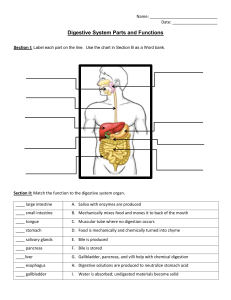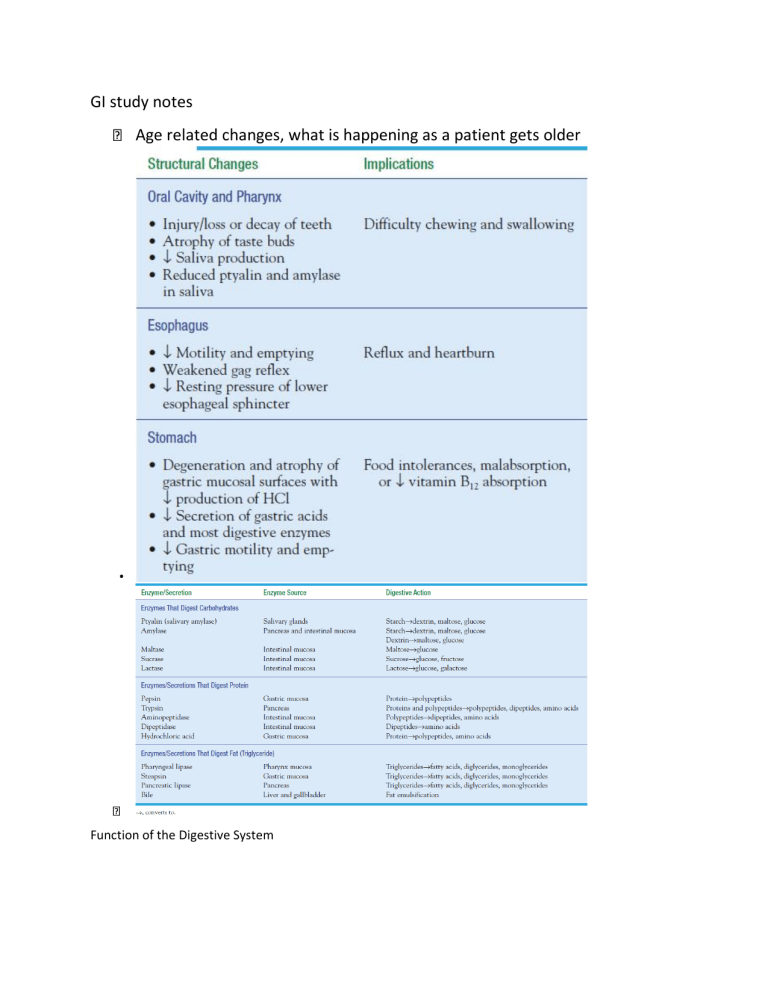
GI study notes Age related changes, what is happening as a patient gets older Function of the Digestive System All cells of the body require nutrients. These nutrients are derived from the intake of food that contains proteins, fats, carbohydrates, vitamins, minerals, and cellulose fibers and other vegetable matter, some of which has no nutritional value. Major functions of the GI tract include: • • • Breakdown of food particles into the molecular form for digestion Absorption into the bloodstream of small nutrient molecules produced by digestion Elimination of undigested unabsorbed foodstuffs and other waste products After food is ingested, it is propelled through the GI tract, coming into contact with a wide variety of secretions that aid in its digestion, absorption, or elimination from the GI tract. How is the body going to compensate to bring the body back to homeostasis? How does nutrition play a role in the GI system? Pancreatic secretions have an alkaline pH due to their high concentration of bicarbonate. This alkalinity neutralizes the acid entering the duodenum from the stomach. Digestive enzymes secreted by the pancreas include trypsin, which aids in digesting protein; amylase, which aids in digesting starch; and lipase, which aids in digesting fats. What is the role of nutrients, absorption, digestion, enzymes. What are their roles? • • • Digestion: begins with the act of chewing, in which food is broken down into small particles that can be swallowed and mixed with digestive enzymes Absorption: Absorption is the major function of the small intestine. Vitamins and minerals absorbed are essentially unchanged. Absorption begins in the jejunum and is accomplished by active transport and diffusion across the intestinal wall into the circulation Elimination: phase of the digestive process that occurs after digestion and absorption when waste products are eliminated from the body Function of the GI organ system: Stomach: left side - under left lobe of liver, • overlays most of pancreas, hollow, and holds about 1,500 mL. Small Intestine: longest segment. 2/3 of intestine. approx. 230 feet of surface area for absorption & secretion. (About 7,000 cm) Function of the Digestive System: Digestion of food Absorption of nutrients (into the bloodstream) Elimination Function of Stomach: stores & secretes fluids HCL (hydrochloric acid)- breaks down food. pH= 1.3- secreted in response to presence of food Pepsin: IMPORTANT for protein digestion Intrinsic Factor: Important for B12 absorption • • Accessory Digestive Organs Pancreas* Trypsin- protein Amylase- Starch Lipase- fats Liver: Bile, secreted by liver, Stored in the Gallbladder Bile aids in emulsifying fats, and absorption Digestive Function 2 types of secretions in colon: Bicarbonate solution Mucus This is slow transport- allowing for reabsorption of water & electrolytes Reaches rectum in about 12 hours As much as ¼ of the waste from 3 days ago can be in rectum Fecal matter is about 75% fluid and 25% waste, largely unaffected by alterations in diet. Brown color is from breakdown of bile Digestive Function: Gerontological Considerations Older Adults: There seems to be an increase in many GI disorders of function & motility Normal changes with aging Loss of teeth Loss of taste Decreased gastric motility & emptying Decreased tone of anal sphincter Assessing the GI System Health History: Pain Dyspepsia Intestinal Gas Nausea / Vomiting Change in bowel habits: color , consistency, frequency Social HX What happens if you don’t get those nutrients Fat soluble ADEK Water soluble BC, where are they absorbed and stored. Intrinsic factor. What is you don’t have a stomach; how does it affect the intrinsic factor and B12, what does B12 do for the body? (liver or stomach) How do electrolytes relate to the GI tract Gastritis, inflammation, what are some of the causes of it (H pylori) Peptic ulcer, what is it? What does it affect and where? Is absorption taking place or bleeding? The main place is anal. What can irritate it? Abdominal assessment? Where are they located? How do we assess them? Lifestyle changes H. Pylori, what type of meds. Diet, smoking, alcohol, when would surgery be in play. What education given to a patient. Gastric cancer, causes, tx Tumor of small intestine, tx for benign and malignant What diagnostic are used for GI tract? ESR/CRP. CBC, BNP electrolytes Diverticulitis, fistula What are the reasons for constipation What are the reasons for diarrhea, more than 3 per day with an altered consistency? Acute, chronic Looking at fluid Constipation: pg 1313 definition recognize why they have it (laxative) Know your CM Valsalva maneuvered, how does it affect and what is the complication of it when straining Hemorrhoids Chronic constipation Non inflammatory, what are some of the pathogens with diarrhea? What is malabsorption, what is the diagnostic? Incontinence, what are the causes, how do we educate? What can we do to help our patients with incontinence? Why does it occur Celiac disease. Autoimmune cannot digest gluten. Lifestyle changes for the patient. IBS: recurrent abdominal pain with bowel movements. Motility, things are not moving or neuroendocrine. What are diagnostic and what are the CM other than diarrhea or constipation? What is medical management for it? Fluids and food, what is the correlation? Page 1318 - Mucosal (transport) disorders causing generalized malabsorption (e.g., celiac disease, Crohn’s disease, radiation enteritis) Luminal disorders causing malabsorption (e.g., bile acid deficiency, Zollinger–Ellison syndrome, pancreatic insufficiency, small bowel bacterial overgrowth, or chronic pancreatitis) Lymphatic obstruction, interfering with transport of fat by products of digestion into the systemic circulation (e.g., neoplasms, surgical trauma). Peritonitis: What to do for it, is it a medical emergency? Appendicitis Diverticulitis Pg. 1325 diagnosed is colonoscopy Small bowel obstruction. LBO electrolytes may require surgery Know your goals of a bowel obstruction TABLE 47-4 Mechanical Causes of Intestinal Obstruction UC think of bloody with pus in it and located in the rectum, descending colon. Is at the bottom. Chrones diarrhea can be from mouth to anus is non-continues TABLE 47-5 Comparison of Crohn’s Disease and Ulcerative Colitis (autoimmune) know. Slow dose immunosuppressant, lifestyle changes. Know the difference between UC and Crohn's, which is continuing and which is not. Gallbladder: main purpose storage and concentration of bile. What is bile, its water, and electrolytes? Main purpose is to break down fat. Pancreases: function of it. Endocrine is your insulin hormones and exocrine digestive enzymes (amylase, lipase, trypsin) what do they digest Chapter 50, it self-digest the pancrease is the acute. Chronic Vitamins are (coenzyme) allow this to occur Endocrine and insulin, what is the purpose of glucose in the body What is pancreatitis? Acute and chronic, know what is happening. Know the tx, pain management, NPO, check BS. What diagnostic? What are some of the enzymes. ERCP Amylase and lipase. Fluids. Usually occurs 24-48 hours after a heavy meal. Severe abdominal pain, tenderness and back pain. Chart 50-3 page 1441 how serious pancreatitis is? Chronic pancreatitis? What causes it. Chronic pancreatitis is an inflammatory disorder characterized by progressive destruction of the pancreas. Chart 50-4 PLAN OF NURSING CARE Pancreatic Cysts, why is it occurring. 4-6 weeks after pancreatitis CA of pancreas 4th leading cause of death in men and 5th in women Pain, jaundice, weight loss, liver failure. If just a tumor can just remove. What is the nursing care s/p, monitor BS Post-surgery from pancreases Alpha cells release glucagon. delta cells, beta cells insulin sumatastatin hormone to tell it to stop Liver Chart 49-1 page 1380 Is the liver firm or soft What is jaundice? The different types Obesity: –Overweight = BMI 25 to 29.9 Obese = BMI exceeding 30 Severe/extreme obese = BMI exceeding 40 Know A,D, K & B12 5 to 6 liters is a safe amount to remove for paracentisis. Cholelithiasis know the RF/Educate patient Chart 50-1 Educate on shoulder pain after surgery d/t air inflation. What is bile? What are the components? The function of the gall bladder.