Fetal Milestones
Milestones
4 wks.: fetal heart begins to beat
8 wks.: all body organs formed
8-12 wks.: FHT can be heard by Doppler device
16 wks.: Baby's sex can be seen
18-20 wks.: Heartbeat can be heard w/ fetoscope. Mother feels movement (*quickening)
24 wks.: Respirations begin. Viability!
28 wks.: Baby can breathe at this time. Surfactant needed
36 wks.: Lungs mature. Has surfactant!
Fetal Development
Preembryonic
stage
1st 2 weeks
Embryonic
Stage
3-8 weeks
Fetal Stage
End of 8
weeks
(stage of the ovum)
Malformations that occur during this stage seldom result in a viable fetus
Every organ system and external structure is present, and the remainder of
gestation is devoted to refining the f(x) of the organ
Twins
Dyzygotic: double ovulation (2 eggs)
Monozygotic: 1 egg divides after fertilization into 2 sep. zygotes
- Develop from single ovum
-Same sex and genotype
2 placentas (sometimes fused)
2 chorions
2 amnions
Twins increase w/ parity (more
kids you have the higher the
chance)
a. How does the fetus grow?
Fertilization
They are also at greater risk for the other complications; congenital
abnormalities including conjoining and twin to twin transfusion
syndrome (TTTS: unequal sharing of nutrients, blood moves from
on twin to the other leaving one w/ too little and the other w/ too
much blood)
Where does the egg implant?
How long is the egg viable? Sperm?
When do females get eggs? Males get sperm?
Who determines the sex of the child?
How long does it take for the sperm to travel to implant?
Fertilization occurs in the ampulla (outer third) section of the fallopian tube
Egg is passed through tube by cilia and takes three days for zygote to move through F. tube towards uterus
Risk factors: smoking, DM, HTN, STIs, lung damage, PID makes cilia not work well, and Fallopian scarring
Implantation occurs in the endometrium (the upper 1/3 of the uterus)
Ectopic preg. Can happen when the egg doesn't move to the uterus (implants in the tube) it puts the mom at risk for a hysterectomy if baby continues to form
DNC abortion
Ova are viable for 24 hrs and sperm are viable for 24-72 hrs
Females are born with all their eggs they’ll ever have (made in utero)
Males produce sperm the entirety of their life
The Y chromosome determines gender and is passed by the father
XX -> girl
XY -> boy
Reproductive Cycle
a. When does it start?
Day 1 – start of period
b. When does ovulation start?
Occurs 14 days before next menstrual period
c. When is a woman most fertile?
d. What are the 3 signs of ovulation?
Signs
-Increase in Basil body temperature
-Spinnbarkeit: mucus becomes thin and stretchy
-Cervix opens slightly to allow sperm to pass
-Decrease estrogen
-Increase in FSH
-Mittelschmerz: unilateral pain from ovary releasing
-
Phases of the menstrual cycle
28-day cycle
Begins w/ menstrual phase: day 1-5
Shedding of endometrium -> bleeding
-
Proliferative phase: day 6-ovulation (~day 14)
LH converts follicle to corpus luteum--> produces progesterone (pro-pregnancy)
Corpus luteum continues to make progesterone until placenta takes over
function
-
Secretory (luteal) phase: Ovulation - ~3 days before menstrual cycle
Estrogen lvls fall
Progesterone lvl increase to support possible preg.
-
Ischemic Phase: ~3 days before menstruation to onset of mense
If fertilizations don’t occur progesterone and estrogen levels drop and corpus luteum degenerates
Hormones
3 protein hormones
HCG (human chorionic gonadotropin) pregnancy test hormone
HCS (human chorionic somatomammotropin) aka HPL (human placenta lactogen) Insulin agonist
Promotes growth for maternal tissue; increases protein and glucose available for the fetus
Relaxin: Promote relaxation of pelvic ligaments and connective tissue, softens cartilage in pelvic joints and symphysis pubis
Pregnancy waddle: curvature of spine
- Relaxes all smooth muscle (uterus, bladder, ureters, and GI tract)
Causes constipation and promotes vasodilation
2 steroid hormones
Estrogen
Progesterone
Hormone
Estrogen
Function
has proliferative function of uterus, breast, and breast tissue
Increases vascularity --> increased nutrients --> increases
size of uterus
-End of preg.: 30 times the daily production in middle
of normal monthly menstrual cycle
Encourages the storage of nutrients and glucose (food
reserve for coming fetus (love handles))
Pharmacological Use
Estrogen is used in birth control pills
Progesterone
Creates a safe environment for sperm and ovum (keeps you
pregnant)
Decreases contractility of the uterus --> keeps baby safely
in uterus
Helps prepare breasts for lactation
Secreted by the corpus luteum, and peaks 8 days after
ovulation (same time implantation occurs)
After the 10th wk. the placenta takes over
production
Can be used to prevent early-stage fetal death
HcG
HcG causes the corpus luteum to secrete estrogen and
progesterone until week 11; after that the placenta takes
over
Pregnancy test hormone
Increased hCG might have multiple babies
Prostaglandins
Present in blood serum 8-10 days after fertilization and
keeps increasing during preg.
HCG double ever 48-72 hrs., peak at 60-80 days, and
then decrease b/w 100 and 130 days post
conception
Present in urine and signals pregnancy
Most responsible for nausea and vomiting
opposite of progesterone also works on GI system (cramps
and loose stools)
Make the smooth muscle/uterus contract
If HCG levels start to fall early on -> nothing stimulates
estrogen and progesterone -> miscarriage or
spontaneous abortion (SAB)
Induces labor
Given to women for clinical abortions
The bowel contracts a lot because all smooth muscle
contracts --> causes diarrhea
Placenta Anatomy
Anatomy of Placenta
Chorionic: fetal side
Outer membrane enclosing the amniotic cavity
Forms fetal part of the placenta
Site of testing
Composed of 2 portions
-Maternal portion: decidua basalis (dirty Duncan)
-Fetal portion: chorionic villi- fetal surface covered by adherent amnion (Shiny Schultz)
Function of placenta:
Exchange nutrient and waste products
Produce human placenta lactogen, estrogen, and progesterone
-Fetal respiration
3rd trimester transfers immunoglobulin providing the fetus w/ passive immunity
-Large particles (bacteria) cannot pass, but smaller ones can (viruses)
Fetal Circulation
-Umbilical cord
2 arteries and 1 vein
Arteries carry deoxygenated blood and waste products
Veins carry oxygenated blood and nutrients
Fetal Heart Rate
160-170 bpm (1st trimester)
Slower as the fetal growth 110-160 bpm
Twice maternal heart rate
Lungs do not function - placenta assumes this function
Umbilical vein -> ductus venosus (bypass liver) -> Rt. atrium -> foramen ovale (bypass
ventricle) -> Lt. Atrium -> Lt. ventricle -> Aorta -> ductus arteriosus (bypass lungs b/w
pulmonary arteries and aorta) -> descending aorta -> umbilical artery -> branches to
of the body
Rt.
lower rest
After birth:
Placenta removed and lungs take in air (air pushes fluids out into arterioles)
Pressures on the Rt. side of heart lowers and Lt. side pressure increases forcing the foramen ovale closed.
1st few hours of life smooth muscles in the ductus arteriosus constrict signaled by decrease of prostaglandin levels from disconnection from placenta and
increase in pO2
Placenta
Amniotic Sac (Amniotic Fluid)
Inner membrane; fluid filled sac
Amniotic fluid f(x)
-Cushions to protect against mechanical injury
-Helps control embryo body temp
-Prevents adherence of amnion (fingers don't web together & doesn't get stuck to the uterus walls; w/o enough fluid fingers band together)
-Allows freedom of movement for baby
-Permits symmetric growth of embryo
-Contain fetal urine and measures kidney functions
Early AF is made by amnion
Later (8-10 wks.) AF is made by fetal urine --> kidney f(X) indicator
Low AF: Potters syndrome-> unable to fix; decreased O^2 to kidneys
High AF: swallowing issues and other defects
Complications
Early problems: poor muscle development and webbing (neck, finger, toes)
Late problems: movement trouble and chord compression
Genetics
Autosomal Recessive Genes: expressed only if the homozygous (inherited gene). When paired w/ a dominant ("normal") gene it will not be expressed, except in
genotype (gene) but not phenotype (appearance)
PKU
Tay-Sachs (Mediterranean Jews)
Cystic Fibrosis
X-linked recessive gene: females do not exhibit disease if she has an X-chromosome without the trait (women carry XX) but will carry the gene
Male will exhibit trait because they carry XY (they only have one X)
Hemophilia
Color blindness
Muscular dystrophy
Haploid: 23 chromosomes
Diploid: 46 chromosomes
Trisomy 21: extra chromosome: 47 rather than 46 (Down Syndrome)
Amniocentesis is confirmation (performed 15-21 wks.)
Age is strongly related to the incidence of down syndrome
Phenotype: physical traits
Genotype: pattern of genes
Autosomal dominant
Huntington’s Disease
Teaching
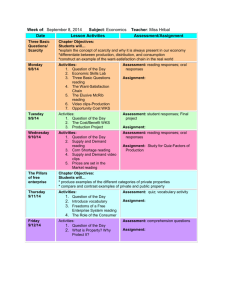
1st Trimester: wk. 0-12
2nd Trimester: wk. 13-24
3rd Trimester: wk. 25-40
Physical and psychological changes
Self-care
Choosing a provider
Prenatal experience
Relief of common early pregnancy
discomforts
Planning for breastfeeding
Dietary lessons
Sexuality in pregnancy
Encourage communication w/ partner
regarding adjustments
Relief of pregnancy discomforts
Prep for childbirth
Development of birth plan
Relaxation techniques
Postpartum self-care
Infant stimulation
Infant care and safety
Safety related to balance
Teach risks and symptoms of preterm labor
Risk Factors for PTL
YMA (young maternal age: < 18)
Smoking
Overweight/underweight
Not getting good prenatal care
Drinking alcohol or using drugs
STIs and UTIs
Pregnant w/ a baby w/ birth defects
Pregnant w/ a baby in vitro fertilization
Pregnant w/ twins
Family/personal h(x) of preterm labor
Getting pregnant too soon after having a baby
Health conditions: HTN, preeclampsia, infections
Symptoms of PTL (know difference b/w true and false labor)
o Backache; usually lower back pain. This will be constant or intermittent, but won't ease even if you change positions or do something else for
comfort
o Contractions every 10 minutes or more often
o AF leaking from vagina
o Flu-like symptoms; nausea, vomiting, or diarrhea
Call Dr. even for mild cases.
If you can't tolerate liquids for more than 8 hrs. you must see Dr. (dehydration)
o
o
o
Increased pressure in your pelvis or vagina
Increased vaginal discharge
Vaginal bleeding; including light bleeding
Nutrition
a. Sources of Iron
b. Sources of folic acid
c. What benefit does folic acid have?
d. Sources of calcium
e. Sources of protein
f. Foods to help with morning sickness/hyperemesis gravidarum
g. Uterine stimulants
h. Foods to avoid
i.
Foods high in mercury
Prenatal Labs
When is it done?
CBC
H&H
Normal values in
preg.:
Hct: 30-47%
Hgb: 12-16
Blood Type & Rh RhoGAM: given at 28
wks and w/in 72 hr
after delivery, invasive
procedures, or trauma
because of maternal
exposure to fetal Rh
antigen
Antibody
(indirect
Coombs)
UA
Every prenatal visit
Glucose
Screen/GTT
24-28 wks
Earlier if pt. at risk
RPR/VDRL
36 wks
What does this test measure?
Gain knowledge of platelets
An epidural anesthetic will be withheld if the platelet count is <100,000 mm^3
Hct: important to monitor for eclampsia (HTN)
Hgb: decreased Hgb is important to monitor because the EBL during a…
C-section delivery is 1000 mL
Vaginal delivery is < 500 mL
25% increase in erythrocytes and 50% increase in plasma volume
Eclampsia: High BP and protein in the urine and usually previously diagnosed w/
preeclampsia to develop seizures or coma
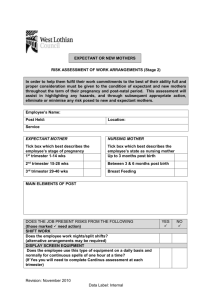
Rh Sensitization & Rh Factor
Occurs when you have a Rh - mom and Rh+ fetus
1st offspring is not affected by the antibodies
2nd pregnancy: hemolysis occurs because the mother's antibodies enter baby through placenta
and causes erythroblastosis fetalis: increase of immature RBC's in fetal circulation that will result
in; hyperbilirubinemia, anemia, hypoxia, CHF, neuro damage, hydrops fetalis (extreme swelling)
Continued RBC destruction results in jaundice and leads to Kernicterus (sever jaundice and
neuro damage)
Indirect Coombs' Test: determines if Rh- mom has developed anti-bodies
Direct Coombs' Test: performed on infant's blood after birth to identify maternal antibodies to RBCs
Spilling glucose is OK because glucose reabsorption impaired in pregnancy
Protein: Trace to +1 is ok. Increased protein may indicate preeclampsia
WBC: UTI -- if UTI goes untreated --> kidney infection --> lead to early labor and low birth wgt
Ketones: indicate diabetes
Preeclampsia - HTN
Glucose Tolerance Test
Screens for GDM (gestational DM)
Administer 50 g oral glucose, assess after 1 hr.
BS > 140 mg/dl is abnormal. Further testing needed (OGTT)
Insulin during 1st trimester: therapy remains the same
2nd and 3rd Trimester: Insulin needs may need to be increased
Test screens for Syphilis
Syphilis: A fetus can end up aborted or more commonly an intrauterine death (IUD) can occur.
Early neonatal death can also occur, and the survivors may develop features of congenital syphilis
such as bone abnormalities, hepatitis, anemia, and active neuro-syphilis
HIV test/ screening requires informed consent
HIV/HPV
Herpes
If lesions are present C-section will be performed
If there is no outbreak, vaginal birth is OK
Toxoplasmosis: transmitted by uncooked meats or handling cat litter.
HSV
TORCH
infections
Other infection
Rubella
CMV (cytomegalovirus) Teach mom to stay away from ppl. w/ CMV. Transmitted through urine,
semen, cervical vagina secretions, feces, breast milk. There are no licensed treatments for pregnant
women who become infected w/ CMV during preg.
Hep B
HbSAg
W/in 24 hrs. of birth
Rubella titer
Tests for Hep. B
Infants born w/ HBsAG-positive mothers should be treated w/in 12 hrs. of birth
Hep B. vaccine is not contraindicated in pregnancy
IgG antibodies are measured. A titer of 1:10 or greater indicates immunity
Don’t give while mom is pregnant because it is a live vaccine
Also do not get pregnant for 1-3 months after you receive the vaccine
Pts. Who do not have immunity to Rubella should receive a rubella vaccine during postpartum
period to protect future pregnancies while not affecting current pregnancy
AFP
Screening
15-18 wks typically
↑ lvls: NTD
↓ lvls: Trisomy 18/21
It is administered postpartum before discharge, SQ, if titer < 1:8
Sample of mother’s blood
Alpha Fetal Protein, elevated level may indicate neural tube or body wall defects or multiple
gestation
Decreased levels indicate risk of trisomy 18 (Edward’s) or 21 (Down Syn.)
Triple/Quad
screen (MSAFP)
Screening
Optional screen for
pt. at 14-18 wks
Triple: includes AFP, estriol, and beta-hCG
Quad: includes AFP, estriol, Beta-hCG, and inhibin A
Identifies risk for Down syndrome, NTD, and other chromosomal disorders
Elevated hCG w/ low estriol & MSAFP levels indicates risk for trisomy
Cell free DNA
~10 wks
CVS
Diagnostic
10-12 wks
Results available < 1
wk
Amniocentesis
Diagnostic
15-20 wks
30-39 wks: lung mat.
Tests maternal serum for fetal DNA
Determine fetal sex in pregnancies at risk for sex-linked conditions.
98% detection rate for trisomy 13, 18, and 21 (Patau, Edward’s, Down syn.)
If abnormal results, invasive diagnostic tests will be needed such as chorionic villus sampling or
amniocentesis
Chorionic villus sampling: removal of portion of chorionic reflects fetal genetic make-up
Detects fetal karyotype, sickle cell, trisomy 21, muscular dystrophy, and cystic fibrosis
Cannot detect neural tube defects (NTD)
Earlier diagnosis than amniocentesis
AF aspirated
Perform chromosome analysis, AFP markers, karyotyping, and identify sickle cell or cystic fibrosis.
Lung maturity: Lecithin to sphingomyelin ratio (L:S) and phosphatidylglycerol (PE)
L/S ratio 2:1 or greater indicates lung maturity and PE is present in surfactant
Pap smear
Gonorrhea/
Chlamydia
GBS
Gonorrhea / Chlamydia
Can lead to miscarriage or infect baby before or during delivery
35-37 wks
TX: penicillin
Discomforts of Pregnancy
Discomfort
N/V
Group B Strep: caused by normal vaginal flora
- Can be transmitted from birth canal of mother
- Culture anorectal and vaginal area (not cervix)
- If mom positive, IV antibiotic are given to reduce risk of transmission to baby - recommended
once labor begins and Q4hr during active labor until baby is delivered
For mom - can cause bladder and uterine infections
For baby - meningitis, sepsis, pneumonia, stillborn
Factors – Causes, Trimester
Self-Care
↑ hCG, fatigue, and ↑ relaxation of stomach smooth muscles Small, frequent meals, avoiding
Relieve stress by letting them know it won't last forever! It will
odors/triggers, ginger, peppermint,
subside by week 13
carbonated beverages
Urinary Frequency
Pressure on bladder
urinate more frequently, decrease
evening fluid intake, and if you must pee
GO! Increase daytime fluid intake
Leukorrhea (↑ vag. discharge)
↑ mucus production
Cotton underwear, no douching
GERD/Heartburn
Displacement of stomach by enlarging uterus, ↑ progesterone, ↓ Avoid big meals, fatty/fried foods,
gastric motility
timing of last meal
Edema
↓ venous return
Avoid standing for long periods,
elevate legs
Constipation
Bowel sluggishness
Caused by progesterone
↑ fluids, fiber, exercise, stool
softeners
Back Pain
Relaxin, ↑ curvature
Pelvic tilt exercises, body mechanics
Leg Cramps
Electrolyte imbalances
Dorsiflex foot, apply heat to muscle
Dizziness/Syncope
Blood volume changes -> vasodilation, postural hypotension
Change position slowly, avoid
prolonged standing in one position
Braxton Hicks v. Round
ligament pain
BH: no pattern
PTL: progressive pattern
Rest/bath -> if they go away they’re
BH
Signs of Pregnancy – 3 P’s
Presumptive
-Nausea & vomiting; breast tenderness,
-late period, fatigue
Probable
Positive
-Hegar’s, Chadwick’s, Goodells
-Abdominal changes
-Abnormal pap smear
-+ pregnancy test
-Fetal heart rate (FHR) – heard by examiner
-Ultrasound – visualize the baby
-Fetal movement palpated by examiner
Presumptive (subjective): S/S of what woman say. May or not be associated w/ pregnancy
Probable (Objective – but could have another explanation so not 100%): noted by examiner, may or may not be associated w/ pregnancy
Ballottement: technique of using finger to tap against the uterus, through the vagina, to cause the fetus to bounce w/in AF and feeling it rebound
quickly
Braxton Hicks contractions: practice contractions; irregular and usually painless contraction that comes and go throughout pregnancy
Positive signs (diagnostic): noted by examiner and can ONLY be cause by pregnancy
Uterine Changes
THINK HCG
Hegar's sign: softening of uterus
Chadwick's sign: bluish color of cervix
Goodell's sign: softening of the cervix (soft cervix = good sign)
Physiological Changes of Pregnancy
Uterus
Increases in size (hypertrophy) and shape (ovoid shape)
Moves up in abdomen
More vascular
Mucous plug (serves as a barrier to foreign antigens)
Respiratory -> Breathing for 2!
Increased tidal volume
Nasal congestion/stiffness/nosebleed due to vascular congestion of nasal mucosa, capillaries are more fragile in the face, causing nosebleeds
High levels of estrogen and progesterone increase blood flow to all your body's mucous membranes
Respiratory rate increases to 21
Nasal interventions: use cool air vaporizer and normal saline spray
Cardiovascular
Pulse increases 10-15 bpm
CO^2 increased by 50%
BP shouldn't rise but is a possibility
If mom is laying on her back her blood vessels (vena cava and aorta) will be compressed and result w/ not enough blood circulation = Hypotension
Teach mom that a left side-lying position relieves supine Hypotension and increases perfusion to uterus, placenta, and fetus
Trauma w/ suspected spinal cord injury -> decrease BP-> tilt the whole backboard
CPR: displace the uterus 1st!!!
Hematologic
Blood volume increases by 40-50%
Physiologic Anemia of Pregnancy
Due to plasma increase, H&H go down.
Hct drop is 5-7 % (normal value 38-47 %)
Pregnant women Hct: 30-46 %
Skin
Increase in estrogen causes:
Pregnancy mask (chloasma)
Linea nigra (line down center of stomach)
Stretch marks (stridea)
Use sunscreen for chloasma
Stridea will fade from red to silver
Linea nigra will disappear eventually after the birth of the baby
Breasts
Estrogen and progesterone cause breasts to enlarge, colostrum (secreted during last trimester)
Colostrum has antibodies, minerals, and proteins and low levels of sugars and fat.
Very important for baby's first couple of feedings!
GI
N/V, heartburn, decreased tone and motility of smooth muscles, constipation
Musculoskeletal
Pelvic joints relax causing a waddling gait
Relaxin is the hormone responsible for joint relaxing
Lordosis (inward curvature) of the spine
Renal urinary frequency
3rd trimester: baby's head is bigger and compressed on mom's bladder
Increased risk for UTI, but may not show s/s (many symptoms of pregnancy can overshadow UTI symptoms so it can go unnoticed)
UTIs can cause PTL (preterm labor)
Undiagnosed UTIs can travel to kidneys and cause pyelonephritis
Hormonal (Endocrine)
3-5 lbs wgt gain in 1st trimester
10 -12 lbs wgt gain in 2nd and 3rd trimester (one lb. per week)
HcG: support pregnancy, high fluctuation causes n/v
HpL: Insulin agonist. Inhibits insulin so mom can release more glucose for fetal growth
Estrogen: uterine development for fetal growth, stimulates breasts for lactation
Progesterone: maintain endometrium, decreases uterine contractility, causes relaxation of smooth muscles. Promotes retention of fetus
Prostaglandins: contribute to onset of labor (GI smooth muscles -> diarrhea)
Psychological Responses to pregnancy
1st trimester (0-12 wks)
Ambivalence (mixed emotions/maternal response): whether pregnancy is planned or unplanned,
ambivalence is normal
Ambivalence: financial worries about increased responsibility and career concerns
2nd trimester (13-25 wks) {GOLDEN TIME}
Quickening occurs and pregnancy becomes real
Pregnant women accepts pregnancy
Ambivalence wanes
3rd trimester (26-40 wks) {GET THIS THING OUTTA ME OR LEAVE ME ALONE}
Mom becomes introverted and self-absorbed
Mom begins to ignore partner (may strain relationship)
Nagele’s Rule – how to calculate
EDC: estimated date of confinement
Nagele's Rule: 1st day of LMP minus 3 months plus 7 days
Assumptions: 28-day cycle, Accurate LMP, & no oral contraceptives/breastfeeding
McDonald's Method (not as reliable as Nagele's rule; used when mom doesn't remember LMP)
Measure fundal height: Measure from symphysis pubis to top of fundus in cm
GTPAL – know each one and how to interpret
Gravida: # of any pregnancy including present
Primigravida: 1st pregnancy
Multigravida: more than 1 pregnancy
Para: births after 20 wks gestation regardless of whether the infant is born alive or dead
Nullipara: a woman who has not given birth to a viable fetus
Primipara: woman who has had one birth past the point of viability, regardless of dead or alive
Multipara: woman who has had 2 or more births to a viable fetus
GTPAL (OB history)
Gravidity: # of pregnancy including present
Term: # of term infants born after 37 completed wks
Preterm/Para: # of premature infants born b/w 20 and 37 wks
Abortions: # of pregnancies that end in spontaneous or therapeutic abortion prior to 20 weeks
Living: # of living children
Prenatal Visits
Every 4 wks for the 1st 28 wks
Every 2 wks until 36 wks
After 36 wks - every wk until birth
o Unless there is a reason for more frequent visits (Hx of DM, HTN, PTL)
Use of Ultrasound by Trimester
1st: 0-12wks: heartbeat, dating; primary dating
2nd: 13-24wks: heartbeat; structures; 16-18wks can see basic structures, sex of baby (at 12wks can see external genitalia); placenta, AF; sex and
confirm LMP
3rd: 25-40: heartbeat; fetal echo at 28wks – chamber, AF; placenta – previa, low lying; cord and flow; more structures; placental
functioning/health of baby
VEAL CHOP
Draw an example
Variable deceleration
Early deceleration
Late deceleration
Acceleration
Reassuring/ nonreassuring/benign?
Physiology
Cord compression
Description
Pregnancy Parameters
Pregnancy duration:
Early term: 37 0/7 wks through 38 6/7 wks
Full term: 39 0/7 wks through 40 6/7 wks (39-40 wks and 6 days)
Late term: 41 0/7 wks through 41 6/7 wks
Post-term: after 42 wks
Preterm (PTL): 20-37 wks
Abortion: birth that occurs prior to the end of 20 wks gestation; miscarriage
Miscarriage: abortion that occurs naturally; spontaneous abortion (SAB)
Stillbirth: a fetus born dead after 20 completed wks of gestation
Analgesia
Local:
Epidural:
Spinal:
Puodenal:
General Anesthesia:
Fetal Adaptations
Adaptation
How does it work before birth?
What happens after birth?
Intrapartum Complications
Complication
Placenta Previa
Placental Abruption
Uterine Rupture
Prolapsed Cord
Shoulder Dystocia
Physiology
Causes
Risk Factors
S/S
Tx/Interventions
Placenta Acreta
Placenta Increta
Placenta Percreta
Oligohydramnios
Polyhydramnios
Amniotic Fluid
Embolus
Vasa Previa
Succenturiate Lobe
Preterm Labor
Preeclampsia
Stages and Phases of Labor – look @ Exam 2 Prep Assignment
Stage
Stage 1
Early/Latent Phase
Definition
Characteristics
Active
Transition
Stage 2
Stage 3
Stage 4
Method
Continuous
Abstinence
Family Planning
Type
Natural
How it Works?
Pros
Cons
Special Considerations
Natural Family
Planning Method
Natural
Contraceptive
Sponge
Barrier
Diaphragm
Cervical Cap
Cervical Shield
Barrier
Female Condom
Barrier
Male Condom
Barrier
Combined Pill
Hormonal
The Patch (Ortho
Evra)
Hormonal
Shot/Injection
(Depo Provera)
Hormonal
Vaginal Ring
Hormonal
Rod (Implanon)
Implantation
Paraguard
Implantation –
Copper IUD
Mirena
Implantation –
Hormonal IUD
Essure
Permanent
Sterilization Implant
Surgical Sterilization
Permanent
Morning After Pill
Permanent –
Emergency
Contraception
Rhogam – how is it given? When? What is the purpose?
Study Materials to Review
- Exam 2 Prep Assignment
- Exam 3 Prep Assignment
- Mini Med #1 and #2
- Procedure Chart (Exam #2 prep assignment)
- Fetal Well Being test chart (exam 2 prep assignment)
- Final Exam Study Outline (from BB)
- HESI Exam Feedback (from BB)
- HESI Review (by Professor Harrell)