Assessing Lung Sounds
advertisement

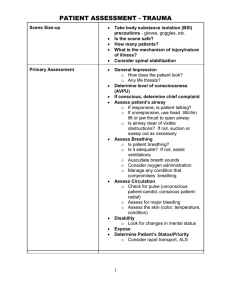
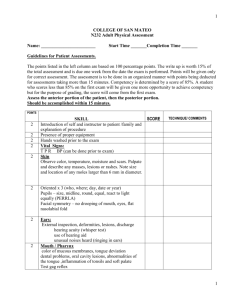
Assessing Lung Sounds (3) Normal Breath Sounds Bronchial breath sounds: loud, harsh and high pitched. Heard over the trachea, bronchi—between clavicles and midsternum, and over main bronchus. Bronchovesicular breath sounds: blowing sounds, moderate intensity and pitch. Heard over large airways, either side of sternum, at the Angle of Louis, and between scapulae. Vesicular breath sounds: soft breezy quality, low pitched. Heard over the peripheral lung area, heard best at the base of the lungs. Crackles ADVENTITIOUS LUNG SOUNDS Characteristics Popping, crackling, bubbling, moist sounds on inspiration Rhonchi Rumbling sound on expiration Pneumonia, emphysema, bronchitis, bronchiectasis High-pitched musical sound during both inspiration and expiration (louder) Emphysema, asthma, foreign bodies Wheezes Dry, grating sound on both inspiration and expiration Pleurisy, pneumonia, pleural infarct Sound Pleural Friction Rub Lung Problem Pneumonia, pulmonary edema, pulmonary fibrosis Assessing Heart Sounds These tones are produced by the closing of valves and are best heard over 5 points: 1.) Second intercostals space along the right sternal boarder. AORTIC AREA 2.) Second intercostals space at the left sternal boarder. PULMONIC AREA 3.) Third intercostals space at the left sternal boarder. ERB’S POINT 4.) Fifth intercostals space along the left sternal boarder. TRICUSPID AREA 5.) Fifth intercostals space, midclavicular line. MITRAL AREA—APEX This is where the Point of Maximal Impulse (PMI) is found—document location (note: with enlarged hearts mitral area may present at anterior axillary line) S1 (“lub”) the start of cardiac contraction called systole. Mitral and tricuspid valves are closing and vibration of the ventricle walls due to increased pressure. S2 (“dub”) end of ventricular systole and beginning of diastole. Aortic and pulmonic valves close. S3 (“Kentucky”) a ventricular gallop heard after S2. Normal in children and young adults, pregnancy, and highly trained athletes. In older adults it is heard in heart failure. Use bell of stethoscope and have pt in the left lateral position. S4 (“Tennessee”) atrial diastolic gallop. Resistance to ventricular filling and heard before S1. Heard in HTN and left ventricular hypertrophy. Listen at apex in left lateral position. Grading Murmurs Grade I Faint; heard with concentration Grade II Faint murmur heard immediately Grade III Moderately loud, not associated with thrill Grade IV Loud and may be associated with a thrill Grade V Very loud; associated with a thrill Grade VI Very loud; heard w/stethoscope off chest, associate w/a thrill Normal B/P for all <120/<80; Prehypertension 120-139/80-89 Guidelines and education site for adult B/P. http://www.nhlbi.nih.gov/hbp/index.html For children & adolescents: http://www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.htm EDEMA: Assess by placing thumb over dorsum of the foot or tibia for 5 seconds 0 No edema 1+ Barely discernible depression 2+ A deeper depression (< 5 mm) w/ normal foot & leg contours 3+ Deep depression (5-10 mm) w/ foot & leg swelling 4+ Deeper depression (> 1 cm) w/ severe foot and leg swelling Sawall RN, MS, MPH, CNS Health Assessment 2005 Note to students: the chart should be used as an organized reference guide and memory refresher and not substituted for assigned class work or a replacement for medical or nursing references. The chart should not be relied upon to provide any medical or nursing care. 1 5 P’s of Circulatory Checks Pain Pallor Paralysis Paresthesia Pulse PULSES: Peripheral pulses should be compared for rate, rhythm, and quality. 0 Absent +1 Weak and thready +2 Normal +3 Full +4 AGE Preemie Term NB 6 Months 1 yr 3 yrs 5 yrs 6 yrs 8 yrs 12 yrs 16 yrs Adult Female Adult Male Averages for Age Grouping WGT (kg) PULSE RESP 1-2 140 < 60 3 125 < 60 7 120 24-36 10 120 22-30 15 110 20-26 18 100 20-24 20 100 20-24 25 90 18-22 40 85-90 16-22 > 50 75-80 14-20 50-75 60-100 12-20 75-100 60-100 12-20 B/P (syst.) 50-60 70 90 ± 30 96 ± 30 100 ± 25 100 ± 20 100 ± 15 105 ± 15 115 ± 20 120 ± 20 90 + age 100 + age Formula to convert from Fahrenheit to Celsius: (5/9)*(deg F-32) to convert from Celsius to Fahrenheit: (1.8*deg C)+32 95º F = 35ºC 96ºF = 35.5ºC 98.6ºF = 37ºC 110ºF = 37.7ºC 101ºF = 38.3ºC 102ºF = 38.8ºC 103ºF = 39.4ºC 104ºF = 40ºC 105ºF = 40.5ºC Bounding P Q R S T Symptom Analysis: This assists the client in describing the problem. Provocate/Palliative: What caused it? What makes it better/worse? Quality/Quantity: How does it feel, sound, look, how much? Region/Radiation: Where is it and does it spread? Severity Scale: Rate on appropriate pain scale. Does it interfere with ADLs? Timing: When did it start? Sudden/gradual? How often? How long does it last? 4 Primary Assessment Techniques: INSPECT, PALPATE, PERCUSS, AUSCULATE What To Observe General appearance and behavior, posture, gait, hygiene, speech, mental status, height, weight, hearing and visual acuity, VS, nutritional status Head and Neck Skull size, shape, symmetry, hair & scalp, auscultate for carotid bruits, clenched jaws, puff cheeks, palpate TMJ, use cotton swab for facial sensations, test EOMs, cover/uncover test, corneal light reflex, Weber and Rinne test, use ophthalmoscope and otoscope, inspect and palpate teeth and gums, test rise of uvula, test gag reflex, test sense of smell and taste, inspect ROM neck, shrug shoulders, palpate all cervical lymph nodes, palpate trachea for symmetry, palpate thyroid gland Upper Extremities Inspect skin, blanche fingernails, palpate peripheral pulses, rate muscle strength, assess ROM, test deep tendon reflexes (DTRs) Posterior Thorax Inspect spine for alignment, assess anteroposterior to lateral diameter, assess thoracic expansion, palpate tactile fremitus, auscultate breath sounds Anterior Thorax Observe respirations. pattern, palpate respirations, excursion, auscultate breath sounds, auscultate heart sounds, inspect jugular veins, perform breast exam Abdomen Auscultate for bowel sounds, inspect, light and deep palpation, percuss for masses and tenderness, percuss the liver, palpate the kidneys, blunt percussion over CVA (posterior thorax) for tenderness Lower Extremities Inspect skin, palpate peripheral pulses, assess for Homan’s sign, inspect and palpate joints for swelling, assess for pedal and ankle edema, assess ROM General Neurologic Test stereognosis-object identification in hands, test graphesthesia-writing on body with closed pen, test two point discrimination, assess temp perception, inspect gait and balance, assess recent and remote memory, test cerebellar function by finger to nose test for upper extreme, and running each heel down opposite shin of lower extremity, test the Babinski reflex. Assessment Area General Survey Sawall RN, MS, MPH, CNS Health Assessment 2005 Note to students: the chart should be used as an organized reference guide and memory refresher and not substituted for assigned class work or a replacement for medical or nursing references. The chart should not be relied upon to provide any medical or nursing care. 2