CLINICAL PRIORITY ACCESS CRITERIA
advertisement
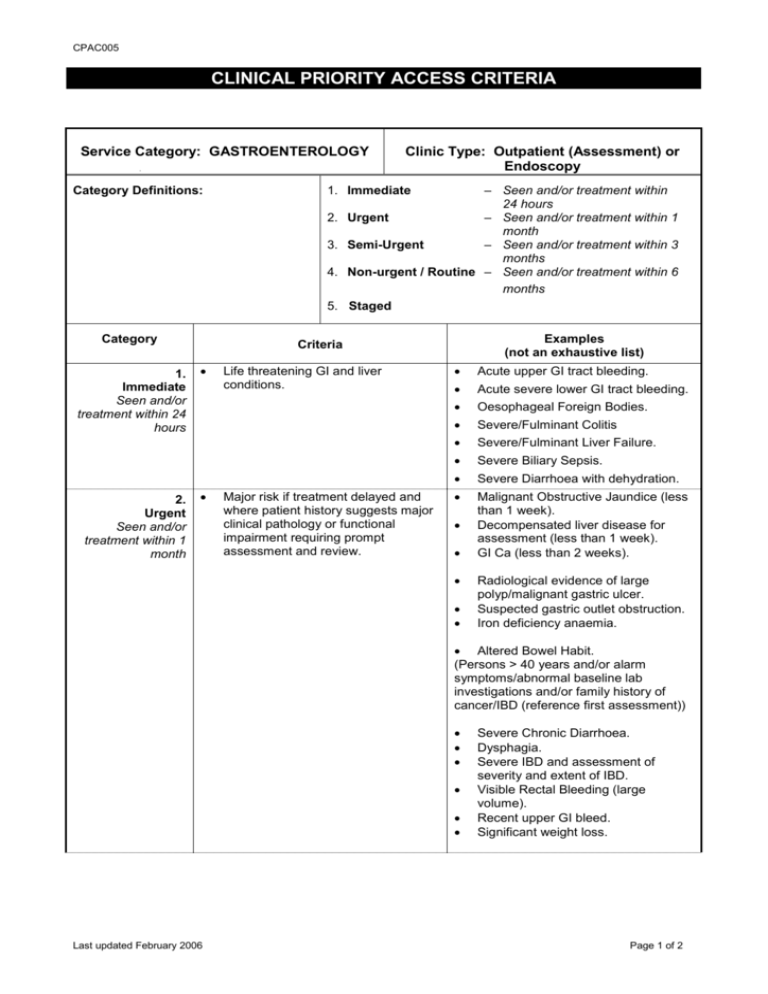
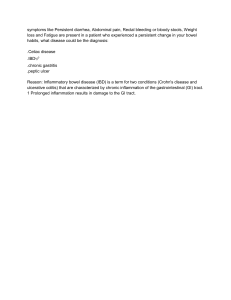
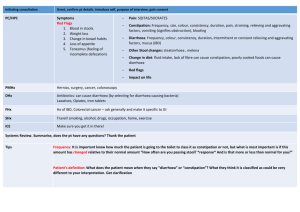
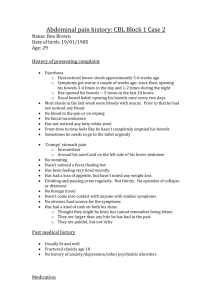
CPAC005 CLINICAL PRIORITY ACCESS CRITERIA Service Category: GASTROENTEROLOGY Category Definitions: 3. 4. 5. 1. Immediate Seen and/or treatment within 24 hours 2. Urgent Seen and/or treatment within 1 month – Seen and/or treatment within 24 hours Urgent – Seen and/or treatment within 1 month Semi-Urgent – Seen and/or treatment within 3 months Non-urgent / Routine – Seen and/or treatment within 6 months Staged 1. Immediate 2. Category Clinic Type: Outpatient (Assessment) or Endoscopy Examples (not an exhaustive list) Criteria Life threatening GI and liver conditions. Major risk if treatment delayed and where patient history suggests major clinical pathology or functional impairment requiring prompt assessment and review. Acute upper GI tract bleeding. Acute severe lower GI tract bleeding. Oesophageal Foreign Bodies. Severe/Fulminant Colitis Severe/Fulminant Liver Failure. Severe Biliary Sepsis. Severe Diarrhoea with dehydration. Malignant Obstructive Jaundice (less than 1 week). Decompensated liver disease for assessment (less than 1 week). GI Ca (less than 2 weeks). Radiological evidence of large polyp/malignant gastric ulcer. Suspected gastric outlet obstruction. Iron deficiency anaemia. Altered Bowel Habit. (Persons > 40 years and/or alarm symptoms/abnormal baseline lab investigations and/or family history of cancer/IBD (reference first assessment)) Last updated February 2006 Severe Chronic Diarrhoea. Dysphagia. Severe IBD and assessment of severity and extent of IBD. Visible Rectal Bleeding (large volume). Recent upper GI bleed. Significant weight loss. Page 1 of 2 CPAC005 3. Semi-Urgent Seen and/or treatment within 3 months 4. Non-urgent Routine Seem and/or treatment within 6 months 5. Planned / Staged Condition resulting in moderate, physical, social or economic disruption. Moderate functional impairment. Minimal functional impairment with minimal restriction of social and/or economic activity. To achieve optimal outcomes. Dyspepsia with / without alarm symptoms (see NOTE). Suspected malabsorption syndromes. Mild diarrhoea. Intermittent vomiting and/or weight loss. Screening for familial Cancer. Altered bowel habits with no alarm symptoms less than 40 years and no family history of colon cancer. Non-cardiac chest pain. Malabsorption. Suspected IBS. Family history of bowel cancer. Complex GI diagnostic problems. NOTE: Alarm symptoms: Anaemia, weight loss, anorexia and vomiting. It should be recognised that most gastroenterology “treatment” is provided in an outpatient or sameday endoscopy setting. Children may require more urgent priority, of Paediatric Medicine criteria. Discussion with a Paediatrician should take place if there is concern. Last updated February 2006 Page 2 of 2