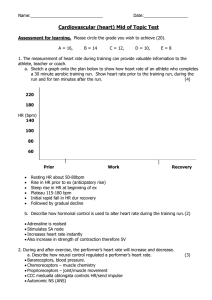
Cardiovascular System Function: to pump blood to all parts of the body Location of the Heart in the Thoracic Cavity -> Mediastinum (“midway”) – central compartment of the thoracic cavity 2. Aortic Valve – controls the blood flow from the left ventricle to the aorta 3. Atrio-Ventricular Valve Tricuspid Valve – right Atrio-Ventricular Valve Bicuspid Valve or Mitral Valve – left AtrioVentricular Valve 1. Heart – anatomical pump; pressure gradient; 2. Blood vessels - passageways Arteries – largest Veins Capillaries – smallest 3. Blood – transport medium (oxygen, carbon dioxide, nutrients, wastes, electrolytes, and hormones) Circulations – forms a figure 8 Pulmonary circulation – heart and lungs Systemic circulation – heart and organ systems Anatomy of the heart Atria Upper chambers RECEIVES blood Ventricle Lower chamber More muscle fibers; pumps blood from the heart Pulmonary arteries – carry blood away from the ventricles Pulmonary veins – return blood from tissues to the atria Valves – controls the blood flow from atrium to ventricle and prevents backflow 1. Pulmonary Valve – controls the blood flow from the right ventricle to the pulmonary arteries Organization of Cardiac Muscles Cardiac walls – composed of spirally arranged cardiac muscle fibers: 1. Endocardium (thin inner) – unique type of epithelial tissue that lines the chambers of the heart 2. Myocardium (thick middle layer) – cardiac muscles that consists of interlacing bundles -> intercalated disc) 3. Epicardium (thin external layer) – covers the heart 4. Pericardium (outermost later) Protects the heart against infection Provides lubrication Fixes the heart to mediastinum 2 layers of pericardium Serous layer Fibrous layer 2 Types of membrane junctions are present within intercalated disc Intercalated disc – composed of cell adhesion molecules that connects cardiac muscle to another by fusion: 1. Gap junctions - connect and facilitate communication between the two muscle cells (electrical signals) 2. Desmosomes – to hold together the two muscles Pericarditis - pericardial sac inflammation Effect: painful friction between two pericardial layers Cause: viral or bacterial infection Electrical Activity of the Heart Autorhythmicity (or automaticity) - the heart rhythmically contracts because of action potentials that it generates by itself 2 specialized types of cardiac muscle cells Electrical activity -> Mechanical activity 1. Contractile cells (99%) “working cells” Do mechanical work of pumping these cells normally do not initiate their action potentials atria, ventricles, valves 2. Autorhythmic cells Non-contractile cardiac cells specialized for initiating and conducting the action potentials responsible for contraction of the working cells Receive electrical signal that initiates action potential for contraction a. Sinoatrial node (SA node) PACEMAKER of the heart Start of the initial electrical activity Interatrial pathway (Bachmann’s) - spreads throughout both atria a group of autorhythmic cells that are located between vena cava and the right atrium b. Atrioventricular node (AV) Located at the base of the right atrium near the septum above between the atria and ventricles Internodal pathways - action potential spread from the atria to the ventricles c. Bundle of His (atrioventricular bundle) Divides to form the bundle branches that curves around the ventricular chambers d. Purkinje fibers (looks like small twigs of a tree branch) Small terminal fibers that extend from the bundle of His Spread throughout the ventricular myocardium Pacemaker Potential in Autorhythmic Cells Pacemaker activity - cardiac autorhythmic cells do not have a resting potential D: Lowest Point K+ : close channels Na+ : open channels Action Potential in Cardiac Contractile Cells Occurs at the ventricular to contract cardiac muscles E: Pacemaker potential (slow depolarization) K+ : closed channels Na+ : opened channels, leak or funny channels (influx) T-type Ca2+ [Tiny channels] : open channels (influx) A: Threshold (fast depolarization) L-type Ca2+ channels [Large channels] open channels (influx) Na+ : close channels B: Peak of the Pacemaker potential Ca2+: close channels K+: open channels C: Repolarization K+ : goes outside the cell 4: Resting potential K+ : open channels (goes outside the cells) 0: Depolarization Na+ : open channels (influx) 1: Repolarization Na+ : close channels (influx) K+ : open channels (fast efflux) 2: Slow entry of Ca2+ K+ : open channels (slow efflux) L-type Ca2+ : open channels (influx) 3: Repolarization K+ : open channels (goes outside the cells) L-type Ca2+ : close channels (influx) Autorhythmic and Contractile Cells Actin and Myosin – responsible for contraction Electrocardiogram (ECG) Biomedical device that records the electrical activity present in body fluids from the cardiac impulse that reaches the body surface, Indirect recording of the actual electrical activity of the heart. Representing the overall spread of activity throughout the heart during depolarization and repolarization P wave rate 60-100 bpm with 10% variation – Normal = 75 Sinus Bradicardycardia: Rate < 60 bpm slow heartbeat Sinus Tachychardia: Rate > 100 bpm fast heartbeat Results from: - Pain/Anxiety - Volume depletion - Pericarditis - Chronotropic drugs (dopamine) Abnormalities in Heart Rhythm Arrhythmia – Any variation from the normal rhythm and sequence of excitation of the heart ECG Waves 3 distinct wave-forms: 1. P wave – ATRIAL depolarization Filling of blood in the atria PR segment (AV nodal delay) – opening the valve 2. QRS wave – VENTRICULAR depolarization Blood is pumped out of the atrium ST SEGMENT– contraction of ventricles; emptying 3. T wave – VENTRICULAR repolarization K+ goes out repolarizing the cell TP segment – relaxing and filling Hearth Rhythm and Heart Rate Normal sinus rhythm – heart rhythm Formula: 1500/(small x big boxes) Other method: 60/0.2 x big box Atrial fibrillation has irregular distance while atrial flutter has equal distance Thromboembolism – blood clot; clogging of vessels Cardio version – small plates with lower voltage input compared to defibrillator Mechanical Events of the Cardiac Cycle Heart Murmurs Contraction Relaxation Resultant changes in blood flow through the heart Cardiac cycle alternate periods Systole – contraction and emptying Diastole – relaxation and filling Stages of Cardiac Cycle 1. Filling phase – ventricles fill during diastole and atrial systole 2. Isovolumetric contraction – ventricles contract, building up pressure ready to pump blood into the aorta/pulmonary trunk 3. Outflow phase (ventricular systole) – the ventricles continue to contract, pushing blood into the aorta and the pulmonary trunk 4. Isovolumetric relaxation (ventricular diastole) – the ventricles relax, ready to re-fill with blood in the next filling phase Laminar (layer) flow - normal flow of the blood in which layers of the fluid slide smoothly over one another does not produce an audible sound Turbulent flow - a turbulent sound/murmurs can be heart from the heart Cardiac Output (CO) - the volume of blood pumped by each ventricle per minute depends on heart rate (HR) and stroke volume (SV) Cardiac Output = Average HR x Average SV Determined by stroke volume Cardiac Reserve - Difference between the cardiac output at rest and the max volume of blood the heart can pump per minute Stroke Volume = EDV - ESV Influence: 1. Intrinsic control related to the extent of venous return 2. Extrinsic control related to the extent of sympathetic stimulation of the heart Ejection Fraction = SV/EDV - Healthy heart – EF= 50% - 70% Heart during strenuous exercise – EF = 90% Failing heart – EF= 30% or less Heart failure (HF) – the inability of CO to keep pace with the body’s demands for supplies and removal of wastes Heart Diseases associated with Coronary circulation (Coronary Artery Disease) 1. Vascular Spasm - Abnormal spastic constriction that transiently narrows the coronary vessels Vasoconstriction of blood vessel because of damaged blood vessel to prevent the leakage of blood 2. Atherosclerosis 3. Thromboembolism - - formation in a blood vessel of a clot (thrombus) that breaks loose and is carried by the blood stream to plug another vessel embolus – piece of clot thrombus – blood clot