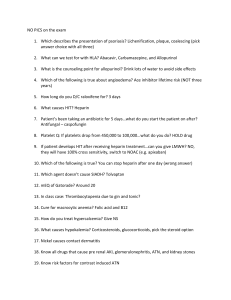
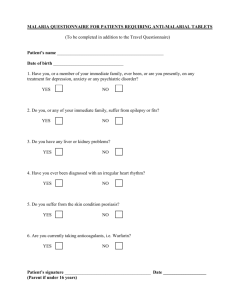
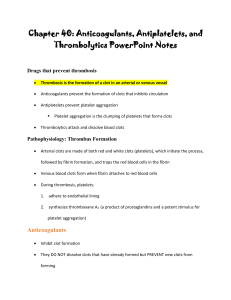
Nursing Implications – Anticoagulants Anticoagulants are considered to be high-alert medications. They can cause great harm if administered incorrectly and without adequate monitoring. Fifty percent of preventable adverse drug events are caused by inaccuracy of dosing and inadequacy of monitoring of anticoagulants, opioids, and insulin. There is a risk of bleeding with all anticoagulants so caution must be taken when they are given to people who are at risk of bleeding. Patients should be taught strategies to minimize bleeding risk and check with the prescriber before taking any other medications including over-the-counter. Some anticoagulants require therapeutic drug monitoring, others do not. Check dosingassociated anticoagulant lab values in a timely manner and understand significance of results. Platelets should be monitored for HIT when taking Heparin When starting Warfarin therapy for DVT or PE, Heparin is often used to give immediate coverage until the oral drug peaks on day 3 of administration. When venipunctures are discontinued, pressure must be held on the site for additional time. It is necessary to discontinue anticoagulants/antiplatelets before procedures/surgery. If hematuria, bruised skin, nose bleeds, are noted HOLD med & notify the provider. If patients fall while on these meds, be aware that bleeding can occur especially if they hit their head during the fall. There is often abdominal bruising with Lovenox which is given by subcutaneous injection. It can be given by standard dosing (DVT prophylaxis) or weight based (actual clot). Warfarin (or eliquis or xarelto) are commonly prescribed with atrial fibrillation to prevent clots. Use great care in patients with GI ulcers, AAA, severe hypertension, recent head injury. Thrombolytics for MI or CVA are given during a narrow window of time after ruling out hemorrhagic bleed and evaluating the neurological deficit. The effect of some anticoagulants/antiplatelets is irreversible. There is no antidote. Know antidotes for heparin and warfarin. Use care with NSAIDs along with these anticoagulants. . Heparin Considerations: The preferred anticoagulant for use during pregnancy is heparin which can be given IV or s.q. The dose may be standard or weight adjusted. Protocols may be used adjust heparin dosing in a hospital setting. Heparin may be given as a continuous infusion and would require an infusion pump. Administration calls for independent double checks for dose and dosage changes. Heparin and low molecular weight heparin are incompatible in a syringe. Protamine sulfate is the antidote. Warfarin Considerations: INR is used for monitoring – target is generally 2.5-3. Wear medic alert bracelet. Avoid high risk behaviors. Avoid excessive dietary vitamin K intake. Warfarin is category X for pregnancy. Check with prescriber before taking any new drugs including OTCs. Fibrinolytic Drugs Considerations: Used for acute MI, alteplase is also used for ischemic stroke, PE, and low-dose for blocked central venous catheters. It is contraindicated in active bleeding and with significant risk of bleeding. Complete any necessary invasive procedures (lab draws, etc.) prior to initiating. Narrow window of opportunity when used for stroke or MI.