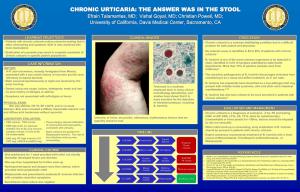
Urticaria Commonly referred to as hives, is swelling of the dermis and one of the most common skin conditions seen in clinical practice with a prevalence of approximately 20 percent in the general population. Urticarial lesions are intensely pruritic, circumscribed, raised, erythematous plaques, often with central pallor. Individual lesions are transient, usually disappearing within 24 hours, not painful and resolve without leaving residual ecchymotic marks on the skin, unless there is trauma from scratching. Acute urticaria — Urticaria is considered acute when it has been present for less than six weeks. Chronic urticaria — Urticaria is considered chronic when it is recurrent, with signs and symptoms recurring most days of the week, for six weeks or longer. More than two-thirds of cases of new-onset urticaria prove to be self-limited. The lesions of acute and chronic urticaria are identical in appearance, so when the problem first develops, it is not possible to differentiate the two disorders. Pathophysiology A. Immune-mediated mast cell activation: 1. Type 1 hypersensitivity • Allergen-bound IgE antibodies bind to high-affinity cell surface receptors on mast cells and basophils. • Release of prostaglandins, leukotrienes, bradykinin, kallikrein results in vasodilation, increased vascular leak and pruritis. 2. Autoimmune: • IgG auto-Abs bind directly to IgE receptors and induce degranulation. B. Nonimmune-mediated mast cell activation: • Direct nonallergic activation of mast cells by certain drugs (opioids) • Drug-induced cyclooxygenase inhibition that activates mast cells by poorly understood mechanisms • Activation by physical or emotional stimuli; mechanism is poorly understood but possibly involves the release of neuropeptides that interact with mast cells Acute urticaria most often results from type I hypersensitivity reactions, a presumptive trigger (drug, food ingestion, insect bite or sting, infection) occasionally can be identified. Chronic urticaria most often results from idiopathic causes and autoimmune mechanism. Acute urticaria: Chronic urticaria: Food Idiopathic Medication Autoantibody-associated Insect sting or bite Infection Contact allergy Transfusion reaction Idiopathic Etiology identified in 40-60% of acute cases and 10-20% in chronic cases Management • H1 antihistamines: mainstay, first-line choice • H2 antihistamines • Glucocorticoids The approach is to treat all patients with H1 antihistamines, adding H2 antihistamines for more severe symptoms and reserving oral glucocorticoids for those patients with prominent angioedema or persistent symptoms despite antihistamines.