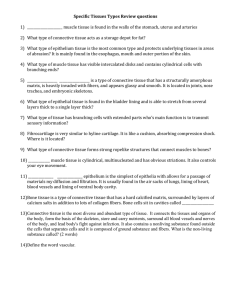
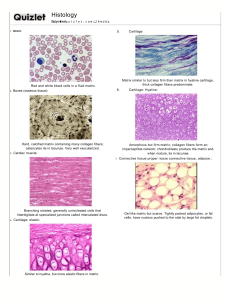
Which type of tissue makes up rings of the trachea A. Compact bone B. Spongy bone C. Hyaline cartilage D. Fibro cartilage E. Elastic cartilage 2. Match the following A. Elastic cartilage 1. Lies in lung tissue B. Fibrocartilage 2. Lies in trachea, bronchi C. Hyaline cartilage 3. Lies in pubic symphysis D. Elastic tissue 4. In external ear 2. Which type of tissue lines the pharynx A. Simple squamous epithelium B. Simple columnar epithelium C. Stratified squamous epithelium D. Ciliated pseudo stratified epithelium with goblet cells E. Both c and d Which type of cartilage is found in the larynx A. Hyaline cartilage B. Elastic cartilage C. Fibro cartilage D. Both a and b E. All the above 4. Which cell is a macrophage found in the skin A. Kupffer cells B. Histiocyte C. Dust cell D. Microglia E. Langerhans cell 5. Which type of fiber has a lot of mitochondria A. Red fibres B. White fibres C. Intermediate fiber D. All the above E. None of the above 6. Which of the following is an element of the central nervous system A. Receptors B. Brachial plexus C. Sciatic nerve D. Ganglia E. Spinal cord 7. During preparation of a routine h&e slide, what allows the tissue to be visualised A. Fixation B. Embedding in paraffin C. Staining D. Slicing E. Dehydration 8. During preparation of a routine h&e slide, how is the tissue preserved A. Fixation B. Embedding C. Staining D. Slicing E. Dehydration 9. Which organelle contains digestive enzymes A. Rough endoplasmic reticulum B. Smooth er C. Lysosome D. Golgi apparatus E. Mitochondria 10. Which cell is a mature bone cell A. Chondrocyte B. Chondroblast C. Osteoclast D. Osteocyte E. Bone lining cell 11. Which cell is a macrophage in the central nervous system A. Kupffer B. Histiocyte C. Dust cell D. Langhern cell E. Miccroglia 12. What do you call a space where the chondrocyte sits A. Space of disse B. Space of mall C. Vacuole D. Lacuna E. Howships lacuna 13. What is woven bone A. Cancellous bone B. Compact bone C. Dense bone D. Immature bone E. Spongy bone 14. Which of the following is a characteristic of cells in the epidermis A. Microvilli B. Stereo cilia C. Cilia D. Keratinisation E. Microvilli and stereocilia 15.during preparation of routine h &e slide, what allows the tissue to hold its form A.fixation B. Embedding C. Staining D. Slicing E. Dehydration 16. What is the cell body of a neurone called A. Ganglion B. Soma C. Astrocyte D. Nissl E. Terminal button 17.what are the basophilic clusters of ribosomes and rough er found in neurons called A. Ganglion B. Perikaryon C. Astrocyte D. Nissl E. Terminal button 18.which layer of the epidermis has cells which have keratohyaline granules A. Stratum basale B. Stratum spinosum C. Stratum granulosum D. Stratum lucidum E. Stratum corneum 19. Which type of tissue lines most of the gastro intestinal tract A. Simple squamous epithelium B. Simple cuboidal epthelium C. Simple columnar epithelium D. Stratified squamous epithelium E. Transitional epithelium 20. What percentage of matrix of cartilage is water A. 0 B. 10-40 C. 40-60 D. 60-80 E. 80-100 21. What are motor neurones A. Unipolar B. Pseudounipolar C. Bipolar D. Multipolar E. Unipolar and pseudo polar 22. What type of tissue makes up the adams apple A. Hyaline cartilage B. Fibrocartilage C. Elastic cartilage D. All the above E. None of the above 23. What type of muscle contains centrally placed nuclei A. Smooth muscle B. Cardiac muscle C. Skeletal muscle D. Smooth and cardiac E. All the above 24. Which fiber is seen in smooth muscle A. Red fibres B. White fibers C. Intermediate fibers D. All the above E. None of the above 25. Which microscope makes things appear three dimensional A. Simple microscope B. Compound microscope C. Phase contrast microscope D. Dissection microscope E. Transition electron microscope 26. What type of glands are the the ceruminous glands A. Sebaceous glands B. Eccrine glands C. Endocrine gland D. Apocrine gland E. Oil gland 27. What type of neuron is most abumdant A. Sensory neurone B. Motor neurone C. Relay neurone D. Interneurone E. All the above 28. What type of tissue is a tendon composed of A. Mucous connective tissue B. Mesenchyme C. Loose irregular connective tissue D. Dense irregular connective tissue E. Dense regular connective tissue 29. Hwat are neurones in the retina A. Unipolar B. Bipolar C. Pseudounipolar D. Multipolar E. Unipolar and pseudounipolar 30.what are the small tunnels seen in bone A. A. Canaliculi B. Sharpey’s fibers C. Trabeculae C. Tone’s process E. Lacuna 31. Which cell is the most abundant cell in the epidermis A. Langerhan cell B. Keratinocyte C. Melanocyte D. Merkel cell E. Fibroblast 32.what type of neurone is multipolar A. Motor neurons B. Interneurones C. Sensory neurones D. Motor neurones and interneurones E. All the above 33. Which cell is a resting osteoclast A. Chondrocyte B. Osteocyte C. Chondroblast D. Osteoclast E. Bone lining cell 34. What type of tissue lines the upper oesophagus A. Simple squamous epithelium B. Simple cuboidal epithelium C. Simple columnar epithelium D. Stratified squamous epithelium E. Transitional epithelium 35. Which of the following is not considered neuroglia A. Astrocytes B. Ependymal cells C. Oligodendrocytes D. Microglia E. Schwann cells 36. Which of the following is not primarily composed of connective tissue A. Spinal cord B. Pubic symphysis C. Ligament D. Areolar tissue E. Organ capsule 37. Connexins are the proteins found in which plasma membrane specialisation A. Desmosomes B. Gap junctions C. Microvilli D. Tight junctions 38. This type of tissue lines the nasal cavity, trachea and bronchi A. Transitional epithelium B. Pseudostratified ciliated columnar epithelium C. Stratified squamous epithelium D.. Stratified columnar epithelium 39. Of the extracellular matrices in these tissues, which of the following is most likely to have collagen type 11 A. Bone B. Fibrocartilage C. Dense irregular connective tissue D. Dense regular connective tissue E. Hyaline cartilage 40. Cement lines are regularly found in A. Cancellous bone B. Osteonal bone C. Trabecular bone D. Immature bone E. None of the above 41. Among the defensive cells of connective tissue, the one that forms antibodies and provides humoral immunity is A. T lymphocyte B. Plasma cells C. Mast cell D. Histiocyte E. None of the above 42. Within the extracellular matrix of connective tissues, this structure consists of small fibres that normally remain unbundled and rorms a useful environment for cells of defense A. Collagen type 1 B. Collagen type 11 C. Collagen type 111 D. Collagen type four E. Elastic fiber 43. The structure described in the previous question mostly occurs in A. Loose connective tissue B. Dense irregular connective tissue C. Dense regular connective tissue D. Cartilage E. Bone 44. Which of the following comes under loose connective tissue A. Areolar tissue B. Adipose tissue C. Reticular tissue D. All the above 45.where is blood liquid tissue usually found A. Chambers of the heart B. Tracha C. Papillary region D. Lymphatic vessels 46. What is the major vfunction of dense irregular connective tissue A. Protection B. Support C. Strong attachment D. None of th above 47. Which of the following statements is not triue A. Adipocytes store triglycerides B. Unctions of bone tissue include protection,support, storage C. Hyaline cartilage lines the external ear D. Extracellular matrix of bone is hard and brittle EN | DE | PT | ES Get help How to study Login Register ANATOMY HISTOLOGY RADIOLOGICAL ANATOMY Search... HistologyGeneralConnective tissue Connective tissue Characteristics Location Cellular component Extracellular matrix Clinical considerations Fibrosis and scarring Carcinoma staging Register now and grab your free ultimate anatomy study guide! Loose connective tissue: want to learn more about it? Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster. What do you prefer to learn with? VIDEOS QUIZZES BOTH “I would honestly say that Kenhub cut my study time in half.” – Read more. Kim BengocheaKim Bengochea, Regis University, Denver Loose connective tissue Author: Adrian Rad BSc (Hons) • Reviewer: Catarina Chaves MD Last reviewed: June 03, 2021 Reading time: 17 minutes Loose connective tissue (Textus connectivus laxus); Image: Loose connective tissue Textus connectivus laxus 1/3 The human body has several types of tissues, a specific one being connective tissue. Situated virtually at every site, both internally and externally, it is crucial for providing strength, elasticity and metabolic support for all other tissues. You can imagine it as a scaffold supporting surrounding structures and the cells which constantly try to maintain homeostasis. In order to perform its function, connective tissue has certain distinct components, such as cells and fibers. The proportions and organizations of the fibers result in several types of connective tissues, one being loose connective tissue. Key facts Category Connective tissue proper Cellular components Resident cells: - fibroblasts - synthesize the components of the extracellular matrix - macrophages - inborn immunity cells that protect the tissue by fagocyting potential pathogenes - mast cells - adaptive immunity cells that mediate wound healing process and alergic reactions - adipocytes - specialized cells that accumulate fat (energy resevoar) - mesenchymal stem cells - stem cells that give rise to fibroblasts and new blood vessels Transient cells: - immune cells: neutrophils, eosinophils, basophils, monocytes, plasma cells, lymphocytes Extracellular matrix components Ground substance - viscous gel with high water content; consists of proteoglycans and glycoproteins Reticular fibers - fibers comprised of collagen type I that give the mechanical strength to the tissue (later the collagen type I is replaced by collagen type III) Elastic fibers - fibers responsible for the flexibility of the tissue Location Dermis, lamina propria of the digestive and respiratory tracts, mucous membranes of reproductive and urinary tracts, glandular stroma, mesentery Clinical relations Fibrosis, scarring, keloids, carcinoma staging This article will first describe some general aspects of connective tissue and then it will zoom into the key components of loose or areolar connective tissue. Contents Connective tissue Components Classification Characteristics Location Cellular component Fibroblasts Macrophages Mast cells Adipocytes Mesenchymal stem cells Extracellular matrix Ground substance Reticular fibers Elastic fibers Clinical considerations Fibrosis and scarring Carcinoma staging + Show all Recommended video: Loose connective tissue Structure and cellular components of loose connective tissue. Connective tissue Components Connective (supporting) tissue is a voluminous, strong, yet elastic type of tissue with significant roles in the human body. It provides mechanical strength, together with physical and metabolic support to all the other types of tissues. You can think of it as a mesh-like matrix that physically connects other tissues between them. This extracellular matrix (ECM) is responsible for the physical properties of connective tissue and it is a major constituent of this tissue type. The ECM is a mixture of protein fibers and ground substance. The protein fibers, these being collagen and elastin, are responsible for providing connective tissue with tensile strength and elasticity, respectively. The ground substance is a wet gel that permits the exchange of nutrients and wastes between cells and the blood. It is composed of glycoproteins and complex carbohydrates. In addition to the ECM, connective tissue also has a cellular component. The cells can be separated into two groups, resident and transient. Resident cells, such as fibroblasts, myofibroblasts, adipocytes and certain immune cells are always present in connective tissue. Their main roles is to secrete, maintain, recycle, repair and protect the ECM and surrounding tissue structures. Wondering how you're going to consolidate your knowledge? Look no further than our connective tissue quizzes and free labeling worksheets. Transient cells are those that can migrate to the connective tissue in response to specific stimuli, such as tissue injury and inflammation. They circulate via blood and lymphatic vessels, which enrich all connective tissue, except cartilage. They are mostly immune cells, such as neutrophils, eosinophils, basophils, monocytes, plasma cells, and lymphocytes. All cells, resident and transient, perform their functions inside the ECM component of connective tissue. Classification Connective tissue is classified according to the composition and organization of the ECM and cellular components, as follows: Classification of the connective tissue Embryonic connective tissue Mesenchyme Muscous connective tissue Connective tissue proper Loose connective tissue Dense connective tissue (regular and irregular) Specialized connective tissues Cartilage Bone Adipose Blood For more details about connective tissue, take a look at the following study unit: Cells and tissues Cells and tissues Explore study unit Characteristics Loose connective tissue (LCT), also called areolar tissue, belongs to the category of connective tissue proper. Its cellular content is highly abundant and varied. The ECM is composed of a moderate amount of ground substance and two main types of protein fibers: elastic and reticular fibers. The ground substance occupies a high volume in comparison to the fibers. It plays a significant role in the diffusion of gases, nutrients and metabolic wastes between the cells and the vessels that perfuse the tissue. Out of the types of fibers, the reticular ones predominate, but they are thin and loosely arranged. All of these characteristics give LCT a delicate and flexible consistency that is not very resistant to stress. Location Dermis; Image: Dermis 1/4 Synonyms: Corium The areolar tissue is found beneath the dermis layer and is also underneath the epithelial tissue of all the body systems that have external openings. It is also a component of the lamina propria of the digestive and respiratory tracts, the mucous membranes of reproductive and urinary system, the stroma of glands, and the hypodermis of the skin. It is also found in the mesentery which is surrounding the intestine. Due to its position, LCT is a major site of inflammatory and immune reactions. This is where potential pathogens that have breached the skin are challenged and hopefully destroyed by the immune system. LCT is also well-vascularized to facilitate effective immune cell migration. Cellular component Fibroblasts Fibroblast (Fibroblastus); Image: Fibroblast Fibroblastus 1/3 Fibroblasts are the most numerous cell type in LCT. They synthesize both types of fibers and the complex carbohydrates of the ground substance. Usually, only the nuclei are visible after hematoxylin and eosin (H&E) staining, which appear condensed, elongated and disclike. The nucleolus can be evident sometimes. The cytoplasm is composed of thin, pale-staining and flattened processes extending into the matrix. Fibroblasts reside close to collagen fibers, resulting in an inability to clearly distinguish the cytoplasm. During periods of wound repair or active growth, fibroblasts become activated and produce ECM. Their nuclei are large with a prominent nucleolus. The cytoplasm is more extensive, displays basophilia due to increased amounts of rough endoplasmic reticulum (rER) and a prominent Golgi apparatus. Myofibroblasts are a specific type of activated fibroblasts associated with tissue repair. In addition to the typical characteristics of activated fibroblasts described above, they also exhibit characteristics of smooth muscle cells upon examination with a transmission electron microscope (TEM). Such characteristics include bundles of longitudinal actin filaments and dense bodies within the cytoplasm. The nucleus also appears to be undulated. The cytoplasmic processes of different myofibroblasts can contact each other. These contact points contain gap junctions for intercellular communication. The smooth muscle cell characteristics permit the myofibroblasts to anchor the ECM, strengthen it and transmit their contractions throughout the ECM during wound contraction. Macrophages T issue-resident macrophages (histiocytes) are derived from monocytes that mature after migrating into connective tissue. Transient macrophages enter connective tissue in response to tissue injury and inflammation. Macrophages are phagocytes and they protect the LCT by ingesting potential pathogens and cell debris. Subsequently, they can activate the adaptive immune system by releasing cytokines and presenting antigens, if required. Monocyte; Image: Monocyte 1/4 In light microscopy, they are usually identified by the presence of ingested material within the cytoplasm following phagocytosis. Their nucleus is kidney shaped. Lysosomes are abundant and can be identified using a stain for acid phosphatase activity. The ultrastructure of macrophages, as seen with TEM, displays additional characteristics. The cytoplasmic surface is folded and has many finger like projections called pseudopodia. The heterochromatin is clumped around the nuclear envelope. Other apparent components are endocytic vesicles, phagolysosomes, residual bodies, ER and the Golgi apparatus. Mast cells Mast cell (Mastocytus); Image: Mast cell Mastocytus 1/2 Mast cells arise from hematopoietic stem cells in the bone marrow. They travel as agranular and immature cells through the peripheral circulation. They mature upon entering connective tissue and develop their characteristic granules. High affinity Fc receptors are expressed on their surface to which IgE antibodies bind and aggregate. This triggers mast cell degranulation, which involves exocytosis of granule content such as histamines, serine proteases, chemoattractants, leukotrienes and interleukins. These vasoactive mediators are important in mounting an immune response, but they can also cause the typical symptoms of allergic reactions. Mast cells are distributed in the connective tissue throughout the body, with the exception of the brain and spinal cord. They appear as large and ovoid, with a spherical nucleus. The cytoplasm is filled with basophilic granules, together with small amounts of rER, mitochondria and Golgi apparatus. The granules become apparent after staining with basic dyes, such as toluidine blue, following glutaraldehyde fixation. The granules appear membrane bound in TEM. Adipocytes Brown adipose tissue (Textus adiposus fuscus); Image: Brown adipose tissue Textus adiposus fuscus 1/2 Adipocytes are specialized cells that gradually accumulate fat, in the form of triglycerides, within their cytoplasm. They are residents throughout LCT, either in isolation or in small clusters. Whenever they accumulate in large numbers, they form a specialised type of connective tissue, called adipose tissue. The stored fat is a significant energy store. These cells also have an endocrine role by regulating energy metabolism. Adipose tissue can be of two types: brown and white. Brown adipose tissue is present during fetal life but diminishes in the first 10 years of life. White adipose tissue (WAT) is the predominant one in adults. It forms a layer called subcutaneous tissue within the LCT. Externally, this subcutaneous layer is located underneath the skin and thermally insulates the body. Internally, it is located around organs and peritoneal structures. Adipocyte (Adipocytus); Image: Adipocyte Adipocytus 1/3 Synonyms: Fat cell Adipocytes are large and usually spherical cells containing a single and large lipid droplet in the centre of the cytoplasm. This lipid mass compresses the nucleus, flattens it and displaces it to one side, giving it a signet-ring appearance when stained with H&E. The cytoplasm is reduced to a small rim around the periphery. Adipose tissue appears as a mesh of paled stained polygons connected by thin strands of cytoplasm and ECM. Blood vessels are apparent in “islands” where several adipocytes meet. Adipocytes are also surrounded by reticular fibers. The ultrastructure of these cells reveals the presence of vimentin filaments in the portion between the contained lipid and surrounding cytoplasm. In addition, the perinuclear cytoplasm contains a small Golgi apparatus. The smooth ER is also abundant and prominent in comparison to rough ER, especially within a thin rim of cytoplasm surrounding the lipid droplet. Mesenchymal stem cells A specific type of adult stem cells are located in LCT, called mesenchymal stem cells (MSCs). They are lineage specific cells and occupy specific sites, called niches. They give rise to fibroblasts and new blood vessels. If you are curious to find out even more information about loose connective tissue, take a look below: Loose connective tissue Loose connective tissue Explore study unit Extracellular matrix Ground substance Ground substance is a clear and viscous gel with a high water content. In routine H&E staining the ground substance is not visible because it is lost during the preparation procedure. It appears as a virtually empty background filled with cells and fibers. Ground substance occupies the greatest proportion in LCT, being responsible for the flexible consistency of this tissue type. It consists of proteoglycans, which are composed of complex carbohydrates called glycosaminoglycan molecules (GAGs) and glycoproteins. GAGs are long and unbranched polysaccharide chains composed of repeating disaccharide units. Each unit contains a uronic acid and either a glucose or galactose derivative. GAGs attract many water molecules due to their highly negatively charged nature, giving the ground substance a gel like consistency. There are seven types of GAGs in total, the most predominant one being hyaluronate (hyaluronic acid). It is also the longest, being composed of thousands of sugars. Hyaluronate is important in the assembly of proteoglycan aggregates, which provides turgidity to LCT and makes it an excellent shock absorber. Glycoproteins form a smaller but important part of the ground substance. They help stabilize the ECM by binding ECM proteins like GAGs, collagens and proteoglycans. They also help in linking the ECM to the surface of cells. The two most important glycoproteins in LCT are fibronectin (the most abundant) and fibrillin. Fibronectin controls the deposition and orientation of collagen fibers in the ECM. To do this, they bind to collagen itself, GAGs like heparan sulfate and cell membrane receptors, such as integrins. Fibrillin is required for the deposition of elastin fibers, ultimately becoming incorporated within the fibers themselves and around them. Ground substance - histological slide Ground substance - histological slide Reticular fibers Reticular fibers; Image: Reticular fibers 1/3 Synonyms: Reticular fibres Reticular fibers are the most common type of fibers in LCT. They actually consist of collagen fibrils, which are composed of type III collagen. The building block of these collagen fibrils are tropocollagen monomers, which are secreted by fibroblasts. Each monomer consists of three polypeptide chains, called alpha chains, bound into a helical protein. They polymerise longitudinally and transversely in the ECM, forming collagen fibrils. The collagen fibrils constituting reticular fibers are narrower, do not bundle into thick fibers, are more branched and contain more sugar groups in comparison to the typical type I collagen. The fibers form a delicate and branched mesh that supports the resident cells of LCT and provide early mechanical strength. As a result, these networks are primarily located at sites of wound healing and scar tissue formation, where new ECM is synthesized by fibroblasts. At the end of the process, they are replaced by stronger type I collagen fibers. Reticular fibers can be made visible by the periodic-acid Schiff reaction or silver staining procedures, giving them a black and threadlike appearance. Elastic fibers Elastic fibers; Image: Elastic fibers 1/3 Synonyms: Elastic fibres The flexibility of LCT is also due to elastic fibers, not just due to the high content of ground substance. They are thin structures that are arranged in a branching pattern to form a 3D network within the ECM. They are interwoven with collagen fibers to prevent tearing from excessive stretching. The building blocks of elastic fibers is elastin, the precursor of which is tropoelastin, which is synthesized by fibroblasts. The enzyme lysyl hydroxylase polymerises the monomers within the ECM. Formation of elastic fibers results from deposition of elastin on fibrillin glycoproteins, resulting in fibrillin being incorporated in the final version of the fibers. Such fibers are present in high amounts within structures that frequently adjust their shape, such as blood vessels walls, lungs, skin and urinary bladder. Elastic fibers appear as delicate threads within the ECM. They are stained by eosin, although not readily, so they cannot be easily distinguished from collagen fibers. However, they have a degree of refractility, which can facilitate their recognition. Alternatively, they can be stained specifically using dyes like orcein or resorcinfuchsin. Pelvis Different types of loose connective tissue and related structures (20 structures). START QUIZ 60 Basic structure identification questions 19 Advanced structure identification questions 15 Exam questions (Question bank) Clinical considerations Fibrosis and scarring Following cellular and tissue damage, an inflammatory reaction ensues that eliminates the damaging agent and clears away the dead tissue. Further repair begins with proliferation and differentiation of mesenchymal cells from the periphery of normal tissue into fibroblasts and myofibroblasts. These cells enter the damaged area, in which growth of new capillary blood vessels has also begun. The fibroblasts and myofibroblasts begin secreting new ECM, filling the damaged area with fibro-collagenous material. Over time, remodelling takes place to maximise collagen strength and reduce the numbers of capillary vessels. This process can result in normal functioning, but more often than not, the tissue is not completely restored. Carcinoma staging Carcinoma is a type of cancer originating from the epithelium. Since the epithelium is such a predominant human body tissue, both internally and externally, there are quite a number of carcinoma types, which can affect various organs. As you have seen, underneath the epithelium is the lamina propria, which is the classic example of LCT. The extent of invasion of the lamina propria is a feature used to determine the stage and prognosis of several carcinoma types. For example, urogenital cancer is considered noninvasive until the tumor has completely penetrated the lamina propria (CIS, Ta, T1 stages). Once the cells have passed the lamina propria, the cancer is considered invasive (T2 and beyond). Similar classifications are carried out for gastric and colon cancers, using the lamina propria as a reference point. Loose connective tissue: want to learn more about it? Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster. What do you prefer to learn with? VIDEOS QUIZZES BOTH “I would honestly say that Kenhub cut my study time in half.” – Read more. Kim BengocheaKim Bengochea, Regis University, Denver Freie Universität BerlinDemocritus University of ThraceHochschule Fresenius University of Applied SciencesUniversity of Colorado Denver | Anschutz Medical Campus INFO Pricing License illustrations ABOUT US Team Partners Jobs Contact Imprint Terms Privacy ANATOMY Basics Upper extremity Lower extremity Spine and back Thorax Abdomen and pelvis Head and neck Neuroanatomy Cross sections HISTOLOGY General Systems Fetal tissues RADIOLOGICAL ANATOMY Head and neck Abdomen and pelvis Upper extremity Lower extremity Thorax HOW TO STUDY Anatomy learning strategies Free eBook Labeling diagrams Benefits of Kenhub Success stories KENHUB IN ... German Spanish Portuguese Russian OUR QUALITY COMMITMENT Our quality commitment Grounded on academic literature and research, validated by experts, and trusted by more than 1 million users. Read more. Copyright © 2021 Kenhub. All rights reserved.