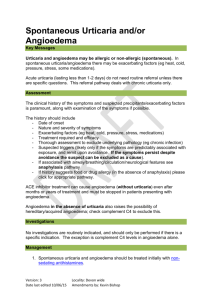
- It characteristically dermatomal - It is often confined to a single dermatome - It is limited to one dermatome in normal hosts, but can occasionally affect two or three neighbouring dermatomes - Involvement of Cutaneous may be patchy or confluent, with skin changes beginning with redness and inflammation followed by the development of clusters of small, clear vesicles. - Patient usually complains of localized pain and an erythematous vesicular rash that follows a dermatomal distribution. - While pain is the most common symptom of zoster and can precede the rash by days to weeks and most patients describe a deep burning sensation or report dysesthesias - Some patients have a few scattered vesicles located at a distance away from the involved dermatome and this has no particular prognostic significance - Herpes zoster may also result in meningeal inflammation and clinical encephalitis - Occasionally, VZV reactivation affects motor neurons in the spinal cord and brain stem resulting in motor neuropathies Common Characteristics of Urticaria - Lesions can appear anywhere on the surface of the skin - It has variable number, size and shape - Usually occurs in a few hours (<24 hours) leaving behind normal skin - Half the patients with urticaria have associated episodes of angioedema - Itching is minimal and the swelling may last for several days - Itching is prominent - Erythematous macules - Edematous wheals with a surrounding flare Treatment of Urticaria A. Patient education B. Eliminate triggers: - If the cause of urticaria is recognised then it should be removed and eliminate triggers is considered to be most effective. C. First-line Therapies: - Histamine is the main mediator of urticaria with H1 receptor causing the itch, whealing and flare. - H1 antihistamines are the first line of treatment and they act as inverse agonists of H1 receptors. - While it is believed that combine antihistamines of 2 different groups (sedating and non-sedating or a long acting and short acting) can lead to better control of urticaria symptoms. - Antihistamines reduce pruritus, flatten wheals, shorten wheal duration and reduce wheal numbers. - Chlorpheniramine and pheniramine can be taken at night if sleep is disturbed by urticaria. D. Second-line Therapies: - Second-line therapies may be considered when urticaria does not respond well to antihistamines. - The most common drugs are corticosteroid, adrenaline and doxepin. - Corticosteroid drugs can stabilize mast cell membranes and inhibit further histamine release. It can also reduce the inflammatory effects of histamine and other mediators. - Adrenaline can be used in anaphylactic shock or severe anaphylactoid reactions and angioedema of the oropharynx in severe acute allergic urticaria and idiopathic angioedema. Dosage should be 0.3 0.5mg of adrenalin should be administered intramuscularly. E. Other Treatment: - Vitamins K and B12 may be useful in some cases of chronic urticaria. - Medications are available to reduce permeability of the vessels: Calcium and Vitamins C and P. -