MCQ
OF
Davidson’s
Principles and Practice of
th
20 Edition
This book is downloaded from the
Website www.studentconsult.com
CONTENTS
Serial
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
1
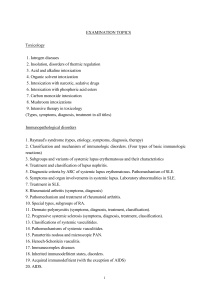
Subject
Good prescribing
Molecular mechanisms of disease
Immunological factors in disease
Environmental & nutritional factors in disease
Principles of infectious disease
Ageing and disease
Critical care and emergency medicine
Poisoning
Medical psychiatry
Oncology
Palliative care and pain management
Infectious diseases
HIV infection and the human AIDS
Sexually transmitted infections
Clinical biochemistry and metabolism
Kidney and urinary tract disease
Cardiovascular disease
Respiratory disease
Endocrine disease
Diabetes mellitus
Alimentary tract and pancreatic disease
Liver and biliary tract disease
Blood disorders
Musculoskeletal disorders
Neurological disease
Skin disease
Part 1
Question
3
5
7
9
12
15
16
19
23
25
27
28
35
37
39
42
48
59
68
73
77
85
91
98
104
113
Part 2
Answer
118
120
123
125
128
131
133
136
139
142
144
146
153
156
158
163
170
181
188
195
200
208
213
221
227
238
No of
Question
11
14
16
21
17
8
16
19
15
11
6
44
15
9
25
44
80
48
36
24
54
40
43
42
68
25
PART
1
QUESTIONS
2
Chapter
1 GOOD PRESCRIBING
Answers page 118
Question 1. Warfarin has a low
therapeutic index. What exactly does this
term mean?
A) It causes adverse effects at doses close
to the usual therapeutic range
B) It is effective at low plasma
concentrations
C) It causes toxicity at low plasma
concentrations
D) It has a low incidence of adverse
effects and toxicity
E) It is only effective at high plasma
concentrations
life-threatening haemorrhage, compared
with 40 of the treatment group. Based only
on these data, what would be the number
of patients treated to cause one lifethreatening haemorrhage (i.e. the number
needed to treat to cause one episode of
harm, NNTH, sometimes called 'the
number needed to harm')?
A) 2
B) 16
C) 25
D) 31
E) 50
Question 2. In a randomised, double-blind
placebo-controlled trial of a new inhaler
for asthma there were half as many acute
severe exacerbations in patients who took
the inhaler every day for 1 year compared
with placebo. The study authors quote a
number needed to treat (NNTB) of 25 for
the benefit of preventing one severe
exacerbation in 1 year. Based on these
data, which one of the following
statements is valid?
A) Only 1 in 25 patients will experience
any benefit from taking the new inhaler
B) On average, two severe exacerbations
will be prevented for every 50 patients
treated for 1
year with the new inhaler
C) On average, two severe exacerbations
will be prevented for every 25 patients
treated with the new inhaler for 2 years
D) Patients treated with the new inhaler
for 1 year are 25% less likely to have a
severe exacerbation during that time than
those not treated
E) The number needed to harm is greater
than 25
Question 4. Before you prescribe a new
drug for heart disease, your patient asks
you how likely it is to help him. After a
quick search you find the following
information from clinical trials relating to
the risk of myocardial infarction over 5
years while taking the drug:
• Risk of a myocardial infarction without
the new drug: 20%
• Risk of a myocardial infarction with the
new drug: 17%
• Absolute risk reduction: 3%
• Relative risk reduction: 15%
• Number needed to treat (to prevent one
myocardial infarction): 33 (95%
confidence interval: 30.4 to 35.6)
How would you express this information
to the patient?
A) Taking this drug for 5 years will reduce
your chance of a heart attack by 15%
B) If you take the drug for 5 years, there is
a 15% chance that it will prevent you from
having a heart attack
C) Taking this drug for 5 years will reduce
the chances of your having a heart attack
by 3%
D) If 100 people like you were to take this
drug for 5 years it would prevent 15 heart
attacks
E) There is a 1 in 33 chance that taking
this drug for 5 years will reduce your
chance of a heart attack by 95%
Question 3. A new drug is shown to
reduce mortality from sepsis from 310 out
of 1000 in the placebo group to 250 out of
1000 in the treatment group. A total of 20
of the placebo group develop
3
Question 5. A drug company
representative tells you that a new drug,
'Potentol', is 10 times more potent than the
currently popular drug of the same class,
'Weakol'. Which of the following
statements concerning the two drugs can
be made with greatest confidence?
A) The maximum effect of Potentol will
be greater than the maximum effect of
Weakol
B) Potentol will be a more effective drug
C) Potentol and Weakol must act on
different receptors
D) Potentol will have a more favourable
adverse effects profile
E) The dose-response curve for Potentol
lies to the left of the curve for Weakol
Question 6. The dose of which one of the
following drugs should be reduced in
patients with mild renal insufficiency?
A) Co-amoxiclav (amoxicillin plus
clavulanic acid)
B) Paracetamol
C) Digoxin
D) Simvastatin
E) Furosemide
Question 7. Which one of the following
drug combinations is most likely to be
harmful?
A) Digoxin and warfarin
B) Paracetamol and dihydrocodeine
C) Trimethoprim and sulfamethoxazole
D) Allopurinol and azathioprine
E) Atenolol and ciclosporin
Question 8. Which one of the following
pieces of information must be included in
a drug prescription outside hospital in the
UK?
4
A) The prescribing doctor's General
Medical Council (GMC) registration
number
B) The route of administration of the drug
C) The condition that is being treated
D) The proprietary name of the prescribed
drug
E) The duration of treatment
Question 9. Which one of the following is
not required on a prescription for a
controlled drug?
A) Patient's date of birth
B) Doctor's address
C) Patient's address
D) Exact size of each dose specified in
words and figures
E) Total quantity to be dispensed
Question 10. Treatment with which one of
the following drugs is often initiated with
a loading dose?
A) Codeine
B) Amiodarone
C) Atenolol
D) Allopurinol
E) Furosemide
Question 11. In a trial of a new treatment
for fulminant sepsis the mortality in the
treatment group is 20%, whereas the
mortality in the placebo group is 40%.
What is the relative risk of death with the
new treatment?
A) 0.1
B) 0.2
C) 0.4
D) 0.5
E) 2.0
Chapter
2
MOLECULAR
MECHANISMS OF
DISEASE
Answers page 120
Question 1. Which of the following
human cells contain 46 chromosomes?
A) Erythrocytes
B) Spermatozoa
C) Platelets
D) Neutrophils
E) Ova
Question 2. The term 'transcription' refers
to which of the following cellular
processes?
A) Activation of second messengers such
as adenyl cyclase
B) Formation of messenger RNA from
DNA by RNA polymerase
C) Splicing out of introns from RNA
D) Protein synthesis from RNA on
ribosomes
E) Protein modification in the Golgi
apparatus
Question 3. Mutation of the CFTR gene in
patients with cystic fibrosis mediates its
effect by interfering with which of the
following cellular processes?
A) Protein modification in the Golgi
apparatus
B) Active transport of sodium and
potassium via the Na/K ATPase pump on
the cell membrane
C) Chloride transport through channels on
the cell membrane
D) Endocytosis of extracellular debris
E) Binding of transcription factors in lung
tissue to upstream gene promoters
Question 4. All of the following
molecules except one bind to intracellular
receptors. Which is the exception?
A) Vitamin A
B) Glucocorticoids
C) Noradrenaline (norepinephrine)
D) Triiodothyronine
E) Oestrogen
5
Question 5. Which of the following
statements about cell death by apoptosis is
true?
A) The process only occurs in elderly
individuals
B) Cell destruction occurs by an antibodymediated process
C) The cell membrane remains intact
D) There is an associated acute
inflammatory response
E) It is the major mechanism underlying
myocyte death in acute myocardial
infarction
Question 6. A 45-year-old man is
diagnosed with Huntington's disease. He
and his wife have non-identical twins, now
aged 19. After genetic counselling, one of
the twins undergoes testing for the
Huntingtin gene which is found to be
positive. What is the risk of the other twin
inheriting the Huntingtin gene?
A) Zero
B) 25%
C) 50%
D) 75%
E) 100%
Question 7. Which of the following
conditions is not correctly paired with its
usual mode of inheritance?
A) Wilson's disease - autosomal recessive
B) Friedreich's ataxia - autosomal
recessive
C) Familial adenomatous polyposis coli autosomal dominant
D) Haemochromatosis - autosomal
dominant
E) Myotonic dystrophy - autosomal
dominant
Question 8. What is the underlying
chromosomal abnormality in Down's
syndrome?
A) 45,XO
B) 47,XXY
C) Trisomy 13
D) Trisomy 18
E) Trisomy 21
Question 9. Which one of the following
familial cancer syndromes is associated
with mutations in BRCA genes?
A) Von Hippel-Lindau disease
B) Peutz-Jeghers syndrome
C) Li-Fraumeni syndrome
D) Hereditary non-polyposis colorectal
cancer (HNPCC)
E) Familial breast/ovarian cancer
Question 10. Which one of the following
conditions does not show autosomal
dominant inheritance?
A) Gilbert's disease
B) Congenital adrenal hyperplasia
C) Familial hypercholesterolaemia
D) Marfan's syndrome
E) Adult polycystic kidney disease
Question 11. Which one of the following
features is not characteristic of Turner's
syndrome?
A) Only females are affected
B) Short stature
C) Webbed neck
D) Secondary amenorrhoea
E) Coarctation of the aorta
6
Question 12. A man with haemophilia A
is married to a woman who is not a carrier
for haemophilia. They are planning to start
a family and so attend the genetic
counselling clinic. What advice would you
give them?
A) A son would have haemophilia and a
daughter would have a 50% chance of
being a carrier
B) A son would have haemophilia and a
daughter would have a 100% chance of
being a carrier
C) A son would be unaffected and a
daughter would have a 50% chance of
being a carrier
D) A son would be unaffected and a
daughter would have a 100% chance of
being a carrier
E) A son would have a 50% chance of
being a carrier and a daughter would have
haemophilia
Question 13. Which one of the following
terms refers to the proportion of
individuals inheriting an abnormal gene
who go on to exhibit clinical disease?
A) Anticipation
B) Imprinting
C) Penetrance
D) Lyonisation
E) Translocation
Question 14. The cluster of cerebellar
haemangioblastoma, renal cell carcinoma
and phaeochromocytoma occurs in which
one of the following conditions?
A) Peutz-Jeghers syndrome
B) Von Hippel-Lindau disease
C) Li-Fraumeni syndrome
D) Wermer's syndrome
E) Gardner's syndrome
Chapter
3
IMMUNOLOGICAL
FACTORS IN DISEASE
Answers page 123
Question 1. Which of the following is a
component of the acquired immune
response in humans?
A) Low pH of skin
B) Secretion of lysozyme
C) Colonisation with commensal bacteria
D) Phagocytes
E) T lymphocytes
Question 2. A gardener cuts his finger
while using a rusty knife. Over the
following 24 hours, his finger becomes
red, warm and painful. Which cell type is
most important in immune defence during
these initial stages of infection?
A) Eosinophils
B) Neutrophils
C) T cells
D) B cells
E) Basophils
Question 3. The infection described in the
previous question (Q2) spreads and the
gardener is given a course of antibiotics by
his general practitioner. Which of the
following blood tests would be most
useful in monitoring his response to
treatment?
A) C-reactive protein (CRP)
B) T-cell count
C) Complement (C3 and C4)
D) Immunoglobulin IgM levels
E) Immunoglobulin IgG levels
Question 4. A 48-year-old man presents
with progressive visual loss and is found
to have fulminant cytomegalovirus (CMV)
infection of the retina. He also has
recurrent oral candidiasis. A deficiency of
which of the following immune
components is most likely to cause these
problems?
7
A) Phagocyte deficiency
B) Complement deficiency
C) T-lymphocyte deficiency
D) Antibody deficiency
E) Neutrophil deficiency
Question 5. A 35-year-old man presents
with his third episode of meningococca
meningitis. What is the most likely
primary immune deficiency that could
account for
This ?
A) Complement deficiency
B) T-cell deficiency
C) Neutrophil deficiency
D) Antibody deficiency
E) Primary cytokine deficiency
Question 6. A 30-year-old woman, who is
known to be hepatitis C-positive, develops
joint pain, microscopic haematuria and a
purpuric rash. Which diagnosis would best
explain her symptoms?
A) Anti-phospholipid syndrome
B) Autoimmune thrombocytopenia
C) Liver cirrhosis
D) Cryoglobulinaemia
E) Autoimmune hepatitis
Question 7. A 30-year-old woman is
being investigated for recurrent
miscarriages. She has recently developed a
deep venous thrombosis and is on
warfarin. Which of the following tests
would be most useful in investigating her
underlying disease?
A) Erythrocyte sedimentation rate
B) Rheumatoid factor
C) T-cell count
D) Anticardiolipin antibodies
E) Lupus anticoagulant
Question 8. An 8-year-old boy presents
with recurrent bacterial chest infections
and bronchiectasis. What is the most likely
primary immune deficiency that could
account for this?
A) Complement deficiency
B) T-cell deficiency
C) Neutrophil function disorder
D) Antibody deficiency
E) Cytokine defect
Question 9. Which of the following
measures is least likely to form part of the
management of a patient with an antibody
deficiency syndrome?
A) Long-term prophylactic antibiotics
B) Vaccination with live attenuated
vaccines
C) Intravenous immunoglobulin infusion
D) Aggressive treatment of even mild
infections
E) Monitoring of immunoglobulin levels
Question 10. In DiGeorge syndrome,
abnormal development of which of the
following structures leads to immune
deficiency?
A) Thymus
B) Pituitary
C) Thyroid
D) Parathyroid
E) Spleen
Question 11. Which one of the following
human leucocyte antigen (HLA)
genotypes is strongly associated with
ankylosing spondylitis?
A) HLA-DR3
B) HLA-B27
C) HLA-DR4
D) HLA-B12
E) HLA-DR2
Question 12. According to the Gell and
Coombs classification of hypersensitivity,
which of the following is an example of a
type II (antibody-mediated) reaction?
A) Acute anaphylaxis
8
B) Acute cell-mediated transplant
rejection
C) ABO blood transfusion reaction
D) Farmer's lung
E) Nickel hypersensitivity
Question 13. Which of the following
conditions is associated with anticentromere antibodies?
A) CREST syndrome
B) Rheumatoid arthritis
C) Systemic lupus erythematosus
D) Sjögren's syndrome
E) Mixed connective tissue disease
Question 14. Which of the following
conditions is particularly associated with
anti-Ro and anti-La antibodies?
A) Dermatomyositis
B) Drug-induced lupus
C) Mixed connective tissue disease
D) Diffuse scleroderma
E) Sjögren's syndrome
Question 15. c-ANCA (anti-neutrophil
cytoplasmic antibody with cytoplasmic
fluorescence) is commonly associated with
which one of the following conditions?
A) Churg-Strauss syndrome
B) Wegener's granulomatosis
C) Henoch-Schönlein purpura
D) Temporal arteritis
E) Rheumatoid vasculitis
Question 16. Which of the following best
describes the characteristic features of the
amyloid diseases?
A) Extracellular deposition of insoluble
proteins
B) Intracellular deposition of insoluble
proteins
C) Extracellular deposition of soluble
proteins
D) Intracellular deposition of soluble
proteins
E) Intracellular deposition of insoluble
carbohydrates
Chapter
4
ENVIRONMENTAL AND
NUTRITIONAL FACTORS IN
DISEASE
Answers page 125
Question 1. Which one of the following
terms describes the number of new cases
of a disease occurring in a population at
risk during a defined period of time?
A) Rate of the disease
B) Prevalence of the disease
C) Relative risk of the disease
D) Attributable risk of the disease
E) Incidence of the disease
Question 2. A nuclear power station is
built in close proximity to a village with a
population of 3000 (village X). The
residents are concerned about the rising
incidence of disease Z. The incidence of
disease Z in village X in 1 year was 150
cases. In a matched population of 3000
people not living in proximity to a nuclear
power station, the incidence of disease Z is
30 cases per year. What is the relative risk
of disease Z in village X?
A) 5
B) 10
C) 3
D) 30
E) 50
Question 3. Regular cigarette smoking has
been associated with an increased risk of
developing all of the following diseases
except one. Which is the exception?
A) Peripheral vascular disease
B) Peptic ulcer disease
C) Bronchogenic carcinoma
D) Ulcerative colitis
E) Stroke
9
Question 4. After which one of the
following interventions is a patient most
likely to be abstinent from cigarettes 6
months later?
A) Bupropion
B) Nicotine replacement therapy (NRT)
C) NRT plus behavioural support
D) Behavioural support
E) Opportunistic advice from the doctor
Question 5. Which one of the following
statements about the physiological
adaptations that occur at high altitude is
true?
A) The oxyhaemoglobin dissociation
curve moves to the right
B) In those acclimatised to high altitude,
2,3-DPG production is decreased
C) In those acclimatised to high altitude,
erythropoietin (Epo) production is
decreased
D) Full physiological adaptation to altitude
is complete in 3-4 hours in most
individuals
E) Hypoventilation is one of the adaptive
mechanisms used by the body when
ascending to high altitude
Question 6. A traveller on an expedition
to the Andes (altitude 3850 m) becomes
unwell on the third day of the trip. He
initially complains of breathlessness, dry
cough and fatigue. The cough
subsequently becomes productive of
bloody sputum and on examination he is
found to be hypoxic with crepitations in
both lung fields. What is the likeliest
diagnosis?
A) Acute mountain sickness
B) Pulmonary embolism
C) High-altitude pulmonary oedema
D) Acute respiratory distress syndrome
E) Pneumothorax
Question 7. In a patient diagnosed with
acute mountain sickness, the appearance
of which of the following clinical features
should lead to a review of the diagnosis?
A) Headache
B) Visual loss
C) Difficulty sleeping
D) Fatigue
E) Nausea and vomiting
Question 8. Which one of the following is
not a complication of near-drowning?
A) Haemoptysis
B) Hypotension
C) Metabolic alkalosis
D) Dehydration
E) Cardiac arrhythmias
Question 9. Non-starch polysaccharides
(NSP) are the most important source of
fibre in the human diet. Which one of the
following is not classed as an NSP?
A) Hemicellulose
B) Cellulose
C) Pectin
D) Linoleic acid
E) Gums
Question 10. The calorific value of one
gram of protein is 5 kcal. How many
calories are in one gram of fat?
A) 5 kcal
B) 7 kcal
C) 9 kcal
D) 12 kcal
E) 17 kcal
Question 11. Which one of the following
statements regarding dietary proteins is
false?
A) The term 'biological value' of a protein
refers to the relative proportions of
essential amino acids which it contains
B) Proteins typically contribute < 20% to
overall energy intake
C) Some essential amino acids cannot be
obtained from vegetarian diets,
necessitating the use of supplements
D) Essential amino acids are so called
because they cannot be synthesised in
humans, but are essential for the synthesis
of important proteins
E) The 'energy density' of protein (in
kcal/g) is lower than that of fat
10
Question 12. Which one of the following
statements regarding artificial nutritional
support in hospital is true?
A) Aspiration pneumonia is a recognised
complication of parenteral feeding
B) High-energy supplement drinks are an
adequate replacement for normal diet in
the hospital inpatient
C) Parenteral nutrition is preferable to
enteral feeding in most cases
D) Hyperosmolar feeding solutions can be
administered through a wide-bore venous
cannula inserted into a large peripheral
vein
E) Feeding via a central (subclavian or
internal jugular) line carries a higher risk
of sepsis than feeding via a percutaneous
endoscopic gastrostomy (PEG) tube
Question 13. Which one of the following
drug treatments is most likely to lead to
weight gain?
A) Thyroxine
B) Combined oral contraceptive pill
C) Metformin
D) Sibutramine
E) Omeprazole
Question 14. Which one of the following
statements regarding obesity is true?
A) Obesity is defined by World Health
Organization criteria as a body mass index
(BMI) of 25 kg/m2 and above
B) Obesity is more common in smokers
C) Hypothyroidism is an irreversible cause
of obesity
D) Known genetic mutations account for
60% of the susceptibility to obesity
E) Obese people have a higher basal
metabolic rate than lean people
Question 15. Obesity is associated with an
increased risk of all of the following
conditions except one. Which is the
exception?
A) Coronary heart disease
B) Non-alcoholic steatohepatitis
C) Osteoporosis
D) Endometrial cancer
E) Obstructive sleep apnoea
Question 16. Which of the following
interventions is likely to produce the
greatest magnitude of weight loss in
patients with morbid obesity?
A) Bariatric gastric surgery
B) Modified diet
C) Orlistat
D) Graded exercise programme
E) Sibutramine
Question 17. Which of the following is
not a fat-soluble vitamin?
A) Vitamin K
B) Vitamin A
C) Vitamin D
D) Vitamin C
E) Vitamin E
Question 18. Which one of the following
vitamins is incorrectly matched with its
deficiency state?
A) Vitamin C Scurvy
B) Vitamin B2 (riboflavin) Beri-beri
C) Niacin (nicotinic acid) Pellagra
D) Folate (folic acid) Neural tube defects
in the fetus
E) Vitamin A Night blindness
Question 19. The district nurse asks you
to review an 84-year-old man at his home.
She has been administering regular
dressings for a chronic venous stasis ulcer
that has been slow to heal, but is now
concerned that he has developed several
11
large bruises and has been bleeding from
his gums. Routine blood tests have also
revealed a mild iron-deficiency anaemia.
You suspect that there is a nutritional
element to his complaints. Which of the
following vitamins is the patient most
likely to be deficient in?
A) Vitamin C
B) Vitamin A
C) Vitamin B1
D) Vitamin B12
E) Vitamin K
Question 20. Which one of the following
inorganic nutrients is incorrectly paired
with its deficiency state?
A) Iodine Congenital hypothyroidism
B) Calcium Impaired bone mineralisation
C) Fluoride Discoloration of teeth
D) Zinc Dermatitis and chronic diarrhoea
E) Selenium Cardiomyopathy in children
Question 21. All of the following except
one are clinical features suggestive of
severe adult malnutrition. Which is the
exception?
A) Thinning of hair
B) Increased skinfold thickness over the
triceps
C) Dependent oedema
D) Amenorrhoea or impotence
E) Dryness of skin with occasional
pigmented patches
Chapter
5
PRINCIPLES OF
INFECTIOUS DISEASE
Answers page 128
Question 1. Which one of the following
statements regarding infectious agents is
incorrect?
A) Bacteria possess a cell wall
B) Viruses contain either DNA or RNA
C) Prions are highly complex structures
consisting of > 100 different proteins
D) Fungal cells contain a defined nucleus
E) Viruses cannot reproduce autonomousl
Question 2. Which one of the following
organisms is incorrectly matched with its
mode of transmission?
A) Legionella Water aerosol
B) Salmonella Faecal-oral
C) Listeria Ingestion
D) Hepatitis A Needlestick injury
E) Tetanus Direct skin penetration
Question 3. Which one of the following
vaccines is inactivated (as opposed to
live)?
A) Pertussis
B) Measles
C) Mumps
D) BCG (tuberculosis)
E) Rubella
Question 4. Which one of the following
vaccines is not given to children until the
second year of life?
A) HiB (Haemophilus influenzae type B)
vaccine
B) Oral polio vaccine
C) Meningitis group C vaccine
D) MMR (measles, mumps, rubella)
vaccine
E) DPT (diphtheria, pertussis, tetanus)
vaccine
12
Question 5. Which of the following
measures is of least importance in the
management of asplenic patients?
A) Yearly receipt of the polyvalent flu
vaccine
B) Yearly receipt of the pneumococcal
vaccine
C) Receipt of the meningococcal C
vaccine
D) Prophylactic antibiotics prior to dental
procedures
E) Long-term daily dose of penicillin
Question 6. Which one of the following
conditions is a notifiable disease in the UK
under the Public Health (Infectious
Diseases) Regulations 1988?
A) Chicken pox
B) HIV
C) Scabies
D) Syphilis
E) Meningococcal meningitis
Question 7. Which one of the following
human pathogens is correctly matched
with its most common method of
identification?
A) Streptococcus pyogenes Polymerase
chain reaction (PCR)
B) Hepatitis B virus Blood culture
C) Neisseria gonorrhoeae Direct
microscopy
D) Mycobacterium tuberculosis Enzymelinked immunosorbent assay (ELISA)
E) Candida albicans Complement fixation
test
Question 8. Which one of the antibiotics
below is correctly paired with its
predominant mode of action?
A) Penicillin Disrupts bacterial protein
synthesis by binding to the 50S subunit of
bacterial ribosomes
B) Gentamicin Inhibits cell wall synthesis
C) Ciprofloxacin Inhibits DNA gyrase,
thereby blocking DNA replication
D) Minocycline Inhibits dihydrofolate and
tetradihydrofolate reductase to block
bacterial folate synthesis
E) Erythromycin Forms superoxides that
damage proteins, nuclear acid and lipids
Question 9. One of the following
definitions of terms relating to the
pharmacokinetics of antibiotics is
incorrect.Which is it?
A) Minimum inhibitory concentration
(MIC) is the lowest concentration of an
antibiotic required to inhibit 50% of the
colonies of a particular organism
B) t{1/2} (plasma half-life) of an antibiotic
is the time taken for the concentration of
the drug in the body to be reduced by half
C) Post-antibiotic effect (PAE) is the
clinically useful property of some classes
of antibiotic whereby inhibition of
microbial replication continues beyond the
time when the MIC is reached in plasma
D) Inoculum effect is the reduction in
activity of an antibiotic by the presence of
large numbers of organisms despite
apparent MIC-based sensitivity
E) Synergism is the enhanced efficacy
achieved by co-administration of two
different antibiotics that exceeds the effect
predicted by their combined MICs
13
Question 10. In which one of the
following clinical scenarios is the
suggested prophylactic agent inappropriate
for the purpose described?
A) Prevention of spontaneous bacterial
peritonitis in a patient with
cirrhosis Norfloxacin
B) Prevention of bacteraemia in a postsplenectomy
patient Phenoxymethylpenicillin
C) Prevention of endocarditis in a patient
with a prosthetic mitral valve undergoing
tooth extraction Amoxicillin
D) Prevention of gas gangrene in a patient
with a contaminated wound Flucloxacillin
E) Prevention of varicella infection in a
healthy newborn exposed to varicella
zoster during delivery Varicella immune
globulin
Question 11. Which one of the following
statements regarding ß-lactam antibiotics
is incorrect?
A) Benzylpenicillin, flucloxacillin and
meropenem are all subtypes of this class
B) They are bactericidal antibiotics
C) Most patients with established allergy
to benzylpenicillin are also allergic to
cephalosporins
D) Synergism occurs in combination with
the aminoglycosides (e.g. gentamicin)
E) Potential side-effects include
gastrointestinal upset and interstitial
nephritis
Question 12. A previously healthy 14year-old girl is admitted to the paediatric
intensive care unit with a severe lower
respiratory tract infection (LRTI).
Serological investigations subsequently
reveal very high titres of Mycoplasma
pneumoniae. Which of the following
antibiotics is most effective against this
organism?
A) Flucloxacillin
B) Metronidazole
C) Clarithromycin
D) Co-amoxiclav
E) Ceftriaxone
Question 13. An 83-year-old lady is
admitted to the stroke unit with a right
partial anterior circulation stroke after
being found at home on the floor,
surrounded by vomit. On day 2 of her
admission, she develops a productive
cough, and oxygen saturations fall from
96% to 89% on air. Her temperature is
38.5°C. She has coarse crepitations at the
right base and opacification of the right
lower zone on chest X-ray. While awaiting
the results of microbiological
investigations, which one of the following
antibiotic regimens would you prescribe?
A) IV ceftriaxone and metronidazole
B) IV vancomycin alone
C) IV benzylpenicillin and flucloxacillin
D) Oral co-amoxiclav and clarithromycin
E) IV amoxicillin alone
Question 14. Which of the following
adverse effects is least likely to occur as a
result of aminoglycoside (e.g. gentamicin)
administration?
A) Renal toxicity
B) Cochlear toxicity
C) Neuromuscular blockade following
rapid IV infusion
D) Hepatotoxicity
E) Nausea and vomiting
Question 15. Which one of the following
statements regarding ciprofloxacin is true?
A) It has poor oral bioavailability
14
B) It has potent anti-Gram-negative
properties, but little or no anti-Grampositive activity
C) Side-effects involving the
gastrointestinal tract and skin are frequent
and troublesome
D) It has a small volume of distribution
and poor tissue penetration
E) Oral absorption is enhanced by
administration with food
Question 16. Which one of the following
statements about glycopeptide antibiotics
(such as vancomycin) is incorrect?
A) Rapid infusion may produce an
anaphylactoid reaction from histamine
release
B) They exhibit good activity against
meticillin-resistant Staphylococcus aureus
(MRSA)
C) Therapeutic monitoring of drug levels
is required
D) Cover against Gram-negative
organisms is poor
E) They have good oral bioavailability
Question 17. Which one of the following
antimicrobials is incorrectly matched with
its adverse side-effect?
A) Chloramphenicol 'Grey baby syndrome'
B) Minocycline Tooth discoloration in
children
C) Doxycycline Photosensitivity
D) Ketoconazole Nephrotoxicity
E) Erythromicin Cholestatic jaundice
Chapter
6 AGEING AND DISEASE
Answers page 131
Question 1. Features of ageing include all of
the following except one. Which is the
exception?
A) Reduced glomerular filtration rate
B) Lens opacification
C) Neuronal loss
D) Increased insulin secretion
E) Reduced maximum heart rate
Question 2. Which of the following drugs is
least likely to contribute to recurrent falls in an
elderly patient?
A) Codeine phosphate
B) Temazepam
C) Amitriptyline
D) Omeprazole
E) Furosemide
Question 3. Which one of the following is not
an established risk factor for recurrent falls in
the elderly?
A) Cognitive impairment
B) Depression
C) Osteoarthritis
D) Visual impairment
E) Bisphosphonate therapy
Question 4. A 79-year-old man is referred to
the day hospital with recurrent falls. He has a
history of hypertension and type II diabetes.
He normally takes aspirin, amlodipine,
metformin and simvastatin. Blood pressure is
121/86 mmHg when supine, falling to 96/61
mmHg when standing. What would the most
appropriate initial treatment be?
A) Continue current treatment
B) Continue current treatment and start
fludrocortisone
C) Stop amlodipine
D) Stop amlodipine and start bendrofluazide
E) Stop all medication except aspirin
Question 5. Causes of acute confusion in the
elderly include all of the following except one.
Which is the exception?
A) Pulmonary embolism
B) Urinary tract infection
C) Recent prescription for tramadol
15
D) Alzheimer's disease
E) Hyponatraemia
Question 6. Which one of the following
statements regarding urinary incontinence is
true?
A) It is a feature of normal ageing
B) It can be caused by hypocalcaemia
C) It affects 50% of women over the age of 65
D) Bladder catheterisation is usually the firstline treatment
E) Laxatives may be helpful
Question 7. An 82-year-old man is referred to
the medical outpatient clinic with recurrent
dizzy spells. He describes periodic
lightheadedness occurring several times a
week, typically lasting for less than 1 minute.
Symptoms are unrelated to posture. He has
never lost consciousness and denies chest pain
or palpitations. He has a past history of
hypertension and osteoarthritis and normally
takes atenolol and paracetamol. Examination is
unremarkable and the resting ECG normal.
What would the most useful initial
investigation be?
A) Cervical spine X-ray
B) 24-hour ambulatory ECG
C) Echocardiogram
D) CT head scan
E) MRI head scan
Question 8. An 86-year-old lady on the care of
the elderly ward is found to have a coin-shaped
lesion suggestive of a malignancy on a routine
chest X-ray. She has a profound expressive
dysphasia resulting from a previous stroke and
suffers from severe chronic obstructive
pulmonary disease. Which of the following
factors should least influence further
investigation and management?
A) The patient's comorbidity
B) The patient's ability to tolerate the available
treatments
C) Chronological age
D) Biological age
E) An advance directive prepared by the
patient
Chapter
7
CRITICAL CARE AND
EMERGENCY MEDICINE
Answers page 133
Question 1. You are asked to prescribe
fluids for a 66-year-old, previously well
man on the high-dependency unit, who
returned from a radical prostatectomy 8
hours ago. Preoperatively, his blood
pressure was 145/78 mmHg. He lost 2
litres of blood in theatre and has since
received intravenous fluids and 4 units of
red cells. In the past 4 hours his
intravenous intake has consisted of a 500
ml bag of 0.9% saline. He is alert and
complains of feeling thirsty. He does not
have an epidural. The observation chart
shows:
Which of the following is the most
appropriate fluid regimen to prescribe?
A) 6-hourly Hartman's solution
B) 8-hourly alternating 0.9% saline and
5% dextrose, with potassium
supplementation
C) 4-hourly 0.9% saline
D) Immediate transfusion with O-negative
blood
E) 250 ml of gelofusine over 15 minutes
Question 4. A 65-year-old patient in the
ICU appears to be making an excellent
recovery from pneumonia but then
deteriorates acutely. He has the following
observations:
Which of the following diagnoses is the
most likely cause of his deterioration?
A) Major haemorrhage
B) Pulmonary embolism
C) Septic shock (pre-volume load)
D) Neurogenic shock
E) Acute left ventricular failure secondary
to myocardial infarction
Question 2. Which of the following
haemodynamic parameters is represented
by pulmonary artery wedge pressure
(PAWP)?
A) Central venous pressure
B) Pulmonary arterial pressure
C) Left atrial pressure
D) Systemic capillary pressure
E) Intrathoracic pressure
Question 6. Which of the following drugs
causes an increase in systemic vascular
resistance?
A) Sodium nitroprusside
B) Noradrenaline (norepinephrine)
C) Dobutamine
D) Dopexamine
E) Glyceryl trinitrate (GTN)
Question 3. Which of the following
factors has the least direct bearing on
central venous pressure?
A) Pulmonary artery pressure
B) Systemic arterial pressure
C) Venous tone
D) Intravascular volume
E) Intrathoracic pressure
16
Question 5. Which one of the following
would be the best intramuscular dose of
adrenaline (epinephrine) in a patient with
acute anaphylactic shock and airway
compromise?
A) 1 ml of 1 in 1000 adrenaline
B) 1 ml of 1 in 10 000 adrenaline
C) 1 ml of 1 in 100 000 adrenaline
D) 10 ml of 0.1% adrenaline
E) 10 ml of 1% adrenaline
Question 7. Which one of the following
forms part of the diagnostic criteria for
acute respiratory distress syndrome
(ARDS)?
A) Normal chest X-ray
B) PaCO2 > 6.5
C) Blood pressure < 90/50 mmHg
D) Pulmonary artery wedge pressure
(PAWP) < 15 mmHg
E) Increased lung compliance
Question 8. A patient presents critically ill
in type 1 respiratory failure with the
following arterial blood gas
measurements:
E) There is a metabolic alkalosis in the
second ABG
Which of the following conditions is least
likely to explain these findings?
A) Diamorphine overdose
B) Pulmonary embolus
C) Acute asthma
D) Pneumothorax
E) Pulmonary oedema
Question 12. A 35-year-old man is
admitted to the ICU with abdominal sepsis
following a laparotomy for a ruptured
appendix. He is systemically unwell and
requires ventilation. One day postoperatively, bleeding is noticed from his
abdominal wound and sites of line
insertion. The following results are
obtained from tests of coagulation:
Question 9. In which of the following
conditions is continuous positive airways
pressure (CPAP) usually most effective?
A) Acute severe asthma
B) Pulmonary oedema secondary to left
ventricular failure (LVF)
C) Exacerbation of chronic obstructive
pulmonary disease (COPD)
D) Narcotic drug overdose
E) Neuromuscular disorder leading to
respiratory failure
Question 10. This series of arterial blood
gas (ABG) measurements was taken from
the same patient 24 hours apart:
Which one of the following statements is
true?
A) There is a respiratory alkalosis in the
first ABG
B) There is a respiratory acidosis in the
second ABG
C) Arterial bicarbonate (HCO3-) must be
lower in the second ABG
D) Pulmonary gas exchange has improved
in the second ABG
17
Question 11. Which of the following
metabolic derangements is most likely to
cause coma?
A) Hyperkalaemia
B) Hypercalcaemia
C) Hypokalaemia
D) Hyponatraemia
E) Hyperuricaemia
Which of the following is the most likely
underlying problem?
A) Warfarin effect
B) Heparin effect
C) Disseminated intravascular coagulation
(DIC)
D) Haemolytic uraemic syndrome (HUS)
E) Idiopathic thrombocytopaenic purpura
Question 13. Which one of the following
is an appropriate strategy for controlling
intracranial pressure in a patient with a
head injury?
A) 30° head-down tilt
B) Use intravenous dextrose to reduce
plasma sodium
C) Use of positive end-expiratory pressure
(PEEP) ventilation
D) Mild hyperventilation to reduce PaCO2
to 4-4.5 kPa
E) Aggressive fluid resuscitation to keep
CVP above 20 cmH2O
Question 14. Which of the following
complications is associated with treatment
of ventilated patients with ranitidine?
A) Stress ulceration
B) Ischaemic bowel
C) Hyperbilirubinaemia
D) Pneumonia
E) Acute tubular necrosis
Question 15. A 72-year-old patient with a
history of ischaemic heart disease is being
monitored in the surgical high-dependency
unit following drainage of an intraabdominal abscess. At 2000 hours he
complains of feeling nauseated and
feverish. He is referred to the critical care
team. Below is his observation chart for
the previous 6 hours (breathing air):
18
He is transferred to the ICU. Which of the
following measures would be most
appropriate as part of his further
management?
A) Intubation and ventilation
B) Administration of a diuretic
C) Central venous catheterisation
D) Commencement of inotrope infusion
E) Haemofiltration
Question 16. The patient from the
previous question is resuscitated over the
next 6 hours in the ICU. Despite him
receiving 4 litres of intravenous fluid, his
blood pressure and urine output fail to
improve significantly. An oesophageal
cardiac output monitor is placed and
demonstrates a cardiac output of 8
litres/min. (A normal cardiac output would
be 5 litres/min for a man of this size.)
Which of the following is the likeliest
diagnosis?
A) Hypovolaemic shock
B) Septic shock
C) Anaphylactic shock
D) Cardiogenic shock
E) Obstructive shock
Chapter
8
POISONING
Answers page 136
Question 1. A rural hospital Accident and
Emergency department is overwhelmed
when 21 people present with poisoning
due to contamination of the local water
supply. They all have small pupils, muscle
fasciculation, excessive salivation and
lacrimation, vomiting, diarrhoea and
hyper-reflexia. What is the likeliest
contaminant?
A) Amphetamine-related compounds
B) Methadone
C) Organophosphate insecticides
D) Arsenic
E) Fluoride
Question 2. A 19-year-old girl is brought
to hospital by her partner, having been
found unconscious at home after a night
out. Her partner has brought an empty
bottle of the tricyclic antidepressant,
amitriptyline, which he believes she has
taken in overdose. You meet her on her
arrival at the hospital Accident and
Emergency department. What is the
priority on her arrival at the hospital?
A) A history from the partner of the
estimated dose and any possible coingestants, such as alcohol
B) Cardiac monitoring and/or a portable
defibrillator in case of cardiac arrhythmias
C) Assess the patient's pulse rate to
identify any tachyarrhythmia
D) Ensure a patent airway
E) Administer 100% oxygen
19
Question 3. Which of the following drugs
is most effectively removed by
haemodialysis?
A) Paracetamol
B) Venlafaxine
C) Amitriptyline
D) Metformin
E) Aspirin
Question 4. Activated charcoal may be
useful in the treatment of overdose with all
of the following drugs except one. Which
is the exception?
A) Theophylline
B) Ethanol
C) Paracetamol
D) Quinine
E) Carbamazepine
Question 5. Which of the following drugs
is the most appropriate treatment for
paracetamol overdose?
A) Glucagon
B) Gamma-hydroxybutyrate
C) Desferrioxamines
D) N-acetylcysteine
E) Pralidoxime
Question 6. A 16-year-old female with
anorexia is brought to hospital by her
mother 2 hours after attempting suicide by
taking 22 g of paracetamol. She was
drowsy when her mother found her, and
on arrival at hospital she is unresponsive
to pain. Observations on admission are as
follows:
After assessment and appropriate
management of airway, breathing and
circulation, which of the following is the
most appropriate next step in her
management?
A) Give activated charcoal via a
nasogastric tube
B) Give N-acetylcysteine intravenously
C) Administer vitamin K intravenously to
prevent hepatic coagulopathy
D) Urgently measure blood paracetamol
levels
E) Communicate with the mother to be
certain of the timing of the overdose and
to identify possible co-ingestants
Question 7. A 21-year-old patient is
brought to the hospital Accident and
Emergency department by the police on a
Sunday morning. He had been arrested at
an all-night party but on the way to the
police station, became very agitated and
appeared unwell. On arrival he complains
of thirst and nausea, and on examination
exhibits large pupils, hypertension and
global hyper-reflexia. He admits to illicit
drug use the night before. Which of the
following substances is the most likely
cause of his symptoms?
A) Methanol
B) Gammahydroxybutyrate (GHB)
C) Ecstasy (MDMA)
D) Heroin
E) D-lysergic acid diethylamide (LSD)
20
Question 8. A known drug addict is
brought to hospital, having been found in a
collapse. He has a respiratory rate of 3
breaths per minute and pinpoint pupils,
and is completely unresponsive to painful
stimuli. Which of the following drug
treatments should he receive?
A) Flumazenil
B) Naloxone
C) Desferrioxamine
D) Adrenaline (epinephrine)
E) Glucagon
Question 9. A 62-year-old lady is brought
to hospital by her son-in-law after being
found at home behaving strangely. She is
on several medications for cardiac disease,
including warfarin, and has recently
started a drug for depression. Observations
on admission are as follows
When you see her she is confused and
disorientated but appears to be able to hear
normally. She complains of seeing a
yellow hue over everything and vomits
three times. The cardiac monitor shows
sinus bradycardia with brief selfterminating runs of ventricular
tachycardia. Her ECG shows downwardsloping ST segment depression. Toxicity
from which one of the following agents
best explains her presentation?
A) Warfarin
B) Verapamil
C) Quinine
D) Fluoxetine
E) Digoxin
Question 10. An unkempt 43-year-old
man staggers into the hospital Accident
and Emergency department smelling
strongly of alcohol and complaining that
he cannot see. He vomits twice on arrival
and is incontinent of urine. His blood
results are as follows:
Question 12. A patient with an overdose
has been successfully treated with
desferrioxamine. What agent was
ingested?
A) Iron
B) Paracetamol
C) Aspirin
D) Lead
E) Cyanide
Question 13. A 23-year-old man is
brought to the hospital Accident and
Emergency department by the ambulance
service. He is drowsy, speaking
incoherently and has small pupils.
Observations on admission are as follows:
Toxicity from which of the following
drugs best explains his presentation?
A) Amitriptyline
B) Diamorphine
C) Temazepam
D) Cocaine
E) Venlafaxine
What is the diagnosis?
A) Diabetic ketoacidosis (DKA)
B) Ethanol poisoning
C) Salicylate poisoning
D) Methanol poisoning
E) Carbon monoxide (CO) poisoning
Question 11. Which one of the following
agents is used in the treatment of overdose
with ß-blockers?
A) N-acetylcysteine
B) Calcium gluconate
C) Naloxone
D) Methionine
E) Glucagon
21
Question 14. Treatment of paracetamol
overdoses is usually decided by referring
to this nomogram:
A patient with which of the following
conditions should be treated according to
the normal risk line?
A) Anorexia nervosa
B) Epilepsy treated with phenytoin
C) Chronic alcoholism
D) Chronic malnourishment
E) Co-ingestion of ecstasy (MDMA)
Question 15. A 45-year-old woman is
brought to hospital at 2330 hours by her
partner, who found her lying in bed with
three empty packets of paracetamol. She
tells you that she attempted suicide by
taking some of the tablets that morning,
but then took more tablets in the
afternoon, and some more after watching
the ten o'clock news. Her partner has
brought the packets to hospital. She is
normally healthy and is on no regular
medications. How would you decide
whether to administer N-acetylcysteine?
A) Treat if the most recent dose was more
than 75 mg/kg
B) Treat if a paracetamol level taken 4
hours after the last dose is above the
normal-risk treatment line on a standard
nomogram
C) Treat if a paracetamol level taken 4
hours after the last dose is above the highrisk treatment line on a standard
nomogram
D) Treat if the total 24-hour dose was
more than 150 mg/kg
E) Treat if the total 24-hour dose was
more than 75 mg/kg
Question 16. Which one of the following
drugs does not usually cause bradycardia
in overdose?
A) Atenolol
B) Digoxin
C) Lithium
D) Verapamil
E) Diltiazem
22
Question 17. A pet snake is brought to the
hospital Accident and Emergency
department by the friends of a patient who
was bitten by it some 12 hours previously.
The patient was dead on arrival at the
hospital. A medical student examining the
snake to identify it is accidentally bitten on
the forearm. Which of the following is the
most important action to take before
intravenous administration of the specific
antivenin?
A) Inject 0.02 ml of saline-diluted
antivenin subcutaneously and observe the
injection site for 10 minutes
B) Apply a tourniquet to the affected limb
C) Incise the bite and aspirate the poison
D) Check prothrombin time and fibrinogen
levels
E) Check renal function and creatine
kinase (CK) levels
Question 18. Overdose with which one of
the following agents causes large pupils?
A) Morphine
B) Aspirin
C) Paracetamol
D) Amitriptyline
E) Atenolol
Question 19. A blood level would be most
useful in the management of poisoning
with which of the following agents?
A) Aspirin
B) Fluoxetine
C) Morphine
D) Quinine
E) Organophosphates
Chapter
9 MEDICAL PSYCHIATRY
Answers page 139
Question 1. Pressure of speech and
grandiose ideas are most suggestive of
which of the following psychiatric
conditions?
A) Mania
B) Schizophrenia
C) Generalised anxiety disorder
D) Obsessive-compulsive disorder
E) Depression
Question 2. Common somatic symptoms
of anxiety disorders include all of the
following except one. Which is the
exception?
A) Sweating
B) Palpitations
C) Constipation
D) Dizziness
E) Breathlessness
Question 3. Which one of the following is
not a risk factor for suicide?
A) Male sex
B) Unemployed
C) Alcohol misuse
D) Living alone
E) Age under 45
Question 4. As the house officer on call
you are asked to review a patient who
appears to be hallucinating. The patient
describes seeing large spiders crawling
over the floor and the bed. Which of the
following features, elicited through a
careful mental state examination, would
point most strongly to an organic cause for
these hallucinations?
A) Impaired cognition and drowsiness
B) Pressure of speech
C) Unshakeable belief that spiders are
from another planet
D) Associated auditory hallucinations
E) Flat, blunted affect
23
Question 5. Which one of the following
statements regarding electroconvulsive
therapy (ECT) is false?
A) Use has declined since the advent of
antidepressant drugs
B) It is of proven efficacy for severe
depressive illness
C) It is rarely used due to the high
incidence of serious side-effects
D) It may cause both anterograde and
retrograde amnesia
E) It requires a general anaesthetic and
paralysis with muscle relaxants
Question 7. Which of the following
psychiatric drugs may interact with foods
rich in tyramine, such as cheese and red
wine, to produce a potentially fatal
hypertensive crisis?
A) Tricyclic antidepressants
B) Dopamine receptor antagonists
C) Monoamine oxidase inhibitors
D) Selective serotonin re-uptake inhibitors
E) Benzodiazepines
Question 8. Which one of the following
statements regarding antidepressant drug
treatments is true?
A) They are more effective than
psychological treatments for mild to
moderate depression
B) Selective serotonin re-uptake inhibitors
(SSRIs) have greater anticholinergic sideeffects and are more dangerous in
overdose than tricyclic antidepressants
C) The majority of patients experience an
improvement in symptoms within one
week of starting treatment
D) Newer antidepressants have greater
efficacy than older agents such as tricyclic
antidepressants
E) Treatment should be continued for at
least 6 months to reduce the high risk of
relapse
Question 9. Adverse effects associated
with lithium therapy include all of the
following except one. Which is the
exception?
A) Tremor
B) Teratogenicity
C) Hypothyroidism
D) Diabetes mellitus
E) Convulsions
Question 10. Which one of the following
is not a 'first-rank' symptom of
schizophrenia?
A) Thought insertion
B) Poverty of speech
C) Delusional perception
D) Passivity experiences
E) Auditory hallucinations in the third
person
Question 11. A 23-year-old male is
brought to Accident & Emergency by the
police after exhibiting bizarre behaviour.
He is extremely agitated and claims that he
is being followed by various agencies, all
with apparently sinister intent. Which one
of the following would make the diagnosis
of schizophrenia least likely?
A) Incomprehensible speech
B) Claims by the patient that the above
agencies were stealing thoughts from his
head
C) No previous history of mental illness
D) Ingestion of amphetamines within the
last 24 hours
E) Lack of insight
Question 12. Which one of the following
is not a recognised criterion for alcohol
dependence?
A) Feeling of compulsion to drink
B) Priority of drinking over other activities
C) Relief of withdrawal symptoms by
further drinking
24
D) Driving under the influence of alcohol
E) Reinstatement of drinking behaviour
after abstinence
Question 13. A 55-year-old male with a
long history of alcohol excess is admitted
to a medical ward, having been found by
neighbours in a state of gross self-neglect.
On admission he is noted to be confused
and very unsteady on his feet. On
examination he is clearly malnourished,
disorientated in time, person and place and
exhibits horizontal jerk nystagmus on
lateral gaze. He does not smell of alcohol
and there are no features of chronic liver
disease. Which of the following is the
likeliest diagnosis?
A) Korsakoff's syndrome
B) Hepatic encephalopathy
C) Delirium tremens
D) Wernicke's encephalopathy
E) Acute alcohol intoxication
Question 14. With reference to the patient
from the previous question (Q13) who has
Wernicke's encephalopathy, which of the
following steps should be undertaken first
in his management?
A) Rehydration with IV dextrose
B) CT scan of the brain
C) High-dose intravenous thiamin
(Pabrinex)
D) Oral benzodiazepines
E) Full septic screen
Question 15. All of the following except
one are diagnostic criteria for anorexia
nervosa. Which is the exception?
A) Body mass index 17.5 or less
B) Avoidance of high-calorie foods
C) Self-induced vomiting or purgation
D) Distortion of body image
E) Amenorrhea for at least 3 month
Chapter
10 ONCOLOGY
Answers page 142
Question 1. All of the following
statements except one are correct
epidemiological associations of
malignancy. Which is the exception?
A) BRCA 1 gene and ovarian cancer
B) Asbestos exposure and mesothelioma
C) Schistosomiasis and squamous bladder
cancer
D) Human papillomavirus and
oesophageal cancer
E) Adenopolyposis coli (APC) gene and
colorectal cancer
Question 5. A 63-year-old woman
receiving chemotherapy for breast cancer
attends the hospital accident and
emergency department, complaining of
headache, malaise and a dry cough.
Routine observations show a temperature
of 38.5°C, pulse of 104 bpm, BP of 128/83
mmHg, respiratory rate of 20 and oxygen
saturation of 97% on air. Examination is
otherwise unremarkable. Initial
investigations reveal the
following
Question 2. Which one of the following is
a risk factor for breast carcinoma?
A) Early menarche
B) Fibrocystic breast disease
C) Premature menopause
D) First full-term pregnancy at age 16
E) Multiple endocrine neoplasia (MEN)
type I
Question 3. Which one of the following is
not a recognised extrapulmonary
manifestation of bronchial carcinoma?
A) Syndrome of inappropriate antidiuretic
hormone secretion (SIADH)
B) Acanthosis nigricans
C) Finger clubbing
D) Eaton-Lambert syndrome
E) Ectopic adrenocorticotrophic hormone
(ACTH) production
Question 4. Which one of the following
tumour markers is not paired with the
correct malignancy?
A) Carcinoembryonic antigen (CEA) and
colonic carcinoma
B) Alpha-fetoprotein (AFP) and bladder
carcinoma
C) Prostate-specific antigen (PSA) and
prostatic carcinoma
D) CA-125 and ovarian carcinoma
E) Human chorionic gonadotrophin
(HCG) and choriocarcinoma
25
What should the next step in her treatment
be?
A) Perform a full septic screen and start
antibiotics if cultures are positive
B) Take blood cultures and start broadspectrum antibiotics immediately
C) Insert a central line to allow
measurement of central venous pressure
D) Administer granulocyte-colony
stimulating factor (G-CSF) to stimulate
white blood cell production
E) Discharge her home to prevent her
contracting a hospital-acquired infection
Question 6. A 73-year-old man with
known prostate cancer is admitted to
hospital with a 24-hour history of back
pain and difficulty walking. Examination
of the lower limbs reveals bilaterally
increased tone with reduced power, brisk
reflexes and extensor plantars. What
would the most useful investigation be?
A) Plain X-ray of the spine
B) Spinal CT scan
C) Spinal MRI scan
D) Nerve conduction studies
E) Electromyography
Question 7. A 76-year-old man
undergoing treatment for lung cancer
attends hospital with polyuria, thirst and
mild confusion. Initial blood tests reveal a
corrected calcium level of 3.02 mmol/l
(reference range 2.12-2.62). What is the
most important initial treatment?
A) Intravenous saline
B) Intravenous bisphosphonate
C) Intravenous furosemide
D) Calcium gluconate
E) Calcitonin
Question 8. A 68-year-old man with
small-cell lung cancer complains of
worsening shortness of breath and a
persistent headache. On examination, the
jugular venous pressure is raised but nonpulsatile, prominent vessels are seen on
the chest wall and there is facial oedema.
What is the most likely diagnosis?
A) Congestive heart failure
B) Lymphangitis carcinomatosa
C) Nephrotic syndrome
D) Superior vena caval obstruction
E) Side-effects of radiotherapy
26
Question 9. A 55-year-old woman with
breast cancer is admitted to hospital
complaining of headaches which are worst
in the morning, together with nausea and
vomiting. The result of a CT head scan is
show:
Which one of the following would be the
best initial treatment?
A) Furosemide
B) Dexamethasone
C) Radiotherapy
D) Chemotherapy
E) Surgical resection of the abnormal
lesions
Question 10. Which of the following sideeffects is least likely to result from
radiotherapy?
A) Pulmonary fibrosis
B) Erythema and desquamation of the skin
C) Ischaemic heart disease
D) Peripheral neuropathy
E) Diarrhoea
Question 11. Which one of the following
statements about the drug tamoxifen is
true?
A) It commonly causes neutropenia
B) It should be offered to all patients with
breast cancer
C) It is an alkylating agent
D) Evidence supports its use in metastatic
breast cancer only
E) It exerts its effect by acting as an
oestrogen receptor antagonist
Chapter
11
PALLIATIVE CARE AND
PAIN MANAGEMENT
Answers page 144
Question 1. All of the following features
except one suggest a neuropathic origin of
pain. Which is the exception?
A) Occurs in an area of sensory loss
B) Is burning in nature
C) Occurs in response to non-painful stimuli
D) Has a better response to non-steroidal antiinflammatory drugs (NSAIDs) than tricyclic
antidepressants
E) Is associated with abnormal unpleasant
sensations
Question 2. Which one of the following pain
treatments is least appropriately paired with
the type of pain?
A) Bone pain Non-steroidal anti-inflammatory
drugs (NSAIDs)
B) Liver capsule pain Opioids
C) Raised intracranial pressure Corticosteroids
D) Neuropathic pain Anticonvulsants
E) Abdominal colic Antispasmodics
Question 3. A patient with widespread
metastatic prostatic carcinoma complains of
troublesome, constant pain at multiple sites.
He takes regular paracetamol, codeine and
ibuprofen at full dose but continues to
experience severe pain. According to the WHO
analgesic ladder, what is the most appropriate
next step in his pain management?
A) Replace codeine with a strong opioid such
as morphine
B) Replace ibuprofen with a strong opioid such
as morphine
C) Replace ibuprofen with an alternative nonsteroidal anti-inflammatory drug (NSAID)
such as diclofenac
D) Add dihydrocodeine to existing
medications
E) Add a neuropathic agent to existing
medications
Question 4. Which one of the following
statements regarding side-effects of strong
opioids used in cancer pain is true?
A) Nausea and vomiting tend to worsen with
increased duration of treatment
27
B) Excessive salivation is common
C) Constipation should be managed with a
reduction in dose rather than laxative agents
D) Respiratory depression is more likely to be
a problem in acute dosing than with patients on
regular opioids
E) Sedation and drowsiness are uncommon in
patients under 65 years
Question 5. A patient with metastatic
pancreatic carcinoma was admitted to hospital
from home with a 4-day history of worsening
drowsiness and confusion. Her dose of 12hourly controlled-release (CR) morphine had
been doubled 1 week previously, as her pain
had been poorly controlled. On admission she
has a Glasgow Coma score of 13 (E3 M6 V4),
with small pupils and periodic myoclonic
jerks. After 24 hours free of opiates she is now
much more alert but starting to experience pain
again. Which of the following would be the
best strategy for managing her pain?
A) Restart her CR morphine at the same dose
and also prescribe 'as required' doses of
immediate-release (IR) morphine
B) Restart her CR morphine at the same dose
but withhold 'as required' doses
C) Reduce the CR morphine to the previous
dose (prior to adjustment) and also prescribe
'as required' doses of IR morphine
D) Change from CR morphine to regular IR
morphine at a lower equivalent dose and also
prescribe 'as required' doses of IR morphine
E) Change from CR morphine to a fentanyl
patch at a lower equivalent dose and also
prescribe 'as required' doses of oral IR
morphine
Question 6. A patient with advanced bowel
cancer presents with persistent large-volume
vomiting and severe colicky abdominal pain.
Abdominal imaging reveals multiple levels of
gastrointestinal obstruction. Which one of the
following antiemetics is contraindicated?
A) Cyclizine
B) Metoclopramide
C) Levomepromazine
D) Ondansetron
E) Prochlorperazin
Chapter
12 INFECTIOUS DISEASES
Answers page 146
Question 1. A gap-year student returns
from the Far East with a temperature of
39°C. You take a detailed history of
exposures. Which one of the following
exposures is incorrectly paired with the
resulting infection?
A) Fresh-water swimming Schistosomiasis
B) Unprotected sexual contact Hepatitis B
C) Unpasteurised milk Leptospirosis
D) Tick bite Typhus
E) Mosquito bite Dengue fever
Question 2. All of the following except
one are infective causes of splenomegaly.
Which is the exception?
A) Brucellosis
B) Falciparum malaria
C) Giardiasis
D) Leishmaniasis
E) Subacute bacterial endocarditis
Question 3. A 24-year-old medical
student returns from her elective in
Mauritius and attends the tropical diseases
unit with an intensely itchy rash on her
foot, present since just before she came
home. She admits to having walked
barefoot a lot while abroad. On
examination, there is a serpiginous linear
lesion on the sole of her foot. It is now 7-8
cm in length, and she says that it has been
elongating. What is the most likely
diagnosis?
A) Staphyloccus aureus cellulitis
B) Cutaneous larva migrans
C) Scabies
D) Onchocerciasis
E) Strongyloidiasis
28
Question 4. A traveller, returning from
East Africa to the UK with a fever of
38.7°C, has a full blood count performed
as part of his initial work-up. This reveals
an eosinophilia (eosinophil count 0.6 ×
109). Which one of the following
diagnoses is least consistent with this
finding?
A) Schistosomiasis
B) Strongyloidiasis
C) Ascariasis
D) Tuberculosis
E) Filariasis
Question 5. Regarding measles, which
one of the following statements is correct?
A) The incubation period is 5 days to
onset of rash
B) Koplik's spots on the retina are
pathognomonic
C) Antibiotics should be given to prevent
the development of bacterial pneumonia
D) Infants are protected for the first 6
months of life by passive immunity from
maternal antibodies
E) Children with the disease should be
offered vaccination as soon as they
recover
Question 6. Which of the following
pairings of childhood exanthems and their
complications is incorrect?
A) Rubella Myocarditis
B) Measles Subacute sclerosing
panencephalitis (SSPE)
C) Human erythrovirus 19 (parvovirus
B19) Anaemia
D) Mumps Orchitis
E) Chickenpox Pneumonia
Question 7. A 76-year-old gentleman
presents to his general practitioner with a
2-day history of burning discomfort
around the left side of his chest. On
examination, you find a vesicular rash in a
band-like distribution around his left side:
Question 10. All of the following
statements about cytomegalovirus (CMV)
are true except one. Which is the
exception?
A) In immunosuppressed patients,
infection may cause sight-threatening
retinitis
B) In pregnant women, the infection may
have neurological sequelae for the fetus
C) In healthy young adults, infection is
usually asymptomatic
D) The peak incidence of acquisition is in
the sixth decade
E) The virus is shed in saliva, urine and
semen
Which of the following is the most likely
causative organism?
A) Treponema pallidum
B) Herpes simplex virus
C) Varicella zoster virus
D) Staphylococcus aureus
E) Human erythrovirus 19 (parvovirus
B19)
Question 11. A 19-year-old male attends
his general practitioner 3 days after
returning from back-packing in South-east
Asia. He complains of headache,
generalised aches and pains, painful eye
movements and a rash. He recalls a
number of mosquito bites in the week
prior to returning home but appears to
have taken appropriate antimalarial
prophylaxis throughout the trip and since
his return. On examination, he has
lymphadenopathy, a temperature of
38.2°C, and a maculopapular morbilliform
rash on his trunk. Which one of the
following diagnoses is most likely?
A) Salmonella
B) Schistosomiasis
C) Leishmaniasis
D) Dengue
E) Strongyloidiasis
Question 8. Which one of the following
statements about smallpox is true?
A) It has been used as a bioterrorist agent
B) Infection carries a mortality rate of
90%
C) The vesiculo-pustular rash is most
dense on the trunk, with sparing of the
extremities
D) No successful vaccine has ever been
developed
E) It is caused by a DNA poxvirus
Question 9. A 14-year-old boy, living in
London, is brought to the hospital accident
and emergency department by his mother
with a 6-day history of malaise, fever and
sore throat. He gives no history of recent
foreign travel. His temperature is 38°C.
On examination, you note that he has an
inflamed pharynx, cervical
lymphadenopathy, a tender enlarged liver
and a palpable spleen. What is the most
likely diagnosis?
A) Infectious mononucleosis
B) Malaria
C) Influenza
D) Mumps
E) Listeriosis
29
Question 12. Fifteen patients in a large
care of the elderly unit in the UK develop
nausea and vomiting in the space of 3
days. A number of nursing and medical
staff also report vomiting. Which one of
the following agents is the most likely
cause of the outbreak?
A) Meticillin-resistant Staphylococcus
aureus (MRSA)
B) Clostridium difficile
C) E. coli
D) Calicivirus
E) Norovirus
Question 13. Infection with
Staphylococcus aureus is commonly
responsible for all of the following
conditions except one. Which is the
exception?
A) Endocarditis
B) Pneumonia
C) Hepatitis
D) Osteomyelitis
E) Cellulitis
Question 14. A 16-year-old girl is brought
to the hospital accident and emergency
department by her parents, having
developed a high fever, headache and sore
throat over the last 12 hours. She tells you
that she has just finished menstruating. On
examination, she has a temperature of
38.6°C, blood pressure of 90/40 mmHg
and a generalised erythematous blanching
rash. There are no signs of meningism or
petechiae. Which of the following is the
most likely diagnosis?
A) Infectious mononucleosis
B) Staphylococcal toxic shock syndrome
C) Scarlet fever
D) Rubella
E) Rheumatic fever
Question 15. Which of the following
conditions is least likely to occur as a
consequence of streptococcal infection?
A) Scarlet fever
B) Endocarditis
C) Rheumatic fever
D) Glomerulonephritis
E) Haemolytic uraemic syndrome
30
Question 16. All of the following except
one are recognised clinical features of
brucellosis. Which is the exception?
A) Pyoderma gangrenosum
B) Uveitis
C) Meningitis
D) Endocarditis
E) Septic arthritis
Question 17. A 24-year-old student
presents to the dermatology clinic with an
expanding red macule on her left calf; this
appeared 2 weeks previously, shortly after
returning from holiday in Connecticut,
USA. She reports that the lesion has been
progressively increasing in size since it
appeared. On examination, the lesion now
measures approximately 15 cm across and
appears to be clearing from the centre
outwards. Which of the following is the
likely diagnosis of her rash?
A) Necrobiosis lipoidica
B) Erythema nodosum
C) Pyoderma gangrenosum
D) Cellulitis
E) Erythema chronicum migrans
Question 18. With reference to the patient
from the previous question (Q17), the
diagnosis of Lyme borreliosis is confirmed
by polymerase chain reaction (PCR)
testing of her urine. She is not pregnant
and has no known allergies. Which of the
following is the most appropriate
treatment?
A) 14-day course of doxycycline
B) 1-month course of clarithromycin
C) 1-month course of metronidazole
D) Observation only
E) 14-day course of penicillin
Question 19. A 45-year-old male who is a
keen water-skier is brought to the
infectious diseases unit with a 24-hour
history of jaundice, fever and nosebleeds.
There is no history of recent foreign travel.
On examination, his temperature is 39°C,
he is deeply jaundiced and has an enlarged
liver. His conjunctivae are hyperaemic and
there is a marked purpuric rash on the
trunk and limbs. Blood results are as
follows:
Question 21. Which of the following
statements about staphylococcal food
poisoning is false?
A) Dairy products and cooked meat are an
important source of infection
B) Refrigeration of food products
encourages the growth of heat-stable
enterotoxins
C) Symptoms arise within 1-6 hours of
ingestion of contaminated foodstuffs
D) Vomiting is a more common symptom
than diarrhoea
E) A marked neutrophilia is common
Question 22. Which one of the following
statements is incorrect with regard to
Escherichia coli?
A) It is the most common cause of
travellers' diarrhoea
B) The incubation period of
enterotoxigenic E. coli (ETEC) is 1-2 days
C) Enteropathic E. coli (EPEC) is an
important cause of infant diarrhoea
D) Enterohaemorrhagic E. coli (EHEC)
may lead to haemolytic uraemic syndrome
E) Entero-invasive E. coli (EIEC) causes
symptoms through production of an
enterotoxin
Which of the following is the most likely
diagnosis?
A) Listeriosis
B) Hepatitis A
C) Meningococcal sepsis
D) Weil's disease (leptospirosis)
E) Infectious mononucleosis (Epstein-Barr
virus)
Question 20. Which type of transmission
does typhoid fever demonstrate?
A) Droplet spread
B) A bite from an infected animal vector
C) Faecal-oral
D) Sexual
E) Blood-borne, i.e. needlestick injuries
31
Question 23. Which of the following
antibiotics is used as first-line therapy for
symptomatic infection with Clostridium
difficile?
A) Co-amoxiclav
B) Metronidazole
C) Cefuroxime
D) Clarithromycin
E) Clindamycin
Question 24. Which one of the following
gastrointestinal infections does not cause
bloody diarrhoea?
A) Cholera
B) Salmonella
C) Shigella
D) Entamoeba histolytica
E) Campylobacter
Question 25. Which one of the following
statements is correct regarding the
correction of fluid and electrolyte balance
in the patient with acute diarrhoea?
A) 48 hours of diarrhoea in the average
adult will result in a fluid deficit of half a
litre
B) Intravenous fluid replacement is
preferable to oral rehydration for most
patients with acute diarrhoea
C) Oral rehydration solution (ORS)
contains carbohydrate, sodium, potassium
and chloride
D) Prolonged bouts of diarrhoea result in
the development of a metabolic alkalosis
E) Infants with gastroenteritis should not
be breastfed while they have diarrhoea
Question 26. A sales executive, recently
returned to the UK from Ukraine, is
referred to the local infectious diseases
unit by his general practitioner with a sore
throat of unusual appearance. On arrival,
he is tachycardic with a heart rate of 110
bpm, and has a mild pyrexia of 37.7°C.
There is a slight blood-stained discharge at
the nasal orifices. His neck is visibly
swollen. Examination of the mouth reveals
a greyish-green membrane overlying the
tonsils, which does not come off with
gentle scraping with the tongue depressor.
What is the likely diagnosis?
A) Streptococcal throat infection
B) Diphtheria
C) Oral candidiasis
D) Mumps
E) Tonsillar carcinoma
Question 27. A 45-year-old Indian man
visiting his family in the UK is brought to
the infectious diseases unit by his son who
is concerned about the appearance of what
he terms a 'rash' on his father's back. On
examination, there are three well-defined
hypopigmented macules that are
completely anaesthetic. You note that both
the patient's median and ulnar nerves are
palpably thickened bilaterally, with
variable sensory loss distal to the wrists in
both upper limbs. Which of the following
is the most likely underlying diagnosis?
A) Toxoplasmosis
B) Botulism
C) Cutaneous leishmaniasis
D) Leprosy
E) Tuberculosis
Question 28. With regard to the patient in
the previous question (Q27), which one of
the following investigations will confirm
the diagnosis of leprosy?
A) Leprosy serology
B) Polymerase chain reaction (PCR) of
serum for Mycobacterium leprae DNA
C) Microscopy of split skin smears
D) Nasal swab
E) Blood culture
Question 29. Which of the following
antimicrobial agents is commonly used in
the treatment of leprosy?
A) Clindamycin
B) Chloroquine
C) Chloramphenicol
D) Rifampicin
E) Penicillin V
Question 30. Which of the following
organisms is responsible for cat scratch
disease?
A) Toxoplasma gondii
B) Chlamydia psittaci
C) Rickettsia rickettsii
D) Bartonella henselae
E) Coxiella burnetti
32
Question 31. A 19-year-old gap-year
student returns to the UK after working for
6 weeks in West Africa on a charity
project. Shortly after returning, he presents
to his general practitioner with a 4-day
history of intermittent fevers, tiredness,
headache and general malaise. On
examination, he is mildly jaundiced. His
heart rate is 110 bpm and temperature is
38.2°C. He has a palpable spleen and a
tender liver edge but no rash or
lymphadenopathy.
Question 34. Which of the following
statements regarding the treatment and
chemoprophylaxis of malaria is correct?
A) Chloroquine resistance is rare
B) Falciparum malaria is still largely
sensitive to quinine
C) Chemoprophylaxis with doxycycline
should be continued for 7 days after
leaving a malarious area
D) Quinine is associated with troublesome
neuropsychiatric side-effects
E) Fansidar is suitable for
chemoprophylaxis
Question 35. Which one of the following
statements regarding visceral
leishmaniasis is incorrect?
A) It is transmitted from human to human
by the sandfly
B) Both splenomegaly and hepatomegaly
are common clinical features
C) Dermatological manifestations include
black discoloration of the skin
D) Blood tests typically reveal
thrombocytosis and neutrophilia
E) The treatment of choice is pentavalent
antimony
Which one of the following is the most
likely diagnosis?
A) Leishmaniasis
B) Falciparum malaria
C) HIV seroconversion illness
D) Q fever
E) Infectious mononucleosis
Question 32. All of the following except
one are potential complications of
falciparum malaria. Which is the
exception?
A) Convulsions
B) Acute renal failure
C) Nephrotic syndrome
D) Hypoglycaemia
E) Metabolic acidosis
Question 33. Which one of the following
investigations is diagnostic for malaria?
A) Thin blood film
B) Full blood count
C) Blood culture
D) Serology for P. falciparum
E) Coagulation screen
33
Question 36. A 19-year-old woman is
referred by her general practitioner to the
local dermatology department, 3 months
after returning from a trip to Central
America. She has an ulcer on the lateral
aspect of her calf, which has failed to heal
with a 2-week course of flucloxacillin. It
began 1 month previously as a raised red
'lump', then increased in size to about 6
cm, before ulcerating and developing a
crust. Swabs of the ulcer have grown skin
commensals only, but a biopsy shows
numerous parasites. What is the most
likely diagnosis?
A) Toxoplasmosis
B) Cutaneous leishmaniasis
C) Babesiosis
D) Plasmodium vivax malaria
E) Trypanosomiasis
Question 37. Infection with which one of
the following organisms is most
commonly associated with cardiac
complications, including dilated
cardiomyopathy and conduction defects?
A) Toxoplasma gondii
B) Trypanosoma cruzi
C) Leishmania donovani
D) Ancylostoma braziliense
E) Cytomegalovirus
Question 38. Which of the following is a
vector for African trypanosomiasis
(African sleeping sickness)?
A) African sandfly
B) Tsetse fly
C) Mosquito
D) Ixodes tick
E) Freshwater snail
Question 39. With regard to
toxoplasmosis, which one of the following
statements is incorrect?
A) Domestic cats are important hosts in
the life cycle of Toxoplasma gondii
B) Infection is asymptomatic in the
majority of individuals
C) Congenital toxoplasmosis is
characterised by retinochoroiditis,
microcephaly and hydrocephalus
D) Serological tests are available for the
detection of past and present infection
with Toxoplasma gondii
E) The most common presenting features
of acquired toxoplasmosis are fever,
photophobia and a non-specific rash
Question 40. Which one of the following
statements regarding amoebiasis is
correct?
A) The parasite typically invades the small
bowel
B) The incubation period of the
Entamoeba histolytica cyst is 48 hours
C) Clinically, the disease manifests as
diarrhoea alternating with constipation,
with the presence of blood and mucus
D) Diagnosis is made on stool culture
34
E) The infection is responsive to penicillin
antibiotics
Question 41. Which one of the following
features is least characteristic of
strongyloidiasis?
A) Abdominal pain
B) Urticaria
C) Diarrhoea
D) Motile larvae on stool microscopy
E) Neutrophilia
Question 42. A 53-year-old man, recently
returned to the UK from a holiday in
Indonesia, presents with a tender,
erythematous right leg and thigh. On
examination, his right leg is swollen,
warm, painful and red along the length of
its medial aspect. There is marked
oedema. He also has an acutely tender
right testicle and swelling of the right
inguinal lymph nodes. A full blood count
reveals eosinophilia. Which one of the
following is the most likely diagnosis?
A) Acute streptococcal cellulitis
B) Filiariasis
C) Cutaneous larva migrans infection
D) Tinea pedis
E) Histoplasmosis
Question 43. Which of the five senses is
most commonly affected by infection with
Onchocerca volvulus (onchocerciasis)?
A) Vision
B) Taste
C) Hearing
D) Touch
E) Smell
Question 44. The following are all
recognised sequelae of chronic infection
with schistosomiasis except one. Which is
the exception?
A) Hydronephrosis
B) Oesophageal varices
C) Splenomegaly
D) Urticaria
E) Recurrent urinary tract infection
Chapter
13
HIV INFECTION AND
THE AIDS
Answers page 153
Question 1. Which of the following best
describes the human immunodeficiency
virus (HIV)?
A) Single-stranded RNA virus
B) Double-stranded RNA virus
C) Single-stranded DNA virus
D) Double-stranded DNA virus
E) Prion
Question 2. What is the main mode of
transmission of HIV in northern Europe
and the United States?
A) Blood transfusion
B) Heterosexual transmission
C) Homosexual transmission
D) Intravenous drug use
E) Vertical (mother to child) transmission
Question 3. Which of the following
exposures has the highest transmission risk
for HIV?
A) Genital mucous membrane contact
B) Intravenous drug use using a
contaminated needle
C) Being born to a mother who is HIVpositive but not on highly active
antiretroviral therapy (HAART)
D) Homosexual intercourse between two
men
E) Receipt of infected blood products
Question 4. Which one of the following
options best characterises the virological
and immunological progression of HIV
infection in the first 4-8 weeks following
exposure?
A) CD4 count rises, viral load falls
B) CD4 count falls, viral load rises
C) Both CD4 count and viral load rise
D) Both CD4 count and viral load fall
E) CD4 count remains stable, viral load
rises
35
Question 5. Which one of the following is
not an AIDS-defining disease?
A) Pulmonary tuberculosis
B) Kaposi's sarcoma
C) Cytomegalovirus retinitis
D) Oropharyngeal candidiasis
E) Cerebral toxoplasmosis
Question 6. Which one of the following
statements regarding Cryptosporidium
infection is incorrect?
A) Patients typically present with profuse,
bloody diarrhea
B) It tends to occur when the CD4 count is
< 200 cells/mm3
C) Definitive diagnosis is made on stool
microscopy
D) Complications include cholecystitis,
cholangitis and pneumonitis
E) Cryptosporidium is a protozoal enteric
pathogen
Question 7. Which one of the following
pathogens is least likely to be responsible
for chronic diarrhoea in the HIV-positive
patient?
A) Isospora
B) Mycobacterium avium intracellulare
C) Microsporidium
D) Cytomegalovirus
E) Toxoplasma
Question 8. Which one of the following
options would not be supportive of a
diagnosis of Pneumocystis carinii
(jirovecii) pneumonia?
A) 2-3-week history of shortness of breath
B) A cough productive of green sputum
C) Marked oxygen desaturation on
exercise
D) A lack of response to penicillin
antibiotics
E) Pyrexia
Question 9. Which one of the following
statement regarding cryptococcal
meningitis is true?
A) The organism is identified on
cerebrospinal fluid (CSF) microscopy with
Ziehl-Neelsen staining
B) The majority of affected patients have a
CD4 count > 200 cells/mm3
C) Deafness and blindness are the most
common complications
D) Neck stiffness is invariably present
E) Penicillin is the treatment of choice
Question 10. A 27-year-old HIV-positive
patient with a CD4 count of 20 cells/mm3
presents to the hospital accident and
emergency department with visual
difficulties. He reports a 6-week history of
flashing lights and dark 'clouds' floating in
front of his eyes. In the past fortnight he
has experienced problems with driving,
narrowly escaping a collision with a
cyclist whom he did not see on the road
beside him. On examination, the
conjunctivae are injected and fundoscopy
reveals haemorrhagic exudates near the
retinal vessels. What is the likeliest
diagnosis?
A) Bacterial conjunctivitis
B) Herpes simplex keratitis
C) Anterior uveitis
D) Cytomegalovirus (CMV) retinitis
E) Acute retinal necrosis
Question 11. A 37-year-old homosexual
male who is HIV-positive (CD4 count 300
cells/mm3) is found on a routine visit to
the infectious diseases clinic to have
purplish-blue papules across the bridge of
his nose; these have appeared in the last 4
months. He is otherwise asymptomatic. On
examination, he has cervical
lymphadenopathy and
hepatosplenomegaly. Which one of the
following diagnoses is most likely?
A) Seborrhoeic dermatitis
B) Disseminated cutaneous herpes simplex
C) Molluscum contagiosum
D) HIV-associated lymphoma
E) Kaposi's sarcoma
36
Question 12. Which one of the following
is not a characteristic side-effect of
treatment with nucleoside reverse
transcriptase inhibitors (NRTIs)?
A) Cranial nerve palsies
B) Peripheral neuropathy
C) Pancreatitis
D) Anaemia
E) Lipoatrophy
Question 13. Which one of the following
statements about protease inhibitors (PIs)
is incorrect?
A) They act by preventing posttranslational cleavage of polypeptides into
functional viral proteins
B) They cause glucose intolerance and
frank diabetes in a proportion of patients
C) Metabolism is via the P450 system of
enzymes
D) They improve the lipid profile of most
patients by lowering total cholesterol and
low-density lipoprotein (LDL), and by
raising high-density lipoprotein (HDL)
E) Monitoring of plasma levels helps to
optimise antiviral effect and reduce
toxicity
Question 14. All of the following except
one are advantages of non-nucleoside
reverse transcriptase inhibitors (NNRTIs)
over other anti-HIV agents. Which is the
exception?
A) Once-daily dosing
B) Good oral bioavailability
C) Lower tablet numbers than with NRTIs
D) No association with fat redistribution
E) Low incidence of drug rashes
Question 15. Which one of the following
opportunistic infections is incorrectly
matched with its appropriate prophylactic
agent?
A) Tuberculosis Rifampicin and isoniazid
B) Toxoplasmosis Erythromycin
C) Pneumocystis carinii (jirovecii)
pneumonia Co-trimoxazole
D) Cryptococcus Itraconazole
E) Mycobacterium avium intracellulare
(MAI) Azithromycin
Chapter
14
SEXUALLY TRANSMITTED
INFECTIONS
Answers page 156
Question 1. Worldwide, which of the
following is the most common curable
sexually transmitted infection (STI)?
A) Syphilis
B) Gonorrhoea
C) Chlamydia
D) Trichomonas vaginalis
E) HIV
Question 2. A 22-year-old heterosexual
male presents to the STI clinic with a 2week history of purulent urethral discharge
and dysuria. He has been sexually active
in the past month with two new partners.
Gram-stained smear of urethral exudate
shows Gram-negative diplococci, along
with prominent polymorphonuclear cells.
What is the most likely cause for the
gentleman's urethral discharge?
A) Non-gonococcal urethritis
B) Syphilis
C) Genital warts
D) Gonorrhoea
E) Staphylococcal infection
Question 3. A 23-year-old girl presents to
her GP, with a 3-day history of a painful
rash over her perineum. This was preceded
by 2 days of 'flu-like symptoms'. She has
been sexually active with a new partner for
the last 6 weeks and takes the oral
contraceptive pill, but does not use barrier
contraception. On examination, she has a
cluster of small vesicles on both labia
majora. Which is the most appropriate
next investigation?
A) High vaginal swab
B) Urethral swab
C) HIV test
D) Swab of the contents of a vesicle
E) Urine microscopy and cultu
37
Question 4. Which of the following
genotypes of human papillomavirus
(HPV) is associated with dysplastic
conditions and cancers of the genital tract?
A) HPV 6 and 11
B) HPV 16 and 18
C) HPV 10 and 15
D) HPV 6 only
E) HPV 10 and 13
Question 5. A 34-year-old Englishwoman
is referred to the local gynaecology
outpatient department with a 2-year
history of intermittent pelvic pain. In her
history, she also describes dyspareunia and
occasional post-coital bleeding. She and
her husband have been trying to conceive
without success for the past 18 months.
Examination of the external genitalia is
unremarkable. On per vaginam
examination, you see an inflamed cervix,
which is partly covered by a mucopurulent
discharge. Which of the following
diagnoses is most likely?
A) Syphilis
B) Herpes simplex type 1 infection
C) Herpes simplex type 2 infection
D) Trichomoniasis
E) Chlamydial infection
Question 6. A 35-year-old lady is referred
to Gynaecology triage with a 7-day history
of a profuse, foul-smelling vaginal
discharge. She is very distressed by this, as
the quantities produced are necessitating
the use of sanitary towels. On speculum
examination, the external genitalia are
entirely normal but the vagina itself is
slightly inflamed. High and low vaginal
swabs are taken, as well as a wet film of
some of the discharge, which is sent
immediately for microscopy. Motile
flagellate organisms are seen in large
numbers. What is the diagnosis?
A) Trichomoniasis
B) Bacterial vaginosis
C) Herpes simplex type 2 infection
D) Chlamydial infection
E) Gonorrhoea
Question 7. Which one of the following is
not a feature of secondary syphilis?
A) Condylomata lata
B) Meningitis
C) Generalised lymphadenopathy
D) A maculo-papular rash on the trunk and
limbs
38
E) Syphilitic chancre
Question 8. Which one of the following is
not a feature of congenital syphilis?
A) Hutchinson's incisors
B) Saddle nose
C) Sabre tibia
D) Webbed neck
E) Mulberry molars
Question 9. A 17-year-old female
reluctantly attends her GP to discuss the
problem of a 2-month history of a whitish
vaginal discharge and vulval pruritus. She
is not sexually active and her only past
medical history is of acne, for which she
takes regular minocycline. On
examination, her external genitalia are
inflamed and traces of a curd-like
discharge can be seen at the vaginal
orifice. What is the most likely diagnosis?
A) Human papillomavirus infection
B) Vaginal candidiasis
C) Chlamydial infection
D) Toxic shock syndrome (TSS)
E) Gonorrhoea
Chapter
15
CLINICAL BIOCHEMISTRY
AND METABOLISM
Answers page 158
Question 1. A typical adult male has a
total body water of 40 litres. How much of
this is located within the extracellular fluid
compartment?
A) 25 litres
B) 15 litres
C) 9 litres
D) 6 litres
E) 3 litres
Question 2. The most abundant cation
within the intracellular fluid compartment
is:
A) Sodium
B) Chloride
C) Potassium
D) Hydrogen
E) Calcium
Question 3. A blood sample is analysed
after significant in vitro haemolysis has
occurred. Which of the following spurious
results is most likely to occur in the
measured electrolytes?
A) High sodium
B) High potassium
C) Low sodium
D) Low potassium
E) High chloride
Question 4. The total body content of
which ion is a principal determinant of
ECF volume?
A) Sodium
B) Potassium
C) Calcium
D) Chloride
E) Bicarbonate
39
Question 5. What proportion of filtered
sodium is normally reabsorbed within the
proximal tubule?
A) 90%
B) 65%
C) 40%
D) 25%
E) 5%
Question 6. Which one of the following
clinical signs would be an unexpected
finding in the presence of hypovolaemia?
A) Low jugular venous pulse
B) Reduced skin turgor
C) Bradycardia
D) Postural hypotension
E) Reduced urine output
Question 7. The normal physiological
response to loss of sodium and water
comprises all of the following except one.
Which is the exception?
A) Enhanced conversion of
angiotensinogen to angiotensin I
B) Reduced glomerular filtration rate
C) Activation of the sympathetic nervous
system
D) Increased release of atrial natriuretic
peptide
E) Stimulation of thirst
Question 8. Which one of the following
clinical conditions would be least likely to
cause sodium and water excess?
A) Chronic renal failure
B) Nephrotic syndrome
C) Conn's syndrome
D) Congestive cardiac failure
E) Addison's disease
Question 9. The diuretic furosemide acts
principally at which of the following sites
within the kidney?
A) Glomerulus
B) Proximal tubule
C) Loop of Henle
D) Early distal tubule
E) Collecting ducts
Question 10. Which one of the following
metabolic abnormalities is most likely to
be caused by treatment with a thiazide
diuretic?
A) Hypocalcaemia
B) Hyponatraemia
C) Hyperkalaemia
D) Hypermagnesaemia
E) Hypoglycaemia
Question 11. Which one of the following
conditions is a cause of hypovolaemic
hyponatraemia?
A) Primary polydipsia
B) Hyperlipidaemia
C) Nephrotic syndrome
D) Syndrome of inappropriate ADH
secretion (SIADH)
E) Diuretic therapy
Question 12. During an employment
medical, a 59-year-old male is found to
have a plasma sodium of 126 mmol/l. He
is asymptomatic and clinical examination
reveals no abnormal findings other than
mild obesity. Further blood tests reveal a
plasma osmolality of 250 mmol/kg
(normal range 280-290 mmol/kg) and a
urine osmolality of 360 mmol/kg. Which
of the following is the likeliest diagnosis?
A) Diuretic abuse
B) Primary polydipsia
C) Nephrotic syndrome
D) Syndrome of inappropriate ADH
secretion (SIADH)
E) Cranial diabetes insipidus
Question 13. Aside from identifying and
treating possible underlying causes, what
is the most appropriate initial management
for the patient in the previous question
who has SIADH?
A) Infusion of 0.9% saline (normal saline)
B) Infusion of hypertonic saline
40
C) Increased oral salt intake
D) Fluid restriction of 1-1.5 litres per day
E) Demeclocycline therapy
Question 14. Which of the following
drugs is most likely to cause SIADH?
A) Metformin
B) Carbamazepine
C) Digoxin
D) Amiodarone
E) Alendronate
Question 15. Which one of the following
ECG changes is most typical of
hyperkalaemia?
A) Peaked P wave
B) Presence of U wave
C) ST segment depression
D) Peaked T wave
E) Narrowed QRS complex
Question 16. Which one of the following
would be most likely to produce
hypokalaemia (plasma K < 3.5 mmol/l)?
A) Addison's disease
B) Amiloride therapy
C) Conn's syndrome
D) Rhabdomyolysis
E) Acute renal failure
Question 17. Treatment with which one of
the following drugs is most likely to lead
to hyperkalaemia?
A) Bendroflumethiazide
B) Warfarin
C) Ramipril
D) Salbutamol
E) Calcium resonium
Question 18. Which one of the following
treatments for hyperkalaemia is not used
to lower the concentration of plasma
potassium?
A) Insulin
B) Salbutamol
C) Calcium resonium
D) Dialysis
E) Calcium gluconate
Question 19. Which one of the following
conditions would be most likely to cause a
normal anion gap metabolic acidosis?
A) Sepsis
B) Salicylate poisoning
C) Starvation
D) Diabetic ketoacidosis
E) Renal tubular acidosis
Question 20. The following laboratory
results are obtained from a patient on a
general surgical ward:
Urine pH: 5.5
What is the acid-base abnormality?
A) Raised anion gap metabolic acidosis
B) Normal anion gap metabolic acidosis
C) Metabolic alkalosis
D) Respiratory acidosis
E) Respiratory alkalosis
Question 21. Which one of the following
disorders is most likely to be responsible
for the results seen in the previous
question? (shown again below)
Urine pH: 5.5
A) Gastric outlet obstruction
B) Acute renal failure
C) Traveller's diarrhea
D) Hypothyroidism
E) Salicylate ingestion
Question 22. Which of the following
lipoproteins is primarily responsible for
reverse cholesterol transport?
A) Chylomicrons
B) Very low-density lipoprotein
41
C) Low-density lipoprotein
D) Intermediate-density lipoprotein
E) High-density lipoprotein
Question 23. Which one of the following
clinical features is more characteristic of
hypertriglyceridaemia than
hypercholesterolaemia?
A) Xanthelasma
B) Corneal arcus
C) Eruptive xanthomas
D) Achilles tendon xanthomas
E) Premature cardiovascular disease
Question 24. Regarding therapy with
HMGCoA reductase inhibitors (statins),
which one of the following statements is
true?
A) The incidence of rhabdomyolysis is
around 10%
B) In patients with hypercholesterolaemia
and risk factors for atherosclerosis, they
reduce the risk of coronary events but not
stroke
C) They inhibit endogenous cholesterol
synthesis
D) They lead to a modest reduction in
high-density lipoprotein (HDL) cholesterol
E) They have a greater effect on
triglyceride levels than low-density
lipoprotein (LDL) cholesterol levels
Question 25. Which one of the following
clinical features would be an unexpected
finding in an attack of acute intermittent
porphyria?
A) Acute abdominal pain
B) Bullae on sun-exposed areas of skin
C) Behavioural disturbance
D) Hypertension and tachycardia
E) Constipation
Chapter
16
KIDNEY AND URINARY
TRACT DISEASE
Answers page 163
Question 1. A renal bruit is associated
with which of the following disorders?
A) Conn's syndrome
B) Hypertensive nephropathy
C) Wegener's granulomatosis
D) Polyarteritis nodosa
E) Renal artery stenosis
Question 2. The following are all causes
of a palpably enlarged kidney except one.
Which is the exception?
A) Polycystic kidney disease
B) Renal cell carcinoma
C) Diabetic nephropathy
D) Hydronephrosis
E) Renal amyloidosis
Question 3. In a 70 kg man who has a
normal diet, what is the minimum volume
of urine production required each day to
excrete the daily solute load?
A) 15 ml
B) 50 ml
C) 100 ml
D) 500 ml
E) 1200 ml
Question 4. All of the following except
one would be expected to cause an
increase in serum urea concentration.
Which is the exception?
A) Severe burns
B) Reduction in glomerular filtration rate
(GFR)
C) Malnutrition
D) Dehydration
E) Upper gastrointestinal haemorrhage
42
Question 5. Serum creatinine is often used
as a surrogate measure of glomerular
filtration rate (GFR). Which of the
following best describes the relationship
between the change in serum creatinine
concentration and GFR?
A) Negative exponential
B) Direct proportion (positive linear)
C) Inverse proportion (negative linear)
D) Positive exponential
E) 'Build-up' exponential
Question 6. Which of the following is
freely filtered in the normal glomerulus?
A) Albumin
B) Glucose
C) Red blood cells
D) Platelets
E) Fibrinogen
Question 7. The presence of red cell casts
on urine microscopy is most likely to be
due to which one of the following?
A) Urethral trauma
B) Urinary tract infection
C) Bladder carcinoma
D) Ureteric stone
E) Post-streptococcal glomerulonephritis
Question 8. When serum creatinine is
used as a guide to renal excretory function,
which one of the following might lead to
under-estimation of the degree of renal
impairment?
A) Upper gastrointestinal haemorrhage
B) Reduced muscle bulk
C) Excessive dietary protein
D) Liver failure
E) Catabolic state
Question 9. Intravenous urography (IVU)
is superior to renal ultrasound for which
one of the following purposes?
A) Detection of urothelial malignancy
B) Assessing size and symmetry of
kidneys
C) Distinguishing between solid and cystic
masses
D) Identifying hydronephrosis
E) Assessing renal blood flow
Question 10. Which of the following
investigations provides most information
on the relative contribution of each kidney
to overall renal function?
A) Renal biopsy
B) Renal ultrasound
C) Magnetic resonance imaging (MRI) of
kidneys
D) Dimercaptosuccinic acid (DMSA)
isotope renogram
E) Renal arteriogram
Question 11. Which one of the following
is a contraindication to renal biopsy?
A) Haematuria
B) Kidneys < 60% normal size
C) Anaemia
D) Rapid deterioration in renal function
E) Angiotensin-converting enzyme (ACE)
inhibitor therapy
Question 12. Which of the following
organisms is the most common cause of
community-acquired lower urinary tract
infection (UTI)?
A) Escherichia coli
B) Staphylococcus aureus
C) Pseudomonas aeruginosa
D) Klebsiella spp.
E) Proteus mirabilis
Question 13. A 73-year-old man collapses
at home following a stroke. He is found 24
hours later, still lying on the floor. On
admission to hospital he appears only
mildly dehydrated but is in acute renal
failure. He is treated with IV fluids but
remains oliguric and his renal function
continues to deteriorate. Dipstick
urinalysis is strongly positive for blood but
43
microscopy reveals no red cells. What is
the most likely diagnosis?
A) Renal calculus
B) Urinary sepsis
C) Rapidly progressive glomerulonephritis
D) Renal infarction
E) Rhabdomyolysis
Question 14. A 68-year-old man reports
visible blood in his urine for the past 8
weeks. He is otherwise asymptomatic and
has no history of renal disease. Urine
culture has been negative on two
occasions and serum creatinine is within
the normal range. Repeat urinalysis shows:
Blood +++, Protein nil. Which of the
following pairs of investigations would
now be most appropriate for this patient?
A) Renal biopsy and intravenous
urography (IVU)
B) Cytological analysis of urine and
microscopy for acid-fast bacilli
C) Cystoscopy and renal ultrasound
D) Prostatic biopsy and prostate-specific
antigen (PSA) level
E) Anti-glomerular basement membrane
(GBM) and c-ANCA (antineutrophil
cytoplasmic antibodies)
Question 15. Which of the following
conditions would not account for the
finding of proteinuria on routine testing
with standard dipsticks?
A) Urinary tract trauma
B) Urinary tract infection
C) Transitional cell bladder carcinoma
D) Minimal change nephropathy
E) Microalbuminuria
Question 16. A 55-year-old man with
persistent proteinuria on dipstick analysis
has 3.6 g of protein in a 24-hour urine
collection. Which one of the following
disorders would account for this?
A) Persistent urinary tract infection
B) Acute tubular necrosis
C) Transitional cell carcinoma
D) Chronic interstitial nephritis
E) Focal segmental glomerulosclerosis
Question 17. Which of the following
abnormalities is most commonly
associated with the nephrotic syndrome?
A) Impaired clotting
B) Lymphatic obstruction
C) Excessive urinary sodium loss
D) Centripetal obesity
E) Hypercholesterolaemia
Question 18. Which of the following is
least likely to cause polyuria?
A) Polydipsia
B) Cranial diabetes insipidus
C) Lithium therapy
D) Hypocalcaemia
E) Diabetes mellitus
Question 19. Anticholinergics are most
useful in the treatment of which of the
following patterns of incontinence?
A) Urge incontinence
B) Stress incontinence
C) Overflow incontinence
D) Continual incontinence
E) Neurogenic incontinence
Question 20. A patient complains of
erectile dysfunction. He is taking the
following regular medications. Which one
is most likely to be responsible?
A) Valsartan
B) Ibuprofen
C) Sildenafil
D) Fluoxetine
E) Atenolol
44
Question 21. A patient presents for the
first time with renal failure and no
previous blood results are available.
Which of the following features would
most strongly suggest chronic impairment
of renal function?
A) Presence of haematuria and proteinuria
B) Serum potassium > 6.5 mmol/l
C) Urine output < 500 ml/day
D) Bilateral small kidneys on renal
ultrasound
E) Clinical evidence of dehydration
Question 22. Which of the following
drugs is most likely to increase the risk of
renal failure in a patient receiving
intravenous X-ray contrast for a
radiological procedure?
A) Heparin
B) Ibuprofen
C) Insulin
D) Diazepam
E) N-acetylcysteine
Question 23. A patient is diagnosed with
pre-renal acute renal failure. She is taking
the drugs listed below. Which one is least
likely to worsen her condition?
A) Furosemide
B) Lisinopril
C) Diclofenac
D) Amoxicillin
E) Bendroflumethiazide
Question 24. What is the main
physiological function of the medullary
concentration gradient?
A) Promotes water reabsorption from
urine
B) Secretes water into urine
C) Increases glomerular filtration rate
(GFR)
D) Promotes sodium reabsorption from
urine
E) Controls renal vasomotor tone
Question 25. A previously well patient is
admitted to the renal ward with severe
acute renal failure and the following blood
results:
She is treated with 20 units of intravenous
Actrapid insulin and 50 ml of 50%
dextrose, as well as salbutamol nebulisers.
Her blood tests are repeated 2 hours later
and show:
????NOT FOUND IN THE WEB SITE???????
Which of the following is the most
appropriate treatment at this stage to
reduce her serum potassium
concentration?
A) A further 20 units of soluble shortacting insulin (Actrapid) with 50 ml of
50% dextrose
B) IV calcium gluconate
C) IV sodium bicarbonate 1.26%
D) Calcium resonium
E) Haemodialysis
Question 26. A 62-year-old lady presents
in acute renal failure with severe bilateral
loin pain. A renal tract ultrasound shows
dilatation of both ureters and dilatation of
the collecting system within both kidneys,
probably due to retroperitoneal fibrosis.
Blood results are shown below:
Which of the following is the most
appropriate treatment?
A) Haemodialysis
B) Continuous veno-venous
haemofiltration (CVVH)
C) Bilateral nephrostomies
D) 1.5 litre/day fluid restriction
E) Suprapubic bladder catheterisation
45
Question 27. Which of the following
biochemical abnormalities in venous blood
is least likely to be present in a patient
with untreated chronic renal failure?
A) Reduced bicarbonate
B) Elevated parathyroid hormone (PTH)
C) Reduced phosphate
D) Elevated cholesterol
E) Reduced calcium
Question 28. Which of the following
statements about the management of
anaemia in patients with chronic renal
failure is most accurate?
A) Treatment with human recombinant
erythropoietin is only beneficial in patients
with a subnormal plasma erythropoietin
level
B) Target haemoglobin should be 130-140
g/l to achieve maximal benefit
C) Transferrin saturation should be
maintained below 20% to avoid iron
overload
D) Patients not receiving dialysis should
receive oral rather than parenteral
erythropoietin
E) Complications of erythropoietin include
hypertension and hypercoagulability
Question 29. In patients with hypertension
and proteinuria, which of the following
classes of drug has been shown to be most
effective in retarding the progression of
chronic renal failure?
A) Beta-blockers
B) Angiotensin-converting enzyme (ACE)
inhibitors
C) Calcium channel blockers
D) Nitrates
E) Thiazide diuretics
Question 30. Which of the following
factors does not contribute to the increased
risk of cardiovascular mortality in patients
with chronic renal failure?
A) Hypercholesterolaemia
B) Vascular calcification
C) Hypertension
D) Enhanced platelet function
E) Anaemia
Question 31. Deficiency of which one of
the following contributes to renal
osteodystrophy?
A) 1V-hydroxylase
B) Phosphate
C) Aluminium
D) 25-hydroxycholecalciferol
E) Parathyroid hormone
Question 32. Which of the following
adverse features of chronic renal failure is
least effectively treated by haemodialysis?
A) Accumulation of uraemic toxins
B) Abnormal electrolyte balance
C) Fluid overload
D) Anaemia
E) Acidosis
Question 33. Which of the following
statements about the differences between
peritoneal dialysis (PD) and haemodialysis
(HD) is true?
A) PD requires a more restrictive diet than
HD
B) PD enables a more efficient transfer of
solutes than HD
C) PD may be performed less frequently
than HD
D) Symptomatic fluid shift is less common
with PD than HD
E) Previous abdominal surgery is more
likely to impede HD than PD
Question 34. Which one of the following
is an absolute contraindication to renal
transplantation?
A) Age > 55 years
B) Active anti-glomerular basement
membrane (GBM) disease
C) Diabetes mellitus
D) Past history of malignant melanoma
excised 4 years ago
E) Previous failed renal transplant
Question 35. Deterioration of renal
function on commencement of
angiotensin-converting enzyme (ACE)
inhibitor therapy is most characteristic of:
A) Diabetic nephropathy
B) Hypertensive nephropathy
C) Adult polycystic kidney disease
D) Renal artery stenosis
E) Goodpasture's syndrome
46
Question 36. A 26-year-old man presents
with the nephrotic syndrome. Which of the
following conditions is most likely to be
the underlying cause?
A) Acute tubular necrosis
B) Membranous nephropathy
C) Post-streptococcal glomerulonephritis
D) Anti-glomerular basement membrane
(GBM) disease
E) Small-vessel vasculitis
Question 37. Which of the following
causes of glomerular disease is most likely
to present as rapidly progressive
glomerulonephritis?
A) Membranous nephropathy
B) Focal segmental glomerulosclerosis
C) Goodpasture's disease (anti-glomerular
basement membrane (anti-GBM) disease)
D) Diabetic nephropathy
E) Mesangiocapillary glomerulonephritis
Question 38. Which of the following
glomerular diseases is most likely to
respond to treatment with corticosteroids?
A) Minimal change nephropathy
B) IgA nephropathy
C) Primary focal segmental
glomerulosclerosis
D) Diabetic nephropathy
E) Post-streptococcal glomerulonephritis
Question 39. In addition to renal failure in
early adulthood, which of the following is
associated with Alport's syndrome?
A) Pulmonary haemorrhage
B) Gastrointestinal telangiectasia
C) Osteopenia
D) Intellectual impairment
E) Sensorineural deafness
Question 40. Which of the following is
not associated with adult polycystic kidney
disease (APKD)?
A) Hepatomegaly
B) Hypertension
C) Subarachnoid haemorrhage
D) Urinary tract infection
E) Renal cell carcinoma
Question 41. Which of the following is
least likely to precipitate acute urinary
retention in a patient with benign prostatic
hyperplasia (BPH)?
A) Alcohol excess
B) Alpha-adrenoceptor blockers
C) Constipation
D) Prostatic infection
E) Anticholinergic agents
Question 42. All of the following except
one are characteristic findings in a patient
presenting with metastatic prostate cancer.
Which is the exception?
A) Lytic bony metastases
B) Elevated alkaline phosphatase
C) Positive radioisotope bone scan
D) Prostate specific antigen (PSA) > 100
ng/ml
E) Enlarged, irregular prostate on rectal
examination
47
Question 43. Which of the following
hormones is least likely to be secreted by a
renal adenocarcinoma?
A) Erythropoietin
B) Adrenaline (epinephrine)
C) Parathyroid hormone-related peptide
D) Human chorionic gonadotrophin
E) Renin
Question 44. Which one of the following
drugs is associated with the development
of glomerulonephritis?
A) Ciclosporin
B) Gentamicin
C) Angiotensin-converting enzyme (ACE)
inhibitors
D) Penicillamine
E) Lithium
Chapter
17
CARDIOVASCULAR
DISEASE
Answers page 170
Question 1. Which one of the following
statements about the jugular venous pulse
(JVP) is true?
A) The height reflects left atrial pressure
B) The JVP falls with abdominal
compression
C) It is best examined with the patient
supine
D) Large systolic waves are associated
with tricuspid regurgitation
E) Prominent a waves suggest atrial
fibrillation
Question 2. In the majority of individuals,
the atrioventricular (AV) node is supplied
by the:
A) Left main stem artery
B) Left anterior descending artery
C) Circumflex artery
D) Right coronary artery
E) Obtuse marginal artery
Question 3. A 57-year-old man presents
with an acute myocardial infarction
affecting the anterior part of the septum
and anterior wall of the left ventricle.
Which of the following vessels is most
likely to have been occluded?
A) Left anterior descending artery
B) Circumflex artery
C) Right coronary artery
D) Right posterior descending artery
E) Obtuse marginal artery
48
Question 4. Which one of the following
statements regarding the nerve supply of
the heart is correct?
A) Beta1-adrenoceptors mediate negatively
chronotropic effects
B) Beta2-adrenoceptors mediate positively
inotropic effects
C) Adrenergic fibres reach the heart via
the vagus nerves
D) Cholinergic nerve fibres act on the
sinoatrial node to slow heart rate
E) Parasympathetic nerve fibres act on
muscle fibres in the atria and ventricles to
reduce the strength of myocardial
contraction
Question 5. Which one of the following is
not an appropriate indication for an
exercise (stress) ECG?
A) Evaluation of stable angina
B) Evaluation of unstable angina
C) Assessment of prognosis following a
myocardial infarction
D) Assessment of outcome following
coronary angioplasty
E) Diagnosis of exercise-induced
arrhythmias
Question 6. Which of the following
symptoms is most suggestive of
myocardial ischaemia?
A) Epigastric discomfort after eating
B) Exertional breathlessness and wheeze
C) Exertional breathlessness and throat
tightness
D) Breathlessness with perioral and digital
paraesthesia
E) Rapid palpitation on exertion
Question 7. A 58-year-old woman
presents with dyspnoea and central chest
and throat tightness, which occur when
walking her dog and force her to stop and
rest. She has smoked 20 cigarettes a day
for the last 30 years. Examination is
unremarkable apart from some lesions
around her eye:
Question 10. Which of the following
disorders is most likely to present with
isolated right heart failure?
A) Aortic stenosis
B) Mitral regurgitation
C) Systemic hypertension
D) Dilated cardiomyopathy
E) Recurrent pulmonary emboli
Question 11. Which of the following
findings on clinical examination is most
suggestive of left heart failure over right
heart failure?
A) Raised jugular venous pressure (JVP)
B) Hepatomegaly
C) Fine bi-basal crepitations
D) Peripheral oedema
E) Ascites
What abnormality is likely to be found on
blood tests?
A) Renal impairment
B) Hypercholesterolaemia
C) Hyperthyroidism
D) Hyperglycaemia
E) Hypocalcaemia
Question 8. The patient from the previous
question (Q7) is found to have a normal
12-lead ECG and chest X-ray. Which of
the following would be the most
appropriate next investigation?
A) Coronary angiogram
B) Exercise ECG
C) Echocardiogram
D) 24-hour tape
E) Pulmonary function tests
Question 9. The patient from the previous
two questions (Q7 and Q8) undergoes an
exercise ECG, which is positive but shows
no high-risk features. Blood tests confirm
a raised plasma cholesterol of 7.2 and
blood pressure is 158/92 mmHg. All of the
following are appropriate secondary
prevention measures except one. Which is
the exception?
A) Aspirin
B) Ramipril
C) Spironolactone
D) Simvastatin
E) Smoking cessation
49
Question 12. A 68-year-old man presents
with acute pulmonary oedema. Which one
of the following examination findings is
most suggestive of pre-existing structural
heart disease?
A) Elevated jugular venous pressure
B) Basal lung crepitations
C) Displaced apex beat
D) Gallop rhythm
E) Cool, clammy peripheries
Question 13. Which of the following
cardiac medications most commonly
causes peripheral oedema?
A) Digoxin
B) Amlodipine
C) Atenolol
D) Nicorandil
E) Ramipril
Question 14. A patient presents with
severe bilateral lower limb pitting oedema.
Which of the following features would
suggest a cause other than chronic cardiac
failure?
A) Raised jugular venous pressure
B) Hepatomegaly
C) Peripheral muscle wasting
D) Hyponatraemia
E) Heavy proteinuria
Question 15. A 63-year-old man with
ischaemic heart disease attends the
cardiology clinic with worsening
symptoms of chronic heart failure. His
treatment is modified. Three weeks later,
routine blood tests by the GP reveal a
serum potassium of 6.5 mmol/l (reference
range 3.6-5.1). Which of the following
drugs is the most likely culprit?
A) Furosemide
B) Ramipril
C) Digoxin
D) Bisoprolol
E) Aspirin
Question 16. Which one of the following
treatments should be avoided in patients
with acute left ventricular failure?
A) Intravenous glyceryl trinitrate
B) Non-invasive positive pressure
ventilation
C) Beta-blockers
D) Loop diuretics
E) Intravenous morphine
Question 17. Angiotensin receptor
blockers (ARBs) are frequently used in
patients intolerant of ACE inhibitors.
Which of the following adverse effects of
ACE inhibitor therapy is most likely to be
improved by switching to an ARB?
A) Renal impairment
B) Postural hypotension
C) Dry cough
D) Hyperkalaemia
E) Hyponatraemia
Question 18. All of the following agents
except one have been shown to reduce
mortality in patients with chronic heart
failure. Which is the exception?
A) Angiotensin receptor blockers
B) ACE inhibitors
C) Beta-blockers
D) Loop diuretics
E) Spironolactone
50
Question 19. Which one of the following
diagnoses is least likely to account for an
episode of loss of consciousness?
A) Carotid sinus syndrome
B) Transient ischaemic attack
C) Stokes-Adams attack
D) Ventricular tachycardia
E) Hypertrophic obstructive
cardiomyopathy
Question 20. In differentiating cardiac
syncope from seizures, which one of the
following most strongly suggests cardiac
syncope?
A) No warning prior to blackout
B) Cyanosis during unconscious period
C) Urinary incontinence
D) Brief twitching during unconscious
period
E) Rapid recovery (< 1 min) following the
collapse
Question 21. A patient admitted to the
coronary care unit with an acute anterior
myocardial infarction loses consciousness
during the morning ward round. Below is
a rhythm strip taken from his continuous
cardiac telemetry:
What is the most urgent priority in this
patient's management?
A) IV amiodarone
B) External cardiac pacing
C) IV adrenaline (epinephrine)
D) Endotracheal intubation and ventilation
E) Defibrillation
Question 22. A 74-year-old man with
severe pneumonia on the medical highdependency unit suffers a cardiac arrest.
The cardiac monitor shows asystole.
Cardiopulmonary resuscitation (CPR) is
commenced and IV adrenaline
(epinephrine) is administered. Which one
other drug should be given at this stage?
A) Amiodarone
B) Atropine
C) Lidocaine
D) Magnesium sulphate
E) Sodium bicarbonate
Question 23. Which of the following
disorders characteristically produces a
loud first heart sound (S1)?
A) Atrial septal defect
B) Mitral stenosis
C) Aortic regurgitation
D) Left ventricular hypertrophy
E) Constrictive pericarditis
Question 24. Wide fixed splitting of the
second heart sound occurs in which one of
the following disorders?
A) Patent ductus arteriosus
B) Aortic stenosis
C) Ventricular septal defect
D) Mitral regurgitation
E) Atrial septal defect
Question 25. A fourth heart sound is least
likely to be heard in which of the
following conditions?
A) Systemic hypertension
B) Aortic stenosis
C) Hypertrophic cardiomyopathy
D) Atrial fibrillation
E) Ischaemic heart disease
Question 26. The combination of a third
heart sound and soft first heart sound is
most characteristic of which of the
following disorders?
A) Aortic regurgitation
B) Pulmonary stenosis
C) Mitral regurgitation
D) Atrial septal defect
E) Ventricular septal defect
Question 27. Which of the following
conditions is most likely to produce a
murmur in early diastole?
A) Ventricular septal defect (VSD)
B) Mitral stenosis
C) Tricuspid regurgitation
D) Aortic regurgitation
E) Pulmonary stenosis
Question 28. Which one of the following
not a cause of sinus tachycardia?
A) Anaemia
B) Raised intracranial pressure
C) Thyrotoxicosis
D) Phaeochromocytoma
E) Nebulised salbutamol
51
Question 29. A 58-year-old woman
presents to the hospital Accident and
Emergency department with sudden onset
of palpitations. Below is a rhythm strip of
her ECG before and after carotid sinus
massage:
What is the cause of her palpitations?
A) Atrial fibrillation
B) Atrial tachycardia
C) Atrial flutter
D) Atrioventricular (AV) nodal re-entry
tachycardia
E) Sinus tachycardia
Question 30. A 47-year-old man presents
to the hospital Accident and Emergency
department with palpitations and is found
to be in atrial fibrillation (AF) with a rapid
ventricular rate. He cardioverts
spontaneously but this is his third such
episode in the last 2 years. He is otherwise
well and drinks no alcohol. Blood pressure
is 152/88 mmHg. Routine blood tests are
normal and an echocardiogram reveals no
structural heart disease. Which of the
following medications would be the most
appropriate first-line therapy to prevent
further episodes?
A) Bisoprolol
B) Verapamil
C) Ramipril
D) Digoxin
E) Amiodarone
Question 31. Which one of the following
is a contraindication to DC cardioversion
for persistent atrial fibrillation?
A) Age over 75
B) Atrial fibrillation present for > 1 year
C) Moderate to severe left ventricular
impairment
D) Subtherapeutic INR
E) Relapse after two previous
cardioversions
Question 32. Which one of the following
medications would not be suitable for rate
control in persistent atrial fibrillation?
A) Digoxin
B) Atenolol
C) Verapamil
D) Diltiazem
E) Amlodipine
Question 33. Intravenous adenosine is
most likely to restore sinus rhythm in
which of the following tachyarrhythmias?
A) Atrial flutter
B) Atrial fibrillation
C) Atrioventricular (AV) nodal re-entrant
tachycardia
D) Atrial tachycardia
E) Ventricular tachycardia
Question 34. A 24-year-old woman
presents to her GP with recurrent episodes
of palpitation. She describes several
episodes where she has suddenly felt her
heart beating very rapidly. They last
anywhere from a few minutes to an hour
before self-terminating. She feels very
frightened during these episodes and is
worried she may have a serious heart
condition. Examination is normal and she
appears to be in sinus rhythm. A segment
of her 12-lead ECG is shown below.
What is the likely diagnosis?
A) Paroxysmal atrial fibrillation
B) Panic attacks
C) Wolff-Parkinson-White syndrome
D) Ventricular ectopic beats
E) Recurrent ventricular tachycardia
Question 35. The patient in the previous
question (Q34) finds these episodes of
palpitation distressing and asks about
treatment to prevent further episodes.
Which of the following is the treatment of
choice?
A) Digoxin
B) Dual chamber pacemaker
C) Verapamil
D) Catheter ablation of accessory pathway
E) Amiodarone
52
Question 36. A 55-year-old man is
brought to the emergency department by
ambulance after collapsing at work. His
ECG shows a broad complex tachycardia:
Which of the following features most
strongly favours a diagnosis of ventricular
tachycardia (VT) over supraventricular
tachycardia with bundle branch block?
A) History of ischaemic heart disease
B) Termination with IV adenosine
C) Presence of capture and fusion beats on
ECG
D) QRS duration of 150 ms
E) Right axis deviation on ECG
Question 37. The patient in the previous
question (Q36) is diagnosed with
ventricular tachycardia (VT). He is aware
of his heart racing but is otherwise
asymptomatic. Heart rate is 170 bpm.
Blood pressure is 110/70 mmHg. There is
no evidence of pulmonary oedema. What
is the most appropriate next treatment?
A) IV metoprolol
B) IV amiodarone
C) IV flecainide
D) DC cardioversion
E) Overdrive pacing
Question 38. Below is an ECG recording
from a patient on the coronary care unit,
who is on continuous telemetry. She had
been admitted the previous day with an
episode of syncope:
What is the diagnosis?
A) Idioventricular rhythm ('slow
ventricular tachycardia')
B) Ventricular fibrillation
C) Torsades de pointes
D) Supraventricular tachycardia with
aberrant conduction
E) Sick sinus syndrome
Question 39. What abnormality is most
likely to be seen on a 12-lead ECG from
the patient in the previous question (Q38)
when she was in sinus rhythm?
A) ST elevation
B) Prolonged PR interval
C) Broad QRS complexes
D) Prolonged QT interval
E) Delta wave
Question 40. Which of the following
drugs is most likely to cause a prolonged
QT interval?
A) Omeprazole
B) Digoxin
C) Clarithromycin
D) Diazepam
E) Morphine
Question 41. Which of the following drug
treatments is most appropriate for a patient
with torsades de pointes?
A) Magnesium
B) Amiodarone
C) Lidocaine
D) Digoxin
E) Sotalol
Question 42. A 77-year-old patient is
referred to the cardiology outpatient clinic
with recurrent dizzy spells, and a 24-hour
tape is performed. The ECG strip below is
recorded during a typical episode of
dizziness:
What rhythm abnormality is shown?
A) First-degree atrioventricular (AV)
block
B) Mobitz type I second-degree AV block
C) Mobitz type II second-degree AV block
D) Third-degree (complete) heart block
E) Junctional rhythm
53
Question 43. What is the most appropriate
management of the patient in the previous
question (Q42)?
A) Review in 6 months and consider
treatment if any syncopal episodes
B) Start amiodarone and repeat 24-hour
tape
C) Atrial pacemaker
D) Dual-chamber pacemaker
E) Implantable cardiac defibrillator
Question 44. Which one of the following
is not a manifestation of digoxin toxicity?
A) Nephrotoxicity
B) Altered colour vision
C) Bradycardia
D) Vomiting
E) Ventricular tachycardia
Question 45. Which of the following
features renders an atherosclerotic plaque
most vulnerable to rupture?
A) Thick fibrous cap
B) Calcification
C) Lipid-rich core
D) Extensive collagenous cross-struts
E) High concentration of smooth muscle
cells
Question 46. Which one of the following
is not an independent risk factor for
atherosclerosis?
A) Systolic hypertension
B) Raised high-density lipoprotein (HDL)
cholesterol
C) Hyperhomocysteinaemia
D) Central obesity
E) Diabetes mellitus
Question 47. A 60-year-old man is
referred to the cardiology outpatient
department with a 6-month history of
exertional chest pain relieved by rest and
glyceryl trinitrate (GTN) spray. As part of
his assessment he undergoes an exercise
ECG. Which of the following features on
exercise ECG would be the strongest
indication for proceeding to coronary
angiography?
A) Rise in systolic blood pressure of 60
mmHg during test
B) Widespread 1-2 mm upward-sloping
ST depression during stage 2 of the Bruce
protocol without symptoms
C) Failure to complete stage 1 of the
Bruce protocol due to hip pain
D) Chest pain and 2-3 mm horizontal ST
depression in lateral leads during stage 4
of the Bruce protocol
E) Chest pain and 1-2 mm downwardsloping ST depression in inferior leads
during stage 1 of the Bruce protocol
Question 48. Which one of the following
drugs is not an anti-anginal agent?
A) Clopidogrel
B) Atenolol
C) Diltiazem
D) Nicorandil
E) Isosorbide mononitrate
Question 49. Which one of the following
features is least consistent with a diagnosis
of unstable angina?
A) Chest pain on minimal exertion
B) Persistent ST segment elevation on
ECG
C) No preceding history of stable angina
D) More than two episodes of chest pain at
rest in the last 24 hours
E) T wave inversion on ECG
54
Question 50. A 68-year-old man with a
long history of angina presents with a
worsening of anginal symptoms. He was
previously able to walk up to 1 mile before
the onset of symptoms but for the past few
days has been experiencing pain after just
50 yards and, on one occasion, at rest.
Which of the following factors would have
the least impact on his short-term risk of
death or acute myocardial infarction?
A) Recurrent pain at rest
B) ST segment depression on ECG
C) Elevated serum cholesterol
D) Persistent deep T-wave inversion on
ECG
E) Elevated serum troponin
Question 51. The patient from the
previous question (Q50) is admitted to
hospital and an admission ECG reveals 1
mm ST depression in leads V5 and V6. In
the absence of any contraindications,
which of the following would be the
optimal combination of antiplatelet agents
and anticoagulants to prescribe?
A) Aspirin alone
B) Aspirin and low molecular weight
heparin
C) Aspirin and clopidogrel
D) Aspirin, clopidogrel and low molecular
weight heparin
E) Aspirin, clopidogrel and warfarin
Question 52. After 48 hours of optimal
medical treatment, the patient from the
previous question (Q51) is still
experiencing occasional short-lived
episodes of chest pain at rest. His ECGs
while he is pain-free are normal, but those
taken during pain show recurrence of ST
segment depression in the lateral leads.
Troponin T is modestly elevated. What
would be the best investigation to perform
next in this patient?
A) 24-hour ECG
B) Exercise ECG
C) Echocardiogram
D) Myocardial perfusion scan
E) Coronary angiogram
Question 53. A 48-year-old man presents
with a 6-hour history of severe central
chest pain. He is unable to give much
history but declares that the pain is the
worst he has ever felt. He was previously
well with no history of cardiovascular
disease. On examination he appears pale,
sweaty and distressed. His ECG is shown
below:
What is the diagnosis?
A) Aortic dissection
B) Acute anterior myocardial infarction
C) Acute inferior myocardial infarction
D) Unstable angina
E) Pericarditis
Question 54. The patient from the
previous question (Q53) with acute
anterior ST elevation myocardial
infarction (MI) is treated immediately with
IV morphine, sublingual glyceryl trinitrate
and aspirin. He appears less distressed but
his heart rate is 118 bpm and blood
pressure is 195/115 mmHg. Heart sounds
1 and 2 are present with no added sounds
or murmurs and the chest is clear to
auscultation. Which of the following
options would be the +best next step in his
management?
A) Thrombolysis
B) IV magnesium
C) Sublingual nifedipine
D) IV metoprolol
E) Oral ramipril
55
Question 55. A 62-year-old woman
presents with a 2-hour history of severe
chest pain and has the following ECG:
While awaiting thrombolysis, she
complains of lightheadedness. Her pulse
rate is 38 beats per minute and telemetry
shows sinus bradycardia. What is the most
appropriate next treatment?
A) Insertion of temporary pacing wire
B) IV atropine
C) External cardiac pacing
D) IV isoprenaline
E) IV atenolol
Question 56. Which one of the following
long-term treatments does not confer
prognostic benefit in survivors of acute
myocardial infarction (MI)?
A) Aspirin
B) Angiotensin-converting enzyme (ACE)
inhibitor
C) Beta-blocker
D) Statin
E) Isosorbide mononitrate
Question 57. In a patient with peripheral
arterial disease, which one of the
following features suggests the worst
prognosis?
A) Claudication distance of 50-100 metres
B) Night pain
C) Diminished pedal pulses
D) Ankle:brachial pressure index (ABPI)
ratio of 0.8
E) Bruit over femoral artery
Question 58. In a patient presenting with
acute lower limb ischaemia, which one of
the following clinical features would
favour a diagnosis of embolism over
thrombosis in situ?
A) Onset of symptoms over hours
B) History of intermittent claudication
C) Previously undiagnosed atrial
fibrillation
D) Absent contralateral lower limb pulses
E) Presence of bruits
Question 59. Which one of the following
clinical features is least consistent with a
type B aortic dissection?
A) Severe tearing chest pain
B) Elevated blood pressure
C) Asymmetry of femoral pulses
D) New early diastolic murmur
E) Acute renal failure
Question 63. A 53-year-old male with
hypertension has been taking 10 mg of
ramipril for several months. Despite this,
his blood pressure control remains
suboptimal. There are no compliance
issues. Which one of the following agents
would be the best add-on therapy?
A) Angiotensin receptor blocker
B) Beta-blocker
C) Calcium channel antagonist
D) Hydralazine
E) Alpha-blocker
Question 60. Which of the following is
not a recognised risk factor for essential
hypertension?
A) Hyperlipidaemia
B) Obesity
C) High salt intake
D) Intrauterine growth retardation
E) Alcohol excess
Question 64. A 19-year-old man presents
with recent onset of breathlessness and
sharp, central chest pain exacerbated by
movement and coughing. His heart rate is
110 beats per minute. On auscultation
there is a soft pansystolic murmur and a
pericardial friction rub. Echocardiography
demonstrates mitral regurgitation.
Antistreptolysin O antibody titres (ASOT)
are 500 U/ml (normal range < 200). What
is the likeliest diagnosis?
A) Infective endocarditis
B) Viral myocarditis
C) Acute rheumatic fever
D) Viral pericarditis
E) Dressler's syndrome
Question 61. The following endocrine
diseases are all recognised causes of
secondary hypertension except one. Which
is the exception?
A) Acromegaly
B) Congenital adrenal hyperplasia
C) Conn's syndrome
D) Phaeochromocytoma
E) Addison's disease
Question 65. In the patient from the
previous question (Q64), which one of the
following features would clinch the
diagnosis of rheumatic fever?
A) Temperature > 38oC
B) Positive throat swab culture
C) Cardiac dilatation on echocardiography
D) First-degree block on ECG
E) Flitting polyarthritis
Question 62. A 77-year-old woman in
good health is found by her general
practitioner to have persistently elevated
blood pressure, with a typical reading of
162/84 mmHg. Which of the following
agents would be the most appropriate
initial treatment?
A) Angiotensin-converting enzyme (ACE)
inhibitor
B) Angiotensin receptor blocker
C) Beta-blocker
D) Thiazide diuretic
E) Alpha-blocker
56
Question 66. A 53-year-old lady
complains of progressively worsening
exertional dyspnoea associated with
deterioration in exercise tolerance over the
past 2 years. On examination her pulse is
irregularly irregular and of small volume.
There is a low-pitched mid-diastolic
murmur audible at her apex. What is the
likeliest cause of her breathlessness?
A) Dilated cardiomyopathy
B) Ischaemic heart disease
C) Ventricular septal defect
D) Mitral stenosis
E) Aortic regurgitation
Question 67. With reference to the patient
from the previous question (Q66) who has
mitral stenosis, which one of the following
features would suggest that her condition
has been complicated by pulmonary
hypertension?
A) Loud first heart sound (S1)
B) Opening snap
C) Pansystolic murmur radiating to the
axilla
D) Tapping apex beat
E) Loud pulmonary component of second
heart sound (P2)
Question 71. A 64-year-old man is found
to have an ejection systolic murmur during
a routine medical examination. Which of
the following associated clinical signs
would lend most support to a diagnosis of
aortic stenosis?
A) Displaced apex beat
B) Loud aortic component of second heart
sound (A2)
C) Louder in inspiration
D) Wide pulse pressure
E) Slow-rising carotid pulse
Question 68. Which one of the following
would be a contraindication to mitral
balloon valvuloplasty?
A) Mitral valve orifice < 2 cm2
B) Concomitant mitral regurgitation
C) Mobile valvular apparatus
D) Atrial fibrillation
E) Enlarged left atrium
Question 73. You are asked to examine a
dyspnoeic patient on the cardiology ward.
She has bounding peripheral pulses, a
blood pressure of 190/70 mmHg, a
displaced, heaving apex beat and a loud
early diastolic murmur. Which of the
following underlying pathologies would
be least likely to account for these
physical findings?
A) Rheumatic heart disease
B) Acute aortic dissection
C) Syphilitic aortitis
D) Marfan's syndrome
E) Ankylosing spondylitis
Question 69. The following are all
recognised causes of mitral regurgitation
except one. Which is the exception?
A) Papillary muscle rupture
B) Dilated cardiomyopathy
C) Acute rheumatic fever
D) Subacute bacterial endocarditis
E) Congenitally bicuspid mitral valve
Question 70. Which one of the following
features is likely to be found in mitral
regurgitation but not in mitral stenosis?
A) Irregularly irregular pulse
B) Third heart sound (S3)
C) Right ventricular heave
D) Accentuated pulmonary component of
second heart sound
E) Bi-basal crepitations
57
Question 72. A patient with known aortic
stenosis is followed up annually in the
cardiology outpatient clinic. Which of the
following would be the strongest
indication for aortic valve replacement?
A) Syncopal episodes
B) Prolonged murmur and thrusting apex
beat on examination
C) Left bundle branch block on ECG
D) Reduced valve area on
echocardiography
E) High pressure gradient between left
ventricle and aorta at cardiac
catheterisation
Question 74. A patient with a history of
long-standing rheumatic mitral stenosis
presents with a 6-week history of malaise,
drenching sweats and lethargy. On
examination she has poor dentition, a
temperature of 38.5°C and a loud
pansystolic murmur at apex radiating to
axilla. You suspect a diagnosis of subacute
bacterial endocarditis. Which of the
following microorganisms is the likeliest
culprit?
A) Viridans streptococci
B) Staphylococcus aureus
C) Coxiella burnetti
D) Coagulase-negative staphylococci
E) Haemophilus
Question 78. An 18-year-old boy, who
previously attended the paediatric
cardiology clinic but defaulted from
follow-up after his 14th birthday, now
presents to his GP with increasingly severe
breathlessness, fatigue and reduced
exercise tolerance. On examination he is
centrally cyanosed with clubbing of the
fingers and toes. Which of the following is
the most likely underlying congenital
cardiac abnormality?
A) Ventricular septal defect
B) Coarctation of the aorta
C) Pulmonary stenosis
D) Bicuspid aortic valve
E) Patent foramen ovale
Question 75. Echocardiography confirms
the presence of a vegetation on the mitral
valve and mitral regurgitation. Six sets of
blood cultures are sent. While awaiting
results, which of the following antibiotic
regimens would be the most appropriate
empirical treatment?
A) Flucloxacillin
B) Benzyl penicillin
C) Gentamicin
D) Benzyl penicillin and gentamicin
E) Vancomycin and flucloxacillin
Question 79. Which one of the following
does not constitute a component of Fallot's
tetralogy?
A) Pulmonary stenosis
B) Ventricular septal defect
C) Overriding aorta
D) Patent ductus arteriosus
E) Right ventricular hypertrophy
Question 76. According to the modified
Duke criteria, which one of the following
is considered a major criterion for the
diagnosis of infective endocarditis?
A) Pyrexia > 38°C
B) Pre-existing aortic stenosis
C) Splinter haemorrhages
D) Vegetations on echocardiography
E) Osler's nodes
Question 77. A continuous machinery
murmur, loudest over the left second
intercostal space, is associated with which
of the following congenital cardiac
abnormalities?
A) Atrial septal defect
B) Ventricular septal defect
C) Patent ductus arteriosus
D) Tricuspid atresia
E) Pulmonary stenosis
58
Question 80. A patient who immigrated to
the UK from West Africa 18 months ago
presents with progressive ankle swelling
and abdominal distension. On examination
he has marked bilateral lower limb
oedema, a palpably enlarged liver and
ascites. His jugular venous pulse is
elevated and rises during inspiration. Lung
fields are clear to auscultation. His chest
X-ray is shown below:
Which of the following is the likeliest
underlying aetiology?
A) Tuberculosis
B) TrypanosomiasisC) Syphilis
D) Malaria
E) Haemochromatosis
Chapter
18 RESPIRATORY DISEASE
Answers page 181
Question 1. A 21-year-old woman
presents to the hospital accident and
emergency department with an acute
exacerbation of asthma. Which of the
following features in her presentation
would give greatest cause for concern?
A) Peak expiratory flow (PEF) 40% of
predicted
B) Inability to complete sentences in one
breath
C) PaCO2 of 5.8 kPa
D) Respiratory rate of 30 breaths per
minute
E) Sinus tachycardia of 120 beats per
minute
Question 2. A 67-year-old lifelong
smoker with a history of one previous
myocardial infarction attends the
respiratory clinic with shortness of breath.
On examination she is clinically
hyperinflated, and has a respiratory rate of
19 breaths per minute at rest and quiet
vesicular breath sounds bilaterally.
Bilateral ankle oedema is present to the
mid-calves. Pulmonary function tests show
a forced vital capacity (FVC) of 70%
predicted, a forced expiratory volume in 1
second (FEV1) of 25% predicted and an
FEV1:FVC ratio of 55%. These
abnormalities are only partially reversed
by inhaled salbutamol. Which of the
following conditions is the most likely
diagnosis?
A) Asthma
B) Chronic obstructive pulmonary disease
(COPD)
C) Congestive cardiac failure
D) Sarcoidosis
E) Bronchial carcinoma
59
Question 3. The patient with COPD from
the previous question (Q2) has the
following arterial blood gas (ABG) results:
How should these results be interpreted?
A) Compensated metabolic acidosis
B) Compensated respiratory acidosis
C) Mixed respiratory and metabolic
alkalosis
D) Compensated metabolic alkalosis
E) Mixed respiratory and metabolic
acidosis
Question 4. In the treatment of stable
COPD, which one of the following
interventions will provide the greatest
survival benefit?
A) Home nebuliser with salbutamol
B) Long-acting ß2-agonist
C) Oral steroid therapy
D) Smoking cessation
E) Daily inhaled tiotropium
Question 5. A previously well, nonsmoking, 24-year-old Turkish woman
presents to the hospital accident and
emergency department with a 1-day
history of non-productive cough, chills
and sore throat. Her voice is not hoarse but
there is a harsh rasping sound from her
throat with each breath and she is unable
to swallow her own saliva. Her routine
observations are:
Which of the following is the most
appropriate initial action?
A) Carefully examine the throat under
direct vision
B) Check arterial blood gases
C) Perform a CT scan of the chest and
neck
D) Transfer to a critical care environment
and consider endotracheal intubation by an
experienced anaesthetist
E) Administer nebulised bronchodilator
Question 7. With reference to the patient
in the previous question (Q6), which of the
following investigations would be of
greatest use in establishing a diagnosis?
A) CT scan of thorax
B) Lateral chest X-ray
C) Serum rheumatoid factor, anti-nuclear
factor and anti-DNA antibodies
D) Pleural aspiration
E) Arterial blood gas
Question 8. The patient from the previous
two questions (Q6 and Q7) has 30 ml of
serous fluid aspirated from his left pleural
space and sent for analysis. Initial
biochemistry results are shown below,
along with the results of some routine
blood tests:
Which of the following conditions is the
most likely cause of his pleural effusion?
A) Nephrotic syndrome
B) Parapneumonic effusion
C) Thoracic duct occlusion
D) Acute pancreatitis
E) Congestive cardiac failure
Question 6. This chest X-ray was taken
from a 69-year-old man who presented
with confusion and a vague history of
increasing shortness of breath:
Which of the following clinical signs is
most likely to be present on examination
of the chest?
A) Bronchial breathing at left base
B) Reduced chest expansion on right side
C) Stony dull percussion note at left base
D) Inspiratory crepitations at left base
E) Reduced cricosternal distance
60
Question 9. A 34-year-old woman
presents to the hospital accident and
emergency
department with sudden onset of acute
severe breathlessness. She is able to talk in
broken sentences. She reports that she
cannot get enough air and also feels
tingling in both fingertips. She has had
several similar episodes in the past. On
examination, she appears very distressed.
Respiratory rate is 30 breaths per minute
but examination of her chest reveals no
abnormal findings. Oxygen saturations on
air are 99%. What is the most likely
diagnosis?
A) Psychogenic hyperventilation
B) Acute asthma
C) Pneumothorax
D) Pulmonary oedema
E) Pneumonia
Question 10. A previously healthy 35year-old man presents with fever,
tachypnoea and hypoxia on air. Which one
of the following features would not lend
support to a diagnosis of Pneumocystis
carinii (jirovecii) pneumonia?
A) Oropharyngeal candidiasis
B) Rusty, golden yellow-coloured sputum
C) Poor response to standard antibiotics
D) Marked worsening of hypoxia on
exertion
E) Normal chest X-ray but nodular
ground-glass attenuation on highresolution CT
Question 11. An 18-year-old asthmatic
patient presents to the hospital accident
and emergency department 1 hour after
developing breathlessness and wheeze. On
admission she is struggling to complete
sentences in one breath, and has a peak
flow of 150 l/min (her best peak expiratory
flow rate (PEFR) is 310 l/min) and
widespread wheeze throughout her chest.
Observations are shown below:
All of the following are appropriate steps
in her immediate management except one.
Which is the exception?
A) High-concentration oxygen
B) Nebulised salbutamol
C) Systemic corticosteroids
D) Nebulised ipratropium
E) Intravenous aminophylline
Question 12. After 1 hour of treatment
with salbutamol, oxygen, systemic
corticosteroids and intravenous
magnesium, the patient in the previous
question (Q11) has made no improvement
and appears to be tiring. Her PEFR is now
100 l/min and auscultation of the chest
reveals quiet wheeze bilaterally. Below are
the results of arterial blood gas
measurements taken on admission (first
ABG) then repeated after treatment
(second ABG), both on 60% O2:
61
Which of the following would be the most
appropriate next step?
A) Discharge with advice to return if the
wheeze worsens
B) Admit to the medical ward for
overnight observation
C) Refer to the intensive treatment unit for
consideration of mechanical ventilation
D) Refer to the high-dependency unit for a
trial of non-invasive ventilation
E) Reduce oxygen concentration to 28%
and repeat the ABG in 1 hour
Question 13. Which of the following best
describes the mode of action of
ipratropium?
A) ß2-adrenoceptor agonist
B) Leukotriene receptor antagonist
C) Corticosteroid
D) Anticholinergic
E) Cholinergic agonist
Question 14. A patient presents to the
respiratory clinic complaining of 6 months'
history of cough. Respiratory examination
and chest X-ray are normal. Which of the
following is least likely to explain her
symptom?
A) Treatment with ramipril
B) Post-nasal drip
C) Gastro-oesophageal reflux disease
D) Viral pneumonia
E) Asthma
Question 15. A previously fit and healthy
54-year-old woman returns to the UK
from a family holiday in Spain. She
reports fever, rigors, right-sided pleuritic
chest pain and general fatigue over the last
24 hours. On examination her temperature
is 37.8°C, she appears confused,
respiratory rate is 32/min, heart rate
110/min, BP 88/50 mmHg and SaO2 92%
on high-concentration oxygen.
Examination findings relating to the right
side of the chest are as follows: reduced
expansion, dull percussion note, bronchial
breathing, increased vocal resonance and
whispering pectoriloquy. Initial blood tests
show a D-dimer of 1000 U, white cell
count of 15 × 109/l and serum urea of 10
mmol/l. Which one of the following
statements is true concerning the
management of this patient?
A) Therapeutic dose low-molecular weight
heparin should be commenced to treat
pulmonary embolism
B) Aggressive fluid resuscitation is
necessary immediately
C) Antibiotic therapy should begin
following the results of sputum culture
D) The most appropriate antibiotics are an
oral aminopenicillin in combination with
an oral macrolide
E) She should be admitted to a general
medical or general respiratory unit
Question 16. A 62-year-old lady with
mild chronic obstructive pulmonary
disease is admitted following sudden onset
of shortness of breath at rest and left-sided
pleuritic chest pain. Her chronic cough is
unchanged and she denies any
haemoptysis or change in sputum
production. Her only medications are an
as-required ß2-agonist inhaler and
oestrogen replacement therapy. Clinical
examination reveals tachypnoea at rest and
signs of hyperinflation. There is no audible
wheeze on auscultation. Observations are
as follows:
• respiratory rate 22/min, heart rate 102
beats per minute, BP 140/72 mmHg, SpO2
88% on air
• ECG shows sinus tachycardia but no
other abnormality
• chest X-ray shows hyperexpanded lung
fields with no evidence of pneumothorax,
collapse or consolidation.
62
What is the likeliest cause of her
presentation?
A) Infective exacerbation of COPD
B) Pulmonary embolism
C) Acute left ventricular failure
D) Psychogenic hyperventilation
E) Pneumonia
Question 17. With reference to the patient
in the previous question (Q16), which of
the following investigations would be
most likely to confirm the diagnosis?
A) Computed tomography pulmonary
angiogram (CTPA)
B) Echocardiogram
C) Plasma D-dimer level
D) Ventilation/perfusion (V/Q) scan
E) High-resolution CT (HRCT) scan of
thorax
Question 18. A 23-year-old man is rushed
to hospital after complaining of severe
left-sided chest pain whilst drinking in a
bar. On arrival at the hospital accident and
emergency department he is in
considerable distress and too short of
breath to give a meaningful history. His
blood pressure in the ambulance was
83/40 mmHg. He is maintaining his
airway but his trachea is shifted to the
right and he has distended neck veins.
Which of the following is the most
appropriate way to get enough diagnostic
information to begin treatment?
A) Chest X-ray
B) Percussion and auscultation of the lung
fields
C) ECG
D) Arterial blood gas analysis
E) Check for flapping tremor (asterixis)
Question 19. A 50-year-old patient is
referred to the respiratory clinic with
shortness of breath. On examination he has
finger clubbing, central cyanosis and fine
end-inspiratory crepitations at both lung
bases. Which of the following types of
pathology would be most consistent with
all these examination findings?
A) Chronic obstructive pulmonary disease
(COPD)
B) Extrathoracic restrictive lung disease
C) Fibrotic lung disease
D) Left ventricular failure
E) Cystic fibrosis
Question 20. What is the primary
anatomical source of normal healthy
breath sounds?
A) Larynx and central airways
B) Small bronchi
C) Terminal bronchioles
D) Respiratory bronchioles
E) Opening of alveoli
Question 21. Which of the following is
the correct description of the normal lobes
of the lungs?
A) Two lobes on the right, three on the left
B) Two lobes on the right, one on the left
C) Three lobes on the right and left
D) Three lobes on the right, two on the left
E) One lobe on the right, two on the left
Question 22. A 29-year-old lady presents
to the dermatology clinic with tender, red,
raised lesions on her shins. She also
complains of joint pains and pyrexial
symptoms. A chest X-ray shows bilateral
hilar lymphadenopathy (BHL) but no other
abnormality. Which of the following is the
most likely explanation for these findings?
A) Tuberculosis
B) Lymphoma
C) Sarcoidosis
D) Wegener's granulomatosis
E) Rheumatoid arthritis
63
Question 23. This flow-volume loop
(labelled 'patient A') was taken during
pulmonary function testing at a respiratory
clinic:
Which of the following statements is true?
A) The pattern of flow limitation suggests
large airway obstruction
B) Obstruction is equally severe during
inspiration and expiration
C) The limitation of vital capacity
indicates a restrictive defect
D) Reduced mid-expiratory flow indicates
collapse of small intrathoracic airways
E) Patient A could produce a normal
reading on a peak flow meter
Question 24. This is a graph of lung
volume plotted against time:
What is the parameter labelled 'A' (red
arrow)?
A) Residual volume
B) Inspiratory capacity
C) Tidal volume
D) Vital capacity
E) Functional residual capacity
Question 25. A 23-year-old known
asthmatic is admitted with acute severe
breathlessness and tightness in his chest.
On examination, polyphonic wheeze is
heard throughout both lung fields, but is
quieter on the right. There is some
response to initial medical therapy, but
after 15 minutes of standard treatment he
remains tachypnoeic and distressed.
Which of the following investigations is
most urgent?
A) Chest X-ray
B) Urea and electrolytes
C) ECG
D) Doppler ultrasound of leg veins
E) Direct laryngoscopy
Question 29. At 0200 hrs, the on-call
respiratory physician is called to see a
patient who was admitted at 1600 hrs with
an acute exacerbation of chronic
obstructive pulmonary disease (COPD).
This is her first admission with chest
problems. She is centrally cyanosed and
drowsy and has bounding peripheral
pulses. What is the most urgent
investigation?
A) Chest X-ray
B) Arterial blood gas (ABG) analysis
C) Blood samples for salicylates and
paracetamol levels
D) ECG
E) CT of the head
Question 26. Which of the following
treatments has been shown to prolong life
in chronic obstructive pulmonary disease
(COPD)?
A) Long-term oxygen therapy
B) Inhaled tiotropium
C) PRN salbutamol
D) Furosemide
E) Sildenafil (Viagra)
Question 30. Below are the arterial blood
gases of the patient in the previous
question (Q29):
Question 27. In the investigation of a
solitary lung nodule, which of the
following tends to suggest benign, rather
than malignant, pathology?
A) Spiculated appearance
B) Size > 3 cm
C) Long smoking history
D) Calcification on chest X-ray
E) Hilar lymphadenopathy
Question 28. Which of the following is
not a risk factor for obstructive sleep
apnoea/hypopnoea syndrome (OSAHS)?
A) Male sex
B) Obesity
C) Protuberant mandible
D) Acromegaly
E) Hypothyroidism
64
Which one of the following treatments is
most appropriate?
A) Increase to 40% Venturi oxygen
B) Decrease to 28% Venturi oxygen
C) Administer 15 l/min oxygen via trauma
(reservoir bag) mask
D) Remove oxygen
E) Mechanical ventilatory support
Question 31. Which one of the following
conditions is more likely to cause type II
respiratory failure rather than type I?
A) Pulmonary fibrosis
B) Pneumothorax
C) Acute respiratory distress syndrome
D) Pulmonary embolus
E) Severe kyphoscoliosis
Question 32. A 56-year-old man is
referred for investigation of recurrent
pneumonia. He suffers from asthma,
which seems poorly controlled despite
regular use of high doses of fluticasone
and salmeterol. He reports on-going
cough, wheeze and sticky, difficult-toclear sputum and requires frequent courses
of oral corticosteroids. He has never
smoked, keeps no pets, complies with
therapy and has worked in the same office
for 12 years. Chest X-rays show evidence
of a left lower lobe collapse 1 year ago and
more recently a right middle lobe collapse.
The peripheral blood count shows an
eosinophil count of 0.6 × 109/l. Which one
of the following statements is true?
A) He should be investigated for
carcinoma of the bronchus
B) Cystic fibrosis is the most likely
diagnosis
C) A trial of itraconazole should be
considered
D) Induced sputum is likely to be rich in
neutrophils
E) Prolonged therapy with high-dose oral
corticosteroids should be considered
Question 33. Which of the following
classes of drug may precipitate an acute
attack of asthma?
A) Beta-adrenoceptor agonists
B) Non-steroidal anti-inflammatory drugs
C) Calcium channel blocking drugs
D) Histamine H1 receptor antagonists
E) Leukotriene receptor antagonists
Question 34. In a patient with a clinical
history compatible with asthma, which one
of the following clinches the diagnosis?
A) Clinical improvement during a course
of oral steroids
B) A 20% improvement in forced
expiratory volume in 1 second (FEV1)
following administration of a
bronchodilator
C) An 8% spontaneous change in peak
expiratory flow (PEF) during 1 week of
home monitoring
D) A normal chest X-ray
E) Elevated peripheral blood eosinophil
count
65
Question 35. A 34-year-old man with
asthma sees his general practitioner and
explains that his asthma is still
troublesome despite the recent addition of
a low-dose inhaled corticosteroid to his
prescription. He is currently on regular
low-dose inhaled steroid therapy and an
as-needed short-acting ß2-adrenoceptor
agonist. Which of the following is the
most appropriate next step in drug
treatment?
A) Short-term oral corticosteroid therapy
B) Addition of long-acting ß2adrenoceptor agonist
C) Addition of short-acting anticholinergic
bronchodilator
D) One-week course of empirical
antibiotic therapy
E) Addition of leukotriene receptor
antagonist
Question 36. All of the options below
describe clinically stable patients with
chronic obstructive pulmonary disease and
forced expiratory volume in 1 second
(FEV1) < 1.5 litres on optimal medical
therapy. Patients breathed air for at least
20 minutes before arterial blood gases
(ABGs) were taken. Which one patient
meets the criteria for long-term oxygen
therapy (LTOT)?
A) 65-year-old smoker with maximum
PaO2 of 5.9 kPa on two ABGs 3 weeks
apart
B) 71-year-old ex-smoker with maximum
PaO2 of 7.5 kPa on two ABGs 3 weeks
apart
C) 76-year-old ex-smoker with bilateral
pitting oedema to knees and maximum
PaO2 of 7.7 kPa on two ABGs 3 weeks
apart
D) 79-year-old ex-smoker with congestive
cardiac failure and maximum PaO2 of 7.6
kPa on two ABGs 3 weeks apart
E) 85-year-old ex-smoker with pulmonary
hypertension and PaO2 of 8.7 kPa on two
ABGs 3 weeks apart
Question 37. What is the usual pattern of
inheritance in cystic fibrosis?
A) Autosomal recessive
B) Autosomal dominant
C) X-linked recessive
D) X-linked dominant
E) New mutations are most common
Question 40. A previously healthy 58year-old smoker presents with a 2-month
history of cough productive of bloodstreaked sputum. His chest X-ray is shown
below:
Question 38. Which of the following
drugs is most likely to cause alveolitis in
chronic use?
A) Digoxin
B) Amiodarone
C) Nifedipine
D) Furosemide
E) Atenolol
Question 39. A 64-year-old lady who
recently travelled to the UK from Baghdad
presents with a 3-month history of loss of
appetite, weight loss, pyrexial symptoms
and productive cough. On examination she
is pyrexial at 38.4°C and has
hepatosplenomegaly. After 2 weeks in
hospital all cultures have been negative so
a liver biopsy is taken. This shows
caseating liver granulomas. What is the
underlying diagnosis?
A) Sarcoidosis
B) Tuberculosis
C) Lymphoma
D) Bronchogenic carcinoma
E) Amyloidosis
Question 39. A 64-year-old lady who
recently travelled to the UK from Baghdad
presents with a 3-month history of loss of
appetite, weight loss, pyrexial symptoms
and productive cough. On examination she
is pyrexial at 38.4°C and has
hepatosplenomegaly. After 2 weeks in
hospital all cultures have been negative so
a liver biopsy is taken. This shows
caseating liver granulomas. What is the
underlying diagnosis?
A) Sarcoidosis
B) Tuberculosis
C) Lymphoma
D) Bronchogenic carcinoma
E) Amyloidosis
66
Which one of the following abnormalities
is apparent on the chest X-ray?
A) Left upper lobe collapse
B) Left lower lobe collapse
C) Right upper lobe collapse
D) Right middle lobe collapse
E) Right lower lobe collapse
Question 41. The same patient from the
previous question (Q40) then has some
routine blood
tests:
Which of the following is the most likely
unifying diagnosis?
A) Tuberculosis
B) Small-cell bronchogenic carcinoma
C) Bronchial adenocarcinoma
D) Sarcoidosis
E) Aspergilloma
Question 42. Which of the following
histological subtypes of lung cancer is
most commonly associated with
hypercalcaemia in the absence of bony
metastases?
A) Small-cell carcinoma
B) Bronchoalveolar carcinoma
C) Squamous carcinoma
D) Adenocarcinoma
E) Adenosquamous carcinoma
Question 43. All of the following except
one are contraindications to surgical
resection in bronchial carcinoma. Which is
the exception?
A) Continued cigarette smoking
B) Malignant pleural effusion
C) Involvement of contralateral
mediastinal lymph nodes
D) Forced expiratory volume in 1 second
(FEV1) of 0.8 litres
E) Presence of bony metastases
Question 44. Which of the following is
not normally associated with persistent
pulmonary arterial hypertension?
A) Chronic venous thromboembolism
B) Progressive systemic sclerosis
C) Chronic obstructive pulmonary disease
D) Chronic exposure to high altitude
E) Asthma
Question 45. Which of the following
disorders is not associated with the
development of pulmonary fibrosis?
A) Systemic lupus erythematosus
B) Rheumatoid arthritis
C) Systemic sclerosis
D) Rheumatic fever
E) Sarcoidosis
Question 46. All of the following
treatments except one are used in the
management of primary pulmonary
hypertension. Which is the exception?
A) Sildenafil (Viagra)
B) Warfarin
C) Intravenous prostacyclin infusion
D) Heart-lung transplantation
E) Intravenous endothelin
67
Question 47. A 28-year-old gentleman
with no prior history of chest trouble is
referred following the receipt of a chest Xray report performed as part of routine
occupational health screening. For the last
10 years he has been employed by a
fireplace firm as a stone cutter. The
factory is extremely dusty and although he
has been supplied with a face mask, he
finds it uncomfortable to wear. His chest
X-ray shows multiple well-circumscribed
3-5 mm nodular opacities predominantly
in the mid- and upper zones Which one of
the following statements is correct?
A) The most likely diagnosis is miliary
tuberculosis
B) The most likely diagnosis is silicosis
C) The disease is unlikely to progress
following cessation of exposure
D) Lung function is likely to show an
obstructive defect
E) Screening of the other employees is
unnecessary
Question 48. A 60-year-old man has been
undergoing treatment for stage IIIA
Hodgkins disease. He received
chemotherapy with adriamycin,
bleomycin, vinblastine and dacarbazine.
Several months later he developed a dry
cough, exertional breathlessness and
intermittent pyrexia. Examination revealed
fine late inspiratory crackles. The full
blood count was normal (including white
cell count), and sputum samples were
negative for acid-fast bacilli and bacterial
pathogens. Serology showed no evidence
of infection with atypical pathogens. The
chest X-ray showed diffuse
reticulonodular shadowing. Which one of
the following statements is correct?
A) Bronchoalveolar lavage would be the
investigation of choice to diagnose
Pneumocystis carinii (jirovecii)
pneumonia (PCP)
B) The clinical scenario could be
explained by bleomycin toxicity
C) Lung function tests would be expected
to show an obstructive defect
D) Lung toxicity could be decreased by
the administration of G-CSF therapy
E) The appearances on high-resolution CT
(HRCT) scan are likely to be diagnostic
Chapter
19 ENDOCRINE DISEASE
Answers page 188
Question 1. Which of the following
molecules does not contain iodine?
A) Thyroxine (T4)
B) Thyroid-stimulating hormone (TSH)
C) Triiodothyronine (T3)
D) Reverse triiodothyronine (rT3)
E) Amiodarone
Question 2. A 38-year-old woman is
referred to the medical outpatient clinic
with a 6-month history of heat intolerance,
palpitations and weight loss despite a
normal appetite. Examination reveals a
fine tremor and sinus tachycardia but is
otherwise unremarkable. Blood tests show
the following results:
TSH receptor antibodies are detected in
her serum. What is the most likely
diagnosis?
A) Toxic multinodular goiter
B) Toxic thyroid adenoma
C) Graves' thyrotoxicosis
D) Secondary thyrotoxicosis due to a
pituitary tumour
E) Factitious thyrotoxicosis
Question 3. A 59-year-old man with
clinical and biochemical evidence of
thyrotoxicosis undergoes 99mtechnetium
scanning (scintigraphy) of the thyroid.
This reveals a well-defined area of
increased isotope uptake with no uptake
through the rest of the gland. What is the
most likely diagnosis?
A) Thyroiditis
B) Papillary thyroid carcinoma
C) Toxic multinodular goiter
D) Medullary carcinoma of the thyroid
E) Toxic thyroid adenoma
68
Question 4. Which of the following ocular
signs of thyrotoxicosis is not specific to
Graves' disease?
A) Exophthalmos
B) Lid lag
C) Periorbital oedema
D) Chemosis
E) Ophthalmoplegia
Question 5. Which of the following
autoantibodies are most strongly
associated with Graves' disease?
A) Anti-thyroid peroxidase antibodies
B) Anti-thyroglobulin antibodies
C) Anti-nuclear antibodies (ANA)
D) Thyroid-stimulating hormone (TSH)
receptor antibodies (TRAb)
E) Anti-neutrophil cytoplasmic antibodies
(ANCA)
Question 6. A 75-year-old woman attends
the hospital accident and emergency
department with palpitations. Her past
medical history is unremarkable, although
she has recently developed a troublesome
tremor. ECG reveals atrial fibrillation with
a ventricular rate of 145 bpm. Blood
pressure is 129/68 mmHg. Blood tests
show biochemical evidence of
thyrotoxicosis. What would be the most
appropriate initial treatment?
A) Digoxin
B) Propranolol
C) Verapamil
D) Amiodarone
E) DC cardioversion
Question 7. All of following except one
are recognised causes of hypothyroidism.
Which is the exception?
A) Hashimoto's thyroiditis
B) Post-partum thyroiditis
C) Graves' disease
D) Hyperprolactinaemia
E) Radioactive iodine treatment for
hyperthyroidism
Question 8. A 52-year-old woman attends
her general practitioner with a 1-year
history of fatigue, cold intolerance, weight
gain and pain in her left hand at night.
Blood tests reveal the following:
The most appropriate initial management
would be:
A) Arrange an ultrasound scan of the
thyroid
B) Arrange a 99mtechnetium scan of the
thyroid
C) Start treatment with thyroxine
D) Start carbimazole
E) Do not start treatment now but recheck
thyroid function tests in 3 months
Question 9. Which of the following might
necessitate a decrease in the maintenance
dose of thyroxine in patients with primary
hypothyroidism?
A) Pregnancy
B) Normal ageing
C) Treatment for epilepsy with phenytoin
D) Treatment for tuberculosis with
rifampicin
E) Development of coeliac disease
69
Question 10. A 74-year-old woman is
brought to the hospital accident and
emergency department with severe
drowsiness. According to her daughter,
she has become increasingly fatigued and
lethargic over the past year and has gained
considerable weight. Her memory has also
deteriorated but over the last few days she
has become significantly more confused
and drowsy. On examination, her Glasgow
Coma Score is 12/15, temperature is
32.4°C, blood pressure 96/53 mmHg and
pulse 48 bpm. She is pale and her face and
hands appear puffy. A provisional
diagnosis of myxoedema coma is made
and urgent thyroid function tests are
requested. The most appropriate initial
management would be to:
A) Wait for the thyroid function test
results
B) Give oral thyroxine via a nasogastric
tube
C) Give IV triiodothyronine
D) Give IV triiodothyronine and IM
hydrocortisone
E) Insert a temporary transvenous pacing
wire
Question 11. All of the following except
one are recognised complications of
subtotal thyroidectomy for Graves'
thyrotoxicosis. Which is the exception?
A) Facial nerve injury
B) Transient hypocalcaemia
C) Keloid scar formation
D) Hoarse voice
E) Primary hypothyroidism
Question 12. Which of the following
statements is true of the drug carbimazole
in the treatment of Graves' disease?
A) It reduces peripheral conversion of
thyroxine (T4) to triiodothyronine (T3)
B) There is a 30% risk of agranulocytosis
C) The risk of relapse is greater than 30%
within 2 years of stopping the drug
D) It is preferable to propylthiouracil in
treating hyperthyroidism in breastfeeding
mothers
E) It is associated with an increased risk of
thyroid malignancy
Question 13. Serum calcitonin levels are
useful in monitoring response to treatment
of which thyroid condition?
A) Medullary carcinoma
B) Thyroid lymphoma
C) Riedel's thyroiditis
D) Follicular carcinoma
E) Hashimoto's thyroiditis
Question 14. Which one of the following
is not employed in the investigation and
treatment of papillary carcinoma of the
thyroid?
A) Fine needle aspiration of the thyroid
B) Carbimazole
C) Total thyroidectomy
D) Radioactive iodine
E) Measurement of serum thyroglobulin
Question 15. All of the following except
one are causes of hypogonadotrophic
hypogonadism. Which is the exception?
A) Pituitary adenoma
B) Anorexia nervosa
C) Cystic fibrosis
D) Autoimmune gonadal failure
E) Excessive physical exercise
Question 16. Which of the following
statements is true regarding postmenopausal oestrogen-containing
hormone replacement therapy (HRT)?
A) Treatment is usually continued until the
age of 65
B) Women with an intact uterus should
receive both oestrogen and progesterone
C) It has been demonstrated to reduce the
risk of ischaemic heart disease
D) It is a useful adjuvant treatment for
thrombophilia
E) It reduces the risk of breast cancer
Question 17. Which of the following is
least likely to cause hyperprolactinaemia?
A) Bromocriptine
B) Metoclopramide
C) Pituitary adenoma
D) Pregnancy
E) Hypothyroidism
70
Question 18. All of the following
measures except one have a role in the
treatment of polycystic ovarian syndrome
(PCOS). Which is the exception?
A) Metformin
B) Combined oral contraceptive pill
C) Gliclazide
D) Weight loss
E) Cyproterone acetate
Question 19. All of the following are
recognised features of Turner's syndrome
except one. Which is the exception?
A) Short stature
B) Coarctation of the aorta
C) Widely spaced nipples
D) Webbing of the neck
E) Low follicle-stimulating hormone
(FSH) and luteinising hormone (LH)
levels
Question 20. Which one of the following
statements is true of Klinefelter's
syndrome?
A) It is associated with a 47XYY
karyotype
B) Affected individuals suffer from
hypogonadotrophic hypogonadism
C) There is an increased incidence of
gynaecomastia
D) Treatment with growth hormone is
usually required
E) Testes are usually absent
Question 21. Which of the following
tumour markers is most useful in the
diagnosis and prognosis of testicular
tumours?
A) Carcinoembryonic antigen (CEA)
B) Prostate-specific antigen (PSA)
C) Lactate dehydrogenase (LDH)
D) Alpha-fetoprotein (AFP)
E) CA125
Question 22. Which one of the following
statements regarding parathyroid hormone
PTH) is false?
A) It is a polypeptide hormone
B) It inhibits 1V-hydroxylation of vitamin
D in the kidney
C) It stimulates calcium resorption from
bone
D) It promotes calcium resorption from
renal tubules
E) Its release is inhibited by
hypercalcaemia
Question 23. All of the following except
one are recognised causes of
hypercalcaemia. Which is the exception?
A) Primary hyperparathyroidism
B) Secondary hyperparathyroidism
C) Tertiary hyperparathyroidism
D) Multiple myeloma
E) Squamous cell bronchial carcinoma
Question 24. Which cluster of features is
classically seen in multiple endocrine
neoplasia (MEN) type 2 (Sipple's
syndrome)?
A) Hyperparathyroidism, pituitary
adenoma, pancreatic neuro-endocrine
tumour
B) Hyperparathyroidism, follicular thyroid
carcinoma, phaeochromocytoma
C) Hyperparathyroidism, medullary
thyroid carcinoma, phaeochromocytoma
D) Hyperparathyroidism, small cell lung
carcinoma, colon carcinoma
E) Phaeochromocytoma, renal cell
carcinoma, cerebellar haemangioblastoma
Question 25. A 41-year-old woman with
Graves' disease undergoes subtotal
thyroidectomy. Twenty-four hours postoperatively she complains that she is
unable to straighten her fingers. She also
describes tingling around her mouth. What
pattern of abnormalities is most likely to
be seen on blood testing?
A) High calcium, high phosphate, low
parathyroid hormone
B) High calcium, low phosphate, high
parathyroid hormone
C) Low calcium, high phosphate, low
parathyroid hormone
71
D) Low calcium, high phosphate, high
parathyroid hormone
E) Low calcium, high phosphate, normal
parathyroid hormone
Question 26. Which one of the following
skeletal changes is not a feature of primary
hyperparathyroidism?
A) Osteophyte formation
B) Reduced bone mineral density
C) Osteitis fibrosa cystica
D) Chondrocalcinosis
E) Terminal resorption in the phalanges
Question 27. A 43-year-old woman
attends her GP with a 1-year history of
progressive weight gain and malaise. She
bruises easily and has trouble climbing
stairs. She also has increased facial hair.
On examination she has a body mass index
of 32 kg/m2. Her abdomen is obese with
visible striae, although her arms and thighs
appear wasted. What is the most likely
diagnosis?
A) Conn's syndrome
B) Cushing's syndrome
C) Addison's disease
D) Phaeochromocytoma
E) Congenital adrenal hyperplasia
Question 28. What is the most common
cause of Cushing's syndrome?
A) Pituitary adenoma
B) Adrenal adenoma
C) Adrenal carcinoma
D) Chronic glucocorticoid therapy
E) Ectopic adrenocorticotrophic (ACTH)
syndromes
Question 29. What is the most useful
initial diagnostic investigation in a patient
with suspected Cushing's syndrome?
A) Random plasma cortisol measurement
B) Short Synacthen test
C) Overnight dexamethasone suppression
test
D) Oral glucose tolerance test
E) Twenty-four-hour urine metanephrines
Question 30. Which of the following
clinical and serum biochemical parameters
is most consistent with Addison's disease?
A) High blood pressure, low sodium, high
potassium
B) Low blood pressure, low sodium, high
potassium
C) Low blood pressure, high sodium, high
potassium
D) Low blood pressure, high sodium, low
potassium
E) High blood pressure, high sodium, high
potassium
Question 31. Which of the following
drugs is the most appropriate medical
treatment for hypertension associated with
Conn's syndrome?
A) Bendroflumethiazide
B) Atenolol
C) Perindopril
D) Amlodipine
E) Spironolactone
Question 32. A 32-year-old man describes
a 4-month history of recurrent headaches
associated with sweating and palpitations.
During one of these episodes he is found
to have a blood pressure of 210/105
mmHg and pulse of 112 bpm. A 24-hour
urine collection shows elevated
metanephrine and normetanephrine
excretion. An abdominal CT scan shows a
large left adrenal mass. What is the most
appropriate first-line antihypertensive
agent?
A) Atenolol
B) Phenoxybenzamine
C) Ramipril
D) Nifedipine
E) Bendroflumethiazide
Question 33. A 17-year-old woman with a
strong family history of diabetes mellitus
is brought to the hospital accident and
emergency department after collapsing at
home. On arrival she has a Glasgow Coma
Score of 9/15. Laboratory blood glucose is
1.2 mmol/l. Plasma insulin levels are
elevated and C-peptide levels are low. Her
condition improves following treatment
72
with IV dextrose. She has had three
similar episodes over the preceding 6
months. What is the most likely diagnosis?
A) Insulinoma
B) Alcohol excess
C) Diabetes mellitus
D) Administration of exogenous insulin
E) Sulphonylurea ingestion
Question 34. Excessive secretion of which
hormone is responsible for carcinoid
syndrome?
A) Gastrin
B) Vasoactive intestinal peptide (VIP)
C) Glucagon
D) 5-hydroxytryptamine (5-HT)
E) Somatostatin
Question 35. A 29-year-old man is
referred to the medical outpatient clinic
with a 3-month history of polyuria. He
describes increasing thirst and drinks large
volumes of fluid. On examination he
appears euvolaemic. A water deprivation
test reveals the following results:
The most likely diagnosis is:
A) Diabetes mellitus
B) Nephrogenic diabetes insipidus
C) Cranial diabetes insipidus
D) Addison's disease
E) Syndrome of inappropriate antidiuretic
hormone secretion (SIADH)
Question 36. A 43-year-old man is
referred to the endocrinology clinic with a
1-year history of headaches and sweating.
His shoe size has increased and his
wedding ring no longer fits. Which of the
following is the investigation of choice in
establishing the cause of his symptoms?
A) Oral glucose tolerance test
B) CT head scan
C) MRI head scan
D) Insulin tolerance test
E) 24-hour urinary cortisol measurement
Chapter
20 DIABETES MELLITUS
Answers page 195
Question 1. Which one of the following is
a physiological action of insulin?
A) Increased lipolysis
B) Increased gluconeogenesis
C) Increased ketogenesis
D) Decreased glycogenolysis
E) Decreased protein synthesis
Question 2. All of the following are
causes of secondary diabetes mellitus
except one. Which is the exception?
A) Acromegaly
B) Corticosteroid treatment
C) Haemochromatosis
D) Phaeochromocytoma
E) Addison's disease
Question 3. All of the following
statements about type 1 diabetes are true
except one. Which is the exception?
A) Viral infection has been implicated in
the aetiology
B) There is an association with pernicious
anaemia
C) There is destruction of the pancreatic
islet ß-cells
D) Treatment with insulin is essential
E) Concordance rates between
monozygotic twins are greater than 90%
Question 4. All of the following
statements except one are true of type 2
diabetes. Which is the exception?
A) It is frequently detected incidentally on
blood testing
B) It is associated with the metabolic
syndrome
C) Ketoacidosis is a common complication
D) There is an increased risk of ischaemic
heart disease
E) The prevalence is higher than that of
type 1 diabetes
73
Question 5. A 58-year-old lady presents to
her GP with a 6-month history of general
malaise and fatigue. The GP does routine
blood tests and finds her to have a fasting
glucose of 7.5 mmol/l. A repeat fasting
glucose 1 month later is 7.4 mmol/l. The
most appropriate next step would be to:
A) Repeat a fasting glucose measurement
in 1 month's time
B) Perform an oral glucose tolerance test
C) Measure C-peptide levels
D) Explain to the patient that she has
diabetes mellitus
E) Reassure the patient that she has normal
glucose tolerance
Question 6. What is the most common
cause of glycosuria?
A) Type 1 diabetes
B) Type 2 diabetes
C) A low renal threshold for glucose in an
otherwise healthy individual
D) Urine testing immediately after a meal
in an otherwise healthy individual
E) Pyelonephritis
Question 7. What is the most informative
method of assessing a patient's glycaemic
control in the diabetic outpatient clinic?
A) Performing urine dipstick analysis for
glucose
B) Performing urine dipstick analysis for
protein
C) Measuring plasma glucose
D) Measuring glycated haemoglobin
(HbA1C)
E) Careful analysis of the patient's dietary
intake according to carbohydrate
exchanges
Question 8. A 23-year-old man with type
1 diabetes presents to the hospital
Accident and Emergency department with
a 24-hour history of nausea, poor appetite
and feeling unwell. Initial investigations
show the following results:
What is the most immediate management
priority?
A) Administration of intravenous insulin
and intravenous saline
B) Administration of intravenous insulin
and intravenous potassium
C) Administration of intravenous insulin
and broad-spectrum antibiotics
D) Administration of intravenous insulin
and intravenous sodium bicarbonate
E) Central line insertion to enable accurate
monitoring of fluid balance
Question 9. A 63-year-old man with
diabetes presents to the hospital Accident
and Emergency department with a 4-day
history of feeling tired and unwell. He
complains of severe thirst. On examination
he appears dehydrated with a pulse of 116
bpm and blood pressure of 114/68 mmHg.
After routine investigations, he is found to
be in a hyperosmolar non-ketotic
hyperglycaemic state. Which one of the
following statements regarding this
condition is true?
A) Higher doses of insulin are usually
required compared to diabetic ketoacidosis
B) Subcutaneous heparin should be
administered within the first 24 hours
C) There is usually a profound metabolic
acidosis
D) People with types 1 and 2 diabetes are
affected equally
E) Large volumes of intravenous sodium
bicarbonate are often needed
74
Question 10. Features of hypoglycaemia
include all the following except one.
Which is the exception?
A) Sweating
B) Kussmaul breathing
C) Confusion
D) Coma
E) Tachycardia
Question 11. You are asked to review a
67-year-old lady on the ward with insulintreated type 2 diabetes, who is
complaining of nausea, sweating and
palpitations. Blood glucose strip testing
gives a reading of 2.6 mmol/l. What would
be the most appropriate initial
management?
A) Intravenous dextrose
B) Intramuscular glucagon
C) Intravenous glucagon
D) Oral carbohydrate
E) Taking a blood sample for a formal
laboratory measurement of blood glucose
Question 12. A 73-year-old lady with type
2 diabetes presents to hospital with an
acute myocardial infarction (MI). She
normally takes metformin. What is the
most appropriate way to maintain
glycaemic control in the peri-infarct
period?
A) Continue metformin at the current dose
B) Continue metformin at a higher dose
C) Stop metformin and monitor blood
glucose readings over the first 24 hours
D) Stop metformin and commence a
sulphonylurea
E) Stop metformin and commence
intravenous insulin
Question 13. A 29-year-old pregnant
woman is referred to clinic with a
diagnosis of gestational diabetes. What
would the best treatment be?
A) Gliclazide alone
B) Metformin alone
C) Insulin alone
D) Insulin plus gliclazide
E) Insulin plus metformin
Question 14. What is the correct perioperative management of an insulintreated type 2 diabetic patient undergoing
a laparotomy?
A) Position the patient at the head of the
operation list and omit insulin until after
the operation
B) Administer his or her usual
subcutaneous insulin pre-operatively and
monitor blood glucose
C) Administer half his or her usual
subcutaneous dose pre-operatively and
monitor blood glucose
D) Start an intravenous infusion of
dextrose and insulin in place of the
patient's usual therapy
E) Give him or her one dose of an oral
anti-diabetic agent to prevent high blood
glucose levels peri-operatively
Question 15. A patient with type 2
diabetes and a body mass index of 34
kg/m2 has suboptimal glycaemic control
with dietary therapy alone. Which of the
following would be the most appropriate
first-line pharmacological treatment?
A) Gliclazide
B) Metformin
C) Rosiglitazone
D) Insulin
E) Metformin plus insulin
Question 16. Which of the following
statements about the thiazolidinediones
(glitazones) is false?
A) They act by binding to peroxisome
proliferator-activated receptor-W (PPAR-W)
B) They do not increase insulin secretion
C) They are particularly useful in diabetic
patients with left ventricular dysfunction
D) They are useful agents in obese type 2
diabetic patients
E) They rarely cause hypoglycaemia
Question 17. Which one of the following
drugs is correctly paired with its
predominant side-effect?
A) Metformin X hypoglycaemia
B) Metformin X weight gain
C) Gliclazide X lipohypertrophy
D) Glipizide X hypoglycaemia
E) Rosiglitazone X lactic acidosis
75
Question 18. What is the biggest cause of
mortality in diabetic patients?
A) Ischaemic heart disease
B) Hypoglycaemia
C) Renal failure
D) Diabetic ketoacidosis
E) Infection
Question 19. Which of the following
fundal abnormalities is not typical of
diabetic retinopathy?
A) Hard exudates
B) Microaneurysms
C) Flame haemorrhages
D) Cotton wool spots
E) Venous loops and beading
Question 20. Which one of the following
retinal appearances is a key feature of preproliferative diabetic retinopathy?
A) Microaneurysms with hard exudates
B) Papilloedema
C) Neovascularisation
D) Venous beading with cotton wool spots
E) Pre-retinal haemorrhage
Question 21. A 61-year-old man with type
2 diabetes has evidence of background
diabetic retinopathy when examined at the
diabetic clinic. He normally takes
gliclazide, metformin and lisinopril. What
is the most appropriate management?
A) Urgent referral to an ophthalmologist
for laser photocoagulation
B) Routine referral to an ophthalmologist
C) Regular follow-up in the diabetic clinic
but no referral to ophthalmology
D) Stop metformin and follow up in the
diabetic clinic
E) Stop lisinopril and follow up in the
diabetic clinic
Question 22. In the absence of
contraindications, which of the drugs in
the following list is the optimal antihypertensive agent in a diabetic patient
with microalbuminuria?
A) Bendroflumethiazide (bendrofluazide)
B) Atenolol
C) Ramipril
D) Doxazosin
E) Amlodipine
Question 23. All of the following
statements except one are true of diabetic
neuropathy. Which is the exception?
A) The incidence can be reduced by strict
glycaemic control
B) Motor, sensory and autonomic nerves
can all be involved
C) The majority of patients are
asymptomatic
D) Charcot joints are a recognised
complication
76
E) It is typically associated with painful
foot ulcers
Question 24. Which one of the following
is a feature of diabetic autonomic
neuropathy?
A) VI nerve palsy
B) Carpal tunnel syndrome
C) Diabetic amyotrophy
D) Gastroparesis
E) Stocking distribution of sensory loss in
the legs
Chapter
21
ALIMENTARY TRACT AND
PANCREATIC DISEASE
Answers page 200
Question 1. Which one of the following
features on clinical examination would
suggest a kidney rather than a spleen as
the cause of a palpable left upper quadrant
mass?
A) Cannot palpate above it
B) Presence of a notch
C) Dullness to percussion
D) Extends towards the right iliac fossa
E) Rounded mass
Question 2. The major enzyme
responsible for protein digestion in the
small bowel is:
A) Trypsin
B) Amylase
C) Lipase
D) Cholecystokinin
E) Pepsin
Question 3. The enzyme amylase is
principally responsible for the breakdown
of which one of the following?
A) Protein
B) Cholesterol
C) Glycogen
D) Bile salts
E) Triglycerides
Question 4. The gut hormone
cholecystokin (CCK) produces all of the
following effects except one. Which is the
exception?
A) Gallbladder contraction
B) Increased secretion of pancreatic
enzymes
C) Satiety
D) Increased gastric acid secretion
E) Relaxation of the sphincter of Oddi
77
Question 5. A 55-year-old lady with a 3month history of progressive dysphagia
and weight loss is investigated with a
barium swallow:
What is the most likely diagnosis?
A) Achalasia
B) Oesophageal candidiasis
C) External oesophageal compression by
bronchial carcinoma
D) Oesophageal carcinoma
E) Myasthenia gravis
Question 6. Which of the following tests
is most useful in the assessment of
pancreatic exocrine function?
A) Faecal elastase
B) CT scan of abdomen
C) 3-day faecal fat
D) Fasting blood glucose
E) Lactose hydrogen breath test
Question 7. The urea breath test is useful
in the diagnosis of which one of the
following conditions?
A) Bacterial overgrowth
B) Helicobacter pylori infection
C) Lactose intolerance
D) Fat malabsorption
E) Coeliac disease
Question 8. In which of the following
causes of dysphagia would oesophageal
manometry be most likely to provide the
diagnosis?
A) Myasthenia gravis
B) Bulbar palsy
C) Pseudobulbar palsy
D) Carcinoma of oesophagus
E) Achalasia
Question 9. An otherwise fit and well 40year-old man presents with a history of
troublesome dyspepsia. Which of the
following features in his presentation
would be the strongest indication for
proceeding to upper gastrointestinal
endoscopy?
A) Poor response to antacids
B) Symptoms worse at night
C) Family history of peptic ulcer disease
D) Symptoms persistent for > 3 months
prior to treatment
E) Associated difficulty in swallowing
Question 10. Which of the following
drugs is least likely to be implicated in a
patient presenting with vomiting?
A) Erythromycin
B) Codeine phosphate
C) Atenolol
D) Cisplatin
E) Digoxin
Question 11. In patients presenting with
acute upper gastrointestinal haemorrhage,
all of the following factors except one are
associated with an increased risk of death.
Which is the exception?
A) Pulse > 100 bpm
B) Mallory-Weiss tear as the cause of
bleeding
C) Visible but non-bleeding vessel present
at endoscopy
D) Age over 60 years
E) Associated renal failure
78
Question 12. A patient presents with acute
lower gastrointestinal bleeding and
features of shock. Which of the following
conditions would be least likely to account
for this presentation?
A) Diverticular disease
B) Angiodysplasia
C) Meckel's diverticulum
D) Bowel ischaemia
E) Anal fissure
Question 13. In the assessment of
diarrhoea, which one of the following
clinical features most strongly suggests a
colonic aetiology?
A) Right iliac fossa pain
B) Undigested food in stool
C) Blood and mucus in stool
D) Large-volume stool
E) Abdominal bloating
Question 14. Which one of the following
physical consequences of malabsorption is
incorrectly matched with the
corresponding vitamin or mineral
deficiency?
A) Acrodermatitis enteropathica Zinc
B) Purpura and bruising Vitamin K
C) Koilonychia Iron
D) Peripheral neuropathy Vitamin C
E) Night blindness Vitamin A
Question 15. A patient recently
commenced on a new medication
complains of constipation. Which of the
following drugs is most likely to be
implicated?
A) Erythromycin
B) Digoxin
C) Orlistat
D) Metformin
E) Verapamil
Question 16. Which of the following
conditions is least likely to cause oral
ulceration?
A) Coeliac disease
B) Kaposi's sarcoma
C) Behçet's disease
D) Herpes simplex virus
E) Psoriasis
Question 17. Which one of the following
factors does not predispose to gastrooesophageal reflux disease (GORD)?
A) Pregnancy
B) High intake of coffee
C) Weight loss
D) Delayed gastric emptying
E) Hiatus hernia
Question 18. Which one of the following
statements is true of Barrett's oesophagus?
A) It refers to neoplastic change in the
normal squamous cells of the lower
oesophagus
B) The majority of patients with the
condition ultimately develop carcinoma of
the oesophagus
C) It is associated with increased alcohol
intake
D) Patients with the condition should
undergo regular endoscopic surveillance
with biopsies
E) Antireflux surgery has been shown to
induce regression of the condition
Question 19. A 34-year-old man presents
with severe retrosternal burning
discomfort, worse at night and after large
meals and eased by various 'over-thecounter' antacid remedies. There are no
other symptoms and his general health is
good. Which of the following statements
concerning his condition is true?
A) Upper gastrointestinal endoscopy is
mandatory to exclude Barrett's oesophagus
B) A history of weight gain prior to the
onset of symptoms would raise doubt as to
the diagnosis
C) Proton pump inhibitors (PPIs) and H2receptor antagonists are equally effective
in relieving symptoms and inducing
healing of oesophagitis
D) Recurrence of symptoms following
cessation of medical treatment is common
E) Antireflux surgery is rarely successful
in relieving symptoms
Question 20. A 57-year-old woman
presents with a 12-month history of slowly
progressive dysphagia for solids, eased by
drinking liquids. She also experiences
intermittent episodes of severe chest pain.
79
A barium swallow is performed:
What is the most likely diagnosis?
A) Diffuse oesophageal spasm
B) Achalasia
C) Systemic sclerosis
D) Carcinoma of oesophagus
E) Myasthenia gravis
Question 21. Which one of the following
statements is true concerning carcinoma of
the oesophagus?
A) The overall 5-year survival is
approximately 40%
B) CT is superior to endoscopic ultrasound
in local staging
C) A history of painful, intermittent
dysphagia for solids and liquids is the
usual presenting complaint
D) The presence of hoarseness suggests
mediastinal invasion
E) Symptomatic relief of swallowing
difficulties is best achieved by palliative
radiotherapy
Question 22. A 45-year-old male presents
with a 10-month history of recurrent,
'gnawing' epigastric pain. The pain does
not radiate and can be absent for up to a
month at a time but, when present, seems
to be relieved by eating. He has also
experienced occasional vomiting. With
which of the following diagnoses would
his symptoms fit best?
A) Chronic peptic ulcer
B) Biliary colic
C) Chronic pancreatitis
D) Mesenteric ischaemia
E) Crohn's disease
Question 23. The patient from the
previous question (Q22) who has
suspected peptic ulcer disease has an
endoscopy performed. This reveals a
chronic duodenal ulcer. The CLO test is
positive. Which one of the following
statements regarding further management
is false?
A) Treatment with acid-suppressant
therapy and H. pylori eradication is likely
to cure the ulcer
B) Advice should be given that cigarette
smoking increases the risk of ulcer
complications and reduces the chance of
healing
C) It is unlikely the patient will require
surgery for the ulcer
D) The patient should be given specific
advice on dietary restriction
E) Non-steroidal anti-inflammatory drugs
(NSAIDs) should be avoided
Question 24. Which one of the following
statements concerning the bacterium
Helicobacter pylori is true?
A) It is a Gram-positive rod
B) It produces an enzyme called 'urease'
that lowers the surrounding pH
C) It exclusively colonises gastric-type
epithelium
D) Strains expressing the enzyme cagA
are less often associated with disease
E) On colonising the stomach it induces
increased secretion of somatostatin from D
cells
Question 25. All of the following
statements concerning the consequences of
H. pylori infection are true except one.
Which is the exception?
A) The majority of colonised individuals
remain healthy and asymptomatic
B) It is the most common cause of chronic
gastritis
C) Around 40% of patients with duodenal
ulcer are infected with H. pylori
D) It is a recognised risk factor for the
development of gastric cancer
E) Some gastric lymphomas may be cured
solely by H. pylori eradication
80
Question 26. Which of the following is
least likely to occur as a complication of
partial gastrectomy?
A) Weight gain
B) Flushing, sweating and lightheadedness
after meals with large carbohydrate
content
C) Postprandial diarrhoea and abdominal
discomfort
D) Anaemia
E) Early satiety
Question 27. A 32-year-old woman
presents with severe recurrent epigastric
pain. Endoscopy reveals multiple ulcers in
the duodenum, stomach and oesophagus.
There is no history of ingestion of nonsteroidal anti-inflammatory drugs
(NSAIDs) and tests for H. pylori are
negative. Serum gastrin levels are grossly
elevated. What is the likely diagnosis?
A) Covert NSAID abuse
B) Carcinoid syndrome
C) Zollinger-Ellison syndrome
D) Crohn's disease
E) Biliary reflux
Question 28. All of the following except
one are recognised risk factors for gastric
carcinoma. Which is the exception?
A) Autoimmune chronic gastritis
B) Zollinger-Ellison syndrome
C) Cigarette smoking
D) H. pylori infection
E) Familial adenomatous polyposis (FAP)
Question 29. Which one of the following
conditions is not associated with coeliac
disease?
A) Type 1 diabetes mellitus
B) Pernicious anaemia
C) Conn's syndrome
D) Primary biliary cirrhosis
E) Dermatitis herpetiformis
Question 30. The differential diagnosis of
subtotal villous atrophy includes all of the
following conditions except one. Which is
the exception?
A) Tropical sprue
B) AIDS enteropathy
C) Giardiasis
D) Dermatitis herpetiformis
E) Mesenteric ischaemia
Question 31. Which of the following
statements is true concerning coeliac
disease in adults?
A) Patients are intolerant of maize and rice
B) Peak onset is in the third decade
C) Almost all patients who do not follow a
gluten-free diet are symptomatic
D) Adhering to a strict gluten-free diet
increases the risk of metabolic bone
disease
E) There is an increased risk of T-cell
lymphoma
Question 32. A 55-year-old male presents
with a 6-hour history of severe, constant
upper abdominal pain radiating to the
back. He drinks approximately 80 units of
alcohol per week. On examination there is
marked epigastric tenderness but no
guarding or rebound tenderness. Which of
the following tests is likely to be most
useful in reaching a positive diagnosis?
A) Plain abdominal X-ray
B) C-reactive protein
C) Erect chest X-ray
D) ECG
E) Serum amylase
Question 33. All of the following except
one are uncommon but recognised causes
of acute pancreatitis. Which is the
exception?
A) Azathioprine therapy
B) Mumps
C) Hypocalcaemia
D) Hypothermia
E) Seat belt injury
81
Question 34. Which one of the following
is not an adverse prognostic factor in acute
pancreatitis?
A) White blood cell count 16 ×
109/l (normal range 4-11 × 109/l)
B) Urea 20 mmol/l (normal range 2.5-6.6
mmol/l)
C) Albumin 28 g/l (normal range 35-50
g/l)
D) Amylase 1000 U/l (normal range < 100
U/l)
E) Glucose 14 mmol/l (normal range 3.65.8 mmol/l)
Question 35. Concerning the management
of acute pancreatitis, which one of the
following statements is true?
A) Hypocalcaemia should be corrected
urgently if the corrected calcium falls
below 2.0 mmol/l
B) Enteral feeding should be started at an
early stage in patients with severe
pancreatitis
C) Prophylaxis of thromboembolism is
inadvisable in the first 48 hours
D) In gallstone pancreatitis, emergency
endoscopic retrograde
cholangiopancreatography (ERCP) and
stone extraction should be avoided if there
is evidence of ascending cholangitis
E) Opiate analgesia is usually not require
Question 36. Which one of the following
would be considered an unexpected
clinical feature in chronic pancreatitis?
A) Steatorrhoea
B) Weight loss
C) Pain relieved by drinking alcohol
D) Recurrent hypoglycaemia
E) Skin pigmentation over the back
Question 37. A 56-year-old lady presents
with a 4-week history of weight loss and
progressively worsening jaundice with
pruritus. On examination she is deeply
icteric and has a palpable gallbladder.
What is the likeliest diagnosis?
A) Chronic cholecystitis
B) Hepatocellular carcinoma
C) Ascending cholangitis
D) Carcinoma of pancreas
E) Amoebic abscess
Question 38. Which one of the following
statements regarding carcinoma of the
pancreas is true?
A) The majority of tumours are amenable
to potentially curative resection
B) The body of the pancreas is the most
common site of origin
C) Coeliac plexus neurolysis is useful in
relieving pruritus
D) The liver is a common site for
metastatic deposits
E) The prognosis is better than for
carcinoma of the ampulla of Vater
Question 39. Which one of the following
pathological features would favour a
diagnosis of ulcerative colitis over Crohn's
disease?
A) Presence of fistulae
B) Proximal colitis with rectal sparing
C) Lymphoid aggregates and
microgranulomas
D) Ulceration within the small intestine
E) Inflammation limited to the mucosa
Question 40. Which of the following
would be least expected to provoke a
relapse ('flare') of ulcerative colitis?
A) Loss of job
B) Cigarette smoking
C) Ankle sprain treated with oral
diclofenac
D) Viral laryngitis
E) Course of antibiotics for falsely
suspected urinary tract infection
Question 41. A 19-year-old male presents
with a 10-day history of bloody diarrhoea
and lower abdominal pain associated with
fever, malaise and anorexia. Which of the
following investigations would be least
helpful in establishing a diagnosis?
A) Stool culture and microscopy
B) Sigmoidoscopy and rectal biopsy
C) Blood cultures and serological tests of
infection
D) Serum albumin
E) Examination of stool for Clostridium
difficile toxin
82
Question 42. With reference to the patient
in the previous question (Q41) who has
bloody diarrhoea and lower abdominal
pain, stool is negative for culture,
Clostridium difficile toxin, ova and cysts.
Sigmoidoscopy and rectal biopsy reveal
typical features of ulcerative colitis. In the
assessment of the severity of this attack,
all of the following except one suggest
severe disease. Which is the exception?
A) 10 bowel motions per day
B) Stool volume 200 g/24 hrs
C) Temperature of 38°C on 2 consecutive
days
D) Pulse 110 bpm
E) Erythrocyte sedimentation rate 80
mm/hr
Question 43. The patient from the
previous question (Q42) has several
clinical and laboratory parameters
indicating severe ulcerative colitis. Which
one of the following is true regarding the
management of this attack?
A) Nutritional support, if required, should
be provided intravenously rather than
enterally
B) The patient should be treated with
intravenous corticosteroids
C) Surgery should not be considered until
he has had at least 10 days of maximal
medical therapy
D) Prophylaxis of venous
thromboembolism with heparin should be
avoided
E) Sulfasalazine overcomes the need for
surgery in around 80% of patients who fail
to respond to corticosteroids
Question 44. On the fourth day of medical
treatment the patient from the previous
question (Q43) does not show any signs of
improvement. A plain abdominal X-ray is
performed:
Which one of the following statements is
true?
A) It is unusual for this complication to
occur in the first attack of colitis
B) The original diagnosis of ulcerative
colitis was probably incorrect
C) The patient should be referred for
urgent colectomy
D) No further action should be taken but
the X-ray should be repeated in 24 hours
E) Azathioprine treatment may avoid the
need for surgery in patients with this
complication
Question 45. Which one of the following
statements concerning intestinal
complications of inflammatory bowel
disease (IBD) is incorrect?
A) In ulcerative colitis, colonic perforation
may occur without the development of
toxic megacolon
B) In Crohn's disease, enterovesical
fistulation may present with pneumaturia
C) The risk of developing colon cancer in
ulcerative colitis is related to both the
extent and the duration of colitis
D) Both conditions may present with acute
life-threatening haemorrhage
E) Diarrhoea in ulcerative colitis may be
due to enteroenteric fistulae
83
Question 46. Which one of the following
systemic complications of inflammatory
bowel disease is not related to the activity
of bowel disease?
A) Conjunctivitis
B) Primary sclerosing cholangitis
C) Erythema nodosum
D) Arthralgia
E) Pyoderma gangrenosum
Question 47. Concerning the management
of Crohn's disease, which one of the
following statements is false?
A) Due to high rates of relapse, infliximab
therapy should be combined with diseasemodifying agents
B) Maintenance of remission is improved
by cessation of cigarette smoking
C) Corticosteroids are preferred to
methotrexate for maintaining remission
D) Surgical intervention should be
conservative to minimise loss of viable
intestine
E) Azathioprine is an effective
maintenance treatment
Question 48. Which one of the following
clinical features is least suggestive of
irritable bowel syndrome (IBS)?
A) Colicky abdominal pain relieved by
defaecation
B) Sensation of incomplete defaecation
C) Symptoms disturbing sleep
D) Alternating diarrhoea and constipation
E) Passage of mucus
Question 49. Regarding the management
of irritable bowel syndrome (IBS), which
one of the following statements is true?
A) Patients with constipation as the
predominant symptom benefit most from
tricyclic antidepressant therapy
B) Elimination diets are the mainstay of
treatment
C) Probiotics are of proven benefit
D) Reassurance alone may lead to
resolution of symptoms
E) All patients should be advised to
increase dietary fibre
Question 50. A 75-year-old lady presents
with a 2-hour history of sudden-onset
severe abdominal pain and per rectum
bleeding. Other than a stroke 2 years ago
she keeps well. She has been on aspirin
and ramipril since her stroke and takes
digoxin for an irregular heart rhythm. On
examination she is very distressed; her
abdomen is soft with no evidence of
peritonism. Bowel sounds are audible. An
arterial blood gas shows a metabolic
acidosis. What is the likeliest diagnosis?
A) Ruptured aortic aneurysm
B) Acute small bowel ischaemia
C) Perforated peptic ulcer
D) Diverticulitis
E) Irritable bowel syndrome
Question 51. A 73-year-old lady is
admitted to hospital with a severe
community-acquired pneumonia. She is
treated with intravenous antibiotics and on
the sixth day of her admission develops
profuse diarrhoea associated with
cramping lower abdominal pain. What test
is most likely to reveal the cause of her
diarrhoea?
A) Stool microscopy for ova and parasites
B) Barium enema
C) Stool culture for Escherichia coli
D) Legionella serology
E) Stool analysis for Clostridium difficile
toxin
84
Question 52. With regard to colonic
polyps, which one of the following
statements is true?
A) They usually present with lower
gastrointestinal bleeding or anaemia
B) The size of the polyp has no bearing on
the risk of malignant change
C) Asymptomatic polyps found at
colonoscopy should be biopsied but not
removed
D) Polyps with a villous architecture carry
a higher risk of malignant change than
those with tubular architecture
E) The polyps in Peutz-Jeghers syndrome
are predominantly colonic adenomas
Question 53. All of the following except
one are recognised risk factors for
colorectal cancer. Which is the exception?
A) Presence of colorectal adenomas
B) Smoking
C) High dietary calcium
D) Acromegaly
E) Long-standing extensive ulcerative
colitis
Question 54. A 68-year-old lady presents
to her GP with tiredness and weight loss
and is found to have iron deficiency
anaemia. On examination there is a
palpable mass in the right iliac fossa.
Which of the following is the most
appropriate next investigation to establish
the diagnosis?
A) Flexible sigmoidoscopy
B) Abdominal CT scan
C) Abdominal ultrasound
D) Colonoscopy
E) Serum carcinoembryonic antigen
(CEA)
Chapter
22
LIVER AND BILIARY TRACT
DISEASE
Answers page 208
Question 1. Which of the following is not
a function of the liver?
A) Synthesis of clotting factors
B) Production of vitamin K
C) Production of glucose during fasting
D) Storage of copper
E) Excretion of potentially toxic
compounds
Question 2. In a hepatic acinus, zone 3 is
closest to the central hepatic vein. Which
of the following statements concerning
zone 3 is true?
A) It is exposed to the highest
concentrations of toxins
B) It is closer to the bile duct than zones 1
and 2
C) It is the primary site of bile salt
formation
D) It has a good oxygen supply relative to
zones 1 and 2
E) It is the primary site of lipolysis in the
liver
Question 3. A hospital inpatient is noted
to have an elevated gamma-glutamyl
transferase (GGT) with otherwise normal
liver function tests. She is taking the
following regular medications. Which one
is most likely to have caused this
abnormality?
A) Omeprazole
B) Paracetamol
C) Phenytoin
D) Ibuprofen
E) Sodium valproate
85
Question 4. Of the following conditions,
which is the most likely cause of jaundice
accompanied by a seven-fold elevation of
alanine aminotransferase and two-fold
elevation of alkaline phosphatase?
A) Viral hepatitis
B) Acute cholecystitis
C) Gilbert's syndrome
D) Haemolysis
E) Pancreatic carcinoma
Question 5. Which one of the following is
most suggestive of haemolysis as the
cause of jaundice?
A) Pale stools
B) Raised alanine aminotransferase (ALT)
C) Presence of spider naevi
D) Bilirubinuria
E) Raised reticulocyte count
Question 6. Which one of the following
coagulation factors depends on vitamin K
for complete synthesis in the liver?
A) Factor IV
B) Factor V
C) Factor VIII
D) Factor IX
E) Factor XI
Question 7. Which of the following tests
provides the most information about
hepatic synthetic function within the last
12 hours?
A) Activated partial thromboplastin time
(APTT)
B) Albumin
C) Fibrinogen
D) Urea
E) Prothrombin time (PT)
Question 8. Which one of the following is
a contraindication to percutaneous liver
biopsy?
A) Chronic obstructive pulmonary disease
(COPD) with forced expiratory volume in
1 second (FEV1)/forced vital capacity
(FVC) of 37%
B) Failure to comply with fasting
requirements
C) Platelet count of 190
D) Prothrombin time prolonged by 2
seconds
E) Family history of haemochromatosis
Question 9. A jaundiced patient has the
following liver function test (LFT) results:
Which one of the following is the most
appropriate initial investigation to identify
the underlying problem?
A) Endoscopic retrograde
cholangiopancreatography (ERCP)
B) Hepatic portal venography
C) Abdominal X-ray
D) Abdominal ultrasound
E) Liver biopsy
Question 10. Only one of the following
options associates the disease with the
correct initial diagnostic test. Which is it?
A) Wilson's disease Transferrin saturation
B) Primary biliary cirrhosis
(PBC) Antimitochondrial antibody (AMA)
C) Alpha1-antitrypsin
deficiency Caeruloplasmin
D) Primary sclerosing cholangitis Antiendomysial antibody
E) Coeliac disease 24-hour urinary copper
Question 11. A patient presents to her GP
after noticing that the whites of her eyes
have become yellow. Direct questioning
also reveals that her urine has been very
dark for several days. Which of the
following diagnoses is the most likely
explanation for these symptoms?
A) Carotenaemia
B) Cholestatic jaundice
C) Hyperbilirubinaemia secondary to
Gilbert's syndrome
86
D) Rhabdomyolysis
E) Dehydration
Question 12. A 47-year-old man with a
history of alcoholic cirrhosis is well
known on the general medical ward after
recurrent admissions for drainage of
ascites. He presents with confusion, fever
(38.5°C), ascites and abdominal pain.
Which of the following investigations is
most important to establish the diagnosis?
A) Stool culture and microscopy for ova,
cysts and parasites
B) Diagnostic laparoscopy
C) Abdominal ultrasound scan
D) CT scan of abdomen
E) Ascitic fluid white cell count
Question 13. Which of the following is
the first-line drug of choice to treat chronic
ascites secondary to hepatic cirrhosis?
A) Furosemide
B) Spironolactone
C) Digoxin
D) Bendroflumethiazide
E) Vasopressin
Question 14. Which of the following
blood results confers the worst prognosis
on a patient with acute liver failure
secondary to paracetamol overdose?
A) Prothrombin time (PT) > 100 secs
B) Aspartate aminotransferase (AST) > 6
times normal
C) Alanine aminotransferase (ALT) > 2.5
times normal
D) Platelets < 100 × 109/l
E) Albumin < 35 g/dl
Question 15. Which of the following
examination findings is not characteristic
of a palpable spleen?
A) A palpable mass that the examiner
cannot get above
B) Dull to percussion
C) May be balloted
D) Moves with respiration
E) Felt superficially
Question 16. Which of the following
statements about primary biliary cirrhosis
is true?
A) It is more common in men
B) Transplant is contraindicated because
of the high risk of disease recurrence
C) Pruritus is a more common presenting
feature than jaundice
D) A positive antinuclear antibody is
diagnostic
E) Immunosuppression prevents disease
progression
Question 17. Which of the following
drugs is most useful in a patient with a
suspected variceal haemorrhage, where
urgent upper gastrointestinal endoscopy is
not available?
A) Noradrenaline (norepinephrine)
B) Activated protein C
C) Dopamine
D) Terlipressin
E) Ciprofloxacin
Question 18. Which of the following
viruses is not capable of causing infection
without concurrent infection with another
hepatitis virus?
A) Hepatitis A
B) Hepatitis B
C) Hepatitis C
D) Hepatitis D
E) Hepatitis E
Question 19. Which one of the following
statements about hepatitis A virus (HAV)
infection is true?
A) It is commonly spread by sexual
transmission
B) It may be spread by the faecal-oral
route
C) A chronic carrier state occurs in a
minority of infected patients
D) No vaccine is available
E) Anti-HAV of IgG type is useful
diagnostically
Question 20. Which one of the following
statements about hepatitis B infection is
true?
A) It may be spread in faeces
B) The route of infection does not affect
clinical course
C) It is caused by an RNA virus
87
D) No vaccine is available
E) It may cause cirrhosis
Question 21. In a patient with suspected
hepatitis B infection, which of the
following serological tests is most
suggestive of previous exposure to
hepatitis B virus?
A) HBsAg alone
B) HBsAg and HBeAg
C) HBsAb alone
D) Anti-HBc IgM alone
E) Anti-HBc IgG and HBsAb
Question 22. A 23-year-old nurse is found
to have abnormal liver function tests, and
serological tests for hepatitis B are
performed. He has a positive titre for antiHBs but no other positive serological tests.
What is the significance of this finding?
A) It indicates a hepatitis B chronic carrier
state
B) It suggests acute hepatitis B
C) It effectively rules out hepatitis B as the
cause of his illness
D) It is consistent with convalescence
following acute hepatitis B
E) It indicates concurrent infection with
hepatitis D
Question 23. Which one of the following
statements about infection with hepatitis B
virus (HBV) is false?
A) The majority of patients make a full
recovery from acute infection
B) Chronic infection may lead to
hepatocellular carcinoma
C) HBeAg-negative patients respond less
well to treatment
D) Antiviral therapy usually results in
resistant mutants of HBV
E) Treatment with interferon is ineffective
in chronic infection
Question 24. Which one of the following
statements is true of hepatitis C infection?
A) It is usually sexually transmitted
B) A minority of patients exposed to the
virus will become chronically infected
C) Once infected, cure is impossible
D) Liver transplantation is contraindicated
due to the risk of reinfection of the
transplanted liver
E) Acute infection is usually
asymptomatic
Question 25. Which of the following
statements about alcoholic liver disease
(ALD) is true?
A) Once cirrhosis develops, abstinence
does not affect prognosis
B) There is a genetic predisposition
C) Binge drinkers are more likely to
develop ALD than those with a consistent
intake
D) The presence of fatty liver (steatosis)
on biopsy suggests an alternative diagnosis
E) Transplantation is contraindicated
Question 26. A 34-year-old woman is
referred to the gastrointestinal clinic after
her GP discovers abnormal liver function
tests (LFTs). She denies alcohol abuse or
sexual risk factors. She received a blood
transfusion in the UK in 2002 following a
road traffic accident. Her past medical
history includes obesity (body mass index
= 42), type 2 diabetes mellitus and
anxiety/depression. What is the most
likely cause of her deranged LFTs?
A) Occult drug overdose
B) Alcoholic liver disease
C) Non-alcoholic fatty liver disease
D) Hepatitis B infection
E) Hepatitis A infection
Question 27. A 42-year-old hospital
inpatient, with previously normal liver
function and weighing 73 kg, develops
abnormal liver function tests. She has
taken the following medications at
therapeutic doses in the last 28 days.
Which one is most likely to have caused
the problem?
A) Co-amoxiclav
B) Paracetamol
C) Temazepam
D) Morphine
E) Furosemide
Question 28. A 37-year-old man presents
to his GP complaining of tiredness,
polyuria and thirst. On examination, he is
found to have 4 cm hepatomegaly and a
greyish pigmentation to his skin.
Urinalysis reveals a large amount of
glycosuria. His past medical history
includes osteoarthritis, for which he takes
88
regular ibuprofen. Which of the following
provides the best unifying diagnosis?
A) Wilson's disease
B) Diabetes insipidus
C) Acute viral hepatitis
D) Infectious mononucleosis
E) Hereditary haemochromatosis
Question 29. With reference to the patient
in the previous question (Q28) who has
hereditary haemochromatosis, which of
the following is the most appropriate
initial treatment?
A) Liver transplant
B) Weekly venesection of 500 ml blood
C) Warfarin
D) Hepatic lobe resection
E) Metformin
Question 30. A 25-year-old patient
presents with an episode of acute hepatitis
from which he recovers spontaneously and
is discharged from hospital with a
presumptive diagnosis of occult drug use.
A year later he presents with fatigue,
tremor at rest affecting both hands, and
occasional wild, purposeless movements
of his upper limbs. The admitting hospital
doctor
notes an abnormality on examination of
the eyes:
What is the most likely diagnosis?
A) Ecstasy (MDMA) abuse
B) Budd-Chiari syndrome
C) Wilson's disease
D) Hereditary haemochromatosis
E) Amanita phalloides poisoning
Question 31. Which of the following
treatments is most appropriate for Wilson's
disease (hepatolenticular degeneration)?
A) Penicillamine
B) Desferrioxamine
C) Exchange transfusion
D) Venesection
E) Smoking cessation
Question 32. World-wide, which of the
following is the most important risk factor
for hepatocellular carcinoma?
A) Alcoholic liver disease
B) Haemochromatosis
C) Non-alcoholic steatohepatitis (NASH)
D) Alpha1-antitrypsin deficiency
E) Chronic viral hepatitis
Question 33. An overweight 41-year-old
woman with a body mass index of 32
presents with a 5-day history of severe
right upper quadrant pain. Initially the pain
was intermittent, lasting for 2 hours then
subsiding, but for the past 12 hours it has
been constant. On examination she is
pyrexial (38.5°C) and there is tenderness
and rigidity in the right upper quadrant.
Her white cell count is 18 × 109/l and Creactive protein 130 mg/l. Liver function
tests (LFTs) and amylase are within the
normal range. Which of the following
diagnoses is most likely?
A) Biliary colic
B) Acute pancreatitis
C) Acute cholecystitis
D) Mirizzi's syndrome
E) Choledocholithiasis
Question 34. Which one of the following
hormones causes contraction of the
gallbladder and release of bile acids in the
fed state?
A) Insulin
B) Somotostatin
C) Cholecystokinin
D) Glucagon
E) Noradrenaline (norepinephrine)
89
Question 35. Which of the following
patterns of symptoms is most
characteristic of acute blockage of the
cystic duct by a gallstone?
A) Recurrent epigastric pain, radiating to
the back, lasting 2 hours then subsiding
spontaneously
B) Constant severe interscapular pain
associated with sweating and hypotension
C) Constant severe epigastric pain and
recurrent vomiting
D) Intermittent burning epigastric pain
relieved by drinking milk
E) Crushing, heavy epigastric pain
radiating to the jaw associated with
sweating, nausea and a terror of imminent
death
Question 36. Which of the following
investigations is most appropriate for the
initial diagnosis of acute symptomatic
gallstone disease?
A) CT of the abdomen
B) Abdominal ultrasound scan
C) Chest X-ray
D) Plain abdominal X-ray
E) Kidney-ureter-bladder (KUB) X-ray
Question 37. Which of the following is
most important before performing a
transjugular intrahepatic portosystemic
shunt insertion (TIPSS)?
A) Sclerotherapy to oesophageal varices
B) Correction of any coagulopathy with
fresh-frozen plasma
C) Normalisation of urea and electrolytes
D) Cessation of alcohol abuse
E) Psychiatric evaluation
Question 38. Which one of the following
statements about alcoholic liver disease is
true?
A) The characteristic pathological lesion is
microvesicular steatosis
B) Once fatty change has developed, the
condition is irreversible
C) Cholestasis and hepatitis are both
common presentations
D) Cirrhosis is an inevitable consequence
of chronic alcoholism
E) Beverages containing less than 10%
alcohol are unlikely to cause liver damage
Question 39. In which one of the
following conditions is hepatomegaly least
likely to be found on clinical examination?
A) Alcoholic hepatitis
B) Hepatic venous outflow obstruction
(Budd-Chiari syndrome)
C) Hepatic metastases
D) Haemochromatosis
E) Chronic hepatitis C infection
90
Question 40. Which of the following
factors is least likely to be a precipitant of
hepatic encephalopathy?
A) Constipation
B) Upper gastrointestinal bleed
C) Hypokalaemia
D) Hypoglycaemia
E) Urinary tract infection
Chapter
23 BLOOD DISORDERS
Answers page 213
Question 1. Which one of the following
statements regarding red blood cells is
false?
A) They are derived from megakaryocytes
B) Production is stimulated by
erythropoietin from the kidneyss
C) Increased production is associated with
increased numbers of circulating
reticulocytes
D) Mature red blood cells have a
biconcave disc shape
E) Mature red blood cells do not possess a
nucleus or mitochondria
Question 2. Which one of the following
conditions is not typically associated with
an eosinophilia?
A) Asthma
B) Hay fever
C) Eczema
D) Pneumococcal infection
E) Hookworm infection
Question 3. Which of the following drugs
is most likely to induce neutropenia?
A) Omeprazole
B) Prednisolone
C) Carbimazole
D) Ciprofloxacin
E) Alendronate
Question 4. Which one of the following
conditions is most likely to produce a
microcytosis on blood film examination?
A) Autoimmune haemolytic anaemia
B) Alcohol excess
C) Thalassaemia
D) Vitamin B12 deficiency
E) Hypothyroidism
91
Question 5. The presence of target cells
on the peripheral blood film is most likely
to be explained by which of the following
disorders?
A) Myelofibrosis
B) Cirrhosis
C) Haemolytic uraemic syndrome
D) Lead poisoning
E) Vitamin B12 deficiency
Question 6. All of the following except
one are causes of splenomegaly. Which is
the exception?
A) Chronic myeloid leukaemia
B) Multiple myeloma
C) Alcoholic cirrhosis
D) Malaria
E) Myelofibrosis
Question 7. Which one of the following
statements regarding the coagulation
cascade is true?
A) Most clotting factors are synthesised in
the bone marrow
B) Coagulation by the extrinsic pathway is
initiated by the interaction of factor VII
with tissue factor
C) The intrinsic pathway is the major
mechanism underlying coagulation in vivo
D) Heparin exerts its anticoagulant effect
by binding to protein C
E) The final step in the cascade is the
conversion of prothrombin to thrombin
Question 8. Which one of the following
clotting factors does not require vitamin K
for its activation?
A) Factor II
B) Factor V
C) Factor VII
D) Factor IX
E) Factor X
Question 9. Which one of the following
statements regarding the prothrombin time
is false?
A) It assesses the extrinsic pathway of the
coagulation cascade
B) It is prolonged in patients taking
warfarin
C) It provides an accurate assessment of
platelet function
D) It is normal in haemophilia A
E) It is prolonged in patients with factor X
deficiency
Question 10. In a patient presenting with a
bleeding disorder, which of the following
clinical features would be most suggestive
of a coagulation defect as opposed to a
platelet disorder?
A) Epistaxis
B) Haemarthrosis
C) Menorrhagia
D) Prolonged bleeding from superficial
cuts
E) Purpura
Question 11. All of the following
statements regarding haemophilia A are
correct except one. Which is the
exception?
A) The condition shows X-linked
recessive inheritance
B) There is deficiency of factor VIII
C) Muscle haematomas are a characteristic
manifestation
D) Desmopressin aggravates the tendency
to bleeding
E) It may be complicated by secondary
osteoarthritis
Question 12. A 29-year-old woman
attends hospital with a painful swollen
right leg. She flew back to the UK from
Australia 2 days previously. According to
the Wells scoring system, her clinical risk
of deep vein thrombosis (DVT) is 'high'.
Which of the following tests is the most
appropriate first step in her investigation?
A) Coagulation screen
B) Plasma D-dimer
C) Doppler ultrasound scan of the leg
D) Venous plethysmography
E) Thrombophilia screen
92
Question 13. Which one of the following
statements about ABO red cell groups is
true?
A) The most common blood group in the
UK is group B
B) Individuals with blood group AB will
have circulating antibodies against both A
and B antigens
C) Infusion of group A red cells to a group
O recipient should cause no more than a
mild transfusion reaction
D) Patients with group B blood group can
only receive group B red cells
E) ABO incompatibility reactions are
mediated by complement
Question 14. Which one of the following
statements regarding the Rhesus D (RhD)
blood group is false?
A) Around 85% of Caucasians express the
RhD red cell antigen
B) Anti-RhD antibodies of IgG type can
cross the placenta
C) Transfusion of RhD-negative blood to
an RhD-positive woman may result in
production of anti-RhD antibodies
D) Rhesus antibodies may cause severe
anaemia and hyperbilirubinaemia in RhDpositive fetuses
E) RhD-negative women of child-bearing
potential exposed to RhD-positive blood
should receive anti-RhD immunoglobulin
(anti-D)
Question 15. A 73-year-old woman on a
regular transfusion programme is admitted
for a blood transfusion. Her baseline
observations are satisfactory. Twenty
minutes into the transfusion she is noted to
have a temperature of 37.9°C. She feels
well in herself and examination is
otherwise unremarkable. What is the most
appropriate course of action?
A) Stop transfusion and give oral iron
instead
B) Stop transfusion and administer IV
chlorphenamine and hydrocortisone
C) Administer broad-spectrum antibiotics
D) Give paracetamol and continue
transfusion at a slower rate
E) Take an urgent blood sample for a
repeat 'group and screen' test
Question 16. In the UK blood products
are screened for all of the following
infections except one. Which is the
exception?
A) Human immunodeficiency virus (HIV)
B) Syphilis
C) Hepatitis B
D) Hepatitis C
E) Creutzfeldt-Jakob disease (CJD)
Question 17. Long-term use of which of
the following drugs can lead to iron
malabsorption?
A) Omeprazole
B) Ferrous sulphate
C) Aspirin
D) Mesalazine
E) Sodium valproate
Question 18. A 76-year-old man is
admitted to hospital with a 4-month
history of increasing shortness of breath,
lethargy and weight loss. He has a past
history of angina, and takes aspirin,
atenolol and simvastatin. Examination is
unremarkable. Blood tests reveal the
following:
Which of the following would be the most
appropriate initial investigation?
A) Abdominal ultrasound scan
B) Abdominal CT scan
C) Upper gastrointestinal endoscopy
D) Cystoscopy
E) Laparoscopy
Question 19. All of the following except
one are recognised causes of iron
deficiency anaemia. Which is the
exception?
A) Pregnancy
B) Coeliac disease
C) Cold agglutinin disease
D) Partial gastrectomy
E) Menorrhagia
Question 20. Which one of the following
tests is the most specific indicator of iron
deficiency in the investigation of patients
with anaemia?
A) Reduced mean cell volume
B) Reduced transferrin saturation
C) Low serum iron
D) Reduced ferritin
E) Raised total iron binding capacity
(TIBC)
Question 21. Which one of the following
statements regarding vitamin B12
deficiency is false?
A) Mean cell volume is usually raised
B) It may be caused by terminal ileal
Crohn's disease
C) Neutrophil hypersegmentation on the
blood film is characteristic
D) It is often due to dietary deficiency
E) There may be associated pancytopenia
Question 22. Which of the following
neurological findings is not a feature of
vitamin B12 deficiency?
A) Cognitive impairment
B) Nystagmus
C) Ataxic gait
D) Extensor plantar responses
E) Symmetrical peripheral neuropathy
93
Question 23. Which one of the following
statements about folate is true?
A) Deficiency may result from pernicious
anaemia
B) Dairy products offer a rich source of
folate
C) Total body stores are small
D) The Schilling test is useful in
establishing the reason for folate
deficiency
E) Serum folate is the most accurate
indicator of overall body stores
Question 24. A 29-year-old woman
attends her GP with increasing lethargy
and malaise. Blood tests reveal the
following:
Question 25. In a patient with haemolytic
anaemia, which of the following findings
would be most suggestive of intravascular
haemolysis?
A) Raised reticulocyte count
B) Haemosiderinuria
C) Raised lactate dehydrogenase (LDH)
D) Splenomegaly
E) Positive direct Coombs test
Question 26. Which one of the following
statements about hereditary spherocytosis
is false?
A) It usually shows autosomal dominant
inheritance
B) Pregnancy can precipitate a
megaloblastic crisis
C) It may lead to the development of
cholesterol gallstones
D) Patients should receive treatment with
folic acid
E) The anaemia may be improved by
splenectomy
Question 27. Deficiency of which of the
following enzymes is associated with
haemolytic anaemia?
A) Alpha-glucosidase
B) Red cell transketolase
C) Glucose-6-phosphate dehydrogenase
D) Lactate dehydrogenase
E) Tyrosine kinase
Which of the following diagnoses is most
consistent with these results?
A) Coeliac disease
B) Pernicious anaemia
C) Autoimmune haemolytic anaemia
D) Hereditary spherocytosis
E) Anaemia of chronic disease
94
Question 28. Which one of the following
statements regarding sickle-cell disease is
true?
A) Sickle-cell trait results in an increased
susceptibility to falciparum malaria
B) The condition shows X-linked
inheritance
C) Haemoglobin electrophoresis
demonstrates a predominance of HbF
D) Sickle-cell anaemia is usually
accompanied by a reticulocytosis
E) With optimal medical care for sicklecell anaemia, life expectancy is unaffected
Question 29. Which one of the following
is not a clinical manifestation of sickle-cell
disease?
A) Peripheral neuropathy
B) Dactylitis
C) Avascular necrosis of the hip
D) Splenic infarction
E) Pulmonary fat embolism
Question 30. A 25-year-old Spanish man
is referred to the haematology clinic after a
routine full blood count is found to be
abnormal. Blood tests reveal the
following:
Investigations reveal the following:
What is the most likely diagnosis?
A) Aplastic anaemia
B) Chronic myeloid leukaemia (CML)
C) Acute myeloid leukaemia (AML)
D) Non-Hodgkin lymphoma
E) Myelodysplastic syndrome
Question 32. A 58-year-old woman is
referred to the haematology clinic with an
abnormal full blood count. She describes a
6-month history of tiredness, weight loss
and shortness of breath. On examination
there is marked hepatosplenomegaly but
no lymphadenopathy. Investigations reveal
the following:
What is the most likely diagnosis?
A) Alpha-thalassaemia
B) Beta-thalassaemia major
C) Beta-thalassaemia minor
D) Sickle-cell disease
E) Congenital sideroblastic anaemia
Question 31. A 59-year-old man is
referred to the haematology clinic with a
3-month history of progressive lethargy.
He complains of recurrent sore throat and
has recently noticed bleeding from his
gums when he brushes his teeth. He has
also noticed that he bruises easily. He
appears pale but examination is otherwise
unremarkable.
95
What is the most likely diagnosis?
A) Hodgkin's disease
B) Acute myeloid leukaemia (AML)
C) Acute lymphoblastic leukaemia
D) Chronic myeloid leukaemia (CML)
E) Chronic lymphocytic leukaemia
Question 33. Which haematological
condition is associated with the
Philadelphia chromosome [t(9;22)]?
A) Myelofibrosis
B) Myelodysplastic syndrome
C) Multiple myeloma
D) Chronic lymphocytic leukaemia
E) Chronic myeloid leukaemia (CML)
Question 34. Which one of the following
statements about chronic lymphocytic
leukaemia (CLL) is false?
A) In the majority of cases, the diagnosis
is made incidentally following a routine
full blood count
B) There is a monoclonal proliferation of
B lymphocytes
C) Hyposplenism is a frequent finding
D) The condition is associated with
autoimmune haemolytic anaemia
E) Chlorambucil may be used as first-line
therapy for patients receiving active
treatment
Question 37. A 69-year-old man describes
a 6-month history of lethargy, weight loss
and lower back pain. Blood tests reveal the
following:
Question 35. Which one of the following
statements about myelodysplasia is false?
A) It predominantly affects elderly
individuals
B) It often progress to acute myeloid
leukaemia (AML)
C) Peripheral blood cytopenias are a
characteristic feature
D) Bone marrow aspiration reveals a
hypocellular marrow
E) Curative treatment is not possible in the
majority of patients
Question 36. A 26-year-old man presents
with a 6-week history of a painless
swelling in his neck. On examination he
has painless rubbery cervical
lymphadenopathy but no other palpable
lymph nodes or splenomegaly. Following
lymph node biopsy (see below)
the diagnosis of Hodgkin lymphoma is
made:
What abnormality is shown in the biopsy?
A) Auer rod
B) Reed-Sternberg cell
C) Ringed sideroblast
D) Howell-Jolly body
E) Burr cell
96
What is the most likely diagnosis?
A) Waldenström's macroglobulinaemia
B) Multiple myeloma
C) Renal cell carcinoma with bony
metastases
D) Primary hyperparathyroidism
E) Non-Hodgkin lymphoma
Question 38. The diagnosis of multiple
myeloma requires 2 out of 3 diagnostic
criteria. Which of the following pairs of
results would clinch the diagnosis?
A) Presence of serum paraprotein and
raised plasma calcium
B) Erythrocyte sedimentation rate (ESR) >
100 mm/hr and increased malignant
plasma cells in bone marrow
C) Raised alkaline phosphatase (ALP) and
positive radioisotope bone scan
D) Bence Jones protein in urine and lytic
lesions on plain X-ray
E) Presence of serum paraprotein and
widespread lymphadenopathy
Question 39. Which one of the following
statements regarding polycythaemia rubra
vera is false?
A) Splenomegaly is a common finding
B) Progression to myelofibrosis may occur
C) There is an increased risk of ischaemic
stroke
D) Symptoms are improved by
venesection
E) Aspirin is contraindicated
Question 40. Which condition is
characterised by the combination of
microangiopathic haemolytic anaemia,
neurological signs and renal impairment?
A) Idiopathic thrombocytopenic purpura
B) Thrombotic thrombocytopenic purpura
C) Hereditary haemorrhagic telangiectasia
D) Primary thrombocythaemia
E) Henoch-Schönlein purpura
Question 41. A 74-year-old man is
referred to the medical outpatient clinic
with a 6-month history of weight loss,
fevers and night sweats. He has no
significant past medical history. On
examination there is painless rubbery
97
cervical, axillary and inguinal
lymphadenopathy. There is also palpable
hepatosplenomegaly. Blood tests show a
mild normocytic, normochromic anaemia.
CT confirms the clinical findings and also
demonstrates bulky mediastinal and
retroperitoneal lymph nodes. What is the
most likely diagnosis?
A) Chronic myeloid leukaemia
B) Multiple myeloma
C) Hodgkin's disease
D) Non-Hodgkin lymphoma
E) Myelofibrosis
Question 42. Which one of the following
statements regarding disseminated
intravascular coagulation (DIC) is false?
A) The condition may be precipitated by
Gram-negative septicaemia
B) Thrombocytopenia is a characteristic
finding
C) Fibrinogen levels are elevated
D) D-dimer levels are elevated
E) There is a significant risk of
haemorrhage
Question 43. All of the following
statements about heparin are correct
except one. Which is the exception?
A) Unfractionated intravenous heparin
potentiates the activity of antithrombin
B) Severe bleeding secondary to
intravenous heparin can be reversed with
protamine
C) The anticoagulant effect of low
molecular weight heparin can be assessed
using the activated partial thromboplastin
time (APTT)
D) Thrombocytopenia is a recognised
complication of treatment with heparin
E) Heparin exerts its anticoagulant effect
more quickly than warfarin
Chapter
24 MUSCULOSKELETAL
DISORDERS
Answers page 221
Question 1. A 70-year-old lady who has
recently noticed some hearing difficulty is
found to have a greatly increased plasma
alkaline phosphatase concentration with
normal calcium, phosphate and
parathyroid hormone (PTH) levels. What
is the most likely diagnosis?
A) Osteomalacia
B) Rickets
C) Renal osteodystrophy
D) Paget's disease
E) Osteoporosis
Question 2. A 76-year-old man with type
2 diabetes and longstanding osteoarthritis
of the knees and hips presents to the
hospital accident and emergency
department with a 72-hour history of
progressive pain and swelling of his right
knee. He was recently treated by his
general practitioner for an episode of
cellulitis. On examination, his temperature
is 38.5°C and there is a warm, tense
effusion with marked tenderness and
overlying erythema. Which of the
following is the most likely diagnosis?
A) Haemarthrosis
B) Trauma
C) Septic arthritis
D) Acute gout
E) First presentation of rheumatoid
arthritis
Question 3. With reference to the patient
from the previous question (Q2) who has
suspected septic arthritis, which of the
following investigations would be of
greatest help in confirming the diagnosis?
A) Full blood count
B) C-reactive protein (CRP)
C) X-ray of knee joint
D) Joint aspiration
E) Ultrasound scan of knee joint
98
Question 4. Which one of the following
statements is true with regard to
fibromyalgia?
A) The erythrocyte sedimentation rate
(ESR) is usually elevated
B) Symptoms of pain predominantly arise
from peripheral joints
C) Exacerbations of symptoms are often
associated with stressful life events
D) Systemic steroids form the cornerstone
of treatment
E) Muscle biopsy is the definitive
investigation
Question 5. Which of the following
clinical features is least typical of
osteoarthritis?
A) Joint pain aggravated by activity and
relieved by rest
B) Involvement of large joints
C) Prolonged morning stiffness
D) Presence of Bouchard's nodes
E) Palpable crepitus over affected joint
Question 6. All of the following except
one may form part of the management of
osteoarthritis. Which is the exception?
A) Aerobic and strengthening exercises
B) Non-steroidal anti-inflammatory drugs
C) Total joint replacement
D) Methotrexate
E) Provision of a walking stick
Question 7. A lady is referred to a
rheumatologist by her general practitioner
with suspected rheumatoid arthritis. Which
one of the following features would not
provide support for this diagnosis?
A) Morning stiffness lasting more than an
hour
B) The presence of anti-double-stranded
DNA (anti-dsDNA) antibodies on blood
tests
C) Periarticular osteopenia and marginal
erosions on X-ray
D) Symmetrical pattern of arthritis
E) Duration of symptoms greater than 6
weeks
Question 8. All of the following except
one are well-recognised extra-articular
features of rheumatoid arthritis. Which is
the exception?
A) Episcleritis
B) Pyoderma gangrenosum
C) Pericarditis
D) Alopecia
E) Pulmonary nodules
Question 9. A gentleman of 70 with
longstanding rheumatoid arthritis is found
on a routine blood test to have a white cell
count of < 1 × 109/l. He complains of
abdominal pain, and on examination you
find generalised lymphadenopathy and
splenomegaly. Which of the following is
the most likely diagnosis?
A) Malaria
B) Acute lymphatic leukaemia (ALL)
C) Felty's syndrome
D) Portal hypertension secondary to
alcoholic liver disease
E) Overwhelming septicaemia
Question 10. All of the following clinical
features affecting the hands except one are
characteristic of rheumatoid arthritis.
Which is the exception?
A) Bouchard's nodes
B) Swan neck deformity
C) Piano key deformity
D) Subluxed metacarpophalangeal joints
E) Rupture of the extensor tendons
99
Question 11. Which one of the following
agents is not classified as a diseasemodifying antirheumatic drug (DMARD)?
A) Sulfasalazine
B) Naproxen
C) Penicillamine
D) Sodium aurothiomalate (gold)
E) Azathioprine
Question 12. All of the following except
one are documented side-effects of antiarthritic drugs. Which is the exception?
A) Renal impairment with ciclosporin
B) Pulmonary fibrosis with methotrexate
C) Bone marrow suppression with
azathioprine
D) Keratitis with hydroxychloroquine
E) Gastritis with non-steroidal antiinflammatory drugs (NSAIDs)
Question 13. All of the following except
one are characteristic features of
ankylosing spondylitis. Which is the
exception?
A) Raised erythrocyte sedimentation rate
and C-reactive protein
B) Strongly positive rheumatoid factor
C) Association with HLA-B27
histocompatibility antigen
D) Extraspinal features including anterior
uveitis and aortic incompetence
E) 'Bamboo' spine appearance on X-ray
Question 14. Recognised patterns of
psoriatic arthritis include all of the
following except one. Which is the
exception?
A) Asymmetric oligoarthritis
B) Arthritis mutilans
C) Symmetrical polyarthritis
D) Atlanto-axial instability
E) Distal interphalangeal joint arthritis
Question 15. A 50-year-old man presents
to his general practitioner with an acute
episode of gout. The GP takes a full
history and decides that a likely risk factor
is one of his medications. Which one of
the following drugs would be the most
likely candidate?
A) Bendroflumethiazide
B) Paracetamol
C) Perindopril
D) Atenolol
E) Clopidogrel
Question 19. Which one of the following
statements regarding osteoporosis is true?
A) The most common biochemical profile
is a normal serum calcium and phosphate
with a raised alkaline phosphatase
B) It is less likely to occur in women who
have an early menopause
C) It is highly unlikely in the absence of
symptoms
D) Weight-bearing exercise is protective
E) Bone mineral density Z-score of less
than -2.5 is diagnostic
Question 16. All of the following
statements about gout are true except one.
Which is the exception?
A) A typical attack presents with rapid
onset of severe pain in a single distal joint
B) There is a male preponderance of the
disease
C) Allopurinol is often used in the
treatment of an acute attack
D) High alcohol intake is a risk factor for
the condition in susceptible individuals
E) The monosodium urate crystals
deposited within affected joints are
negatively birefringent when viewed under
polarised light
Question 20. Which of the following
clinical features is least suggestive of
systemic lupus erythematosus (SLE)?
A) Raynaud's phenomenon
B) Scarring alopecia
C) A photosensitive, erythematous malar
rash
D) Sclerodactyly
E) Oral ulcers
Question 17. All of the following except
one are associated with pseudogout
(calcium pyrophosphate dihydrate crystal
deposition). Which is the exception?
A) Hyperparathyroidism
B) Acromegaly
C) Wilson's disease
D) Haemochromatosis
E) Advancing age
Question 18. All of the following factors
except one would increase the likelihood
of a patient developing osteoporosis in
later life. Which is the exception?
A) Cigarette smoking
B) Anorexia nervosa
C) Hypothyroidism
D) Family history of osteoporosis
E) Long-term therapy with oral
corticosteroids
100
Question 21. Which one of the following
statements is true with regard to the use of
bisphosphonates in osteoporosis?
A) They inhibit bone resorption
B) They have been shown to reduce the
risk of fracture in patients with normal
bone mineral density
C) They reduce the risk of fracture but do
not influence bone mineral density
D) There is no effective oral preparation
E) They stimulate bone formation
Question 22. A 46-year-old builder
presents to his general practitioner with a
1-week history of back pain. Which one of
the following features in his presentation
would provide the greatest cause for
concern?
A) Sudden onset of the pain while lifting a
heavy load at work
B) A history of intermittent episodes of
low back pain in the past
C) Pain varying with physical activity but
generally relieved by rest
D) Difficulty passing urine
E) Tenderness of the paraspinous muscles
Question 23. Which one of the following
conditions is associated with a
seronegative arthritis?
A) Systemic lupus erythematosus
B) Rheumatoid arthritis
C) Systemic sclerosis
D) Psoriasis
E) Sjögren's syndrome
Question 24. Which one of the following
is not considered a risk factor for
development of gastrointestinal ulceration,
perforation and bleeding induced by nonsteroidal anti-inflammatory drugs
(NSAIDs)?
A) Age > 60 years
B) Concomitant oral corticosteroid use
C) Concomitant respiratory disease
D) Past history of peptic ulcer disease
E) H. pylori colonisation of the stomach
Question 25. Which one of the following
is a characteristic feature of Reiter's
disease?
A) Conjunctivitis
B) Subcutaneous nodules
C) Strong female preponderance
D) Precipitated by streptococcal throat
infection
E) Positive rheumatoid factor
Question 26. Which one of the following
statements regarding dual energy X-ray
absorptiometry (DXA) bone scanning is
incorrect?
A) The Z-score compares the patient's
bone density to that of an age-matched
control
B) A T-score of -2.5 is indicative of
osteoporosis
C) DXA is indicated in patients with an
early menopause who have not received
hormone replacement therapy
D) The preferred measurement sites for
bone mineral density are the hip and the
lumbar spine
E) DXA bone scanning involves the
intravenous injection of radioisotope
Question 27. A 24-year-old woman with
sclerodactyly and symptoms suggestive of
Raynaud's phenomenon is diagnosed with
systemic sclerosis. Which one of the
101
following statements is true regarding her
treatment?
A) Calcium channel blockers such as
nifedipine may help symptoms of
Raynaud's phenomenon
B) Angiotensin-converting enzyme (ACE)
inhibitors are contraindicated due to the
risk of precipitating a hypertensive renal
crisis
C) Systemic steroids are useful for treating
skin changes
D) H2-receptor antagonists are more
effective than proton pump inhibitors for
treatment of oesophageal reflux
E) There are no effective oral treatments
for pulmonary hypertension
Question 28. Which one of the following
findings on clinical examination is
characteristic of dermatomyositis?
A) Weakness of the distal musculature
B) Tender nodules on the finger pulps
C) A violaceous rash around the eyes
D) Nail pitting
E) Peripheral oedema
Question 29. As the admitting doctor on a
general medical ward, you see a patient
who has been referred from primary care
and is suspected of having
dermatomyositis. Which of the following
investigations (all of which may support or
refute the diagnosis) should you order
first?
A) Electromyography (EMG)
B) Serum creatine kinase (CK)
C) Muscle biopsy
D) CT chest/abdomen/pelvis
E) MRI
Question 30. A 23-year-old lady who
complains of dry eyes and mouth has a
positive Schirmer's test. Serological tests
are positive for antinuclear antibody
(ANA) and rheumatoid factor. Which of
the following is the most likely unifying
diagnosis?
A) Systemic lupus erythematosus (SLE)
B) Sjögren's syndrome
C) Conjunctivitis
D) Rheumatoid arthritis
E) Dehydration
Question 31. All of the following
statements about Sjögren's syndrome are
true except one. Which is the exception?
A) There is an association with HLA-B27
B) There is a female preponderance
C) Enlargement of the salivary glands is
frequently found
D) There is an association with other
autoimmune diseases such as primary
biliary cirrhosis and myasthenia gravis
E) There is an increased risk of developing
lymphoma
Question 32. Which one of the following
features is most typical of polymyalgia
rheumatica?
A) A normal erythrocyte sedimentation
rate (ESR)
B) Poor response to oral corticosteroid
treatment
C) Marked muscle wasting
D) Muscle stiffness and tenderness
E) Mean age of onset of 30 years
Question 33. A 75-year-old lady is
admitted to the medical admissions unit in
the early hours of the morning with a
temporal headache, visual disturbance and
pain on chewing. On examination, she has
decreased visual acuity in her right eye
and tenderness over the right scalp. The
erythrocyte sedimentation rate (ESR) is 95
mm/hr. Which is the most important action
to take?
A) Order a CT of the brain
B) Request an ophthalmology review in
the morning
C) Request a temporal artery biopsy
D) Give 30 mg of dihydrocodeine for pain
relief
E) Give 60 mg of prednisolone by mouth
Question 34. All of the following
statements except one are true of
polyarteritis nodosa. Which is the
exception?
A) Skin manifestations include palpable
purpura and livedo reticularis
B) There is an association with hepatitis B
infection
C) It is a large-vessel vasculitis
D) Peripheral nerve palsies may be
associated
E) Severe hypertension is a recognised
complication
102
Question 35. With regard to the anatomy
of bone, which is the one incorrect
statement below?
A) The normal skeleton consists of both
cortical and trabecular bone
B) Cortical bone is formed from Haversian
systems
C) Osteoclasts are responsible for bone
formation
D) The most abundant protein in bone is
collagen
E) Bone is mineralised with calcium and
phosphate
Question 36. With regard to the anatomy
of joints, which is the one incorrect
statement below?
A) The costochondral joint is an example
of a fibrocartilaginous joint
B) Synovial joints always include two
surfaces covered with articular cartilage
C) Articular cartilage has a rich vascular
supply
D) Synovial fluid is an ultrafiltrate of
plasma containing proteoglycans
E) The joint capsule is in part formed from
ligament
Question 37. Plain radiography of joints is
often a helpful aid to diagnosis in bone
and joint disease. Which is the one
incorrect association in the following list
of radiographic findings?
A) Bony osteophytes and subchondral
sclerosis with osteoarthritis
B) Diffuse narrowing of the joint space
with rheumatoid arthritis
C) Soft tissue swelling with septic arthritis
D) Looser's zones with osteomalacia
E) Osteopenia with Paget's disease of bone
Question 38. Which one of the following
statements about blood tests often used in
rheumatology is incorrect?
A) A high titre of rheumatoid factor at first
presentation of rheumatoid arthritis is a
poor prognostic factor
B) Anti-double-stranded DNA (antidsDNA) antibodies are highly specific for
systemic lupus erythematosus (SLE)
C) Antinuclear antibody (ANA) is a highly
sensitive test for SLE
D) The serum creatine kinase is often
elevated in dermatomyositis
E) Serum biochemistry is usually normal
in osteomalacia
Question 39. A number of weeks after
commencing a new tablet for her blood
pressure, a 49-year-old lady with
hypertension presents to her general
practitioner with a photosensitive rash
affecting her face and hands and newonset arthralgia. The GP also finds
microscopic haematuria on urinalysis and
suspects drug-induced lupus. Which of the
following medications is most likely to
have caused this presentation?
A) Atenolol
B) Lisinopril
C) Minoxidil
D) Hydralazine
E) Nifedipine
103
Question 40. A 12-year-old boy is brought
to clinic by his mother with a rash on his
legs that has appeared over the last 3 days.
He also complains of pain in his knees and
hands, and in the last 24 hours has
developed central abdominal pain. Prior to
this episode he was entirely well, apart
from what his mother describes as a 'cold'
2 weeks ago. On examination, you find a
palpable purpuric rash over the buttocks
and lower limbs. What is the likeliest
diagnosis?
A) Still's disease
B) Henoch-Schönlein purpura
C) Kawasaki disease
D) Rheumatic fever
E) Juvenile idiopathic arthritis
Question 41. With reference to the patient
in the previous question (Q40) who has
suspected Henoch-Schönlein purpura,
which of the following investigations is
least likely to contribute to the diagnosis?
A) Dipstick and microscopy of urine for
red cells
B) Urea and electrolytes (U&E)
C) Full blood count (FBC)
D) Chest X-ray
E) Skin biopsy
Question 42. Which one of the following
conditions is least likely to occur as a
complication of Marfan's syndrome?
A) Lens dislocation
B) Spontaneous pneumothorax
C) Aortic dissection
D) Mitral valve prolapse
E) Pulmonary embolism
Chapter
25 NEUROLOGICAL DISEASE
Answers page 227
Question 1. The nerve root values
corresponding to the biceps tendon reflex
are:
A) C4/C5
B) C5/C6
C) C6/C7
D) C7/C8
E) C8/T1
Question 2. The myelin sheath
surrounding peripheral nerve axons is
formed by:
A) Astrocytes
B) Oligodendrocytes
C) Microglial cells
D) Schwann cells
E) Ependymal cells
Question 3. Which of the following
neurological deficits is most likely to
result from an isolated left temporal lobe
lesion in a right-handed individual?
A) Expressive dysphasia
B) Receptive dysphasia
C) Right hemiparesis
D) Right hemisensory loss
E) Right-sided neglect
Question 4. A 63-year-old man attends the
neurology outpatient clinic with his wife.
His wife reports that for the last few
months he has been behaving completely
out of character; for instance, he has been
shouting and undressing in public. During
the consultation he makes inappropriate
sexual references. On examination he has
a positive grasp reflex. This presentation
would fit best with a lesion in which of the
following sites?
A) Frontal lobe
B) Dominant parietal lobe
C) Non-dominant parietal lobe
D) Dominant temporal lobe
E) Non-dominant temporal lobe
104
Question 5. Which disorder is suggested
by a 3 cycles/second 'spike and wave'
pattern on the electroencephalogram
(EEG)?
A) Juvenile myoclonic epilepsy
B) Childhood absence epilepsy
C) Secondary generalised epilepsy
D) Sporadic Creutzfeldt-Jakob disease
E) Motor neuron disease
Question 6. Nerve conduction studies are
most likely to be helpful in which of the
following conditions?
A) Motor neuron disease
B) Myasthenia gravis
C) Multiple sclerosis
D) Carpal tunnel syndrome
E) Lambert-Eaton syndrome
Question 7. Which of the following
imaging modalities is most likely to yield
diagnostic information in a patient with
suspected multiple sclerosis?
A) Plain skull X-ray
B) Carotid Doppler ultrasound (duplex)
scan
C) CT head scan with contrast
D) CT head scan without contrast
E) MRI head scan
Question 8. A 48-year-old man presents to
the hospital accident and emergency
department with possible meningitis.
Which one of the following would not be a
contraindication to immediate lumbar
puncture?
A) Thrombocytopenia
B) A Glasgow coma score of 10/15
C) Reduced power in the left leg with an
extensor plantar response
D) Current treatment with aspirin
E) Papilloedema
Question 9. Which of the following
features is least consistent with the
headache of raised intracranial pressure?
A) Associated with morning vomiting
B) Worsens as the day progresses
C) Exacerbated by coughing
D) Presence of papilloedema
E) Relieved by simple analgesia
Question 10. A 33-year-old woman
attends her general practitioner with a 4week history of persistent headache. She
describes the sensation of a 'tight band'
around her head but denies any nausea or
visual disturbance. The headache is worse
at the end of the day and responds poorly
to paracetamol. She has managed to
continue working as a shop assistant. What
is the most likely diagnosis?
A) Temporal arteritis
B) Migraine
C) Tension headache
D) Viral meningitis
E) Intracranial space-occupying lesion
Question 11. A 25-year-old woman
attends hospital with a 12-hour history of
intense, throbbing pain on the right side of
her head. She has vomited twice and finds
it uncomfortable to look at bright light.
She gives no history of any visual
disturbance or unusual sensations prior to
the onset of pain. She has experienced two
similar but milder episodes over the last 3
months. What is the most likely diagnosis?
A) Subarachnoid haemorrhage
B) Migraine
C) Viral meningitis
D) Intracranial space-occupying lesion
E) Cluster headache
Question 12. Which of the following
drugs is most useful in the treatment of an
acute severe migraine attack?
A) Sumatriptan
B) Propranolol
C) Pizotifen
D) Sodium valproate
E) Amitriptylin
105
Question 13. Which one of the following
features is characteristic of cluster
headache?
A) More frequent in females
B) Episodic attacks lasting 12-24 hours
C) Patients able to continue normal
activities during pain
D) Pain is predominantly occipital
E) Associated nasal congestion and
conjunctival injection
Question 14. In a patient presenting with
vertigo, which one of the following
features most strongly suggests a central
rather than peripheral (labyrinthine)
cause?
A) Episodes provoked by head movement
B) Persistent nystagmus
C) Tinnitus and distorted hearing
D) Positive Hallpike manoeuvre
E) Vomiting
Question 15. In a patient presenting with a
blackout, which one of the following
features is most suggestive of a seizure?
A) No warning prior to blackout
B) Severely bitten tongue
C) Urinary incontinence
D) Extreme pallor during the unconscious
period
E) Rapid recovery following the collapse
Question 16. A 54-year-old man
experiences partial motor seizures
characterised by uncontrollable jerking of
the right arm and leg. What is the most
likely anatomical focus of seizure activity?
A) Right pre-central gyrus
B) Right post-central gyrus
C) Left pre-central gyrus
D) Left post-central gyrus
E) Left temporal lobe
Question 17. Which one of the following
is not a cause of partial seizures?
A) Astrocytoma
B) Cerebral abscess
C) Cerebral infarction
D) Alcohol withdrawal
E) Intracerebral haemorrhage
Question 18. A 49-year-old teacher is
referred to the medical outpatient clinic
following a first seizure. He has no
significant past medical history. What
advice would you offer him about driving
if he lived in the UK?
A) He can continue driving provided that
he is accompanied at all times
B) He can resume driving once established
on anticonvulsant therapy
C) He should refrain from driving until
seizure-free for 3 months
D) He should refrain from driving until
seizure-free for 1 year
E) He should not drive again
Question 19. Which of the following
drugs is first-line anticonvulsant therapy
for primary generalised tonic-clonic
epilepsy?
A) Phenytoin
B) Gabapentin
C) Levetiracetam
D) Sodium valproate
E) Topiramate
Question 20. First-line drug treatment for
status epilepticus is:
A) IV phenytoin
B) IV propofol
C) IV diazepam
D) IV sodium valproate
E) IV Phenobarbital
Question 21. Which one of the following
clinical signs is caused by lower motor
neuron lesions?
A) Hypertonia
B) Muscle fasciculations
C) Brisk tendon reflexes
D) Clonus
E) Extensor plantar responses
Question 22. Which one of the following
conditions is most likely to be associated
with a resting tremor?
A) Cerebellar stroke
B) Hepatic encephalopathy
C) Essential tremor
D) Parkinson's disease
E) Thyrotoxicosis
106
Question 23. Which one of the following
involuntary movements is incorrectly
paired with its definition?
A) Chorea - jerky, small-amplitude,
purposeless movements
B) Athetosis - slow writhing movements
of the limbs
C) Dystonia - involuntary adoption of an
abnormal posture
D) Hemiballismus - brief, non-purposeful
twitching of muscle groups
E) Tics - repetitive semi-purposeful
movements
Question 24. You are asked to examine a
59-year-old man admitted to the neurology
ward. Examination reveals loss of joint
position and vibration sensation over the
right side of the body, with loss of pain
and temperature sensation over the left
side of the body. There is weakness of the
right arm and leg associated with
increased tone, brisk reflexes and an
extensor plantar. There is no motor deficit
on the left side of the body. Cranial
nerves, including facial sensation, are
intact. What is the most likely cause of
these findings?
A) Left cerebral hemisphere lesion
B) Right-sided cervical spinal cord lesion
C) Left-sided cervical spinal cord lesion
D) Transverse cervical spinal cord lesion
E) Peripheral neuropathy
Question 25. You are asked to review a
patient with reduced consciousness. He is
lying silently with his eyes closed. He
makes no response to any verbal prompts
but when you apply supraorbital pressure
he opens his eyes, makes moaning noises
and attempts to remove your hand. These
findings are consistent on repeated testing.
Based on this data what is his Glasgow
Coma Scale score?
A) 6
B) 7
C) 8
D) 9
E) 10
Question 26. Which one of the following
statements is true of dementia?
A) Prominent visual hallucinations suggest
Pick's disease
B) All patients with severe Alzheimer's
disease should receive a trial of
anticholinesterase drugs
C) Disturbance of language function in the
early stages is an indication for brain
biopsy
D) Recurrent urinary tract infections are a
frequent cause
E) Imaging of the brain (CT or MRI)
should be performed in most patients
Question 27. Which one of the following
is not a feature of cerebellar disease?
A) Ataxia
B) Dysarthria
C) Hyperreflexia
D) Nystagmus
E) Dysdiadochokinesis
Question 28. Which of the following
visual deficits is most likely to occur
secondary to a right parietal stroke?
A) Right homonymous hemianopia
B) Left homonymous hemianopia
C) Right homonymous lower
quadrantanopia
D) Left homonymous lower
quadrantanopia
E) Left homonymous upper
quadrantanopia
Question 29. A 34-year-old woman
complains of double vision on looking to
the right. Eye movement testing confirms
diplopia on rightward gaze. Covering the
right eye causes disappearance of the outer
image. What is the most likely cause of the
diplopia?
A) Right oculomotor (III) nerve lesion
B) Left oculomotor (III) nerve lesion
C) Right trochlear (IV) nerve lesion
D) Right abducens (VI) nerve lesion
E) Left abducens (VI) nerve lesion
107
Question 30. A 74-year-old man
complains of headache and double vision.
On examination the left eye is looking
downwards and abducted with a ptosis.
The right eye appears normal. The left
pupil is dilated and unresponsive but the
right pupil shows normal reactivity to
light. What is the most likely site of the
lesion?
A) Left oculomotor (III) nerve
B) Left trochlear (IV) nerve
C) Left abducens (VI) nerve
D) Left levator palpebrae superioris
muscle
E) Left constrictor pupillae muscle
Question 31. A 68-year-old man with an
apical bronchial carcinoma is found to
have a partial right ptosis associated with a
small right pupil and reduced sweating on
the right side of the face. What name is
given to this constellation of features?
A) Cavernous sinus syndrome
B) Horner's syndrome
C) Lambert-Eaton syndrome
D) Sjögren's syndrome
E) Holmes-Adie syndrome
Question 32. Which one of the following
statements regarding Bell's palsy is false?
A) Patients may experience hyperacusis
B) Spontaneous recovery occurs in the
majority of patients
C) Treatment with prednisolone may be of
benefit
D) The ability to wrinkle the forehead is
preserved
E) Patients have difficulty closing the eye
on the affected side
Question 33. Which one of the following
is an indication for an urgent CT head scan
in a patient presenting with a suspected
stroke?
A) Previous ischaemic stroke
B) Presence of a carotid bruit
C) Clinical features of a total anterior
circulation stroke
D) Treatment with aspirin
E) Treatment with warfarin
Question 34. Which of the following
presentations is least consistent with a
diagnosis of transient ischaemic attack
(TIA)?
A) Monocular blindness
B) Facial asymmetry and slurred speech
C) Expressive dysphasia
D) Loss of consciousness
E) Left hemiparesis
Question 35. A 73-year-old man presents
with a right hemiparesis and expressive
dysphasia secondary to an infarct in the
territory of the left middle cerebral artery.
Blood pressure is 153/82 mmHg, serum
cholesterol is 4.4 mmol/l and the ECG
shows sinus rhythm with no abnormalities.
Which of the following medications is
least likely to be of benefit in preventing a
further ischaemic stroke?
A) Ramipril
B) Bendroflumethiazide
C) Aspirin
D) Warfarin
E) Simvastatin
Question 36. Which of the following
ischaemic stroke patients who have
undergone carotid duplex scanning would
be most likely to benefit from left carotid
endarterectomy?
A) Right middle cerebral artery territory
infarct with good functional recovery,
75% left carotid artery stenosis
B) Left middle cerebral artery territory
infarct with good functional recovery,
60% left carotid artery stenosis
C) Left middle cerebral artery territory
infarct with good functional recovery,
80% left carotid artery stenosis
D) Left middle cerebral artery territory
infarct with persistent dense right
hemiparesis and profound dysphasia, 90%
left carotid artery stenosis
E) Left cerebellar hemisphere infarct with
good functional recovery, 80% left carotid
artery stenosis
108
Question 37. A 43-year-old woman
attends the hospital accident and
emergency department with a 1-hour
history of sudden-onset, severe occipital
headache. On examination she is
photophobic with neck stiffness. What is
the most appropriate first-line
investigation?
A) Skull X-ray
B) CT head scan
C) CT cerebral angiography
D) Lumbar puncture
E) Carotid Doppler ultrasound (duplex)
scan
Question 38. Which one of the following
is not a risk factor for cerebral venous
thrombosis?
A) Oral contraceptive pill
B) Dehydration
C) Facial erysipelas
D) Factor V Leiden deficiency
E) Hypercholesterolaemia
Question 39. Which one of the following
statements regarding multiple sclerosis is
true?
A) The peak age of onset is between 50
and 60 years
B) It is more common in males
C) It follows a relapsing and remitting
course in the majority of patients
D) Impairment of memory is a common
presenting feature
E) The presence of oligoclonal bands of
IgG in cerebrospinal fluid is diagnostic
Question 40. Which one of the following
treatments is first-line in treating acute
relapses of multiple sclerosis?
A) Interferon beta
B) Methylprednisolone
C) IV immunoglobulin
D) Plasmapheresis
E) Azathioprine
Question 41. Which one of the following
statements about Alzheimer's disease is
true?
A) 70% of individuals over the age of 80
years are affected
B) Senile plaques and neurofibrillary
tangles are characteristic features on brain
histology
C) Impairment of long-term memory is the
earliest feature in the majority of patients
D) CT head findings are diagnostic for the
condition
E) Progression can be halted by early
treatment with anticholinesterases
Question 42. A 73-year-old man is
admitted to hospital with declining
mobility. On examination there is a resting
tremor affecting the right hand. Muscle
tone in the arms is increased. He has
difficulty when asked to fasten his buttons.
What is the most likely diagnosis?
A) Alzheimer's disease
B) Parkinson's disease
C) Huntington's disease
D) Myotonic dystrophy
E) Motor neuron disease
Question 43. Which one of the following
is not a feature of the gait of Parkinson's
disease?
A) Reduced arm swing
B) Wide-based gait
C) Impaired balance on turning
D) Slow to start walking
E) Shortened stride length
Question 44. Which one of the following
statements regarding the treatment of
Parkinson's disease is true?
A) Levodopa can be used without a
peripheral dopa-decarboxylase inhibitor in
many patients
B) Young patients with Parkinson's
disease should be commenced on levodopa
as early as possible
C) Levodopa is more effective at relieving
tremor than bradykinesia or rigidity
D) Dyskinesia secondary to levodopa can
be improved by modifying the dosing
regimen
E) Anticholinergic drugs are
contraindicated
109
Question 45. Which one of the following
drugs is most likely to cause parkinsonism
as a side-effect?
A) Amitriptyline
B) Diazepam
C) Phenytoin
D) Fluoxetine
E) Haloperidol
Question 46. Which one of the following
statements regarding Huntington's disease
is false?
A) It has autosomal recessive inheritance
B) It is due to a trinucleotide repeat
C) Successive generations are often
affected at an earlier age
D) Cognitive impairment is a frequent
finding
E) Genetic screening is available for
family members of affected individuals
Question 47. A 68-year-old man is
referred to the neurology outpatient clinic
with a 1-year history of progressive
bilateral arm and leg weakness. On
examination there is global muscle
wasting with muscle fasciculations in the
upper arms and thighs. There is
generalised muscle weakness, worse
distally and on the left. Reflexes are brisk
throughout and plantars are extensor.
Sensory examination is normal and cranial
nerves are intact. What is the most likely
diagnosis?
A) Myotonic dystrophy
B) Motor neuron disease
C) Guillain-Barré syndrome
D) Cerebrovascular disease
E) Myasthenia gravis
Question 48. A 34-year-old woman
attends the hospital accident and
emergency department with a 6-hour
history of headache, fever and neck
stiffness. On examination she has a
temperature of 39.1°C, pulse of 108 bpm,
blood pressure of 110/58 mmHg and
oxygen saturation of 98% on air. Glasgow
Coma Score is 15/15. A purpuric rash is
noted over her chest and arms. There is
evidence of neck stiffness and
photophobia but no focal neurological
deficit is identified. What would the most
appropriate initial management be?
A) Arrange a CT head scan
B) Transfer the patient to the ward and
perform a lumbar puncture
C) Administer IV benzylpenicillin
D) Administer IV acyclovir
E) Insert a central venous line
Question 49. Which one of the following
statements regarding poliomyelitis is
false?
A) The condition is caused by a viral
infection
B) Upper motor neuron signs predominate
C) Physiotherapy is useful in maintaining
mobility
D) Invasive ventilation may be required
E) An effective oral vaccine is available
Question 50. A 73-year-old man is
brought to the hospital accident and
emergency department after experiencing
a seizure. His family state that he has been
complaining of headaches and nausea for
3 months. His only past medical history is
of type 2 diabetes mellitus. A contrastenhanced CT head scan is shown below:
What is the most likely diagnosis?
A) Subdural haematoma
B) Subarachnoid haemorrhage
110
C) Cerebral abscess
D) Creutzfeldt-Jakob disease (CJD)
E) Herpes simplex encephalitis
Question 51. Which one of the following
statements regarding tetanus is true?
A) The responsible bacterium, Clostridium
tetani, infects the spinal cord and brain
B) Multiplication of the organism occurs
only in areas with good oxygenation
C) The typical initial presentation is with
headache, fever and drowsiness
D) Antibiotics are of no value in treatment
E) Tetanus antitoxin should be
administered in all suspected cases
Question 52. Which one of the following
statements regarding Creutzfeldt-Jakob
disease (CJD) is false?
A) The causative agent is a protein
B) Myoclonic jerks are a characteristic
feature
C) Cognitive function is usually preserved
D) Patients with variant CJD are typically
younger than those with sporadic CJD
E) No curative treatment is available
Question 53. Which one of the following
statements regarding intracranial
neoplasms is true?
A) The majority are primary neoplasms
B) Primary intracerebral tumours do not,
generally, metastasise outside the central
nervous system
C) CT is superior to MRI for imaging
posterior fossa tumours
D) Dexamethasone aggravates oedema
surrounding cerebral tumours
E) Gliomas have a better prognosis than
meningiomas
Question 54. Which one of the following
statements regarding acoustic neuroma is
true?
A) Conductive deafness is a common
finding
B) There is an association with tuberous
sclerosis
C) Cerebellar signs may be present
D) CT is the investigation of choice
E) Radiotherapy is the treatment of choice
Question 55. A 25-year-old woman is
referred to the neurology clinic with a 6month history of recurrent headaches. She
denies any other symptoms. Her only past
medical history is of acne, for which she
takes oxytetracycline. On examination she
has a body mass index of 34. Fundoscopy
reveals papilloedema but neurological
examination is otherwise unremarkable. A
CT head scan is normal. The cerebrospinal
fluid (CSF) opening pressure at lumbar
puncture is elevated, but CSF protein,
glucose and cell count are normal. What is
the most likely diagnosis?
A) Normal pressure hydrocephalus
B) Cerebral astrocytoma
C) Idiopathic (benign) intracranial
hypertension
D) Subarachnoid haemorrhage
E) Cerebellar abscess
Question 56. Which of the following
drugs is most likely to be effective in the
treatment of idiopathic (benign)
intracranial hypertension?
A) Furosemide
B) Bendroflumethiazide
C) Spironolactone
D) Amiloride
E) Acetazolamide
Question 57. Which one of the following
clinical features is not characteristic of
normal pressure hydrocephalus?
A) Dementia
B) Urinary incontinence
C) Headache
D) Gait apraxia
E) Higher incidence in old age
Question 58. A 45-year-old man attends
his general practitioner after developing
sudden-onset lower back pain while lifting
a sofa. He also describes pain shooting
down the back of his right leg. On
examination the straight leg raise test is
positive on the right. Sensation is reduced
over the sole and lateral border of the right
foot. Plantar flexion of the ankle is weak
on the right, and the right ankle jerk is
absent. Which nerve root is affected?
A) L3
B) L4
111
C) L5
D) S1
E) S2
Question 59. What is the most appropriate
first-line treatment for a patient presenting
with severe lower back pain secondary to
lumbar disc herniation, associated with
nerve root compression?
A) Bed rest
B) Analgesia and early mobilization
C) Steroid injection
D) Spinal radiotherapy
E) Surgical decompression
Question 60. A 76-year-old man with
metastatic prostate cancer is admitted to
hospital with lower back pain and
deteriorating mobility. He also describes a
2-day history of urinary incontinence.
Neurological examination of the lower
limbs reveals bilaterally increased tone
with weakness, brisk reflexes and extensor
plantars. No deficit is noted in the upper
limbs or cranial nerves. There is reduced
sensation below his mid-abdomen. What is
the most likely cause for the deterioration?
A) Cerebral metastases
B) Cervical cord compression
C) Thoracic cord compression
D) Cauda equina syndrome
E) Peripheral neuropathy
Question 61. Which investigation is most
likely to yield useful diagnostic
information in suspected cases of spinal
cord compression?
A) Plain X-ray of the spine
B) Spinal CT scan
C) Spinal MRI scan
D) Nerve conduction studies
E) Isotope bone scan
Question 62. Which one of the following
is least likely to cause peripheral
neuropathy?
A) Diabetes mellitus
B) Chronic alcohol excess
C) HIV infection
D) Multiple sclerosis
E) Vitamin B12 deficiency
Question 63. Which one of the following
drugs is most likely to cause peripheral
neuropathy?
A) Amiodarone
B) Furosemide
C) Haloperidol
D) Amoxicillin
E) Lansoprazole
Question 64. A 54-year-old woman
attends her general practitioner with a 2week history of tingling in her right hand.
Her symptoms often wake her from sleep.
On examination sensation is reduced over
the palmar aspect of the right thumb, index
and middle fingers and over the radial half
of the ring finger. There is weakness of
thumb abduction. Which nerve is affected?
A) Radial nerve
B) Median nerve
C) Ulnar nerve
D) Axillary nerve
E) Musculocutaneous nerve
Question 65. Which one of the following
statements about Guillain-Barré syndrome
is false?
A) The condition is often preceded by a
diarrhoeal illness
B) There is a lower motor neuron pattern
of muscle weakness
C) Lumbar puncture demonstrates
increased cerebrospinal fluid protein with
a normal white cell count
D) Respiratory muscles are not affected
E) IV immunoglobulin reduces the
duration of illness
112
Question 66. A 29-year-old woman is
referred to the medical outpatient clinic
with a 4-month history of intermittent
double vision. She also complains of
difficulty combing her hair without taking
frequent rests. Examination of the upper
limbs initially reveals normal power, but
this declines with repeated testing.
Sensation is normal. What is the most
likely diagnosis?
A) Duchenne muscular dystrophy
B) Oculopharyngeal muscular dystrophy
C) Myasthenia gravis
D) Chronic fatigue syndrome
E) Temporal arteritis
Question 67. Which one of the following
statements about myasthenia gravis is
false?
A) The condition is caused by
autoantibodies directed against
acetylcholine receptors
B) The condition may affect respiratory
muscles
C) The Tensilon test can be helpful in
making the diagnosis
D) Thymectomy may improve prognosis
in patients without thymoma
E) The presence of muscle paralysis with
fasciculation, sweating and excessive
salivation suggests a myasthenic crisis
Question 68. Which one of the following
features is characteristic of myotonic
dystrophy?
A) Autosomal recessive inheritance
B) Hirsutism
C) Delayed relaxation of skeletal muscle
D) Calf muscle hypertrophy
E) Autoantibodies directed against
presynaptic voltage-gated calcium
channels at the neuromuscular junction
Chapter
26
SKIN DISEASE
Answers page 238
Question 1. A 45-year-old gentleman
presents with well-demarcated scaly
plaques on his scalp, elbows and knees.
On examination you also notice some nail
abnormalities:
What is the diagnosis?
A) Lichen planus
B) Drug eruption
C) Chronic plaque psoriasis
D) Atopic eczema
E) Pityriasis rosea
Question 2. Which one of the following
statements regarding psoriasis is
incorrect?
A) It has a predilection for the extensor
surface of the limbs
B) It is the only skin disease to
demonstrate the Köbner phenomenon
C) The Auspitz sign may be demonstrated
by lifting a psoriatic scale
D) Nail changes include pitting and
subungual hyperkeratosis
E) Psoriatic pustules are sterile
Question 3. Which of the following
factors would be least likely to provoke a
worsening of psoriasis?
A) Beta-blockers
B) Lithium
C) Penicillin antibiotics
D) Stress
E) Antimalarial treatment
113
Question 4. Which one of the following
systemic agents is not used in the
management of psoriasis?
A) Methotrexate
B) Psoralen
C) Ciclosporin
D) Acitretin
E) Gold
Question 5. Which one of the following
statements regarding urticaria is incorrect?
A) It may be caused by physical agents
such as cold and pressure
B) Episodes often last longer than 24
hours
C) The pathophysiology involves
degranulation of mast cells
D) Antihistamines may help the condition
E) Appropriate investigations would
include total IgE and complement levels
Question 6. A 15-year-old male presents
with a rash consisting of small, scaly
salmon-pink macules of raindrop
appearance on his back. He gives a recent
history of a sore throat. You suspect a
diagnosis of guttate psoriasis. Which one
of the following organisms is most likely
to be associated with this presentation?
A) Streptococcus pyogenes
B) Trichophyton rubrum
C) Proprionobacterium acnes
D) Borrelia burgdorferi
E) Sarcoptes scabiei
Question 7. A 28-year-old woman with
type 1 diabetes mellitus presents to the
clinic with these yellow waxy-looking
plaques on her anterior shin:
What is the diagnosis?
A) Discoid eczema
B) Granuloma annulare
C) Psoriasis
D) Necrobiosis lipoidica
E) Erythema nodosum
Question 8. Which of the following
statements regarding necrobiosis lipoidica
is most accurate?
A) The condition only occurs in diabetics
B) Severity of the lesion is closely
correlated with glycaemic control
C) There is an infective component to the
pathogenesis
D) Topical or intralesional steroids may be
useful
E) The lesions very rarely ulcerate
Question 9. A 68-year-old retired labourer
presents with the following lesion on the
side of the nose:
What is the diagnosis?
A) Squamous cell carcinoma
B) Nodular melanoma
C) Cellulitis
D) Actinic keratosis
E) Basal cell carcinoma
114
Question 10. Which one of the following
statements about basal cell carcinoma is
true?
A) Deep, penetrating lesions should be
treated with cryotherapy
B) Metastatic spread to regional lymph
nodes occurs early
C) Tumour recurrence following treatment
carries a poor prognosis
D) Most lesions resolve spontaneously
E) Local invasion is more common than
haematogenous spread
Question 11. All of the following features
of a mole except one would give cause for
concern. Which is the exception?
A) Itch
B) Bleeding
C) Warty texture with 'stuck-on'
appearance
D) Recent change in shape
E) Presence of irregular pigmentation
Question 12. Which one of the following
statements regarding classification of
malignant melanoma is incorrect?
A) Lentigo maligna melanoma mainly
occurs on the exposed skin of the elderly
B) Acral lentiginous melanoma occurs on
the palms and the soles
C) Superficial spreading melanoma has a
radial growth phase
D) Amelanotic melanomas are more
common than the pigmented variety
E) The excision margins of a nodular
melanoma are dependent on its Breslow
thickness
Question 13. All of the following except
one are risk factors for development of
skin cancer. Which is the exception?
A) Dark skin and black hair
B) A strong history of sun exposure
C) A family history of melanoma
D) An outdoor occupation
E) The genetic defect, xeroderma
pigmentosum
Question 14. A 4-year-old girl is brought
to the clinic by her mother with a
distressing itchy rash on the flexor aspects
of her elbows and knees and on her face.
She has had a similar rash since early
infancy. She takes inhalers for asthma but
has not been exposed to any other
medications. On examination, you find an
erythematous papular rash in the flexures,
which is obviously excoriated and has
prominent lichenification. Which one of
the following is the most likely diagnosis?
A) Atopic eczema
B) Scabies
C) Contact dermatitis
D) Psoriasis
E) Lichen planus
Question 15. Which one of the following
would not feature in the management of a
child with atopic eczema?
A) Greasy emollients
B) Topical steroids
C) Patient education
D) Dithranol
E) Avoidance of known irritants
Question 16. Involvement of the oral
mucous membranes would be an
unexpected finding in which one of the
following disorders?
A) Systemic lupus erythematosus (SLE)
B) Pemphigus
C) Lichen planus
D) Bullous pemphigoid
E) Stevens-Johnson syndrome
Question 17. With regard to hair loss,
which one of the following statements is
incorrect?
A) Discoid lupus erythematosus causes a
non-scarring alopecia
B) Exclamation mark hairs are
pathognomonic of alopecia areata
C) Vitiligo, autoimmune thyroid disease
and trisomy 21 are all associated with
alopecia areata
D) Alopecia totalis describes complete
loss of scalp hair with preservation of
body hair
E) Androgenetic alopecia may occur in
both males and females
115
Question 18. A 19-year-old woman
presents with this erythematous, painful,
nodular eruption on the anterior aspect of
both shins:
Which of the following steps is least
appropriate in her initial work-up and
management?
A) Chest X-ray
B) Full drug history
C) Antibiotics
D) Antistreptolysin O (ASO) titre
E) Simple analgesia
Question 19. Which one of the following
statements concerning the definitions of
skin lesions is incorrect?
A) Vesicles are less than 5 mm in diameter
B) Papules are solid elevations of skin less
than 5 mm in diameter
C) Macules are usually raised
D) Telangiectasia are visibly dilated small
cutaneous vessels
E) Excoriation is the result of scratching
Question 20. Which one of the following
skin conditions is not typically itchy?
A) Lichen planus
B) Atopic eczema
C) Dermatitis herpetiformis
D) Bullous impetigo
E) Psoriasis
Question 21. Which one of the following
is not associated with photosensitivity?
A) Thiazide diuretics
B) Tetracycline antibiotics
C) Amiodarone
D) Hydroxychloroquine
E) Atenolol
Question 22. All of the following
statements regarding staphylococcal
scalded skin syndrome (SSSS) are correct
except one. Which is the exception?
A) The causative organism is
Staphylococcus aureus
B) Clinical features include fever, skin
tenderness and erythema
C) Patients are usually over the age of 18
years
D) Blisters arise from a split in the skin
below the stratum corneum
E) Intravenous antibiotics are an important
part of initial management
Question 23. Which one of the following
nail changes is matched correctly with its
associated condition?
A) Koilonychia Folate deficiency
B) Onycholysis Psoriasis
C) Leuconychia Fibrosing alveolitis
116
D) Beau's lines Lichen planus
E) Clubbing Atrial septal defec
Question 24. Which one of the following
is not a cause of porphyria cutanea tarda?
A) Alcohol excess
B) Haemochromatosis
C) Genetic defect
D) Diabetes mellitus
E) HIV
Question 25. The following are all
recognised precipitants of erythema
multiforme except one. Which is the
exception?
A) Mycoplasma infection
B) Digoxin
C) Herpes simplex infection
D) Penicillin antibiotics
E) Underlying malignancy
PART
2
ANSWERS
117
Chapter
1 GOOD PRESCRIBING
Question 1. A) It causes adverse effects
at doses close to the usual therapeutic
range
Explanation: It is easier to think of a
'narrow' therapeutic index: that is, there is
a narrow range between the dose
necessary to have an effect and the dose
necessary to cause toxicity.
Question 2. B) On average, tow sever
exacerbations will be prevented for
every 50 patients treated for 1 year with
the new inhaler.
Explanation: The NNTB expresses the
number of patients who must be treated
with a drug to obtain a single beneficial
outcome over a given time: in this case, to
prevent a severe acute asthma
exacerbation during treatment for 1 year.
A is false because some patients may
experience benefits other than the
prevention of a severe exacerbation. At
first glance it may appear that B and C are
both true. Looking at B, it is correct to say
that the effect of a drug on the first 25
patients treated should, on average, be the
same as the effect on the next 25, so if we
treat 50 patients we will prevent, on
average, two severe exacerbations.
However, C is one step too far; we cannot
infer from a trial lasting only 1 year that
the benefit will be identical in subsequent
years. In the words of the philosopher
Francis Bacon, 'The subtlety of nature is
many times greater than the subtlety of
argument.' The only way to find out if C is
true is to do another experiment, one that
lasts for 2 years.
Question 3. E) 50
Explanation: The absolute risk of lifethreatening haemorrhage is 2% in the
placebo group (20/1000) and 4% in the
treatment group (40/1000). Thus, with
respect to life-threatening haemorrhage,
118
the absolute increase in harm in the
treatment group = 4% - 2% = 2% = 0.02.
The number needed to harm (i.e. the
number of patients that need to be treated
to produce one additional life-threatening
haemorrhage) is the inverse of this: 1/0.02
= 50
Question 4. A) Taking this drug for 5
years will reduce your chance of a heart
attack by 15%
Explanation: The only true statement is
A. Relative risk (RR) for a given outcome
is calculated as: risk with treatment/risk
without treatment. The principles
underlying the absolute and relative risk
reductions and the number needed to treat
are explained in the link below.
Question 5. E) The dose-response curve
for Potentol lies to the left of the curve
for Weakol
Explanation: The potency of a drug is
merely a description of how much of it is
required to have a given effect. Thus, the
more potent drug will have the same effect
at smaller doses, but the maximum effects
and adverse effects of the two drugs could
be the same. A more potent drug gives a
response at a lower dose; therefore the
dose-response curve is shifted to the left.
Question 6. C) Digoxin
Explanation: Digoxin is extensively
excreted via the kidneys and has a narrow
therapeutic index, so severe toxicity can
occur at usual doses in a patient with renal
impairment. Paracetamol and simvastatin
are relatively safe in renal insufficiency.
Larger doses of furosemide are often
required to achieve an adequate diuresis in
renal insufficiency, although clearly
furosemide and other diuretics should be
avoided altogether if the cause of renal
impairment is hypovolaemia.
Question 7. D) Allopurinol and
azathioprine
Explanation: Allopurinol inhibits
xanthine oxidase, preventing the
breakdown of a metabolite of azathioprine,
mercaptopurine. This leads to an effective
overdose of azathioprine, which can cause
bone marrow suppression, resulting in
neutropenia and potentially catastrophic
immune compromise. The dose of
azathioprine should be reduced by 75% if
allopurinol is co-prescribed. Paracetamol
500 mg plus dihydrocodeine 10 mg (codydramol) is available in a combined
formulation. Digoxin and warfarin are
commonly prescribed together in atrial
fibrillation. Trimethoprim plus
sulfamethoxazole are used in combination
(as co-trimoxazole) in the treatment of
Pneumocystis carinii (jirovecii)
pneumonia. Some calcium channel
blockers increase ciclosporin blood
concentrations, but there is no interaction
of ciclosporin with ß- blockers
119
Question 8. B) The route of
administration of the drug
Explanation: The essential elements of a
drug prescription outside hospital can be
found in the link below.
Question 9. A) Patient's date of birth
Explanation: All of the other components
are essential legal requirements for
prescriptions for controlled drugs
Question 10. B) Amiodarone
Explanation: A loading dose of
amiodarone achieves a more rapid effect.
Question 11. D) 0.5
Explanation: Relative risk (RR) for a
given outcome is calculated as: risk with
treatment divided by risk without
treatment = 20/40 = 0.5.
Chapter
2
MOLECULAR
MECHANISMS OF
DISEASE
Question 1. D) Neutrophils
Explanation: The DNA in most human
cells is packaged into 22 pairs of
autosomal chromosomes, and one pair of
sex chromosomes (XX in females and XY
in males), giving a total of 46. Exceptions
are gametes (sperm and ova) which have
23 chromosomes, red blood cells which
are anucleate, and platelets which are
formed by cell fragmentation and contain
no DNA.
Question 2. B) Formation of messenger
RNA from DNA by RNA polymerase
Explanation: A gene is a region of DNA
which encodes a specific protein.
Transcription refers to the creation of
RNA from cellular DNA; translation is the
synthesis of protein from RNA.
Question 3. C) Chloride transport
through channels on the cell membrane
Explanation: Cystic fibrosis is an
autosomal recessive condition which
predominantly affects the lungs but also
has consequences in the pancreas, gut and
male reproductive system. Mutation of the
CFTR gene results in defective chloride
transport through channels in the cell
membrane. In the lungs, this leads to the
accumulation of thick respiratory
secretions and superadded infection.
Question 4. C) Noradrenaline
(norepinephrine)
Explanation: Steroids (e.g.
glucocorticoids, mineralocorticoids, sex
steroids), thyroid hormones, and vitamins
A and D mediate their effect by binding to
intracellular receptors. The activated
receptors act as transcription factors and
regulate gene expression. Catecholamines
(e.g. adrenaline/epinephrine and
noradrenaline/norepinephrine) do not
120
influence gene expression but rather bind
to G-protein-linked receptors on the cell
surface, and transmit their signal via
second messenger systems.
Question 5. C) The cell membrane
remains intact
Explanation: Apoptosis refers to
programmed cell death in which cells
undergo 'suicide'. The process is critical
for cell turnover and tissue remodelling,
and occurs from embryogenesis through to
old age. It is mediated by the activation of
specific genes. The cell membrane
remains intact despite cell death; toxic
cellular enzymes are therefore not
released, in contrast to necrosis, and there
is no inflammatory response. The
apoptotic cell is removed by phagocytosis.
Cell death in any ischaemic process such
as myocardial infarction involves necrosis
rather than apoptosis.
Question 6.C) 50%
Explanation: Huntington's chorea is an
autosomal dominant disorder and so only
one abnormal copy of the gene is required
to cause the disease. Children with one
affected parent therefore have a 50%
chance of inheriting the abnormal gene
from that parent. Non-identical (dizygotic)
twins are formed by the fusion of two
separate sperm with two separate ova;
genes are acquired independently from
both parents and the risk of disease is 50%
for each child. Identical (monozygotic)
twins have the same genetic composition,
and so if one twin has inherited the
abnormal gene then so must the other.
This highlights the importance of family
counselling before genetic testing.
Question 7. D) Haemochromatosis autosomal dominant
Explanation: Haemochromatosis is a
disorder characterised by iron overload
and is inherited as an autosomal recessive
trait. It is caused by mutation in the HFE
gene, and the carrier frequency of the
abnormal gene in the general population is
10%. Clinical expression usually occurs
earlier in males than in females, as
menstrual blood losses protect against iron
overload.
Question 8. E) Trisomy 21
Explanation: Clinical features of Down's
syndrome include learning difficulties,
congenital heart disease, characteristic
facies and a single palmar crease.
121
Question 9.E) Familial breast/ovarian
cancer
Explanation: Familial breast and ovarian
cancer is a familial cancer syndrome with
autosomal dominant inheritance associated
with mutations in the BRCA1 or BRCA2
genes.
Question 10.B) Congenital adrenal
hyperplasia
Explanation: Congenital adrenal
hyperplasia is an autosomal recessive
disorder due to a defect in one of the
enzymes involved in steroid biosynthesis.
The most common abnormality is a
deficiency of 21-hydroxylase, resulting in
variable deficiencies of glucocorticoids
and mineralocorticoids. Adult polycystic
kidney disease has autosomal dominant
inheritance, although the rarer infantile
polycystic kidney disease is autosomal
recessive.
Question 11. D) Secondary
amenorrhoea
Explanation: Turner's syndrome (45,XO)
is a chromosomal disorder that affects
only females. Affected individuals never
menstruate (i.e. primary amenorrhoea) and
are infertile. Secondary amenorrhoea, on
the other hand, refers to the cessation of
periods in a female who has previously
menstruated. Other features of Turner's
syndrome include widely spaced nipples, a
wide carrying angle and the absence of
secondary sex characteristics.
Question 12. D) A son would be
unaffected and a daughter would have a
100% chance of being a carrier
Explanation: The abnormal gene in
haemophilia A lies on the X chromosome,
and the condition is inherited as an Xlinked recessive trait. In this example, the
prospective father has the abnormal gene
on his X chromosome, and the mother has
two normal X chromosomes. A son would
inherit the Y chromosome (not the
abnormal X chromosome) from the father,
and so could not inherit the haemophilia
gene. A daughter would inevitably inherit
the abnormal X chromosome from the
father, and a normal X chromosome from
the mother. She would therefore be a
carrier for haemophilia A. Female carriers
often exhibit no clinical features, although
slightly reduced levels of factor VIII may
result in a mild bleeding disorder.
122
Question 13. C) Penetrance
Explanation: Penetrance describes the
proportion of individuals with an abnormal
genotype who exhibit clinical disease.
Penetrance varies for different conditions,
and is often affected by the interaction of
genetic and environmental factors. Some
conditions (e.g. Huntington's disease) have
very high penetrance. Anticipation is the
development of disease at a younger age
and with greater severity in successive
generations; this phenomenon is often seen
in conditions caused by triplet repeats (e.g.
myotonic dystrophy). Genomic imprinting
refers to the development of a different
phenotype depending on whether the
abnormal gene was inherited from the
mother or father. Translocation is the
exchange of genetic material between two
different chromosomes; for instance, the
t(9,22) translocation (the Philadelphia
chromosome) is strongly associated with
chronic myeloid leukaemia. Lyonisation is
the random inactivation of one of the two
X chromosomes in the female fetus, and
explains why female carriers of X-linked
recessive conditions (e.g. haemophilia A)
can exhibit mild clinical disease if the
normal copy is inactivated in some cells.
Question 14. B) Von Hippel-Lindau
disease
Explanation: Von Hippel-Lindau disease
is a familial cancer syndrome with
autosomal dominant inheritance. It occurs
due to mutation in the VHL gene.
Chapter
3
IMMUNOLOGICAL
FACTORS IN DISEASE
Question 1. E) T lymphocytes
Explanation: The immune system is
broadly divided into innate defences and
adaptive responses. Innate defences are
non-specific, fast response systems that do
not exhibit memory; the acquired (or
adaptive) immune response is targeted
against the specific antigen, and changes
in specificity and magnitude after initial
exposure (memory). T lymphocytes are an
essential component of the acquired
immune response
Question 2. B) Neutrophils
Explanation: Neutrophils play an
important role in the initial stages of
infection, killing microorganisms directly
and non-specifically amplifying the
immune response. T and B cells form part
of the adaptive immune response which is
more specific, but slower to respond.
Question 3 A) C-reactive protein (CRP)
Explanation: C-reactive protein (CRP) is
an acute phase protein which increases
within hours of infection and falls rapidly
on resolution. Levels may increase up to
×1000 normal, making it a useful test for
monitoring treatment response.
Complement levels may rise as part of an
acute phase response, but do not exhibit
the same magnitude of response as CRP
(×2-4-fold). In addition, complement may
be consumed during infection, making it
an unreliable indicator of treatment
response. Immunoglobulin levels rise
much more slowly in response to
infection (days to weeks), making these a
less useful indicator.
123
Question 4. C) T-lymphocyte deficiency
Explanation: This is a typical
presentation of T-lymphocyte deficiency,
which can cause increased susceptibility to
viral,
fungal and mycobacterial infections. The
most common cause of T-lymphocyte
deficiency worldwide is HIV infection.
Question 5. A) Complement deficiency
Explanation: Formation of the membrane
attack complex of complement is essential
in defence against Neisseria meningitides
and other encapsulated bacteria.
Question 6. D) Cryoglobulinaemia
Explanation: The combination of joint
pain, microscopic haematuria and a
purpuric rash is suggestive of small-vessel
vasculitis. In patients with hepatitis C, this
is most commonly caused by cryoglobulin
deposition. Autoimmune
thrombocytopenia can cause a purpuric
rash but does not commonly cause
microscopic haematuria or joint pain.
More on Cryoglobulinaemia
Question 7. D) Anticardiolipin
antibodies
Explanation: Anticardiolipin antibodies
are associated with recurrent fetal loss and
arterial and venous thrombosis. Patients
with primary or secondary
antiphospholipid syndrome may have a
positive lupus anticoagulant in addition to,
or instead of anticardiolipin antibodies, but
this cannot be assessed in patients on
warfarin.
Question 8. D) Antibody deficiency
Explanation: Recurrent bacterial infection
of the upper and lower respiratory tract
with end organ damage is a common
presentation of patients with primary
antibody deficiency. Common organisms
include Haemophilus influenzae and
Streptococcus pneumoniae.
Question 9. B) Vaccination with live
attenuated vaccines
Explanation: Live vaccines should always
be avoided in immunocompromised
patients (and patients in whom immune
deficiency is suspected) because of the
risk of iatrogenic infection.
Question 10. A) Thymus
Explanation: DiGeorge syndrome is a
congenital disorder characterised by
thymic aplasia. Normally, T lymphocytes
mature in the thymus; in the absence of a
thymus, T cells fail to mature and patients
are susceptible to fungal, viral and
mycobacterial infections. Patients with
DiGeorge syndrome also have failure of
parathyroid development, but this causes
abnormal calcium metabolism and does
not lead to immune deficiency.
Question 11. B) HLA-B27
Explanation: Patients who carry HLA-B27
are 90 times more likely than other
individuals to develop ankylosing
spondylitis.
Question 12. C) ABO blood transfusion
reaction
Explanation: Type II reactions are
characterised by antibodies to cell surface
antigens. In ABO transfusion reactions,
124
anti-blood group antibodies bind to blood
group determinants on the surface of red
cells and cause cell killing.
Question 13. A) CREST syndrome
Explanation: If you have difficulty
remembering the various associations
between autoantibodies and connective
tissue disorders you are certainly not
alone! However, specific autoantibody
profiles can provide useful diagnostic
information and are favourites with
postgraduate examiners. The CREST
variant of scleroderma is associated with
anti-centromere antibodies (which can be
remembered because they both begin with
'c'). In contrast, the diffuse variant is
commonly associated with anti-Scl70.
Question 14. E) Sjögren's syndrome
Explanation: Anti-Ro/La antibodies are
associated with Sjögren's syndrome and
systemic lupus erythematosus (SLE).
Drug-induced SLE is associated with antihistone antibodies.
Question 15. B) Wegener's
granulomatosis
Explanation: Wegener's granulomatosis is
commonly associated with the presence of
a c-ANCA, and is often also associated
with antibodies to proteinase 3. ChurgStrauss syndrome is associated with pANCA.
Question 16. A) Extracellular
deposition of insoluble proteins
Explanation: The amyloidoses are
characterised by the extracellular
deposition of insoluble protein complexes.
Chapter
4
ENVIRONMENTAL AND
NUTRITIONAL FACTORS IN
DISEASE
Question 1. E) Incidence of the disease
Explanation: Incidence of a disease (often
confused with prevalence) refers to the
number of new cases occurring in the
population at risk during a defined period
of time. Prevalence is determined by both
the incidence and the duration of the
disease.
Question 2. A) 5
Explanation: The relative risk is the
incidence in the exposed population
divided by the incidence in the unexposed
population. In this case, that means 150
cases per 3000 people living in village X
versus 30 cases per 3000 people living
remote from the nuclear power plant:
(150/3000)/(30/3000) = 150/30 = 5
Question 3. D) Ulcerative colitis
Explanation: Smoking tobacco
dramatically increases the chances of
developing a large number of diseases,
including A, B, C and E. However, it has
been noted in observational studies that
smokers with ulcerative colitis appear to
have fewer flares in their disease.
Question 4. C) NRT plus behavioural
support
Explanation: NRT plus behavioural
support leads to rates of abstinence at 6
months of up to 12%. In the absence of
any intervention, the rate of success is
only of the order of 2%.
Question 5. A) The oxyhaemoglobin
dissociation curve moves to the right
Explanation: The oxyhaemoglobin curve
describes the relationship between the
amount of O2 bound to haemoglobin and
the partial pressure of oxygen. In response
to the reduction in partial pressure of
oxygen at high altitude and the resulting
fall in arterial oxygen saturation, a number
of physiological adaptations occur. These
125
develop over a few days and include
increased production of 2,3-DPG and
erythropoietin. Epo increases red cell
production while 2,3-DPG shifts the
oxyhaemoglobin curve to the right,
thereby decreasing the affinity of the
haemoglobin molecule for oxygen
(therefore oxygen is 'off-loaded' to the
tissues more readily). Hyperventilation
occurs, rather than hypoventilation,
stimulated by hypoxic drive.
Question 6.
C) High-altitude pulmonary oedema
Explanation: This is a fairly classical
description of high-altitude pulmonary
oedema (HAPE). The most important
treatments are immediate descent and
administration of oxygen.
Question 7. B) Visual loss
Explanation: Acute mountain sickness is
a common syndrome in travellers to
altitudes of > 3000 m; it comprises
headache, fatigue, anorexia, nausea and
vomiting, difficulty sleeping and
dizziness. Visual loss, as well as
behavioural change, confusion and loss of
consciousness, is more likely to be seen as
part of the rare and life-threatening
syndrome, high-altitude cerebral oedema
(HACE).
Question 8. C) Metabolic alkalosis
Explanation: Near-drowning is inevitably
characterised by hypoxaemia and a
metabolic acidosis. Acute lung injury
results from inhalation of water, leading to
a ventilation-perfusion mismatch. This
tends to resolve over 48-72 hours unless
infection supervenes. Other complications
of near-drowning include haemoptysis,
hypotension, dehydration and cardiac
arrhythmias, in addition to hypothermia.
Question 9. D) Linoleic acid
Explanation: NSP is, in its simplest
terms, the natural packaging of plant
foods. By definition, dietary fibre cannot
be digested by human enzymes. It
therefore passes into the colon, improving
transit and preventing constipation.
Linoleic acid is a polyunsaturated fatty
acid, i.e. a lipid rather than a carbohydrate.
Question 10. C) 9 kcal
Explanation: Fat is the most energy-dense
component of the human diet, providing 9
kcal/g. This compares with carbohydrate
and protein, both of which provide 5
kcal/g. Alcohol has a calorific value of 7
kcal/g.
Question 11. C) Some essential amino
acids cannot be obtained from
vegetarian diets, necessitating the use of
supplements
Explanation: While the biological value
of protein of animal origin is generally
higher than that of vegetable origin, a
suitable combination of different vegetable
sources can provide the full range of
essential amino acids with a sufficient
protein nutritive value. This is known as
the complementary value of proteins, and
is the basis on which adequate protein may
be obtained from a vegan or vegetarian
diet without the use of supplements.
Question 12. E) Feeding via a central
(subclavian or internal jugular) line
carries a higher risk of sepsis than
feeding via a percutaneous endoscopic
gastrostomy (PEG) tube
Explanation: Hospitalised patients are at
high risk of nutritional deficiency; their
requirements are often increased by
illness, and yet their capacity to consume
an adequate diet may be impaired. Many
therefore require some form of nutritional
support. Whenever possible, the enteral
route should be used as this preserves the
integrity of the mucosal barrier, reducing
the risk of bacteraemia. 'Supplement'
drinks should be used to support, not
replace, a normal diet. With parenteral
126
nutrition, hyperosmolar solutions (which
are required in those patients with high
nutritional needs) may be administered
only into central veins, as they would
cause thrombophlebitis if administered
peripherally. Although aspiration
pneumonia is a recognised complication of
feeding by nasogastric tube, feeding via a
central line carries a higher overall risk of
infection.
Question 13. B) Combined oral
contraceptive pill
Explanation: Weight gain is a wellrecognised side-effect of oestrogen
therapy. Metformin may lead to minor
weight reduction and is usually the most
appropriate first-line drug treatment for
glycaemic control in obese patients with
type 2 diabetes. Sibutramine is one of the
drug treatments available for obesity and
reduces food intake through ß1adrenoceptor and 5-hydroxytryptamine
receptor agonist activity in the central
nervous system.
Question `14. E) Obese people have a
higher basal metabolic rate than lean
people
Explanation: Obesity is defined as a BMI
> 30 (weight in kilograms divided by
height in metres squared). One of the few
'benefits' of smoking is that it protects
against obesity, although of course it has
many other adverse effects. There are a
number of potentially reversible causes of
obesity, including hypothyroidism,
Cushing's syndrome and insulinomas,
which should be considered, particularly if
the patient gives a history of having
recently begun to gain substantial weight
for the first time or at a faster rate than
previously. Although approximately 60%
of variation in BMI is attributable to
genetic factors, the genetic basis for
obesity remains poorly understood. Single
mutations in a few genes (e.g. leptin) do
cause severe childhood obesity but in the
vast majority it is a polygenic disorder.
The basal metabolic rate of obese
individuals is actually higher than that of
lean subjects.
Question 15. C) Osteoporosis
Explanation: Obesity has adverse effects
on both mortality and morbidity. However,
it protects against osteoporosis by
increasing both mechanical stress on bones
and sex steroid synthesis in adipose tissue.
Question 16. A) Bariatric gastric
surgery
Explanation: All of the interventions
above can be used in the appropriate
circumstances as part of the management
of obesity. Bariatric surgery is the most
effective in the short and long (10-year)
term, although it also has significant risks
of complications.
Question 17. D) Vitamin C
Explanation: Vitamin C is water-soluble.
This means that a large proportion of the
vitamin C content of vegetables and fruit
is lost when these foods are boiled in
water.
Question 18. B) Vitamin B2
(riboflavin) Beri-beri
Explanation: A deficiency in vitamin B1
(thiamin) causes beri-beri. This manifests
in three different forms:
• infantile, occurring in the breastfeeding
children of thiamin-deficient mothers
• dry or neurological beri-beri,
characterised by peripheral neuropathy
and wrist/foot drop
• wet beri-beri, characterised by
generalised oedema, due to congestive
cardiac failure.
Deficiency in vitamin B2, riboflavin, is
very rare because it is found in many food
types. When deficiency does occur, it
mainly affects the tongue and lips,
manifesting as glossitis, angular stomatitis
and cheilosis.
Question 19. A) Vitamin C
Explanation: Elderly people who are
socially and geographically isolated may
not have ready access to fresh fruit and
vegetables, the most abundant source of
vitamin C (ascorbic acid). This vitamin is
important in the formation of collagen;
127
when it is deficient, defective collagen
formation impairs healing of wounds,
causes capillary haemorrhage and reduces
platelet adhesiveness (normal platelets are
rich in ascorbate). This manifests
clinically as perifollicular and petechial
haemorrhages, easy bruising, swollen
gums which bleed easily, and occasionally
gastrointestinal bleeding. Ascorbic acid is
also a powerful reducing agent, which
converts the ferric form of iron found in
the diet to the more readily absorbable
ferrous form, thereby increasing body iron
absorption.
Question 20. C) Fluoride Discoloration
of teeth
Explanation: There are about 16 essential
inorganic elements in the human diet. It is
chronic excessive intake of fluoride (e.g. >
10 ppm in the water supply) that causes
discoloration of teeth, via a process known
as fluorosis. Fluoride increases the
resistance of enamel to acid attack and
protects against dental caries. A national
policy of fluoridating the water in the
Republic of Ireland was introduced in the
1950s, following which the country's
edentulous rate fell by more than 60%.
The addition of traces of fluoride (at 1
ppm) to public water supplies is now
widespread practice.
Question 21. B) Increased skinfold
thickness over the triceps
Explanation: In addition to body mass
index, a useful measurement in the
assessment of nutritional status is skinfold
thickness over the triceps; this is decreased
in malnutrition due to loss of subcutaneous
fat. This measurement can be subtracted
from mid-arm circumference to estimate
muscle mass. Many of the clinical features
of starvation represent physiological
adaptations to undernutrition. For
example, it is disadvantageous to have
children born to an undernourished mother
and into a famine environment, so
reproductive function is suppressed as part
of the physiological response to
undernutrition.
Chapter
OF
5 PRINCIPLES
INFECTIOUS DISEASE
Question 1. C) Prions are highly
complex structures consisting of > 100
different proteins
Explanation: Prions are the simplest of all
infectious agents, consisting of a single
protein molecule which can catalyse a
change in a host protein. Viruses only
contain one type of genetic material, either
DNA or RNA, and require a host cell
(either prokaryotic or eukaryotic) in order
to reproduce. Fungal cells have a defined
nucleus, in contrast to bacteria, whose
nuclear material is not organised into a
specific organelle.
Question 2. D) Hepatitis A Needlestick
injury
Explanation: In contrast to hepatitis B
and C, which are transmitted by sexual
contact, blood transfusions and needlestick
injuries, hepatitis A is spread by the
faecal-oral route.
Question 3. A) Pertussis
Explanation: All of the above apart from
pertussis are live attenuated vaccines and
should not cause infection in the
immunocompetent recipient. However,
they should be given with caution or
avoided in those who are
immunosuppressed or pregnant, or who
have an acute infection. Inactivated
vaccines include pertussis, HiB
(Haemophilus influenzae type B), and
pneumococcal. The 'awkward one' in this
classification system is poliomyelitis, for
which both a live attenuated and an
inactivated form exist. The Salk form is
inactive (remember the 'k' in Salk is also in
killed) and the Sabin form is live.
Question 4. D) MMR (measles, mumps,
rubella) vaccine
Explanation: With the exception of the
MMR vaccine, all of the above should be
128
given to children at the age of 2 months or
as soon as possible thereafter, as natural
immunity declines. MMR is given during
the second year of life. Uptake of this
vaccine has declined in recent years
following reports of a link between receipt
of the vaccine and the development of
autism. These claims are without
foundation, but have unfortunately shaken
public confidence in the vaccine.
Question 5. A) Yearly receipt of the
polyvalent flu vaccine
Explanation: Asplenic patients have
heightened susceptibility to encapsulated
organisms such as Streptococcus
pneumoniae, Neisseria meningitidis and
Haemophilus influenzae. While the flu
vaccine is not contraindicated in asplenic
patients, it provides protection against a
viral infection, and is, therefore, not
mandatory. All asplenic patients should
have prophylactic antibiotics prior to
dental procedures, as there is a risk of
disseminated infection. Daily penicillin
prophylaxis is also a standard
recommendation. All asplenic patients
should be encouraged to carry a card or
wear a MedicAlert bracelet explaining
their condition.
Question 6. E) Meningococcal
meningitis
Explanation: Certain diseases which are
thought to have important implications for
public health are classified as 'notifiable',
meaning that notification of cases to the
local public health authority is
compulsory. This is so that outbreaks of
highly contagious conditions can be
recognised, and appropriate measures put
in place to control further spread of the
condition. In the UK both meningitis (of
any cause) and meningococcal sepsis are
notifiable.
Question 7. C) Neisseria
gonorrhoeae Direct microscopy
Explanation: Strategies for identifying
micro-organisms can be broadly
categorised into direct demonstration (e.g.
microscopy with or without appropriate
staining), molecular diagnostic methods
(e.g. PCR) and immunodiagnosis (e.g.
ELISA, Western blot,
immunofluorescence). Strep. pyogenes is
most commonly identified on culture,
hepatitis B is identified initially by
immunodiagnosis, and if positive, viral
load is subsequently determined by PCR.
Gonococcus is most often identified on
microscopic examination of biological
fluid such as urine or urethral discharge
(Gram-negative diplococci); sensitivities
may subsequently be determined on
culture. Mycobacterium tuberculosis is
also identified initially by microscopy
aided by the use of Ziehl-Neelsen staining.
Candida albicans may be identified either
on direct microscopy or on culture of
biological fluids.
Question 8. C) Ciprofloxacin Inhibits
DNA gyrase, thereby blocking DNA
replication
Explanation: Knowledge of how
antibiotics work is important for
understanding their spectrum of activity
and mechanisms of resistance.
Question 9. A) Minimum inhibitory
concentration (MIC) is the lowest
concentration of an antibiotic required
to inhibit 50% of the colonies of a
particular organism
Explanation: The MIC is the lowest
concentration of an antibiotic required to
inhibit 90% of the colonies of a particular
organism.
129
Question 10. D) Prevention of gas
gangrene in a patient with a
contaminated wound Flucloxacillin
Explanation: The recommended
prophylaxis for gas gangrene is
benzylpenicillin 600 mg 6-hourly for 5
days or metronidazole 500 mg 8-hourly
for 5 days. Although chicken pox is
common in childhood and the vast
majority survive without sequelae, it is an
important cause of mortality in newborn
infants and in severely
immunocompromised patients. Both
groups should therefore receive varicella
immune globulin if they have been
exposed to the virus. The rationale behind
endocarditis prophylaxis prior to dental
procedures is that transient bacteraemia,
from organisms commensal to the mouth,
often develops following invasive dental
procedures and may colonise damaged or
artificial heart valves, leading to
endocarditis.
Question 11. C) Most patients with
established allergy to benzylpenicillin
are also allergic to cephalosporins
Explanation: Approximately 10% of
penicillin-sensitive patients are allergic to
cephalosporins, although anaphylaxis to
second- and third-generation
cephalosporins is exceedingly rare, even in
the presence of established penicillin
allergy. Beta-lactam antibiotics are
bactericidal, meaning that they kill
bacteria. They act by inhibiting synthesis
of the bacterial cell wall, which is essential
for survival of bacteria in osmotically
challenging environments.
Question 12. C) Clarithromycin
Explanation: Clarithromycin is a
macrolide antibiotic useful in the treatment
of infections caused by Gram-positive,
rickettsial, chlamydial and Mycoplasma
infections. Had Legionella, another
'atypical' organism, been identified as the
cause (best diagnosed by polymerase chain
reaction detection of the Legionella
antigen in urine), then rifampicin would be
an appropriate antibiotic to add.
Question 13. A) IV ceftriaxone and
metronidazole
Explanation: The history suggests the
possibility of an aspiration pneumonia,
and empirical antibiotic therapy must
therefore cover Gram-negative organisms
and anaerobes in addition to the usual
causes of community-acquired pneumonia.
Anti-anaerobic activity will be provided
by metronidazole while ceftriaxone, a
third-generation cephalosporin, has
excellent Gram-negative activity as well as
providing Gram-positive cover. Given the
history of recent stroke and possible
aspiration, the method of administration of
the antibiotic may be of importance, and
the IV route may be the most appropriate.
Question 14. D) Hepatotoxicity
Explanation: Aminoglycoside antibiotics
are highly nephrotoxic, an effect
potentiated by concomitant administration
of vancomycin, cisplatin, amphotericin B
or contrast media. The ototoxicity results
from the enhanced cellular penetration
demonstrated by aminoglycosides in the
hair cells in the cochlea. Hearing damage
and vertigo tend to be permanent.
Aminoglycosides impair neuromuscular
transmission and should not be given to
patients with myasthenia gravis. Larger
doses given rapidly by the IV route may
result in a transient myasthenic syndrome
in those with normal neuromuscular
function. Gastrointestinal upset is a
relatively common adverse effect but
hepatotoxicity does not occur. In order to
avoid important complications, serum
levels of the aminoglycosides must be
checked on a regular basis, and the dosing
regimen adjusted to ensure that toxic
levels are not reached.
Question 15. B) It has potent antiGram-negative properties, but little or
no anti-Gram-positive activity
Explanation: Fluoroquinolones such as
ciprofloxacin have excellent oral
bioavailability, a large volume of
distribution and good intracellular
penetration (the drug concentrates in
phagocytes, facilitating its distribution).
130
Although newer quinolones such as
moxifloxacin and levofloxacin have
enhanced anti-Gram-positive activity,
ciprofloxacin has excellent anti-Gramnegative activity with little or no antiGram-positive activity. Side-effects of this
drug are infrequent and generally mild. Its
oral bioavailability, as mentioned above, is
excellent, but is impaired by coadministration of food, antacids, ferrous
sulphates and multivitamins.
Question 16. E) They have good oral
bioavailability
Explanation: No useful oral absorption of
glycopeptide antibiotics is achieved, and
administration is always by the IV route
(except in the treatment of Clostridium
difficile diarrhoea). The anaphylactoid
reaction caused by rapid histamine release
from mast cells in response to a rapid
infusion of vancomycin is known as 'red
man' syndrome. Nephrotoxicity is another
potential side-effect, the risk of which is
greatly reduced by monitoring of antibiotic
serum levels to ensure that toxic
concentrations are not reached. No
antibiotic in this class has any significant
activity against Gram-negative organisms
but both vancomycin and teicoplanin are
useful against MRSA.
Question 17. D)
Ketoconazole Nephrotoxicity
Explanation: Ketoconazole is an oral
antifungal agent that can cause
hepatotoxicity. 'Grey baby syndrome'
describes the dose-dependent cyanosis and
circulatory collapse that occur in infants
due to inability to conjugate
chloramphenicol and excrete it in urine.
All tetracycline antibiotics bind to metallic
ions in bones and teeth, causing
discoloration, and therefore should be
avoided in children and in pregnancy.
Tetracyclines also photosensitise and
patients should be warned about this and
advised to use sun-screen. Erythromicin
causes a cholestatic jaundice in some
patients, which abates when the drug is
stopped.
Chapter
6 AGEING AND DISEASE
Question 1. D) Increased insulin
secretion
Explanation: Ageing is a normal
physiological process and effects are seen
in several organ systems. They do not
usually interfere with organ function under
normal conditions, but reserve capacity is
reduced and so organ failure can be
precipitated by minor illness. Pancreatic _cell function declines with age, resulting in
reduced insulin secretion.
Question 2, D) Omeprazole
Explanation: Falls are an extremely
common presentation in elderly patients
and are often multifactorial. Sedative
drugs (e.g. benzodiazepines,
antipsychotics, antidepressants), opiates
and diuretics are common culprits.
Polypharmacy in itself is also a risk factor.
Proton pump inhibitors are generally well
tolerated and cause relatively few sideeffects.
Question 3. E) Bisphosphonate therapy
Explanation: Elderly patients who present
with recurrent falls are often frail with
multiple medical problems. The annual
risk of falling increases linearly with the
number of risk factors, from 8% with no
risk factors to 78% with four or more. In
patients who experience recurrent falls,
osteoporosis prophylaxis with calcium and
vitamin D supplements, and treatment of
established osteoporosis with
bisphosphonates are important
considerations that may reduce the risk of
fracture.
131
Question 4. C) Stop amlodipine
Explanation: Postural hypotension (drop
in BP of > 20 mmHg systolic or > 10
mmHg diastolic on standing from supine)
is a cause of dizziness and falls, and is
often related to medication. This patient
has a documented postural BP drop, and a
trial without amlodipine (a
dihydropyridine calcium channel blocker)
would be reasonable. Neither simvastatin
nor metformin causes postural
hypotension and there is no compelling
reason to stop the drug. Fludrocortisone is
a mineralocorticoid that causes salt and
water retention, which can be used to treat
postural hypotension; however, it can
precipitate heart failure and should be used
with caution when withdrawal of
hypotensive medication fails to resolve the
problem.
Question 5. D) Alzheimer's disease
Explanation: Almost any acute illness can
present with confusion in the elderly;
examples include infections, vascular
events, metabolic derangements and drugs
(particularly opioid analgesics and
sedatives). Alzheimer's disease causes
chronic cognitive impairment rather than
acute confusion. On the other hand, acute
cerebrovascular events may occur in
vascular dementia and can cause acute
confusion.
Question 6. E) Laxatives may be helpful
Explanation: Urinary incontinence affects
15% of women and 10% of men aged over
65. It should never be considered to be due
to ageing alone and requires investigation.
Causes of incontinence include severe
constipation (treatable with laxatives) and
hypercalcaemia. Catheterisation should
not generally be considered as first-line
treatment but may be needed in refractory
cases or if there is local skin damage.
Question 7. B) 24-hour ambulatory
ECG
Explanation: The self-limiting nature of
this patient's symptoms, together with the
absence of a postural element or other
associated symptoms, suggests that
transient arrhythmias may be the cause.
Ageing is associated with an increased
incidence of sinoatrial disease.
Furthermore, this patient is on ratelimiting treatment in the form of a _blocker. A 24-hour ambulatory ECG
132
would therefore be the most useful initial
test. Echocardiography may be helpful if
there are clinical signs of valvular disease
or an abnormal ECG. CT brain scans are
useful if cerebrovascular disease or mass
lesions are suspected, but these tend not to
present with episodic lightheadedness
alone.
Question 8. C) Chronological age
Explanation: Decisions about the
appropriate level of intervention in elderly
patients depend on individual
circumstances and often require careful
thought. Multiple comorbidities, likely
tolerance of interventions, patient and
family wishes, and advance directives
('living wills') should all be borne in mind.
Many elderly people remain fit and active
into their nineties, whereas others become
severely disabled by illness in their
seventies; 'biological' age is therefore
generally more useful than 'chronological'
age in making decisions about treatment.
Chapter
CARE AND
7 CRITICAL
EMERGENCY MEDICINE
Question 1. E) 250 ml of gelofusine over
15 minutes
Explanation: The falling blood pressure,
urine output and central venous pressure,
combined with thirst and tachycardia, are
highly suggestive of hypovolaemia. The
diagnosis can be confirmed and partly
treated by giving a rapid fluid challenge
with gelofusine or saline. O-negative
blood is precious and administration is
associated with a higher complication rate,
so it should be conserved for acutely lifethreatening emergencies.
Question 2. C) Left atrial pressure
Explanation: As direct measurement of
left atrial pressure is not practical, PAWP
is used as a surrogate.
Question 3. B) Systemic arterial
pressure
Explanation: Central venous pressure
(CVP) or right atrial pressure (RAP) is
often measured in critically ill patients to
help guide intravascular fluid replacement.
Accurate interpretation of CVP values
requires a knowledge of the physiological
factors that influence it.
Central venous pressure is largely
determined by the combination of:
• intravascular volume
• venous tone
• pulmonary artery pressure (and right
ventricular function)
• intrathoracic pressure.
Systemic arterial pressure does not directly
affect right atrial pressure but may affect it
indirectly, through altering one of the
above parameters. For example, persistent
systemic hypertension may lead to left
heart failure, which in turn may lead to
increased pulmonary artery pressure,
ultimately resulting in a rise in right atrial
pressure.
133
Question 4. B) Pulmonary embolism
Explanation: Interpreting these data may
initially seem daunting. However, a logical
approach to the causes of shock leads to
the correct answer.
There are a limited number of problems
that can cause shock. We can immediately
rule out the 'distributive' causes (septic,
anaphylactic and neurogenic) because we
know that cardiac output is low. This
leaves hypovolaemic, cardiogenic and
obstructive causes. Hypovolaemia is less
likely because the CVP is high. CVP
represents right atrial pressure, whereas
PAWP represents left atrial pressure.
Cardiogenic shock tends to affect both
ventricles, so both CVP and PAWP would
be elevated. The fact that PAWP is low
and CVP is high suggests some kind of
obstruction between the right and left
ventricles. This pattern is typical of the
haemodynamic compromise caused by
massive pulmonary embolus.
If you found this question tricky, try
having a look at the link below. There is
another question on shock later in the
chapter to test your understanding.
Question 5. A) 1 ml of 1 in 1000
adrenaline
Explanation: Adrenaline (epinephrine) is
one of the few drug doses that it is
important to memorise, because there
won't be much time to check when you
need to use it. Low volumes are used for
intramuscular injections, and in true
anaphylaxis the dose is 1 mg. If it is given
intravenously, it is more likely to cause
arrhythmia, so the dose is titrated in 0.1
mg boluses by an experienced doctor.
What mass of adrenaline is in 1 ml of each
of the solutions listed? The system seems
unnecessarily complex but can be easily
understood by memorising one key fact:
that all dose strengths refer to grams per
millilitre.
Thus, 1 in 1000 is 1 gram in 1000
millilitres = 1 gram/litre = 1 mg/ml. This
is the concentrated solution for
intramuscular injection in anaphylaxis.
Likewise, 1 in 10 000 has 1 gram in 10
000 millilitres = 0.1 grams/litre = 0.1
mg/ml. This is the concentration found in
minijet syringes on cardiac arrest trolleys.
In the context of a cardiac arrest, it is
given as a 10 ml bolus. In other situations,
it is normally titrated in 1 ml boluses.
Finally, 1% means 1 gram in 100
millilitres = 10 grams/litre = 10 mg/ml.
Question 6.
B) Noradrenaline (norepinephrine)
Explanation: Noradrenaline
(norepinephrine) acts primarily in the
peripheral vasculature, causing intense
vasoconstriction, with relatively little
direct effect on the heart. Its major clinical
use is in hyperdynamic sepsis, when there
is low systemic vascular resistance and
blood pressure despite a high cardiac
output. In these circumstances
vasoconstriction is desirable to restore BP,
even at the expense of a small reduction in
cardiac output.
Dobutamine and dopexamine are
sometimes called 'ino-dilators', since they
increase cardiac contractility whilst
simultaneously causing systemic
vasodilatation. Sodium nitroprusside and
GTN are both nitric oxide donors that
cause profound systemic vasodilatation.
134
Question 7. D) Pulmonary artery wedge
pressure (PAWP) < 15 mmHg
Explanation: The four defining
characteristics of ARDS are: hypoxaemia,
bilateral infiltrates on chest X-ray, PAWP
< 15 mmHg (this rules out left ventricular
failure as the cause of the pulmonary
pathology) and decreased lung
compliance.
Question 8. A) Diamorphine overdose
Explanation: The others are all common
causes of type 1 respiratory failure in the
critically ill. Diamorphine overdose
decreases respiratory drive, which
decreases ventilation, which allows CO2 to
accumulate.
Question 9. B) Pulmonary oedema
secondary to left ventricular failure
(LVF)
Explanation: CPAP is an effective
treatment to improve oxygenation in LVF.
It does not increase ventilation (the
volume of air shifted in and out of the
lungs) so it is not a good treatment for
disorders characterised by hypoventilation,
such as COPD, narcotic drug overdose and
neuromuscular disorders. These patients
may benefit from bi-level positive airway
pressure, which does support ventilation.
Drug overdose patients are not normally
treated in this way because they are at risk
of aspiration pneumonitis, so the airway
must be protected with a cuffed
endotracheal tube.
CPAP is contraindicated in acute severe
asthma as it worsens hyperexpansion, so
decreasing ventilation, which may be fatal.
Question 10. C) Arterial bicarbonate
(HCO3-) must be lower in the second
ABG
Explanation: The first ABG shows
normal acid-base status and significant
hypoxia on air. The second ABG shows a
metabolic acidosis, and the patient is still
very hypoxic despite receiving 40% O2.
The PaO2 should have increased but it has
hardly changed at all, so pulmonary gas
exchange has probably worsened in the
second ABG.
The metabolic acidosis is easy to diagnose
without being told the HCO3-. PaCO2 has
decreased but the patient is acidaemic.
These H+ ions must have come from
somewhere but they have not come from
CO2. Thus, there must be a metabolic
acidosis.
Question 11. D) Hyponatraemia
Explanation: Hyponatraemia is
particularly likely to cause coma when its
onset is acute. The other options do not
directly obtund consciousness.
Question 12. C) Disseminated
intravascular coagulation (DIC)
Explanation: Systemic sepsis may
provoke DIC, a potentially life-threatening
coagulopathy. This characteristically
consumes fibrinogen, platelets and clotting
factors, and leaves the circulating blood
lacking in adequate clotting factors to
support normal clotting. This leads to
abnormal bleeding and prolonged APTT
and PT.
Question 13. D) Mild hyperventilation
to reduce PaCO2 to 4-4.5 kPa
Explanation: Intracranial pressure must
be prevented from rising in head injury
patients. Simple measures, such as a 30°
head-up tilt, and tight control of fluid
balance to prevent dehydration or fluid
overload, are believed to help. PEEP
should be avoided, since it reduces venous
return from the brain, potentially
increasing intracranial pressure in headinjured patients. Current evidence suggests
135
that maintaining PaCO2 at the low end of
the normal range is the best management
for control of intracranial pressure. This
causes mild cerebral vasoconstriction but
not enough to cause cerebral ischaemia.
Normal saline is used to prevent plasma
sodium falling below 140 mmol/l.
Question 14. D) Pneumonia
Explanation: Ranitidine reduces gastric
acid secretion and is used to prevent stress
ulceration. However, its use does increase
the development of ventilator-associated
pneumonia in patients on long-term
ventilation.
Question 15. C) Central venous
catheterisation
Explanation: This patient is almost
certainly going to require aggressive fluid
resuscitation. Monitoring his central
venous pressure (CVP) will help to guide
the rate of intravascular fluid replacement
and may help to reduce the risk of
precipitating pulmonary oedema.
There is no clear indication for ventilatory
support in this patient; he is sufficiently
alert to communicate his symptoms, and
his SpO2 is 96% on air. Inotropes should
not be started at this point because
adequate volume resuscitation has not
been achieved. There is no indication at
present for haemofiltration. Diuretics are
likely to be counterproductive since he
already appears to be fluid-deplete.
Question 16. B) Septic shock
Explanation: Hypovolaemia and
cardiogenic and obstructive shock are all
associated with a low cardiac output.
Shock with a high cardiac output may be
caused by sepsis, anaphylaxis, neurogenic
shock and vasodilating drugs. There is no
history of rash, bronchospasm,
angioedema or sudden circulatory
collapse, so we can rule out anaphylaxis.
Likewise, there is no history of spinal cord
injury or administration of a large dose of
a vasodilating drug.
Chapter
8
POISONING
Question 1. C) Organophosphate
insecticides
Explanation: These are the classic acute
features ('toxidrome') of organophosphate
poisoning. A full description of the
syndrome is found in the link below.
Cholinergic symptoms are a prominent
feature of organophosphate poisoning. A
popular mnemonic for cholinergic
symptoms is 'sludge':
Salivation
lacrimation
Urination
diarrhoea
gastrointestinal cramps
semesis
Question 2. D) Ensure a patent airway
Explanation: The priority in a patient
with poisoning is the same as in any
acutely unwell patient: assessment of the
airway, breathing and circulation (ABC).
Assessing the airway is usually a simple
matter of asking the patient to speak, but
requires a more detailed assessment in the
unconscious patient. If there are any signs
of compromise, a chin lift or jaw thrust
should be performed. All of the other
measures are appropriate, but ultimately
futile if the airway is not patent.
Question 3. E) Aspirin
Explanation: Aspirin is widely available
and dangerous in overdose, so it is
important to understand the key features of
the management of salicylate poisoning.
Only a few drugs are 'able' to be removed
by haemodialysis and most of them can be
remembered easily:
Question 4. B) Ethanol
Explanation: With the exception of
ethanol, all of the drugs listed bind to
activated charcoal. It is usually only of
benefit if given within an hour of
ingestion, although repeated doses can be
used for theophylline, quinine,
136
carbamazepine and dapsone poisoning.
Some drugs, particularly small molecules
and ions, are poorly adsorbed by activated
charcoal.
Question 5. D) N-acetylcysteine
Explanation: Intravenous infusion of Nacetylcysteine is the standard treatment for
paracetamol overdose in the UK.
Methionine is a suitable oral alternative.
Question 6. E) Communicate with the
mother to be certain of the timing of the
overdose and to identify possible coingestants
Explanation: Even in large doses in highrisk patients, paracetamol overdose is
often asymptomatic in the first 24 hours.
The coma, hypotension and bradycardia
cannot be explained by paracetamol alone
and the most likely explanation is
concomitant overdose of another drug
(probably opiates or benzodiazepines).
Activated charcoal is not recommended
for patients presenting more than 1 hour
after paracetamol overdose. Nacetylcysteine can cause anaphylactoid
reactions; it is effective if given in the first
10 hours after overdose, so it is safer to
wait for a paracetamol level before starting
treatment. Vitamin K has no place in the
acute management of paracetamol
overdose. In fact, giving vitamin K would
be counterproductive because the
prothrombin time is used to monitor
progress and potential need for liver
transplantation. Paracetamol levels less
than 4 hours after overdose are
uninterpretable.
Question 7. C) Ecstasy (MDMA)
Explanation: The presentation includes
the classic features of ecstasy (MDMA)
abuse. GHB causes sedation and coma,
and LSD is a hallucinogen with relatively
low intrinsic toxicity.
Question 8. B) Naloxone
Explanation: Although this presentation
may be due to an overdose of opiates or
benzodiazepines, the specific
benzodiazepine antagonist flumazenil is
rarely used, as it can precipitate seizures
and lethal cardiac arrhythmias. On the
other hand, naloxone, an opioid
antagonist, is relatively safe although,
following administration, the patient may
wake up very quickly and become agitated
or violent, especially if too much is given
too quickly. Aim to titrate to a Glasgow
coma score of 13-14.
Question 9. E) Digoxin
Explanation: This is a classic description
of digoxin toxicity, which due to
dependence on renal clearance and a
narrow therapeutic index, can occur
without intentional overdose. The
yellowing of vision is known as
xanthopsia. Verapamil overdose can cause
vomiting and bradycardia but no visual
disturbance. Quinine overdose causes
visual disturbance, deafness, and nausea
and vomiting. With large overdoses,
cardiac effects can occur, including
impaired conduction and
tachyarrhythmias. It does not cause the
classic 'reverse-tick' ECG changes seen
with digoxin toxicity. Fluoxetine is
relatively safe in overdose; the major sideeffect of selective serotonin reuptake
inhibitors (SSRIs) is gastrointestinal upset.
Question 10. D) Methanol poisoning
Explanation: There is a raised anion gap
metabolic acidosis. This indicates the
presence of large quantities of an
unmeasured anion, such as salicylate,
ketone bodies, lactate or metabolites of
methanol. So, with the exception of
ethanol, all of the options listed could
cause this acidosis. DKA is unlikely with a
normal glucose, and if CO poisoning were
137
the cause of the acidosis, the lactate would
be elevated. A raised anion gap metabolic
acidosis is a classic feature of advanced
salicylate poisoning, but methanol
poisoning is more likely in this case, as it
often causes blindness and is a common
cause of poisoning in alcoholics. Methanol
poisoning is managed by administration of
ethanol or 4-methylpyrazole (4MP), which
competitively inhibits alcohol
dehydrogenase and thus limits formation
of toxic metabolites such as formate,
which cause blindness.
Question 11. E)Glucagon
Explanation: N-acetylcysteine and
methionine both replenish hepatic
glutathione to protect the liver from the
effects of paracetamol toxicity; calcium
gluconate is used in overdose with calcium
channel blockers; naloxone is effective in
opioid overdoses. IV glucagon and
adrenaline (epinephrine) are used if
needed in overdoses with _-blockers
Question 12. A) Iron
Explanation: Desferrioxamine is a
chelating agent used in severe iron
poisoning.
Question 13. B) Diamorphine
Explanation: Opiate overdoses cause
small 'pinpoint' pupils and respiratory
depression. Overdose with tricyclic
antidepressants, alcohol, cocaine,
amphetamine or antihistamines can cause
large pupils. Benzodiazepines such as
temazepam cause respiratory depression,
but do not cause small pupils.
Question 14. E) Co-ingestion of ecstasy
(MDMA)
Explanation: Malnourishment and
anorexia deplete the liver of protective
glutathione. Alcohol, phenytoin and
several other drugs induce hepatic
enzymes that increase the rate of
conversion of paracetamol to highly toxic
metabolites
Question 15. D) Treat if the total 24hour dose was more than 150 mg/kg
Explanation: In a 'staggered overdose'
such as this, a paracetamol level is
uninterpretable and cannot reliably be used
to guide treatment. Instead, the quantity of
drug ingested per kg of body weight is
used as a guide. The patient does not
belong to a high-risk group so the dose to
determine the need for treatment will be
150 mg/kg/24 hours.
poison are ineffective and, indeed, are
potentially harmful. Other investigations
may be necessary, but should not be
prioritised ahead of antivenin
administration. For a full discussion on the
assessment and management of snake-bite
victims, see the link below.
Question 16. C) Lithium
Explanation: All of the other drugs listed
can cause severe bradycardia in overdose.
Question 18. D) Amitriptyline
Explanation: Overdose with tricyclic
antidepressants such as amitriptyline,
alcohol, cocaine, amphetamines or
antihistamines can cause large pupils.
Opiate and organophosphate overdoses
cause small pupils.
Question 17. A) Inject 0.02 ml of salinediluted antivenin subcutaneously and
observe the injection site for 10 minutes
Explanation: Anaphylactic reactions to
antivenins are common and potentially
lethal. Sadly, tourniquets and aspiration of
Question 19. A) Aspirin
Explanation: The management of
overdose with aspirin, paracetamol or iron
is determined by the blood concentration,
the time since the overdose was taken and
the clinical features.
138
Chapter
9 MEDICAL PSYCHIATRY
Question 1. A) Mania
Explanation: Characteristic features of
mania which may be apparent in the
mental state examination include
restlessness, excess energy, elated mood,
'pressure of speech' (rapid speech that is
difficult to interpret), 'flight of ideas'
(flitting rapidly between loosely related
topics) and grandiose thoughts (e.g.
patients may believe they are particularly
gifted or have special powers).
Question 2. C) Constipation
Explanation: Somatic symptoms may
dominate the clinical picture in anxiety
disorders. Diarrhoea is far more common
in anxiety than constipation, as evidenced
by the queue outside the toilets before
final medical examinations!
Question 3. E) Age under 45
Explanation: Although deliberate selfharm is more common in women than in
men and in young adults than the elderly,
completed suicide is more common in men
and those over the age of 45.
Question 4. A) Impaired cognition and
drowsiness
Explanation: Impairment of cognition
and consciousness, particularly in a
medical inpatient, would point to delirium
as the cause of these hallucinations.
Important causes to consider would
include infection, metabolic disturbance,
hypoxia, alcohol withdrawal and drug
side-effects. The nature of the
hallucinations is also of diagnostic value
as auditory hallucinations suggest a
functional psychosis such as
schizophrenia, while hallucinations in
other modalities (especially vision)
suggest an organic cause such as delirium
139
or temporal lobe epilepsy. Pressure of
speech is characteristic of mania while
a flat affect is suggestive of depressive
disorder. Delusions are a strong pointer
towards a psychotic disorder.
Question 5. C) It is rarely used due to
the high incidence of serious side-effects
Explanation: Despite its negative image
amongst the general public, ECT remains
a highly useful treatment for severe
depressive disorder, particularly when
complicated by psychosis or risk of
starvation. It is now remarkably safe, has
very few side-effects and is of proven
efficacy in severe depressive disorder.
Question 6. C) Electroconvulsive
therapy
Explanation: Electroconvulsive therapy is
reserved for the treatment of severe
depressive disorder. Psychological
treatments such as graded exposure,
cognitive behavioural therapy and
relaxation techniques have an important
role in the management of anxiety
disorders. Beta-blockers help to alleviate
the somatic symptoms of anxiety.
Benzodiazepines are effective anxiolytics
in the short term but readily lead to
dependence and so are not a long-term
treatment option. Where drug treatment is
required, an antidepressant with anxiolytic
properties such as citalopram is the
treatment of choice.
Question 7. C) Monoamine oxidase
inhibitors
Explanation: These drugs are now rarely
prescribed in the UK but it is still
important to know of this potentially
dangerous interaction.
Question 8. E) Treatment should be
continued for at least 6 months to
reduce the high risk of relapse
Explanation: Cognitive behavioural
therapy and interpersonal therapy are as
effective as antidepressants in the
treatment of mild to moderately severe
depression, although the latter are
preferred for severe depression. The
various classes of antidepressant are
equally effective and hence choice is
largely dictated by tolerability of sideeffects and toxicity in overdose. SSRIs and
newer antidepressants such as venlafaxine
cause less troublesome side-effects and are
less dangerous in overdose than tricyclics.
Although three-quarters of patients
respond to drug treatment, it commonly
takes up to 4 weeks for improvement to
occur and response within the first 2
weeks is unusual. It is vital to explain this
to patients on initiating treatment to
maximise treatment concordance.
Question 9. D) Diabetes mellitus
Explanation: Lithium is the drug of
choice for the maintenance treatment of
bipolar disorder. It has a narrow
therapeutic range, meaning there is only a
small difference between the required
therapeutic dose and the dose at which
toxicity develops. Features of lithium
toxicity include tremor, nausea, vomiting
and convulsions. Side-effects, as opposed
to toxic effects, occur even when levels
remain within the therapeutic range,
particularly with long-term treatment.
These include renal impairment,
hypothyroidism, nephrogenic diabetes
insipidus (not diabetes mellitus) and
weight gain. Lithium is highly teratogenic
and must never be prescribed in the first
term of pregnancy.
140
Question 10. B) Poverty of speech
Explanation: First-rank symptoms are
characteristic of schizophrenia and carry
high diagnostic value. Poverty of speech,
although not a first-rank symptom, is a
feature of chronic schizophrenia, along
with other 'negative symptoms' such as
blunted mood and apathy. More
information on the diagnosis of
schizophrenia can be found in the link
from the next question.
Question 11. D) Ingestion of
amphetamines within the last 24 hours
Explanation: Although the possibility of
schizophrenia should still be considered,
recent drug misuse strongly suggests an
organic psychosis, which is one of the
main differentials of schizophrenia.
Question 12. D) Driving under the
influence of alcohol
Explanation: Alcohol consumption
associated with psychological, physical
and social problems constitutes harmful
use. Alcohol dependence is a more
restricted term, the criteria for which are
shown in the link below.
Question 13. D) Wernicke's
encephalopathy
Explanation: The combination of
confusion, ataxia and nystagmus suggests
Wernicke's encephalopathy. Other eye
signs, including ophthalmoplegia and
ptosis, may also feature.
Question 14. C) High-dose intravenous
thiamin (Pabrinex)
Explanation: Wernicke-Korsakoff
syndrome is a rare but important effect of
chronic alcohol misuse caused by
deficiency of thiamin (vitamin B1). In
Wernicke's encephalopathy there is an
acute presentation with confusion, ataxia,
nystagmus and ophthalmoplegia. This
condition is reversible but without prompt
treatment it may progress to Korsakoff's
syndrome: severe and irreversible loss of
short-term memory with consequent
inability to make new memories.
Treatment of Wernicke's and prevention of
141
Korsakoff's requires the immediate
administration of high-dose thiamin,
usually in intravenous form (Pabrinex). IV
dextrose may precipitate or exacerbate
Wernicke's and must not be given before
adequate thiamin replacement in a patient
in whom the diagnosis is suspected.
Question 15. C) Self-induced vomiting
or purgation
Explanation: Recurrent bouts of binge
eating followed by vomiting, purgation or
dieting are a feature of bulimia nervosa
rather than anorexia nervosa.
Chapter
10 ONCOLOGY
Question 1. D) Human papillomavirus
and oesophageal cancer
Explanation: Human papillomaviruses 16
and 18 are associated with cervical intraepithelial neoplasia (CIN) and subsequent
cervical carcinoma, not with oesophageal
cancer. The detection of CIN by cervical
smear testing forms the basis of the UK
screening programme for cervical cancer.
Question 2. A) Early menarche
Explanation: Risk factors for breast
carcinoma include advancing age, early
menarche, late menopause, postmenopausal obesity, personal or family
history of breast malignancy, inheritance
of BRCA 1 or 2 genes, some benign breast
conditions (e.g. lobular carcinoma in situ,
atypical hyperplasia), prolonged use of
hormone replacement therapy, previous
radiotherapy for Hodgkin lymphoma and
smoking. Early full-term pregnancy
reduces the risk. Fibrocystic breast change
is a benign condition which results in
increased breast lumpiness and tenderness,
but is not associated with breast cancer. In
MEN there is an increased risk of
malignancy in endocrine glands; for
example, in MEN I, tumours affect the
pancreas, pituitary and parathyroids.
Question 4. B) Alpha-fetoprotein (AFP)
and bladder carcinoma
Explanation: Tumour markers detected in
the blood can help in the diagnosis of
certain types of cancer, but due to lack of
specificity are often more useful in
monitoring response to treatment and
identifying relapse. Alpha-fetoprotein
(AFP) may be elevated in hepatocellular
carcinoma and testicular cancers.
Question 5. B) Take blood cultures and
start broad-spectrum antibiotics
immediately
Explanation: Neutropenic sepsis (fever of
38°C for over 1 hour in a patient with a
neutrophil count < 1.0 × 109/l) is most
often a complication of chemotherapy and
is a life-threatening emergency. Urgent
treatment with appropriate broad-spectrum
IV antibiotics is essential and must not be
delayed pending results of cultures and Xrays. G-CSF can be used in selected cases
to stimulate white blood cell production,
but is not the initial treatment and should
only be given on specialist advice. If the
patient develops septic shock she may well
require invasive monitoring, but this is
unnecessary in the current context.
Question 3. B) Acanthosis nigricans
Explanation: Non-metastatic
manifestations of lung cancer include
finger clubbing, neurological problems
(e.g. Eaton-Lambert syndrome, cerebellar
signs) and excess hormone secretion
(ADH resulting in hyponatraemia, ACTH
leading to Cushing's syndrome, and
parathyroid hormone (PTH)-related
peptide causing hypercalcaemia).
Acanthosis nigricans, a velvety thickening
and pigmentation of the major flexures,
particularly the axillae, is associated with
tumours of the upper gastrointestinal tract.
Question 6. C) Spinal MRI scan
142
Explanation: The rapid onset of bilateral
upper motor neuron signs in a patient with
prostatic carcinoma is strongly suggestive
of spinal cord compression secondary to
metastatic disease and is an oncological
emergency. Other important clues in the
history and examination would be
sphincter disturbance or sensory loss.
Spinal MRI is the investigation of choice
to identify cord compression. CT is useful
to look at bony structures, but has poorer
resolution than MRI for soft tissues such
as the spinal cord and nerve roots. Nerve
conduction studies and electromyography
are used in the assessment of peripheral
neuropathies and myopathies.
Question 7 A) Intravenous saline
Explanation: Hypercalcaemia in
malignancy can occur due to metastatic
bone disease or as a non-metastatic
manifestation secondary to parathyroid
hormone (PTH)-related peptide production
by tumour cells. The resulting osmotic
diuresis often renders patients severely
dehydrated. Treatment with large volumes
of intravenous saline corrects the fluid
deficit and lowers serum calcium over a
period of hours. Bisphosphonates (e.g.
pamidronate) lower serum calcium over a
few days and can be given following
rehydration in severe cases. Forced
diuresis (using saline and furosemide) and
calcitonin are occasionally used in very ill
patients. Calcium gluconate is used in the
treatment of hypocalcaemia.
Question 8
D) Superior vena caval
obstruction
Explanation: This patient has features of
superior vena caval obstruction (SVCO),
which is usually due to malignancy (e.g.
lung cancer, lymphoma). Obstruction of
the SVC leads to facial suffusion and
143
oedema of the upper body. Veins on the
chest wall become prominent as collateral
channels open up. Treatment options for
SVCO include radiotherapy and stenting.
Question 9
B) Dexamethasone
Explanation: The CT scan shows multiple
cerebral metastases associated with
cerebral oedema; these are causing midline
shift. The steroid dexamethasone reduces
oedema and is therefore the initial
treatment of choice. Palliative
radiotherapy is often the next step, but
there is little evidence for this. Surgery in
the presence of multiple metastases and
oedema would not be appropriate. There is
little evidence to support the use of
chemotherapy.
Question 10 D) Peripheral
neuropathy
Explanation: Ionising radiation mediates
its effect by causing damage to DNA.
Tumour cells and healthy cells are both
affected, resulting in a range of adverse
effects. Neuropathies are associated with
various chemotherapeutic agents but not
typically with radiotherapy, although it
can cause a brachial plexopathy.
Question 11 E) It exerts its effect by
acting as an oestrogen receptor
antagonist
Explanation: Tamoxifen is an oestrogen
receptor antagonist and should be
considered as adjuvant therapy in all
women with breast cancer expressing
oestrogen receptors (ER); it has no role in
ER-negative breast cancer. Tamoxifen is a
hormonal treatment, not a
chemotherapeutic agent, and is therefore
not associated with bone marrow
suppression.
Chapter
CARE AND
11 PALLIATIVE
PAIN MANAGEMENT
Question 1. D) Has a better response to
non-steroidal anti-inflammatory drugs
(NSAIDs) than tricyclic antidepressants
Explanation: Neuropathic pain is
typically described as burning, stabbing or
pulsing. It often responds favourably to
tricyclic antidepressants and
anticonvulsants, but suboptimally to
opioids and NSAIDs.
Question 2. B) Liver capsule
pain Opioids
Explanation: Liver capsule pain is caused
by stretching of the capsule due to hepatic
enlargement. It is usually associated with a
tender, palpably enlarged liver. It responds
well to corticosteroids but is poorly
responsive to both NSAIDs and opioids.
Question 3. A) Replace codeine with a
strong opioid such as morphine
Explanation: The WHO analgesic ladder
dictates that analgesia should be
prescribed that is appropriate for the
severity of the pain, and increased until the
pain is controlled. For severe pain not
controlled by a combination of weak
opioid (codeine) and non-opioids
(paracetamol and NSAIDs), as in this case,
the appropriate step is to give the patient a
full trial of strong opioids in place of the
weak opioid. It is an important principle of
the ladder that patients should not move
'sideways', i.e. change from one drug to
another drug of similar potency. At each
step of the analgesic ladder adjuvant
agents (such as anticonvulsants for
neuropathic pain) should be considered.
However, the pain in this case is unlikely
to be neuropathic and a strong opioid is
definitely indicated.
144
Question 4. D) Respiratory depression is
more likely to be a problem in acute
dosing than with patients on regular
opioids
Explanation: Nausea and vomiting occur
initially but usually settle after a few days.
Dry mouth, rather than excessive
salivation, is a common side-effect.
Laxative agents are often prescribed
routinely in patients starting strong opioids
to prevent problems with constipation.
Respiratory depression can be treated with
the opioid antagonist, naloxone. Opioids
can cause dose-related sedation and
drowsiness in patients of all ages, although
elderly patients tend to be more sensitive.
Question 5. D) Change from CR
morphine to regular IR morphine at a
lower equivalent dose and also prescribe
'as required' doses of IR morphine
Explanation: The patient developed
opioid toxicity as a result of the steep
increase in her morphine dose. Whenever
the opioid requirements of a patient with
continuous pain are unclear (e.g. starting
strong opioid for the first time, inadequate
pain control or adjusting dose in light of
toxicity), the correct process is as follows:
• Prescribe IR oral morphine 4-hourly.
• In addition, prescribe an 'as required'
dose of the same strength to be given
when the patient has pain that is not
controlled by the regular prescription
(breakthrough pain).
• Review adequacy of pain control,
requirement for breakthrough analgesia
and presence of side-effects daily.
145
• Increase the regular 24-hour dose by the
sum of the breakthrough doses over the
previous 24 hours (unless there are
significant problems with side-effects).
• Only when the correct dose has been
established should the patient be converted
to a longer-acting preparation such as CR
oral morphine or a transdermal fentanyl
patch.
In the above case the patient may benefit
from switching to an alternative strong
opioid once the correct dose has been
established. It would also be important to
ensure adequate hydration and appropriate
use of adjuvant agents.
Question 6 B) Metoclopramide
Explanation: Metoclopramide is
contraindicated in the presence of colic
because of its prokinetic effect.
Chapter
12 INFECTIOUS DISEASES
Question 1. C) Unpasteurised
milk Leptospirosis
Explanation: Leptospirosis (Weil's
disease) is caused by infection with the
spirochaete, Leptospira interrogans, which
enters humans by direct contact, often
through swimming in water contaminated
with rat urine. Mosquitoes may transmit
dengue fever, filiariasis and, most
importantly, malaria. Hepatitis B may be
contracted from contaminated blood
products, unprotected sexual intercourse
and the use of intravenous drugs.
Brucellosis and salmonellosis may be
contracted through drinking unpasteurised
milk.
Question 5. D) Infants are protected for
the first 6 months of life by passive
immunity from maternal antibodies
Explanation: The incubation period in
measles is 14 days. Koplik's spots are
pathognomonic of measles but appear on
the internal buccal mucosa not the retina.
Bacterial pneumonia complicates the
disease in around 4% of cases and
accounts for many measles-related deaths,
but antibiotics should not be given unless
there is clinical evidence of superinfection
(see evidence-based medicine box in link).
Vaccination after recovery is pointless, as
survival of infection confers life-long
immunity.
Question 2. C) Giardiasis
Explanation: The flagellate protozoon,
Giardia lamblia, colonises the small
bowel, where it may cause diarrhoea,
abdominal discomfort and malabsorption.
Question 6. A) Rubella Myocarditis
Explanation: Rubella infection in early
pregnancy may lead to severe congenital
malformation but rarely causes
complications in childhood, with most
cases being subclinical. Infection with
human erythrovirus 19 (previously known
as parvovirus B19) transiently depresses
bone marrow function. This is usually
mild but, in individuals with reduced red
cell lifespan (e.g. spherocytosis), it may
lead to life-threatening anaemia.
Question 3. B) Cutaneous larva migrans
Explanation: The history and description
of the rash are classical for cutaneous larva
migrans (CLM), which is caused by the
dog hookworm, Ancylostoma caninum.
The foot is the most common site, but
lesions of CLM may also be seen on the
breasts, buttocks and elbows. Treatment
options include albendazole and
ivermectin.
Question 4. D) Tuberculosis
Explanation: Eosinophils play an
important role in combatting helminths,
phagocytosing immune complexes and
modulating type 1 hypersensitivity
reactions. Eosinophilia is therefore most
commonly seen with parasitic infections
and allergy. Tuberculosis causes a
monocytosis.
146
Question 7. C) Varicella zoster virus
Explanation: The clinical description and
rash are typical of shingles, caused by
herpes zoster. The virus remains dormant
in the dorsal root ganglion of sensory
nerves and can be reactivated at any time.
Question 8. E) It is caused by a DNA
poxvirus
Explanation: Smallpox has been
eradicated world-wide since 1980, when
WHO coordinated a successful
vaccination campaign. Since eradication,
the vaccine is no longer routinely used but
is still available. The disease has a 30%
mortality rate. In contrast to chickenpox,
the rash is worst on the face and
extremities. Smallpox has recently
returned to media prominence due to
concern over its potential as a bioterrorist
weapon.
Question 9. A) Infectious mononucleosis
Explanation: The symptoms, clinical
findings, lack of travel history and age
group all point towards a diagnosis of
infectious mononucleosis, caused by the
Epstein-Barr virus.
Question 10. D) The peak incidence of
acquisition is in the sixth decade
Explanation: The first peak in virus
acquisition is in early childhood, when it is
passed readily in communal environments
such as nurseries and school. The second
peak occurs in teenage years. In most
cases primary infection is asymptomatic,
but carriers often continue to excrete virus
for months or years. Serious consequences
of the infection usually occur in the
immunosuppressed, in whom it may cause
CMV retinitis, and in pregnant women,
when there is a 40% risk of spread to the
fetus, 10% of whom will have serious
neurological sequelae.
Question 11. D) Dengue
Explanation: Despite the apparent
compliance with chemoprophylaxis, it
would be vital to consider the diagnosis of
malaria in this and any other patient
recently returned from an endemic area
who has a fever. Such patients should have
urgent thick and thin blood films sent to
look for the Plasmodium falciparum
parasite. Nevertheless, by far the more
likely diagnosis in this scenario would be
dengue fever, considering the recent travel
history, mosquito bites and the symptoms
described. The mosquito, Aedes aegypti, is
147
the principal vector, and the incubation
period is 2-7 days, with the rash appearing
between days 3 and 5 of the symptomatic
infection. A more serious form of the
infection, dengue haemorrhagic fever, can
also occur, particularly in children in
South-east Asia.
Question 12. E) Norovirus
Explanation: Norovirus (Norwalk agent)
is the cause of many of the outbreaks of
'winter vomiting disease' that close wards
in hospitals each winter in the UK. After a
48-hour incubation period, the virus
causes a vomiting illness that lasts 2-3
days.
Question 13. C) Hepatitis
Explanation: Staph. aureus is a normal
commensal of human skin, but can cause
serious infection when it breaches this
barrier. This is particularly so if foreign
material is present: for example, in
prosthetic joints and cannulae.
Question 14. B) Staphylococcal toxic
shock syndrome
Explanation: Staphylococcal toxic shock
syndrome is a life-threatening condition
that presents with high fever, systemic
upset, a generalised erythematous
blanching rash and haemodynamic
compromise, before progressing rapidly to
multi-organ failure. It is caused by
infection with certain strains of
Staphylococcus aureus that produce a
toxin known as toxic shock syndrome
toxin 1 (TSST1). A major aetiological
factor is the use of vaginal tampons,
particularly when they are not removed in
a timely fashion, as Staph. aureus can
grow in and around the tampon with
subsequent liberation of TSST1. In the
case above, the diagnosis of
meningococcal sepsis would also have to
be considered.
Question 15. E) Haemolytic uraemic
syndrome
Explanation: Scarlet fever most often
results from uncomplicated streptococcal
pharyngitis or tonsillitis. Various
streptococcal species, including the
viridans group, may be responsible for
endocarditis. In rheumatic fever,
antibodies generated in response to
infection with certain strains of group A
streptococci cross-react with cardiac
myosin and sacrolemmal membrane
proteins, leading to inflammation in the
endocardium, myocardium and
pericardium. An immune-mediated
reaction following streptococcal infection
may also lead to glomerulonephritis but
haemolytic uraemic syndrome is a
consequence of infection with certain
strains of E. coli, most notably E. coli
O157.
Question 16. A) Pyoderma
gangrenosum
Explanation: Brucellae are intracellular
organisms that can survive within the body
for long periods of time, causing nonspecific symptoms and signs in various
organ systems. The acute phase of the
illness is marked by high swinging
temperature, rigors and lethargy. Physical
findings that are non-specific include
lymphadenopathy and splenomegaly.
Brucellosis may cause erythema nodosum
but is not associated with pyoderma
gangrenosum.
Question 17. E) Erythema chronicum
migrans
Explanation: Erythema chronicum
migrans is the rash associated with Lyme
disease, caused by infection with
spirochaetes of the genus Borrelia. The
main vector is the tick Ixodes, whose bites
transmit the disease to humans. The early
disease is localised, manifesting as a skin
reaction around the site of the tick bite.
The infection may then disseminate to
produce widespread systemic effects such
as arthralgia, meningitis, cranial nerve
palsies and peripheral neuropathy. Late
advanced disease produces arthritis,
encephalopathy and acrodermatitis
chronica atrophicans.
148
Question 18. A) 14-day course of
doxycycline
Explanation: In the absence of
contraindications, a 14-day course of
amoxicillin or a tetracycline antibiotic
such as doxycycline is indicated.
Disseminated Lyme disease may require
more prolonged therapy, with up to 30
days of treatment. Where there is
neurological involvement
(neuroborreliosis), parenteral therapy,
usually with a broad-spectrum
cephalosporin, is required for 3-4 weeks.
Question 19. D) Weil's disease
(leptospirosis
Explanation: This dramatic presentation
with fever, haemorrhages, jaundice,
purpura, renal impairment and conjuctival
hyperaemia is a classical of Weil's disease,
a spirochaetal infection caused by
leptospires. These highly motile organisms
are shed in the urine of animal hosts,
especially rats, and infection may occur
during prolonged immersion in
contaminated water. The disease is
therefore more common is freshwater
sports enthusiasts, such as this patient.
Meningococcal sepsis must be considered
in any patient presenting with fever and
purpura, but this man's age and the
presence of jaundice and hyperaemic
conjuctivae make it less likely. His age
also reduces the likelihood of infectious
mononucleosis, which does not usually
present in such dramatic fashion. Hepatitis
A may present with fever, jaundice and
raised transaminases, but would not
account for some of the other features.
Listeriosis tends to affect
immunocompromised patients and
pregnant women.
Question 20. C) Faecal-oral
Explanation: Typhoid and paratyphoid
fevers (the enteric fevers) are transmitted
by the faecal-oral route. It is important not
to confuse them with typhus, a rickettsial
infection transmitted by ticks.
Question 21. B) Refrigeration of food
products encourages the growth of heatstable enterotoxins
Explanation: Correct storage of food and
good food-handling practices limit the
incidence of staphylococcal food
poisoning. As Staph. aureus is a
commensal of human skin (and
particularly nasal passages), poor hand
hygiene among food servers and handlers
is a frequent cause of cases. Nausea and
profuse vomiting are the predominant
symptoms and are due to production of an
enterotoxin by the organism rather than
active infection. This explains the rapid
onset of symptoms, which first arise 1-6
hours after food ingestion. The enterotoxin
is also responsible for the typical rise in
neutrophil count.
Question 22. E) Entero-invasive E. coli
(EIEC) causes symptoms through
production of an enterotoxin
Explanation: EIEC causes symptoms by
direct invasion of the colonic mucosa and
presents in a very similar fashion to
Shigella dysentery. Approximately 10-15
percnt; of patients with the O157 serotype
of EHEC will develop haemolytic uraemic
syndrome, characterised by acute renal
failure, and intravascular haemolysis. It
occurs with greatest frequency in the very
young and the very old. Management may
include dialysis and/or transfusion. E. coli
is also the most common cause of
travellers' diarrhoea.
Question 23. B) Metronidazole
Explanation: A 10-day course of oral
metronidazole is first-line therapy for
established Cl. difficile infection; oral
vancomycin is used if there is no response.
Almost all antibiotics predispose to Cl.
difficile infection, particularly broadspectrum penicillins (e.g. co-amoxiclav),
second/third generation cephalosporins
(e.g. cefuroxime) and clindamycin.
149
Question 24. A) Cholera
Explanation: The bacterium, Vibrio
cholerae, causes acute watery diarrhoea.
The stool is typically 'rice water' in nature,
consisting of clear fluid with flecks of
mucus. This contrasts with the other
organisms listed, which may directly
invade the mucosa of the small bowel, or
produce cytotoxins that damage and
ulcerate the mucosa with inflammation,
producing a bloody diarrhoea.
Question 25. C) Oral rehydration
solution (ORS) contains carbohydrate,
sodium, potassium and chloride
Explanation: Replacement of fluid losses
is by far the most important aspect of the
management of acute gastroenteritis. The
average adult with 48 hours of moderate
diarrhoea will be 1-2 litres depleted.
Adequate rehydration requires
replacement of this deficit and on-going
diarrhoeal losses in addition to normal
daily fluid requirement. While intravenous
replacement may be required for those
who cannot keep up with losses by oral
intake alone (e.g. in persistent vomiting),
the vast majority of cases can be managed
with appropriate oral rehydration. ORS
contains both electrolytes and a source of
carbohydrate to allow absorption to take
place. Prolonged bouts of diarrhoea will
result in a metabolic acidosis, due to the
loss of bicarbonate-rich secretions from
the gastrointestinal tract distal to the
stomach. Infants with gastroenteritis
should definitely continue to breastfeed, as
milk is sterile and nutritious, and contains
the correct balance of electrolytes.
Question 26. B) Diphtheria
Explanation: Although diphtheria was
eradicated from the developed world in the
mid-20th century, it remains an important
source of illness in the developing world,
and recent years have seen the occurrence
of outbreaks in South-east Asia and parts
of the former USSR. The 'bull neck' and
'wash-leather' grey-green membrane
covering the tonsils are characteristic of
the acute presentation. Treatment is
threefold, including administration of
diphtheria antitoxin, antibiotics (penicillin
or erythromycin) and isolation. A
streptococcal sore throat will
characteristically look red and raw; oral
candidiasis is whitish in appearance, and
has a predilection for the tongue rather
than the tonsils; mumps usually affects a
younger age group and may cause a
swollen neck, but not the other findings;
tonsillar cancer is exceedingly rare and
does not really fit with this acute
presentation.
Question 27. D) Leprosy
Explanation: A history of skin lesions
and thickened peripheral nerves should
lead to strong suspicion of leprosy. About
70% of the world's leprosy patients live in
India, so this gentleman's ethnic origin is
also a clue.
Question 28. C) Microscopy of split skin
smears
Explanation: Although the diagnosis of
leprosy is largely clinical, based on the
presence of cardinal features, the finding
of acid-fast bacilli in split skin is
confirmatory and also useful for
monitoring response to treatment. M.
leprae still cannot be grown in vitro and
neither serology nor PCR testing for
leprosy DNA is sensitive enough for
diagnostic purposes.
Question 29. D) Rifampicin
Explanation: Rifampicin is a potent
bactericidal for Mycobacterium leprae but
should always be given in combination
with other antileprotics. Multidrug
treatment (MDT) is crucial to treatment
success because of the emergence of
resistant strains of the bacillus.
150
More than 12 million patients have now
been successfully treated with MDT.
Question 30. D) Bartonella henselae
Explanation: B. henselae causes cat
scratch disease, a common benign
condition that arises in children and young
adults following a scratch from a cat. A
vesicle or papule develops at the site of the
injury, and subsequently the patient
develops lymphadenopathy which may
last for up to 4 months after the skin lesion
has resolved. Bartonella isolates are
sensitive to ß-lactam antibiotics,
rifampicin, erythromycin and
tetracyclines. Organisms of the Bartonella
group may also cause a life-threatening
endocarditis, particularly in the homeless,
which requires intravenous antibiotics and
valve replacement.
Question 31. B) Falciparum malaria
Explanation: A history of intermittent
fevers following return from travel in an
endemic area should always arouse
suspicion of malaria, the most dangerous
form of which is falciparum malaria.
Jaundice is common due to a combination
of haemolysis and hepatic dysfunction,
anaemia develops rapidly and tender
hepatosplenomegaly is typical. Infectious
mononucleosis could potentially present
with similar features but the lack of sore
throat, lymphadenopathy or rash and the
recent travel history favour malaria. With
a corresponding history of unprotected
sexual intercourse, the timing would be
right for HIV seroconversion illness (2-6
weeks after initial infection), which may
present non-specifically with fever and
malaise but would not produce anaemia
and jaundice. The other two options are
highly unlikely.
Question 32. C) Nephrotic syndrome
Explanation: Infection with Plasmodium
malariae but not Plasmodium falciparum
may cause glomerulonephritis and
nephrotic syndrome in children. Renal
complications of falciparum malaria
include acute renal failure secondary to
acute tubular necrosis, occasionally with
Question 33. A) Thin blood film
Explanation: A thin blood film allows
identification of the species of parasite as
well as estimation of parasitic load. Full
blood and coagulation screen will
commonly reveal abnormalities but are not
diagnostic. Culture and serological tests
play no role in the diagnosis.
Question 34. B) Falciparum malaria is
still largely sensitive to quinine
Explanation: P. falciparum is now
resistant to chloroquine almost worldwide, but not to quinine which is the drug
of choice. Mefloquine, not quinine, may
occasionally cause severe neuropsychiatric
side-effects. Mefloquine or doxycycline
chemoprophylaxis should be started 1
week before travel to a malarious area and
continued for 4 weeks after. Fansidar has
resulted in deaths from both
agranulocytosis and Stevens-Johnson
syndrome and should not be used for
chemoprophylaxis.
Question 35. D) Blood tests typically
reveal thrombocytosis and neutrophilia
Explanation: Characteristically,
pancytopenia is found on full blood count,
rather than thrombocytosis and
neutrophilia.
Question 36. B) Cutaneous
leishmaniasis
Explanation: The history of the lesion,
recent travel to an endemic area and
biopsy findings of parasites in the dermis
all make cutaneous leishmaniasis (CL) by
far the most likely diagnosis. The
incubation period is typically 2-3 months.
Although all of the above are protozoal
infections, only CL gives a cutaneous
ulcer as described.
Question 37. B) Trypanosoma cruzi
Explanation: American trypanosomiasis
(Chagas disease) commonly occurs in
South and Central America, and is
transmitted to humans by contact with the
faeces of the reduviid bug. Between 10%
and 30% of cases with chronic infection
develop a cardiomyopathy characterised
by cardiac dilatation, varying degrees of
atrioventricular block, arrhythmias and
151
sudden death.
Question 38. B) Tsetse fly
Explanation: The bite of the tsetse fly is
painful and often causes local
inflammation.
Question 39. E) The most common
presenting features of acquired
toxoplasmosis are fever, photophobia
and a non-specific rash
Explanation: The most common clinical
presentation of toxoplasmosis is with
painless enlargement of lymph nodes,
particularly cervical nodes. Photophobia
and a rash do not normally feature. The
risks of transmission to the fetus are
greatest in the third trimester; however, the
overall incidence and severity of
congenital disease are greatest in the first
trimester.
Question 40. C) Clinically, the disease
manifests as diarrhoea alternating with
constipation, with the presence of blood
and mucus
Explanation: Amoebiasis is a form of
dysentery, which is spread to humans by
ingestion of cysts of E. histolytica in water
or uncooked food. Vegetative trophozoite
forms emerge from cysts in the large
bowel and invade the mucous membrane.
The incubation period ranges from 2
weeks to many years. Diagnosis is made
by direct microscopy of stools, looking for
motile trophozoites. Intestinal amoebiasis
responds rapidly to oral metronidazole.
Question 41. E) Neutrophilia
Explanation: Strongyloidiasis is a disease
caused by the nematode Strongyloides
stercoralis, which is common in the Far
East. It is characterised by a marked
eosinophilia. Allergic phenomena, such as
urticaria, wheeze and arthralgia, are often
seen in conjunction with the
gastrointestinal symptoms. Ivermectin is
the treatment of choice.
Question 42. B) Filiariasis
Explanation: Filarial worms are tissuedwelling nematodes; toxins released by the
adult worm after dissemination in the
human blood stream cause dilatation of the
lymphatic vessels, leading to lymphatic
dysfunction and the chronic limb
manifestation of elephantiasis. In the acute
phase, the presentation is as described
above, with fever, erythema and
tenderness along the course of the
inflamed lymphatic vessels and
epididymo-orchitis. The treatment of
choice is diethylcarbamazine (DEC).
Question 43. A) Vision
Explanation: Onchocerciasis, otherwise
known as river blindness, is the result of
infection by the filarial Onchocerca
volvulus, transmitted by flies of the genus
Simulium. It is endemic in sub-Saharan
Africa, where it leaves almost half a
million people with visual impairment
152
every year. Eye disease is heralded by
itching, lacrimation and conjunctival
injection. 'Snowflake' deposits are
classically seen at the edge of the cornea.
The treatment of choice is ivermectin,
which is also in widespread use as a
prophylactic agent.
Question 44. D) Urticaria
Explanation: Urticaria is a manifestation
of acute schistosomal infection.
Schistosoma haematobium
characteristically affects the urinary tract,
causing the chronic complications of
recurrent urinary tract infections, bladder
or ureteric stone formation, and
hydronephrosis. The eggs of S. mansoni
and S. japonicum are deposited in the
liver, where they may lead to portal
hypertension and consequent development
of splenomegaly, progressive ascites and
oesophageal varices.
Chapter
INFECTION AND
13 HIV
THE AIDS
Question 1. A) Single-stranded RNA
virus
Explanation: HIV is a single-stranded
RNA virus. It consists of a protein core,
surrounded by a lipid membrane which is
lined by a matrix protein studded with
glycoprotein. The virus requires a host cell
(a CD4-positive cell) in order to replicate,
and to integrate its own genetic material
into that of the host.
Question 2. C) Homosexual
transmission
Explanation: The relative importance of
the various modes of HIV transmission
shows marked geographical variation. In
northern Europe, where blood products are
routinely and scrupulously screened for
HIV and where highly active antiretroviral
therapy (HAART) and needle exchange
programmes are more readily available,
the main mode of transmission is from
men who have sex with men (MSM). In
Africa, by contrast, the most frequent
modes of transmission are heterosexual
and vertical. China and Eastern Europe
have a much greater proportion of cases in
intravenous drug-users.
Question 3. E) Receipt of infected blood
products
Explanation: Receipt of infected blood or
blood products carries a 90% risk of
transmission to the recipient. The other
transmission risks are:
• Vertical transmission 15-40%
• Intravenous drug users 0.5-1%
• Genital mucous membrane contact 0.20.5%
• Non-genital mucous membrane contact <
0.1%
153
Question 4. B) CD4 count falls, viral
load rises
Explanation: Primary infection with HIV
is symptomatic in 70-80% of cases,
presenting with symptoms suggestive of a
flu-like illness. This coincides with a surge
in the plasma HIV-RNA levels to > 1
million copies/ml, and a fall in the CD4
count to 300-400 cells/mm3.
Question 5. D) Oropharyngeal
candidiasis
Explanation: The acquired
immunodeficiency syndrome (AIDS) is
defined by the development of specified
opportunistic infections, tumours etc. (see
link below) in a patient with HIV
infection. These tend to become manifest
with varying degrees of
immunosuppression, so that there is a
correlation between the CD4 count and the
specific diseases likely to occur.
Oesophageal but not oropharyngeal
candidiasis is considered an AIDSdefining illness.
Question 6. A) Patients typically present
with profuse, bloody diarrhea
Explanation: One of the cardinal features
of Cryptosporidium infection is that the
diarrhoea is watery and cholera-like, as
opposed to bloody. When prolonged, it is
an AIDS-defining illness that occurs when
the CD4 count falls below 200 cells/mm3.
As the cysts are chlorine-resistant, all
HIV-infected patients are advised to boil
their drinking water.
Question 7. E) Toxoplasma
Explanation: Toxoplasma is a pathogen
of the nervous system, causing spaceoccupying cysts within the brain that lead
to focal neurological signs. The typical
radiological appearance is of multiple
ring-enhancing lesions on contrast CT or
MRI of brain. Toxoplasma causes
subclinical infection in the
immunocompetent individual; it occurs in
HIV-positive patients when the CD4 count
falls below 100 cells/mm3. All of the other
pathogens listed can cause chronic
diarrhoea in the immunosuppressed.
Question 8. B) A cough productive of
green sputum
Explanation: Pneumocystis carinii (now
renamed jirovecii) pneumonia is an AIDSdefining illness that affects the respiratory
tract, causing a dry cough, pyrexia, and
breathlessness disproportionate to clinical
and radiological signs. Exercise-related
desaturation is a common feature.
Diagnosis is based on cytology of induced
sputum samples or bronchoalveolar
lavage, as the organism cannot be
cultured. First-line treatment is high-dose
co-trimoxazole and steroids. Pneumocystis
infection occurs when the CD4 count falls
below 200 cells/mm3. Many patients who
are HIV-positive with CD4 counts at or
below this level will be on prophylactic
co-trimoxazole or an alternative.
Question 9. C) Deafness and blindness
are the most common complications
Explanation: Cryptococcus is identified
on microscopy of CSF that has been
stained with India ink. It is the most
common cause of meningitis in late-stage
HIV infection, and tends to occur only
once the CD4 count has fallen below 100
cells/mm3. The typical signs of meningism
are often absent, and the presenting
features may be non-specific, with
headache, fever, vomiting and mild
confusion. Deafness and blindness may
result from prolonged elevation of
intracranial pressure. Cryptococcus
neoformans is a budding encapsulated
yeast, and therefore penicillin-based
antibiotic regimens are ineffective.
154
Amphotericin given intravenously is the
treatment of choice. Once infection has
been successfully treated, fluconazole can
be given as prophylaxis until immunity
has recovered.
Question 10. D) Cytomegalovirus
(CMV) retinitis
Explanation: The symptoms given in the
history, along with the time-scale of the
visual loss and the physical findings, are
all suggestive of CMV retinitis. This is an
important disease; although the incidence
has plummeted since the introduction of
highly active antiretroviral therapy
(HAART), the infection is sightthreatening, particularly if the macula is
affected. It tends to occur when the CD4
count falls below 50 cells/mm3. Treatment
involves the initiation of antivirals for
CMV (e.g. ganciclovir, cidofovir) and
HAART, if not already instituted. Visual
loss may result if treatment is not started
promptly.
Question 11. E) Kaposi's sarcoma
Explanation: Options A-C form part of
the differential diagnosis of HIV-related
skin disease but do not fit well with this
presentation. Although HIV-associated
lymphoma may cause lymphadenopathy
and hepatosplenomegaly, it would not
account for the cutaneous appearances
described and tends to occur with lower
CD4 counts (median CD4 count at
diagnosis is 50 cells/mm3). Kaposi's
sarcoma, an AIDS-defining disease, is a
tumour that affects cutaneous, oral and
visceral sites. It may follow an indolent or
a fulminant course, with visceral
involvement often following cutaneous
disease. The pattern of disease mirrors the
CD4 count, with accelerated disease more
common in those with low CD4 counts.
Question 12. A) Cranial nerve palsies
Explanation: The neurological sideeffects of NRTIs tend to affect peripheral
rather than central nerves. All drugs in this
class act by incorporating themselves into
the host DNA, inhibiting further
lengthening of the complementary strand
to the viral RNA template. NRTIs form
one of the cornerstones of highly active
antiretroviral therapy (HAART, most
usually two NRTIs and a protease
inhibitor). Below is a list of side-effects
paired with the drug with which they are
most strongly associated:
• Pancreatitis ddI
• Anaemia Zidovudine (ZDV)
• Peripheral neuropathy d4T, ddI, ddC
• Lipoatrophy d4T, ZDV
Question 13. D) They improve the lipid
profile of most patients by lowering
total cholesterol and low-density
lipoprotein (LDL), and by raising highdensity lipoprotein (HDL)
Explanation: Protease inhibitors are
associated with a worsening of lipid
profile, causing a rise in total cholesterol
and LDL, and a fall in HDL in 30-50% of
patients. This effect, combined with the
insulin resistance also caused by PIs, leads
to an overall increased risk of ischaemic
heart disease in these patients. The other
major side-effect of PI therapy is fat
redistribution, characterised by peripheral
fat wasting (cheeks, temples, limbs and
buttocks) and central adiposity.
155
Question 14. E) Low incidence of drug
rashes
Explanation: Rash/drug eruption is a
major class-specific side-effect of
NNRTIs, up to and including
manifestations as severe as StevensJohnson syndrome. The action of this class
of drug is to inhibit the action of reverse
transcriptase by binding near to the active
enzyme site. NNRTIs have a half-life of >
24 hours, allowing for once-daily dosing.
Their incorporation into a HAART regime
involves combination with two NRTIs.
The other major disadvantage of NNRTIs
is the potential for development of crossresistance to all drugs in the class, through
a single mutational change. Other sideeffects include dizziness, vivid dreams,
insomnia, poor concentration and
depression.
Question 15. B)
Toxoplasmosis Erythromycin
Explanation: Appropriate prophylaxis for
toxoplasmosis would be co-trimoxazole.
The decision to institute prophylaxis is
generally dependent on CD4 levels, in that
prophylaxis will be started when the CD4
count falls to a level at which the patient is
deemed to have much greater
susceptibility to that particular infection.
For example, for Pneumocystis carinii
pneumonia, the indication to commence
co-trimoxazole is when the CD4 count
falls below 200 cells/mm3
Chapter
TRANSMITTED
14 SEXUALLY
INFECTIONS
Question 1. D) Trichomonas vaginalis
Explanation: There are approximately
340 million curable STIs reported on a
yearly basis to the World Health
Organization, of which 170 million cases
represent Trichomonas vaginalis.
Chlamydia is responsible for 92 million
cases, gonorrhoea for 62 million cases,
and syphilis for 12 million cases. In the
UK, the most common treatable STIs are
chlamydia and gonorrhoea. It is important
to remember that some STIs, especially
chlamydial infection, may remain silent
for many years and therefore go
undiagnosed.
Question 2. D) Gonorrhoea
Explanation: The presence of Gramnegative diplococci on a smear of urethral
exudate makes gonococcal urethritis the
most likely diagnosis; culture may
subsequently confirm the organism. Note
that if a patient has been sexually active
with two new partners in the past month,
then the likelihood of an STI is increased.
Question 3. D) Swab of the contents of a
vesicle
Explanation: The most likely diagnosis in
the above case is genital herpes, which is
diagnosed by sending swabs of vesicular
fluid or ulcers for polymerase chain
reaction examination for detection of
herpes simplex virus (HSV) DNA.
Although HSV-2 is classically associated
with anogenital herpes, HSV-1 is found in
about 50% of cases in the UK, as well as
being the most common strain found in
orolabial herpes.
156
Question 4. B) HPV 16 and 18
Explanation: HPV 16 and 18 have been
linked to neoplasia of the genital tract.
HPV 6 and 11 are the relatively benign
strains that cause anogenital warts.
Question 5. E) Chlamydial infection
Explanation: The most commonly
diagnosed curable STI in the UK is
chlamydia, with 100 000 new cases
detected each year. Chlamydia is far more
frequently diagnosed than the next most
common curable STI, gonorrhoea, with 22
000 cases reported each year. Chlamydia
is usually asymptomatic, but may cause
symptoms of pelvic inflammatory disease
such as those described above. In either
scenario, it may eventually cause damage
to the Fallopian tubes, and subsequently
infertility or ectopic pregnancy. Other rare
complications in either sex include
conjunctivitis and Reiter's syndrome.
Question 6. A) Trichomoniasis
Explanation: Motile flagellate protozoa
seen on a wet mount of vaginal material
are diagnostic of trichomoniasis. The
organism involved is Trichomonas
vaginalis, and the treatment of choice is
metronidazole.
Question 7. E) Syphilitic chancre
Explanation: A chancre is an indurated
ulcer, which is the primary lesion of
syphilis; it occurs in the first days of
symptomatic infection. It begins as a dull
red macule, which becomes papular and
eventually ulcerates. Draining lymph
nodes may also become enlarged but are
painless. The chancre is usually located on
the penis in men or on the labia in women.
Chancres may also occur on the vaginal
wall and on the cervix. In 10% of cases,
extra-genital sites such as fingers, lips,
tongue and nipple may be involved.
Secondary syphilis occurs 6-8 weeks after
the chancre, when the treponemes have
disseminated to produce multi-system
disease.
Question 8. D) Webbed neck
Explanation: Congenital syphilis is
associated with a number of stigmata,
many of which are eponymous. The
157
chances of ever encountering any of these
signs in clinical practice are infinitesimally
small but some of them do still appear in
postgraduate examinations! Webbed neck
is, of course, associated with Turner's
syndrome.
Question 9. B) Vaginal candidiasis
Explanation: The clinical picture best fits
candidiasis. Options A, C and E would be
unlikely in a woman of this age who is not
sexually active, and the history would not
fit with any of these. Although TSS could
occur in this patient, it would present in an
entirely different way. A further clue to
the diagnosis lies in the fact that the
patient is on long-term antibiotic therapy
for acne; this would, of course, predispose
her to candidal infection, as the antibiotics
disrupt the natural flora of the female
genital tract, allowing overgrowth of
pathogens such as Candida albicans.
Chapter
BIOCHEMISTRY
15 CLINICAL
AND METABOLISM
Question 1. B) 15 litres
Explanation: In a typical adult male, total
body water is around 40 litres and
constitutes around 60% of overall body
weight. The majority of this, around 25
litres, is contained within cells (the
intracellular fluid compartment). The bulk
of the remaining 15 litres (the extracellular
fluid compartment) is found within the
interstitial fluid between cells and only a
small proportion of this (3 litres)
comprises plasma.
Question 2. C) Potassium
Explanation: The dominant cation in the
intracellular fluid (ICF) compartment is
potassium while the dominant cation in the
extracellular fluid (ECF) compartment is
sodium. The major force maintaining the
difference in cation concentration between
the ICF and ECF is the activity of the
sodium-potassium pump, integral to all
cell membranes.
Question 3. B) High potassium
Explanation: Haemolysis during or after
collection of a blood sample causes
contamination of the plasma compartment
by intracellular components. As potassium
is the dominant cation within the
intracellular fluid compartment, this leads
to a spuriously high plasma potassium
concentration. In clinical practice this is
one of the most common explanations for
the finding of a high plasma potassium
concentration and it is usually prudent to
repeat the test, particularly if the result is
unexpected. True hyperkalaemia is,
however, a life-threatening emergency and
treatment should not be delayed pending
the result of a repeat sample if significant
ECG changes are present.
158
Question 4. A) Sodium
Explanation: Since the great majority of
the body's sodium content is located in the
ECF, total body sodium is a principal
determinant of ECF volume. Importantly,
when sodium balance is disturbed, any
tendency for plasma sodium concentration
to change is usually corrected by the
osmotic mechanisms controlling water
balance. Consequently, disorders in
sodium balance present chiefly as altered
ECF volume (hyper- or hypovolaemia)
rather than altered sodium concentration.
Question 5. B) 65%
Explanation: Around 65% of the filtered
sodium load is reabsorbed in the proximal
tubule, a further 25% in the thick
ascending limb of the loop of Henle and
some 6% in the early distal tubule. Sodium
handling in the late distal tubule and
collecting duct is under the influence of
aldosterone, which can increase
reabsorption over the range of 2-3% of the
filtered sodium load. A further small
component (< 1%) occurs in the medullary
collecting duct; this component is
inhibited by atrial natriuretic peptide. A
knowledge of the processes mediating
sodium reabsorption and the factors which
regulate it is essential for understanding
disturbances of extracellular fluid volume
and their management.
Question 6. C) Bradycardia
Explanation: Tachycardia, not
bradycardia, is a clinical feature of
hypovolaemia.
Question 7. D) Increased release of
atrial natriuretic peptide
Explanation: Atrial natriuretic peptide
(ANP) is one of several neurohumoral
mediators that act to inhibit sodium
reabsorption, contributing to natriuresis
(increased urinary sodium excretion)
during periods of sodium and volume
excess. Release of ANP is reduced in
response to loss of sodium and water.
Activation of the renin-angiotensinaldosterone system is the most important
neurohumoral response to salt and water
depletion.
Question 8. E) Addison's disease
Explanation: Addison's disease is a cause
of sodium and water depletion and may
present with features of profound
hypovolaemia. Note that in normal health
a number of physiological mechanisms
serve to match urinary sodium excretion
closely to sodium intake, such that excess
sodium intake does not lead to
hypervolaemia. Various disease states
may, however, impair these mechanisms
or render them counterproductive,
triggering a sequence of events that
ultimately results in sodium and water
excess (see link below). An awareness of
these events is important both for
understanding the pathophysiology of
hypervolaemia in various clinical
conditions and for providing a rational
basis for treatment.
Question 9. C) Loop of Henle
Explanation: All diuretics act by
inhibiting sodium reabsorption at some
point in the nephron. Furosemide belongs
to the potent class of 'loop diuretics' which
inhibit sodium reabsorption in the thick
ascending limb of the loop of Henle by
blocking the apical Na,K,2Cl transporter.
The link below is very useful for
understanding the mechanisms by which
different classes of diuretic achieve both
their therapeutic effects and their sideeffects.
159
Question 10. B) Hyponatraemia
Explanation: Treatment with either
thiazide or loop diuretics may produce a
wide range of metabolic abnormalities,
though these are frequently subclinical.
Both may lead to hyponatraemia through
excess sodium loss with relative retention
of water, especially in high vasopressin
(ADH) states such as congestive heart
failure. Note that the effect of loop and
thiazide diuretics on calcium excretion
differs, with the former increasing urinary
calcium excretion and the latter reducing
it. Thus a thiazide diuretic may lead to
mild hypercalcaemia, not hypocalcaemia.
Question 11. E) Diuretic therapy
Explanation: Hyponatraemia (Na < 135
mmol/l) is a common electrolyte
abnormality but it is easily misunderstood.
This is because disturbances in sodium
balance are manifest principally as
changes in ECF volume status (hypo- or
hypervolaemia) rather than changes in
plasma sodium concentration (the plasma
sodium concentration is often normal).
Abnormalities of plasma sodium
concentration are, instead, usually due to
disturbances of body water content. Thus
in all cases of hyponatraemia there is
retention of water relative to sodium and
the most useful guide to the underlying
cause is assessment of the ECF volume
status (which in turn reflects total body
sodium). In hypovolaemic hyponatraemia
(e.g. diuretic therapy, diarrhoea and
vomiting) there is a sodium deficit with a
relatively smaller water deficit; in
euvolaemic hyponatraemia (e.g. SIADH,
primary polydipsia) there is water
retention alone with no change in total
body sodium; and in hypervolaemic
hyponatraemia (e.g. congestive cardiac
failure, nephrotic syndrome) there is
sodium retention with relatively greater
water retention. Hyperlipidaemia is an
artefactual cause of apparent
hyponatraemia.
Question 12. D) Syndrome of
inappropriate ADH secretion (SIADH)
Explanation: The pointers towards a
diagnosis of SIADH in this case are:
• no features on examination of hypo- or
hypervolaemia (i.e. euvolaemic
hyponatraemia)
• urinary osmolality that is inappropriately
high for the plasma osmolality. (In the
face of a plasma osmolality of 250
mmol/kg, the urine should be maximally
dilute ( 50 mmol/kg) and should certainly
not have an osmolality greater than
plasma.)
Diabetes insipidus is a cause of
hypernatraemia rather than hyponatraemia
due to inadequate production of ADH.
Question 13. D) Fluid restriction of 11.5 litres per day
Explanation: Patients with SIADH have
normal total body sodium but an excess of
water (euvolaemic hyponatraemia). The
most appropriate treatment is therefore not
to increase sodium intake but to restrict
water intake. Demeclocycline may be a
useful second-line treatment if the rise in
plasma Na with fluid restriction is
inadequate. An important general point
regarding the management of
hyponatraemia is that the rate of correction
of the plasma Na should be determined by
the rate of onset of the hyponatraemia. An
over-rapid correction in chronic
hyponatraemia may lead to large water
shifts out of neurons and consequent
irreversible brain damage (central pontine
myelinolysis).
Question 14. B) Carbamazepine
Explanation: SIADH has many
underlying causes including tumours,
intracranial pathology, pulmonary
disorders and a variety of drugs.
Carbamazepine is a well-recognised and
common cause of drug-induced SIADH.
Question 15. D) Peaked T wave
Explanation: Hyperkalaemia is a
dangerous electrolyte abnormality
requiring prompt attention as it may lead
to ventricular arrhythmias and asystolic
cardiac arrest. Early ECG changes include
160
peaking of the T wave and flattening or
loss of the P wave. A more serious change
is broadening of the QRS complex that
often heralds an impending serious
arrhythmia. Flattened T waves, ST
depression and U waves are all changes
associated with hypokalaemia.
Question 16. C) Conn's syndrome
Explanation: The corticosteroid hormone,
aldosterone, is the most important factor in
adjusting potassium secretion to match
potassium load. It acts on the nephron to
stimulate both potassium and hydrogen ion
secretion and increase sodium
reabsorption, effectively conserving
sodium at the expense of potassium and
hydrogen. The altered potassium excretion
usually acts to maintain tight control of
plasma potassium concentration within the
narrow normal range. In Conn's syndrome
there is excess production of aldosterone
by a unilateral adrenocortical adenoma,
resulting in primary hyperaldosteronism.
This leads to hypertension through excess
sodium and water retention, usually
accompanied by hypokalaemia through
excessive potassium secretion, and
metabolic alkalosis. All of the other
options would be more likely to result in
hyperkalaemia.
Question 17. C) Ramipril
Explanation: ACE inhibitors such as
ramipril inhibit the conversion of
angiotensin I to angiotensin II. One of the
effects of angiotensin II is to stimulate
aldosterone production in the zona
glomerulosa of the adrenal cortex. The
major function of aldosterone is to
promote reabsorption of sodium in the late
distal tubule and collecting ducts of the
kidney at the expense of potassium and
hydrogen. Thus a reduction in aldosterone
activity will lead to decreased potassium
secretion and decreased sodium
reabsorption, explaining why ACE
inhibitors (and aldosterone antagonists
such as spironolactone) may lead to
hyperkalaemia and reduced body sodium.
Question 18. E) Calcium gluconate
Explanation: All of the above treatments
have a role in the management of
hyperkalaemia but calcium gluconate is
used to stabilise myocardial conductive
tissue membranes in severe hyperkalaemia
(usually only in the presence of significant
ECG changes) and not to lower plasma
potassium concentration. Inhaled _2
agonists (e.g. salbutamol) and intravenous
glucose and insulin (e.g. 50 ml of 50%
dextrose with 5 units Actrapid) act by
shifting potassium into cells, whereas
dialysis and calcium resonium remove
potassium from the body. All medical
students and junior doctors should be
familiar with the management of
hyperkalaemia, as severe hyperkalaemia is
a life-threatening but reversible medical
emergency.
Question 19. E) Renal tubular acidosis
Explanation: The anion gap is the
difference between the main measured
cations (Na and K) and anions (Cl and
HCO3) in plasma. It is composed mainly
of phosphate, sulphate and negative
charges on plasma proteins. The normal
value of the anion gap is around 15
mmol/l.
Renal tubular acidosis and diarrhoea are
the two most common causes of a normal
anion gap acidosis. Sepsis may lead to
tissue hypoxia and a consequent lactic
acidosis; salicylate poisoning typically
produces an initial respiratory alkalosis
followed by a raised anion gap metabolic
acidosis. Both diabetic ketoacidosis and
starvation ketosis result in accumulation of
acidic ketone bodies.
161
Question 20. C) Metabolic alkalosis
Explanation: More on Patterns of acidbase disturbance
Question 21. A) Gastric outlet
obstruction
Explanation: The patient has a
hypochloraemic, hypokalaemic metabolic
alkalosis with paradoxically acidic urine.
This fairly classical pattern of biochemical
disturbance is seen with persistent severe
vomiting, as might occur with gastric
outlet obstruction. The factors that
contribute are explained in detail in the
link below. Essentially, large quantities of
sodium, chloride, potassium and hydrogen
ions, as well as water, are lost in the
vomit. The overriding response of the
kidney is salt and water conservation,
principally through increased aldosterone
release. This maintains the alkalosis and
hypokalaemia, as sodium is conserved at
the expense of hydrogen and potassium
ions. Thus the most effective method of
correcting the alkalosis is intravenous
sodium chloride (with potassium
supplementation) to interrupt the volumeconserving mechanisms and allow the
kidney to excrete excess alkali in the
urine.
Question 22. E) High-density
lipoprotein
Explanation: Reverse cholesterol
transport refers to the transfer of
cholesterol from cholesterol-laden cells to
the liver (for excretion) and cholesterolrequiring tissues. This protects peripheral
tissues (including blood vessel walls) from
excessive cholesterol accumulation. Highdensity lipoprotein (HDL) is primarily
responsible for reverse cholesterol
transport and low levels of HDL
cholesterol are associated with increased
risk of atherosclerosis.
Question 23. C) Eruptive xanthomas
Explanation: Xanthelasma and corneal
arcus are fairly non-specific signs of
hyperlipidaemia seen in a variety of lipid
disturbances and the elderly. On the other
hand, xanthomas of the Achilles or
extensor digitorum tendons are highly
suggestive of familial
hypercholesterolaemia (moderate to severe
hypercholesterolaemia resulting from an
autosomal dominantly inherited mutation
of the LDL receptor gene). Although a
correlation exists between
hypertriglyceridaemia and risk of coronary
heart disease, hypercholesterolaemia is a
far more important risk factor and more
closely associated with the development of
cardiovascular disease. Eruptive
xanthomas, as well as lipaemia retinalis
and hepatosplenomegaly, may be found in
severe hypertriglyceridaemia.
Question 24. C) They inhibit
endogenous cholesterol synthesis
Explanation: The primary action of
statins is to inhibit endogenous synthesis
of cholesterol in the liver. This leads to upregulation of the LDL receptor and hence
increased clearance of LDL cholesterol
from the circulation. The incidence of
rhabdomyolysis is very low, less than 1%.
162
Studies have demonstrated significant
reduction in stroke as well as coronary
heart disease. The lipid response includes
a mild increase in HDL cholesterol, whilst
the decrease in triglyceride is usually less
than that in LDL.
Question 25. B) Bullae on sun-exposed
areas of skin
Explanation: The porphyrias are
disorders of the haem biosynthetic
pathway that can be broadly divided into
two categories according to pattern of
presentation:
• Non-acute or cutaneous porphyrias (e.g.
porphyria cutanea tarda) are characterised
by photosensitive skin manifestations that
occur due to excess production and
accumulation of porphyrins in the skin.
• Acute or neurovisceral porphyrias (e.g.
acute intermittent porphyria) present with
acute episodes of abdominal pain and
features of autonomic dysfunction (e.g.
hypertension, tachycardia, constipation),
often in conjunction with neuropsychiatric
manifestations and/or acute neuropathy
(usually motor). There are no skin
manifestations in acute intermittent
porphyria.
Chapter
AND URINARY
16 KIDNEY
TRACT DISEASE
Question 1. E) Renal artery stenosis
Explanation: A bruit over one of the renal
arteries may raise suspicion of renal artery
stenosis, though it is neither a sensitive nor
a specific sign. Other situations in which
the diagnosis may be suspected include
significant deterioration of renal function
after starting an angiotensin-converting
enzyme (ACE) inhibitor or the finding of
significant renal impairment in a patient
with widespread vascular disease
elsewhere.
Question 2. C) Diabetic nephropathy
Explanation: Diabetic nephropathy is not
a cause of enlarged kidneys but is one of
the most common causes of chronic renal
failure, often with small shrunken kidneys.
Question 3. D) 500 ml
Explanation: The minimum urine volume
required to remove the daily solute load in
maximally concentrated urine is 300-500
ml. Higher volumes are clearly preferable
in health.
Question 4. C) Malnutrition
Explanation: Urea is excreted by the
kidneys, so levels rise following a
reduction in GFR. However, serum urea
concentration is an imperfect guide to
renal function since it is also influenced by
several other parameters. As urea is a byproduct of protein catabolism, its
production and serum levels are increased
by high-protein diets or catabolic states.
Upper gastrointestinal haemorrhage is
effectively a large protein meal while
malnutrition is a cause of low protein
intake. Urea is also reabsorbed, to a
variable extent, in the renal tubules;
dehydration increases the proportion of
filtered urea that is reabsorbed and
therefore causes a rise in blood levels
163
independent of production or GFR.
Question 5. A) Negative exponential
Explanation: The importance of
understanding this relationship is clear
from the graph in the link below. A large
fall in GFR may occur before serum
creatinine is elevated outside the normal
range.
Question 6. B) Glucose
Explanation: Glucose is freely filtered at
the glomerulus and reabsorbed actively in
the proximal tubules. Glycosuria results
when the capacity of proximal
reabsorption is saturated, because of either
high serum glucose or low reabsorption
capacity (low renal threshold). Large
proteins such as albumin and fibrinogen,
as well as cells, are not normally filtered.
Question 7. E) Post-streptococcal
glomerulonephritis
Explanation: Red cell casts are
characteristic of glomerular bleeding (the
casts are formed in the renal tubules) and a
common finding in cases of poststreptococcal glomerulonephritis. The
other options listed cause bleeding from
lower down in the urinary tract and do not
lead to the formation of casts.
Question 8. B) Reduced muscle bulk
Explanation: Creatinine is freely filtered
in glomeruli and not reabsorbed in tubules,
so that serum creatinine is an index of
glomerular filtration rate (GFR). Under
normal circumstances, creatinine is
released from muscle at a fairly constant
rate, so the greater a patient's muscle bulk,
the more creatinine he or she will produce.
Changes in serum creatinine levels are
therefore a better guide to renal function
than a single one-off value. It is important
to note that patients with significant renal
impairment may well have a serum
creatinine within the normal range,
particularly if frail or malnourished.
Because urea is a by-product of hepatic
protein metabolism, liver failure, protein
catabolism and dietary protein intake have
a much bigger effect on urea concentration
than creatinine. A significant upper
gastrointestinal bleed is equivalent to a
large protein meal and will likewise lead
to increased urea production.
Question 9. A) Detection of urothelial
malignancy
Explanation: Renal ultrasound has
superseded IVU for many purposes and is
usually the first-line investigation for renal
imaging. However, IVU provides
excellent definition of the collecting
system and ureters and remains superior to
ultrasound for detecting stones and
urothelial tumours.
Question 10. D) Dimercaptosuccinic
acid (DMSA) isotope renogram
Explanation: DMSA scans allow
quantification of each kidney's relative
contribution to renal function and can
detect the presence of scarring. In general,
the other investigations listed yield little
functional information regarding the
kidneys.
Question 11. B) Kidneys < 60% normal
size
Explanation: Small shrunken kidneys are
difficult to biopsy and usually indicate
irreversible chronic renal disease.
Consequently, complications are more
frequent and results rarely helpful. Far
164
from being a contraindication, acute renal
failure is one of the most common
indications for renal biopsy. Haematuria
may also be an indication, especially if
associated with proteinuria or renal
impairment. Antiplatelet drugs (aspirin
etc.) and anticoagulants, but not ACE
inhibitors, should be omitted for elective
biopsies; indeed, uncontrolled
hypertension is a contraindication to
biopsy.
Question 12. A) Escherichia coli
Explanation: E. coli is by far the most
common cause of community-acquired
UTI. The other options listed occur with
greater frequency in the hospital setting,
although E. coli remains the most
prevalent.
Question 13. E) Rhabdomyolysis
Explanation: All of the options listed
could conceivably account for
deteriorating renal function accompanied
by dipstick-positive haematuria, but the
absence of red cells on microscopy is
characteristic of myoglobinuria occurring
as a consequence of rapid muscle
breakdown. This patient is at risk of
rhabdomyolysis from having lain on the
floor for 24 hours.
Question 14. C) Cystoscopy and renal
ultrasound
Explanation: The priority in persistent
haematuria is to exclude an anatomical
bleeding lesion. This is particularly
important in older patients who are at
greater risk of malignancy. IVU may be
considered if cystoscopy and ultrasound
fail to reveal a cause, as it provides
detailed imaging of the ureters. It would
be unusual for prostate cancer or urinary
tuberculosis to present with isolated
macroscopic haematuria as the only
symptom. Similarly, the absence of
additional symptoms, lack of proteinuria
and presence of normal renal function do
not provide evidence of inflammatory
renal disease or an indication for renal
biopsy.
Question 15. E) Microalbuminuria
Explanation: Microalbuminuria is usually
the earliest sign of renal dysfunction in
diabetes mellitus and is associated with an
increased risk of cardiovascular events in
people without diabetes. It is not detected
on standard urine dipstick tests and must
therefore be specifically screened for in
diabetic patients using ultra-sensitive
sticks and/or through formal measurement
of the urinary albumin:creatinine ratio.
Question 16. E) Focal segmental
glomerulosclerosis
Explanation: This is a very high level of
proteinuria. More than 3 g/24 hrs is in the
'nephrotic' range and is invariably caused
by glomerular disease. Focal segmental
glomerulosclerosis is a relatively common
cause of nephrotic syndrome; the other
disorders listed affect the urinary tract
distal to the glomerulus.
Question 17. E) Hypercholesterolaemia
Explanation: Nephrotic syndrome
describes the consequences of heavy
urinary protein loss. The most
characteristic manifestation is generalised
oedema from a combination of decreased
serum oncotic pressure
(hypoalbuminaemia) and avid renal
sodium retention (secondary
hyperaldosteronism due to decreased
intravascular volume). Other wellrecognised features, which are explained
in the link below, include marked
hypercholesterolaemia, hypercoagulability
and increased susceptibility to infection.
Question 18. D) Hypocalcaemia
Explanation: Causes of polyuria are:
• excessive fluid consumption (polydipsia)
• osmotic diuresis (e.g. in diabetes mellitus
due to hyperglycaemia)
• reduced secretion of antidiuretic
hormone (cranial diabetes insipidus)
• resistance of the renal tubules to the
actions of antidiuretic hormone
(nephrogenic diabetes insipidus).
Nephrogenic diabetes insipidus has a
number of underlying causes including
interstitial renal disease, lithium therapy,
hypokalaemia and hypercalcaemia (which
165
also causes an osmotic diuresis). Cranial
diabetes insipidus is often idiopathic but
may occur secondary to head injury or an
intracranial tumour.
Question 19. A) Urge incontinence
Explanation: Anticholinergics reduce
detrusor muscle tone and may give
symptomatic relief to patients with urge
incontinence. Stress incontinence is a
common problem, particularly in
multiparous women, but anticholinergics
are not usually effective. Treatment is with
physiotherapy to strengthen pelvic floor
musculature and, in severe cases, surgery.
Question 20. E) Atenolol
Explanation: Beta-blockers are a
common cause of erectile dysfunction.
Sildenafil (Viagra) is a phosphodiesterase
5 inhibitor used as a treatment for erectile
dysfunction. Fluoxetine is a selective
serotonin reuptake inhibitor in common
use as an antidepressant. Interestingly, in a
randomised, double-blinded trial, valsartan
appeared to boost sexual performance in
middle-aged Italian males.
Question 21. D) Bilateral small kidneys
on renal ultrasound
Explanation: The other options given
here (haematuria, proteinuria, oliguria,
dehydration and hyperkalaemia) may all
be present in either acute or chronic renal
failure. In some cases it may be difficult to
determine the rate of onset of the renal
problem, but radiological evidence of
shrunken kidneys usually indicates chronic
disease.
Question 22. B) Ibuprofen
Explanation: Non-steroidal antiinflammatory drugs such as ibuprofen
have been shown to increase the risk of
contrast nephropathy. Intravenous fluid
and N-acetylcysteine are thought to have a
protective role.
Question 23. D) Amoxicillin
Explanation: Furosemide is a loop
diuretic and bendroflumethiazide
(formerly known as bendrofluazide) is a
thiazide diuretic. They are particularly
potent in combination and will impair
renal sodium and water reabsorption,
exacerbating hypovolaemia and
hypoperfusion. Lisinopril is an
angiotensin-converting enzyme (ACE)
inhibitor, which will prevent the
compensatory constriction of efferent
renal arterioles. Diclofenac, a nonsteroidal anti-inflammatory drug, will
prevent the compensatory dilatation of
renal resistance arteries. Both of these
drugs worsen renal failure in patients with
critically impaired renal perfusion.
Question 24. A) Promotes water
reabsorption from urine
Explanation: The medullary
concentration gradient is a key mechanism
of water reabsorption, enabling the
production of highly concentrated urine. It
is often lost in acute tubular necrosis
(ATN) and this can lead to a 'diuretic
phase' in which an inappropriately large
volume of urine is produced during
recovery from ATN.
Question 25. E) Haemodialysis
Explanation: Severe hyperkalaemia may
lead to life-threatening arrhythmias, and
resistant hyperkalaemia in the context of
acute renal failure is one of the strongest
indications for dialysis. Calcium gluconate
may also be appropriate treatment here but
is not used to lower serum potassium;
rather it acts to stabilise the myocardium
and should be given if the hyperkalaemia
is accompanied by ECG changes. Sodium
bicarbonate would be of little benefit as
the patient is not acidotic, and the other
conservative measures listed are unlikely
to achieve a sufficient reduction in serum
potassium.
166
Question 26. C) Bilateral nephrostomies
Explanation: Nephrostomies are
radiologically inserted drains that allow
urine to drain directly from the renal pelvis
and thereby decompress obstructed urinary
systems. Most patients with post-renal
acute renal failure will recover with relief
of the obstruction without the need for
renal support and, from the information
given, there is no compelling indication
for urgent renal replacement therapy here.
Fluid restriction is not indicated and,
indeed, fluid supplementation may be
required once the obstruction is relieved as
patients often experience a 'postobstructive diuresis'. Retroperitoneal
fibrosis causes ureteric obstruction, so
catheterisation would be unhelpful and
potentially dangerous as the bladder is
likely to be empty.
Question 27. C) Reduced phosphate
Explanation: Hyperphosphataemia is
typical in chronic renal failure due to a
combination of reduced phosphate
excretion and secondary
hyperparathyroidism. The elevated PTH
occurs as an 'appropriate' physiological
response to hypocalcaemia (hence
secondary hyperparathyroidism), which in
turn is due to deficiency of active (1Vhydroxylated) vitamin D.
Declining renal function is associated with
metabolic acidosis that should be treated
with sodium bicarbonate.
Hypercholesterolaemia is very common in
patients with chronic renal failure
(particularly with significant proteinuria)
and may contribute to the greatly
increased risk of cardiovascular events in
these patients.
Question 28. E) Complications of
erythropoietin include hypertension and
hypercoagulability
Explanation: In patients with significant
anaemia, plasma erythropoietin (EPO)
should be elevated; a level within the
normal range is therefore inappropriately
low and indicates inadequate EPO
production. The target haemoglobin level
is around 100-120 g/dl; significantly
higher targets may be associated with
increased cardiovascular mortality. Iron
deficiency is a common contributing factor
to anaemia in chronic renal failure and a
cause of suboptimal response to EPO;
transferrin saturation should therefore be
maintained above 20%. Human
recombinant EPO is currently only
available in intravenous and subcutaneous
preparations. Hypertension and
hypercoagulability are both wellrecognised side-effects of EPO.
Platelet function is actually impaired in
chronic renal failure ('uraemic platelets')
and this is accompanied by an increased
bleeding tendency.
Question 29. B) Angiotensin-converting
enzyme (ACE) inhibitors
Explanation: Aggressive control of blood
pressure is very important in patients with
chronic renal disease, both to slow the
deterioration in renal function and to
reduce the risk of cardiovascular
complications such as myocardial
infarction and stroke. All of the above
drugs may be used for this purpose;
however, ACE inhibitors are antiproteinuric and have been shown to have
'renoprotective effects' independent of
blood pressure lowering.
Question 32. D) Anaemia
Explanation: Dialysis essentially replaces
the functions of urine - excretion of solutes
and excess fluid, control of acid-base and
removal of toxins - but it does not replace
the endocrine functions of the kidney, such
as production of erythropoietin and
metabolism of vitamin D.
Question 30. D) Enhanced platelet
function
Explanation: Cardiovascular disease is by
far the leading cause of death in patients
with chronic renal failure. Hypertension
occurs in approximately 80% of patients
and is a major risk factor for myocardial
infarction, stroke and heart failure.
Hypercholesterolaemia is very common
and may also contribute to accelerated
atherosclerosis. Anaemia is an
independent predictor of left ventricular
hypertrophy. Patients with chronic renal
failure often have a heavily calcified
arterial tree and this may be so severe as to
cause limb ischaemia.
167
Question 31. A) 1L-hydroxylase
Explanation: One of the functions of the
kidney is conversion of the inactive form
of vitamin D (25-hydroxycholecalciferol)
to its active metabolite (1,25
dihydroxycholecalciferol) by the enzyme
1V-hydroxylase. Diminished activity of
this enzyme leads to deficiency of active
vitamin D, resulting in hypocalcaemia and
secondary hyperparathyroidism (see link
below). Hyperphosphataemia then occurs
from a combination of the secondary
hyperparathyroidism and reduced renal
phosphate excretion. Accumulation of
aluminium often occurs in dialysis patients
and may be associated with a wide range
of pathology.
Question 33. D) Symptomatic fluid shift
is less common with PD than HD
Explanation: Peritoneal dialysis is less
efficient than haemodialysis and must be
performed more often. However, fluid
shifts are less rapid, so peritoneal dialysis
is less likely to cause symptoms associated
with hypotension such as lightheadedness
and cramps. Abdominal scarring from
previous surgery may make peritoneal
dialysis impossible, but will not affect
haemodialysis.
Question 34. B) Active anti-glomerular
basement membrane (GBM) disease
Explanation: Active anti-GBM disease is
considered an absolute contraindication to
renal transplant because of the likelihood
of recurrence in the transplanted kidney.
Transplantation is routinely offered to
patients in their fifties in most centres.
Previous skin cancer is not directly
relevant if the lesion has been successfully
removed. However, 50% of Caucasian
renal transplant patients develop skin
malignancy within 15 years of
transplantation, so patient 'D' must be
advised to present early with any
suspicious lesions. Some patients with
chronic renal failure and diabetes mellitus
may be suitable for simultaneous pancreas
and kidney transplantation.
Question 35. D) Renal artery stenosis
Explanation: The response of the kidney
to a reduction in renal perfusion pressure
(such as occurs with flow-limiting stenosis
in a renal artery) includes activation of the
renin-angiotensin-aldosterone system
through increased renin production. The
resulting rise in angiotensin II
concentration mediates constriction of the
efferent arteriole and thereby maintains
glomerular perfusion pressure distal to the
stenosis. ACE inhibitors abolish this
compensatory mechanism and may
precipitate a marked reduction in
glomerular filtration rate; close monitoring
of renal function is therefore essential on
starting any patient on an ACE inhibitor or
angiotensin receptor blocker.
Question 36. B) Membranous
nephropathy
Explanation: Membranous nephropathy is
the most common cause of nephrotic
syndrome in adults. In contrast, anti-GBM
disease, post-streptococcal
glomerulonephritis and small-vessel
vasculitis tend to cause a 'nephritic' pattern
of clinical findings. Acute tubular necrosis
causes renal interstitial dysfunction and
usually presents with acute renal failure.
168
The link below provides a simple and
memorable summary of the spectrum of
clinical presentations of
glomerulonephritis.
Question 37. C) Goodpasture's disease
(anti-glomerular basement membrane
(anti-GBM) disease)
Explanation: As the name suggests,
rapidly progressive glomerulonephritis
(RPGN) may lead to a rapid deterioration
in renal function over days to weeks. It is
usually associated with the histological
appearance described as focal segmental
necrotising glomerulonephritis or
Question 38. A) Minimal change
nephropathy
Explanation: Minimal change disease
remits, in most cases, with corticosteroid
therapy. In contrast, the other conditions
listed characteristically exhibit a poor
response to steroids.
Question 39. E) Sensorineural deafness
Explanation: Alport's syndrome is an Xlinked recessive disorder that may present
with new renal failure in adulthood. It is
associated with sensorineural deafness and
ocular abnormalities.
Question 40. E) Renal cell carcinoma
Explanation: APKD is not associated
with an increased risk of renal cancer. The
liver may be massively enlarged but liver
failure is unusual. Subarachnoid
haemorrhage occurs in 10% of patients.
Question 41. B) Alpha-adrenoceptor
blockers
Explanation: Alpha-adrenoceptor
antagonists (e.g. tamsulosin) are used to
improve urinary flow in BPH. All of the
other options are precipitants of acute
urinary retention.
Question 42. A) Lytic bony metastases
Explanation: Bone is by far the most
common site of metastatic deposits in
prostate cancer but these characteristically
produce osteosclerotic rather than
osteolytic lesions on plain X-ray. Bony
involvement may also be indicated by an
isolated rise in alkaline phosphatase and
'hotspots' on radioisotope bone scans. In
practice, high levels of PSA (> 100 ng/ml)
are highly suggestive of distant bony
metastases. In prostate cancer the gland is
usually enlarged and feels hard and
irregular, often with obliteration of the
median sulcus. However, it is worth noting
that 10-15% of tumours are not palpable
on rectal examination.
169
Question 43. B) Adrenaline
(epinephrine)
Explanation: Renal adenocarcinomas
may secrete a wide variety of peptides that
can produce a range of systemic effects.
Adrenaline (epinephrine) is not usually
secreted by renal adenocarcinoma, but
may be secreted by a
phaeochromocytoma; these two tumours
may coexist in the von Hippel-Lindau
syndrome.
Question 44. D) Penicillamine
Explanation: All of the agents listed
above are potentially nephrotoxic through
a variety of mechanisms (see link below)
but penicillamine is a rare cause of
membranous nephropathy.
Chapter
17 CARDIOVASCULAR
DISEASE
Question 1. D) Large systolic waves are
associated with tricuspid regurgitation
Explanation: The internal jugular vein
drains directly into the right atrium and the
height of the pulse reflects right atrial
pressure. It should be viewed with the
patient at 45 degrees. Abdominal
compression causes the JVP to rise
(hepato-jugular reflux). This may aid
identification of the pulsation and help
distinguish it from an arterial pulsation. As
a waves are caused by atrial systole, they
are absent in atrial fibrillation.
Question 2. D) Right coronary artery
Explanation: The right coronary artery
supplies the AV node in 90% of
individuals, and supplies the sinoatrial
node in 60%. It also supplies the inferior
aspect of the heart. Inferior myocardial
infarction is therefore often associated
with transient sinus bradycardia and AV
block.
Question 3. A) Left anterior descending
artery
Explanation: Although the exact coronary
anatomy varies greatly between
individuals, the left anterior descending
artery normally gives branches to the
anterior part of the septum and the anterior
wall and apex of the left ventricle.
Question 4. D) Cholinergic nerve fibres
act on the sinoatrial node to slow heart
rate
Explanation: Sympathetic stimulation
increases heart rate (positively
chronotropic) and force of contraction
(positively inotropic) via _1-adrenoceptors.
Beta2-receptors are found predominantly
in the vasculature where they mediate
vasodilatation. Parasympathetic fibres run
in the vagus nerve and act to slow heart
rate (negatively chronotropic) through
170
effects on the sinoatrial and
atrioventricular nodes but do not influence
force of contraction. Parasympathetic
effects are mediated by acetylcholine and
are therefore also termed 'cholinergic'.
Question 5. B) Evaluation of unstable
angina
Explanation: Stress tests are
contraindicated in the presence of unstable
angina, decompensated heart failure and
severe hypertension.
Question 6. C) Exertional breathlessness
and throat tightness
Explanation: Myocardial ischaemia can
sometimes present with breathlessness
rather than chest pain. A sensation of
throat tightness often accompanies this.
Epigastric discomfort after eating could
represent inferior wall ischaemia but is
more likely to be dyspeptic. Wheeze is a
feature of bronchospasm and not
myocardial ischaemia. Accompanying
paraesthesia would suggest
hyperventilation syndrome. Exertional
palpitation would suggest either an
exercise-related arrhythmia or possibly
anaemia.
Question 7. B) Hypercholesterolaemia
Explanation: The abnormality shown in
the picture is xanthelasma, which, along
with tendon xanthomas and corneal arcus,
is a clinical manifestation of
hypercholesterolaemia. Eruptive
xanthomas would be more suggestive of
hypertriglyceridaemia.
Question 8. B) Exercise ECG
Explanation: The exercise tolerance test
(stress ECG) is highly useful in patients
with symptoms suggestive of angina. It
may help to confirm or refute the
diagnosis as well as identify patients with
high-risk features. Such patients may
require further evaluation with coronary
angiography.
Question 9. C) Spironolactone
Explanation: The goal of secondary
prevention is to reduce the risk of future
adverse events such as myocardial
infarction. This entails measures to correct
modifiable risk factors such as smoking
cessation, weight loss, optimal blood
pressure control and lipid-lowering
therapy, as well as antiplatelet therapy.
Although both an ACE inhibitor and a
statin are clearly indicated in this patient to
correct hypertension and
hypercholesterolaemia respectively, recent
trial data suggest that all patients with
vascular disease benefit from angiotensinconverting enzyme (ACE) inhibition and
that all patients with coronary heart
disease should receive statin therapy
irrespective of serum cholesterol.
Spironolactone is an aldosterone
antagonist beneficial in the treatment of
severe chronic heart failure and also as a
diuretic, particularly in cirrhotic patients
with ascites.
Question 10. E) Recurrent pulmonary
emboli
Explanation: Repeated pulmonary
thromboembolic events may lead to
increased pulmonary vascular resistance,
pulmonary hypertension and ultimately
right heart failure. The other disorders
present more commonly with left-sided
heart failure. Note, however, that
chronically elevated left atrial pressure
will also lead to pulmonary hypertension,
so any cause of left heart failure may
eventually result in concurrent right
ventricular failure.
171
Question 11. C) Fine bi-basal
crepitations
Explanation: A raised JVP and pitting
oedema may accompany the marked salt
and water retention in left heart failure but
are also characteristic findings in right
heart failure. Isolated right heart failure
does not lead to pulmonary venous
congestion. Hepatomegaly and ascites are
features of severe right heart failure.
Question 12. C) Displaced apex beat
Explanation: A displaced apex beat
suggests left ventricular enlargement. In
acute de novo heart failure there is no time
for left ventricular dilatation and hence the
finding of a displaced apex beat implies
chronic, underlying cardiac pathology.
The other features listed are all simply
manifestations of acute heart failure.
Question 13. B) Amlodipine
Explanation: Peripheral oedema is a
common side-effect of dihydropyridine
calcium channel blockers, such as
amlodipine and nifedipine, as they lead to
increased capillary permeability.
Question 14. E) Heavy proteinuria
Explanation: A raised jugular venous
pressure and hepatomegaly are both signs
of chronic heart failure. Severe chronic
heart failure is a catabolic state and
commonly causes weight loss and muscle
wasting (cardiac cachexia).
Hyponatraemia may be caused by diuretic
therapy but is also a feature of severe heart
failure.
Heavy proteinuria of greater than 3.5
g/day suggests nephrotic syndrome.
Question 15. B) Ramipril
Explanation: The mineralocorticoid
hormone aldosterone acts to conserve salt
and water at the expense of potassium (and
hydrogen ions) in the distal convoluted
tubule and collecting ducts of the kidney.
The principle stimulus to aldosterone
production is angiotensin II. Thus agents
that inhibit the renin-angiotensinaldosterone system (e.g. ACE inhibitors,
angiotensin receptor blockers) or the
actions of aldosterone (e.g.
spironolactone) may lead to
hyponatraemia and hyperkalaemia.
Loop diuretics such as furosemide
typically cause hypokalaemia.
Question 16. C) Beta-blockers
Explanation: Although a useful treatment
in patients with chronic stable heart
failure, _-blockers must be avoided in
patients with acute or decompensated heart
failure due to their negatively inotropic
effects. The other treatments listed are all
commonly used to good effect in the
management of acute pulmonary oedema.
Question 17. C) Dry cough
Explanation: As well as converting
angiotensin I to angiotensin II, the
angiotensin-converting enzyme (ACE) is
also responsible for breakdown of
bradykinin, a vasodilating peptide.
Increased bradykinin levels may be
responsible for the dry cough associated
with ACE inhibitors. As shown in the link
below, ARBs do not interfere with
bradykinin metabolism and are much less
likely to cause cough. Unfortunately they
share all of the more serious adverse
effects of ACE inhibitors such as renal
dysfunction and electrolyte disturbance.
172
Question 18. D) Loop diuretics
Explanation: Loop diuretics are first-line
treatment to relieve symptoms in patients
with chronic heart failure but have not
been shown to improve outcomes. It
would be ethically difficult to conduct a
heart failure trial in which diuretics were
withheld. The other agents listed have all
been shown to reduce cardiovascular
mortality and morbidity in patients with
chronic heart failure in large-scale
randomised controlled trials.
The treatment of chronic heart failure is a
topic of major importance and a
comprehensive guide, including the
evidence base for treatments, is provided
in the link below.
Question 19. B) Transient ischaemic
attack
Explanation: Transient loss of
consciousness is due to temporary global
cerebral dysfunction from either cerebral
hypoperfusion (syncope) or generalised
electrical discharge (seizure). Transient
ischaemic attacks, by definition, produce
focal cerebral dysfunction and the term
should not be applied to patients
presenting with blackouts. Basilar
ischaemia can cause loss of consciousness
but is very uncommon. Cardiac syncope
occurs with arrhythmia or structural heart
disease. The former is usually due to
profound bradycardia (e.g. Stokes-Adams
attack) or ventricular tachyarrhythmias.
The latter commonly occur with exertion
(e.g. severe aortic stenosis), when
profound hypotension results from a
combination of reduced cardiac output and
fall in peripheral vascular resistance. In
carotid sinus syndrome, hypersensitivity of
the carotid baroreceptors causes
inappropriate vasodilatation, provoking
recurrent episodes of blackout or altered
consciousness.
Question 20. E) Rapid recovery (< 1
min) following the collapse
Explanation: Events immediately before,
during and after a blackout may provide
useful clues to the cause. Cardiac syncope
often occurs without any warning (e.g.
Stokes-Adams attack) or may be preceded
by chest pain, palpitation or
lightheadedness (e.g. tachyarrhythmia). A
history of aura preceding the blackout
suggests seizure but is frequently lacking,
perhaps due to post-ictal retrograde
amnesia. For this reason a lack of
premonitory symptoms is a fairly poor
discriminator between the two. Urinary
incontinence and brief twitching activity
are often taken as evidence of seizure but
may actually occur with any cause of
blackout. Cyanosis during the unconscious
period suggests seizure, while extreme
'death-like' pallor is characteristic of
cardiac syncope. A rapid recovery with
full reorientation within 1 minute is very
suggestive of cardiac syncope and
virtually excludes seizure, which is
characterised by prolonged confusion,
drowsiness and disorientation.
Question 21. E) Defibrillation
Explanation: The rhythm strip shows
ventricular fibrillation characterised by
completely chaotic electrical activity. The
only effective treatment is defibrillation. If
delivered immediately this will restore
cardiac output in more than 80% of
patients, but the chances of successful
outcome fall by around 10% with each
minute's delay.
Question 22. B) Atropine
Explanation: In a cardiac arrest scenario,
atropine should be administered as a single
dose of 3 mg when the rhythm is either
asystole or pulseless electrical activity
with an electrical rate of less than 60 beats
per minute.
Question 23. B) Mitral stenosis
Explanation: The classical low-pitched
rumbling diastolic murmur of mitral
stenosis is often very difficult to hear and
a loud first heart sound may be the most
prominent auscultatory finding.
173
Question 24. E) Atrial septal defect
Explanation: In atrial septal defect there
is a left to right shunt because left atrial
pressure exceeds right atrial pressure. The
resulting increase in right ventricular
stroke volume prolongs right ventricular
ejection time and hence pulmonary valve
closure - accounting for the wide splitting.
The split between the sounds does not vary
with respiration because the septal defect
equalises pressures between the left and
right side of the heart throughout the
respiratory cycle. The increased right
ventricular stroke volume may also
produce a systolic flow murmur over the
pulmonary valve.
Question 25. D) Atrial fibrillation
Explanation: A fourth heart sound is due
to atrial contraction against a stiff left
ventricle and is therefore not present in
atrial fibrillation.
Question 26. C) Mitral regurgitation
Explanation: In contrast to a fourth heart
sound, which is always pathological, a
third heart sound may be a normal
physiological finding (e.g. in young adults
or pregnancy). The combination of a third
heart sound and soft first heart sound may
occur in mitral regurgitation or heart
failure.
Question 27. D) Aortic regurgitation
Explanation: The murmurs of VSD,
tricuspid regurgitation and pulmonary
stenosis all occur in systole. Mitral
stenosis typically produces a mid-diastolic
murmur. The soft early diastolic murmur
of aortic regurgitation is best heard with
the patient sitting forward in held
expiration and is often described as 'the
absence of silence' following the second
heart sound. The link below provides a
comprehensive guide to the evaluation of
heart murmurs.
Question 28. B) Raised intracranial
pressure
Explanation: Raised intracranial pressure
is associated with hypertension and
bradycardia.
Question 29. C) Atrial flutter
Explanation: Vagal manoeuvres, such as
carotid sinus massage or Valsalva
manoeuvre, slow conduction through the
AV node and may terminate AV nodal reentry tachycardia or reveal flutter waves
(as in this case) in atrial flutter.
Question 30. A) Bisoprolol
Explanation: Beta-blockers are the drug
of choice to prevent occasional paroxysms
of AF and are particularly useful when
there is associated hypertension (as in this
case), ischaemic heart disease or cardiac
failure. Verapamil and digoxin are both
used as rate-limiting agents in persistent
AF but are not effective for preventing
paroxysms. ACE inhibitors are effective
antihypertensives but have no antiarrhythmic properties. Amiodarone is
associated with troublesome side-effects
that restrict its use to those in whom other
measures have failed.
Question 31. D) Subtherapeutic INR
Explanation: Therapeutic anticoagulation
for at least 4 weeks before and 4 weeks
after elective DC cardioversion is essential
to minimise the risk of cerebral embolism.
All of the other factors listed would reduce
the chance of a successful long-term
outcome from cardioversion but are not, in
themselves, contraindications. In patients
with relapse following previous DC
cardioversion, anti-arrhythmic therapy
may reduce the risk of further recurrence
and help maintain sinus rhythm.
Question 32. E) Amlodipine
Explanation: Digoxin and _-blockers are
both suitable options for rate control in
atrial fibrillation. The other three options
listed are calcium channel blockers
(CCBs). The non-dihydropyridine CCBs
(e.g. verapamil) act predominantly by
slowing conduction at the AV node and
exert powerful rate-limiting effects.
174
On the other hand, the dihydropyridine
CCBs (e.g. amlodipine, nifedipine) act on
the peripheral vasculature to produce
vasodilatation. These agents are used
mainly as antihypertensives and may
actually cause reflex tachycardia.
Diltiazem exerts both rate-limiting and
vasodilating properties and may be used
for rate control in AF.
Question 33. C) Atrioventricular (AV)
nodal re-entrant tachycardia
Explanation: Adenosine transiently
blocks conduction through the AV node
and may therefore terminate AV nodal reentrant tachycardia. It may be of
diagnostic value in atrial flutter as the
slowing of conduction often reveals flutter
waves but does not cardiovert this rhythm.
It can also be of use in distinguishing
between ventricular tachycardia and a
supraventricular tachycardia with aberrant
conduction. Vagal manoeuvres such as
carotid sinus massage also slow or
transiently block AV conduction and may
be tried before adenosine.
Question 34. C) Wolff-Parkinson-White
syndrome
Explanation: The resting ECG shows a
short PR interval and slurred upstroke of
the QRS complex (known as a delta
wave), suggesting an accessory pathway
between the atria and ventricles. The
presence of an accessory pathway in
association with symptoms is known as
Wolff-Parkinson-White syndrome.
Question 35. D) Catheter ablation of
accessory pathway
Explanation: Percutaneous catheter
ablation of the accessory pathway is the
treatment of choice in patients with
symptomatic Wolff-Parkinson-White
(WPW) syndrome. It is important to note
that both digoxin and verapamil should be
avoided in WPW as they shorten the
refractory period of the accessory
pathway. Amiodarone prolongs the
refractory period and can be used as
prophylactic therapy but is associated with
troublesome long-term side-effects and is
less effective than catheter ablation.
Question 36. C) Presence of capture and
fusion beats on ECG
Explanation: A history of ischaemic heart
disease (particularly previous myocardial
infarction) and a QRS duration of > 140
ms both favour the diagnosis of VT.
However, capture and fusion beats (see
link below) are pathognomonic of VT and
therefore the best answer. Other features
that favour VT are extreme left axis
deviation (not right axis), lack of response
to carotid sinus massage/IV adenosine and
evidence of atrioventricular dissociation.
Note: VT is by far the most common cause
of a broad complex tachycardia and if
there is any doubt, manage as VT.
Question 37. B) IV amiodarone
Explanation: In any patient with VT the
priority is to determine if there is a cardiac
output. Pulseless VT is managed as a
cardiac arrest in the same way as
ventricular fibrillation. In patients with a
cardiac output the next step is to establish
if there is haemodynamic compromise
(e.g. systolic BP < 90; features of shock),
in which case the appropriate treatment is
urgent DC cardioversion (under general
anaesthetic unless unconscious).
Patients, such as the one above, who
tolerate the arrhythmia well may be treated
in the first instance with IV amiodarone
or, less commonly, IV lidocaine. They
must be monitored closely for signs of
deterioration with full resuscitation
facilities nearby.
Question 38. C) Torsades de pointes
Explanation: Torsades de pointes literally
means 'twisting points' and the ECG above
shows the characteristic pattern of rapid
irregular complexes that seem to oscillate
around a fixed central axis.
Question 39. D) Prolonged QT interval
Explanation: Torsades de pointes is a
complication of prolonged QT interval.
175
Question 40. C) Clarithromycin
Explanation: Macrolide antibiotics are a
well-known cause of QT interval
prolongation, should be avoided in
patients with long QT syndrome, and
should not be used with other drugs known
to cause QT prolongation, such as
amiodarone and sotalol.
Question 41. A) Magnesium
Explanation: IV magnesium should be
given in all cases. Class III antiarrhythmics, such as amiodarone and
sotalol, prolong the QT interval and may
exacerbate the situation.
Question 42. D) Third-degree
(complete) heart block
Explanation: Third-degree AV block
(complete heart block) results from
complete failure of conduction at the AV
node. Atrial impulses occur as usual,
giving rise to normal P waves. The AV
block results in a bradycardic ventricular
escape rhythm, usually associated with
wide QRS complexes due to the abnormal
activation of the ventricles. In some cases,
the escape rhythm can arise from the AV
node itself (nodal escape) and a narrowcomplex bradycardia develops. There is no
relationship between atrial and ventricular
activity on the ECG (AV dissociation).
Question 43. D) Dual-chamber
pacemaker
Explanation: This patient has a double
indication for pacemaker. Patients with
symptomatic bradyarrhythmias associated
with atrioventricular block should receive
permanent pacemakers. In addition,
patients with complete heart block may
derive prognostic benefit from pacemaker
implantation, even in the absence of
symptoms.
Question 44. A) Nephrotoxicity
Explanation: Digoxin has a narrow
therapeutic range and is predominantly
renally excreted. Consequently renal
impairment may lead to digoxin toxicity
and any of features B-E, but
nephrotoxicity does not result from
digoxin toxicity.
Question 45. C) Lipid-rich core
Explanation: Complications of
atherosclerotic plaque rupture, notably
myocardial infarction, stroke and acute
limb ischaemia, are the most common
cause of premature death in the developed
world. Understanding the mechanisms that
lead to plaque instability and developing
novel therapeutic strategies to reduce the
risk of rupture are therefore areas of major
importance.
Question 46. B) Raised high-density
lipoprotein (HDL) cholesterol
Explanation: Elevated HDL cholesterol is
protective against atherosclerosis. Raised
low-density lipoprotein (LDL) cholesterol
and, to a lesser extent, triglycerides
increase the risk of atherosclerosis.
Question 47. E) Chest pain and 1-2 mm
downward-sloping ST depression in
inferior leads during stage 1 of the
Bruce protocol
Explanation: The most convincing ECG
evidence of myocardial ischaemia is the
demonstration of reversible ST segment
depression or elevation that corresponds
with the timing of the patient's symptoms.
Horizontal and downward-sloping ST
depression usually indicate myocardial
ischaemia, while upward-sloping ST
depression is less specific. Of the above
scenarios, D and E would both constitute a
positive test, but in E there is ischaemia at
low workload - a high-risk finding and
therefore an indication for coronary
angiography. In scenario D, ischaemia
occurs only at high workload and effort
tolerance is good, both of which are
reassuring features. A rise in pulse and BP
are normal haemodynamic responses to
exercise, whereas a fall in BP during a
stress test is a high-risk finding.
176
The test result in scenario C should be
classed as 'inconclusive'; coronary
angiography may provide useful
diagnostic information but other forms of
stress test could also be considered (see
link).
Question 48. A) Clopidogrel
Explanation: Clopidogrel is an
antiplatelet drug used in patients intolerant
of aspirin. It reduces the risk of adverse
events such as myocardial infarction in
patients with stable angina but does not
relieve symptoms. The combination of
aspirin and clopidogrel is also used in the
management of acute coronary syndromes
and after percutaneous coronary
intervention. A comprehensive discussion
of anti-anginal drugs can be found in the
link below.
Question 49. B) Persistent ST segment
elevation on ECG
Explanation: Although unstable angina
may be associated with transient ST
elevation, the presence of persistent ST
elevation in the context of ischaemicsounding chest pain suggests an acute ST
elevation myocardial infarction. Other
causes of ST elevation include pericarditis
and a left ventricular aneurysm (usually a
long-term complication of a large anterior
myocardial infarction).
Question 50. C) Elevated serum
cholesterol
Explanation: Elevated serum cholesterol
is a risk factor for the development of
coronary artery disease and should be
addressed as part of a secondary
prevention strategy, but it is not a marker
for adverse outcomes in patients with
acute coronary syndromes.
Question 51. D) Aspirin, clopidogrel and
low molecular weight heparin
Explanation: The link below includes the
evidence base for this combined treatment.
Additional treatment with a glycoprotein
IIb/IIIa inhibitor (e.g. abciximab,
tirofiban) may further improve outcomes
in refractory cases, particularly in the
context of percutaneous coronary
intervention.
Question 52. E) Coronary angiogram
Explanation: This patient with unstable
angina has failed to settle with medical
therapy and has several high-risk features
including recurrent pain at rest, ECG
changes and an elevated troponin. He
should therefore undergo coronary
angiography with a view to
revascularisation through either
percutaneous coronary intervention or, if
appropriate, bypass surgery.
Question 53. B) Acute anterior
myocardial infarction
Explanation: The ECG shown was
actually taken from a 48-year-old man
who had developed severe chest pain 6
hours earlier. It shows acute full-thickness
anterior myocardial infarction. He has ST
elevation in leads I, aVL and V2-V6, and
has already developed Q waves in leads
V3-V5.
Question 54. D) IV metoprolol
Explanation: This patient has
uncontrolled hypertension which is a
relative contraindication to thrombolysis.
If thrombolysis is the reperfusion strategy
of choice for this patient, then urgent
control of blood pressure is required
before initiating therapy. This could be
achieved with either sublingual nifedipine
or IV metoprolol (oral ACE inhibitor
would take too long to have an effect). In
patients without contraindications (e.g.
heart failure or bradycardia) intravenous _blockers relieve pain, reduce arrhythmias
and improve short-term mortality, making
them the best option here. Large-scale
trials in acute MI have shown no survival
benefit from use of magnesium or calcium
channel blockers.
177
Primary percutaneous coronary
intervention (PCI) is an alternative
reperfusion therapy to thrombolysis that is
resource-intensive but produces better
outcomes. It is used in patients in whom
thrombolysis is contraindicated. In some
countries, it is supplanting thrombolysis as
the first-line reperfusion treatment for ST
elevation MI. The term 'rescue PCI' refers
to the use of PCI in patients for whom
thrombolysis has failed to achieve
reperfusion.
Question 55. B) IV atropine
Explanation: The admission ECG shows
acute inferolateral myocardial infarction
(MI). Inferior MI is often complicated by
sinus bradycardia and transient
atrioventricular (AV) block, due to
ischaemia of the sinus node and AV node
respectively. The correct initial treatment
for symptomatic sinus bradycardia is
atropine 0.6 mg IV repeated, if necessary,
to a maximum of 3 mg. AV block may
also respond to atropine or resolve with
reperfusion but, if symptomatic, may
require temporary pacemaker insertion. A
permanent pacemaker is very rarely
needed as the block almost always
resolves within 7-10 days.
Question 56. E) Isosorbide mononitrate
Explanation: In addition to lifestyle
modifications, and in particular smoking
cessation, the first four agents listed form
the core of secondary prevention following
acute MI. Aspirin reduces the risk of
further infarction and other vascular events
by 25% and _-blockers reduce long-term
mortality by 25%. The benefits of ACE
inhibitors and statins following MI extend
to patients with preserved left ventricular
function and serum cholesterol levels
within the normal range. Isosorbide
mononitrate offers no prognostic benefit
but might improve symptoms in patients
who continue to experience exertional
angina post-infarction.
Question 57. B) Night pain
Explanation: Chronic lower limb
ischaemia manifests as two distinct
clinical entities: intermittent claudication
(IC) and critical limb ischaemia (CLI).
The latter is by far the more dangerous
condition; it is almost always due to severe
multi-level disease and carries a high risk
of limb loss and mortality within a matter
of months. Night pain is one of the
cardinal features of CLI.
Diminished pedal pulses are a common
finding in both IC and CLI and the
presence of a bruit provides no
information on disease severity. ABPI, on
the other hand, is a simple but useful guide
to severity. A ratio of 0.8 is typical of IC;
it is usually < 0.5 in CLI.
Question 58. C) Previously undiagnosed
atrial fibrillation
Explanation: An obvious embolic source
such as atrial fibrillation would increase
the probability of embolism, particularly if
it were a new finding, as the patient would
almost certainly not be anticoagulated. All
of the other features listed would favour
thrombotic occlusion of a previously
diseased artery.
Question 59. D) New early diastolic
murmur
Explanation: Type B dissections may
involve the descending aorta and aortic
arch but, by definition, spare the ascending
aorta. A new early diastolic murmur
suggests aortic regurgitation and hence
involvement of the aortic root.
Question 60. A) Hyperlipidaemia
Explanation: The pathogenesis of
essential hypertension is poorly
understood but all of the factors listed
other than hyperlipidaemia (which is a risk
factor for atherosclerosis) are contributing
environmental factors.
178
Question 61. E) Addison's disease
Explanation: The vast majority (95%) of
patients with hypertension have no
specific underlying pathology but in a
small proportion of patients the elevated
blood pressure may be due to endocrine
disease, renal disease, drugs or coarctation
of the aorta. Addison's disease (primary
adrenal insufficiency) frequently presents
with hypotension.
Question 62. D) Thiazide diuretic
Explanation: Thiazide diuretics (e.g.
bendrofluazide) or calcium channel
blockers are recommended first-line
therapy for elderly patients with
hypertension.
Question 63. C) Calcium channel
antagonist
Explanation: See Guide to management
of hypertension
Question 64. C) Acute rheumatic fever
Explanation: This teenage patient has
evidence of recent streptococcal infection
(ASOT > 200 U/ml), pericarditis and
mitral regurgitation, making rheumatic
fever the most likely diagnosis.
Question 65. E) Flitting polyarthritis
Explanation: The diagnosis of acute
rheumatic fever is based on the revised
Jones criteria, and requires evidence of
recent streptococcal infection as well as
two or more major manifestations, or one
major and two or more minor
manifestations. This patient already has
sufficient evidence of streptococcal
infection in the form of elevated
antistreptolysin O titres so a positive throat
swab is incorrect. He currently fulfils one
of the major criteria ('carditis') and cardiac
dilatation would simply provide further
evidence of this criterion. Fever and a
prolonged P-R interval are both minor
criteria so neither one would be sufficient
for diagnosis. Flitting polyarthritis is
another of the major criteria (seen in 75%
of patients) and would therefore clinch the
diagnosis. The revised Jones criteria are
included in the link below.
Question66. D) Mitral stenosis
Explanation: The signs listed are typical
of mitral stenosis, as is the history of
slowly progressive symptoms. Atrial
fibrillation is an extremely common
complication owing to left atrial
enlargement. Aortic regurgitation typically
causes an early diastolic murmur and large
volume pulse.
Question 67. E) Loud pulmonary
component of second heart sound (P2)
Explanation: A loud S1, opening snap
and tapping apex beat are all classical
signs of mitral stenosis. The presence of a
pansystolic murmur radiating to the axilla
would suggest concomitant mitral
regurgitation. Clinical findings suggestive
of pulmonary hypertension include a loud
P2 and parasternal heave (right ventricular
hypertrophy), signs of tricuspid
regurgitation (secondary to right
ventricular dilatation) such as systolic
waves in the jugular venous pulse and,
ultimately, signs of right ventricular
failure such as pitting oedema and ascites.
Question 68. B) Concomitant mitral
regurgitation
Explanation: Mitral balloon valvuloplasty
is the treatment of choice for patients who
fulfil the necessary criteria. The presence
of mitral regurgitation is a
contraindication.
Question 69. E) Congenitally bicuspid
mitral valve
Explanation: This one is a bit of a trick
question, as the normal mitral valve is
bicuspid. A congenitally bicuspid aortic
valve (usually tricuspid) may predispose to
either aortic stenosis or regurgitation.
179
Question 70. B) Third heart sound (S3)
Explanation: Atrial fibrillation,
pulmonary congestion and pulmonary
hypertension (loud P2 and right ventricular
heave) commonly complicate both mitral
stenosis and regurgitation.
A third heart sound is caused by rapid
filling of the left ventricle during diastole;
therefore, its presence effectively excludes
significant mitral stenosis but is
characteristic of mitral regurgitation.
Question 71. E) Slow-rising carotid
pulse
Explanation: A slow-rising pulse is a
characteristic finding in aortic stenosis,
often accompanied by a narrow pulse
pressure, heaving but non-displaced apex
beat and a soft A2.
In general, left-sided heart murmurs are
louder in expiration; right-sided heart
murmurs are louder in inspiration.
Question 72. A) Syncopal episodes
Explanation: Reduced valve area and a
high pressure gradient across the valve are
both indicators of severity in aortic
stenosis, but the presence of symptoms is
by far the most important indication for
valve replacement.
Question 73. B) Acute aortic dissection
Explanation: Bounding pulses, a wide
pulse pressure and displaced apex beat are
characteristic of severe chronic aortic
regurgitation due to left ventricular
dilatation and increased stroke volume
consequent upon chronic volume overload
of the left ventricle. Syphilitic aortitis,
rheumatic heart disease, Marfan's
syndrome and ankylosing spondylitis are
all well-recognised causes. However, in
acute aortic regurgitation (e.g. secondary
to involvement of aortic root in acute
aortic dissection) there is no time for
compensatory hypertrophy and dilatation
of the ventricle. The apex beat is therefore
not displaced and the clinical picture tends
to be dominated by features of heart
failure and hypotension.
Question 74. A) Viridans streptococci
Explanation: Streptococci of the viridans
group are the most common cause of
native valve endocarditis, accounting for
30-40% of cases. They tend to cause
subacute endocarditis with a presentation
like the one described above. In contrast,
Staph. aureus endocarditis usually
presents as a severe acute febrile illness. It
is a common organism in IV drug
misusers, often affecting right-sided
valves. Coagulase-negative staphylococci,
such as Staph. epidermidis, are frequent
culprits in prosthetic valve endocarditis.
Coxiella burnetti is the causative agent in
Q fever, a cause of culture-negative
endocarditis.
Question 75. D) Benzyl penicillin and
gentamicin
Explanation: In this patient with subacute
endocarditis, streptococci are the most
likely causative agents and, therefore,
combined treatment with benzyl penicillin
and gentamicin is the best choice of
empirical therapy. The management of
infective endocarditis, including rationale
for choice of antibiotic, is described in the
link below.
Question 76. D) Vegetations on
echocardiography
Explanation: See Modified Duke criteria
180
Question 77. C) Patent ductus
arteriosus
Explanation: More on Patent ductus
arteriosus
Question 78. A) Ventricular septal
defect
Explanation: This patient has developed
Eisenmenger's syndrome and therefore the
original underlying abnormality must have
involved a left-right shunt, e.g. ventricular
septal defect or patent ductus arteriosus. In
patent foramen ovale there is a connection
between the left and right side of the heart
but no significant shunt. The other options,
in isolation, are not associated with
shunting of blood and are not causes of
cyanotic heart disease.
Question 79. D) Patent ductus
arteriosus
Explanation: More on Tetralogy of Fallot
Question 80. A) Tuberculosis
Explanation: The patient has symptoms
and signs of severe right heart failure with
no obvious features of left heart failure, a
normal-sized heart and heavy calcification
of the pericardium. The diagnosis is
constrictive pericarditis. In a patient from
West Africa the most likely underlying
diagnosis would be tuberculosis. This is a
common presenting feature of AIDS in
West Africa and he should be offered HIV
testing. Haemochromatosis and
trypanosomiasis may both cause a
cardiomyopathy.
Chapter
18 RESPIRATORY
DISEASE
Question 1. C) PaCO2 of 5.8 kPa
Explanation: The other features all
suggest a severe asthma attack but only
answer C is a life-threatening feature.
Patients with acute severe asthma should
have a depressed PaCO2 on account of the
increased alveolar ventilation. Even a
normal PaCO2 is a sign that the patient is
struggling to overcome the obstruction to
airflow and, perhaps, beginning to tire
from the effort of breathing. In this case
the PaCO2 is at the high end of the normal
range and, in addition to other appropriate
measures, the intensive treatment unit
should be alerted.
Question 2. B) Chronic obstructive
pulmonary disease (COPD)
Explanation: This lifelong smoker has an
obstructive ventilatory defect that is not
reversible by inhaled bronchodilators. Her
lungs are hyperexpanded and there is no
clinical evidence of pulmonary oedema or
fibrosis.
Question 3. B) Compensated respiratory
acidosis
Explanation: The results show a
respiratory acidosis (high PaCO2) that is
completely offset by a metabolic alkalosis
(high HCO3-), so that the overall pH of the
blood is normal. By far the most likely
explanation for this is chronic type II
respiratory failure with metabolic
compensation. The only theoretical
alternatives are complete respiratory
compensation for metabolic alkalosis or
concomitant but unrelated respiratory
acidosis and metabolic alkalosis. In
practice, the former does not occur and the
latter is extremely unlikely.
181
Question 4. D) Smoking cessation
Explanation: Smoking cessation is one of
the very few interventions shown to
prolong life in COPD. Nebulised and
inhaled ß2-agonists provide symptomatic
relief but do not influence prognosis. Oral
steroids are useful in the treatment of acute
exacerbations but have no role in
maintenance treatment; inhaled steroids
may reduce the number of acute
exacerbations and hospital admissions in
patients with severe disease and frequent
exacerbations. Tiotropium is a once-daily
inhaled anticholinergic treatment which
improves both symptoms and effort
tolerance but, like ß2-agonists, has not
been shown to reduce mortality.
Question 5. D) Transfer to a critical
care environment and consider
endotracheal intubation by an
experienced anaesthetist
Explanation: The likely diagnosis is acute
epiglottitis. The acute onset makes noninfectious causes of stridor, such as
tumour compression of the trachea, less
likely, so a CT would be of limited use. In
epiglottitis, the problem is the potential for
sudden airway occlusion. Nebulised
bronchodilators will offer no benefit,
while arterial blood gas analysis is
unlikely to provide much useful
information and may exacerbate the
situation by distressing the patient.
Examination of the throat is extremely
dangerous and should be avoided. The
patient must be managed with intravenous
antibiotics in facilities appropriate for
endotracheal intubation if necessary.
Question 6. C) Stony dull percussion
note at left base
Explanation: The patient has a moderate
to large left-sided pleural effusion which
will manifest clinically as reduced
expansion of the left hemithorax
accompanied by stony dullness to
percussion, reduced or absent breath
sounds, and reduced or absent vocal
resonance over the left base and mid-zone.
Large effusions can cause tracheal and
mediastinal shift although, from the chest
X-ray, there does not appear to be any
tracheal deviation in this case.
Question 7. D) Pleural aspiration
Explanation: The patient has a unilateral
pleural effusion. The most helpful
investigation in establishing the cause will
be evaluation of the pleural fluid obtained
by simple aspiration. The appearance of
the fluid should be noted (e.g. bloodstained, purulent) and it should then be
sent for biochemical, microbiological and
cytological analysis.
Question 8. B) Parapneumonic effusion
Explanation: The pleural effusion is an
exudate. We know this because the pleural
fluid protein is more than half the plasma
protein content and also because the
pleural fluid LDH is > 60% of the plasma
LDH (see Light's criteria in the link
below). Nephrotic syndrome and cardiac
failure cause transudative effusions. Acute
pancreatitis is highly unlikely in the
absence of either abdominal pain or a
raised serum amylase. Thoracic duct
occlusion causing chylothorax is very rare
and the pleural aspirate would have a
milky rather than serous appearance. The
diagnosis of parapneumonic effusion is
further supported by the patient's
confusion, the raised white cell count and
the low pH of the pleural fluid.
Establishing the cause of a pleural effusion
is a commonly encountered problem in
clinical practice and more information can
be found in the link below.
182
Question 9. A) Psychogenic
hyperventilation
Explanation: Psychogenic
hyperventilation is, to a large extent, a
diagnosis of exclusion, and alternative
possibilities such as pneumothorax and
particularly pulmonary embolism should
always be considered. However, there are
several pointers towards the diagnosis
here, most notably the inability to take a
deep breath, history of recurrent episodes,
absence of chest signs and reassuring
oxygen saturations. The hyperventilation
causes a respiratory alkalosis that may
lead to paraesthesiae in the hands and feet
and carpopedal spasm - both useful
distinguishing features.
Question 10. B) Rusty, golden yellowcoloured sputum
Explanation: Pneumocystis carinii
pneumonia (PCP) (caused by
Pneumocystis jirovecii) typically presents
with a dry, non-productive cough; rustybrown spit is a classical finding in
pneumococcal pneumonia. PCP is a
common and life-threatening infection in
AIDS sufferers. At presentation, dyspnoea,
fever and a dry cough are usual. The
dyspnoea is out of proportion to the chest
X-ray changes; indeed, many patients have
a normal chest X-ray and most have no
focal abnormalities on chest auscultation.
Induced sputum is the diagnostic test of
choice for PCP. Clinical findings
suggestive of HIV infection, such as
oropharyngeal candidiasis or oral hairy
leukoplakia, would also raise suspicion.
Question 11. E) Intravenous
aminophylline
Explanation: This patient has several
features to suggest this is an acute severe
asthma exacerbation (respiratory rate >
25/min, heart rate > 115, PEF < 50%
predicted, inability to speak in sentences)
and she should be managed accordingly.
Options A-D are all key steps but
intravenous aminophylline should only be
used in patients who fail to respond to
these and other measures (e.g. intravenous
magnesium) and, even then, usually under
specialist supervision. More information
on assessment of asthma severity can be
found in Q1 and further details of the
management of asthma exacerbations in
the link below.
Question 12. C) Refer to the intensive
treatment unit for consideration of
mechanical ventilation
Explanation: The patient has deteriorated
significantly despite maximal medical
therapy and this is now a life-threatening
asthma attack (PEF < 33% predicted, high
alveolar/arterial oxygen gradient, rising
PaCO2, quiet breath sounds, exhaustion).
She is likely to require intubation and
mechanical ventilation imminently and
should be referred to ITU without delay.
Note that, although non-invasive
ventilation may be useful in exacerbations
of COPD, it has no role in the
management of acute severe asthma.
Likewise, in acute asthma, the presence of
a high or rising PaCO2 must not be taken
as an indication to reduce oxygen
concentration but rather as a warning of
deterioration and possible need for
intubation and mechanical ventilation.
Question 13. D) Anticholinergic
Explanation: Ipratropium is an
anticholinergic bronchodilator. Tiotropium
is a newer, once-daily preparation.
Nebulised ipratropium forms part of the
treatment of acute severe asthma but its
main use is in the management of COPD.
183
Question 14. D) Viral pneumonia
Explanation: Viral pneumonia is very
unlikely to have lasted several months and
would be associated with chest X-ray
changes. The other options in this question
are reasonable differential diagnoses for a
patient with a persistent cough, although
bronchogenic carcinoma must also be
considered, particularly in smokers. Cough
may be the dominant symptom in asthma
with little or no breathlessness or wheeze.
Question 15. B) Aggressive fluid
resuscitation is necessary immediately
Explanation: Community-acquired
pneumonia is by far the likeliest diagnosis
here; non-specific elevation of D-dimer
occurs in a number of conditions other
than pulmonary embolism, including
pneumonia. She has severe sepsis with
evidence of haemodynamic compromise
and requires prompt, aggressive fluid
resuscitation, ideally with monitoring of
both urine output and central venous
pressure; she may require inotropic
support and invasive ventilation if her
condition does not improve. Current
British Thoracic Society guidelines
specify four markers of severity in
community-acquired pneumonia, known
as the CURB score:
• confusion
• urea > 7 mmol/l
• respiratory rate > 30/min
• low BP (systolic < 90 mmHg or diastolic
< 60 mmHg).
This patient has all four markers and is
undoubtedly in the severe category. She
requires immediate treatment with
intravenous third-generation cephalosporin
and macrolide; it is inappropriate to delay
pending the results of cultures. Her
management should be supervised in a
high-dependency or intensive care unit.
Management on a general medical or
general respiratory ward is inappropriate
for someone this ill.
Question 16. B) Pulmonary embolism
Explanation: The sudden onset of
symptoms, pleuritic chest pain and lack of
change in sputum favour the diagnosis of
pulmonary embolism over infective
exacerbation of COPD. She also has a risk
factor for thromboembolism in the form of
oestrogen-containing hormone
replacement therapy. One would expect
chest X-ray changes in acute left
ventricular failure or pneumonia;
psychogenic hyperventilation should not
be considered as a diagnosis in the
presence of hypoxia.
Question 17. A) Computed tomography
pulmonary angiogram (CTPA)
Explanation: In a patient with preexisting lung disease such as COPD, in
whom a pulmonary embolism (PE) is
suspected, CTPA is undoubtedly the
investigation of choice. A V/Q scan may
be hard to interpret, as existing lung
disease may cause perfusion defects and
the majority of such cases are reported as
'indeterminate'. Echocardiography may
help in the urgent diagnosis of massive PE
in patients with circulatory collapse by
identifying features of acute right heart
strain, but is less likely to be helpful in this
situation. The value of D-dimer is the high
negative predictive value conferred by a
low result. It is, however, non-specific and
a positive D-dimer, no matter how high,
would not confirm the diagnosis. HRCT is
mainly used in the assessment and
diagnosis of diffuse interstitial lung
disease and bronchiectasis.
Question 18. B) Percussion and
auscultation of the lung fields
Explanation: The most likely diagnosis is
tension pneumothorax, which can and
must be diagnosed on clinical
examination. Reduced breath sounds and
hyper-resonant percussion note on the
affected side confirm the diagnosis, and
immediate needle thoracocentesis should
be performed.
184
Question 19. C) Fibrotic lung disease
Explanation: These are all classical
findings in pulmonary fibrosis. Cystic
fibrosis presents at an earlier age;
however, severe bilateral bronchiectasis
might explain the findings, although the
crackles would tend to be coarse.
Question 20. A) Larynx and central
airways
Explanation: A useful fact to help
understand examination findings.
Question 21. D) Three lobes on the
right, two on the left
Explanation: This crucial fact is essential
for correct interpretation of all lung
imaging.
Question 22. C) Sarcoidosis
Explanation: The skin lesion described is
characteristic of erythema nodosum. The
combination of erythema nodosum,
arthralgia, constitutional symptoms and
isolated BHL on chest X-ray is highly
suggestive of sarcoidosis.
Question 23. D) Reduced midexpiratory flow indicates collapse of
small intrathoracic airways
Explanation: The loop shows the classical
pattern of intrathoracic small airways
obstruction, as seen in chronic obstructive
pulmonary disease (COPD). Large airway
obstruction limits peak inspiratory and/or
peak expiratory airflow (depending on the
site of obstruction), producing a plateau on
the loop. Vital capacity is frequently
reduced in obstructive ventilatory defects,
but the proportional reduction in forced
expiratory volume in 1 second (FEV1) is
greater, giving a reduced FEV1/vital
capacity (VC) ratio. The loop shows that
peak expiratory flow is reduced. At a
given lung volume, the limitation of flow
is much greater during expiration than
inspiration, indicating dynamic collapse of
the small intrathoracic airways.
Question 24. E) Functional residual
capacity
Explanation: A full explanation of all of
the above terms and uses of respiratory
function tests in clinical practice can be
found in the link below.
Question 25. A) Chest X-ray
Explanation: Pneumothorax should be
excluded in any apparent acute severe
asthma exacerbation, especially when
there are supportive clinical findings.
Question 26. A) Long-term oxygen
therapy
Explanation: Long-term domiciliary
oxygen therapy has been shown to
improve survival in selected patients with
COPD.
Question 27. D) Calcification on chest
X-ray
Explanation: Calcification may be found
in malignant tumours, particularly on CT,
but more often it indicates a granuloma,
perhaps from old tuberculosis.
Question 28. C) Protuberant mandible
Explanation: A recessed mandible is
associated with airway obstruction during
sleep.
Question 29. B) Arterial blood gas
(ABG) analysis
Explanation: The most likely cause of
this patient's deterioration is type II
respiratory failure. An ABG is essential to
confirm this, assessing the severity and
guiding further management.
Question 30. E) Mechanical ventilatory
support
Explanation: This patient is in extremis
and at high risk of imminent cardiac arrest
because of hypoxia. Her normal
bicarbonate shows that this is an acute not
a chronic deterioration, therefore probably
reversible. Her oxygen must not be
reduced, but unfortunately increasing it is
unlikely to be enough to save her,
particularly as this may further decrease
her respiratory drive. The best solution is
mechanical ventilatory support, which can
be delivered by non-invasive bi-level
ventilation or by intubation in an ITU.
Question 31. E) Severe kyphoscoliosis
Explanation: Type I respiratory failure
refers to hypoxia (PaO2 < 8 kPa) with a
normal or low PaCO2 (i.e. failure of
oxygenation) and is primarily caused by
ventilation-perfusion mismatch.
185
Type II respiratory failure is hypoxia
(PaO2 < 8 kPa) in the presence of
hypercapnia (PaCO2 > 6.6 kPa) and is due
to inadequate ventilation (not 'blowing off'
sufficient CO2). It is important to bear in
mind that any cause of type I respiratory
failure may progress to type II if
exhaustion supervenes.
Question 32. C) A trial of itraconazole
should be considered
Explanation: The most likely diagnosis is
allergic bronchopulmonary aspergillosis
(ABPA), caused by a hypersensitivity
reaction to Aspergillus fumigatus.
Common manifestations include fever,
breathlessness, cough productive of
bronchial casts and worsening of asthmatic
symptoms, which may be accompanied by
radiographic evidence of transient diffuse
pulmonary infiltrates and lobar or
segmental pulmonary collapse. Other
characteristic features include an elevated
peripheral blood eosinophilia (> 0.5 ×
109/l), positive skin test to an extract of A.
fumigatus, serum precipitating antibodies
to A. fumigatus and an elevated total
serum IgE. Fungal hyphae of A. fumigatus
may be seen on microscopic examination
of sputum (which will be rich in
eosinophils). The optimum maintenance
therapy for ABPA is uncertain. Regular
therapy with low-dose oral corticosteroid
therapy (prednisolone 7.5-10 mg daily) is
prescribed to suppress the
immunopathological responses and
prevent progression to tissue damage.
Therapy with itraconazole may be
beneficial in some patients. As this patient
has never smoked and lobar collapses have
occurred in two different sites, lung cancer
is unlikely.
Question 33. B) Non-steroidal antiinflammatory drugs
Explanation: Non-steroidal antiinflammatory drugs and ß-blockers are the
drugs most frequently implicated in
exacerbations of asthma. Beta-agonists
and leukotriene receptor antagonists are
used in the management of asthma.
Question 34. B) A 20% improvement in
forced expiratory volume in 1 second
(FEV1) following administration of a
bronchodilator
Explanation: All of these may be present
in an asthmatic patient, but only B
clinches the diagnosis according to current
criteria. Asthma is a very common disease,
so a knowledge of the diagnosis is
essential.
Question 35. B) Addition of long-acting
ß2-adrenoceptor agonist
Explanation: It is always important in this
situation to check inhaler technique,
adherence to treatment and avoidance of
aggravating factors first before increasing
drug therapy. Long-acting inhaled ß2agonists (e.g. salmeterol) are first choice
of add-on therapy for patients whose
symptoms are inadequately controlled on
regular inhaled corticosteroid and an asrequired short-acting ß2-agonist. Asthma
treatment is guided by a stepwise
treatment model, based on good clinical
evidence and detailed in the link below.
Question 36. C) 76-year-old ex-smoker
with bilateral pitting oedema to knees
and maximum PaO2 of 7.7 kPa on two
ABGs 3 weeks apart
Explanation: Criteria for LTOT are based
on two sets of ABG measurements taken
at least 3 weeks apart in clinically stable
patients on optimal medical therapy. To
qualify, patients must have stopped
smoking and demonstrate either:
• PaO2 < 7.3 kPa (and FEV1 < 1.5 litres)
• PaO2 7.3-8 kPa plus pulmonary
hypertension, peripheral oedema or
nocturnal hypoxaemia.
Only the patient in C meets these
requirements. LTOT is one of the few
treatments that favourably alters prognosis
in COPD. More information can be found
in the link below.
Question 37. A) Autosomal recessive
Explanation: The gene for CFTR (cystic
fibrosis transmembrane conductance
regulator) is on the long arm of
chromosome 7. A defect in the genes
encoding CFTR from both parents is
required for clinical disease.
186
Interestingly, heterozygotes (who have
one normal and one abnormal CFTR gene)
appear to have some protection from fluid
loss in gastroenteritis such as cholera.
Question 38. B) Amiodarone
Explanation: See list of Drug-induced
respiratory diseases
Question 39. B) Tuberculosis
Explanation: Caseating granulomas are a
classic finding in tuberculosis, which is
often discovered after a 'cryptic'
presentation such as this, particularly in
the elderly.
Question 40. C) Right upper lobe
collapse
Explanation: This chest X-ray has the
classic appearance of right upper lobe
collapse. The link below shows the chest
X-ray features associated with collapse of
the other lobes.
Question 41. B) Small-cell bronchogenic
carcinoma
Explanation: Lobar collapse in a smoker
is commonly due to lung cancer. Of the
various histological subtypes of bronchial
carcinoma, small-cell carcinoma most
commonly causes hyponatraemia through
ectopic inappropriate secretion of
antidiuretic hormone (ADH).
Question 42. C) Squamous carcinoma
Explanation: Squamous cell cancers may
cause hypercalcaemia by secreting ectopic
parathyroid hormone (PTH). Small-cell
carcinomas commonly secrete antidiuretic
hormone (ADH) and adrenocorticotrophic
hormone (ACTH).
Question 43. A) Continued cigarette
smoking
Explanation: Cigarette smoking is a
contraindication to domiciliary oxygen
therapy but this is on the grounds of safety
(oxygen is a fire hazard). It is not a
contraindication to surgical resection of
bronchial carcinoma.
Question 44. E) Asthma
Explanation: Asthmatic patients often
have relatively normal lung function at
rest so asthma is not usually associated
with chronic hypoxaemia and the majority
of patients have normal pulmonary artery
pressures. In contrast, the other conditions
listed cause progressive pulmonary
hypertension, which is associated with
increased complications and mortality.
Question 45. D) Rheumatic fever
Explanation: Connective tissue disorders
may lead to pulmonary fibrosis and a
variety of other respiratory complications.
Rheumatic fever may cause pleurisy or a
pleural effusion, but not fibrosis.
Question 46. E) Intravenous endothelin
Explanation: Endothelin is a potent
pulmonary vasoconstrictor. The endothelin
receptor antagonist bosentan has shown
some promising results in pulmonary
hypertension.
Question 47. B) The most likely
diagnosis is silicosis
Explanation: This history and the chest
X-ray appearances are highly suggestive
of silicosis. Silicosis results from the
inhalation of crystalline or free silica,
usually in the form of quartz. Occupations
at risk include stonemasons, sandblasters
and miners. Silica is highly fibrogenic and
even when exposure to dust ceases, the
187
disease is often progressive. The patient
should, therefore, be removed from the
offending environment as soon as
possible. Enlargement of the hilar glands
with an 'egg-shell' pattern of calcification
is said to be a characteristic chest X-ray
appearance but is uncommon and nonspecific. The appearances described are
not those of miliary tuberculosis; however,
it should be remembered that patients with
silicosis may be at increased risk of
tuberculosis - so-called 'silicotuberculosis'.
The recognition of occupational lung
disease should prompt screening of the
workplace to identify other affected
individuals.
Question48. B) The clinical scenario
could be explained by bleomycin
toxicity
Explanation: It is correct to consider a
diagnosis of PCP; however, induced
sputum is generally the investigation of
choice. Bronchoalveolar lavage may be
considered as a second-line investigation.
In this case induced sputum samples for
PCP and cytomegalovirus were negative
and the most likely diagnosis was
bleomycin-induced pneumonitis. Lung
function tests classically show a restrictive
defect and patients typically desaturate on
exertion. HRCT will confirm the presence
of interstitial inflammation but is not
usually diagnostic.
Chapter
19 ENDOCRINE DISEASE
Question 1. B) Thyroid-stimulating
hormone (TSH)
Explanation: The thyroid is the only
tissue which makes significant
physiological use of iodine. The functional
unit of the thyroid gland is the follicle,
consisting of central colloid surrounded by
follicular epithelial cells. Inorganic iodide
is trapped and transported into these cells
and organified by the enzyme thyroid
peroxidase; thereafter the iodine is bound
to thyroglobulin protein. This iodinated
molecule is cleaved to release the thyroid
hormones thyroxine (T4) and
triiodothyronine (T3). T4 can be converted
to either T3 or rT3 in peripheral tissues. A
dietary iodide intake greater than 100 µg
per day is necessary for thyroid hormone
synthesis. Thyroid-stimulating hormone
(TSH, thyrotrophin) is a glycoprotein
released from the anterior pituitary which
stimulates the whole process, and is
subject to negative feedback from T4 and
T3. TSH does not contain iodine. The antiarrhythmic drug amiodarone contains
large amounts of iodine.
Question 3. E) Toxic thyroid adenoma
Explanation: In toxic adenoma there is
increased isotope uptake by the adenoma.
However, excessive thyroxine production
by the adenoma inhibits pituitary thyroidstimulating hormone (TSH) secretion so
that the remainder of the thyroid gland is
suppressed, resulting in negligible isotope
uptake. In toxic multinodular goitre there
is patchy uptake by the hyperfunctioning
nodules. Thyroiditis is associated with low
isotope uptake by the thyroid as the
follicular cells are not functioning
normally during a temporary inflammation
of the gland. (The excess thyroid hormone
is released from stores within the follicle,
rather than synthesised de novo.) Thyroid
malignancies are not usually associated
with derangements of thyroid function and
are visible as 'cold' (low-uptake) areas on a
scintigraphy scan. Medullary carcinoma
arises from the parafollicular C cells
which produce calcitonin. A very useful
guide to establishing the diagnosis in
thyrotoxicosis is provided in the link
below.
Question 2. C) Graves' thyrotoxicosis
Explanation: The raised T4 with
undetectable TSH levels indicates primary
thyrotoxicosis. The most common cause of
thyrotoxicosis is the autoimmune
condition, Graves' disease. TSH receptor
antibodies are very rare in patients without
autoimmune thyroid disease and their
presence therefore confirms the diagnosis.
Note, however, that 5-20% of patients
with Graves' disease are negative for these
antibodies; had the result been negative
rather than positive, this would not have
excluded the diagnosis of Graves' disease
and further tests (thyroid scintigraphy)
might have been required.
Question 4. B) Lid lag
Explanation: Lid retraction (visible sclera
above the iris) and lid lag (delay in
downward movement of the upper eyelid
during downgaze) can occur with all
causes of thyrotoxicosis. They result from
the effect of increased sympathetic activity
on the levator palpebrae superioris
muscles. The other listed ocular features
are only seen in Graves' disease, although
their presence is unrelated to the severity
of the thyrotoxicosis. Ophthalmoplegia
and diplopia result from swelling and
eventual fibrosis of the extraocular
muscles. Other features specific to Graves'
are pretibial myxoedema and thyroid
acropachy (finger clubbing).
188
Question 5. D) Thyroid-stimulating
hormone (TSH) receptor antibodies
(TRAb)
Explanation: Stimulating TRAb
antibodies are responsible for stimulating
the TSH receptors and causing
thyrotoxicosis. Occasionally, blocking
TRAb antibodies cause episodes of
hypothyroidism in patients with
autoimmune thyroid disease. Routine
assays cannot distinguish stimulating from
blocking antibodies but TRAbs are present
in up to 95% of patients with Graves'
disease and are rare in patients with other
forms of thyroid disease.
Question 6. B) Propranolol
Explanation: Thyrotoxicosis is an
important cause of atrial fibrillation (AF).
Of the agents listed above, the nonselective _-blocker propranolol is best for
AF associated with hyperthyroidism and is
also useful for many other symptoms of
hyperthyroidism (particularly tremor)
which are mediated by increased
sympathetic activity. Ventricular rate in
thyrotoxic patients with AF
characteristically responds poorly to
digoxin. Prolonged use of amiodarone can
lead to hyper- or hypothyroidism. Acute
DC cardioversion is reserved for those
patients who are haemodynamically
compromised by the rapid ventricular rate.
Two other key elements of this patient's
management will be definitive treatment
of her thyrotoxicosis and anticoagulation
(thromboembolic complications are
particularly common in thyrotoxic AF).
Question 7. D) Hyperprolactinaemia
Explanation: The most common causes of
hypothyroidism in the UK are autoimmune
disease (including Hashimoto's thyroiditis)
and thyroid failure following
thyroidectomy or radio-iodine therapy.
Transient thyroiditis (e.g. de Quervain's
thyroiditis, post-partum thyroiditis) is
often associated with an initial thyrotoxic
phase, followed by transient
hypothyroidism. Although Graves' disease
usually causes hyperthyroidism, the
thyroid-stimulating hormone (TSH)
receptor antibodies can sometimes have a
blocking effect rather than a stimulatory
one, resulting in hypothyroidism.
189
Hyperprolactinaemia does not cause
hypothyroidism but may occur as a result
of primary hypothyroidism due to
increased hypothalamic thyrotrophinreleasing hormone (TRH) secretion (TRH
stimulates prolactin release).
Question 8. C) Start treatment with
thyroxine
Explanation: This patient has primary
hypothyroidism, as indicated by the low T4
level with raised TSH. She has clinical
symptoms of hypothyroidism and
treatment with thyroxine is required. The
positive anti-thyroid peroxidase antibody
result suggests an autoimmune cause such
as Hashimoto's disease. Imaging of the
thyroid gland is unlikely to provide any
additional information, and such cases can
generally be managed in the primary care
setting. Carbimazole is used in the
treatment of hyperthyroidism.
Question 9. B) Normal ageing
Explanation: As phenytoin and
rifampicin are liver enzyme inducers, they
increase metabolism of thyroxine, often
necessitating an increase in the thyroxine
dose. In coeliac disease there is
malabsorption, so a higher dose of oral
thyroxine may be required. Pregnancy is
associated with increased levels of
thyroid-binding globulin; a greater
proportion of thyroid hormone is therefore
bound to protein, and an increased
thyroxine dose may be needed to maintain
the same levels of free active thyroid
hormone. Ageing leads to a reduction in
thyroxine clearance and smaller doses of
thyroxine are often required.
Question 10. D) Give IV
triiodothyronine and IM hydrocortisone
Explanation: Myxoedema coma is a rare
presentation of hypothyroidism. It has a
50% mortality rate and needs urgent
treatment even before biochemical
confirmation of the diagnosis. IV
triiodothyronine replacement is required.
Unless it is clear that the patient has
primary hypothyroidism (e.g.
thyroidectomy scar), hydrocortisone
should also be administered to cover the
possibility of coexisting corticosteroid
deficiency due to hypothalamic or
pituitary disease. In hypopituitarism,
administration of thyroid hormone in
advance of hydrocortisone replacement
can be dangerous, as the increase in
metabolic rate may precipitate an adrenal
crisis. Supportive measures (e.g. oxygen,
IV fluids and rewarming) are also
important, but the bradycardia is
appropriate to her slow metabolic rate and
is likely to respond to hormone
replacement.
Question 11. A) Facial nerve injury
Explanation: Complications of subtotal
thyroidectomy are rare. A hoarse voice or
change in voice quality can result from
damage to the recurrent laryngeal branch
of the vagus (X) nerve, but there is no risk
of injury to the facial (VII) nerve. Around
25% of patients become hypothyroid
following surgery and require temporary
treatment with thyroxine, but permanent
hypothyroidism is rare. Transient (10%) or
permanent (rare) hypocalcaemia can occur
due to damage to the parathyroid glands or
their blood supply, and careful monitoring
of serum calcium is important during the
post-operative period. Exacerbation of
Graves' ophthalmopathy is thought to be a
complication of radio-iodine treatment
(not surgery), and prophylactic therapy
with corticosteroids reduces this risk.
Question 12. C) The risk of relapse is
greater than 30% within 2 years of
stopping the drug
Explanation: The antithyroid drugs
carbimazole and propylthiouracil act by
inhibiting the iodination of tyrosine and
thereby reducing thyroid hormone
synthesis.
190
Since episodic relapse and remission is the
most common pattern in the natural
history of Graves' thyrotoxicosis,
carbimazole is usually given for 12-18
months in the anticipation that the disease
will be in remission when the drug is
discontinued. However, thyrotoxicosis
recurs in at least 50% of patients within 2
years of stopping treatment. Subtotal
thyroidectomy or radioactive iodine
therapy may then be preferred.
Agranulocytosis is a rare side-effect of
carbimazole, occurring in 0.2% of
patients; patients are therefore advised to
undergo urgent testing of their full blood
count in the event of a sore throat or fever.
Although carbimazole and
propylthiouracil are only excreted in small
amounts in breast milk, propylthiouracil is
thought to be safer.
Question 13. A) Medullary carcinoma
Explanation: Medullary carcinoma arises
from the parafollicular C cells of the
thyroid. Tumour cells secrete calcitonin,
and serum levels can be used to monitor
response to treatment. The condition
presents in middle age with a firm thyroid
mass, and treatment is by total
thyroidectomy. Thyroid function tests are
normal and there is no role for radioiodine therapy.
Question 14. B) Carbimazole
Explanation: 'Differentiated' (papillary
and follicular) thyroid carcinomas usually
present as palpable nodules for which the
initial investigation of choice is fine
needle aspiration cytology. They are
usually treated by total thyroidectomy
followed by a large dose of 131iodine to
ablate any residual thyroid tissue.
Subsequent long-term treatment with
thyroxine at a dose sufficient to suppress
thyroid-stimulating hormone (TSH)
secretion is required, and recurrence can
be detected by secretion of thyroglobulin
into the blood. Papillary and follicular
carcinoma have 20-year survival rates of
95% and 60% respectively.
Question 15. D) Autoimmune gonadal
failure
Explanation: In hypogonadotrophic
hypogonadism there is deficiency of
follicle-stimulating hormone (FSH) and
luteinising hormone (LH), the
gonadotrophins. This may be due to
structural disease of the pituitary or
hypothalamus (e.g. pituitary adenoma), or
to 'functional' gonadotrophin deficiency
secondary to other influences (e.g. chronic
illness, stress, malnutrition, excessive
exercise). Primary gonadal failure, on the
other hand, is associated with elevated
gonadotrophin levels due to a loss of
negative feedback (hypergonadotrophic
hypogonadism).
Question 16. B) Women with an intact
uterus should receive both oestrogen
and progesterone
Explanation: Oestrogen replacement in
post-menopausal women reduces
vasomotor symptoms (e.g. hot flushes,
sweats) and prevents osteoporotic
fractures. There is, however, an increased
risk of breast and endometrial cancer,
thromboembolic disease, ischaemic heart
disease and stroke. For these reasons, HRT
should not be continued long-term, and
many authorities recommend that
treatment is only continued beyond the age
of 50 if there are unacceptable symptoms
of oestrogen deficiency. In women with an
intact uterus, unopposed oestrogen therapy
is more likely to cause endometrial
malignancy; combined cyclical treatment
with progesterone is therefore
recommended to induce regular
withdrawal bleeds.
Question 17. A) Bromocriptine
Explanation: High serum prolactin levels
may be physiological (e.g. stress,
pregnancy) or pathological. Prolactin
secretion from the anterior pituitary is
normally inhibited by dopamine from the
hypothalamus. Pituitary tumours can cause
hyperprolactinaemia by directly secreting
prolactin (prolactinoma) or by
compressing the infundibular stalk and
thereby interfering with the inhibitory
effect of dopamine. Anti-dopaminergic
drugs (e.g. antiemetics and antipsychotics)
can also cause high prolactin levels.
191
Bromocriptine, on the other hand, is a
dopamine agonist used in the treatment of
prolactinoma. Primary hypothyroidism
leads to increased hypothalamic
thyrotrophin-releasing hormone (TRH)
secretion by negative feedback, which in
turn stimulates prolactin release from the
pituitary.
Question 18. C) Gliclazide
Explanation: PCOS is associated with
insulin resistance and obesity. Weight loss
and treatment with insulin-sensitising
drugs such as metformin are beneficial;
gliclazide is a sulphonylurea which
enhances insulin secretion but not insulin
sensitivity, and has no role in PCOS. The
combined oral contraceptive pill enables
cyclical delivery of oestrogen and
progesterone, which regulates menstrual
cycles and improves hirsutism by
suppressing androgen production from the
ovary. Cyproterone acetate is an androgen
receptor antagonist (which also has
progesterone agonist effects) and is useful
in combating hirsutism in PCOS.
Question 19. E) Low follicle-stimulating
hormone (FSH) and luteinising
hormone (LH) levels
Explanation: Turner's syndrome affects 1
in 2500 females and is usually associated
with the 45XO karyotype. Ovarian
development during gestation is abnormal.
The ovaries are therefore unable to
produce adequate oestrogen, and the loss
of negative feedback leads to elevated
levels of FSH and LH. The short stature
responds in part to growth hormone
therapy.
Question 20. C) There is an increased
incidence of gynaecomastia
Explanation: Klinefelter's syndrome
affects 1 in 1000 males and is usually
associated with the 47XXY karyotype.
There is dysgenesis and subsequent
fibrosis of the seminiferous tubules, and
affected individuals usually have small,
firm testes. Tall stature (due to androgen
deficiency and failure to close the
epiphyseal growth plates) is common, and
growth hormone treatment is not required.
Impaired testicular function results in
androgen deficiency, which in turn leads
to elevated follicle-stimulating hormone
(FSH) and luteinising hormone (LH)
levels due to loss of negative feedback
(hypergonadotrophic hypogonadism). The
lack of androgens leads to gynaecomastia,
failure of development of secondary sex
characteristics and infertility.
Question 21. D) Alpha-fetoprotein
(AFP)
Explanation: Teratomas often secrete Vfetoprotein (AFP), and both teratomas and
seminomas secrete _-human chorionic
gonadotrophin (_-HCG); serum levels of
these tumour markers are potentially
useful in diagnosis and prognosis.
Question 22. B) It inhibits 1Lhydroxylation of vitamin D in the
kidney
Explanation: PTH is a polypeptide
hormone secreted by the parathyroid
glands in response to low serum calcium
levels. Its actions lead to an increase in
serum calcium. This is mediated by
increased calcium resorption from bone
and increased renal absorption of calcium.
Vitamin D derived from sunlight and from
the diet initially undergoes 25hydroxylation in the liver to 25-hydroxyvitamin D, which then undergoes 1Vhydroxylation in the kidney to form active
1,25-dihydroxy-vitamin D. PTH stimulates
the latter step. Activated vitamin D
increases gut absorption of calcium,
thereby further increasing calcium levels.
192
Question 23. B) Secondary
hyperparathyroidism
Explanation: Primary
hyperparathyroidism is usually due to a
parathyroid adenoma, but can be due to
parathyroid hyperplasia or, in rare cases,
parathyroid carcinoma. Elevated
parathyroid hormone (PTH) levels result
in hypercalcaemia. Secondary
hyperparathyroidism occurs as a response
to hypocalcaemia (e.g. in chronic renal
failure), and calcium levels are therefore
normal or low. Prolonged secondary
hyperparathyroidism can ultimately lead to
autonomous PTH hypersecretion with
consequent hypercalcaemia (tertiary
hyperparathyroidism). Malignancy can
lead to elevated serum calcium due to
bony metastases, paraneoplastic
phenomena (mediated by PTH-related
peptide, e.g. in squamous cell bronchial
carcinoma) or myeloma.
Question 24. C) Hyperparathyroidism,
medullary thyroid carcinoma,
phaeochromocytoma
Explanation: MEN syndromes are rare
autosomal dominant disorders
characterised by tumours or hyperplasia in
multiple glands. Differentiated thyroid
cancers (e.g. follicular carcinoma) are not
a feature. Option A describes MEN type 1,
and option E describes von Hippel-Lindau
syndrome.
Question 25. C) Low calcium, high
phosphate, low parathyroid hormone
Explanation: This patient has
hypoparathyroidism resulting from
damage to the parathyroid glands during
her thyroidectomy. Since the net effect of
parathyroid hormone (PTH) is to increase
serum calcium and decrease phosphate,
this results in hypocalcaemia and
hyperphosphataemia. Carpopedal spasm is
a manifestation of tetany and is
characteristic of hypocalcaemia. In carpal
spasm, the metacarpophalangeal (MCP)
joints are flexed and the interphalangeal
(IP) joints extended. Other features of low
calcium include tingling in the hands and
feet and around the mouth, stridor and
seizures. Chvostek's and Trousseau's signs
may be positive.
Question 26. A) Osteophyte formation
Explanation: Hyperparathyroid bone
disease is now rare thanks to earlier use of
surgical parathyroidectomy. Osteitis
fibrosa cystica results from bone
resorption by osteoclasts with subsequent
fibrous tissue deposition within the
lacunae. Bone mineral density is reduced
and subperiosteal erosions and terminal
resorption can be seen in the phalanges.
Calcium pyrophosphate crystal deposition
within the articular cartilage (especially
the knees) leads to chondrocalcinosis and
pseudogout. Osteophytes are a
characteristic radiological finding in
osteoarthritis.
The overnight dexamethasone suppression
test involves administration of 1 mg of the
synthetic glucocorticoid dexamethasone at
bedtime with measurement of plasma
cortisol as soon as practicable after waking
the next morning. In healthy individuals,
endogenous adrenocorticotrophic hormone
(ACTH) secretion is inhibited and plasma
cortisol is therefore suppressed to < 60
nmol/l. Failure to suppress endogenous
cortisol secretion is consistent with
Cushing's syndrome. Alternative screening
tests include measurement of cortisol in a
24-hour urine sample or of
cortisol:creatinine ratio in an overnight
urine sample.
Question 27. B) Cushing's syndrome
Explanation: Cushing's syndrome is
caused by excessive glucocorticoid levels,
which may be exogenous or endogenous
in origin. Addison's disease results from
primary adrenocortical insufficiency. In
Conn's syndrome there is excess
mineralocorticoid secretion by an adrenal
adenoma. Phaeochromocytoma arises
from a tumour of catecholamineproducing enterochromaffin cells, most
commonly from the adrenal medulla.
Question 30. B) Low blood pressure,
low sodium, high potassium
Explanation: In Addison's disease there is
primary adrenocortical insufficiency.
Mineralocorticoid (aldosterone) deficiency
leads to hypotension, hyponatraemia and
hyperkalaemia. Glucocorticoid (cortisol)
deficiency causes hypotension and
hyponatraemia. Patients can present with
chronic features (e.g. fatigue, weight loss,
anorexia) or with an acute adrenal crisis
associated with circulatory collapse. The
latter is a medical emergency requiring
urgent treatment with IV fluids and
hydrocortisone.
Question 28. D) Chronic glucocorticoid
therapy
Explanation: Prolonged administration of
glucocorticoids in supra-physiological
quantities (e.g. in patients with asthma or
inflammatory bowel disease) is the most
common cause of Cushing's syndrome. In
patients who have not received
glucocorticoid therapy, pituitary adenoma
is the most common cause (Cushing's
disease).
Question 29. C) Overnight
dexamethasone suppression test
Explanation: The first step is to establish
whether or not the patient has Cushing's
syndrome; further investigations are then
required to determine the cause. Random
plasma cortisol levels are unhelpful in
view of the diurnal variation in cortisol
secretion.
193
Question 31. E) Spironolactone
Explanation: In Conn's syndrome there is
an aldosterone-secreting adrenal adenoma.
Aldosterone promotes sodium and water
retention and increases renal potassium
excretion. High mineralocorticoid levels
therefore result in hypertension and
hypokalaemia. The diuretic spironolactone
is a mineralocorticoid receptor antagonist
and is therefore first-line treatment.
Surgical resection of the diseased adrenal
gland is usually recommended.
Question 32. B) Phenoxybenzamine
Explanation: The clinical features and
investigation findings are consistent with
phaeochromocytoma. Hypertension results
from excessive secretion of
catecholamines (adrenaline/epinephrine
and noradrenaline/norepinephrine) from
the tumour. Initial antihypertensive
treatment is with the V-blocker,
phenoxybenzamine. If the V-blockade
induces a marked reflex tachycardia or if
there is persistent hypertension, then a _blocker can be added. A _-blocker must
not be given before an V-blocker, as
blockade of _2-receptors (which have a
vasodilatory action when activated) can
result in unopposed V-mediated
vasoconstriction and precipitate a
hypertensive crisis.
Question 33. D) Administration of
exogenous insulin
Explanation: Endogenous insulin is cosecreted with C-peptide (both are formed
from the cleavage of pro-insulin from the
pancreas). High insulin levels associated
with low C-peptide levels during
hypoglycaemia therefore indicate an
exogenous origin of the insulin. The
family history of diabetes in this patient
suggests that she may have access to a
relative's insulin at home. In insulinoma
and sulphonylurea ingestion, the
hyperinsulinaemia is endogenous and Cpeptide levels are therefore also elevated.
Hypoglycaemia in alcohol excess and
hypopituitarism is not due to increased
insulin secretion; insulin and C-peptide
levels are therefore low.
Question 34. D) 5-hydroxytryptamine
(5-HT)
Explanation: Carcinoid syndrome is
caused by ectopic production of the
vasoactive hormone 5-HT by a carcinoid
tumour. Clinical manifestations include
flushing, wheezing and diarrhoea, as well
as cardiac valvular abnormalities. The
most common site of carcinoid tumours is
the small bowel, but for carcinoid
syndrome to occur, the vasoactive
hormones must gain access to the systemic
circulation. Since hormones secreted into
194
the portal circulation are metabolised by
the liver, carcinoid syndrome usually
occurs only when such tumours have
spread to the liver or outside the GIT.
Question 35. C) Cranial diabetes
insipidus
Explanation: Diabetes insipidus is
characterised by the production of large
volumes of dilute urine. It is secondary to
deficient production/release of ADH by
the hypothalamus/posterior pituitary
(cranial diabetes insipidus) or to reduced
responsiveness of the renal tubules to
ADH (nephrogenic diabetes insipidus). In
healthy individuals, water deprivation
leads to increased ADH secretion. This
causes increased water retention by the
kidneys with the resultant formation of
concentrated urine (> 600 mOsm/kg) and
maintenance of normal plasma osmolality
(280-290 mOsm/kg). In diabetes insipidus,
the kidneys are unable to retain water
despite water deprivation. Plasma
therefore becomes concentrated (> 300
mOsm/kg) and the urine is not maximally
concentrated (i.e. it is < 600 mOsm/kg). In
cranial diabetes insipidus (ADH
deficiency) the urine does concentrate
after administration of the ADH analogue
DDAVP, but in nephrogenic diabetes
insipidus (ADH resistance) there is a
minimal response to DDAVP.
Question 36. A) Oral GTT.
Explanation: This patient has
acromegaly. It is caused by excessive
growth hormone (GH) secretion by a
pituitary adenoma. The diagnosis is
confirmed by measuring plasma GH levels
during an oral glucose tolerance test; in
normal subjects plasma GH suppresses to
< 2 mU/l, but fails to do so in patients with
acromegaly. It is important to evaluate the
other pituitary hormones (including
thyroid function tests) and to image the
pituitary (MRI scan); however, as in most
circumstances in endocrinology, scanning
is usually performed after the biochemical
diagnosis has been established. Insulin
tolerance tests may be used to diagnose
GH deficiency (not GH excess).
Chapter
20 DIABETES MELLITUS
Question 1. D) Decreased glycogenolysis
Explanation: Insulin is an anabolic
hormone, and its secretion increases in
response to a rise in blood glucose. Its
actions are to reduce blood glucose levels
and promote energy storage (therefore
only D is true), inhibit ketogenesis, and
increase fat and protein synthesis.
Question 2. E) Addison's disease
Explanation: Growth hormone,
catecholamines, corticosteroids and
glucagon are all counter-regulatory
hormones, as they respond to the stress of
hypoglycaemia and oppose the actions of
insulin. They may all therefore cause
diabetes when present in excess, e.g. in
acromegaly, phaeochromocytoma or
Cushing's syndrome. Addison's disease
involves immune destruction of the
adrenals, resulting in reduced
glucocorticoid production, and so blood
glucose levels tend to be low. In
haemochromatosis, pancreatic iron
overload can impair insulin secretion,
leading to diabetes.
Question 3. E) Concordance rates
between monozygotic twins are greater
than 90%
Explanation: Type 1 diabetes is mediated
by autoimmune destruction of the insulinproducing ß-cells in the pancreas.
Treatment with insulin is therefore
essential to prevent uncontrolled
hyperglycaemia and ketoacidosis. The
condition is thought to be triggered by
environmental factors (e.g. viral infection)
in genetically susceptible individuals.
However, concordance between
monozygotic twins is only 35% in type 1
diabetes, compared with rates approaching
100% in type 2 diabetes. Type 1 diabetes
is associated with other autoimmune
conditions, including pernicious anaemia,
195
Addison's disease and thyroid disease.
Question 4. C) Ketoacidosis is a
common complication
Explanation: Diabetic ketoacidosis
develops in type 1 diabetes because of
severe insulin deficiency, but is rarely a
feature of type 2 diabetes, as sufficient
insulin secretion to suppress lipolysis is
usually retained. Type 2 diabetes has a
much higher prevalence and is a major risk
factor for cardiovascular disease. Unlike
type 1 diabetes, it is often asymptomatic
and detected incidentally. One of the
characteristics of type 2 diabetes is insulin
resistance. The combination of type 2
diabetes, hypertension, hyperlipidaemia
and central obesity constitutes the
metabolic syndrome, also known as the
insulin resistance syndrome, which
strongly predisposes to ischaemic heart
disease.
Question 5. D) Explain to the patient
that she has diabetes mellitus
Explanation: The World Health
Organization (WHO) criteria for
diagnosing diabetes mellitus are shown in
the link below. C-peptide is the connecting
peptide which links the A and B chains of
insulin, and is secreted from the islet ßcells with insulin in equimolar
concentrations. It can be measured in the
assessment of hypoglycaemia to establish
whether excess insulin originates from an
exogenous or endogenous source and,
occasionally, to determine endogenous
insulin secretory reserve in a patient with
diabetes; however, it is not used to make
the diagnosis of diabetes.
Question 6. C) A low renal threshold for
glucose in an otherwise healthy
individual
Explanation: The most common cause of
glycosuria is a low renal threshold for
glucose, which results in glucose 'spilling
over' into the urine. This is most often
found in pregnancy and in young people.
In some healthy individuals there is a rapid
rise in blood glucose after meals, which
can exceed the renal threshold and lead to
transient glycosuria. Pyelonephritis can
lead to protein, blood, nitrites and
leucocytes in urine, but not typically
glucose.
Question 7. D) Measuring glycated
haemoglobin (HbA1C)
Explanation: Glycated haemoglobin
(HbA1C) is formed by the non-enzymatic
attachment of glucose to haemoglobin.
Measurement of HbA1C provides an
estimate of glycaemic control over the
lifespan of red blood cells. (Red cells have
a lifespan of 120 days, but the turnover of
the pool in the circulation means that
HbA1C reflects blood glucose over the
previous 8 weeks.) The target level is
usually 7% or less, as this reduces the risk
of developing microvascular
complications. Pre-prandial blood glucose
measurements are useful to patients at
home for monitoring glycaemic control
and adjusting insulin doses. Assessment of
urine glucose is of limited value since it
varies according to the renal threshold.
Question 8. A) Administration of
intravenous insulin and intravenous
saline
Explanation: In diabetic ketoacidosis
(DKA), severe insulin deficiency leads to
hyperglycaemia and the generation of
ketone bodies. The hyperglycaemia results
in glycosuria and an osmotic diuresis,
through which patients can become
severely dehydrated. The initial priorities
in managing DKA are therefore
administration of intravenous saline and
insulin.
196
Although serum potassium levels are often
initially high, patients are usually depleted
in total body potassium, and intravenous
infusion of potassium should be given
once potassium falls below 5.0 mmol/l.
Sodium bicarbonate is rarely needed, may
be dangerous and should be administered
only under expert supervision. Central
venous access may be required to assist
with fluid management, but is not the most
urgent step. Antibiotic therapy would be
required if there was evidence of overt
infection as the precipitating cause of the
DKA.
Question 9. B) Subcutaneous heparin
should be administered within the first
24 hours
Explanation: Hyperosmolar non-ketotic
hyperglycaemia (HONK) principally
affects patients with type 2 diabetes. It is
characterised by severe hyperglycaemia
and marked dehydration, but patients are
not acidotic because ketone production is
not increased. Smaller doses of insulin are
required than for treatment of diabetic
ketoacidosis. There is a high risk of
thromboembolic complications in HONK
due to the severe dehydration, and low
molecular weight heparin should therefore
be given.
Question 10. B) Kussmaul breathing
Explanation: Sweating and tachycardia
are stimulated by sympathetic activation in
hypoglycaemia. Confusion and altered
consciousness result from
neuroglycopenia. Kussmaul breathing (air
hunger) is a feature of diabetic
ketoacidosis as a response to the metabolic
acidosis.
Question 11. D) Oral carbohydrate
Explanation: Although the accuracy of
blood glucose strip testing kits is variable,
this patient has clinical features and a
glucose reading consistent with
hypoglycaemia, so prompt treatment is
required. If a patient is conscious and able
to swallow, then oral carbohydrate is the
treatment of choice. If not, then IV
dextrose or IM glucagon should be
administered. Laboratory samples should
be obtained (for glucose, insulin, Cpeptide, toxicology drug screen) before
treatment in patients with unexplained
suspected 'spontaneous' hypoglycaemia, as
this avoids potentially complex attempts to
reproduce the hypoglycaemia later.
However, hypoglycaemia in diabetic
patients who are treated with insulin or
with a sulphonylurea is probably related to
their treatment.
Question 12. E) Stop metformin and
commence intravenous insulin
Explanation: Studies suggest that strict
glycaemic control in the peri-infarct period
improves long-term prognosis after an MI.
This is usually achieved with insulin, often
in the form of an intravenous infusion
(sliding scale). The study most often cited
is the DIGAMI study (diabetes mellitus,
insulin glucose infusion in acute
myocardial infarction), which showed a
reduction in mortality of 25% in patients
treated with an insulin infusion, compared
with standard treatment over a follow-up
period of 3.5 years (though this has not
been confirmed in subsequent studies).
Oral anti-diabetic agents are usually
discontinued until the recovery period
after MI. Metformin in particular should
be withheld because of the small risk of
lactic acidosis in the event of impaired
systemic perfusion.
197
Question 13. C) Insulin alone
Explanation: The development of
diabetes during pregnancy is associated
with increased maternal and fetal
morbidity and mortality. Hyperglycaemia
can result in teratogenic effects and
macrosomia. Strict blood glucose control
with insulin is therefore important. Oral
anti-diabetic agents may be harmful to the
fetus and should not be given during
pregnancy.
Question 14. D) Start an intravenous
infusion of dextrose and insulin in place
of the patient's usual therapy
Explanation: Adequate control of
hyperglycaemia is important in the perioperative period. For type 2 diabetic
patients undergoing minor operations, it is
reasonable to place them first on the
operating list and to omit their morning
oral anti-diabetic agent or insulin until
after the operation. However, for type 2
diabetic patients undergoing major
surgery, and for all type 1 diabetic
patients, blood glucose should be
controlled by means of an intravenous
insulin infusion.
Question 15. B) Metformin
Explanation: Sulphonylureas (e.g.
gliclazide) act by stimulating endogenous
insulin secretion. A major side-effect of
this class of drug is weight gain, and so
they would not generally be considered
first-line treatment in obese patients.
Metformin (a biguanide) works by
increasing insulin sensitivity and does not
cause weight gain, so is a better choice in
this patient. Thiazolidinediones (e.g.
rosiglitazone, pioglitazone) also act by
improving insulin sensitivity, but are not
usually prescribed as first-line treatment.
Insulin treatment is sometimes required in
type 2 diabetes, but tends to be initiated
when glycaemic control with oral agents is
suboptimal.
Question 16. C) They are particularly
useful in diabetic patients with left
ventricular dysfunction
Explanation: The thiazolidinedione class
of drugs, also known as glitazones or
TZDs, includes rosiglitazone and
pioglitazone. They act by binding to a
nuclear receptor called peroxisome
proliferator-activated receptor-W (PPAR-W),
particularly in fat cells. This results in
altered expression of genes involved in
metabolism and thereby enhances insulin
sensitivity. Insulin secretion itself is not
affected. They are useful in obese patients
with type 2 diabetes, in whom insulin
resistance is often severe. Although they
do cause weight gain, this is usually in
subcutaneous rather than intra-abdominal
adipose tissue and is therefore thought to
be metabolically 'benign'. They have few
side-effects, but can cause salt and water
retention, and are therefore contraindicated
in heart failure.
Question 17. D)
Glipizide N hypoglycaemia
Explanation: Sulphonylureas (e.g.
gliclazide, glipizide) stimulate insulin
secretion and hence cause weight gain and
can induce hypoglycaemia. Metformin
increases insulin sensitivity and does not
cause hypoglycaemia, but frequently
causes nausea and diarrhoea. It is also
contraindicated in patients with renal
impairment, liver dysfunction,
symptomatic heart failure and sepsis
because of the risk of lactic acidosis.
Question 18. A) Ischaemic heart disease
Explanation: Macrovascular disease is
the major cause of mortality in diabetes,
particularly myocardial infarction and
stroke. Macrovascular disease also causes
significant morbidity in the form of
coronary heart disease, cerebrovascular
disease and peripheral vascular disease.
Microvascular complications include
diabetic retinopathy, nephropathy and
neuropathy. Their incidence is related to
poor glycaemic control and causes serious
morbidity but is not the major cause of
death.
198
Question 19. C) Flame haemorrhages
Explanation: Flame haemorrhages are a
feature of hypertensive retinopathy but are
not usually a feature of diabetic
retinopathy. Hard exudates (due to leakage
from abnormal capillaries), blot and dot
haemorrhages, and cotton wool spots
(caused by areas of retinal ischaemia) are
found in both diabetic and hypertensive
retinopathy. Microaneuryms and venous
beading occur in diabetic retinopathy.
Question 20. D) Venous beading with
cotton wool spots
Explanation: Microaneurysms, dot
haemorrhages and hard exudates are
features of background diabetic
retinopathy. The finding of hard exudates
near the macula indicates diabetic
maculopathy, which is sight-threatening.
Venous beading, cotton wool spots and
intra-retinal microvascular abnormalities
(IRMAs) occur in pre-proliferative
disease. New vessel formation
(neovascularisation) is the key feature of
proliferative diabetic retinopathy. Rupture
of these vessels can result in pre-retinal
haemorrhage. Papilloedema is a feature of
grade IV hypertensive retinopathy but may
also be seen in other conditions, including
raised intracranial pressure. The
classification of retinopathy is detailed in
the link below.
Question 21. C) Regular follow-up in
the diabetic clinic but no referral to
ophthalmology
Explanation: Background retinopathy
requires regular fundoscopy to identify
progression but is not in itself an
indication for ophthalmology referral.
Patients with pre-proliferative and
proliferative retinopathy should be
referred urgently to ophthalmology for
further assessment and consideration of
retinal laser photocoagulation. Progression
of retinopathy is related to poor glycaemic
control and elevated blood pressure, and
so anti-diabetic agents and
antihypertensives should not be stopped.
Question 22. C) Ramipril
Explanation: Diabetic nephropathy is a
major cause of end-stage renal failure. Its
development is related to poor glycaemic
control. The presence of microalbuminuria
heralds the development of overt
nephropathy. The risk of progression can
be reduced by good glycaemic control and
aggressive treatment of elevated blood
pressure. Angiotensin-converting enzyme
(ACE) inhibitors provide greater benefit
from equal blood pressure lowering than
other antihypertensive agents. They reduce
intra-glomerular pressure and urinary
protein excretion and are therefore the
preferred agents in patients with
microalbuminuria.
Question 23. E) It is typically associated
with painful foot ulcers
Explanation: Like all diabetic
microvascular complications, the
development of neuropathy can be
prevented or delayed by good glycaemic
control. Sensory, motor and autonomic
nerves can all be affected, but patients are
often asymptomatic, particularly in the
early stages. Sensory neuropathy
classically gives rises to a 'glove and
199
stocking' distribution of sensory loss
distally. Motor involvement can cause
progressive proximal muscle weakness,
commonly accompanied by severe pain.
Motor and sensory function of individual
cranial and peripheral nerves can also be
affected (mononeuropathy and
mononeuritis multiplex). Peripheral
sensory neuropathy can ultimately result in
grossly deforming neuroarthropathy of the
feet (Charcot joint) due to loss of pain
sensation. Although neuropathy can give
rise to foot ulcers, these are typically
painless (unlike ischaemic ulcers).
Question 24. D) Gastroparesis
Explanation: Autonomic neuropathy can
affect sympathetic or parasympathetic
nerves. Gastroparesis in patients being
treated with insulin can predispose to poor
glycaemic control and hypoglycaemia,
because of unpredictable matching
between carbohydrate absorption and
plasma insulin concentrations. Fast-acting
insulin analogues should be avoided.
Agents that promote gastric emptying,
such as metoclopramide, may be helpful.
Chapter
21 ALIMENTARY TRACT AND
PANCREATIC DISEASE
Question 1. E) Rounded mass
Explanation: The other findings are all
characteristic of an enlarged spleen.
Question 2. A) Trypsin
Explanation: Amylase is involved in
carbohydrate digestion. Lipase cleaves
long chain triglycerides, yielding fatty
acids and monoglycerides.
Cholecystokinin is a hormone with
important effects on gut motility. Pepsin is
active in the stomach, not small bowel,
where it plays a modest role in protein
digestion.
Question 3. C) Glycogen
Explanation: More on Carbohydrate
digestion and absorption
Question 4. D) Increased gastric acid
secretion
Explanation: In addition to the other
factors listed above, CCK suppresses
gastric acid secretion.
Question 5. D) Oesophageal carcinoma
Explanation: The barium swallow shows
a long irregular stricture, typical of an
oesophageal carcinoma. None of the other
options would produce this appearance.
Question 6. A) Faecal elastase
Explanation: Elastase is a proteolytic
enzyme produced by the pancreas. Levels
are reduced in pancreatic exocrine failure,
though it has low sensitivity for detecting
mild disease.Abdominal CT is useful for
assessing pancreatic size and structure, but
not function. Three-day faecal fat is a test
for fat malabsorption. Fasting blood
glucose is a test of pancreatic endocrine
function. The lactose hydrogen breath test
is used in the detection of lactose
intolerance.
200
Question 7. B) Helicobacter pylori
infection
Explanation: Urea breath testing is, in
most cases, the best test for detecting H.
pylori infection as it is accurate, simple
and non-invasive. Bacterial overgrowth
and lactose intolerance may be detected by
the glucose hydrogen breath test and
lactose hydrogen breath tests respectively.
Fat malabsorption can be diagnosed by
either 3-day faecal fat assessment or the
14
C-triolein breath test. Tests for coeliac
disease include coeliac antibodies and
small bowel (usually duodenal) biopsy.
Question 8. E) Achalasia
Explanation: Upper gastrointestinal
endoscopy is, in general, the investigation
of choice in dysphagia to exclude
structural causes and allow biopsy with or
without dilatation of any suspicious
strictures. However, oesophageal
manometry is useful in achalasia where
the characteristic pattern of high-pressure,
non-relaxing lower oesophageal sphincter
with poorly contractile body of
oesophagus confirms the diagnosis.
Question 9. E) Associated difficulty in
swallowing
Explanation: Dyspepsia is extremely
prevalent and usually does not require
investigation, especially in younger
patients. In general, upper gastrointestinal
endoscopy should be reserved for patients
over 55 years old, younger patients
unresponsive to empirical treatment or
those with 'alarm' features, such as
dysphagia, which may point to serious
underlying pathology.
Question 10. C) Atenolol
Explanation: Many antibiotics, analgesics
and cytotoxins may lead to vomiting. Sideeffects of atenolol include tiredness,
impotence and nightmares, but not
vomiting.
Question 11. B) Mallory-Weiss tear as
the cause of bleeding
Explanation: Mortality risk in patients
presenting with acute upper
gastrointestinal bleed is defined by the
'Rockall risk score' which takes into
account age, features of shock,
comorbidity, diagnosis and endoscopic
findings. Mallory-Weiss tear is the
diagnosis associated with the most
favourable outcome.
Question12. E) Anal fissure
Explanation: Anal fissure does not cause
severe acute lower gastrointestinal
bleeding but rather small amounts of fresh
rectal bleeding associated with pain during
defaecation.
Question 13. C) Blood and mucus in
stool
Explanation: A colonic aetiology is
suggested by cramping lower abdominal
pain, blood and mucus in stool, and highfrequency, low-volume stool, often with
tenesmus.
Question 14. D) Peripheral
neuropathy Vitamin C
Explanation: Vitamin C deficiency
produces bleeding gums, poor wound
healing and perifollicular or petechial
bruising (scurvy). Peripheral neuropathy
may be due to vitamin B12 deficiency.
Question 15. E) Verapamil
Explanation: Constipation is a side-effect
of various calcium channel blockers but
particularly verapamil. Diarrhoea is a
common side-effect of macrolide
antibiotics, especially erythromycin.
Likewise, metformin is far more likely to
cause diarrhoea than constipation. Sideeffects of digoxin include nausea,
vomiting, arrhythmia and disturbed vision,
but not constipation.
201
Orlistat is a lipase inhibitor that reduces
absorption of dietary fat and is used in the
management of obesity. Side-effects
include liquid or oily stools and faecal
urgency rather than constipation.
Question 16. E) Psoriasis
Explanation: See list of Causes of oral
ulceration
Question17. C) Weight loss
Explanation: Weight gain may precipitate
or aggravate symptoms by increasing
intra-abdominal pressure, whereas weight
loss may improve symptoms.
Question18. D) Patients with the
condition should undergo regular
endoscopic surveillance with biopsies
Explanation: Barrett's oesophagus refers
to metaplastic rather than neoplastic
change. Although a major risk factor for
oesophageal adenocarcinoma, the vast
majority of patients do not go on to
develop this condition. Neither potent acid
suppression nor antireflux surgery has
been shown to induce regression or even
stop progression of Barrett's oesophagus.
Regular endoscopic surveillance is
recommended.
Question 19. D) Recurrence of
symptoms following cessation of
medical treatment is common
Explanation: The patient is young, is
otherwise well, and has a typical history of
GORD and no worrying features. He can
therefore be treated empirically without
need for further investigation. A history of
weight gain prior to onset of symptoms is
common in GORD and would lend
support to the diagnosis. PPIs are superior
to H2-receptor antagonists in both
relieving symptoms and healing
oesophagitis (see the evidence-based
medicine box in the link below).
Recurrence of symptoms after stopping
acid-suppressing therapy is common and
some patients require long-term low-dose
maintenance therapy. Antireflux surgery is
highly effective in alleviating symptoms.
Question 20. B) Achalasia
Explanation: The barium swallow shows
the characteristic appearance of a dilated
barium-filled oesophagus with fluid level
and distal tapering and a closed lower
oesophageal sphincter. Clues in the history
include the long duration of symptoms, the
easing of swallowing difficulties by
drinking liquids, and the intermittent
episodes of severe chest pain which are
due to oesophageal spasm. Diffuse
oesophageal spasm produces transient
rather than slowly progressive dysphagia.
Myasthenia gravis, as with other
neuromuscular causes of dysphagia, tends
to be worse for liquids rather than solids.
In systemic sclerosis there is usually a
history of severe heartburn. An endoscopy
may still be necessary to exclude
oesophageal carcinoma.
Question 21. D) The presence of
hoarseness suggests mediastinal
invasion
Explanation: The overall 5-year survival
rate is very poor at 6-9% and even after
'potentially curative' surgery remains only
30%. Endoscopic ultrasound is the most
sensitive modality for staging, as CT tends
to understage tumours. Dysphagia is
classically persistent and progressive and
is initially worse for solids. Pain is often
absent due to destruction of mucosal
innervation by the tumour. Endoscopically
directed tumour ablation using laser
therapy or stent insertion is the major
method of improving swallowing.
Mediastinal invasion with involvement of
the recurrent laryngeal nerve may cause
hoarseness.
Question 22. A) Chronic peptic ulcer
Explanation: Of the possibilities above,
chronic peptic ulcer fits best with the
pattern of symptoms. The three
characteristics of ulcer pain are the
recurrent, episodic nature, a relationship to
food and localisation to the epigastrium.
Occasional vomiting occurs in about 40%.
It is worth noting, though, that the history
is actually a poor predictor of the presence
of an ulcer.
202
The pain of chronic pancreatitis and
mesenteric ischaemia tends to be
precipitated rather than relieved by eating,
as does the pain of biliary colic,
particularly with fatty foods. It would be
unusual for Crohn's disease to produce
pain well localised to the epigastrium.
Question 23. D) The patient should be
given specific advice on dietary
restriction
Explanation: Most peptic ulcers are now
cured by H. pylori eradication and acidsuppressing therapy with the result that
elective surgery for peptic ulcer disease
has become a rare event. No special
dietary advice is required, although
patients may themselves wish to avoid
certain foods they feel aggravate
symptoms. If failure to eradicate H. pylori
infection occurs with standard triple
therapy, the patient should first be asked
about compliance with treatment and then
offered second-line therapy.
Question 24. C) It exclusively colonises
gastric-type epithelium
Explanation: H. pylori is a Gramnegative spiral-shaped rod. The enzyme
'urease' produces ammonia from urea,
thereby raising the surrounding pH and
making the environment less hostile for
the bacterium. It is true that H. pylori only
colonises gastric-type epithelium and is,
therefore, only found in the duodenum in
association with patches of gastric
metaplasia. CagA is one of several wellrecognised virulence factors (see Fig.
22.32 in the link below). Colonisation is
associated with depletion of somatostatin
(from D cells) but stimulates release of
gastrin (from G cells).
Question 25. C) Around 40% of patients
with duodenal ulcer are infected with H.
pylori
Explanation: H. pylori infection may be
responsible for 60-70% of cases of gastric
carcinoma. Around 90% of duodenal ulcer
patients and 70% of gastric ulcer patients
are infected. The development of a lowgrade lymphoma known as a 'MALToma'
is closely associated with H. pylori
infection, and superficial MALTomas may
be cured by H. pylori eradication. Despite
all of the above, only a minority of H.
pylori-infected patients develop clinical
disease.
Question 26. A) Weight gain
Explanation: Weight loss rather than
weight gain is common. The usual cause is
reduced dietary intake due to early satiety
from a small gastric remnant. Both
diarrhoea and anaemia may be
multifactorial. Rapid gastric emptying of
food of high osmotic potential may
produce large fluid shifts into the small
intestine, provoking autonomic symptoms.
This is known as 'dumping syndrome'.
Question 27. C) Zollinger-Ellison
syndrome
Explanation: In Zollinger-Ellison
syndrome there is severe peptic ulceration
from gastric acid hypersecretion due to a
gastrin-producing non-ß-cell islet tumour
of the pancreas ('gastrinoma'). Ulcers are
often multiple and refractory to standard
therapy, and may occur in unusual places
such as oesophagus or duodenum. It
comprises part of the MEN type 1
syndrome. Inactivation of pancreatic
enzymes and bile salts by increased acidity
in the small intestine can result in
diarrhoea (seen in more than one-third of
patients) and steatorrhoea. High-dose
proton pump inhibitor therapy heals
ulcers, alleviates diarrhoea and has largely
removed the need for total gastrectomy.
203
Question 28. B) Zollinger-Ellison
syndrome
Explanation: A reduction in the acidity of
the stomach (hypochlorhydria or
achlorhydria) appears to increase gastric
cancer risk, perhaps by permitting
colonisation of the stomach with nitritereducing bacteria which form carcinogenic
N-nitroso-compounds from nitrates.
Autoimmune chronic gastritis and H.
pylori infection may both lead to
achlorhydria, unlike Zollinger-Ellison
syndrome, which markedly increases
gastric acidity. (Although H. pylori
infection normally results in normal or
increased acid secretion, a proportion of
infected individuals become
hypochlorhydric or achlorhydric.)
Question 29. C) Conn's syndrome
Explanation: See list of Disease
associations of coeliac disease
Question 30. E) Mesenteric ischaemia
Explanation: The most common cause of
subtotal villous atrophy in the UK is
coeliac disease but there are a number of
other important causes.
Question 31. E) There is an increased
risk of T-cell lymphoma
Explanation: Patients are intolerant of
wheat, rye, barley and, to a lesser extent,
oats, but not rice, maize or potatoes. Peak
onset is in infancy and early childhood; in
adults the highest incidence occurs in the
40-59 age group. Around 50% of patients
are asymptomatic and many remain
undiagnosed. Metabolic bone disease is
less common in patients who stick strictly
to a gluten-free diet. There is an increased
risk of T-cell lymphoma as well as small
bowel carcinoma and squamous carcinoma
of the oesophagus, although the absolute
risk of developing these malignancies is
very low.
Question 32. E) Serum amylase
Explanation: The above account is
classical of acute pancreatitis. Pain
radiates to the back in 65% of cases;
guarding and rebound tenderness are
typically absent in the early stages as the
inflammation is retroperitoneal. A
markedly elevated serum amylase often
confirms the diagnosis, although in
difficult cases, ultrasound or CT can help
by demonstrating evidence of pancreatic
swelling. Abdominal and erect chest Xrays may exclude other conditions such as
intestinal obstruction or perforated viscus
and an ECG should be performed to
exclude atypical presentation of
myocardial infarction. C-reactive protein
is not helpful diagnostically but is a useful
indicator of severity and prognosis.
Question 36. D) Recurrent
hypoglycaemia
Explanation: Hyperglycaemia, due to the
development of diabetes mellitus, rather
than hypoglycaemia is a common feature
of chronic pancreatitis.
Question 33. C) Hypocalcaemia
Explanation: Hypercalcaemia not
hypocalcaemia is a rare cause of acute
pancreatitis. By far the two most common
aetiologies are alcohol and gallstones.
Question 38. D) The liver is a common
site for metastatic deposits
Explanation: Pancreatic carcinoma has a
dismal prognosis; only 15% of tumours
are amenable to curative resection and,
even in patients who undergo complete
resection, 5-year survival is around 20%.
Around two-thirds of tumours arise from
the head of the pancreas; these frequently
involve the common bile duct, resulting in
obstructive jaundice. Coeliac plexus
neurolysis may be useful in relieving pain,
which often proves extremely difficult to
control with other measures. Ampullary
carcinomas behave less aggressively than
pancreatic carcinomas and have a more
favourable outlook.
Question 34. D) Amylase 1000
U/l (normal range < 100 U/l)
Explanation: Although an elevated serum
amylase is useful in diagnosing acute
pancreatitis, it has no prognostic value.
The other parameters listed are included in
the Glasgow criteria of adverse prognostic
factors.
Question 35. B) Enteral feeding should
be started at an early stage in patients
with severe pancreatitis
Explanation: Hypocalcaemia need only
be corrected if tetany occurs.
Thromboprophylaxis is advised. The
greatest benefit from emergency ERCP
occurs in patients who have ascending
cholangitis (see EBM Box 22.58 in the
link below). Opiate analgesia is required in
nearly all cases. Nutritional support,
preferably by the enteral route, forms an
important part of the management of acute
pancreatitis.
204
Question 37. D) Carcinoma of pancreas
Explanation: This is a fairly typical
presentation of pancreatic carcinoma
(apart from the vanishingly rare sign of
palpable gallbladder). The diagnosis will
be confirmed with abdominal ultrasound
or CT. According to 'Courvoisier's law', a
palpable gallbladder in a jaundiced patient
is unlikely to be due to gallstones, and is
usually the result of distal biliary
obstruction by a carcinoma of the head of
pancreas.
Question39. E) Inflammation limited to
the mucosa
Explanation: There are several important
pathological differences between
ulcerative colitis (UC) and Crohn's disease
(CD), including but not confined to the
following:
• UC only involves the colon, while
Crohn's disease can involve any part of the
gastrointestinal tract from mouth to anus.
• In UC inflammation is confluent and
more severe distally (thus it invariably
involves the rectum but may spread
proximally to involve the remainder of the
colon). In CD changes are patchy with
areas of inflammation interrupted by
islands of normal mucosa. (This may
produce the characteristic 'skip lesion'.)
• In UC the inflammatory process is
superficial, confined to the mucosa and
sparing deeper layers of the bowel wall,
while in CD inflammation is deep and
seen through all layers of the bowel wall.
(Deep ulcers may penetrate through the
bowel wall to initiate fistulae.)
Question 40. B) Cigarette smoking
Explanation: Ulcerative colitis is more
common in non-smokers and, in fact,
cessation of smoking can provoke a
relapse of symptoms. Emotional stress,
intercurrent illness, non-steroidal antiinflammatory drugs (NSAIDs) and
antibiotics are all well-recognised factors
which may precipitate flares.
Question 41. D) Serum albumin
Explanation: Serum albumin is a marker
of disease severity in ulcerative colitis but
does not contribute to the diagnosis. It is
suppressed in any condition producing an
acute phase response.
Question 42. B) Stool volume 200 g/24
hrs
Explanation: Stool volume > 400 g/24 hrs
suggests severe disease. These parameters
are utilised in clinical practice.
205
Question 43. B) The patient should be
treated with intravenous corticosteroids
Explanation: Intravenous corticosteroids
are given as a constant infusion in the
treatment of severe ulcerative colitis.
Question 44. C) The patient should be
referred for urgent colectomy
Explanation: The X-ray shows a grossly
dilated colon due to severe ulcerative
colitis. Toxic megacolon occurs most
commonly during the first attack of colitis
and is associated with a high risk of
perforation. It is, therefore, an indication
for colectomy.
Question 45. E) Diarrhoea in ulcerative
colitis may be due to enteroenteric
fistulae
Explanation: Fistulous connections
between loops of affected bowel
(enteroenteric), or between bowel and
bladder (enterovesical) or vagina
(enterovaginal) are specific complications
of Crohn's disease and do not occur in
ulcerative colitis. Patients with extensive
active colitis of more than 8 years'
duration are at increased risk of colon
cancer and should, therefore, have regular
colonoscopic surveillance.
Question 46. B) Primary sclerosing
cholangitis
Explanation: Primary sclerosing
cholangitis and cholangiocarcinoma are
both more common in ulcerative colitis
but appear to be unrelated to intestinal
disease activity. The other complications
listed tend to be more of a problem during
active bowel disease.
Question 47. C) Corticosteroids are
preferred to methotrexate for
maintaining remission
Explanation: Chronic corticosteroid
treatment is avoided due to the high
incidence of complications with long-term
use and poor efficacy in preventing
relapse. All of the other statements are true
and are useful learning points.
Azathioprine and methotrexate are both
used in maintenance of remission.
Infliximab is highly effective in inducing
remission in active Crohn's but relapse
commonly occurs around 12 weeks after
treatment. It should therefore be given in
combination with either azathioprine or
methotrexate. Surgery is not curative in
Crohn's disease and repeated surgery may
lead to the development of short bowel
syndrome. Cigarette smoking is more
important than any drug treatment in
maintaining remission.
Question 48. C) Symptoms disturbing
sleep
Explanation: Nocturnal symptoms are
uncommon in IBS and pain that wakens a
patient from sleep is often a useful pointer
to organic disease. Other features that
would raise doubt as to the diagnosis
include rectal bleeding and weight loss.
Question 49. D) Reassurance alone may
lead to resolution of symptoms
Explanation: Anxiety over the possibility
of serious organic disease, particularly
cancer, is often a major contributing factor
to symptoms in IBS and many patients
respond to simple explanation and
reassurance. Such patients have a far better
long-term outlook than those who fail to
respond.
206
Question 50. B) Acute small bowel
ischaemia
Explanation: The rapidity of onset,
history of vascular disease and atrial
fibrillation (not on warfarin), paucity of
abdominal findings despite severe
symptoms and metabolic acidosis all point
to acute small bowel ischaemia. Given her
history of atrial fibrillation, a likely
aetiology would be a thromboembolism
from the heart.
Question 51. E) Stool analysis for
Clostridium difficile toxin
Explanation: Cl. difficile is the most
likely cause of this patient's diarrhoea. It is
a very common cause of diarrhoea in
hospital inpatients, particularly those > 65
years with comorbid disease who have had
recent broad-spectrum antibiotic therapy.
Legionella pneumonia can be associated
with gastrointestinal upset but the timing
certainly favours Cl. difficile infection in
this case.
Question 52. D) Polyps with a villous
architecture carry a higher risk of
malignant change than those with
tubular architecture
Explanation: Nearly all forms of
colorectal carcinoma develop from
adenomatous polyps, usually over a period
of 5-10 years, although certain features
such as increased size and villous
architecture increase the risk for malignant
change. Polyps are usually asymptomatic
and are often found incidentally during
colonoscopy; when discovered, they
should be removed whenever possible to
reduce the risk of developing colorectal
cancer. Peutz-Jeghers syndrome is
characterised by the presence of nonneoplastic hamartomatous polyps in the
colon and small bowel (although it is
associated with increased risk of certain
malignancies, e.g. breast, ovary, colon).
Question 53. C) High dietary calcium
Explanation: Dietary calcium decreases
the risk of developing colorectal cancer as
it binds and precipitates faecal bile acids.
Question 54.D) Colonoscopy
Explanation: The combination of occult
gastrointestinal bleeding, weight loss and a
palpable right iliac fossa mass in a patient
of this age group should lead to strong
suspicion of colonic (caecal) carcinoma
and should be investigated as a matter of
207
urgency by colonoscopy. Colonoscopy is
preferable to barium enema in most
instances as it has better sensitivity and
specificity and allows biopsy of lesions
and polypectomy. If the diagnosis is
confirmed then a CT scan may be useful
for detecting hepatic metastases. CEA is
neither sensitive nor specific for
diagnosing colorectal cancer, but in those
patients with a raised CEA who go on to
have resection of the tumour, it may help
in follow-up to detect early recurrences
Chapter
22 LIVER AND BILIARY TRACT
DISEASE
Question 1. B) Production of vitamin K
Explanation: Vitamins are, by definition,
not synthesised in the human body so an
adequate dietary intake and
gastrointestinal absorption of vitamin K is
essential. Vitamin K is a fat-soluble
vitamin and absorption is impaired in
obstructive jaundice, resulting in a
prolonged prothrombin time which is
corrected by vitamin K administration.
Question 2. E) It is the primary site of
lipolysis in the liver
Explanation: Below is a quick reminder
of the structure of the hepatic acinus.
Question 3. C) Phenytoin
Explanation: Phenytoin is a microsomal
enzyme-inducing drug; all of this type of
drug may cause an isolated increase in the
microsomal enzyme GGT. This is a
reflection of hepatic enzyme induction and
does not necessitate any change to therapy.
A list of enzyme-inducing drugs can be
found in the link below. It is important to
learn them as they have interactions with
other drugs, such as reducing the
effectiveness of the oral contraceptive pill
and increasing the toxicity of paracetamol
in overdose.
Question 4. A) Viral hepatitis
Explanation: This is the classic picture of
hepatocellular jaundice.
Question 5. E) Raised reticulocyte count
Explanation: Part of the bone marrow
response to excessive red cell destruction
is premature release of reticulocytes,
resulting in a reticulocytosis. Nucleated
red cell precursors may also appear in the
blood. Bilirubinuria and pale stools both
suggest cholestatic jaundice. As discussed
208
in the previous question, a predominant
rise in ALT suggests a hepatocellular
cause. Spider naevi are a pointer towards
chronic liver disease.
Question 6. D) Factor IX
Explanation: The vitamin K-dependent
clotting factors are II, VII, IX and X. Noone has ever devised a decent mnemonic
for this fact, so you just have to remember
it. Here they are again: 2, 7, 9 and 10.
(1972)
Question 7. E) Prothrombin time (PT)
Explanation: Albumin, fibrinogen and
most coagulation factors are synthesised in
the liver so all of the above tests are, to
some extent, dependent on hepatic
synthetic function, with the exception of
urea which is a by-product of protein
metabolism. The prothrombin time
changes most quickly in response to an
acute liver insult, because of the short
half-life of the clotting factors on which it
depends. Albumin has a much longer halflife and hypoalbuminaemia is a feature of
chronic liver disease.
Question 8. A) Chronic obstructive
pulmonary disease (COPD) with forced
expiratory volume in 1 second
(FEV1)/forced vital capacity (FVC) of
37%
Explanation: The conditions required for
a safe liver biopsy are included in the link
below. There is a risk of causing
pneumothorax if the pleura is punctured
and, in a patient with severe COPD, this is
not only more likely but also potentially
catastrophic.
Question 9. D) Abdominal ultrasound
Explanation: The LFTs show a
cholestatic picture. The most useful initial
investigation is abdominal ultrasound,
particularly to detect biliary obstruction.
Should more detailed imaging of the
biliary tree prove necessary, then either
ERCP or magnetic resonance
cholangiopancreatography (MRCP) may
be helpful. MRCP (followed if necessary
by therapeutic ERCP) is the diagnostic test
of choice, as it carries a lower risk of
complications than ERCP. A very useful
algorithm for the investigation of patients
with jaundice is provided in the link
below.
Question 10. B) Primary biliary
cirrhosis (PBC) Antimitochondrial
antibody (AMA)
Explanation: This is difficult to
remember, but genuinely useful because
AMA has high sensitivity for PBC, being
present in over 95% of cases.
Question 11. B) Cholestatic jaundice
Explanation: Cholestatic jaundice is the
only option here that explains both yellow
sclerae and dark urine. Conjugated
bilirubin from the liver enters the blood
because of a failure of bile flow. As
conjugated bilirubin (unlike unconjugated
bilirubin) is water-soluble, it is filtered by
the kidneys and appears in the urine. More
information on cholestatic jaundice,
including causes and clinical features, is
provided in the link below. Carotenaemia,
caused by eating too much carotene, is
almost always benign and causes
yellowing of the skin but not the sclera.
Gilbert's syndrome describes a congenital
impairment of glucuronyl transferase, that
leads to reduced hepatic uptake of
bilirubin from the blood. This therefore
causes unconjugated hyperbilirubinaemia,
so the sclerae are yellow but the urine is
not dark. In contrast, rhabdomyolysis
causes large amounts of myoglobin to
enter the urine, which can make the urine
appear black but does not cause jaundice.
Dehydration results in highly concentrated
urine but does not cause jaundice.
209
Question 12. E) Ascitic fluid white cell
count
Explanation: This is a classic presentation
of spontaneous bacterial peritonitis, a
common and life-threatening complication
of cirrhosis.
Question 13. B) Spironolactone
Explanation: Aldosterone excess, caused
by impaired hepatic steroid metabolism, is
a key factor in the pathogenesis of ascites
in chronic liver disease (explained in the
link below). Spironolactone is an
aldosterone antagonist, which makes it the
best choice to prevent sodium retention in
cirrhotic patients. Furosemide (a loop
diuretic) is sometimes added to
spironolactone to further promote sodium
excretion in the urine.
Bendroflumethiazide (a thiazide diuretic)
is not often used to treat ascites because
better drugs are available. Vasopressin is a
potent vasoconstrictor and powerfully
promotes water retention. It is used in the
management of hepatorenal syndrome.
Digoxin is not useful in the management
of ascites.
Question 14. A) Prothrombin time (PT)
> 100 secs
Explanation: PT is a better predictor of
poor outcome than liver function tests, and
is used in standard criteria for determining
the need for liver transplant. The following
two prognostic factors (see the link below)
have been shown to confer a > 90%
mortality in acute liver failure secondary
to paracetamol overdose:
• H+ > 50 nmol/l (pH < 7.3)
• Creatinine > 300 µmol/l with PT > 100
secs and grade 3 or 4 encephalopathy.
Question 15. C) May be balloted
Explanation: Distinguishing a grossly
enlarged kidney (for example, in
polycystic kidney disease) from
splenomegaly can be tricky. The correct
technique for palpation of the liver and
spleen is shown in the link below.
Question 16. C) Pruritus is a more
common presenting feature than
jaundice
Explanation: Primary biliary cirrhosis is
more common in women by a factor of 9.
Pruritus is the most common presenting
complaint and may precede jaundice by
years. Positive antinuclear antibodies are
found in only 15% of cases, whereas
antimitochondrial antibodies are of
considerable diagnostic value, present in
over 95% of patients. Immunosuppressive
drugs are not effective, and treatment
mainly palliates symptoms until transplant
becomes necessary. Although 30% of
patients will exhibit disease recurrence in
a transplanted liver, this takes years to
develop and is not a contraindication to
transplant.
Question 17. D) Terlipressin
Explanation: Terlipressin lowers the
portal pressure and is the drug of choice in
this scenario. The somatostatin analogue,
octreotide, is also useful. Noradrenaline
(norepinephrine) and dopamine
predominantly cause peripheral
vasoconstriction. However, in a patient
dying from haemorrhage, fluid
replacement, rather than vasoconstriction,
is the best method to correct hypotension.
Activated protein C is contraindicated in
haemorrhage.
Question 18. D) Hepatitis D
Explanation: Hepatitis D is an incomplete
virus and cannot cause infection without
concurrent infection with hepatitis B.
Question 19. B) It may be spread by the
faecal-oral route
Explanation: Hepatitis A is not usually
spread through blood or conventional
sexual contact, and, unlike hepatitis B and
C, does not induce a chronic carrier state.
A vaccine is available, and immune serum
globulin may be useful in the management
of outbreaks and immunocompromised or
pregnant patients. Anti-HAV antibodies of
IgM type may be useful diagnostically.
210
Question 20. E) It may cause cirrhosis
Explanation: Hepatitis B is commonly
transmitted through blood or sexual
contact. The most common route of
transmission world-wide is vertical during
childbirth; this route of infection carries a
much higher risk of chronic infection (see
the link below), which may ultimately lead
to cirrhosis and hepatocellular carcinoma.
A vaccine is given to all health-care staff
in the UK.
Question 21. E) Anti-HBc IgG and
HBsAb
Explanation: This is difficult but
important to understand. Both the natural
history of infection and the serological
tests are explained in the link below. A
few things are particularly important to
commit to memory: a vaccinated patient
will only have antibody to the surface
protein (content of vaccine) but a patient
who is immune (previously exposed and
cleared) will have antibodies to the whole
virus, i.e. core and surface antibodies.
Note that HbsAg is present in chronic
infection but, likewise, appears in acute
infection; acute infection can be
differentiated from chronic infection by
the presence of anti-HBc IgM.
Question 22. C) It effectively rules out
hepatitis B as the cause of his illness
Explanation: Anti-HBs is found in the
blood of patients who have been
successfully immunised against hepatitis
B. As a nurse, this patient will have been
immunised before taking up employment.
If you're still having trouble with
interpretation of these serological tests,
have another look at the link below
Question 23. E) Treatment with
interferon is ineffective in chronic
infection
Explanation: Interferon treatment is
effective in some patients with hepatitis B.
Question 24. E) Acute infection is
usually asymptomatic
Explanation: Hepatitis C is only rarely
symptomatic in the acute phase, and is
often only discovered once cirrhosis has
developed. About 80% of infected patients
develop chronic infection, which usually
progresses ultimately to cirrhosis.
Treatment with pegylated interferon and
ribavirin can eradicate the virus
completely in some patients. Although
reinfection almost inevitably occurs after
transplant, this treatment may give
otherwise terminally ill patients many
years of a high quality of life, and should
not be withheld for this reason.
Question 25. B) There is a genetic
predisposition
Explanation: Twin studies have revealed
a genetic contribution to ALD, although
there is at least one obvious environmental
factor involved. After a presenting
complication of cirrhosis, most patients
who become abstinent will be alive after 5
years.
Question 26. C) Non-alcoholic fatty liver
disease
Explanation: Obesity is by far the most
common cause of non-alcoholic fatty liver
disease, which also shows an association
with type 2 diabetes mellitus and the
metabolic syndrome. It is the most likely
cause in this patient. The introduction of
tests to detect and exclude infected blood
units has massively reduced the risk of
transmission of hepatitis B and other
viruses through blood transfusion. The
chances of hepatitis B transmission from a
unit of blood in the UK in 2002 were
around 0.24 per 1 000 000 units.
Question 27. A) Co-amoxiclav
Explanation: Co-amoxiclav (amoxicillin
plus clavulanic acid) may cause a
cholestatic hepatitis up to 42 days after a
course of treatment has finished.
Paracetamol in normal doses can cause
liver necrosis, but this only occurs in highrisk patients, such as those with preexisting alcoholic liver disease.
211
Question 28. E) Hereditary
haemochromatosis
Explanation: The combination of joint
pain (caused by chondrocalcinosis),
diabetes mellitus ('bronzed diabetes),
hepatomegaly and hyperpigmentation is
characteristic of hereditary
haemochromatosis, one of the most
common inherited diseases in northern
Europeans. About 90% of patients are
male, perhaps due to the protective effect
of iron loss with menstruation.
Question29. B) Weekly venesection of
500 ml blood
Explanation: The complications of
haemochromatosis arise because of
massive iron overload. The aim of
treatment is to remove this excess iron
safely, and this is done by weekly
venesection until iron levels return to
normal.
Question30. C) Wilson's disease
Explanation: Recurrent acute hepatitis
with parkinsonian features and
choreoathetoid movements suggest
Wilson's disease. The Kayser-Fleischer
rings (shown here) around the cornea are
pathognomonic but easily missed. Of the
other options, hereditary
haemochromatosis usually presents later in
life with advanced liver disease. The
others may cause acute liver failure but do
not cause Kayser-Fleischer rings or
extrapyramidal manifestations. BuddChiari syndrome is hepatic venous
thrombosis, Amanita phalloides is a
profoundly hepatotoxic mushroom, and
ecstasy (MDMA) is a drug of abuse that
may cause liver failure.
Question31. A) Penicillamine
Explanation: Penicillamine is a copper
chelator and is the treatment of choice in
Wilson's disease. It removes copper in the
urine and confers an excellent prognosis,
provided it is commenced before the
development of irreversible liver and
cerebral damage.
Question32. E) Chronic viral hepatitis
Explanation: All of these conditions
predispose to cirrhosis and hepatocellular
carcinoma. Hepatitis B- and C-related
cirrhosis is particularly carcinogenic. In
chronic hepatitis B infection, but not
chronic hepatitis C infection,
hepatocellular carcinoma can also occur in
the absence of cirrhosis.
Question33. C) Acute cholecystitis
Explanation: This is a classic presentation
of acute cholecystitis. Biliary colic causes
pain but not inflammation, and so the
pyrexia and leucocytosis make this
diagnosis less likely. Acute pancreatitis is
highly unlikely, given the normal amylase.
Mirizzi's syndrome (a stricture in the
common hepatic duct caused by gallstones
impacted in the cystic duct) and
choledocholithiasis (stones in the bile
duct) would be expected to cause
abnormal LFTs in a patient with disease
severe enough to present with systemic
symptoms.
Question34. C) Cholecystokinin
Explanation: Cholecystokinin secretion is
increased after a meal. It promotes satiety,
increases pancreatic enzyme secretion,
stimulates gallbladder contraction and
relaxes the sphincter of Oddi.
Question35. A) Recurrent epigastric
pain, radiating to the back, lasting 2
hours then subsiding spontaneously
Explanation: 'Biliary colic' usually lasts
for around 2 hours and occurs
intermittently. It is most commonly felt in
the epigastrium (70%) or right upper
quadrant (20%), and often radiates to the
interscapular region or the tip of the right
scapula. Of the other options, D is
characteristic of dyspepsia and E is
suggestive of an acute myocardial
infarction. B and C are relatively nonspecific presentations but serious
diagnoses such as dissecting thoracic
aneurysm and acute pancreatitis must be
considered.
212
Question36. B) Abdominal ultrasound
scan
Explanation: Ultrasound is quick and
inexpensive and does not expose the
patient to radiation. Stones may be
visualised within the gallbladder and bile
duct, and dilatation of the bile duct may be
seen, indicating distal obstruction of bile
flow.
Question37. B) Correction of any
coagulopathy with fresh-frozen plasma
Explanation: The liver is a highly
vascular organ and life-threatening
haemorrhage may occur following injury
to it. Most patients presenting for TIPSS
have cirrhosis, and impairment of hepatic
synthetic function leading to coagulopathy
is common. This is effectively corrected
by replacing clotting factors by
administering fresh-frozen plasma.
Question38. C) Cholestasis and hepatitis
are both common presentations
Explanation: Alcoholic liver disease is a
common cause of substantial suffering, so
a good understanding of it is important. It
may be detected incidentally in an
asymptomatic individual or may present
with features of cholestasis, hepatitis or
advanced cirrhosis. Alcohol causes several
different pathological lesions including
macrovesicular steatosis. Fatty liver
secondary to alcohol carries a good
prognosis and may be reversible with as
little as 3 months of abstinence. Cirrhosis
is found in only 10% of alcoholics at postmortem. The total amount of alcohol
ingested rather than the concentration
determines the risk of liver damage.
Question39. E) Chronic hepatitis C
infection
Question 40. D) Hypoglycaemia
Explanation: Hypoglycaemia does not
precipitate hepatic encephalopathy but is
an important differential diagnosis in a
patient with liver disease presenting with
confusion or drowsiness.
Chapter
23 BLOOD DISORDERS
Question1. A) They are derived from
megakaryocytes
Explanation: Red blood cell precursors
are called erythroblasts or normoblasts.
These nucleated cells divide and acquire
haemoglobin. The nucleus is then extruded
from the cell. The first non-nucleated red
cell is the reticulocyte. Increased red cell
production is therefore associated with
increased numbers of circulating
reticulocytes. Megakaryocytes give rise to
platelets.
Question2. D) Pneumococcal infection
Explanation: Eosinophils have
phagocytic potential and are involved in
combating parasitic infection. They are
also implicated in allergic reactions (e.g.
atopic asthma, hay fever, eczema).
Bacterial infection typically causes a
neutrophilia.
Question3. C) Carbimazole
Explanation: See list of Drugs causing
neutropenia
Question4. C) Thalassaemia
Explanation: Iron deficiency,
thalassaemia and sideroblastic anaemia all
cause a microcytosis (reduced red cell size
or mean cell volume, MCV). Vitamin B12
or folate deficiency, chronic liver disease,
alcohol excess and hypothyroidism cause a
macrocytosis (i.e. increased MCV).
Question5. B) Cirrhosis
Explanation: Target cells have a central
area of haemoglobinisation and are seen
typically in liver disease, thalassaemia and
post-splenectomy.
Question6. B) Multiple myeloma
Explanation: Chronic myeloid leukaemia,
myelofibrosis and malaria may all produce
massive splenomegaly. Portal
213
hypertension secondary to cirrhosis of the
liver is a common cause of splenomegaly
in the UK. Multiple myeloma, a malignant
proliferation of plasma cells associated
with excess production of a monoclonal
immunoglobulin (paraprotein), may
produce a diverse array of clinical
manifestations but does not cause
splenomegaly.
Question7. B) Coagulation by the
extrinsic pathway is initiated by the
interaction of factor VII with tissue
factor
Explanation: Clotting factors are
synthesised in the liver. The coagulation
process can be activated by one of two
pathways (extrinsic and intrinsic). The
extrinsic pathway is thought to be the
major physiological mechanism in vivo,
and is initiated by the interaction of factor
VII with tissue factor. The final step in the
cascade is the conversion of fibrinogen to
fibrin. Antithrombin, protein C and protein
S are natural inhibitors of the clotting
system. Antithrombin has inhibitory
activity against thrombin and factor Xa.
The binding of heparin to antithrombin
accelerates this inhibitory activity.
Question8. B) Factor V
Explanation: Clotting factors are
synthesised by the liver. Factors II, VII, IX
and X are produced as inactive proteins.
They are activated by a carboxylase
enzyme which requires vitamin K as a cofactor. In this process, vitamin K is
inactivated to an epoxide; it must therefore
be reactivated by a reductase enzyme.
Warfarin inhibits the latter reaction,
reducing the availability of active vitamin
K and thereby exerting an anticoagulant
effect.
Question9. C) It provides an accurate
assessment of platelet function
Explanation: The prothrombin time (PT)
assesses the extrinsic pathway of the
coagulation cascade and is prolonged by
deficiencies of factors II, V, VII and X.
Warfarin leads to prolongation of the PT.
The international normalised ratio (INR) is
used to monitor warfarin treatment; it is
the ratio of the patient's PT to a normal
control PT corrected to the international
thromboplastin. The activated partial
thromboplastin time (APTT) assesses the
intrinsic pathway and is prolonged in
patients with haemophilia A.
Thrombocytopenia and abnormal platelet
function lengthen the bleeding time but do
not affect the PT or APTT.
Question10. B) Haemarthrosis
Explanation: Muscle and joint bleeds
suggest a coagulation defect. Purpura,
prolonged bleeding from superficial cuts,
epistaxis, gastrointestinal haemorrhage
and menorrhagia suggest
thrombocytopenia, abnormal platelet
function or von Willebrand's disease.
Question11. D) Desmopressin
aggravates the tendency to bleeding
Explanation: Haemophilia A is an Xlinked recessive condition characterised by
factor VIII deficiency. There is a spectrum
of severity. Large joint haemarthroses and
muscle haematomas are characteristic.
Recurrent bleeds into joints can lead to
secondary osteoarthritis. Treatment is
usually with factor VIII concentrate.
Desmopressin (vasopressin, antidiuretic
hormone
) can also be used to treat mild bleeds or
cover minor surgery in patients with mild
haemophilia.
214
Question12. C) Doppler ultrasound
scan of the leg
Explanation: A patient's clinical risk of
having a DVT can be established using the
Wells scoring system. Those with a high
or medium risk should undergo definitive
investigation by Doppler ultrasound or
venography. For patients with a low risk,
the plasma D-dimer should be measured; a
normal level excludes a DVT, but a raised
level should prompt ultrasound or
venography. A positive D-dimer is not
diagnostic of a DVT, but a negative Ddimer in patients at low risk of a DVT
essentially excludes the diagnosis.
Depending on the clinical context, a
thrombophilia screen may be indicated
after the diagnosis of venous thrombosis
has been confirmed.
Question13. E) ABO incompatibility
reactions are mediated by complement
Explanation: The ABO system comprises
four different blood groups: O, A, B and
AB. Individuals have antibodies directed
against the A or B antigens that are not
expressed on their own red cells. Group O
blood can therefore be given to all
patients, as the infused red cells do not
express any AB antigens ('universal
donor'), while patients with group AB
blood can safely receive blood of all four
groups, as they do not have antibodies to
either A or B antigens ('universal
recipient'). The transfusion of ABOincompatible blood is the main cause of
fatal acute transfusion reactions, and the
risk is greatest if group A red cells are
infused into a group O recipient. The
recipient's antibodies bind to antigens on
the transfused cells, activating
complement. The resulting lysis of red
blood cells may lead to disseminated
intravascular coagulation and renal failure.
Question14. C) Transfusion of RhDnegative blood to an RhD-positive
woman may result in production of
anti-RhD antibodies
Explanation: IgG antibodies to RhDpositive red cells are produced if such cells
enter the circulation of an RhD-negative
individual (e.g. via blood transfusion or
fetomaternal haemorrhage). If an RhDnegative woman is so sensitised and
subsequently becomes pregnant with a
RhD-positive fetus, then the anti-RhD
antibodies can cross the placenta and
cause severe anaemia and neurological
damage (haemolytic disease of the
newborn). Anti-RhD immunoglobulin
(anti-D) can be given to RhD-negative
pregnant women after potentially
sensitising events to prevent the
development of endogenous Rhesus
antibodies.
Question15. D) Give paracetamol and
continue transfusion at a slower rate
Explanation: Febrile non-haemolytic
transfusion reactions are not uncommon. If
temperature rises by less than 1.5°C and
the patient is otherwise well, then it is
reasonable to administer paracetamol and
continue the transfusion at a slower rate.
Allergic reactions (urticaria,
bronchospasm, angio-oedema) should be
treated with IV chlorphenamine and
hydrocortisone, nebulised salbutamol and
IM adrenaline (epinephrine) according to
their severity. The transfusion should be
stopped, and any unused blood should be
returned to the blood bank together with a
repeat sample for a 'group and screen' test.
Question16. E) Creutzfeldt-Jakob
disease (CJD)
Explanation: Blood products are
routinely screened for HIV, human T
lymphotrophic virus (HTLV), hepatitis B
and C, and syphilis.
Question17. A) Omeprazole
Explanation: Iron is absorbed in the
upper small intestine. Hydrochloric acid
secreted by the stomach helps to maintain
iron in the soluble reduced ferrous (Fe2+)
state, as opposed to the oxidised ferric
(Fe3+) state; the ferrous form is more easily
absorbed.
215
Reduced gastric acid secretion following
long-term proton pump inhibitor therapy
can therefore lead to iron malabsorption.
Aspirin causes iron deficiency by
increasing gastrointestinal blood loss, not
by interfering with its absorption.
Question18. C) Upper gastrointestinal
endoscopy
Explanation: Iron deficiency causes a
microcytic, hypochromic anaemia. The
most common cause in men and postmenopausal women is gastrointestinal
blood loss. This may result from upper or
lower gastrointestinal malignancy, peptic
ulcer disease, inflammatory bowel disease,
diverticular disease, colonic polyps and
angiodysplasia. Aspirin and non-steroidal
anti-inflammatory drugs (NSAIDs) can
exacerbate any blood loss. The
gastrointestinal tract must therefore be
investigated by endoscopy (upper
gastrointestinal endoscopy and
colonoscopy) or barium studies.
Question19. C ) Cold agglutinin disease
Explanation: Iron deficiency occurs when
iron losses or physiological requirements
exceed absorption. (see link below). Cold
agglutinin disease is a cause of
intravascular haemolysis resulting from
the development of IgM antibodies to red
cells. It can occur transiently in association
with Mycoplasma pneumoniae infection or
infectious mononucleosis, or may follow a
chronic course in patients with underlying
lymphoma.
Question 20. D) Reduced ferritin
Explanation: All of the above typically
occur in iron deficiency but plasma ferritin
is the best single confirmatory test on
account of its high specificity (i.e. a low
ferritin is strongly suggestive of iron
deficiency). On the other hand, a normal
ferritin level does not exclude iron
deficiency as levels may be elevated in
systemic inflammation (ferritin is an acute
phase protein) or liver disease, despite
absent bone marrow stores.
Question 21. D) It is often due to dietary
deficiency
Explanation: Vitamin B12 and folate
deficiency lead to impaired DNA
synthesis. This results in a megaloblastic
anaemia associated with a raised mean cell
volume (MCV). The blood film shows
oval macrocytes and hypersegmented
neutrophils. In severe cases there may be
peripheral blood cytopenias. Vitamin B12
is absorbed in the terminal ileum.
Deficiency may therefore arise from
Crohn's disease or surgery affecting this
part of the bowel. B12 deficiency is very
rarely dietary in origin, only affecting
strict vegans.
Question 22. B) Nystagmus
Explanation: Vitamin B12 deficiency is
associated with neurological disease in up
to 40% of patients. Peripheral nerve
involvement gives rise to a 'glove and
stocking' peripheral neuropathy. Spinal
cord damage results in subacute combined
degeneration of the cord; posterior column
involvement causes loss of vibration and
joint position sensation (resulting in
ataxia), and corticospinal tract damage
leads to upper motor neuron signs. In rare
cases, chronic B12 deficiency can lead to
dementia.
Question 23. C) Total body stores are
small
Explanation: Foods rich in folate include
leafy vegetables, fruits and animal protein.
Pregnancy is a common cause of folate
deficiency, especially in twin pregnancies
and hyperemesis gravidarum. Pernicious
anaemia is an autoimmune condition in
which there is antibody-mediated
destruction of gastric parietal cells. This
leads to reduced secretion of intrinsic
factor and impaired absorption of vitamin
B12; folate is unaffected. The Schilling test
is helpful in distinguishing B12 deficiency
secondary to pernicious anaemia from that
resulting from malabsorption. It is,
however, rarely performed in practice.
Serum folate is very sensitive to dietary
intake, and red cell folate provides a more
accurate indicator of folate stores.
216
Question 24. D) Hereditary
spherocytosis
Explanation: The normocytic anaemia,
reticulocytosis, elevated bilirubin and
elevated LDH suggest a haemolytic
process, consistent with either
autoimmune haemolytic anaemia or
hereditary spherocytosis. The presence of
reticulocytes, which are large, accounts for
the MCV at the upper end of the normal
range. One would expect the direct
Coombs test to be positive in autoimmune
haemolytic anaemia, making hereditary
spherocytosis the more likely diagnosis in
this case. The anaemia of chronic disease
may cause a normocytic anaemia but
would not account for the features
suggesting haemolysis. Coeliac disease
may lead to anaemia through iron and/or
folate malabsorption but both are normal
in this case. The normal B12 level excludes
pernicious anaemia.
Question 25. B) Haemosiderinuria
Explanation: Haemosiderinuria occurs
when all other mechanisms for 'mopping
up' free intravascular haemoglobin have
been exhausted and is always indicative of
intravascular haemolysis. Earlier features
include a fall in haptoglobin levels and
formation of methaemalbumin (detected
by the Schumm's test). Reticulocytosis and
elevated LDH may result from any cause
of haemolysis. Splenomegaly may occur
in extravascular haemolysis where
physiological destruction occurs in the
fixed reticulo-endothelial cells in the liver
or spleen. Positive direct Coombs test
indicates immune-mediated destruction of
red cells.
Question 26. C) It may lead to the
development of cholesterol gallstones
Explanation: In most cases of hereditary
spherocytosis there is a compensated
chronic haemolytic state. However, the
condition can be complicated by
haemolytic, aplastic or megaloblastic
crises. The latter results from folate
deficiency, which in turn arises from
increased red cell turnover. This can be
precipitated by pregnancy, and patients
with hereditary spherocytosis should
receive folic acid supplements. The
hyperbilirubinaemia resulting from
haemolysis gives rise to pigment (not
cholesterol) gallstones. The spleen is the
main site of haemolysis, and splenectomy
may therefore improve the anaemia.
Question 27. C) Glucose-6-phosphate
dehydrogenase
Explanation: Glucose-6-phosphate
dehydrogenase is essential for the
intracellular production of NADPH which
protects the red cell against oxidative
stress. Deficiency can result in haemolysis.
Question 28. D) Sickle-cell anaemia is
usually accompanied by a
reticulocytosis
Explanation: Sickle-cell disease is caused
by an amino acid substitution in the beta
globin polypeptide chain. The condition is
inherited as an autosomal recessive trait.
Homozygotes only produce abnormal beta
chains which form abnormal HbS (sicklecell anaemia), while heterozygotes make a
mixture of normal HbA and abnormal HbS
(sickle-cell trait). Individuals with sicklecell trait are usually asymptomatic and
may be relatively resistant to falciparum
malaria. Patients with sickle-cell disease
usually have a compensated anaemia
associated with a reticulocytosis. The high
reticulocyte count represents the body's
attempt to maintain an adequate
haemoglobin concentration in the face of
red cell sickling. Even with optimal
medical care, life expectancy is greatly
reduced.
Question 29. Peripheral neuropathy
Explanation: Hypoxia, dehydration and
infection precipitate sickling. This can
217
lead to a vaso-occlusive crisis, where
plugging of small blood vessels produces
acute severe bone pain (e.g. dactylitis,
avascular necrosis of the hip, pain in the
limbs or vertebrae). Recurrent sickling in
the spleen can cause splenic infarction and
ultimately hyposplenism. Bone marrow
infarction can result in fat emboli to the
lungs and cause pulmonary infarction
(sickle chest syndrome).
Question 30. C) Beta-thalassaemia
minor
Explanation: Normal adult haemoglobin
(HbA) consists of two alpha and two beta
globin chains (V2_2). The thalassaemias are
a group of inherited disorders in which
there is impairment of globin chain
production. In alpha-thalassaemia the
alpha genes are deleted; in betathalassaemia (seen most commonly in the
Mediterranean area) beta chain production
is defective. In beta-thalassaemia major
(seen in homozygotes), HbA production is
absent or grossly reduced; individuals
develop a profound microcytic
hypochromic anaemia, and electrophoresis
reveals increased levels of HbF (V2W2).
Beta-thalassaemia minor (seen in
heterozygotes) results in a microcytic
blood picture with no clinical
manifestations; there is a raised fraction of
HbA2 (V2a2).
Question 31. C) Acute myeloid
leukaemia (AML)
Explanation: This patient has a high
white cell count associated with anaemia
and thrombocytopenia. The hypercellular
bone marrow indicates increased white
cell proliferation with 'spill over' into the
peripheral blood. The excess of immature
blast cells of the myeloid lineage suggests
a diagnosis of AML. Although white cells
are massively increased in number, they
are immature and functionally useless.
They take up increasing amounts of
marrow space at the expense of the normal
haematopoietic stem cells.
Question 32. D) Chronic myeloid
leukaemia (CML)
Explanation: This patient has a marked
leucocytosis originating from the
granulocyte series. The picture is
dominated by mature neutrophils. This
pattern of granulocyte proliferation with
fairly normal cell maturation is consistent
with chronic myeloid leukaemia. In some
cases, CML may transform into an acute
leukaemia (blast crisis phase)
characterised by proliferation of immature
blast cells. Blast crisis is relatively
refractory to treatment and is the major
cause of death in patients with CML.
Question 33. E) Chronic myeloid
leukaemia (CML)
Explanation: Around 95% of patients
with CML possess the Philadelphia
chromosome. This is a chromosomal
abnormality characterised by reciprocal
translocation of genetic material between
chromosomes 9 and 22. The fragment
from chromosome 9 carries the abl
oncogene and joins the breakpoint cluster
region (BCR) on chromosome 22. The
resultant BCR ABL chimeric gene codes
for a tyrosine kinase that stimulates cell
proliferation and plays a causative role in
the disease. The development of imatinib,
a specific inhibitor of BCR ABL tyrosine
kinase activity, has revolutionised the
management of CML.
Question 34. C) Hyposplenism is a
frequent finding
Explanation: Chronic lymphocytic
leukaemia (CLL) has an insidious onset,
and the diagnosis is made incidentally
following a routine full blood count in
70% of patients. The condition most
commonly arises in the elderly, and is
characterised by a monoclonal
proliferation of B lymphocytes. Clinical
features include symptomatic anaemia,
infection, lymphadenopathy, night sweats
and weight loss. Splenomegaly and warm
autoimmune haemolytic anaemia may also
be present. Treatment is generally only
required for patients with systemic
symptoms, bone marrow failure,
progressive lymphadenopathy or
splenomegaly. The oral chemotherapeutic
agent chlorambucil is usually first-line
therapy.
218
Question 35. D) Bone marrow
aspiration reveals a hypocellular
marrow
Explanation: Myelodysplastic syndrome
(MDS) comprises a group of
haematopoietic stem cell disorders
characterised by peripheral blood
cytopenias and abnormal-looking
(dysplastic) blood cells. The marrow is
hypercellular with dysplastic changes. It
predominantly affects elderly patients,
presenting with symptoms of anaemia,
recurrent infections or bleeding. The
condition is incurable in most patients, and
supportive care with transfusion and
antibiotics is the mainstay of treatment.
Given time, all forms of MDS will
ultimately progress to AML, although the
time course to progression is highly
variable.
Question 36. B) Reed-Sternberg cell
Explanation: The characteristic
histological abnormality in Hodgkin
lymphoma is the presence of ReedSternberg cells - large, malignant
lymphoid cells of B-cell origin. Ringed
sideroblasts are erythroid precursors in
which iron has accumulated in the
mitochondria, seen in sideroblastic
anaemia. Auer rods are present in acute
myeloid leukaemia. Burr cells are
irregularly shaped red blood cells typical
of uraemia, and Howell-Jolly bodies are
nuclear remnants commonly seen postsplenectomy; both are detected on the
peripheral blood film.
Question 37. B) Multiple myeloma
Explanation: Multiple myeloma is a
malignant proliferation of plasma cells
associated with excess production of a
monoclonal immunoglobulin
(paraprotein). The plasma cells release
cytokines which stimulate osteoclasts and
result in bone resorption, bone pain,
pathological fractures and hypercalcaemia.
Bone marrow involvement can lead to a
normocytic anaemia. Paraprotein
deposition in the kidneys, hypercalcaemia
and dehydration can all contribute to cause
renal failure. The erythrocyte
sedimentation rate is often elevated. The
paraprotein (most often of the IgG
subtype) can be measured in plasma and
detected by protein electrophoresis.
Question 38. D) Bence Jones protein in
urine and lytic lesions on plain X-ray
Explanation: This is a difficult question
but contains a number of useful learning
points. The diagnosis of multiple myeloma
requires two of the following criteria:
• increased malignant plasma cells in bone
marrow
• serum and/or urinary paraprotein
skeletal lesions (characteristically lytic
lesions).
• Thus, although options A and B would
both be highly suggestive of myeloma,
only option D satisfies the criteria. Bence
Jones protein is an immunoglobulin light
chain produced by plasma cells that
appears in urine. Hypercalcaemia is a
common feature in myeloma, resulting
from lytic bony lesions. The ESR may be
elevated as a result of increased plasma
viscosity from the paraproteinaemia,
although it is worth noting that only 5% of
patients with an ESR persistently > 100
mm/hr actually have myeloma. Lytic bony
lesions, the skeletal hallmark of myeloma,
are best detected by skeletal survey and
not a radioisotope bone scan; in fact, in the
absence of fractures, both plasma ALP and
radioisotope bone scan are normal in
myeloma.
219
Question 39. E) Aspirin is
contraindicated
Explanation: Polycythaemia rubra vera
(PRV) is a myeloproliferative disorder
characterised by an increased red cell mass
and elevated haemoglobin concentration.
Neutrophil and platelet counts are often
also raised. Patients may present with
symptoms of hyperviscosity (e.g.
headache, dizziness, loss of concentration,
lethargy, pruritus). Splenomegaly is
common. The hyperviscosity predisposes
to arterial thrombosis; aspirin reduces this
risk. Venesection reduces red cell mass
and relieves hyperviscosity symptoms.
Question 40. B) Thrombotic
thrombocytopenic purpura
Explanation: Haemolytic uraemic
syndrome (HUS) and thrombotic
thrombocytopenic purpura (TTP) represent
two conditions on a continuum
characterised by microangiopathic
haemolytic anaemia, the formation of
platelet thrombi in the microcirculation
and resultant thrombocytopenia. Other
features include renal failure and
fluctuating neurological signs due to
microvascular thrombosis.
Question 41. D) Non-Hodgkin
lymphoma
Explanation: The combination of
lymphadenopathy and systemic upset in an
elderly patient raises the possibility of
non-Hodgkin lymphoma (NHL).
Hodgkin's disease usually affects young
adults, although there is a second peak at
age 50-70. CML is usually associated with
a marked leucocytosis and does not
typically cause generalised
lymphadenopathy.
Question 42. C) Fibrinogen levels are
elevated
Explanation: Disseminated intravascular
coagulation (DIC) is triggered by
conditions causing exposure of tissue
factor with consequent activation of the
coagulation system via the extrinsic
pathway. Common causes of DIC include
Gram-negative septicaemia and
antepartum haemorrhage. Intravascular
coagulation results in thrombosis with
consumption of platelet and coagulation
factors. The resultant thrombocytopenia,
prolonged prothrombin and activated
partial thromboplastin time lead to a
haemorrhagic state. Fibrinogen levels are
low, and levels of D-dimer (a fibrin
degradation product indicating fibrin
turnover and breakdown) are raised.
Question 43. C) The anticoagulant effect
of low molecular weight heparin can be
assessed using the activated partial
thromboplastin time (APTT)
220
Explanation: Unfractionated IV heparin
exerts its anticoagulant affect by
enhancing the effect of antithrombin,
which itself inhibits the procoagulant
activity of factors IIa, VIIa, IXa, Xa and
XIa. The level of anticoagulation is
monitored using the APTT. Low
molecular weight heparins are
administered subcutaneously on a once- or
twice-daily basis. They augment
antithrombin activity against factor Xa and
do not affect the APTT. The half-life of IV
heparin is around 1 hour, and if a patient
bleeds it is usually sufficient simply to
discontinue the heparin; in severe cases,
heparin can be neutralised with protamine.
It takes warfarin takes several days to
exert its therapeutic effect, and treatment
with heparin is required during this
window. Heparin-induced
thrombocytopenia (HIT) is a recognised
complication, requiring immediate
discontinuation of the drug.
Chapter
24 MUSCULOSKELETAL
DISORDERS
Question 1. D) Paget's disease
Explanation: Paget's disease is a common
condition characterised by increased and
disorganised bone remodelling. The
biochemical picture is that of a normal
calcium, phosphate and PTH, in
conjunction with a raised alkaline
phosphatase. Osteoporosis (in the absence
of a fracture) does not cause any
biochemical abnormality. The fact that the
lady has been complaining of difficulty in
hearing may be significant, as deafness is
a clinical feature of Paget's disease.
Question 2. C) Septic arthritis
Explanation: Although all of the above
may cause an acute monoarthritis, septic
arthritis is the most likely cause, given the
progressive pain, overlying erythema,
pyrexia, recent episode of cellulitis
(representing a possible portal of entry for
infection) and presence of risk factors
(diabetes mellitus, pre-existing joint
disease, age). With crystal synovitis (urate,
pyrophosphate) pain is at its maximum
within the first day; progressive pain and
overlying erythema should always suggest
sepsis.
Question 3. D) Joint aspiration
Explanation: Although a full blood count,
CRP test and X-ray of the joint might
provide useful information, only an
aspirate of fluid from the knee sent for
microscopy, culture and sensitivity can
definitively confirm the diagnosis. Blood
cultures also identify the organism in
around 50% of cases.
221
Question 4. C) Exacerbations of
symptoms are often associated with
stressful life events
Explanation: The principal features of
fibromyalgia are multiple sites of regional
pain, particularly over the neck and back,
and fatigability. In general there is a
discrepancy between the level of disability
reported by the patient and the physical
findings found on examination. Joint
disease, neurological deficit, muscle
wasting and a raised ESR are not features
of fibromyalgia and any of these should
prompt a search for an alternative
explanation. Treatment is symptomatic
and patient education is important, as is
the provision of a graded exercise
programme.
Question 5. C) Prolonged morning
stiffness
Explanation: Morning stiffness in
osteoarthritis tends to be brief, lasting only
a few minutes. Thereafter, pain is related
to movement and weight-bearing, and
relieved by rest. This pattern contrasts
markedly with inflammatory arthritides
such as rheumatoid arthritis, in which
morning stiffness is typically prolonged
(lasting longer than an hour) and
symptoms are exacerbated by inactivity.
Question 6. D) Methotrexate
Explanation: Osteoarthritis is extremely
common and knowledge of the various
aspects of its management is therefore
essential. Methotrexate is a diseasemodifying drug used in the treatment of
the inflammatory arthritides and has no
role in the management of osteoarthritis.
Question 7. B) The presence of antidouble-stranded DNA (anti-dsDNA)
antibodies on blood tests
Explanation: Anti-dsDNA antibodies are
highly specific for systemic lupus
erythematosus and would therefore make
the diagnosis of rheumatoid arthritis
unlikely. The presence of rheumatoid
factor, on the other hand, would be
consistent with the diagnosis and, in
common with the other options listed, is
included in the American Rheumatism
Association diagnostic criteria for
rheumatoid arthritis. Because of its low
specificity, however, a high titre of
rheumatoid factor at presentation has more
prognostic value (it suggests a worse
prognosis) than diagnostic value.
Question 8. D) Alopecia
Explanation: All of the above are
recognised features of rheumatoid arthritis,
with the exception of alopecia. Alopecia is
more commonly associated with systemic
lupus erythematosus.
Question 9. C) Felty's syndrome
Explanation: Although an enlarged
spleen may potentially be found in any of
the above conditions, Felty's syndrome
refers to the association of splenomegaly
and neutropenia with rheumatoid arthritis
and is, therefore, the most likely diagnosis
here. It has a peak incidence in the 50-70year-old age group, typically occurring in
patients with longstanding disease and a
positive rheumatoid factor. In addition to
splenomegaly, clinical features include
recurrent infections, weight loss, leg ulcers
and lymphadenopathy.
Question 10. A) Bouchard's nodes
Explanation: Bouchard's nodes are
posterolateral hard swellings of the
proximal interphalangeal joints,
characteristically seen in nodal generalised
osteoarthritis along with Heberden's nodes
(similar swellings arising from the distal
interphalangeal joints).
222
Question 11. B) Naproxen
Explanation: DMARDs have the
potential to reduce target tissue damage in
rheumatoid arthritis and may therefore
favourably alter the rate of disease
progression. Naproxen is a non-steroidal
anti-inflammatory drug (NSAID) and, as
such, provides symptomatic relief only.
Question 12. D) Keratitis with
hydroxychloroquine
Explanation: All of the above
associations are true with the exception of
D. At very high doses hydroxychloroquine
(though more commonly chloroquine)
may cause retinitis (classically a 'bull's
eye' maculopathy) and not keratitis
(inflammation of the cornea).
Question 13. B) Strongly positive
rheumatoid factor
Explanation: As one of the seronegative
spondarthritides (see Box 25.51 in the link
below), ankylosing spondylitis has no
association with seropositivity for
rheumatoid factor. Rheumatoid factor is
negative or positive only in low titre.
Question 14. D) Atlanto-axial instability
Explanation: Psoriatic arthritis may
present with a variety of different patterns
of joint disease. Atlanto-axial subluxation,
however, is a potentially serious
manifestation of rheumatoid arthritis and
occasionally other conditions (e.g. classic
ankylosing spondylitis, Down's
syndrome).
Question 15. A) Bendroflumethiazide
Explanation: Thiazide diuretics such as
bendroflumethiazide reduce urinary
excretion of uric acid and may therefore
lead to hyperuricaemia and eventual urate
crystal formation. Other drugs that cause
hyperuricaemia include aspirin,
ciclosporin, pyrazinamide and alcohol.
Question 16. C) Allopurinol is often
used in the treatment of an acute attack
Explanation: Allopurinol is not used to
treat acute gout. Management of acute
gout includes appropriate analgesia (often
a non-steroidal anti-inflammatory drug),
oral colchicine, joint aspiration and intraarticular injection with a long-acting
steroid. The most common side-effects of
colchicine are nausea and diarrhoea.
Definitive diagnosis of gout requires
demonstration of negatively birefringent
needle-shaped crystals in a joint aspirate
when viewed under polarised light.
Question 17. B) Acromegaly
Explanation: Sporadic, familial and
metabolic-associated forms of pseudogout
exist. The common feature is deposition of
calcium pyrophosphate crystals in the joint
(most commonly the knee, followed in
frequency by the wrist, shoulder, ankle
and elbow), leading to chondrocalcinosis.
Acromegaly is associated with a secondary
osteoarthritis, but not with pseudogout.
Question 18. C) Hypothyroidism
Explanation: Hyperthyroidism, not
hypothyroidism, is associated with
osteoporosis.
Question 19. D) Weight-bearing exercise
is protective
Explanation: Protective factors include
weight-bearing exercise, high dietary
calcium and late menopause. The
biochemical profile in osteoporosis should
be entirely normal, and any deviation from
this, other than in the context of a fracture
(which may cause a rise in alkaline
phosphatase), should arouse suspicion of
an alternative diagnosis. The diagnosis is
based on the T-score, which measures the
number of standard deviations difference
between the bone mineral density of the
patient and the mean of a normal healthy
population with peak bone mass. The Zscore is the number of standard deviations
from the mean for an age-matched
population, which is a less precise
predictor of risk of fracture than the Tscore.
223
Question 20. D) Sclerodactyly
Explanation: All the skin and mucous
membrane conditions listed are associated
with SLE except for sclerodactyly, which
is a feature of systemic sclerosis.
Question 21. A) They inhibit bone
resorption
Explanation: Bisphosphonates act by
adsorbing to bone surfaces and becoming
incorporated into the bone matrix. When
they are then ingested by osteoclasts in the
process of bone resorption, large amounts
of the drug are released within the cell,
bringing about osteoclast death and a
reduction in bone resorption. They have no
direct stimulatory effect on bone
formation. The increased bone mineral
density is thought to be due to decreased
removal of minerals from existing bone.
Question 22. D) Difficulty passing urine
Explanation: The most important lesson
from this question is that there are socalled 'red flag signs' (see the link below)
which must not be ignored, as they may be
indicative of serious underlying pathology.
All of the other symptoms described are
consistent with simple mechanical low
back pain, which is likely to improve with
time and simple analgesia.
Question 23. D) Psoriasis
Explanation: The term 'seropositive'
refers to arthritis that associates with an
increased prevalence of rheumatoid factor.
Psoriasis is one of a family of conditions the seronegative spondarthritides - that
manifest arthritis with no such increased
association with rheumatoid factor.
Rheumatoid factor has low specificity for
rheumatoid arthritis and occurs with
increased prevalence in a wide range of
conditions.
Question 24. C) Concomitant
respiratory disease
Explanation: Comorbidity does not
increase the incidence of NSAIDassociated gastrointestinal ulceration, but
if a person develops a complication
(bleeding, perforation, obstruction)
comorbidity, especially cardiovascular
disease and diuretic therapy, increases the
associated morbidity and mortality. Coprescription of a proton pump inhibitor
such as omeprazole can reduce the
incidence of NSAID-associated peptic
ulceration, and is particularly important to
consider in those with any of the risk
factors listed above. A past history of
peptic ulcer bleeding or perforation is
usually taken as an absolute
contraindication to oral NSAIDs.
Question 25. A) Conjunctivitis
Explanation: Reiter's disease is the most
common cause of inflammatory arthritis in
men aged 16-35. It consists of the classic
triad of arthritis, urethritis and
conjunctivitis; additional extra-articular
features include keratoderma
blenorrhagica, nail dystrophy, buccal
erosions and circinate balanitis.
Precipitants for Reiter's include bacterial
infections such as Salmonella or
Campylobacter, and also sexually
transmitted infections such as Chlamydia,
but not streptococcal throat infection.
Nodules are a feature of rheumatoid
arthritis.
Question 26. E) DXA bone scanning
involves the intravenous injection of
radioisotope
Explanation: DXA bone scanning
measures the extent to which the passage
of X-ray beams through bone is
attenuated. Since this is determined by the
degree of mineralisation, the relative
density of the bone can be calculated. Two
scores are calculated; the T-score
compares the bone mineral density (BMD)
of the subject to that of a healthy young
person, and the Z-score to that of an agematched control.
224
Both T- and Z-scores refer to numbers of
standard deviations from the mean.
Osteoporosis is defined as a T-score of < 2.5. The preferred sites for measurement
are the lumbar spine and the hip. DXA
scans should not be confused with isotope
bone scans, which involve the intravenous
injection of radioisotope.
Question 27. A) Calcium channel
blockers such as nifedipine may help
symptoms of Raynaud's phenomenon
Explanation: The dihydropyridine
calcium channel blockers help prevent
vasospasm and are a useful treatment for
Raynaud's phenomenon. An ACE inhibitor
is an important prophylactic agent in
reducing the risk of development of a
hypertensive renal crisis, particularly in
patients who have diffuse cutaneous
disease, who are most at risk of this
complication. Other useful treatments
include proton pump inhibitors for
oesophagitis (which is often severe) and
the oral endothelin antagonist bosentan for
pulmonary hypertension. On the other
hand, no agent is known to improve the
cutaneous manifestations of the disease.
Question 28. C) A violaceous rash
around the eyes
Explanation: Recognised cutaneous
features of dermatomyositis include a
violaceous rash around the eyes, Gottron's
papules over the proximal interphalangeal
and distal interphalangeal joints,
periorbital oedema and abnormal nailfold
capillary loops. Weakness of proximal
musculature is a cardinal feature.
Question 29. A) There is an association
with HLA-B27
Explanation: HLA-B27 is strongly
associated with ankylosing spondylitis.
Sjögren's is associated with HLA-B8 and
HLA-DR3.
Question 30. B) Sjögren's syndrome
Explanation: The case described fits best
with a diagnosis of Sjögren's syndrome.
Although the serology would be
compatible with both SLE and rheumatoid
arthritis, the description of
keratoconjunctiva sicca (dry eyes) and
xerostomia (dry mouth) and the
combination of both positive rheumatoid
factor and ANA are typical of Sjögren's.
Question 31. A) There is an association
with HLA-B27
Explanation: HLA-B27 is strongly
associated with ankylosing spondylitis.
Sjögren's is associated with HLA-B8 and
HLA-DR3.
Question 32. D) Muscle stiffness and
tenderness
Explanation: Polymyalgia rheumatica is a
disease of older people; patients are almost
always over 55 years, but there is a mean
age of onset of 70. The ESR is invariably
elevated. There is a rapid and dramatic
response to systemic corticosteroids, with
most patients experiencing relief of
symptoms within 72 hours of first dose.
The most common complaint is of muscle
stiffness and there is often marked muscle
tenderness but no muscle weakness.
Muscle weakness and wasting suggest
primary muscle disease such as
polymyositis.
Question 33. E) Give 60 mg of
prednisolone by mouth
Explanation: The history and exam
findings detailed above are absolutely
classical for temporal or giant cell arteritis.
This is a large-vessel vasculitis affecting,
predominantly, the branches of the
temporal and ophthalmic arteries. It is
sight-threatening, and the correct treatment
once the diagnosis is suspected is
immediate administration of high-dose
oral corticosteroid. Such steroid treatment
will not alter any histological
abnormalities obtained on temporal artery
biopsy if this procedure is undertaken
within 1-2 weeks.
225
Question 34. C) It is a large-vessel
vasculitis
Explanation: Polyarteritis nodosa (PAN)
is a rare vasculitis of small and mediumsized (not large conduit) vessels, which
predominately affects men, is ANCAnegative and may have a number of
manifestations, including arteritis of the
vasa nervorum, leading to peripheral
neuropathy, abdominal pain, fever and
severe hypertension secondary to renal
infarctions. Hepatitis B is a risk factor for
development of PAN, and incidence of
PAN is higher in places such as Alaska
where the infection is endemic.
Question 35. C) Osteoclasts are
responsible for bone formation
Explanation: All of the above are true
with the exception of option C; osteoclasts
are responsible for bone resorption (C for
chewing away at the bone), osteoblasts are
responsible for bone formation (B for
building up bone).
Question 36. C) Articular cartilage has
a rich vascular supply
Explanation: The major learning point
here is that articular cartilage is avascular.
Question 37. E) Osteopenia with Paget's
disease of bone
Explanation: X-rays in Paget's disease
commonly show a mixed picture of
osteosclerosis and focal osteolysis, but not
osteopenia. All of the other radiological
features described are true.
Question 38. E) Serum biochemistry is
usually normal in osteomalacia
Explanation: Osteomalacia is commonly
associated with low serum calcium and
phosphate, accompanied by elevated
alkaline phosphatase. In contrast,
osteoporosis is associated with normal
serum biochemistry. Options B and C
highlight the difference in the sensitivity
and specificity of tests. ANA has a high
sensitivity for lupus (almost 100%), so if a
person tests negative for ANA this
virtually excludes the diagnosis. (High
sensitivity is a desirable quality in a good
screening test.) Anti-dsDNA antibodies,
however, provide a highly specific test for
lupus, meaning that if a person tests
positive for anti-dsDNA antibodies, then
the diagnosis is almost certainly lupus.
Unfortunately, anti-dsDNA has low
sensitivity for lupus.
Question 39. D) Hydralazine
Explanation: Hydralazine, along with
procainaminde, isoniazid, minocycline and
chlorpromazine, can cause a drug-induced
lupus syndrome that commonly presents as
skin rash and arthralgia. Renal
involvement is less common in druginduced lupus than in primary lupus, but
can occur.
226
Question 40. B) Henoch-Schönlein
purpura
Explanation: The combination of
arthritis, abdominal pain and purpura in a
patient of this age suggests a diagnosis of
Henoch-Schönlein purpura. The condition
often follows an upper respiratory tract
infection.
Question 41. D) Chest X-ray
Explanation: A chest X-ray is the least
likely to aid diagnosis. A skin biopsy,
although invasive, would confirm the
diagnosis by demonstrating on
immunofluorescence IgA deposition in the
vessel walls. The serum IgA levels are
also often raised. Henoch-Schönlein
purpura may cause an acute nephritis
leading to haematuria and/or renal failure,
thus U&E and urinalysis are important. An
FBC should be checked in all cases of
purpura to exclude the possibility of
thrombocytopenia (low platelet count).
Question 42. E) Pulmonary embolism
Explanation: Cardiovascular
complications are the leading cause of
death in patients with Marfan's,
particularly aortic dissection which
accounts for 27-48% of deaths. There is no
increased risk of pulmonary embolism.
Chapter
25 NEUROLOGICAL DISEASE
Question 1. B) C5/C6
Explanation: The biceps and supinator
jerks both correspond to the C5/C6 nerve
roots.
Question 2. D) Schwann cells
Explanation: The myelin sheath
surrounding axons is essential for rapid
conduction of the action potential. Myelin
is formed by Schwann cells in the
peripheral nervous system, and by
oligodendrocytes in the central nervous
system (CNS). Astrocytes form the
structural framework for neurons within
the CNS. Microglia are specialised
macrophages. Astrocytes,
oligodendrocytes and microglial cells are
collectively known as glial cells.
Ependymal cells line the cerebral
ventricles.
Question 3. B) Receptive dysphasia
Explanation: The language centres are
located in the dominant hemisphere. The
left hemisphere is dominant in almost all
right-handed individuals and 50% of lefthanded individuals. Lesions to Broca's
area within the frontal lobe cause
expressive dysphasia; damage to
Wernicke's area in the temporal lobe
results in expressive dysphasia.
Question 4. A) Frontal lobe
Explanation: The frontal lobe is
responsible for personality, emotional
control and social behaviour, and lesions
here commonly present with disinhibited
or antisocial behaviour. Associated
physical phenomena may include 'frontal
release signs', i.e. primitive reflexes such
as grasp reflex, rooting reflex and
palmomental response.
227
Question 5. B) Childhood absence
epilepsy
Explanation: Absence epilepsy (formerly
known as petit mal) is a form of
generalised epilepsy encountered in
childhood and is characteristically
associated with a 3 cycles/second 'spike
and wave' pattern on EEG. Individuals
develop altered awareness and often have
a staring appearance lasting for only a few
seconds, followed by rapid recovery.
Question 6. D) Carpal tunnel syndrome
Explanation: The principal use of nerve
conduction studies is to identify damage to
peripheral nerves, determine whether such
damage is focal (e.g. carpal tunnel
syndrome) or diffuse (e.g. polyneuropathy
such as Guillain-Barré syndrome), and
establish if it is predominantly axonal or
demyelinating in nature.
Electromyography (rather than nerve
conduction) is abnormal in motor neuron
disease and myasthenia gravis. Multiple
sclerosis is a disease of the central rather
than the peripheral nervous system.
Question 7. E) MRI head scan
Explanation: Although there is no
specific test for multiple sclerosis, the
demonstration of patchy demyelination of
white matter within the central nervous
system may assist in the diagnosis. MRI is
far more sensitive than CT in detecting
soft tissue abnormalities and is therefore
the investigation of choice.
Question 8. D) Current treatment with
aspirin
Explanation: Lumbar puncture is
contraindicated in the presence of raised
intracranial pressure, as the procedure can
result in the downward shift of intracranial
contents into the spinal canal (coning).
Lumbar puncture should therefore not be
performed if there is papilloedema, a
reduced level of consciousness or focal
neurological signs that may suggest an
underlying space-occupying lesion. It is
also contraindicated in the presence of a
bleeding tendency (e.g. thrombocytopenia,
disseminated intravascular coagulation,
treatment with warfarin). Aspirin
treatment is not a contraindication.
Question 9. B) Worsens as the day
progresses
Explanation: Headache due to raised
intracranial pressure tends to be maximal
on waking in the morning, and improves
or resolves through the day as the upright
posture reduces intracranial pressure. It
often responds well to simple analgesia.
Question 10. C) Tension headache
Explanation: Tension headache is
extremely common and often follows a
chronic course. The pain is usually
generalised and becomes more noticeable
as the day progresses. Although it
responds poorly to analgesia, individuals
are typically able to continue with their
daily activities.
228
Question 11. B) Migraine
Explanation: The history of severe,
throbbing, episodic, unilateral headache
associated with nausea, vomiting and
photophobia in a patient of this age is
highly suggestive of migraine. 'Classical'
migraine consists of a triad of paroxysmal
headache, nausea and vomiting, and an
'aura' of focal neurological events.
However, many patients experience
paroxysmal headache (with or without
vomiting) without aura; this is termed
'common' migraine. When present, the
aura is most often visual, consisting of
shimmering zigzag lines ('fortification
spectra').
Question 12. A) Sumatriptan
Explanation: Avoidance of obvious
precipitants may prevent migraine attacks.
Acute migraine may respond to simple
analgesics (e.g. paracetamol) and antiemetics. Severe attacks can be treated with
one of the 'triptans' (e.g. sumatriptan);
these are 5-hydroxytryptamine agonists
that cause vasoconstriction of the
extracranial arteries, which are thought to
be dilated in migraine. The other agents
listed can all be used to prevent recurrent
migraines but are not useful during an
acute attack.
Question 13. E) Associated nasal
congestion and conjunctival injection
Explanation: Typical cluster headache
comprises episodic severe, unilateral,
periorbital pain. It is associated with
unilateral lacrimation, nasal congestion
and conjunctival injection. Episodes
characteristically last 30-90 minutes and
can occur daily for a few weeks, followed
by respite for several months before
recurrence of another 'cluster'. The
condition is five times more common in
men than women.
Question 14. B) Persistent nystagmus
Explanation: Disorders affecting either
the vestibular nucleus in the brain stem or
its central connections are distinguished
from disorders of the labyrinth by the
persistence of both vertigo and nystagmus.
Positionally induced central vertigo
persists for as long as the head position is
maintained, as does the accompanying
nystagmus. In contrast, peripheral
positional vertigo (and any associated
nystagmus) fatigues quite quickly if the
inducing position is maintained. This
phenomenon of fatigability is seen with
the Hallpike maneouvre (see the link
below). This test is positive in benign
paroxysmal positional vertigo - a
condition, more common in the elderly,
which causes brief episodes of vertigo
with certain head movements. Severe
vertigo lasting a few days associated with
vomiting and ataxia is characteristic of
labyrinthitis. Ménière's disease, another
cause of paroxysmal labyrinthine vertigo,
usually presents initially with tinnitus and
distorted hearing.
Question 15. B) Severely bitten tongue
Explanation: Determining the cause of a
collapse can be difficult and obtaining a
witness account is crucial. Details of the
events immediately before (prodrome) and
after (recovery) provide useful clues.
Vasovagal syncope is typically preceded
by lightheadedness, sensations of heat,
tinnitus and dimming of vision. A history
of aura preceding the blackout suggests
seizure but is often lacking (perhaps due to
post-ictal retrograde amnesia). Cardiac
syncope (e.g. Stokes-Adams attack)
frequently occurs without any warning.
With regard to the event itself, urinary
incontinence and brief twitching of limbs
are non-specific features that may occur
during any syncopal attack. On the other
hand, cyanosis and tongue biting are more
specific to seizure and the finding of a
severely bitten tongue after loss of
consciousness is pathognomonic of a
generalised seizure. Extreme 'death-like'
pallor is characteristic of cardiac syncope.
A prolonged recovery phase characterised
by confusion, headache, drowsiness or
amnesia strongly suggests seizure.
229
Question 16. C) Left pre-central gyrus
Explanation: Partial (focal) seizures
result from paroxysmal discharge of
neurons in a focal area of the cerebral
cortex. The clinical manifestations depend
on the area of cortex involved.
Involvement of the pre-central gyrus
(frontal lobe, motor cortex) causes partial
motor seizures affecting the contralateral
side of the body, while post-central gyrus
(parietal lobe, sensory cortex) activity
leads to partial sensory seizures. Occipital
foci result in partial visual seizures, and
temporal lobe foci can cause rhythmic
smacking of the lips or alterations of
perception (e.g. déjà vu). Partial seizures
are classified as simple partial if
consciousness remains intact, and complex
partial if consciousness is altered. Any
partial seizure may subsequently spread to
the rest of the brain, resulting in a tonicclonic phase (secondary generalisation).
Question 17. D) Alcohol withdrawal
Explanation: Alcohol withdrawal causes
generalised seizures. The other listed
conditions cause focal cerebral pathology
and can therefore result in partial seizures;
these may become secondarily
generalised. Individuals with partial
seizures should undergo brain imaging to
identify focal structural defects.
Question 18. D) He should refrain from
driving until seizure-free for 1 year
Explanation: Patients should be advised
to inform the Driver and Vehicle
Licensing Authority (DVLA) of their
seizure and to refrain from driving until
they are fit-free for 1 year.
Question 19. D) Sodium valproate
Explanation: Anticonvulsant treatment
should generally be considered after two
seizures have occurred. The majority of
patients can be controlled with
monotherapy. Sodium valproate is firstline treatment for primary generalised
epilepsy; carbamazepine is the usual drug
of choice for partial seizures.
Question 20. C) IV diazepam
Explanation: Status epilepticus describes
prolonged seizure activity or recurrent
seizures without full recovery of
consciousness between attacks. It usually
refers to generalised tonic-clonic seizures
and is a medical emergency.
Question 21. B) Muscle fasciculations
Explanation: Muscle wasting and
fasciculations are manifestations of lower
motor neuron lesions (anterior horn cell,
motor root, nerve plexus or peripheral
nerve). All of the other options listed are
signs of upper motor neuron pathology
(motor cortex or corticospinal tracts).
Question 22. D) Parkinson's disease
Explanation: Parkinson's disease is
characteristically associated with a 'pillrolling' tremor which is most pronounced
at rest. The tremor of thyrotoxicosis is best
detected by asking the patient to hold the
arms outstretched (i.e. sustained posture).
Cerebellar lesions cause an intention
tremor which worsens as the hand
approaches a fixed target (identified using
the 'finger-nose' test). A flapping tremor
(asterixis) is observed with metabolic
derangements such as hepatic
encephalopathy and hypercapnia; holding
the arms outstretched with hyperextended
wrists leads to intermittent flapping of the
hands.
Question 23. D) Hemiballismus - brief,
non-purposeful twitching of muscle
groups
Explanation: Hemiballismus refers to
dramatic, flinging movements of the
limbs. These are usually unilateral, and
result from vascular lesions of the
subthalamic structures. The definition
given in option D is that of myoclonus.
Question 24. B) Right-sided cervical
spinal cord lesion
Explanation: This patient has BrownSéquard syndrome, caused by a unilateral
spinal cord lesion.
230
Fibres conveying joint position and
vibration sensation enter the spinal cord at
the posterior horn and pass without
synapsing into the ipsilateral dorsal
columns, from where they ascend to the
brain stem. They synapse with secondorder neurons in the gracile and cuneate
nuclei, which then cross the midline and
ascend to the thalamus. Pain and
temperature sensory fibres, on the other
hand, enter the spinal cord and synapse
with second-order neurons. These cross
the midline at the level of entry and then
ascend in the contralateral spinothalamic
tract to the thalamus. A unilateral cord
lesion will therefore cause ipsilateral loss
of joint position and vibration sensation,
with contralateral loss of pain and
temperature below the level of the lesion.
Ipsilateral upper motor neuron signs
develop due to involvement of the
ipsilateral corticospinal tracts.
Question 25. D) 9
Explanation: •Eye-opening To pain = 2
•Motor response Localises = 5
•Verbal response Incomprehensible
sounds = 2
The Glasgow Coma Scale provides a tool
for objectively assessing a patient's level
of arousal and response to stimuli. It is
particularly useful for monitoring trends in
the level of consciousness.
Question 26. E) Imaging of the brain
(CT or MRI) should be performed in
most patients
Explanation: Anticholinesterases (e.g.
donepezil) may produce modest
improvements in cognitive function in
selected patients with mild or moderate
Alzheimer's disease. Prominent visual
hallucinations would be more suggestive
of Lewy body dementia than Pick's
disease. Infections (e.g. urinary tract
infection, pneumonia) can cause acute
confusion (delirium) and can lead to
decompensation in patients with dementia,
but are not in themselves a cause of
dementia. Brain imaging should be
performed to exclude potentially treatable
pathology (e.g. cerebral tumour, chronic
subdural haematoma), but brain biopsy is
very seldom required.
Question 27. C) Hyperreflexia
Explanation: Features of cerebellar
pathology include ataxia, incoordination of
limb movements (e.g. past pointing),
intention tremor, dysdiadochokinesis
(inability to perform alternating
movements), dysarthria and nystagmus.
Question 28. D) Left homonymous
lower quadrantanopia
Explanation: The anatomy of the visual
pathways is shown in the link below.
Lesions anterior to the optic chiasm cause
visual field defects restricted to one eye,
while lesions posterior to the chiasm cause
homonymous field defects affecting the
contralateral side of the visual field in both
eyes. From the lateral geniculate body in
the thalamus, lower fibres running in the
temporal lobe represent the upper part of
the field, while upper fibres in the parietal
lobe represent the lower part of the field.
A right parietal lesion will therefore cause
a left homonymous lower quadrantanopia.
Question 29. D) Right abducens (VI)
nerve lesion
Explanation: Horizontal diplopia on
rightward gaze implies a problem with
right eye abduction (right VI nerve
stimulates lateral rectus) or left eye
adduction (left III nerve stimulates medial
rectus). A useful tip to remember is that
the outer image always arises from the
paretic eye; the lesion here must therefore
be within the right VI (abducens) nerve or
its nucleus.
Question 30. A) Left oculomotor (III)
nerve
Explanation: The trochlear (IV) nerve
supplies the superior oblique muscle,
while the abducens (VI) nerve supplies
lateral rectus. All other extraocular
muscles are innervated by the oculomotor
(III) nerve. This nerve also supplies
levator palpebrae superioris (which keeps
the upper eyelid open) and the constrictor
pupillae muscle (which mediates papillary
constriction in response to light). Third
nerve palsies therefore lead to ptosis with
a dilated unreactive pupil, and the eye
rests in a 'down and out' position due to
unopposed activity of the lateral rectus and
superior oblique muscles.
231
A Painful third nerve palsy is classical of a
posterior communicating artery aneurysm.
Question 31. B) Horner's syndrome
Explanation: Sympathetic nerve fibres
originating in the hypothalamus pass down
the brain stem and cervical cord to emerge
at T1, then return back up to the eye in
association with the internal carotid artery
and supply the dilator pupillae muscle to
stimulate pupil dilatation. Lesions of the
sympathetic pathway (e.g. due to locally
invasive apical lung tumour) therefore
result in a unilateral small pupil associated
with a partial ptosis and reduced sweating
on that side (Horner's syndrome).
Question 32. D) The ability to wrinkle
the forehead is preserved
Explanation: The term 'Bell's palsy' refers
to an isolated idiopathic facial nerve (VII)
palsy. There is lower motor neuron
weakness on the affected side, with a
facial droop and an inability to wrinkle the
forehead. Other features include difficulty
closing the affected eye, reduced tear and
saliva secretion, and reduced taste
sensation. Hyperacusis may occur if the
nerve to stapedius (a branch of the facial
nerve) is involved. Preservation of the
ability to wrinkle the forehead on the
affected side indicates an upper motor
neuron pattern of facial weakness.
Question 33. E) Treatment with
warfarin
Explanation: Patients who are
anticoagulated with warfarin or who have
a non-iatrogenic coagulopathy require
urgent imaging of the brain to rule out the
possibility of an intracerebral
haemorrhage.
Question 34. D) Loss of consciousness
Explanation: The definition of a TIA is
the rapid onset of a focal neurological
deficit, of presumed vascular origin, that
resolves within 24 hours. It also includes
transient monocular blindness due to
vascular occlusion in the retina (amaurosis
fugax). Basilar ischaemia can cause loss of
consciousness but is very uncommon and,
as a general rule, the diagnosis of TIA
should not be made in patients who
present with episodes of syncope,
dizziness or confusion as these do not
reflect focal cerebral dysfunction.
The evidence to support surgery in
symptomatic patients with moderate (5069%) stenosis and asymptomatic patients
with severe stenosis is less conclusive, as
these patients have a smaller benefit/risk
ratio than patients with severe
symptomatic stenosis. Patients with
stenosis of < 50% do not benefit from
carotid endarterectomy, irrespective of
symptoms. Finally, a patient with severe
residual disability would gain little benefit
from preventing a further stroke within the
same territory and may have a greater risk
of surgical complications.
Question 35. D) Warfarin
Explanation: In addition to lifestyle
modifications, antiplatelet, lipid-lowering
and antihypertensive therapy forms the
cornerstone of secondary prevention for
most patients with an ischaemic stroke.
Recent large-scale randomised trials have
demonstrated the benefit of statins and
antihypertensives in these patients, even
with blood pressure and cholesterol levels
within the 'normal' range. There is no net
benefit in prescribing anticoagulants after
ischaemic stroke to patients in sinus
rhythm. The evidence base for stroke
secondary prevention is included in the
link below.
Question 37. B) CT head scan
Explanation: The clinical signs and
symptoms in this patient are suggestive of
a subarachnoid haemorrhage. An
emergency head CT scan is essential.
About 15% of patients with a
subarachnoid haemorrhage will have a
normal CT scan; in these cases, a lumbar
puncture should be performed 12 hours
following the onset of headache to look for
xanthochromia (breakdown products of
red blood cells).
Question 36. C) Left middle cerebral
artery territory infarct with good
functional recovery, 80% left carotid
artery stenosis
Explanation: Carotid endarterectomy
reduces the risk of stroke in patients with
severe stenosis of the internal carotid
artery but carries a significant risk of
perioperative mortality and stroke.
Decisions on whether to operate must,
therefore, be based on a careful
benefit/risk analysis. The absolute
reduction in risk of future stroke is greatest
for symptomatic patients with 70-99%
stenosis and, in general, outweighs the risk
of surgical complications. Importantly,
symptomatic patients are defined as
patients with a TIA or non-disabling
stroke in the territory of the carotid artery
on the same side as the stenosis in the
preceding 6 months.
232
Question 38. E) Hypercholesterolaemia
Explanation: Cerebral venous thrombosis
is uncommon. Hypercholesterolaemia and
hypertension are risk factors for arterial
thromboembolic disease, but not for
venous occlusion.
Question 39. C) It follows a relapsing
and remitting course in the majority of
patients
Explanation: Multiple sclerosis (MS) is
characterised by inflammation and patchy
demyelination within the central nervous
system (CNS). The condition is more
common in females and peak age of onset
is between 30 and 40 years. MS can
present with diverse neurological features
according to the areas of the CNS
involved. Optic neuritis (optic nerve),
sensory symptoms and leg weakness
(spinal cord), and ataxia (cerebellar fibres)
occur frequently but intellectual function
is usually preserved until the later stages
of the disease. Most patients experience a
relapsing-remitting course, while 20%
have primary progressive MS. Although
there is no single diagnostic investigation,
plaques of CNS demyelination can be seen
on MRI. The presence of oligoclonal
bands of IgG in the cerebrospinal fluid is
consistent with (but not specific for) a
diagnosis of MS.
Question 40. B) Methylprednisolone
Explanation: Pulsed high-dose steroids
(methylprednisolone) reduce the duration
of relapses by means of their antiinflammatory effect. Interferon beta is an
immune modulator which reduces the
number of relapses by 30%. Azathioprine
also has some effect in reducing relapses
and improving long-term outcome.
Plasmapheresis and IV immunoglobulin
are occasionally used in severe disease.
Question 41. B) Senile plaques and
neurofibrillary tangles are
characteristic features on brain
histology
Explanation: Alzheimer's disease is the
most common cause of dementia, affecting
5% of the population over 65 years of age
and 30% over 80. Histology from the brain
typically reveals senile plaques
(containing amyloid) and neurofibrillary
tangles. Although both short- and longterm memory are affected, defects in the
former are generally more obvious and
occur earlier. CT head scan typically
shows cerebral atrophy, but there are no
specific appearances that are
pathognomonic for Alzheimer's disease.
Treatment with anticholinesterase drugs
may lead to modest improvements in
cognitive function in selected patients but
they do not halt progression of the disease.
Question 42. B) Parkinson's disease
Explanation: Parkinson's disease is an
idiopathic condition characterised by
depletion of dopaminergic neurons in the
substantia nigra. It is classically composed
of the triad of tremor, rigidity and
bradykinesia. A fine resting tremor is
usually first seen in the fingers and thumb,
and is characteristically 'pill-rolling' in
nature. Rigidity (increased muscle tone)
causes stiffness and a flexed posture.
Coexistent tremor causes cogwheel
rigidity. Bradykinesia (slowness of
movement) is manifest by slowness of gait
and difficulty with tasks such as fastening
buttons and writing.
Question 43. B) Wide-based gait
Explanation: An unsteady wide-based
gait (ataxia) is a feature of cerebellar
disease. It is also seen in conditions with
impaired joint position sensation.
233
Question 44. D) Dyskinesia secondary to
levodopa can be improved by modifying
the dosing regimen
Explanation: The rationale for giving
levodopa (a dopamine precursor) in
Parkinson's disease is to boost dopamine
production in the remaining dopaminergic
neurons of the substantia nigra. However,
if it is given as monotherapy, more than
90% is decarboxylated peripherally,
preventing it from reaching the brain and
leading to a high incidence of side-effects.
This is overcome by coadministering a
peripheral dopa-decarboxylase inhibitor
(carbidopa or benserazide). As these do
not cross the blood-brain barrier they
prevent conversion to dopamine in the
periphery but allow it to occur in the brain.
Involuntary movements (dyskinesia) are
related to long-term use of levodopa
therapy. Initiation of levodopa should
therefore be delayed until there is
significant disability, especially in younger
patients. Dyskinesia can be improved by
modification of the drug dose and
frequency of administration. Levodopa
may help tremor in some patients but is
generally more effective at relieving
bradykinesia and rigidity. Anticholinergic
drugs may be useful in treating tremor and
rigidity.
Question 45. E) Haloperidol
Explanation: Neuroleptic agents (e.g.
haloperidol, chlorpromazine) and certain
anti-emetics (e.g. metoclopramide) have
anti-dopaminergic actions and can
therefore cause parkinsonism
Question 46. A) It has autosomal
recessive inheritance
Explanation: Huntington's disease is an
autosomal dominant disorder characterised
by involuntary choreiform movements.
Symptoms usually develop in middle age,
by which time individuals have often had
children. Genetic screening is available for
asymptomatic family members after
appropriate counselling. Involuntary
movements are accompanied by
psychiatric symptoms which eventually
progress to frank dementia.
234
Question 47. B) Motor neuron disease
Explanation: Motor neuron disease is a
progressive disorder caused by
degeneration of motor neurons in the
spinal cord and cranial nerve nuclei, and
of pyramidal neurons in the motor cortex.
Patients present with muscle weakness,
and neurological examination reveals a
combination of lower motor neuron (e.g.
wasting, fasciculations) and upper motor
neuron (e.g. increased tone, brisk reflexes,
extensor plantars) signs. Sensation is
normal. Involvement of the lower cranial
nerves may cause bulbar palsy with
dysarthria and dysphagia.
Question 48. C) Administer IV
benzylpenicillin
Explanation: The presence of headache,
fever and neck stiffness in association with
a purpuric rash is strongly suggestive of
meningococcal meningitis. This is a
medical emergency requiring resuscitation
and immediate treatment with empirical
IV antibiotics. Although a lumbar
puncture is required, this must not delay
antimicrobial therapy. A CT head scan
should be performed before lumbar
puncture if there are clinical signs of
possible raised intracranial pressure (e.g.
drowsiness, focal neurological deficit,
seizures).
Question 49. B) Upper motor neuron
signs predominate
Explanation: Poliomyelitis is caused by
an enterovirus. Involvement of anterior
horn cells results in lower motor neuron
signs (flaccid weakness, fasciculations,
areflexia). Treatment consists of bed rest
and physiotherapy. Respiratory muscle
involvement may necessitate invasive
ventilation via a tracheostomy. Childhood
immunisation with an oral vaccine has
dramatically reduced the incidence of
polio in many countries.
Question 50. C) Cerebral abscess
Explanation: The CT scan shows a single
low-density area with ring enhancement in
the right temporal lobe, consistent with a
cerebral abscess. There is associated
cerebral oedema and midline shift to the
left. The condition typically presents over
days or weeks with features of raised
intracranial pressure, seizures and focal
neurological signs. The main differential
diagnosis is a cerebral tumour.
Question 51. E) Tetanus antitoxin
should be administered in all suspected
cases
Explanation: The bacterium Clostridium
tetani is found in soil and usually enters
the body through contaminated wounds. It
multiplies only in anaerobic conditions,
e.g. necrotic tissue. The organism itself
remains localised but produces an
exotoxin that affects anterior horn cells.
The most important early symptom is
spasm of the masseter muscles, which
causes difficulty in opening the mouth and
chewing (trismus or lockjaw). The rigidity
spreads to the rest of the body and causes
violent convulsions. Treatment comprises
IV human tetanus antitoxin to neutralise
absorbed toxin, and wound debridement
and benzylpenicillin to prevent further
toxin production (toxoid).
Question 52. C) Cognitive function is
usually preserved
Explanation: Creutzfeldt-Jakob disease
(CJD) is a spongiform encephalopathy
mediated by a prion protein. Spongiform
change in the brain is associated with
neuronal loss and gliosis in the grey
matter. Clinical features include
myoclonic jerks and a rapidly progressive
dementia. Repetitive slow wave
complexes on EEG are characteristic, and
life expectancy is reduced to 4-6 months.
Question 53. B) Primary intracerebral
tumours do not, generally, metastasise
outside the central nervous system
Explanation: Primary intracerebral
tumours do not metastasise outside the
central nervous system, even if malignant.
235
However, metastases to the brain can
occur from extracranial primary tumours
(e.g. lung, breast, gastrointestinal tract).
MRI offers better resolution than CT, and
is particularly useful for imaging
structures in the posterior fossa (brain
stem and cerebellum). The steroid
dexamethasone reduces oedema
surrounding cerebral tumours, and can
often lead to an improvement in conscious
level. Meningiomas are benign tumours
arising from the meninges, whereas
gliomas (e.g. astrocytoma) arise from the
brain substance; the former are therefore
easier to resect completely and carry a
better prognosis.
Question 54. C) Cerebellar signs may be
present
Explanation: Acoustic neuroma is a
benign tumour arising from the Schwann
cells of the VIII (vestibulocochlear)
cranial nerve. The condition may arise
sporadically or in association with
neurofibromatosis type 2. Sensorineural
deafness is extremely common. The
tumour is located in the cerebellopontine
angle; distortion of the cerebellum can
therefore lead to ataxia and cerebellar
signs in the limbs. As the lesion is situated
in the posterior fossa, MRI is the
investigation of choice. Treatment is by
surgical resection.
Question 55. C) Idiopathic (benign)
intracranial hypertension
Explanation: Idiopathic (benign)
intracranial hypertension is characterised
by raised intracranial pressure in the
absence of a space-occupying lesion or
ventricular dilatation. The condition tends
to affect young obese women. Other risk
factors include drugs (e.g. tetracyclines,
vitamin A), Addison's disease and
withdrawal of steroid therapy. Patients
complain of headache, and papilloedema
is usually the only clinical finding. CT of
the head is normal and lumbar puncture
demonstrates elevated CSF pressure with
normal constituents.
Question 56. E) Acetazolamide
Explanation: Treatment of idiopathic
intracranial hypertension includes weight
loss and withdrawal of precipitating
factors. Other measures to lower
intracranial pressure include the carbonic
anhydrase inhibitor, acetazolamide, and
repeated therapeutic lumbar puncture.
Cervical cord compression would produce
motor and sensory signs in all four limbs
(see the link below). The spinal cord ends
at the T12/L1 spinal level; below this
hangs a collection of nerve roots called the
cauda equina. Lesions compressing the
cauda equina therefore only cause lower
motor neuron signs in the lower limbs.
Question 57. C) Headache
Explanation: Normal pressure
hydrocephalus is characterised by the triad
of gait apraxia, dementia and urinary
incontinence. Headache is not a feature.
The condition predominantly affects older
patients.
Question 61. C) Spinal MRI scan
Explanation: Spinal MRI is the
investigation of choice for identifying
compression of the spinal cord or nerve
roots. Urgent investigation is required to
enable prompt treatment. Soft tissue detail
is excellent, and it is often possible to
determine the reason for the cord
compression (e.g. spinal metastases). This
helps guide further therapy in terms of
surgery or radiotherapy.
Question 58. D) S1
Explanation: Sudden onset of lower back
pain while straining, accompanied by
'sciatica' and a positive straight leg raise
test, suggests lumbar disc herniation with
resultant nerve root compression. The
neurological findings described
correspond to pressure on the S1 root.
Question 59. B) Analgesia and early
mobilization
Explanation: The vast majority of
patients with sciatica recover with a
combination of analgesia and early
mobilisation. Bed rest retards recovery.
Local anaesthetic or steroid injections are
useful if there is associated ligamentous
injury or joint dysfunction. Surgery is
usually considered only if there is no
response to conservative treatment or if
there is progressive neurological disability.
Radiotherapy is useful only in patients
with spinal cord or nerve root compression
secondary to malignancy.
Question 60. C) Thoracic cord
compression
Explanation: This patient has signs of
spinal cord compression, which is likely to
be secondary to bony metastases. The
presence of bilateral upper motor neuron
signs in the legs (spastic paraparesis), with
preserved upper limb function and a
sensory level on the abdomen, suggests
involvement of the thoracic spinal cord.
236
Question 62. D) Multiple sclerosis
Explanation: Peripheral neuropathies can
affect a single nerve (mononeuropathy) or
several discrete nerves (mononeuritis
multiplex), or be generalised
(polyneuropathy). There are multiple
causes, the most common of which are
diabetes mellitus, alcohol excess, GuillainBarré syndrome, hereditary neuropathies,
vitamin deficiencies and drug toxicity.
Question 63. A) Amiodarone
Explanation: See list of Drugs causing
peripheral neuropathy
Question 64. B) Median nerve
Explanation: This patient has carpal
tunnel syndrome, a mononeuropathy
affecting the median nerve. Symptoms are
often self-limiting and a wrist splint may
provide some relief. More severe or
persisting symptoms may require surgical
decompression at the wrist.
Question 65. D) Respiratory muscles are
not affected
Explanation: Guillain-Barré syndrome is
an acute inflammatory polyneuropathy
caused by cell-mediated demyelination of
peripheral and cranial nerves. It is often
preceded by a respiratory infection or
diarrhoeal illness (usually
Campylobacter). Patients develop rapidly
ascending muscle weakness, starting in the
lower limbs and spreading up to the upper
limbs. Involvement of the respiratory
muscles can lead to respiratory failure and
necessitate ventilatory support. The
majority of patients make a complete
recovery over 3-6 months. Early treatment
with IV immunoglobulin or plasma
exchange shortens the duration of
ventilation and improves prognosis.
Question 66. C) Myasthenia gravis
Explanation: The fatigable muscle
weakness is typical of myasthenia gravis.
Symptoms worsen with exercise and as the
day progresses. Features include
intermittent ptosis, diplopia (due to
extraocular muscle involvement), and
weakness of chewing, swallowing,
speaking and limb movement. There is no
sensory deficit. The condition is more
common in women and usually presents
between the ages of 15 and 50 years.
Question 67. E) The presence of muscle
paralysis with fasciculation, sweating
and excessive salivation suggests a
myasthenic crisis
Explanation: Myasthenia gravis is caused
by autoantibodies directed against
acetylcholine receptors in the post-
237
synaptic membrane of the neuromuscular
junction. IV injection of the short-acting
anticholinesterase edrophonium (the
Tensilon test) increases the available
levels of acetylcholine and produces a
transient improvement in muscle power.
Longer-acting anticholinesterases (e.g.
pyridostigmine) are used in the treatment
of myasthenia. Thymectomy in patients
with antibody-positive disease is
associated with a better prognosis,
irrespective of whether or not a thymoma
is present. Sudden, severe weakness in
myasthenia may be due to exacerbation of
the disease (myasthenic crisis) or
excessive treatment with
anticholinesterase drugs (cholinergic
crisis). Differentiating between the two is
vital and the presence of fasciculations,
sweating and excessive salivation suggests
a cholinergic crisis.
Question 68. C) Delayed relaxation of
skeletal muscle
Explanation: Myotonic dystrophy is an
autosomal dominant condition caused by
an expanded triplet repeat on chromosome
19. The characteristic finding is myotonia,
an abnormality of muscle relaxation. This
can be elicited by asking the patient to
make a fist and then rapidly straighten the
fingers; the latter can only be performed
slowly in patients with myotonic
dystrophy. Other features include cardiac
conduction abnormalities, lens opacities,
frontal balding and cognitive impairment.
Autoantibodies to presynaptic calcium
channels are a feature of Lambert-Eaton
myasthenic syndrome.
Chapter
26 SKIN DISEASE
Question 1. C) Chronic plaque psoriasis
Explanation: The picture shows nail
pitting and onycholysis (separation of the
nail from the nail bed), both of which are
classical of psoriasis. Nail changes are
common in psoriasis and also include
subungual hyperkeratosis. Neither the
description nor the clinical photograph
would be consistent with any of the other
differentials listed.
Question 2. B) It is the only skin disease
to demonstrate the Köbner
phenomenon Explanation: The Köbner
phenomenon describes the tendency of a
lesion to arise in areas of previous trauma,
such as skin biopsy sites and old surgical
scars. Although psoriasis does exhibit the
Köbner phenomenon, so do a number of
other conditions, including lichen planus
and vitiligo. Psoriasis classically has a
predilection for the extensor surfaces of
the limbs. The Auspitz sign is
pathognomonic of psoriasis, and describes
the minute capillary bleeding that occurs
on lifting a psoriatic scale. Nail changes
are common and also include onycholysis.
The pustules which may feature are sterile.
Question 3. C) Penicillin antibiotics
Explanation: All of the above have been
associated with flares in psoriasis, except
for penicillin antibiotics. Although not
mentioned above, alcohol intake is
described by many patients as an
exacerbant of psoriasis.
238
Question 4. E) Gold
Explanation: All of the above except gold
are used to good effect in the management
of refractory psoriasis; gold is a diseasemodifying drug used in rheumatoid
arthritis. Psoralens are natural
photosensitisers used in combination with
long-wavelength ultraviolet A (PUVA)
therapy.
Question 5. B) Episodes often last longer
than 24 hours
Explanation: Urticaria refers to an area of
focal dermal oedema secondary to an
increase in capillary permeability. It is
more commonly known by patients as
'hives', and demonstrates a characteristic
weal and flare reaction. Episodes, by
definition, last less than 24 hours. There
are numerous possible precipitants, all of
which trigger mast cell degranulation,
leading to release of histamine and a range
of other inflammatory mediators.
Correspondingly, antihistamines improve
symptoms but do not abolish them
completely.
Question 6. A) Streptococcus pyogenes
Explanation: Guttate psoriasis often
occurs in children and adolescents after a
streptococcal sore throat. The fungus T.
rubrum is a common cause of ringworm of
the trunk. P. acnes is a bacterium which
colonises the pilosebaceous ducts in acne
and produces pro-inflammatory factors. B.
burgdorferi is the causative organism in
Lyme disease, one of the features of which
is erythema chronicum migrans, an
annular skin lesion which spreads, clearing
centrally. S. scabiei causes scabies, an
intensely itchy dermatosis characterised by
'burrows' in the web-spaces of the hands.
Question 7. D) Necrobiosis lipoidica
Explanation: The clinical description and
the photograph correlate best with the
diagnosis of necrobiosis. Skin conditions
which occur with greater frequency in
diabetics than in the normal population
also include acanthosis nigricans and
granuloma annulare.
Question 8. D) Topical or intralesional
steroids may be useful
Explanation: Necrobiosis lipoidica occurs
with greater frequency but not exclusively
in patients with diabetes. There is no
correlation between degree of glycaemic
control and severity of the skin disease,
and although superinfection may occur, no
infective organism is implicated in the
pathogenesis. The lesions readily ulcerate
and subsequently tend to heal slowly.
Question 9. E) Basal cell carcinoma
Explanation: The appearance of this
lesion is classical for a basal cell
carcinoma (BCC) or 'rodent ulcer'. These
are slow-growing tumours of the basal cell
layer of the epithelium that occur most
commonly on the face of elderly
individuals. Their clinical appearance is
characterised by a pearly, telangiectatic
edge, with a central ulcer.
Question 10. E) Local invasion is more
common than haematogenous spread
Explanation: Basal cell carcinomas
(BCCs) are slow-growing tumours which
very rarely metastasise. They are usually
removed by surgical excision. Cryotherapy
has significant comorbidity when used for
anything other than superficial lesions;
radiotherapy can be used for larger lesions,
but surgery tends to produce the best
cosmetic result. Mohs' surgery is a special
kind of 'tissue-conserving' surgery, in
which excised tissue margins are
examined histologically then extended
successively by millimeters until they are
clear. Although time-consuming, this
method ensures that the bare minimum of
tissue is taken.
239
Question 11. C) Warty texture with
'stuck-on' appearance
Explanation: In assessing any mole, the
principal concern is to exclude malignant
melanoma. A naevus with a warty, 'stuckon' appearance is much less worrisome
than one which demonstrates any of the
other features listed. A warty, 'stuck-on'
appearance is more suggestive of a
seborrhoeic wart, which is a benign
epidermal tumour. A useful mnemonic to
help remember worrying features in a
mole is 'ABCDE' this is explained in the
link below.
Question 12. D) Amelanotic melanomas
are more common than the pigmented
variety
Explanation: Melanoma is classified into
four basic subtypes: superficial spreading,
lentigo maligna, nodular and acral
lentiginous. The characteristics of each
should be known. Amelanotic melanomas
(those without pigment) are very rare;
careful examination with a dermatoscope
will usually reveal a few flecks of colour.
Question 13. A) Dark skin and black
hair
Explanation: The phenotype of red hair
and pale skin is associated with an
increased risk of skin cancer, due to
exposure to ultraviolet radiation in the
absence of adequate melanin
pigmentation. The corollary of this is that
those with dark skin have a relatively
reduced risk of developing skin cancer. All
of the other factors mentioned are
associated with an increased risk of skin
cancer.
Question 14. A) Atopic eczema
Explanation: This history is pretty
classical for atopic eczema. The child has
an itchy rash in the skin creases, which
began within the first 2 years of life, and
there is also a history of asthma, one of the
atopic spectrum of disorders. (These
comprise hay fever, asthma and a tendency
towards allergy: for example, to animal
dander.) Lichenification describes the skin
changes that occur with prolonged periods
of scratching and rubbing, resulting in
increased skin markings. It is a feature of
many skin diseases.
Question 15. D) Dithranol
Explanation: Dithranol is an anthralin
used in the topical treatment of psoriasis.
All of the other agents are important
elements of the management of childhood
atopic eczema. Topical steroids should be
used at an appropriate strength for the site
to which they are applied; for instance, as
a general rule, nothing stronger than 1%
hydrocortisone should be applied to the
face, where the skin is thinner than the rest
of the body. It may necessary to use more
potent steroids elsewhere.
Question 16. D) Bullous pemphigoid
Explanation: The paucity of oral mucous
membrane involvement in bullous
pemphigoid is one of the key
distinguishing features between this
condition and pemphigus. Pemphigus and
Stevens-Johnson syndrome may feature
bullous lesions of the mucous membranes.
SLE may feature oral ulceration.
Examination of the mouth of a patient with
lichen planus may reveal Wickham's striae
(a fine white lacy network overlying the
buccal mucosa).
Question 17. A) Discoid lupus
erythematosus causes a non-scarring
alopecia
Explanation: Discoid lupus causes a
scarring alopecia. Alopecia areata
describes a non-scarring patchy hair loss
which is associated with other
autoimmune conditions, including vitiligo
and thyroid disease.
240
A more extensive form of hair loss, called
alopecia totalis, describes loss of all scalp
hair with preservation of body hair.
Alopecia universalis describes loss of all
scalp and body hair. Androgenetic
alopecia may occur in both males and
females.
Question 18. C) Antibiotics
Explanation: The lesions are those of
erythema nodosum, a panniculitis
(inflammation in the deep dermis and
subcutaneous fat). The nodules are
characteristically painful, and although
there are many infective causes such as
tuberculosis and streptococcal infections
(hence a chest X-ray and ASO titre would
be appropriate investigations), antibiotics
do not form part of the management of this
condition. There a number of drug causes,
and it is particularly important to ask
females about oral contraceptive use.
Systemic diseases such as sarcoidosis are
also associated.
Question 19. C) Macules are usually
raised
Explanation: A macule is a small, flat
area of altered colour or texture.
Question 20. D) Bullous impetigo
Explanation: All of the above rashes are
characteristically itchy with the exception
of bullous impetigo, which is a
staphylococcal infection of skin, common
in young children and the
immunocompromised. It occurs when the
infecting staphylococci produce
exfoliatoxin A or B, which causes
blistering lesions to arise.
Question 21. E) Atenolol
Explanation: All the drugs listed above
may cause photosensitivity, with the
exception of atenolol. None of the drugs in
the ß-blocker class are associated with
photosensitivity.
Question 22. C) Patients are usually
over the age of 18 years
Explanation: SSSS is a serious exfoliative
skin condition that predominantly affects
children, particularly neonates.
Question 23. B) Onycholysis Psoriasis
Explanation: Nail changes are common in
psoriasis and include pitting, onycholysis
(separation of the nail plate from the nail
bed) and subungual hyperkeratosis.
Koilonychia (spoon-shaped nails) is a sign
of iron deficiency, while leuconychia
(whitening of the nails) is a rare
manifestation of hypoalbuminaemia.
Fibrosing alveolitis may cause clubbing,
as may cyanotic congenital heart disease.
Beau's lines, transverse grooves in the
nails, are a non-specific manifestation of
any acute illness.
241
Question 24. D) Diabetes mellitus
Explanation: Diabetes is associated with
several skin conditions but not porphyria
cutanea tarda.
Question 25. B) Digoxin
Explanation: Erythema multiforme (EM)
is characterised by targetoid lesions that
have a 'bull's-eye' appearance. Blisters
may feature; severe bullous EM is called
Stevens-Johnson syndrome.