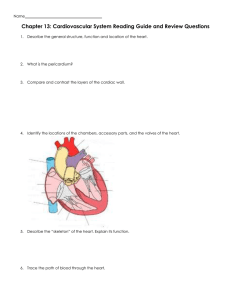
MU School of Health Professions Department of Physical Therapy PT 7890 Case Management I Objectives: Cardiovascular Rehabilitation 1. A&P: Describe blood circulation through the heart pump, including the name, and timing of valves in the cardiac cycle*. Relate the closing of valves to the 1st and 2nd heart sounds. Define End Systolic Volume (ESV), End Diastolic Volume (EDV), Stoke Volume (SV), Ejection Fraction (EF), Cardiac Output (CO). Relate EF, SV, EDV and CO values to the presentation of a failing heart pump. Draw the layers of the heart muscle from superficial to deep. Review coronary artery names, location, and the structures they supply, appreciating anatomic variants, particularly of the RCA and the circumflex artery (see drawing in O’Sullivan p.591, also Coffman syllabus p.23). Draw and label a picture that would be used to explain location of a blocked coronary artery to a patient. Explain the electrical conduction systems in both lay and technical terms and correlate electrical events to the ECG waveform (the cycle of depolarization and re-polarization to different zones of the heart). Define preload, afterload, contractility, and appreciate their interplay in describing heart pump function, both normal and in pump dysfunction / failure (Guide Practice Pattern 6D). Also associate different categories of drugs with their modulation of these 3 elements of pump mechanics. Hillegass C.2. 2. Describe congenital heart defects. Describe heart disease that may be acquired in infancy and childhood, realizing that acquired cardiac diseases or impairments may be compatible with life, and that cardiopulmonary impairments may go unrecognized until adulthood (when they could manifest as CHF, Pulm HTN, Angina, Syncope, Arrhythmias). 3. List and explain the significance of risk factors for heart disease (modifiable and unmodifiable). Explain how risk factor analysis would affect your treatment of a patient who does not have a history of heart disease. Explain how risk factor analysis would affect your treatment of a patient who has a history of heart disease, but is referred to PT for some other problem. Hillegass p.717-718, 693, also ACSM 4. Review the etiology, pathophysiology, and clinical symptoms of coronary artery disease (CAD). Hillegass C.3 5. Review steps in a clinical examination and differential diagnosis for shoulder pain; differentiate musculoskeletal signs and symptoms from visceral (myocardial) signs and symptoms. Discuss the possible relationship between visceral pain and shoulder/arm/hand pathology. Goodman: Physician referral: p.318-320; Overview: Cardiac Chest Pain Patterns: p.321-325; Key Points to Remember: p.325; Subjective Examination: p.326-327. Also p.805-813 6. Outline departmental emergency preparation, including drills, crash cart, and individual responsibilities, for inpatient vs. outpatient settings. Include protocol for caring for patient, significant others. (Sharon Coffman syllabus p.17: “Distress and emergency measures: Code Lab) 7. Explain implications of calling 911: first responders, ambulance; ethical or legal questions regarding patient/family wishes; reimbursement for services. 8. Perform CPR and use AED appropriately. 9. Define and describe 4 types of angina pectoris or coronary insufficiency, and the appropriate clinical response to each situation. Describe how the experience of angina may differ for women. Hillegass p.97-98, p.642-643. Goodman p.780-781 Calculate the Rate Pressure Product (RPP) as an indicator of myocardial oxygen demand (MVO2). RPP is most useful for the patient with stable angina, i.e. titrate exercise intensity so that the RPP is below the anginal threshold. Remember, RPP is not normed, and is only applicable to that individual. RPP = SBP x HR (drop the last 2 digits of the 5 digit number) 10. Describe the continuum of myocardial involvement: ischemia, injury, and infarction, and the resulting zonal impairment of wall motion, electrical conduction, and rhythm. Draw and label a picture that would be used to explain this to a patient. O’Sullivan p.605, also, Hillegass p.413 shows a subendocardial event, which occurs from the inside out. The subendocardium is the most distal to the coronary artery circulation, and perforating veins pass through the myocardium to reach it. 11. Explain the pathologic changes that occur in an MI. and the functional variations that occur when different arteries are blocked. Hint: see Sharon Coffman’s syllabus p.23 (at the bottom of the page) “Related Signs and Symptoms”, to help you categorize your responses. Look at the anatomic areas supplied by the different arteries. Recalling the different layers of the heart muscle (obj. #1), differentiate subendocardial (Hillegass p.413 Fig 9-51C) and transmural infarction (O’Sullivan p.605 Fig. 16-10), and how they may affect an exercise program. Recognize how activity and exercise that is too aggressive may contribute to pathologic changes. 12. Review an ECG strip and calculate HR. Describe or recognize basic changes that can occur during ischemia, injury, and infarct. Recognize a premature ventricular contraction (PVC), and use the number occurring per minute and grouping characteristics as a guide to safe exercise. See O’Sullivan p.602-605, Fig 16.10. Five big boxes = 1 sec. Count 6 seconds, then count the number of QRS spikes within 6 seconds and multiply by 10. Hint: try to pick a QRS spike that falls close to a line as your starting point. Only count the normal QRS spikes to arrive at the bpm. 13. Pharmacology: Define pharmacokinetics, pharmacodynamics. Describe the major categories of pharmaceuticals used to manage cardiovascular disease, give one example of each, state the anticipated beneficial effect, and possible side effects affecting an exercise program. Define and give an example of a positive inotrope and a negative chronotrope. Antihypertensives Hyperlipidemia Anti Clotting Nitrates (cause vasodilation of peripheral smooth muscle to reduce Preload) Antiarrhythmics Heart Failure: 14. Briefly describe information obtained from the following diagnostic procedures: (see Hillegass C.8 reading assignment) Cardiac catheterization or coronary angiogram Cardiac Enzymes: CPK, LDH, Troponin Echocardiogram Exercise Tolerance Test (ETT); Stress Test; Graded Exercise Test (GXT) o active OR pharmacologically induced using adenosine, dobutamine, or dipyridamole (persantine) (incidentally, persantine is also prescribed for Platelet Aggregation Inhibition) o with or without Perfusion Testing (radionuclide study) using Thallium or Technetium (Sestamibi) Ambulatory ECG (telemetry); 24 hour Holter monitor; Telephonometry 15. Explain etiology, and possible S&S of a dissecting aortic aneurysm. 16. Apply specific information about how ejection fraction, cardiac output, and segmental heart wall motion may be important when developing a patient’s exercise program. Apply these measures to the NYHA CHF functional categories 17. Describe indications for, and the procedure for accomplishing percutaneous transluminal coronary angioplasty (PTCA). Draw or describe a stent and explain its use. (Coffman syllabus p.23) 18. Overview Phase I through Phase IV cardiac rehabilitation programs. Provide examples of low energy activities (in METS) that are appropriate during Phase I. Determine the MET level of stair climbing. List diagnoses commonly referred for Phase II Cardiac Rehab. Appreciate the impact of managed care on the eligibility and reimbursement of Phase 2 Cardiac Rehabilitation. O’Sullivan p.616-622; Sharon Coffman syllabus p.12, Hillegass p.682 19. Describe changes to the cardiovascular system that occur with aging. Discuss how typical changes may affect exercise response. (Bottomley p.32-34, Hillegass p.716-717) 20. Explain how changes associated with menopause relate to cardiovascular function. Discuss implications of findings by the WOMENS HEALTH INITIATIVE regarding hormone replacement therapy. Survey current findings in the field of sex-based biology as related to cardiovascular disease (course website). 21. Recognize effects of emotional stress on the heart. Recommend relaxation exercises appropriately. (Kisner & Colby p.196-7: Relaxation Training) 22. Recognize why a coronary artery bypass graft (CABG) operation is performed. Describe the surgery, sources of graft material, post-op precautions for exercise. Outline physical therapist involvement with a CABG patient in a routine case vs. one with complications, (including airway clearance and maintenance of lung volumes). Compare acute rehab goals for the post CABG patient vs. the post MI patient. Sharon Coffman syllabus p.12, O’Sullivan p.633 23. Identify S/S that preclude the initiation or continuation of an exercise session for a patient with CAD, arrhythmia, CHF, or heart transplant. 24. Review the etiology, pathophysiology, and clinical symptoms of Cardiac Pump Dysfunction and Pump Failure, Pattern 4D (Congestive Heart Failure, Cardiomyopathy, Cardiac Muscle Dysfunction). Distinguish Left and Right Heart Failure in terms of etiology and S&S. Given a patient description, determine a New York Heart Association (NYHA) functional classification. Describe characteristics of an exercise program for this population. Hillegass C.3 reading assignment, also Sharon Coffman’s syllabus: p.13-14. 25. Considering that the 200-age formula overestimates target heart rate (THR) for the young, and underestimates for the elderly, use the following alternative methods: o Tanaka et al: HR max = 208 – (0.7 x age) o Karvonen / Heart Rate Reserve: [HR max – Resting HR] x % + Resting HR o Borg 12-13 – “Somewhat Hard” = 60% HR Max o Borg 16 – “Hard – Very Hard” = 85% HR Max Given patient information, use the Tanaka or Karvonen to calculate THR for a desired exercise intensity 26. Explain the effects of sexual activity on the heart in terms of MET level and in lay terms by comparing sexual intercourse to the physical effort involved in other routine activity. 27. Describe the procedure for heart transplant (orthotopic, the most common). Describe differences in exercise response and ECG tracings in the case of a transplant. Describe differences in exercise prescription for heart transplant patient. Hillegass C.12 28. Identify typical psychological issues related to heart disease, and possible ethnic / cultural variations. State epidemiology rates for heart disease by ethnic groups. Find resources for patient and significant other’s questions: prognosis, control of one’s life; return to work; sexuality; fear of sudden death. Develop a position on PT responsibility to help patient deal with these issues. (AHA website for starters) 29. Identify conditions for which pacemakers are commonly prescribed. Given a pacemaker code, explain its function. NASPE / BPEG pacemaker coding system described in ACSM 7th ed. p.194-197, 30. Describe the likely etiology, mechanical affects and pathological results of mitral and aortic valve dysfunction, from stenotic valves and from insufficient/regurgitant valves. Describe medical management. Bottomley p.71, Hillegass p.114 31. Pulse Oximeter (Sp02): list possible sources of error in the results. Under what circumstance might the PulseOx show a normal reading, but the person is dyspnic, cyanotic, or poorly perfused?