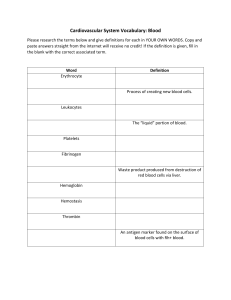
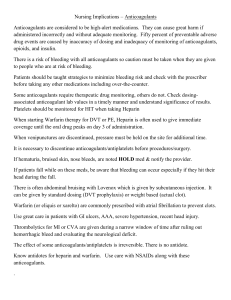
Anticoagulants Name: Suhena Shirin Barbhuiya Roll No: 08 Class: M. Pharm 1st Semester Institute Name: NETES Institute of Pharmaceutical Science Subject: Advance Pharmacology – I ANTICOAGULANTS Anticoagulants are the drugs that is used to reduce the coagulability of blood. Coagulation will occur instantaneously once a blood vessel has been severed. Blood begins to solidify to prevent excessive blood loss and to prevent invasive substances from entering the blood stream. CLASSIFICATION OF ANTICOAGULANTS Anticoagulant Used in vivo Parentral Used in vitro Oral Heparin Sodium Citrate Sodium Oxalate Sodium edetate Parenteral Anticoagulants Indirect thrombin inhibitor Direct thrombin inhibitors * Unfractionated heparin(UFH) * Low molecular weight heparin(LMWH) * Fondaparinux * Danaparoid * Bivalirudin * Argatroban * Desirudin Oral Anticoagulants Vit. K Anatagonists * Warfarin * Acenocoumarol Direct Factor Xa inhibitor * Rivaroxaban * Apixaban Oral direct thrombin inhibitors * Dabigatran Unfractionated heparin(UFH) Normally occurs as a macromolecule in mast cells with histamine. Commercial preparations extracted from beef lung or pig intestine. Mechanism of Action Heparin binds to antithrombin 3 to bring about conformational changes,that makes it faster in binding to thrombin. Then leaves the cpmplex in thrombin bonded to its inhibitor anti thrombin, to again bind to another anti thrombin 3. And the Cycle continues eventually decreasing blood coagulability. Pharmacokinetics of heparin It needs to be given intravenously as oral administration makes it unabsorbable because of tis high negative charge and molecular size. It works immediately after administation. And connot cross blood brin barrier or placental barrier making its use safe during pregnancy. As the heparin reaches live, it immediately gets inactivated and metabolites are excreted into urine. Adverse effects (ADR) Bleeding (Major ADR) Heparine induced thrombocytopenia. Hypersensitivity reactions like skin rashes, urticaria, fever etc. Osteoporosis. Low Molecular Weight Heparine (LMWH) Heparine has been fractionated into LMW form ( MW 3000-7000) by different techniques. LMW Heparines have a different anticoagulant profile i.e., they selectively inhibit factor Xa with little effect on factor IIa. Mechanism of action It increase the action of antithrombin-III on factor Xa (inhibit factor X) but there is no action on thrombin because the molecules are too small to bind to both enzymes and inhibitors. Advantages They have a higher bioavailability and longer T1/2 Have more predictable anticoagulant response because of reduced binding toplasma protein, platelets and osteoblast. There is a lower incidence of thrombocytopenia and osteoporosis as compared to UFH. They are used increasingly in place of UFH ADVERSE EFFECTS AND CONTRAINDICATIONS ARE SAME AS OTHER ANTICOAGULENTS Fondaparinux It is a synthetic parentral anticoagulant. It binds to antithrombin and selectively inactivates factor Xa without an effect on thrombin. It is administered subcutaneously. It is useful inn pulmonary embolism and deep vein thrombosis. It does not require routine laboratory monitoring It should not be administered in patients with renal failure. Parenteral Direct Thrombin Inhibitor They bind directly to thrombin and in activate it. They do not bind to antithrombin-III. Lepirudin inhibits thrombin irreversibly. Argatroban and Bivalirudin inhibit thrombin reversibly. They are used as anticoagulant in patients who are at risk of heparine induced thrombocytopenia. The main adverse effect is bleeding. Vitamin k Antagonist Coumarin (warfarin) Mechanism of action Inhibits the synthesis of biologically active forms of vitamin K dependent coagulation factors that are factor 2,7,9,10. As well as anticoagulant proteins. Warfarin interferes with natural process of vitamin k regeneration by inhibiting vitamin k epoxide reductase. Pharmacokinetics It is almost completely absorbed after oral administration. It is highly bound to plasma proteins and can cross placental barrier. Metabolized in liver and excreted in urine and stool. Adverse effects Bleeding: Most important and common side effect. Teratogenic effect: Warfarin is contraindicated during pregnancy. Skin necrosis: Rare complication that occurs within the 1st week of therapy. Other rare side effects: Diarrhoea, dermatitis, abdominal cramp etc Therapeutic Uses Venous thromboembolism. Atrial fibrillation. Myocardial Infarction. Drug Interactions Medications that decrease the effect of anticoagulants thus increasing the chance of blood clots ---- vit k ---Haloperidol ----Rifampin ---Phenobarbitol Medications that increase the effect of anticoagulants thus increasing the chance of bleeding ---Allopurinol ---Ciprofloxacin ---Aspirin ---Diclofenac THANK YOU