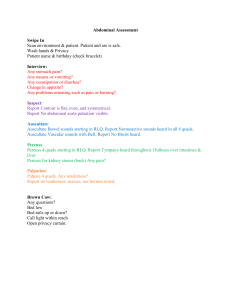
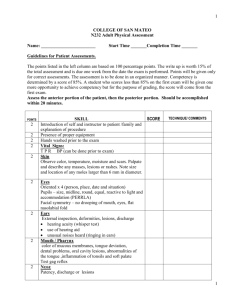
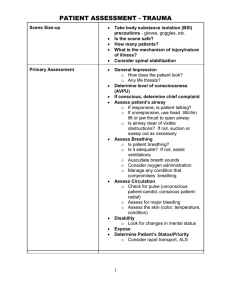
@stylebysumiyah 1 GENERAL ORDER OF THE EXAM * • Inspect → visually observe pt • Palpate → use hands to feel pt • Percuss → light striking of body parts to produce sounds • Auscultate → listening to body w/stethoscope o Bell = low-pitch sound o Diaphragm = high-pitch sound *All systems except GI 4 CLASSICAL ASSUMPTIONS • A & O x 4 (person, place, time, situation) • Vital signs WNL • Visual acuity assessed via Snellen chart (CN 2 – Optic) • Patient is in NAD PREPARATION • Knock on entry • Introduce yourself “Hi, my name is Sumiyah, and I’m a nursing student. I will be performing a physical exam on you today.” Hand hygiene o • GENERAL SURVEY • Physical Appearance o Age, sex, race/ethnicity • Body Structure o Tall/short o Underweight/overweight/average weight o Proportionality of weight to height • Mobility o Ease in ambulation o Ease in movement of limbs • Behavior/Mood o Response to questions o Grooming/hygiene o Affect/speech/eye contact Ex: “Pt is a (#) y/o (gender ident.) of avg. & proportional height & weight, who moves easily & responds to questions. They are well groomed & have appropriate affect to situation.” SKIN Inspect • Entire body → color, lesion, hair distribution • Finger/Toenails → pitting or clubbing • Describe lesions noting number, location, arrangement & type & document later Palpate (Use the back of the hand) • Moisture, temperature, texture, turgor (pinch back of hand), checking for tenting • Note areas of tenderness or induration “I will continue to inspect the rest of the body bilaterally throughout the remainder of my exam” HEAD → NCAT Inspect • Skull → general size & contour • Scalp → lesions or inhabitants • Hair → quantity, texture, distribution, balding • Face → symmetry (eyebrows, palpebral fissures in line with helices of ears, nasolabial folds) Palpate • Skull → deformities or tenderness • Temporal Artery → induration & intensity (2+ = normal) • TMJ → pain, popping or crepitus (pt. open/close mouth) Neuro Test • CN 7 (Facial - motor) → pt. smile, frown, puff cheeks, resist eye opening • CN 5 (Trigeminal - motor) → pt. clench jaw – masseter muscle engaged • CN 5 (Trigeminal - sensory) → light touch x6 (ask pt. close your eyes & say “now” when you feel it) “Pt is normocephalic – atraumatic” NECK Inspect • Obvious masses or pulsations Palpate • Lymph nodes of head & neck; identify chains o Preauricular, postauricular, occipital o Tonsillar, submandibular, submental o Anterior cervical, posterior cervical & deep cervical (lean R/L) o Supraclavicular, infraclavicular o Non-palpable or <1cm, mobile, & nontender • Carotids → pulses • Trachea → deviation • Thyroid → size, symmetry, tenderness, consistency, nodules (palpate from behind) Auscultate • Carotid & Thyroid for bruit Neuro Test • CN 11 – Spinal Accessory (motor) → shrug shoulders, turn head against resistance “CN 2 – 12 are intact” 2 EYES → PERRLA & EOMI Inspect • External Inspection o Eyelashes → point out & away o Conjunctiva/sclerae/cornea → clear & moist o Pupil → size & shape o (3-5mm b/l, round) • 3 Finger Test o Visual fields on confrontation (CN 2 – Optic) (Jazz hands) ▪ Start laterally → Ask pt. stare straight in front & let me know when you see my fingers o 6 cardinal fields of gaze (CN 3, 4, & 6 – Oculomotor, Trochlear & Abducens) (Cat Whiskers) ▪ Ask pt. follow my finger & not move your head o Accommodation & Convergence (CN 2 & 3) (Follow Finger) ▪ Ask pt. to follow my finger as I bring it closer to pt. face & away • 2 Light Test (Pen light) o Direct (CN 2) constrict & consensual (CN 3) light reflexes, consensually constricts o Corneal light reflex → strabismus (shine light & see that the light falls in the same place in both eyes) • 1 Ophthalmoscope Exam (Right Eye to Right Eye) o Catch red light reflex & move closer into pt. o Optic disc → clear, well defined, creamy yellow o 4 sets of retinal vessels o Macula → 2 optic discs away “Pt is PERRLA & EOMI - Pupils are equal, round, reactive to light & accommodation ; Extra ocular movements intact” EARS • Assess gross hearing (CN 8 – Vestibular Cochlear) o Normal conversation o Whisper test/finger rub o Ask pt. to close their eyes & point to the ear where they hear the finger rub o If abnormal, continue to Weber (midline) & Rinne (AC>BC) test Inspect • Auricle → symmetry, lesions, nodules • Special attention to back & top of ears as it is a common site for skin cancer Palpate • Tragus & mastoid → tenderness Otoscopic Exam • Maneuver Auricle o Adults Pinna → up & back o Peds Pinna→ down & back • Inspect canals → cerumen (ear wax), foreign bodies, inflammation, discharge • Inspect TM & note presence of the following/abnormalities o Not bulging or retracted o Pearly gray color o Bony prominences o Cone of light (R ‘ 5; L ‘ 7) MOUTH & PHARYNX 3 Inspect • Lips → swelling, color, lesions (ask pt. to smile) • Teeth & gums → dentition, swelling, color, lesions (ask pt. to open mouth) • Buccal mucosa → color, moisture, lesions • Tongue → lesions, moisture, texture o Pink, moist & well papillated • Presence of Wharton (underneath tongue) & Stenson ducts (upper 2nd molar) • Posterior pharynx → color, exudate, lesions o Non-red, non-injected o Grade tonsils (1-4) • Patency of salivary glands → parotid & submandibular Neuro Test • CN 12 (Hypoglossal) → stick out tongue, noting deviation • CN 9 (Glossopharyngeal - motor/sensory) → press down w/ tongue blade, ask pt. to say “ah,” noting rise & position of uvula • CN 10 (Vagus) → gag reflex NOSE & SINUSES • Assess nasal patency o Ask pt. to occlude one nostril by pinching down & breath in Inspect • Nose → midline • Septum → deviated or perforated • Nasal mucosa → color, exudate, swelling, polyps o Mucosa → moist, pink o Turbinate’s → beefy red Palpate • Frontal & maxillary sinuses → tenderness 4 POSTERIOR LUNGS Inspect • RR & rhythm, overall effort (RR 12-20) • General contour, spine midline • Rib interspaces, accessory muscles (are they using them?), no retractions Palpate • Respiratory expansion (thumbs rise and fall equal bilaterally, note symmetric expansion of hands) • Tactile fremitus – feeling for vibrations diminishing (4 spots) “99” (palmar surface) Percuss • Diaphragmatic excursion (3-5cm) bilaterally o Ask pt. to breathes out → percuss from resonance to dullness o Ask pt. to breathes in → percuss from resonance to dullness o Flat = bone o Dull = organ • 7 spots: intercostal spaces (ICS) → resonance • Percuss right middle lobe (RML) Auscultate • Lung fields: same 7 spots (deep breaths in/out w/ open mouth) o Assess right middle lobe (RML) • Normal clear breath sounds are o BV → superior medial o V → peripheral lung • Note adventitious breath sounds: wheezes, crackles, pleural rubs, stridor ANTERIOR LUNGS (in front of pt.) Inspect • RR & rhythm, overall effort • General contour • Rib interspaces, accessory muscles (are they using them?), no retractions • Transverse: Anterior-Posterior diameter →(2:1) Palpate • Respiratory expansion (thumbs rise & fall equal bilaterally, note symmetric expansion of hands) • Tactile fremitus – feeling for vibrations diminishing (3 spots) “99” (palmar surface) • Fluid = better sound of “99” Percuss • 6 spots: ICS → resonance Auscultate • Lung fields: same 6 spots (deep breaths in/out w/ open mouth) • Normal clear breath sounds (V, BV) • Note adventitious breath sounds 5 Vitals Check Reminders • Radial Pulse o Bilaterally; note differences if any • Blood Pressure o Pt. should be at rest in a comfortable, relaxed position, legs uncrossed o Continue to fill air bladder 30mmHg beyond the disappearance of sounds of turbulent flow to account for the auscultatory gap CV NECK Inspect • Carotid/jugular pulsations, neck vein distention (JVD) Palpate • Carotid pulse → bilaterally (one at a time) Auscultate (Bell) • Carotids → presence/absence of a bruit • Instruct pt. to hold breath/hold breathe w/ pt. CV CHEST Inspect • Precordium → heaves or lifts Palpate • Palmar surface of hand over; o Auscultatory areas (see pics) → thrills o Location of PMI Auscultate • Note murmurs, rubs or gallops Diaphragm and Bell (sitting) • Aortic (2 ICS RSB) → S2 > S1 • Pulmonic (2 ICS LSB) → S2 > S1 • Erb’s Point (3 ICS LSB) → S2 = S1 • Tricuspid (5 ICS LSB) → S1 > S2 • Mitral (5 ICS MCL) → S1 > S2 Bell in the left lateral decubitus position (knees up on side) • Mitral/Left ventricle (PMI) Diaphragm while leaning forward • Aortic & Pulmonic 6 ABDOMEN *Inspect, Auscultate, Percuss, Palpation* (4 quadrants, start at RLQ→ clockwise) Inspect • Stand on pts RIGHT side • Patients arms by their sides, (not above their head) lying down, knees bent → go to bathroom if necessary • Visualize skin-note, symmetry, scars, masses, protuberance, distention, increased or absent aortic pulsations, general size, contour, shape Auscultate • Auscultate for bowel sounds → 4Q, 530x/min (diaphragm) • If absent, listen for 5 mins • Auscultate for abdominal bruits (aorta/renal/iliac/femoral) (bell) “Bowel sounds are normal active in all 4 quadrants” Percuss • Percuss all 4Q’s in a z-like pattern o 2 spots/quad • Identify areas of tympany & dullness o Pay special attention to the flanks for areas of dullness → tympany to dullness • Measure the vertical span of the liver o From lower border: ▪ Tympany →dullness o From upper border: ▪ Resonance → dullness o 6-12 cm at MCL, 4-8 cm at MSL • Percuss for splenomegaly o L anterior axillary line, at lowest intercostal space o Percuss (tympanic) →have pt. breath in →percuss (tympanic) • Tympany to tympany Palpate • Light palpation (1 hand) in all 4 quadrants o Notice any guarding, wincing, rigidity, tenderness • Deep palpation (2 hands) in all 4 quadrants o Note underlying structures/masses • Palpate lower edge of liver o Hold from back with one hand and the other on the edge o Under R costal margin, ask pt to breathe in o Soft, sharp, smooth, non-tender, no nodules • Palpate for splenomegaly o Reach L hand around to support/press L rib cage up, push R hand in toward costal margin o Ask pt. to take a deep breath, palpate for tip of spleen deep to the L costal margin o Normal spleen not palpable (the tip of the spleen) • Palpate for kidneys using “capture maneuver” o Stand on R, ask pt to inhale - put R hand above, L hand below to “capture” kidney o Ask patient to exhale/hold - slowly release R hand to feel kidney ▪ Note size, contour, tenderness o Palpate L kidney on L side o Palpate and estimate abdominal aorta (<3cm) o CVAT → ask pt. to sit upright o Tap with hand/fist at CVA margin bilaterally o Ask pt. if they feel any pain 7 MUSCULOSKELETAL Inspect • Inspect spine for alignment Palpate • Palpate spine for tenderness Range of Motion Test • Assess for asymmetry, erythema, heat, swelling, tenderness, masses, bogginess, crepitus, and limitations in ROM • DIP, PIP, MCP • Wrist, elbows, shoulders ACTIVE o For shoulder: elbow rests at side • Knee, hips, legs o Abduction, adduction ▪ Away/towards body o Internal rotation, external rotation, circumduction o Leg: internal, external, flexion o Ask pt to lie down now • Ankles o Inversion, eversion, plantar flexion, dorsal flexion • Toes o Wiggle o Abduct/adduct • Neck o L/R motion o Circumduction • Spine (while standing) o Lean back, lean forward, rotate side to side o Place hands between pt for support Muscle Strength Test • Assess muscle strength against resistance for shoulders, elbows, wrists, hand grips, fingers, hips, knees, ankles o Hints: ▪ Arms: parallel push/pull; genie up/down ▪ Hand: spread fingers & don’t let me close them; ▪ ▪ ▪ squeeze my fingers as hard as you can • Cross fingers here Hips: thighs push up Knees: shins push out, pull back Feet: push up, push down “Muscle strength graded at 5/5 conducted against resistance” Muscle Grading 5/5 = Good against resistance 4/5 = Less strength 3/5 = against gravity, not resistance 2/5 = contractions 1/5 = very limited 0/5 = flaccid 8 9 NEUROLOGICAL Mental Status: o A & O x 4 (person, place, time, situation) Cranial Nerves: o “CN 2 – 12 are intact” Motor: o “I am assessing for normal muscle bulk and tone” • ROM o “ROM is intact” • **Muscle strength** o Perform (listed on previous page) Sensory: • Spinothalamic tract o Perception of light touch o Cotton ball on diff. dermatomes ▪ 5 different points o Perception of pain (sharp/dull test) ▪ Show and state what a sharp and dull touch is o “The spinothalamic is intact” • Posterior column tract (BILATERALLY) o Vibratory sense ▪ Tuning fork on DIP of thumb and big toe ▪ Hit fork and then stop ▪ Ask pt. to close eyes & state when vibration stops o Proprioception ▪ Demo first. Tell me if thumb or big toe up/down ▪ Demonstrate what it looks like first ▪ Use hands on the outside of thumb of DIP ▪ Ask pt. to close eyes & state up or down o Graphesthesia ▪ Draw # in each hand – “3” or “8” ▪ Ask pt. what # was drawn o “The posterior column is intact” Deep Tendon Reflexes • Brachioradialis, biceps, triceps o Measure 2 inches using hammer o Hit your thumb & not pt. • Patellar, achilles, plantar o Ask pt. to lie down o Plantar: Use the back of the hammer to draw an “L” shape • “I am grading all reflexes at a 2+” Cerebellar Function • Coordination and skilled movements o Rapid alternating movements (patty cake, peddle bike, finger to thumb) o Finger to nose (3 areas each b/l, noting no tremors) ▪ Switch hands o Heel to shin • Romberg test (30 sec standing, eyes closed, & feet together) o Support hands o + exam = swaying • Pronator drift (30 sec standing, eyes closed, arms out) o Palms up o Over/under compensation (tap across both arms) • Evaluate gait and general posture o Ask pt. to walk 10 steps 10 11 changes to dullness over the liver with a skin pencil. 5. Measure the distance between upper and lower border of dullness in cm. Liver span depends on age, sex, and body type. The liver span is normally 6-12 cm (mean liver span is 7 cm for women and 10.5 cm for men). 6. If the liver span is increased, percuss laterally and medially. Normal liver span in the midsternal line is 4-8 cm. Spleen percussion • Liver Span percussion • Increased liver span on percussion indicates an enlarged liver, which can underlie a variety of pathological processes. It is essential to identify both the lower and the upper borders of the liver dullness to distinguish between an enlarged liver (which has an increased span), and a liver displaced downwards as a result of chronic obstructive pulmonary disease (in which case the liver span is normal). 1. Start by locating the right midclavicular line. Lightly percuss in the right midclavicular line upwards starting in the area of tympany below the umbilicus. Bending down to listen carefully to the percussion note might be required. 2. Make a mark where the tympany changes to dullness (lower border) with a skin pencil. 3. Percuss in the right midclavicular line downwards starting at the nipple line to identify an upper border of liver dullness. 4. Mark the point on the abdominal wall where the resonant sound over the lungs • • • The spleen is located slightly posterior to the left midaxillary line and produces an oval area of dullness between the 9th and 11th ribs. Only a small surface of a normal spleen is superficial enough to be detected, and the splenic dullness is often obscured by gastric or colonic tympany. However, an enlarged spleen is expanded towards the midline, anteriorly, and downward, and might be detected by two special percussion maneuvers: Traube's space percussion and/or Castell's maneuver. Percussion of Traube's space, anterior axillary line, and left costal margin. • Along with the other pathological conditions medial expansion of an enlarged spleen can produce dullness on percussion over Traube's space. • With the patient supine and their left arm slightly abducted, percuss from the medial to lateral border of Traube's space. Dullness on percussion or reduction of the area of tympany can result from splenomegaly. 12 Castell's method (checking for a splenic percussion sign). • Percuss in the anterior axillary line in the lower intercostal space. • Ask the patient to take a deep breath, and percuss again. A normal-sized spleen is positioned above the percussion point even when it descends during inspiration, and the percussion tone is tympanic on both expiration and inspiration. If percussion note is dull or becomes dull on inspiration (positive splenic percussion sign), splenomegaly is suspected Capture Maneuver-kidney palpation • • • • • Start with the right side and place one hand under the patient's right flank and the other hand at the right costal margin. Instruct patient to take a deep breath and at the height of inspiration press the fingers of both hands together to try to capture the kidney then have patient exhale and hold Slowly release the pressure and feel for the kidney to slide between your fingersit may not be palpable Try to capture the left kidney –the left kidney is less likely to be palpable If the kidneys are palpable they should be smooth firm and non-tender 13 Abbreviations & Definitions A & O = alert and oriented Apnea = temporary cessation of breathing Avg. = average b/l = bilaterally BV = bronchovesicular lung sounds CN = cranial nerve Crackles = rales, foil rubbing together, rattling sound CVAT = costal vertebral angle tenderness DIP = distal interphalangeal joint Dull = soft, muffled sound, organs Dyspnea = difficulty breathing EOMI = extra ocular movements intact Flat = soft, high-pitched sound, bone GI = gastrointestinal Heave = heart beating out of chest Hyperpnea = extremely deep breathing Hyperresonance = overinflated lung, lower-pitched Hyperventilation = extremely rapid breathing Hypoventilation = extremely slow breathing ICS = intercostal spaces Ident. = identity Kussmaul’s = marked increase in depth & rate LSB = left sternal boarder MCL = midclavicular line MSL = midsternal line mm = millimeters NAD = no acute distress NCAT = normocephalic – atraumatic Orthopnea = body must be upright to breathe Paradoxical = one lung deflates during inhalation PERRLA = pupils are equal, round, reactive to light & accommodation PIP = proximal interphalangeal joint PMI = point of maximum impulse Pt = patient Q = quadrants Rales = small clicking, bubbling Rhonchi = low-pitches snoring sound Resonance = normal breath sounds RR = respiratory rate RSB = right sternal boarder S1 = “lub” closing of AV tricuspid and mitral valve, dull & low-pitched S2 = “dub” closing SA pulmonic and aortic valve Stridor = high pitch wheezing Thrills = vibrations like cat purring TMJ = temporomandibular joint Tympani = loud, drum-like sound found in air-filled viscera V = vesicular lung sounds w/ = with Wheeze = high-pitched sound by narrow airway WNL = within normal limit y/o = years old # = Number & = and PULSES: Peripheral pulses should be compared for rate, rhythm & quality 0 +1 +2 +3 +4 Absent Weak & thready Normal Full Bounding EDEMA: Assess by placing thumb over dorsum of the foot or tibia for 5 seconds 0 +1 +2 No edema Barely discernible depression A deeper depression (<5mm) w/ normal foot & leg contours Deep depression (5-10mm) w/ foot & leg swelling Deeper depression (>1cm) w/ sever foot & leg swelling +3 +4