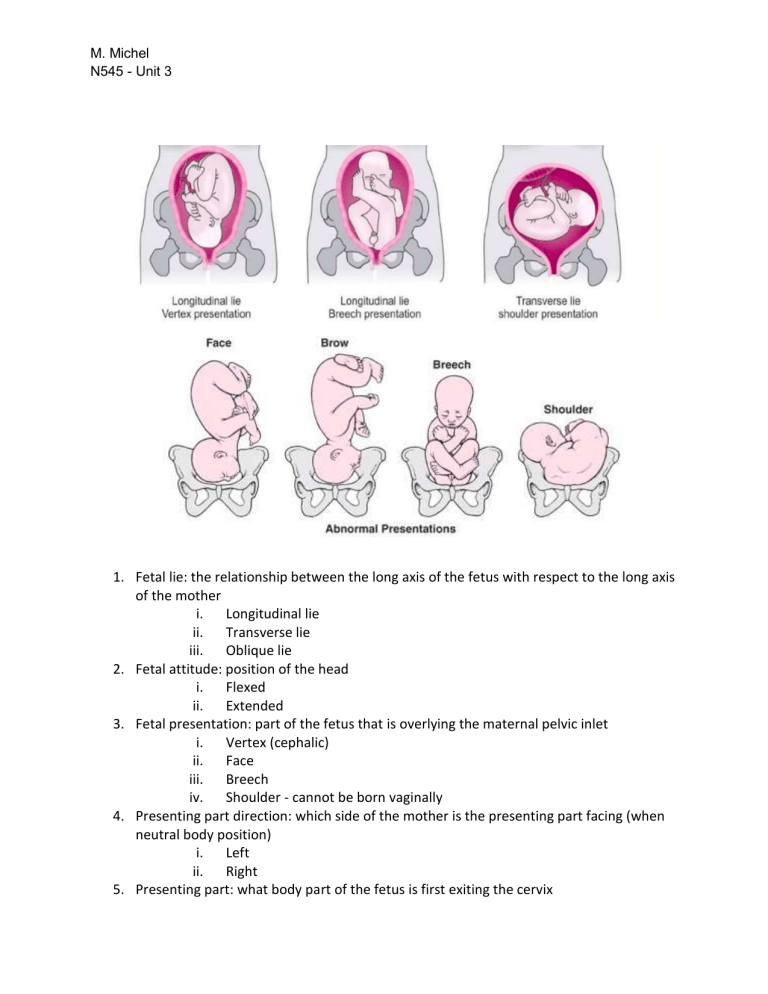
M. Michel N545 - Unit 3 1. Fetal lie: the relationship between the long axis of the fetus with respect to the long axis of the mother i. Longitudinal lie ii. Transverse lie iii. Oblique lie 2. Fetal attitude: position of the head i. Flexed ii. Extended 3. Fetal presentation: part of the fetus that is overlying the maternal pelvic inlet i. Vertex (cephalic) ii. Face iii. Breech iv. Shoulder - cannot be born vaginally 4. Presenting part direction: which side of the mother is the presenting part facing (when neutral body position) i. Left ii. Right 5. Presenting part: what body part of the fetus is first exiting the cervix M. Michel N545 - Unit 3 i. Occiput - head ii. Mentum - face iii. Sacrum 6. Presenting part position: which direction the presenting part is facing on the mother (forward, backward, sideways) i. Anterior ii. Posterior iii. Transverse 7. PRACTICE: ROT ROP OP LOP LOT LOA** LOA and ROA are most common and easiest positions 8. Factors associated with a positive birth experience: (5-7) a. Attending childbirth classes b. Motivation for the pregnancy c. A sense of competency d. Self-confidence, self-esteem e. Feelings of empowerment f. Positive relationship with mate g. Maintaining control during labor h. Support from partner or other individual during labor i. Not being left alone during labor j. Trust in the medical/nursing staff k. Having personal control over breathing patterns, comfort measures l. Choosing a healthcare provider who has a compatible philosophy of care m. Receiving clear information regarding procedures 9. Stages of Birth Process a. First stage: woman has contractions, cervix effaces and dilates completely to 10 cm i. Latent phase: 0-5 cm, usually mild contractions that gradually increase in frequency, duration, and intensity ii. Active phase: 5-7 cm, progressive fetal descent, increasing frequency, duration, and intensity of contractions iii. Transition* phase: 8-10 cm, usually the most intense phase of labor; contractions every 1.5 to 2 mins, lasting 60-90 seconds; feelings of M. Michel N545 - Unit 3 bearing down, rectal pressure, increased bloody show, rupture of membranes iv. Nursing responsibilities during first stage of labor: 1. Auscultate FHR, monitor mom’s vital signs 2. Monitor maternal temp - watch for infection 3. Collect urine sample 4. Palpate uterus during a contraction every 30 minutes to monitor frequency and duration 5. During active phase, may begin vaginal exams to assess cervical dilation and effacement a. Minimize to avoid: bacterial infections 6. Encourage mom to void b. Second stage: woman pushes, gives birth; complete dilation of the cervix to the birth of the newborn i. Crowning - fetal head remains visible between contractions ii. Cardinal movements of birth: watch “Cardinal Movements of Delivery” on Moodle c. Third stage: begins after birth of newborn and ends with delivery of the placenta i. Mom is at extreme risk for _hemorrhage_ until the placenta is delivered. ii. The placenta should be delivered within _30 minutes_ of birth. iii. Nursing responsibilities during third stage: (6) 1. Watch for signs of placental separation: gush of blood, moderate cramping 2. Palpate the _uterus_ for _bogginess_ 3. After placental separation, ask mom to _bear down to assist in delivery of the placenta_ 4. May need to administer oxytocics (Pitocin) to help contract uterus M. Michel N545 - Unit 3 5. Note _time_ of delivery of placenta 6. Possibly cord blood analysis for acidosis if: abnormal FHR, meconium, low APGAR 7. Ensure other staff are following mom’s wishes d. Fourth stage: postpartum period lasting 1-4 hours after delivery; uterus contracts to control bleeding at the placental site i. Nursing responsibilities during fourth stage: 1. Palpate _uterus_ frequently for 4 hours (assessing for _bogginess_) a. Displacement of uterus may be caused by: full bladder encourage mom to void 2. Wash perineum with gauze squares and warmed solution, then dry before placing sanitary pad 3. Encourage mom to move legs to: prevent DVT 4. Assess pain frequently 5. Assist with comfort measures a. Position changes b. Ice pack/pad changes c. Topical medications to reduce perineal edema, discomfort, if needed 6. Inspect and record quantity of vaginal discharge a. Heavy: >1 pad/hr b. Moderate: 1 pad q1-2 hrs c. Light: <1 pad q 2hrs 7. Watch for fundus rising and displacing to right 8. Palpate bladder for distention 9. Transfer from birthing unit after 1 hour or more if condition is stable 10. Offer food/drink to mom and partner 10. Fetal Station: the relationship of the fetal head to mom’s pelvis a. Most narrow part of pelvis: ischial spines = 0 station b. Above ischial spines: -3 → -2 → -1 → 0 c. Below ischial spines: 0 → +1 → +2 → +3 M. Michel N545 - Unit 3 11. Five Factors of the Process of Labor and Birth: a. Passageway: birth canal (mom’s body) b. Passenger: fetus c. Passageway/passenger relationship: fetal orientation and size compared to pelvic size d. Powers: forces of labor - contraction, pushing, etc. e. Psychological considerations *alterations in any of these processes can affect birth outcome for mom or baby 12. Signs of true labor: a. Timing of contractions: regular, get longer, stronger, and closer together b. Change with movement: contractions continue despite position changes c. Strength of contractions: get steadily stronger d. Pain of contractions: usually start in the back and moves to the front 13. Braxton-Hicks contractions: practice contractions; do not get longer, stronger, or closer together; typically resolve with position changes; not painful - feels like a tightening and located in the front of the belly 14. Pain management during labor a. Non-pharmacological methods: i. Deep breathing ii. Distraction iii. Heat iv. Movement, repositioning v. Tubs, water submersion b. Pharmacological methods: i. Epidural anesthesia 1. Monitor vitals, pain, level of sedation, motor and sensory fcn M. Michel N545 - Unit 3 2. Pros: Minimal effects of baby 3. Cons: Requires bedrest, foley, site assessment, can cause “epidural headache” ii. IV pain medications 1. E.g. fentanyl, morphine 2. Monitor respiratory status, pain management, opioid overdose 3. Pros: Less expensive, mom can still move around 4. Cons: Not highly effective, stays in the baby’s system for ~1 week 15. This image shows which medical emergency during childbirth: umbilical cord prolapse a. Appropriate nursing management of the above situation includes: i. If possible, flip mom onto hands (elbows) and knees ii. Manually push presenting part off the umbilical cord iii. Call for help b. Risk for this complication increases with: premature rupture of membranes (PROM) i. Chart color, consistency, smell, and amount of the amniotic fluid (meconium?) 16. Childbirth interventions: a. Cervical ripening i. Prostaglandins ii. Misoprostol (Cytotec) iii. mechanical balloon iv. medications require: continuous fetal monitoring b. Labor induction via stimulation of uterine contractions i. Pitocin - synthetic form of oxytocin ii. Indications: 1. DM, renal disease, preeclampsia/eclampsia, post-term gestation, PROM, mild abruptio placentae, IUGR, etc. iii. Risks to mom: tachysystole, uterine spasms, tetanic contractions, uterine rupture, arrhythmias iv. Risks to baby: retinal hemorrhage, bradycardia, arrhythmias, CNS depression, jaundice c. Episiotomy: surgical cutting of perineum to enlarge vaginal outlet M. Michel N545 - Unit 3 i. Increases risk of severe tearing → fourth degree lacerations, anal sphincter tears ii. Not generally used anymore iii. Spontaneous tears heal faster because: more likely to tear through weak parts of muscle/skin, less bleeding, heals faster d. Forceps-assisted birth i. Used to mechanically pull baby out in cases of dystocia, fetal distress, abnormal presentation ii. Risks to baby: ecchymosis, edema, cephalohematoma, transient facial paralysis, ocular trauma, low APGAR, elevated bilirubin iii. Risks to mom: lacerations of birth canal, extension of median episiotomy into the anus, perineal pain, sexual problems postpartum, incontinence, increased risk for infection e. Vacuum extraction i. Application of suction to baby’s head to aid in speed of delivery ii. Discontinue if: reach three “pop-offs” iii. Contraindications: 1. True CPD 2. Non-vertex presentation 3. Suspicion of coagulation defects 4. Hydrocephalus 5. Fetal scalp trauma f. Cesarean i. Indications (~10): 1. Complete placenta previa 2. Breech presentation 3. Transverse lie 4. Placental abruption and nonreassuring FHR 5. Active genital herpes 6. HR decels 7. >1 previous cesarean 8. Cervical cerclage 9. Cardiac conditions 10. Increased ICP (in mom or baby) 11. Severe respiratory distress 12. HIV infection in mom 13. Severe mental illness ii. Types of incisions 1. Lower uterine segment transverse - best 2. Lower uterine segment vertical - preferred for multiples gestation, abnormal presentation, placenta previa, preterm fetus, macrosomic fetus 3. Classic - only used if rapid birth is needed M. Michel N545 - Unit 3 iii. iv. Risks (~5): 1. Infection 2. Reactions to anesthesia 3. Blood clots, bleeding 4. Risks increase with subsequent pregnancies Unique post-op nursing responsibilities: 1. Evaluate incision and change dressing 2. Position mother on her side 3. Vitals every 15 min, gradually increase time as mom becomes more stable 4. Encouraging breastfeeding, make effort to assist parents in bonding - can be more difficult after cesarean birth 5. Evaluating perineal pad frequently 6. Monitor I/O, observe for signs of blood 7. Constipation reduction strategies: fiber, stool softener