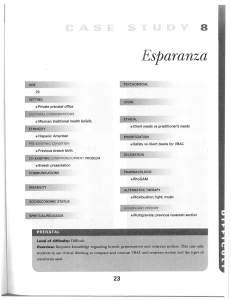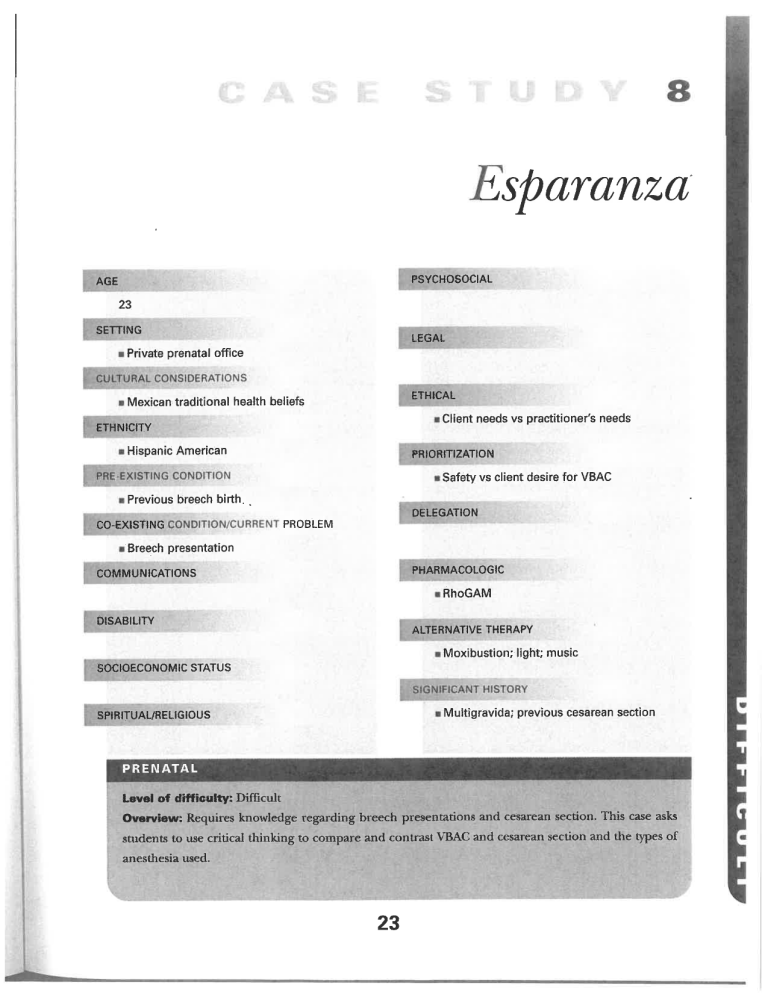
sparanza -/ PSYCHOSOCIAL AGE 23 SETTING LEGAL Private prenatal office ETHICAL Mexican traditional health beliefs Client needs vs practitioner's needs ETHNICITY Hispanic American PRtORlTIZATION Safety vs client desire for VBAC Previous breech birth. DELEGATION PROBLEM CO-EXlSTtNG Breech presentation PHARMACOLOGIC COMMUNICATIONS RhoGAM DISABILITY ALTERNATIVE THERAPY Moxibustion; light; music SOCIOECONOMIC STATUS Multigravida; previous cesarean section SPIRITUAL/RELIGIOUS PRENATAL Level of difficulty: Difficult Overview:Requires knowledgeregardingbreech presentations and cesareansection. This case asks students to use critical thinking to compare and contrast VTBAG and anesthesia used. 23 cesarean section and the types of -RRENATAL CASE STUDIES Client Profile Esparanza, isa_23~year'old'G2P1001'MHF at36wga-Shehada previousce- ^rcanisectlonwithan epidura!in Mexicosixyearsagof^ - breechpresentation"at 5,8,w:lks.ges^onalag^The babyweighed- pounds;She"is~five £eT^inucheds Sln(VBAC) ^^LP W^: lolpounds. this. fcn with shewould like Pregnancy' however she saw even consider doinga VBAC. Case Study ava^^^^^Z six doctors before"shefounu d one' Elpara,nzajeems anxiousat. today'sprenatalvisit-shet^ Acnursethatthe I tt!^he. ad±upwdeTher. ribsandshefearsa""the7cesa;e^ection'^ i. The followingdatais obtainedat thisvisit: Wt 125 lb FHT 140s URQ Fundal height (FH) 35 cm Fetal movement +(FM) Urine chemstrip testing: all negadve No HA, vision changes NoCVAT No edema Questions 1.Whywasit so difficult for Esparanza to find an obstetriGian whowould consider doing a VBAC? Discuss the ethical dilemmas that exis^when the desiresandneedsofthe dientcome in conflictwith those ofthe practitioner. -\ 2.What ar^ the routfne labs for this visit, and are they done at this dme? 3.CompareandcootrastVBACandrepeatce- sarean section for the followiiig: safetyfor both C7 C7. B. mothef and bal^, cost, pdin; long-term effects, ef- fccts onbreastfeeding, andparenting. 4.Her obstetrician asksforherpreviouscesarean section records before he wUl even consider a "s VBAC.Why? 5.Whyarecesareansecdonsustiallydonefor breech presentation? 6.Whenwoulda vagina]deliverybeconsidered for a breechpresentation? C7 c. 7.Howcanthebabybeencouraged tomove to a cephalic presentation? Rgure 1.2 Escms^le^ofbnech presentations. CASE STUDY 8 8. What matemal/fetal conditions contribute to a babypresentingin a breech presentation? 9. Compare and contrast spinal and epidural anesthesia for cesarean section. 10.If the babychangesto a cephalicpresentation in the next two weeks but Esparanza does not go into spontaneouslabor, can she besafelyinduced 11.What.methods can be used if any? 12. Esparanza begins to cry at the 39-week visit \ when she realizes that the baby has not yet changed position. She;says that "Ijiist know it's going to be terrible again.I'll never be able to breastfeedmy babypostpartum; it's so painful." Howshouild the nurse respond? ' foraVBAC? References Biancuzzo, M. (2003). Breastfeedingthe newborn: Clinical strategies for nurses (2nd ed. ). St Louis, MO: Mosby. Littleton, L., & Engebre.tson, J. C. (2002). Maternal, neonatal, and women's health nursing. Clifton Park, NY: Thomson Delmar Learning. Riordan, J., & Auerbach, K. (2005). Breast feeding and human lactation (3rd ed. ). Sudbury, MA: Jones and Bartlett. Simpson, K. R., & Creehan P. A. (2001). AWHONN perinatal nursing (2nd ed. ). Philadelphia: Lippincott, Williams & Wilkins. Ttran, D., & Mack, S. (2000). Complementary therapies for pregnancy and childbirth (2nd ed. ). London: Bailliere Tindall. relatedto safelyduringthisprocedure. Shewill be broughtinto the labor and delivery area and given prostaglandin vaginally. In some cases they may give her a prostaglandinpreparationorallythe nightprior to try to induceher. However, the prostaglandin used orally (Cytotec) has been associated with uterine ruptare and maynot be a good choice with fetal demise. Prostaglandins maycause hyperstimulation leading to placenta abruption and uterine rupture, and they need careful monitoring. Depending on the type used, shewill have to waitfrom 30 minutes to up to six hours prior to oxytocin being used to induce the con- tractions. Sometimes the prostaglandins themselves start contractions. She may experience nausea, vomiting, and diarrhea with the prostaglandin use. Anddiarrheal and antiemedc drugs maybe used. Her vital signswill need to be monitored throughoutthe laboranddelivery.Vaginalexamsshouldbelimited to reduce risk ofinfection. Painmedicadons maybe appropriate; however, they should not be used to protect the stafffrom having to dealwith the mother's grief. Theycan be used to help her dealwith the physicalpain of the induced birth. Ifthey are used to cloud her cogitadve senses in the hope ofrelieving her grief, they maydojust the opposite andmake it harder for her to cope with her loss. Sheneedsemotionalsupport. Thismaybein theform ofa gentle touchor simply remaining at her bedside for a longer dme when she is being checked. Depending on her religious preferences, she might be asked ifshe desires some- onefrom herfaithto be called,or the nursecanevensaya prayerwithher. She maywear a saint's medal or amulet for spiritual protecdon. The nurse should be careful when changing her gown not to lose these. These are ways of showing the mother that she is being caredfor by persons who appreciate her griefand respect her need to experience it. A doula who has experience working with womendeliveringa deadbabywouldbe an excellentsupportfor her. After the birth the mother and father should be given the opportunity to see their baby. This can be difficult since the babyhasbeen deadfor some time. Wrap the babyin a warm blanket andprepare the parents for thefactthat the babywill notfeel like a livebaby.Encourage them to name the babyand, iftheywish,to explore the baby. The nurses should refer to the babyby name. The nurses who are withherin deliveryshouldmakea pointofvisidngwithherpostpartum to allow her an opportunity to ask questions and express her grief. Ended Beginnings by Claudia Panuthos and Catherine Romeo provides some excellent insight into the emotional journeys parents take after the loss of a baby. The stories told by the mothers andfathers clearly demonstrate thatparents, although theyappearto be in a state ofnon-feeling during this period, arevery much aware ofevery person around them andthat thesepersons havea profound impacton howwell theparents can process the grieffor months andyearsafterward. References Panuthos,C., & Romeo, C. (1984). Endedbeginnings.South Hadley,MA: Bergin& Garvey Publishers, Inc. Varney, H., Kriebs, J., & Gegor, C. (2004). Varney's midwifer/ (4th ed. ). Boston: Jones and Bartlett. Case Study 8: Esparanza 1. Whywasit so difficultfor Esparanzato findanobstetricianwhowoiildconsider doing a VBAC? Discuss the ethical dilemmas that exist when the desires and needs of the client come in conflict with those of the pracdtioaer. Although CASE STUDY 8 ^ACcations incarefully selectedcasesissaferthanrepeatcesareansection,the ] Ifa uterine mPturewere have caused many"obste'tricilas ram5I to occur ^refuse toofferthkoption. Otherfactorsthatdiscourage obstetridanTfr^ -nngwomen this choice are that a VBAC delivery alsorequires that the ob. stetncian, stay the hosPital durmS Ae active labor (whereasl sections finally) the comPensati°" for vagina7deliv"ery^s7ess3 ^lb ch!duled)'and' ls thanthatfor at cesarean a a cesarean section-There are many communTde'swhere^rs 1< tlon. lsnolongeravailabletowomen-forcingthem tou"dergounnecessary su^- geryor remain homefor unassistedvaginaldeliveries. 21 whatarethe routme labs for tlus visit and ^g!°Mnand hfm atocrit/H&H) whyare dley done ^ be checked. at this time? Her Hemodil'utio^ ^ye^st ?!tween. _24due and32weel". °fgestationwhenthewoman"ex"pen:e"nce;T^wT; hematocrit asloweTma-ease ml C mass.After 32weeks the red blood cell mass continues to increa7e"whileZ plasma. volumethe increase occurs at a slower rate' with the result'bemg'asUgh't risemH&H end of the third trimester. The hematocritis checLdTt636 to Ae/aPid in"ease in plasma with at w^sto. assessmaterna!sfatus nearterm-Anano^"^ groupB strepto^occu; ^) cultureneedstobedone.Approximately35%ofallwomenhaAorGBS" -thisseldomcausesa problem forthemother, ifthefetuswereto~become mfected during the birth, the infection could become generalized, ie adine"^ infection and death. When GBS isoidendfied7t h7mo?he^ cr^&al n^onafal be offered prophylactic andbiotics during her labor to"protecrt h7' ThLmothe', 'Lurine. is alsochecked for glucose, ketones, protein7n itrites"^d even ^ , leukocytes. HIVtestingandtestingforoAerSTIsmaybeIr^d^^. 3. Compare andcontrast VBAC andrepeat cesarean secdon for the foUowin^ safetyjwboth mother and baby'cost' Pam' long-term effec;7e7f^te7n ;, andparenting. Compare and Contrast VBAC Less chance ofinfections; quicker recovery -^ Safety for Mom RepeatCesareanSecdon Lesschanceofmpture ofutems; although risk is low if client is screened well and prostaglandins and oxytocins are not used Baby is better able to clear excessive fluids from the lungswitha vaginal delivery Less Postpartum much less Feelingsofaccomplishmentand SafetyforBaby SaferonlyifVBACresultedinuterinerupture Cost More Pain Greaterpostpartum for extended period Long-term Effects empowerment If desiredVBAC,mayfeel like a failure:risk for adhesionsandlong-range pain and complications from them Ableto breastfeedimmediately Effects on Breastfeeding Often delayed; baby often gets supplements; usually decreased success rate asdefined by mother Immediatebondingandabilityto hold andcareforbaby;earlierdevelopment ofconfidenceoncaringforbaby Effects on Parenting Delayed due to pain medications for major surgery andinability to take charge ofbaby for an extendedperiod 4. Her obstetrician asks for her previous cesarean secdon records before he will even consider a VBAC. Why? He will want to review the operative records to be certain that a low transverse uterine incision was made in the uterus and that there were no complicadons with healing after the surgery. 5. Whyare cesareansecdonsusuaUydone for breechpresentadon?There is no molding of the fetal head when there is a breech presentadon, thus there is a greaterdangerofanaftercomingheadbeingunableto passthroughthepelvis. This is true especiallysince the smaller bodyparts can begin to birth with less than 10 cm dilatation (Figure 1.2 in core text). Other problems are increased risk for prolapsed cord, uterine rupture, and fractures to the infant, usually to the clavicle or humerus. 6. Whenwould a vaginal delivery be considered for a breech presentadon? A vaginal breech delivery may be consideredwhen the physician is experienced in breech births and the mother is a muldpara with a history of uncomplicated normal spontaneous vaginal deliveries (NSVDs); current low, but normal baby estimated fetal weight (EFW) and the presentation is a complete breech presentation. A complete breech is the position where the fetal thighs and knees are flexed. 7 Howcan the babybe eucouragedto move to a cephalicpresentadon?There are several measures that may help. External version by the obstetrician in the hospital may change the presentation. Sometimes a tocolytic medication is used to relax the uterus while external manipulations are used to move the fetus into a more favorable presentation. This is usually done under ultrasound andwith continuous fetal heart rate monitoring. If the fetus develops distress, a cesarean section is immediately done. The manipulations may cause bleed- ing; therefore, if the mother is Rh negative, RJhoGAM needs to be given. However, after the versions these babies may reverse themselves back to breech prior to delivery. Other methods that have been used to turn a breech are having the mother try using a tilt boardseveral times a day, moxibustion on the fifth toe, and the use ofmusicandlight to the lowerpelvic areato encourage the baby to move toward them. (Moxibustion is a traditional Chinese medicine technique that involves the burning of mugwort, a small spongy herb, to facilitate healing.) 8. What maternal/fetal condidons contribute to a baby presenting in a breech presentation? Uterine relaxation associated with high parity Hydramnios Oligohydramnios Uterine abnormalities Neoplasms Contracted pelvis Fetal anomalies Placenta previa CPD 9. Compare and contrastspinal andepiduralanesthesiafor cesareansection. CASE STUDY Compare and Contrast Epidural -^ Maybeusedinlaboriftryingfora VBAC,then Timing increased if cesarean section is needed Mother mayfeel pulling sensations but not pain Pain/Discomfort None Often reported Spinal Not used for labor Usuallydoesnotfee]anything Post Anesthesia Headache Possible Post Anesthesia Backache Often reported 10. If the babychanges to a cephaUcpresentation m the next two weeks but ranzadoesnotgomtospontaneouslabor,canshebesafelyinducedfor a VBAC? Use ofprostaglandins and oxytocin for VBAC is the one factor that greatly increases risk for uterine rupture. If used, great caution and observation areneeded.Theobstetricianshouldremainwithinthedeliveryunitatalltime's in case an immediate cesarean section is needed. 11. Whatmethodscanbeusedifany?InductionwithanattemptedVBACincreases theriskforruptureduterus. However,sincetheobstetricianmustremainwith a^woman having a VBAC, he or she will often admit several women wishir VBACwho areclose to their due dates andinduce them at the same time. 12. Esparanzabeginstocryatthe39-weekvisitwhensherealizesthatthe 1 n^tyetchangedposition. Shesays,"Ijustknowit'sgoingtobeterribleagau, I'Uneverbe able to breastfeed my babypostpartum; it's sop^d. "~^o^ should thenurse respond? Mexican women tend tofearcesarean^ection'and seen aslifethreatening to themother (Simpson, 2001).Thenurseneedstoal~ . ESParanza to ex press her fears and also needs to listen to what problems she_experienced, last. time sothatshecanaddresseachone. Use'op^ended S!!mCTt!i_e.g" "Te"me aboutyourlastdeliver7-"Esparanzamayseekhelp from a curanderos, a natural healer, to tryto reposition thebaby. References Biancuzzo, M^(2003). Breastfeeding thenewborn: Clinicalstrategies fornurses(2nded. ). St Louis, MO: Mosby. LittIe,t!n'_L;_&Engebretson-J-c-I2002)-Maternal,neonatal,andwomen'shealthnursing. CliftonPark,NY:ThomsonDelmarLearning. Riordan,J.,& Auerbach, K.(2005). Breastfeedingandhuman lactation (3rdcd. ).Sudbury, MA: Jones and Bartlett. ' ---. " ..".. Simpson, K. R, & Creehan P.A. (2001). AWHONN perinatal nursing (2nd ed. ). Philadelohia: Lippincott, Williams & Wilkins. Tiran,D,& Mack,S.(2000). Complementar/ therapiesforpregnancyandchildbirth(2nded.: London: Bailliere Tindall. Case Study 9: Sarah 1. BasedonSarah'sobstetricalhistory,listtwomajorconcernsforthispregnancy. A history ofan LGAinfant, two SAB, repeated urinary tract infecrio^-and yeastinfections, alongwith a babywho experienced RDS, hypoglycemia, and