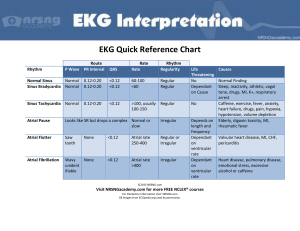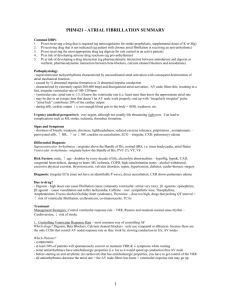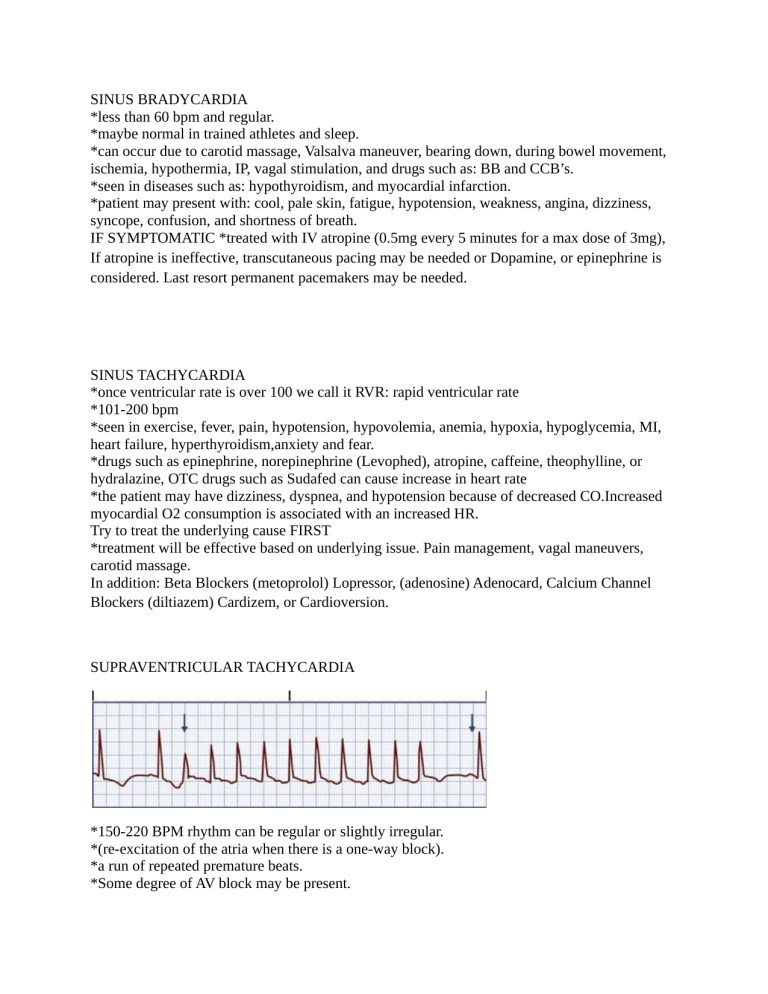
SINUS BRADYCARDIA *less than 60 bpm and regular. *maybe normal in trained athletes and sleep. *can occur due to carotid massage, Valsalva maneuver, bearing down, during bowel movement, ischemia, hypothermia, IP, vagal stimulation, and drugs such as: BB and CCB’s. *seen in diseases such as: hypothyroidism, and myocardial infarction. *patient may present with: cool, pale skin, fatigue, hypotension, weakness, angina, dizziness, syncope, confusion, and shortness of breath. IF SYMPTOMATIC *treated with IV atropine (0.5mg every 5 minutes for a max dose of 3mg), If atropine is ineffective, transcutaneous pacing may be needed or Dopamine, or epinephrine is considered. Last resort permanent pacemakers may be needed. SINUS TACHYCARDIA *once ventricular rate is over 100 we call it RVR: rapid ventricular rate *101-200 bpm *seen in exercise, fever, pain, hypotension, hypovolemia, anemia, hypoxia, hypoglycemia, MI, heart failure, hyperthyroidism,anxiety and fear. *drugs such as epinephrine, norepinephrine (Levophed), atropine, caffeine, theophylline, or hydralazine, OTC drugs such as Sudafed can cause increase in heart rate *the patient may have dizziness, dyspnea, and hypotension because of decreased CO.Increased myocardial O2 consumption is associated with an increased HR. Try to treat the underlying cause FIRST *treatment will be effective based on underlying issue. Pain management, vagal maneuvers, carotid massage. In addition: Beta Blockers (metoprolol) Lopressor, (adenosine) Adenocard, Calcium Channel Blockers (diltiazem) Cardizem, or Cardioversion. SUPRAVENTRICULAR TACHYCARDIA *150-220 BPM rhythm can be regular or slightly irregular. *(re-excitation of the atria when there is a one-way block). *a run of repeated premature beats. *Some degree of AV block may be present. * caused by overexertion, emotional stress, deep inspiration, and stimulants such as caffeine and tobacco, rheumatic heart disease, digitalis toxicity (digoxin toxicity), CAD, and cor pulmonale. *The P wave is often hidden in the preceding T wave. If seen, it may have an abnormal shape.The PR interval may be shortened or normal and the QRS complex is usually normal. *Manifestations include hypotension, palpitations, dyspnea, and angina. *treatment includes vagal stimulation and drug therapy. Common vagal maneuvers include Valsalva maneuver, carotid massage, and coughing. IV adenosine is the drug of choice to convert PSVT to a normal sinus rhythm.This drug has a short half-life (10 seconds). IV β-blockers and calcium channel blockers (diltiazem and verapamil (Calan) *synchronized cardioversion is also used (If other treatments are ineffective) Adenosine (Adenocard) • Injection sites should be as close to the heart as possible (e.g., antecubital area). • Give IV dose rapidly (over 1 to 2 sec) and follow with a rapid 20 mL normal saline flush. • Monitor patient's ECG continuously. Brief period of asystole is common • Observe patients for flushing, dizziness, chest pain, or palpitations. ATRIAL FLUTTER *atrial tachydysrhythmia *Atrial rate is 200 to 350 BPM *regular, sawtooth-shaped flutter waves. 4:1 flutter *associated with CAD, hypertension, mitral valve disorders, pulmonary embolism, chronic lung disease, cor pulmonale, cardiomyopathy, hyperthyroidism, and the use of drugs such as digoxin, quinidine, and epinephrine. *The atrial flutter waves represent atrial depolarization followed by repolarization. ** Patients with atrial flutter have an increased risk of stroke because of the risk of thrombus formation in the atria from the stasis of blood (Give warfarin) *treatment of atrial flutter is to slow the ventricular response by increasing AV block. Calcium Channel (CARDIZEM) Blockers and Beta Blockers. Antidysrhythmics used are: amiodarone, dronedarone, and flecainide Cardio eversion may be performed in an emergency situation Catheter ablation is the treatment of choice for atrial flutter Atrial Flutter ATRIAL FIBRILLATION *total disorganization and loss of atrial contractions *the most common dysrhythmia, increasing with age. Accounts for 17% of all strokes *350-600 BPM *P wave is replaced by a wiggly, chaotic wave. *clots form because of atria blood stasis *often seen in patients with thyrotoxicosis, alcohol intoxication, caffeine use, electrolyte disturbances, stress, or heart surgery. *patient presents with chest pain, dizziness, fatigue, lightheadedness, palpitations, shortness of breath and syncope, neuro changes *oxygen, CARDIZEM to help convert back *treatment includes Calcium Channel Blockers (diltiazem), (metoprolol), dronedarone, and digoxin (Lanoxin, electrical conversion, antidysrhythmic drugs such as amiodarone. *if caught within 48 hours we can cardiovert, without warfarin *cardioversion if needed. Will need to be on Warfarin 3-4 weeks before eversion. *anticoagulation therapy needed because of the high risk of clots. Including dabigatran (Pradaxa), apixaban (Eliquis), and rivaroxaban (Xarelto). Some patients may require a permanent pacemaker. Synchronized Cardioversion -50-150 joules -baby jolt -give versed to calm -protect the airway -must be synced with R wave FIRST DEGREE AV BLOCK *AV conduction is prolonged. PR interval is prolonged, greater than 0.20 seconds. *associated with MI, CAD, rheumatic fever, hyperthyroidism, electrolyte imbalances, vagal stimulation, and drugs such as Digoxin, beta blockers, calcium channel blockers, flecainide. *heart rate is normal and rhythm is regular. *can be a higher sign of AV block *patients are ASYMPTOMATIC *seen in athletes and the young *there is NO TREATMENT for First Degree AV Block SECOND DEGREE AV BLOCK TYPE 1 * gradual lengthening of PR interval greater than 0.20, due to prolonged AV node conduction time. QRS is blocked. *result from drugs such as digoxin or β-blockers. It may also be associated with CAD and other diseases that can slow AV conduction. *result of myocardial ischemia or inferior MI. generally well tolerated. *Atrial rate is regular, but ventricular rate may be slower because of nonconducted or blocked QRS complexes resulting in bradycardia. May appear on EKG as a pattern of grouped beats. *If the patient is symptomatic, treatment includes ATROPINE to increase HR, or a temporary pacemaker needed. SECOND DEGREE AV BLOCK TYPE 2 Wenckebach or Mobitz I *2 P waves to 1 QRS 2:1 ratio *The QRS complex is usually greater than 0.12 second because of bundle branch block. *Atrial rhythm is usually normal. ventricular rhythm is irregular. *associated with rheumatic heart disease, CAD, anterior MI, and drug toxicity. *Patients can have hypotension and myocardial ischemia. *treated with a permanent pacemaker THIRD DEGREE AV BLOCK or (COMPLETE HEART BLOCK) *no impulse from the atria is conducted to the ventricles. *ventricles beat at their own rate.*Atrial and ventricular rhythms are regular but unrelated. *associated with severe heart disease, including CAD, MI, myocarditis, cardiomyopathy, and some systemic diseases such as (scleroderma). Drugs such as digoxin, β-blockers, and calcium channel blockers. *results in ischemia and heart failure, WE GIVE OXYGEN BECAUSE NO CO *treatment includes a pacemaker. Drugs like dopamine and epinephrine are given temporarily to increase HR until pacing is started. PREMATURE VENTRICULAR CONTRACTIONS (PVC) *premature (early) occurrence of a QRS complex *A PVC is wide and distorted in shape *When every other beat is a PVC, the rhythm is called ventricular bigeminy. *When every third beat is a PVC, it is called ventricular trigeminy *Two consecutive PVCs are called a couplet. *3 or more consecutive PVCs is “ventricular tachycardia” (very dangerous) *associated with stimulants such as caffeine, alcohol, nicotine, aminophylline, epinephrine, isoproterenol, and digoxin, electrolyte imbalances, hypoxia, fever, exercise, and emotional stress. *treatment relates to the cause of the PVC’s. (O2 therapy for hypoxia, electrolyte replacement) *rhythm is irregular, P wave is rarely visible, PR interval is not measurable, QRS is wide and distorted lasting more than 0.12 seconds. *usually not harmful unless in a diseased heart. *Treated with drug therapy includes β-blockers, procainamide, or amiodarone. VENTRICULAR TACHYCARDIA *A run of three or more PVCs defines ventricular tachycardia (VT). Loss of atrial contraction. *It is a life-threatening dysrhythmia because of the possibility of development of VF, which is lethal. *VT is associated with MI (scar tissue formation), CAD, significant electrolyte imbalances, cardiomyopathy, long QT syndrome, drug toxicity, and central nervous system disorders. THIS CAUSES THE VENTRICULAR CELLS TO IRRITATE *Ventricular rate is 150 to 250 beats/minute. Rhythm may be regular or irregular. *The QRS complex is distorted in appearance and wide (greater than 0.12 second in duration). *VT can be stable (patient has a pulse) or unstable (patient is pulseless). Presents as SOB, chest pain, palpitations, light headed or dizzy, faiting, or passing out. DX WITH AN EKG *results in hypotension, pulmonary edema, decreased cerebral blood flow, and cardiac arrest. *Treated by determining the underlying cause: GIVE 02…..IVor IV (lidocaine) procainamide, sotalol, or amiodarone is used. Cardioversion is used if drug therapy is ineffective. STABLE: PATIENT HAS A PULSE: Assess patient, Give 02, Start IV. Monomorphic: IV procainamide, sotalol, or amiodarone are used. Polymorphic: IV magnesium or dilantin CARDIOVERSION IF DRUG THERAPY IS INEFFECTIVE UNSTABLE: Patient is pulseless. Start CPR immediately. PULSELESS VTACH and VFIB ARE TREATED THE SAME ...without a pulse, start CPR and initiate ACLS…...then defibrillate. VENTRICULAR FIBRILLATION YOU LOSE VENTRICULAR COORDINATING SIGNALS *Quivering,” with no effective contraction, and consequently no cardiac output occurs. * VF is a lethal dysrhythmia. *occurs in acute MI and myocardial ischemia, CAD, and in chronic diseases such as HF and cardiomyopathy. Other clinical associations are electric shock, hyperkalemia, hypoxemia, acidosis, and drug toxicity, like digoxin toxicity. *HR is not measurable. Rhythm is irregular and chaotic. The P wave is not visible, and the PR interval and the QRS interval are not measurable. *PATIENT PRESENTS AS unresponsive, pulseless, and apneic state. If it is not rapidly treated, the patient will not recover. *TREATED with CPR and advanced cardiovascular life support (ACLS) with the use of defibrillation and definitive drug therapy (epinephrine, vasopressin) ASYSTOLE *total absence of ventricular electrical activity *patients are unresponsive, pulseless, and apneic. *result of advanced heart disease, a severe cardiac conduction system disturbance, or end-stage HF. *Treatment consists of CPR including definitive drug therapy with epinephrine and/or vasopressin, and intubation ANTIDYSRHYTHMIC DRUGS Sodium Channel Blockers *decrease the amount of sodium uptake, decreases excitability of cardiac cells. *procainamide *lidocaine (need levels 1.5-5) *remember NO GRAPEFRUIT JUICE!!!!! *can be used for chronic angina Beta Blockers (LOL’s) *decrease the contractility, decrease the heart rate, decrease SVR, and BP. *decreases the workload of the heart, conserves the oxygen demand, and decreases the SNS response *metoprolol, carvedilol, antolol, propranolol. *always give with food *be careful with COPD, ASTHMA, and DIABETICS. *Monitor BP and HR (hold below 60 BPM)(hold for BP below 90/60) *Monitor blood sugar for hypoglycemia *daily weights *be careful when getting up *PATIENT IN CARDIOGENIC SHOCK CANNOT TAKE BETA BLOCKERS! *can be used to lower blood pressure, slows heart rate. Potassium Channel Blockers *interferes with the potassium uptake *delayed repolarization, lengthens the recovery time, stabilizes the dysrhythmias. *edema and crackles *amiodarone, quinidine, dronedarone. Calcium Channel Blockers *block the calcium uptake *vasodilation, decreased SVR, increased blood flow. *USE CAUTIOUSLY WITH DIGOXIN, INCREASES EFFECTS *procardia, cardizem, calan *used for A-Fib, A-Flutter, and SVT *NO GRAPEFRUIT Other Antidysrhythmics *adenosine (Adenocard) -slows electrical conduction, slows HR, puts it into normal rhythm. -3 second half life -1 nurse gives med and 1 nurse flushes. -6mg over 1-2 seconds. If that does not convert, give another dose within 1-2 minutes of 12mg IV bolus X 2, use a stop-cock if you’re alone. *digoxin (Lanoxin) -dig makes the heart work smarter, not harder. -watch potassium, watch dehydration, magnesium, and renal insufficiency. -caution with Beta Blockers *magnesium -relaxes smooth muscles. *dronedarone (Multaq)n,m -helps a-fib and a-flutter -NO GRAPEFRUIT JUICE TO HELP SPEED UP -atropine -epinephrine -dopamine -pacemaker TO HELP SLOW DOWN -beta blockers -calcium channel blockers -adenosine (antidysrhythmic) -synchronized cardioversion TO HELP RHYTHM (antidysrhythmic) -adenosine -amiodarone (helps maintain rhythm) -dronedarone (Multaq) (diltiazem) CARDIZEM IS THE GO TO FOR A-FLUTTER!!!! DIGOXIN FOR A-FLUTTER AS WELL Amiodarone for maintenance Cardioeversion