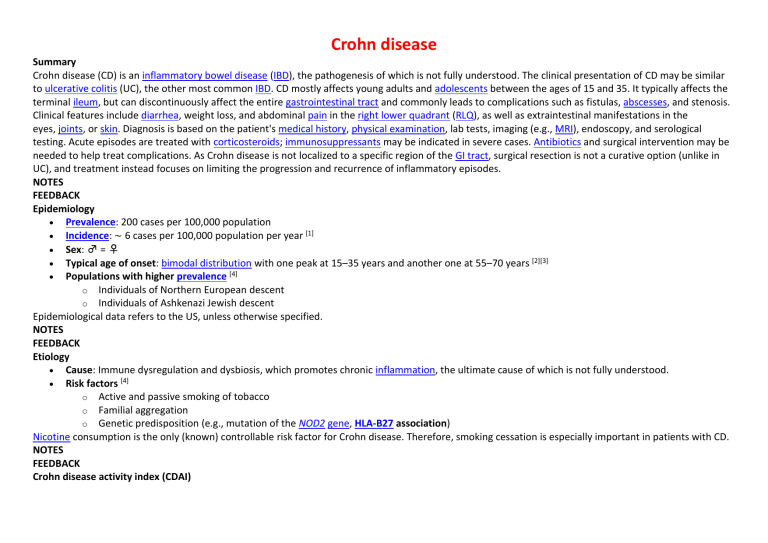
Crohn disease Summary Crohn disease (CD) is an inflammatory bowel disease (IBD), the pathogenesis of which is not fully understood. The clinical presentation of CD may be similar to ulcerative colitis (UC), the other most common IBD. CD mostly affects young adults and adolescents between the ages of 15 and 35. It typically affects the terminal ileum, but can discontinuously affect the entire gastrointestinal tract and commonly leads to complications such as fistulas, abscesses, and stenosis. Clinical features include diarrhea, weight loss, and abdominal pain in the right lower quadrant (RLQ), as well as extraintestinal manifestations in the eyes, joints, or skin. Diagnosis is based on the patient's medical history, physical examination, lab tests, imaging (e.g., MRI), endoscopy, and serological testing. Acute episodes are treated with corticosteroids; immunosuppressants may be indicated in severe cases. Antibiotics and surgical intervention may be needed to help treat complications. As Crohn disease is not localized to a specific region of the GI tract, surgical resection is not a curative option (unlike in UC), and treatment instead focuses on limiting the progression and recurrence of inflammatory episodes. NOTES FEEDBACK Epidemiology Prevalence: 200 cases per 100,000 population Incidence: ∼ 6 cases per 100,000 population per year [1] Sex: ♂ = ♀ Typical age of onset: bimodal distribution with one peak at 15–35 years and another one at 55–70 years [2][3] Populations with higher prevalence [4] o Individuals of Northern European descent o Individuals of Ashkenazi Jewish descent Epidemiological data refers to the US, unless otherwise specified. NOTES FEEDBACK Etiology Cause: Immune dysregulation and dysbiosis, which promotes chronic inflammation, the ultimate cause of which is not fully understood. Risk factors [4] o Active and passive smoking of tobacco o Familial aggregation o Genetic predisposition (e.g., mutation of the NOD2 gene, HLA-B27 association) Nicotine consumption is the only (known) controllable risk factor for Crohn disease. Therefore, smoking cessation is especially important in patients with CD. NOTES FEEDBACK Crohn disease activity index (CDAI) Definition: A validated score used to assess disease activity in Crohn disease calculated using the following variables, assessed over the course of one week: o Number of liquid or soft stools per day o Severity of abdominal pain o General condition o Presence of the following Arthritis/arthralgia Iritis/uveitis Erythema nodosum, pyoderma gangrenosum, or aphthous ulcers Anal fissures, fistulas, or abscesses Other fistulas Fever o Use of antidiarrheal drugs o Abdominal masses o Hematocrit o Percentage above or below standard weight Interpretation o 0–149: asymptomatic remission o 150–220: low to moderate activity o 221–450: moderate to high activity o 451–1100: high activity, fulminant disease NOTES FEEDBACK Pathophysiology Inflammation Inflammation is most likely caused by immune dysregulation. Dysregulation of IL-23-Th17 signaling → unrestrained Th17 cell function → inflammation → local tissue damage (edema, erosions/ulcers, necrosis) → obstruction, fibrotic scarring, stricture, and strangulation of the bowel [5] There is evidence that mutations in the nucleotide oligomerization binding domain 2 (NOD2) protein are involved in the development of Crohn disease, but the exact mechanism is not fully understood. [5] o Loss of function mutations in NOD2 → ↑ susceptibility for bacterial invasion of the intestinal mucosa → unregulated inflammation o Dysfunctional NOD2 → overactivity of NF-κB signaling pathway → ↑ production of proinflammatory cytokines and antimicrobial peptides → chronic autoinflammation Abscess and fistula formation Intestinal aphthous ulcers → transmural fissures and inflammation of the intestinal walls → adherence of other organs or the skin → penetration → microperforation and abscess formation → macroperforation into these structures → fistula formation NOTES FEEDBACK Clinical features CD typically occurs episodically with a 30%-risk of recurring inflammation over the span of one year. If symptoms persist for six months, the disease is considered chronic. Without treatment, relapses and complications are to be expected. Constitutional symptoms [6] Low-grade fever Weight loss Fatigue Intestinal symptoms [6] CD most commonly affects the terminal ileum and colon, but involvement of any part of the GI tract (from mouth to anus, except rectum) is possible. Chronic diarrhea, typically nonbloody Abdominal pain, typically in the RLQ Malabsorption (see “Signs of malabsorption” in “Complications” below) Palpable abdominal mass in the RLQ Enterocutaneous perianal fistulas, often associated with abscess formation [7] Oral aphthae Perianal fistulas and abscesses are often the first signs of Crohn disease. Extraintestinal symptoms [8] Joints: enteropathic arthritis (e.g., sacroiliitis, spondylitis, inflammation of peripheral joints) Eyes o Uveitis o Iritis o Episcleritis Liver/bile ducts: cholelithiasis Urogenital system: urolithiasis (mostly calcium oxalate stones) Skin o Erythema nodosum o Acrodermatitis enteropathica o Pyoderma gangrenosum Associated with various conditions (e.g., IBD, rheumatoid arthritis, and trauma) Manifests with very painful, rapidly-progressive, red spots that can change into purulent pustules or deep ulcerated lesions with central necrosis Commonly located at extensor side of the lower limbs Treated with immunosuppressants (e.g., corticosteroids, cyclosporine A) o Pyostomatitis vegetans NOTES FEEDBACK Diagnostics Approach Diagnosing CD requires the integration of clinical presentation, laboratory tests, and endoscopic, histologic, pathologic and radiologic findings. 1. If a patient presents with symptoms suggestive of CD, conduct blood tests and stool tests (see “Laboratory tests” below) to rule out other possible causes for bowel inflammation/GI symptoms. [9] 2. Confirm diagnosis with endoscopy and/or radiographic imaging and/or biopsy. 3. Perform contrast radiological studies and/or ultrasonography to assess extent, severity, and complications (e.g., abscesses, fistulas, and stenoses) Laboratory tests Blood [9] Blood work o Complete blood count may show signs of pernicious anemia o ↑ Inflammatory markers (↑ CRP, ↑ ESR, ↑ thrombocytes, and ↑ leukocytes) Serology: routine use to establish diagnosis is not recommended due to low sensitivity [10] o o ↑ Anti-Saccharomyces cerevisiae antibodies (ASCA) pANCA most likely negative Stool Stool analysis o Stool culture to rule out bacterial gastroenteritis o Microscopy to examine presence of worm larvae or eggs (ova and parasites) o Identification of bacterial toxins (e.g., toxin of Clostridium difficile) o Detection of fecal calprotectin and/or fecal lactoferrin [11][12] Proteins associated with neutrophils that can be used as a diagnostic tool for inflammatory bowel disease Direct correlation between detected amount of proteins and severity of intestinal inflammation Fecal occult blood test (FOBT) Imaging [13][14] Plain x-ray abdomen: may show bowel distention or pneumoperitoneum Upper GI series with barium swallow and small bowel follow-through (enteroclysis): used to detect fistulas or stenoses, characteristic findings are: o Procedure Water-soluble contrast medium is inserted into the small intestine via a nasopharyngeal tube. Multiple x-rays are taken in a chronological sequence to evaluate each section. o Findings String sign: contrast-filled bowel segment that resembles a string on x-ray Creeping fat: pathognomonic hyperplasia of adipose tissue that results in accumulation of mesenteric fat around the circumference of the intestine [15] May cover more than 50% of the inflamed bowel Correlates with severity of transmural inflammation Ultrasound findings o Gastrointestinal wall thickening caused by inflammation and edema o Possible detection of abscesses/fistulas MR enterography: noninvasive, highly sensitive and specific imaging technique that involves the visualization of an oral contrast medium on MRI and is used in the diagnosis of IBD. o Used to assess the extent and pattern of intestinal inflammation, detect perianal and pelvic disease, and to predict disease activity o Characteristic findings are an edematous thickening of the intestinal wall and enlarged lymph nodes. o Can be done as invasive MRI enteroclysis, during which contrast medium is applied via nasoduodenal tube and the small bowel is distended via an electric infusion pump. Endoscopy [16] Endoscopy confirms the diagnosis, assesses the extent of the disease, differentiates CD from other diseases (e.g., ulcerative colitis, peptic ulcers, etc.), and may also be used as a therapeutic tool (e.g., dilatation of ducts, intestinal loops). Ileocolonoscopy: endoscopic examination of the rectum, colon, and terminal ileum that allows for direct visualization of the intestinal mucosa and sampling of tissue o Procedure: ileocolonoscopy with biopsies at various locations throughout the terminal ileum, colon, and rectum o Characteristic macroscopic findings Segmental/discontinuous pattern of involvement Snail trails: longitudinal ulcerations Pinpoint lesions: small, aphthous hemorrhagic mucosal defects Cobblestone sign: inflamed sections followed by deep ulcerations that resemble cobblestones Erythema and transmural inflammation (all mucosal layers of the intestinal wall are involved) Fissures, fistulas Esophagogastroduodenoscopy o Used to evaluate for involvement of the esophagus, stomach, and duodenum o Findings include aphthae on mucosa Video capsule endoscopy [13] o Used to evaluate small bowel morphology as an adjunctive to regular endoscopy o Should be performed prior to regular endoscopy in suspected small bowel obstruction NOTES FEEDBACK Pathology Skip lesions: a pattern of patchy, discontinuous inflammation in the bowel (affected areas interspersed with normal tissue) Creeping fat Hypertrophic lymph nodes Transmural inflammation o Noncaseating granulomas [17] o o Giant cells Distinct lymphoid aggregates of the lamina propria NOTES FEEDBACK Differential diagnoses MAXIMIZE TABLETABLE QUIZ Crohn disease and ulcerative colitis Symptoms Crohn disease Ulcerative colitis Pathophysiology Mediated by dysfunctional IL-23-Th17 signaling Mediated by Th2 cells Frequency/type of defecation Increased Typically nonbloody, watery diarrhea May be bloody in more severe cases Greatly increased Bloody diarrhea with mucus Tenesmus Urgency Nutritional status Poor or malnourished Mostly normal, but weight loss and malnutrition may occur in severe disease Painful defecation, pain located in LLQ Abdominal cramps and tenderness [18] Physical examination Mostly constant pain in RLQ Palpable abdominal mass Crohn disease and ulcerative colitis Symptoms Extraintestinal manifestations Crohn disease Ulcerative colitis Low-grade fever Nephrolithiasis (e.g., calcium oxalate) Cholelithiasis Skin o o Tachycardia Orthostatic hypotension Primary sclerosing cholangitis Pyoderma gangrenosum Erythema nodosum Eyes Uveitis Episcleritis Mouth: aphthous stomatitis Joints o Peripheral arthritis o Spondylitis Fistulas Common (to skin, bladder, or in between loops) May cause pneumaturia and/or recurrent UTIs Rare Other complications Abscess Strictures (obstructions) Perianal fissures Fulminant colitis Toxic megacolon Perforation Increased due to underlying pathology Increased secondary to immunosuppression Small intestine Colon Non-Hodgkin lymphoma Cholangiocarcinoma Colorectal cancer Cancer risk o o [19] Crohn disease and ulcerative colitis Symptoms Crohn disease Ulcerative colitis ASCA p-ANCA Colon (exception: backwash ileitis) Typical location: terminal ileum and colon with rectal sparing May affect the entire GI tract Pattern of inflammation Discontinuous (skip lesions) Continuous Typical diagnostic findings Cobblestone sign Pinpoint lesions Snail trails Creeping fat String sign Friable mucosa Mucosal ulcerations can be deep or superficial Crypt abscesses Loss of haustra (lead pipe sign) Transmural inflammation Noncaseating granulomas Giant cells Lymphoid aggregates Confined to mucosa and submucosa No granulomas Neutrophilic inflammation of the crypts Corticosteroids Thiopurine analogs (azathioprine, 6-mercaptopurine) Anti-p40 antibodies (e.g., ustekinumab) 5-aminosalicylic acid (e.g., mesalamine) 6-mercaptopurine Calcineurin inhibitors (e.g., cyclosporine, tacrolimus) Antibodies Endoscopy and imaging Location Histology Treatment Medication Crohn disease and ulcerative colitis Symptoms Crohn disease Surgery Ulcerative colitis Alpha 4 integrase inhibitors (e.g., natalizumab, vedolizumab) Possibly antibiotics outside of an acute episode (e.g., ciprofloxacin, metronidazole) Biologics (e.g., infliximab, adalimumab) Noncurative surgery may become necessary to alleviate symptoms Curative surgery possible (proctocolectomy) To remember the most important features of Crohn disease (creeping fat, granuloma, skip lesions, rectal sparing, cobblestone sign), think: The crone and the fat granny skipped over the wrecked cobblestones. Other differential diagnoses Acute appendicitis Infectious gastroenteritis/colitis Noninfectious colitis (ischemic, after radiation therapy, after ingestion of drugs, etc.) Diverticulitis Irritable bowel syndrome Gastrointestinal tuberculosis Malignant intestinal transformations The differential diagnoses listed here are not exhaustive. NOTES FEEDBACK Treatment Approach [13] Therapy of CD is based on the following steps: 1. Treating acute disease 2. Inducing clinical remission 3. Maintaining response/remission Patients should be stratified according to their specific prognostic risk factors. For optimal results, therapy should be as individually tailored as possible. Disease activity should be monitored regularly based on objective markers. Patients should be motivated to engage in lifestyle modifications (see below). Pharmacotherapy Treatment of Crohn disease can be approached in two different ways: step-up therapy and top-down therapy. MAXIMIZE TABLETABLE QUIZ Overview of pharmacotherapy for Crohn disease [13][20] Indication Substance class Symptomatic treatment Acute episode Mild-tomoderate disease Substances Antidiarrheal agents Loperamide Bile acid binders Topical corticosteroids Triamcinolone Topical 5-aminosalicylic acid derivatives (5-ASAs) (e.g., suppository, foam, enema) Topical corticosteroids Oral budesonide Sulfonamides Sulfasalazine First-line: oral corticosteroids Prednisone Overview of pharmacotherapy for Crohn disease [13][20] Indication Substance class Moderate-tosevere disease Severe/fulminant disease Steroidrefractory disease Azathioprine 6-Mercaptopurine Alternatively o Anti-p40 antibodies o Alpha 4 integrin inhibitors Ustekinumab (anti-p40 antibody) Natalizumab, vedolizumab (alpha 4 integrin inhibitors) First-line: IV corticosteroids Methylprednisolone Infliximab, adalimumab, certolizumab (TNFα antibodies) If necessary: azathioprine (or 6mercaptopurine) Steroid-sparing: thiopurine analogs Maintenance therapy Substances First-line: TNF-α antibodies, if necessary in combination with thiopurine analogs Choice of substance depends on which agent was used to induce remission Corticosteroids are contraindicated for maintenance. 5-ASA/sulfasalazine have proven to be inefficient. [21] The following substance classes are available: o Thiopurine analogs o Antimetabolites o TNF-α antibodies o Anti-p40 antibody o Alpha 4 integrin inhibitors Corticosteroids should not be used for long-term maintenance therapy! Surgery Overview Azathioprine, 6-mercaptopurine (thiopurine analogs) Methotrexate (antimetabolite) Infliximab, adalimumab, certolizumab (TNFα antibodies) Ustekinumab (anti-p40 antibody) Natalizumab, vedolizumab (alpha 4 integrin inhibitors) Minimally-invasive resection of affected and nonfunctional intestinal loops while preserving as much intestinal length and function as possible Indicated when medical therapy fails or patient develops severe complications (e.g., obstruction, stricture, abscess) Methods Balloon dilatation: to treat intestinal stenosis Percutaneous drainage: prevents retention of secretions and abscessation Surgical drainage: when application of percutaneous drainage fails Strictureplasty o A surgical procedure that opens up a bowel stricture without having to resect the bowel (bowel-sparing technique) o Indicated after multiple resections Limited resection (e.g., proctocolectomy): in case of obstructions or strictures Crohn disease is mainly treated with medication, but surgical interventions may be required to treat complications or if medical therapy fails. Surgical intervention alone cannot cure Crohn disease and should therefore be considered as a last resort to avoid complications in which significant amounts of bowel are lost (e.g., short bowel syndrome)! Additional considerations Lifestyle modifications Smoking cessation Avoiding certain drugs (e.g., NSAIDs ) Minimizing stress Management of complications and comorbidities Malabsorption syndrome: appropriate substitution of vitamins, calories, protein, zinc, calcium, and iron Bile acid diarrhea: administration of ion-exchange resins to bind bile acids (e.g., cholestyramine) Depression and anxiety: See “Major depressive disorder” and “Generalized anxiety disorder.” Prevention of malignancies Individuals with CD have an increased risk of cancer (especially of the small intestine, colon , and lymphatics). Regular colonoscopies should be performed to minimize risk. People without major colonic involvement are managed according to the general screening guidelines (see ”Screening for colorectal cancer”) Nutrition o Enteral nutrition always take preference over parenteral o If oral food intake is not possible, nasogastric or nasoenteric tube should be used o Secondary lactose intolerance (approx. 30% of cases): lactose-free diet [22] o During acute episodes: avoid dietary fiber NOTES FEEDBACK Complications Intestinal complications Colorectal cancer (especially in the case of pancolitis) Short bowel syndrome and associated issues after surgery Stenosis/strictures → bowel obstruction/(sub)ileus Intestinal perforation → peritonitis Primary sclerosing cholangitis Impaired bile acid reabsorption o Bile acid diarrhea o Bile acid malabsorption → steatorrhea and deficiencies in fat-soluble vitamins Abscess formation/phlegmons: See below. Intestinal fistulas and abscesses [23] Overview o Typically involve the terminal ileum and/or perianal region o Recurrences are common o See “Anal abscess and fistula.” Etiology o Iatrogenic (e.g., abdominal surgery, percutaneous drainage) o Inflammation (e.g., inflammatory bowel disease, appendicitis) Pathophysiology [24] o Inflammation → epithelial defects → epithelial-mesenchymal transition → deeper penetration of cell layers by epithelial cells → tissue damage that organizes as tubular structures that ultimately connect to other organs or the surface o After surgery or percutaneous drainage: deficient anastomoses/sutures or improper healing following intervention (e.g., due to reduced organ blood flow) → leakage of intestinal contents → local infection → abscess formation and/or erosion → fistula formation Clinical features: depend on location of the fistula o Enterovesical/colovesical fistula → pneumaturia (passing of urine together with air)/fecaluria (passing of stool together with urine) → recurrent urinary tract infections (UTIs) o Enterocutaneous fistula → drainage of intestinal content through the skin o Gastrocolic fistula → abdominal pain, weight loss, foul-smelling (feculent) belching Systemic complications Signs of malabsorption syndrome o Weight loss o Failure to thrive and growth failure in children o Anemia Iron deficiency anemia Anemia of chronic disease Megaloblastic anemia (vitamin B12 deficiency due to impaired absorption in the chronically inflamed ileum) Osteoporosis o . Amyloidosis We list the most important complications. The selection is not exhaustive. NOTES FEEDBACK Prognosis CD is a chronic disease that is currently not curable. Life expectancy is normal with proper treatment. [25] 70–90% of all patients will require surgery at some point during their lifetime. [26]