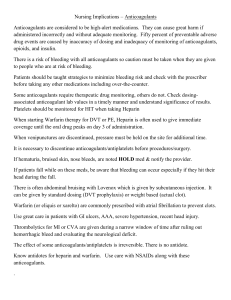
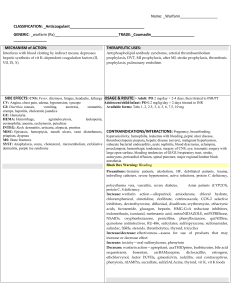
Chapter 40: Anticoagulants, Antiplatelets, and Thrombolytics PowerPoint Notes Drugs that prevent thrombosis Thrombosis is the formation of a clot in an arterial or venous vessel Anticoagulants prevent the formation of clots that inhibits circulation Antiplatelets prevent platelet aggregation Platelet aggregation is the clumping of platelets that forms clots Thrombolytics attack and dissolve blood clots Pathophysiology: Thrombus Formation Arterial clots are made of both red and white clots (platelets), which initiate the process, followed by fibrin formation, and traps the red blood cells in the fibrin Venous blood clots form when fibrin attaches to red blood cells During thrombosis, platelets: 1. adhere to endothelial lining 2. synthesize thromboxane A2 (a product of prostaglandins and a potent stimulus for platelet aggregation) Anticoagulants Inhibit clot formation They DO NOT dissolve clots that have already formed but PREVENT new clots from forming Used in patients with venous and arterial problems that put them at risk for clot formation o Venous Problems: DVT (deep vein thrombosis) and pulmonary embolism (PE) o Arterial Problems: coronary thrombosis, myocardial infarction, cerebrovascular accidents, stroke, or presence of artificial heart valves Heparin Indicated for rapid anticoagulant effect when thrombosis occurs because of DVT, PE, or an evolving stoke o Heparin is primarily used to prevent venous thrombosis, which can lead to PE or stroke Used in open-heart surgery to prevent blood clotting and in patients with disseminated intravascular coagulation (DIC) Heparin combines with antithrombin III, which prevents thrombosis formation by inhibiting thrombin The inhibiting of thrombin prevents the conversion fibrinogen to fibrin and thus the clot is prevented Partial thromboplastin time (PTT) and activated partial thromboplastin time (aPTT) are lab test used to detect deficiencies of certain clotting factors o These tests are used to monitor heparin therapy Heparin can decrease platelet count causing thrombocytopenia Given SQ for prophylaxis or IV for acute thrombosis If hemorrhage occurs during heparin, protamine sulfate is given to reverse the actions of heparin Low-Molecular Weight Heparins (LMWHs) Possess a lower risk of bleeding Frequent lab monitoring of aPTT IS NOT required Enoxaparin, Lovenox, & dalteparin are LMWH LMWHs are prescribed for: 1. DVT and acute PE (pulmonary embolism) after orthopedic or abdominal surgery 2. Hip and knee replacement anticoagulant therapy often includes enoxaparin 3. Abdominal surgery includes dalteparin Administrated SQ once or twice a day: available in prefilled syringes Average treatment lasts 7 to 10 days: treatment usually begins within 24 hours of surgery The half-life of LMWH’s is two to four times longer than heparin Instruct patients not to take antiplatelet drugs such as aspirin while taking LMWHs or heparin: teach patients how to administer SQ injections LMWH’s are contraindicated in patients with: 1. Strokes 2. Peptic ulcers 3. Blood anomalies LMWH’s should NOT be given to patients having eye, brain, or spinal surgery Direct Thrombin Inhibitors Directly inhibit thrombin from converting fibrinogen to fibrin Argatroban and bivalirudin are given IV Desirudin is given SQ Dabigatran is an oral anticoagulant that does not require continuous coagulation monitoring Oral Anticoagulant: Warfarin (Coumadin) Inhibits hepatic synthesis of vitamin K, thus affecting clotting factors Warfarin is primarily used to prevent: Thromboembolic conditions: PE, thrombophlebitis, and embolism formation caused by atrial fibrillation Oral anticoagulants prolong clotting time and are monitored by the prothrombin time (PT) o PT is a lab test that measures the time it takes blood to clot in the presence of certain clotting factors The international normalized ratio (INR) is the laboratory test most frequently used to report PT results o Normal INR is 1.3 to 2 o Patients on Warfarin INR is maintained at 2 to 3 o The desired INR for patients with mechanical heart valves or recurrent systemic embolism is 2.5 to 3.5 Warfarin has a long half-life and drug accumulation can occur and lead to external or internal bleeding o As the nurse, observe for petechiae, ecchymosis, tarry stools, and hematemesis and teach the patient to do the same The antidote for warfarin is Vitamin K, usually takes 24 to 48 hours to be effective: a low dose of vitamin K may be given to patients with an INR of 5.5 For acute bleeding, fresh frozen plasma is indicated Warfarin and Heparin Pharmacodynamics & Pharmacokinetics Heparin is poorly absorbed in the GI tract and is given SQ for prophylactic anticoagulant therapy or by IV for immediate response Warfarin, an oral anticoagulant, is absorbed through the GI; food will delay but no inhibit absorption Warfarin is effective for long-term anticoagulant therapy o PT for warfarin should be 1.5 to 2 times the reference value o INR for warfarin should be 2 to 3 o Higher levels up to 3.5 are usually required for patients with prosthetic heart valves Heparin can be used in pregnancy Warfarin CAN NOT be used during pregnancy Side Effects and Drug Interactions (Warfarin) Bleeding (hemorrhage) is a major adverse effect of Warfarin Patients should be monitored for signs of bleeding such as petechiae, ecchymosis, GI bleeding, ocular hemorrhage, and hematuria Aspirin, NSAIDS, other types of anti-inflammatory drugs, and oral hypoglycemic drugs can displace Warfarin o Acetaminophen should be used instead of aspirin when patients are on Warfarin Vitamin K (phytonadione) is given as a coagulant to decrease bleeding and promote clotting Heparin and Warfarin Comparison Heparin Warfarin Binds with antithrombin Inhibits hepatic synthesis of which inactivates thrombin Vitamin K which decreases Drug Action prothrombin Uses 1. Treat venous thrombosis 2. PE 1. Treatment of DVT 2. PE 3. TIA 3. Thromboembolic 4. Prophylactic for complications cardiac heart valves 4. DIC (heart surgery) Contraindications 1. Hemophilia, 1. Hemophilia, peptic ulcer peptic ulcer 2. Hypertension 2. Hypertension 3. Severe liver or 3. Severe liver or renal disease renal disease 4. Alcoholism Lab Test PTT: 60-70 Seconds PT: 11-15 s Anticoagulant Anticoagulant therapeutic level: therapeutic level 1.5-2x control in 1.25-2.5 control in seconds seconds Normal aPTT: 20-35 Normal INR 1.3-2 seconds Anticoagulant INR 2- Anticoagulant aPTT: 30-85 seconds 3 Prosthetic heart valves INR up to 3.5 Antidote Protamine sulfate Vitamin K (phytonadione) Nursing Process Anticoagulant Assessments Obtain a history of abnormal clotting or health problems such as severe alcoholism or severe liver or renal disease o Warfarin is contraindicated in patients with blood dyscrasias, peptic ulcer, CVA, hemophilia, or severe hypertension Gather drug history that includes use of CAM therapy A baseline PT or INR should be obtained before warfarin is administered Nursing Interventions Monitor vital signs o An increased pulse rate followed by a decreased systolic pressure can indicate external or internal bleeding Monitor PT or INR for Warfarin o PT should be 1.25 to 2.5x the control level o INR should be 2 to 3; except in patients with prosthetic heart valves, INR may be up to 3.5 Monitor PTT and/or aPTT for Heparin o PTT should be 1.5 to 2x the control level o Anticoagulant aPTT should be 30-85 seconds Examine patient’s mouth, nose (epitaxies), urine(hematuria), and skin for bleeding Check stools for occult blood Keep anticoagulant antagonist near o Vitamin K for Warfarin o Protamine Sulfate for Heparin Monitor for Purple-toe syndrome o Rare compilation that usually occurs 3-8 weeks of warfarin therapy o Treat by stopping warfarin and switching to fondaparinux Patient Teaching Teach patient to inform dentist when taking an anticoagulant Use a soft toothbrush to prevent bleeding from gums Use an electric razor because bleeding from cuts may be difficult to control Encourage no smoking; smoking increases drug metabolism so warfarin may need to be increased Teach patients taking warfarin to use acetaminophen instead of aspirin CAM Therapies and Anticoagulants Dong quai, feverfew, garlic, ginger, chamomile tea, ginkgo may increase bleeding when taken with anticoagulants such as warfarin Ginseng may decrease the effect of Warfarin Cranberry may increase INR Antiplatelet Drugs Used to prevent thrombosis in the arteries by suppressing platelet aggregation Antiplatelet therapy is mainly used for prophylactic use in: 1. Prevention of MI or stroke in patients with a family history of these 2. Prevention of repeat MI or stroke 3. Prevention of stroke for patients having TIAs The four most common Antiplatelets are: 1. Aspirin 2. Clopidogrel (Plavix) 3. Dipyridamole (Persantine) 4. Ticlopidine (Ticlid) Clopidogrel is frequently used after MI or stroke to prevent a second event Clopidogrel and aspirin may be prescribed together for a more effective approach in inhibiting platelet aggregation DO NOT take clopidogrel if the patient has a bleeding peptic ulcer, any active bleeding, or intracranial hemorrhage Abciximab, eptifibatide, and tirofiban are used primarily for acute coronary syndromes: for preventing reocclusion of coronary arteries after PTCA Thrombolytics (Alteplase, Tenecteplase, Reteplase) Occlusion of an artery or vein caused by a thrombus results in ischemia that causes tissue necrosis Thrombolytics dissolve a new thrombus or embolus, thus decreasing tissue necrosis For MI: Administer 3-4 hours of the event or within 30 minutes after arrival at the hospital For CVA administer within 3 hours of the event Commonly used thrombolytics include: 1. Alteplase 2. Tenecteplase 3. Reteplase Hemorrhage is the biggest complications o Aminocaproic acid is the antidote used to stop bleeding