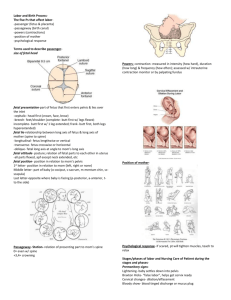
Labor and Delivery Archer Review Crash Course Welcome! ● ● ● ● If you have a question please enter it in the chat! I will do my best to answer questions as we go, but if I miss one will always circle back to you! We will take 1-2 breaks throughout the class Handouts & powerpoint slides are located in the ‘Handouts’ section of your GoToWebinar control panel. You can download and print them from here! If you have any technical issues or questions about streaming, handouts, etc. please email support@archerreview.com Labor Mom - The Four P’s Powers Passageway Passenger Psyche Powers ● Pushing ○ ○ ○ ● Voluntary When fully dilated Push during contractions Contractions ○ ○ Involuntary Uterine muscle contracts around fetus Passageway ● ● Birth canal Pelvis ● Does the baby have enough space to successfully pass through? ○ Width Passenger ● The baby ○ ○ Size ■ Macrosomia <4,000g Tolerating labor? ■ HR decelerations Psyche ● Emotions ○ ○ ○ ○ ● Fear Anger Joy Excitement Support ○ ○ ○ ○ ○ Who is in the room? Father Doula Doctor Midwife Baby ● ● ● ● ● Attitude Lie Presentation/Presenting part Position Station Attitude ● ● The posture of the fetus Relationship of fetal head to maternal spine ○ Flexion - normal ○ Neutral ○ Dorsiflexion ○ Extension Lie ● Relationship of fetal and maternal spines ○ ○ ○ Longitudinal ■ Parallel spines ■ Normal Transverse ■ Perpendicular spines Oblique Presentation ● Presentation - The position of the baby in the birth canal ○ ○ Cephalic ■ Vertex ■ Brow ■ Face Breech ■ Frank ■ Full ■ Footling Cephalic Presentations Breech Presentations Vertex Shoulder presentation Presenting Part ● Presenting part - the part of the fetus that leads through the birth canal ○ ○ ○ ○ ○ Head Foot Shoulder Abdomen Butt Position ● ● The position of the baby in relation to the mom’s pelvis Presenting part and the relationship of that part to the mom ○ ○ ● Anterior, posterior, or transverse Right or left Left occiput anterior ○ Most common Station ● ● How far down in the birth canal the baby is. Measured in relation to mom’s ischial spine ○ ○ Most narrow spot At ischial spine = 0 station Leopold Maneuvers #1 - Fundal Grip #2 - Umbilical grip #3 - Pelvic Grip #4 - Second Pelvic Grip Labor and Delivery Complications Placenta Previa Anatomy Normal Previa Classifications of previa The classification depends on where the placenta is located ● Complete ○ The placenta is completely covering the cervix ● Partial ● Marginal ○ ○ Part of the placenta covers the cervix Placenta covers only the edge of the cervix Complete placenta previa Partial placenta previa Marginal placenta previa Assessment ● ● ● ● Major symptom is PAINLESS bright red bleeding The fact that it is painless is very important That sets it apart from an abruption To assess the bleeding ○ ○ ○ ● ● Pad count to determine the amount Clots Color Ultrasound done to confirm diagnosis Ultrasound will determine type of previa Nursing Interventions ● ● ● Never ever perform a vaginal exam if you suspect a placenta previa! Would never want to irritate the placenta or uterus. Continue to monitor for blood loss. ○ ○ ○ ● Patient may have to stay on the unit to be monitored Preform pad counts Weigh pads ■ 1 gram = 1 mL blood loss. Cesarean section indicated in most cases Patient Education ● Bed rest ○ ● Bleeding ○ ○ ○ ● This may minimize blood loss Report any bleeding that occurs Monitor blood loss Excessive amounts of blood loss may need treatment. Monitor baby ○ If there is excessive blood loss, perfusion to the fetus can be decreased. NCLEX Question You are triaging a new patient in the antepartum unit. They tell you that they started bleeding this morning and were told to come in by their OB. They deny any pain or other symptoms. Which of the following nursing interventions do you anticipate initiating? Select all that apply. a. b. c. d. Bed rest Pad counts Emergency vaginal delivery Vaginal exam Answer: A and B A is correct. The nurse suspects a placenta previa based off of the clients complaint of painless bleeding. With a placenta previa, bed rest is indicated to prevent further bleeding. This is an appropriate nursing intervention to initiate for both the safety of the mother and fetus and should be done right away. B is correct. Pad counts are a way of monitoring the quantity of blood loss. Because the nurse suspects placenta previa and the patient is reporting vaginal bleeding, pad counts are an appropriate nursing intervention to initiate. When obtaining pad counts, they can be done in two ways. If exact quantity of blood loss is not indicated, the nurse can just count the number of pads saturated with blood. If the health care provider orders strict monitoring, the pads will be weighed to obtain the exact number of milliliters of blood lost. When weighing pads, 1 gram is 1 milliliter of blood lost. Pad counts at a minimum should be initiated for any suspected placenta previa, so this is an appropriate nursing intervention. C is incorrect. An emergency vaginal delivery is contraindicated for a patient with suspected placenta previa. Because we believe that the placenta is either partially or fully covering the cervix of this patient, a cesarean section will need to be performed. This may be distressing for some mothers, so be sure to provide education about why this is the safest option for their and their baby’s health. Vagnial deliveries with a placenta previa can cause serious harm to the mother and fetus, and are contraindicated. D is incorrect. Vaginal exams are contraindicated for a patient with a suspected placenta previa. In this patient, we suspect that the placenta is either partially or fully covering the cervix of this patient. That means that if a vaginal exam were to be performed, the hand of the examiner would touch the placenta. We do not want to cause this irritation and exacerbate the bleeding that is already occurring. Vaginal exams are always contraindicated on patients with either confirmed or suspected placenta previa. NCSBN Client Need: Topic: Physiological Integrity Subtopic: Physiological adaptation Reference: Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. Subject: Maternal and Newborn Health Lesson: Labor and Delivery Abruptio Placentae Anatomy Types ● ● Causes massive amounts of painful bleeding. Two types ○ ○ ● Incomplete is only partial separation of the placenta. ○ ○ ● Incomplete Complete Causes internal bleeding Blood backs up behind the placenta Complete is when the placenta completely detaches ○ ○ Causes massive external bleeding Very painful Physiology ● ● ● ● ● ● Once the placenta has detached, it is no longer connected to maternal circulation This mena there is no more perfusion from mom to baby No perfusion means no oxygen or nutrients. This is why an abruption is considered a MEDICAL EMERGENCY ‘ The baby needs oxygen! Stat c-section!! Assessment ● ● ● ● ● ● ● Dark red bleeding Intense abdominal pain Board like abdomen (due to internal bleeding) Rigid uterus Hypotension (Think shock due to blood loss) Maternal tachycardia Fetal bradycardia (fetal distress!!) Interventions ● Monitor for fetal distress ○ ● Monitor maternal bleeding ○ ○ ○ ○ ● ● Signs of distress? Stat c-section! Abdominal pain Board like abdomen Dark red vaginal bleeding Change in fundal height (blood in abdomen?) Keep the BP up with IVF and/or blood products Prepare for delivery - most likely c-section. Previa vs. abruptio Previa - painless bleeding Abruption - Painful bleeding NCLEX Question Which of the following signs and symptoms are expected for your patient experiencing abruptio placenta? Select all that apply. a. b. c. d. Painless bleeding Dark red bleeding Hypotension Rigid abdomen Answer: B, C, and D A is incorrect. Painless bleeding is NOT a sign of abruptio placenta. Rather, it is a sign of placenta previa. In placenta previa, the placenta is covering the cervix. This causes painless bleeding. In abruptio placenta, the placenta separates from the wall of the womb. This causes a massive amount of very painful dark red bleeding. It is important to remember the difference between these two emergencies. Placenta previa presents with painless bleeding, and abruptio placenta presents with painful bleeding. B is correct. Massive amounts of dark red bleeding is a prominent sign of abruptio placenta. This is due to the placenta separating from the wall of the uterus. This massive amount of bleeding causes hypotension as the mother enters hypovolemic shock, and fetal distress as perfusion to the baby decreases dramatically. C is correct. Due to the massive amounts of dark red bleeding, hypotension is a sign of abruptio placenta. When the mother loses large amounts of blood, her blood pressure will drop. This hypovolemia is treated with IV fluids and/or blood products such as PRBCs. D is correct. A rigid, board-like abdomen is a sign of abruptio placenta. This is also due to massive blood loss. As the placenta separates from the wall of the womb blood starts to accumulate in the abdomen, causing it to become rigid, and ‘board-like’. NCSBN Client Need: Topic: Physiological Integrity Subtopic: Physiological adaptation Reference: Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. Subject: Maternal and Newborn Health Lesson: Labor and Delivery Dystocia What is dystocia? “Difficult birth, typically caused by a large or awkwardly positioned fetus, by smallness of the maternal pelvis, or by failure of the uterus and cervix to contract and expand normally.” (Perry et. al., 2013). Causes ● ● ● ● ● Macrosomia Malposition of the fetus Hypotonic contractions Hypertonic contractions Maternal pelvis Macrosomia Extremely large fetus Greater than 4,000 grams Unable to fit through maternal pelvis Malposition of fetus Fetus is not in proper alignment for maternal pelvis. Incorrect positioning means they will not be putting pressure on the pelvis and therefore not causing dilation and effacement. Maternal anatomy of pelvis plays a role too. Hypotonic Contractions Weak and ineffective contractions Not able to work efficiently enough to get fetus through maternal pelvis Hypertonic Contractions Contractions are too strong and too fast. So fast, that they are not allowing the uterus time to relax and refill with proper nutrients. Uncoordinated and not effective to cause dilation and effacement. Maternal Pelvis Anatomy of the maternal pelvis can play a role If it is too narrow for the size of the fetus the shoulder can become stuck during delivery (shoulder dystocia). Assessment Mother: ● ● ● Fetus: Extreme pain (especially with hypertonic contractions) Uncoordinated contractions Labor is not progressing as expected. ○ ○ ○ Dilation Effacement Station ● ● ● Fetal distress If contractions are too strong and too frequent the placenta will not be providing sufficient oxygenation to the fetus. Monitor fetal heart rate for late decelerations. Interventions ● Monitor for fetal distress ○ ● Medications ○ ○ ○ ○ ● ● Notify the health care provider for any fetal distress Pain medications IV Fluids Tocolytics ■ Given for hypertonic contractions Oxytocin ■ Given for hypotonic contractions Rest between contractions! Need to focus during contractions. Patients with hypotonic contractions may be encouraged to walk to try and get the contractions into a pattern. Education ● ● Educate the mother about the pain she is experiencing and her options for medication. Positioning is important for optimal oxygenation to the fetus ○ Left side lying is encouraged. NCLEX Question Which of the following are causes of dystocia? Select all that apply. a. b. c. d. Hypertonic contractions Macrosomia Hypotonic contractions Breech presentation Answer: A, B, C, and D A is correct. Hypertonic contractions are contractions that are too strong and too frequent. This is a cause of dystocia. The contractions are not effective in causing dilation and effacement, and do not help labor progress. They are extremely painful. Treatment for mothers experiencing hypertonic contractions would include tocolytics and pain medication. B is correct. Macrosomia is defined as a fetus that is much larger than average; greater than 4,000 grams. Because of the size of these infants, it is difficult for them to fit through the maternal pelvis. This often causes a specific type of dystocia; shoulder dystocia, where the shoulder of the infant essentially becomes stuck behind the pubic bone and causes prolonged and difficult labor. C is correct. Hypotonic contractions are contractions that are very weak and uncoordinated. They are a cause of dystocia. When contractions are weak and uncoordinated they are ineffective in causing dilation and effacement and labor does not progress as expected. Treatment would include oxytocin or helping the mother walk to get her contractions into a pattern. D is correct. Breech presentation is one type of malpresentation that can cause dystocia. When the fetus is not lined up in a cephalic presentation, fitting through the maternal pelvis becomes very difficult and causes dystocia. NCSBN Client Need: Topic: Physiological Integrity Subtopic: Physiological adaptation Reference: Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. Subject: Maternal and Newborn Health Lesson: Labor and Delivery Break! Back at... Preterm Labor Terminology ● Term - A baby born from 37-40 weeks gestation ● Preterm - A baby born between 20 and 37 weeks ● Preterm labor - Any labor occuring between 20 and 37 weeks ● Viability - The threshold at which an infant can survive outside the womb ○ ● PROM - Premature Rupture of Membranes ○ ● About 20 weeks gestation Rupture of the membranes before labor begins. PPROM - Preterm Premature Rupture of Membranes ○ PROM that occurs before the 37th week of gestation, or prematurely. Assessment ● ● ● Important to determine if it is true labor, or ‘false’ labor. Many women experience Braxton Hicks contractions in their second and third trimester, but these are not indicative of true labor. Assessment of true labor ○ ○ ○ ○ ○ Contractions at regular intervals. Contractions of increasing intensity Pelvic pain Lower back pain Rupture of membranes Interventions ● ● ● Try to stop labor! If at all possible, we want contractions to stop so that the pregnancy can continue and the baby can be born at a normal gestational age. Ways to stop labor: ○ ○ ○ ● ● ● Tocolytics ■ Terbutaline ■ Magnesium Sulfate Bedrest Fluids Must monitor both mother and baby closely Evaluate the mothers contractions and their frequency, and how the fetus is tolerating the contractions. If PROM or PPROM monitor closely for infection. Obstetric Medications ● Tocolytics - slow contractions ○ ○ ○ ○ ● Terbutaline Magnesium-sulfate Indomethacin (prostaglandin inhibitor) Nifedipine (CCB) Oxytocics - stimulate contractions ○ ○ ○ Oxytocin Ergometrine (Methergine) Misoprostol Education ● ● Most important educational point for mothers is what the signs and symptoms of true labor are, so that they know when to call their doctor. Teach mothers to call their OB for: ○ ○ ○ ○ ● Rupture of membranes Regular contractions Contractions that become stronger and more frequent with walking (Braxton Hicks will fade away with walking) Back pain Once preterm labor has begun, educate mothers about tocolytics and the importance of bedrest. NCLEX Question Which of the following are symptoms of true labor? Select all that apply. a. b. c. d. Contractions that dissipate with walking Contractions that come in regular intervals Lower back pain Contractions of consistent intensity Answer: B and C A is incorrect. Contractions that fade away with activity, a change in position, or rehydration are not a sign of true labor. These are more likely Braxton Hicks contractions, which do not indicate labor. They are ‘practice contractions’ for the uterine muscle. True contractions will not fade with activity, come in regular intervals, become closer together as time goes on, and become more intense as time goes on. B is correct. Contractions that come in regular intervals are a sign of true labor. You should educate mothers to seek care for contractions that come in regular intervals, and become stronger and closer together with time. These contractions also will not go away with a change in position or activity. C is correct. Lower back pain is in fact a sign of true labor. Both lower back pain and pelvic pain indicate true labor, and mothers should be educated to seek treatment when such treatments present. ‘False’ labor, or braxton hicks, do not present with these symptoms. They are much weaker than contractions, and typically subside with a change in position or by going on a short walk. D is incorrect. Contractions of consistent intensity indicate braxton hicks, or ‘false’ labor. When a mother is in true labor, her contractions will increase in intensity over time. Education should be provided on the difference between braxton hicks and true labor so that mothers know when to call their OB and seek treatment. NCSBN Client Need: Topic: Physiological Integrity Subtopic: Physiological adaptation Reference: Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. Subject: Maternal and Newborn Health Lesson: Labor and Delivery PROM Definition The rupture of membranes before labor begins. “Rupture of membranes” is when the amniotic sac breaks - when someone says their water broke this is what they mean. This is supposed to happen after labor starts. With the amniotic sac intact there is a buffer between the uterus and the infants preventing contractions. The lack of this can stimulate contractions. Assessment ● Whenever the membranes rupture, always assess the color amount and odor. ○ ○ ○ ○ ● ● ● ● Should be clear Should not have a foul odor Can be just a small amount of fluid up to a few hundred mLs. If the membranes are yellow, green, malodorous, etc…. Worry about infection!! Infection is the major concern with PROM, so that is what your assessment with focus on. Temperature WBCs CRP Interventions ● Nitrazine test ○ ○ ○ ● Monitor for infection ○ ○ ○ ○ ● pH test that differentiates amniotic fluid from urine or other secretions. Strip will turn blue if the fluid is amniotic fluid This will confirm rupture of membranes Temperature WBCs CRP Antibiotics if indicated Fetal monitoring ○ ○ Heart rate Decelerations NCLEX Question Which of the following statements is true regarding premature rupture of membranes (PROM)? Select all that apply. a. b. c. d. PROM is when the membranes rupture before 37 weeks gestation. Membranes are expected to rupture before labor begins A priority nursing intervention with PROM is to monitor for infection. When observing the fluid after rupture of membrane, it should be clear and without odor. Answer: C and D A is incorrect. PROM stands for Premature Rupture of Membranes. This is defined as the rupture of membranes (or “water breaking”), before labor begins. This term is not related to at what gestation the membranes rupture. If the membranes rupture before 37 weeks gestation, the correct terminology is PPROM. This stands for Preterm Premature Rupture of Membranes. The Preterm part of this acronym is what refers to the membranes rupturing before 37 weeks gestation. B is incorrect. It is not expected that the membranes will rupture before labor begins. In a normal delivery, there is rupture of membranes after the mother has begun having regular contractions, dilating, and effacing. When the membranes do rupture before labor has started, it is called PROM, or premature rupture of membranes. C is correct. A priority nursing intervention with PROM is to monitor for infection. When the membranes are ruptured before labor begins, the baby is then exposed to bacteria and pathogens of the outside world. These germs can enter the birth canal and infect both the mother and the infant. One of the most important observations you must make is of the color, odor, consistency, and amount of the amniotic fluid when the rupture of membranes occurs. Any discolored or malodorous fluid may indicate an infection. After the rupture of membranes occurs, the nurse should monitor the mother's temperature, WBC count, CRP, and other markers of infection. D is correct. It is very important to assess the color, odor, consistency, and amount of fluid when rupture of membranes occurs. If the fluid is green or yellow and malodorous, it is indicative of infection. If the fluid is brown or black it is indicative of meconium passing in utero. The expected finding of amniotic fluid is a clear fluid with no odor. NCSBN Client Need: Topic: Physiological Integrity Subtopic: Physiological adaptation Reference: Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. Subject: Maternal and Newborn Health Lesson: Labor and Delivery Postpartum Hemorrhage What is it? Why is it important Postpartum hemorrhage is the major loss of blood (hemorrhage) after a vaginal delivery. Can occur immediately after the delivery, up until 2 weeks after delivery (delayed postpartum hemorrhage) It is one of the major causes of maternal mortality! Almost 3% of women in the US will experience PPH to some degree!! More info: http://www.pphproject.org/maternal-morbidity-mortality.asp Risk factors for PPH ● ● ● ● ● ● ● ● Twins or triplets Macrosomic fetus Preeclampsia Prolonged labor Precipitous labor Use of forceps or vacuum during delivery Placenta previa Abruptio placenta Causes ● Uterine atony ○ ○ ○ ○ This is the inability of the uterus to contract Typically after birth, the uterus contracts to clamp down on all of the blood vessels and stop the bleeding If the uterus does not contract, or ‘clamp down’ hemorrhage will occur. This is the most common cause of PPH ● Injury to the birth canal ● Retention of the placenta ○ ○ ● Could be due to malpresentation of the fetus, use of forceps or vacuum, or a large fetus If the entire placenta is not expelled within 30 minutes of delivery, the mother is at risk for PPH Bleeding disorders ○ ○ DIC Mothers on lovenox or warfarin for pre-existing conditions. Definitions ● 2 types of PPH ○ ○ ● Early - Occurs in the first 24 hours post delivery Late - Occurs after the first 24 hours post delivery To qualify as PPH, the mother must lose 500 ml of blood if she had a SVD and 1,000 ml of blood if she had a cesarean section. Assessment ● Boggy uterus ○ ○ ● Blood loss ○ ○ ○ ● This is a uterus that is not contracting to clamp down on the blood vessels The fundus will feel soft instead of hard as it should. Pad counts - most PPH patients are saturating pads every 15 minutes Puddle of blood in the bed If they try to stand up for the first time there could be a huge gush of blood Shock - if there is large amounts of blood loss leading to hypovolemia ○ ○ ○ ○ ○ Decreased LOC Pale Diaphoretic Hypotensive Tachycardic Interventions ● Fundal massage ○ ○ ○ ● Estimated Blood Loss (EBL) ○ ○ ○ ● Massage the fundus - hard! Warn the mother this will hurt, but you must do it to get the uterus to contract and stop the bleeding. Every 15 minutes at a minimum Weigh pads to estimate the loss 1 g = 1 mL Monitor hemoglobin and hematocrit Mediations ○ ○ ○ Oxytocin Methylergonovine Blood products NCLEX Question Which of the following conditions are considered a risk factor for women to experience postpartum hemorrhage? Select all that apply. a. b. c. d. Microcephaly Dystocia Placenta previa Singleton pregnancy Answer: B and C A is incorrect. Microcephaly is a newborn complication where the newborn is born with a head smaller than average. This is not a risk factor for a woman to experience postpartum hemorrhage. If you selected this answer, you may have gotten it confused with macrosomia, a condition where the infant is larger than average, specifically greater than 4,000g. This is a risk factor for postpartum hemorrhage. B is correct. Dystocia, a prolonged and difficult labor, is a risk factor for postpartum hemorrhage. Prolonged labor specifically can dramatically increase the risk for postpartum hemorrhage. C is correct. Placenta previa is a risk factor for postpartum hemorrhage. In placenta previa, the placenta is covering the cervix of the mother rather than sitting in the fundus of the uterus as it should be. This puts the mother at risk for postpartum hemorrhage. D is incorrect. A singleton pregnancy, or a pregnancy with only one fetus does not pose a risk for postpartum hemorrhage. The risk factor for postpartum hemorrhage is with multiples; such as twins or triplets. NCSBN Client Need: Topic: Physiological Integrity Subtopic: Physiological adaptation Reference: Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. Subject: Maternal and Newborn Health Lesson: Labor and Delivery Prolapsed Umbilical Cord What is a prolapsed cord? ● ● ● Umbilical cord slips through the cervix and into the vagina after rupture of membranes and before the baby descends into the birth canal. During delivery, the prolapsed cord become compressed by the presenting part of the fetus This cuts off oxygen to the fetus Assessment ● ● Cord visualized protruding through vagina Cervical exam ○ ○ ○ Something squishy? Pulsing? Mom feels something between legs Nursing Interventions ● ● ● Elevate the presenting part of the fetus off of the prolapsed cord Keep your hand on the baby’s head lifting it up and call for help Positioning ○ ○ ● ● ● ● Knees-to-chest position - open the pelvis Trendelenburg - let gravity shift the baby off the cord Administer oxygen NEVER ATTEMPT TO PUSH THE CORD BACK IN!!!! Wrap cord in sterile moist towel Emergency Cesarean delivery Fetal Heart Monitoring Terminology Variability ● Fluctuation in the fetal heart rate Acceleration ● A speeding up of the fetal heart rate Deceleration ● A slowing down of the fetal heart rate Reassuring ● The baby looks healthy! Non-reassuring ● Something is wrong with the baby Variability: ● Absent ● Marked ● Moderate Absent Variability - Bad! Marked variability - Can be either bad or good! Moderate variability - Good! Accelerations Accelerations Decelerations ● Early ● Variable ● Late Early decelerations Variable decelerations Late decelerations VEAL CHOP V - Variable E - Early A - Acceleration L - Late C - Cord Compression H - Head Compression O - Okay P - Placental Insufficiency Reassuring ● ● ● Baseline heart rate in the normal range: 110-160 Moderate variability Accelerations Non-Reassuring ● ● ● ● ● Fetal tachycardia - HR >160 Fetal bradycardia - HR <110 Decreased variability Variable decelerations Late decelerations Nursing Interventions - Non-reassuring fetal heart rate LION PIT L: Lay the mother on her LEFT side I: Increase IV fluids O: Oxygen N: Notify the healthcare provider PIT: Discontinue Pitocin NCLEX Question The nurse is taking vital signs on a pregnant client in active labor. When she inflates the blood pressure cuff, she looks at the fetal monitor and notices that the fetal heart rate increases above baseline, and then returns to baseline about 15 seconds later. What is the priority nursing action? a. b. c. d. Notify the healthcare provider. Document and continue to monitor Place the mother on her left side Administer 100% FiO2 via face mask Answer: B A is incorrect. The nurse has observed an acceleration in the fetal heart rate. This is when the fetal heart rate increases by 15 bpm above the baseline. An acceleration lasts about 10-15 seconds, and then the heart rate returns to baseline, as the nurse observes in this question. Accelerations are a reassuring sign observed on a fetal heart rate monitoring strip, and do not need to be reported to the healthcare provider. B is correct. Because the nurse has noted a reassuring sign of the fetal heart rate, it is most appropriate for her to document the finding and continue to monitor the mother. IF the nurse had noticed a non-reassuring sign, other interventions would be necessary. C is incorrect. The nurse has observed an acceleration in the fetal heart rate. This is when the fetal heart rate increases by 15 bpm above the baseline. An acceleration lasts about 10-15 seconds, and then the heart rate returns to baseline, as the nurse observes in this question. Accelerations are a reassuring sign observed on a fetal heart rate monitoring strip, and do not require repositioning of the mother to the left side. D is incorrect. The nurse has observed an acceleration in the fetal heart rate. This is when the fetal heart rate increases by 15 bpm above the baseline. An acceleration lasts about 10-15 seconds, and then the heart rate returns to baseline, as the nurse observes in this question. Accelerations are a reassuring sign observed on a fetal heart rate monitoring strip, and do not require administration of 100% FiO2 via face mask. NCSBN Client Need: Topic: Effective, safe care environment Subtopic: Coordinated care Reference: Leifer, G. (2019). Introduction to maternity and pediatric nursing. Subject: Maternity Nursing Lesson: Problems with Labor and Delivery NCLEX Question The nurse assists a mother in labor to the bathroom, and notes that the fetal heart rate increases from 130 to 190. She sits the mother back down in bed, and the fetal heart rate remains 190. Which of the following nursing actions would be appropriate? Select all that apply. a. b. c. d. Lie the mother down on her left side Decrease the rate of her IV fluids Administer oxygen Continue to monitor the mother Answer: A and C A is correct. The nurse has noted fetal tachycardia. Any increase in fetal heart rate above 160 is considered tachycardia. When it persists for longer than 10 minutes, it is problematic and requires intervention. Any nonreassuring fetal heart rate will require intervention. You can remember these interventions with the mnemonic LION: lie the mother on her left side, increase IV fluids, oxygen, and notify the healthcare provider. In this case, the nonreassuring sign of fetal tachycardia necessitates intervention, and lying the mother on her left side is an appropriate intervention B is incorrect. Decreasing the rate of the mother’s IV fluids is not appropriate. Instead the nurse should increase the rate of IV fluids to help better facilitate blood perfusion to the placenta and fetus. Increasing not decreasing the fluids is the appropriate nursing intervention. C is correct. Administering oxygen is an appropriate nursing intervention for the noted fetal tachycardia. This will go along with repositioning the mother on to her left side, increasing the rate of IV fluid administration, and notifying the healthcare provider. D is incorrect. It is inappropriate to simply continue to monitor the mother. The nurse has noted fetal tachycardia, a nonreassuring sign that requires intervention. The nurse should lie the mother on her left side, increase her IV fluids, administer oxygen, and notify the healthcare provider. NCSBN Client Need: Topic: Effective, safe care environment Subtopic: Coordinated care Reference: Leifer, G. (2019). Introduction to maternity and pediatric nursing. Subject: Maternity Nursing Lesson: Problems with Labor and Delivery But….How do I study?!?! Answer: The Sure Pass Program If you follow the Sure Pass Program and fail the NCLEX, Archer will give you a 100% money back refund for ALL PRODUCTS! Sure Pass Program Details What you get: 1. Immediate on-demand access to most recent live Rapid Prep AND multiple topic-wise webinars, a total of 40 hours, 2-months access. Watch at your own convenience. 2. Registration in next live Rapid Prep course. Attend in person and get the most out of this interactive class! 3. 2 months of On-demand access to the live Rapid Prep 4. Question Bank - access to 2600+ practice questions 5. Customizable learning assessments 6. Printable handouts, slides, notes, and cheat sheets. Sign up for the Sure Pass Program: r o f u o y https://archerreview.com/about-nclex-rn k n a h T r u o g Next live Rapid Prep: joinin se! July 19th & 20th r u o C h 8am-6pm CST s a r C