneumonia Imaging Tc-99m SC in milk feed Burp patient Stomach and thorax in FOV Chest statics Significant positives o Reflux over 15s+ o Seen late o Multiple episodes: Mild (<10), Mod (10-20) and Severe (>20) o Pulmonary aspiration Oesophageal transit Achalasia Diffuse oesophageal spasm Nutcracker oesophagus Imaging Tc-99m SC in 10ml water or milk ROI - upper, mild and lower oesophagus Time activity curves o Transit time <10s o Infants should be cleared by 3.4s ± 1s o 8-16years 4.6 ±1.9s Gastric emptying Imaging Tc-99m in liquid or solid male Liquid - exponential clearance Solids - lag period followed by liber disappearance o By 4hrs stomach should almost be empty o By 6hrs stomach should be empty Radiology: Small bowel obstruction Small bowel obstruction Mechanical obstruction No treatment: 60% mortality Treatment: 5% mortality Symptoms o Abdominal pain and cramps o Nausea o Vomiting o ↓ Stools (constipation) o ↑ High pitched bowel sounds Late signs. Absent bowel sounds due to fatigued bowel Common causes of obstruction • • Extrinsic – Adhesions – Hernia – Abscess – Masses (neoplasms – polyps) – Congenital malrotation: peritoneal bands rare Intrinsic – Inside lumen • Tumor • Gallstones • Foreign body • Intussusceptions – In the wall • Strictures • Inflammatory (Crohn’s) • tumors etc • Vascular insufficiency • Atresia or stenosis What to do • • • • • • History & clinical examination!!!! Abdominal radiograph (AXR) CT Scan Barium studies Small bowel follow through Enteroclysis Questions to answer when looking at AXR 1. 2. 3. 4. 5. 6. Is there obstruction or paralytic ileus? At what level? Partial / complete / closed loop? Cause? Is there strangulation? Is there a perforation? Common XR findings • • No distal gas – No gas in colon/rectum in complete obstruction String of pearls • • • • • Valvulae conniventes – Circular folds Central location Air fluid levels – caution Distended small bowel loops down to obstruction Lower obstruction: more loops tend to stack up as stepladder CT • • • • • Used more than barium Site and maybe the cause No need for oral contrast and differentiate a prolonged obstruction where bowel is dilated and atonic with abrupt site of narrowing For ileus where dilated continue into colon and no abrupt narrowing of bowel Small bowel faceses sign – No normally solid faeces in small bowel traps air and can be seen – Incomplete obstruction may not be clearly noted on CT and enteroclyses with CT may be the answer Causes of obstruction • • • • • • • Voluvulus – Closed loop obstruction where mesentery twists and bowel dilates (proximal and distal obstruction) Hernia – Can use CT but more clinical diagnosis Tumour Gall stone ileus – Gallstone can cause obstruction in ileum Bezoar – Organic body in the bowel Intusussception – Bowel within the bowel – Seen as coiled spring Adynamic ileus • Topic: To compare changes with that of Small bowel obstruction • Rö sign in adynamic ileus is retention of gas and fluid in dilated large and small bowel with ↓ or no bowel sounds • No demonstrable point of obstruction • Dilated stomach part of this complex – not seen in obstruction • Possible causes o Post surgery o Peritonitis o Electrolyte inbalance o Acute chest disease (MI or CCF) o Metabolic disorders o Medication • Variants o Pancreatitis o Appendicitis o Acute cholecystitis