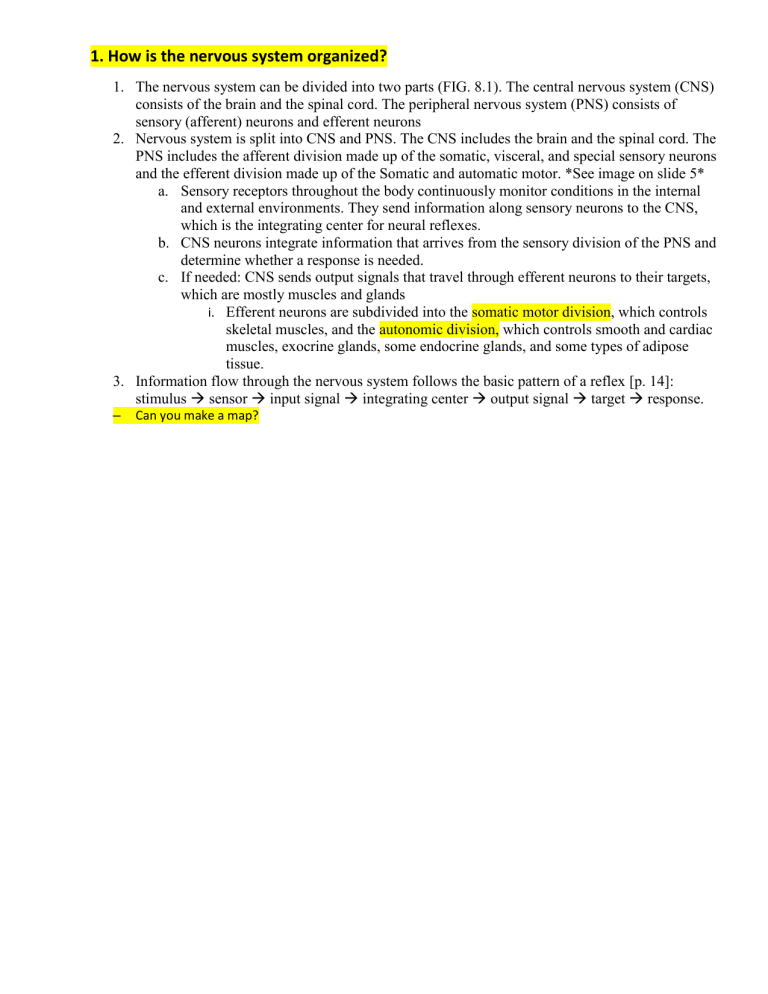
1. How is the nervous system organized?
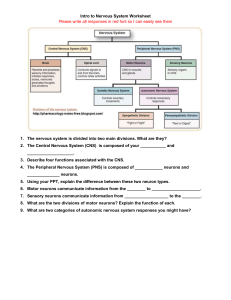
1. The nervous system can be divided into two parts (FIG. 8.1). The central nervous system (CNS)
consists of the brain and the spinal cord. The peripheral nervous system (PNS) consists of
sensory (afferent) neurons and efferent neurons
2. Nervous system is split into CNS and PNS. The CNS includes the brain and the spinal cord. The
PNS includes the afferent division made up of the somatic, visceral, and special sensory neurons
and the efferent division made up of the Somatic and automatic motor. *See image on slide 5*
a. Sensory receptors throughout the body continuously monitor conditions in the internal
and external environments. They send information along sensory neurons to the CNS,
which is the integrating center for neural reflexes.
b. CNS neurons integrate information that arrives from the sensory division of the PNS and
determine whether a response is needed.
c. If needed: CNS sends output signals that travel through efferent neurons to their targets,
which are mostly muscles and glands
i. Efferent neurons are subdivided into the somatic motor division, which controls
skeletal muscles, and the autonomic division, which controls smooth and cardiac
muscles, exocrine glands, some endocrine glands, and some types of adipose
tissue.
3. Information flow through the nervous system follows the basic pattern of a reflex [p. 14]:
stimulus sensor input signal integrating center output signal target response.
–
Can you make a map?
–
2. Discuss the anatomy of a neuron
•
•
•
•
•
•
Neurons are uniquely shaped cells with long processes (dendrites) that extend outward from the nerve
cell body.
Dendrites receive incoming signals/axons which carry outgoing info.
The shape, number, and length of axons and dendrites vary from one neuron to the next, but these
structures are an essential feature that allows neurons to communicate with one another and with other
cells.
Can be classified structurally or functionally
Structurally: neurons classified by # of processes originating from cell body (model most commonly
used is multipolar)
– Multipolar neurons in the CNS look different from multipolar efferent neurons
– In other structural neuron types, the axons and dendrites may be missing or modified
– Pseudounipolar neurons have the cell body located off one side of a single long process that is
called the axon (Fig. 8.2a). (During development, the dendrites fused and became part of the
axon.)
– Bipolar neurons have a single axon and single dendrite coming off the cell body (Fig. 8.2b)
– Anaxonic neurons lack an identifiable axon but have numerous branched dendrites (
Functionally: sensory (afferent) neurons, interneurons, and efferent (somatic motor and autonomic)
neurons.
– Sensory neurons carry information about temperature, pressure, light, and other stimuli from
sensory receptors to the CNS
– Peripheral sensory neurons are pseudounipolar, with cell bodies located close to the CNS and
very long processes that extend out to receptors in the limbs and internal organs. In these sensory
neurons, the cell body is out of the direct path of signals passing along the axon (Fig. 8.2a). In
contrast, sensory neurons in the nose and eye are much smaller bipolar neurons. Signals that
begin at the dendrites travel through the cell body to the axon
– Neurons that lie entirely within the CNS are known as interneurons
– Efferent neurons, both somatic motor and autonomic, are generally very similar to the neuron in
Figure 8.2e. The axons may divide several times into branches called collaterals {col-, with +
lateral, something on the side}. Efferent neurons have enlarged endings called axon terminals.
Many autonomic neurons also have enlarged regions along the axon called varicosities
– Nerves that carry only afferent signals are called sensory nerves, and those that carry only
efferent signals are called motor nerves. Nerves that carry signals in both directions are
mixed nerves
3. Discuss anterograde and retrograde transport
Axons are specialized to convey chemical and electrical signals. The axon cytoplasm is filled with many types of
fibers and filaments but lacks ribosomes and endoplasmic reticulum. For this reason, proteins destined for the axon
or the axon terminal must be synthesized on the rough endoplasmic reticulum in the cell body The proteins are
then moved in vesicles down the axon by a process known as axonal transport
– Anteretrograde: Forward transport that moves vesicles and mitochondria from the cell body
to the axon terminal
– Retrograde: Backward transport returns old cellular components from axon terminal to cell
body for recycling. Nerve growth factors and some viruses also reach cell body via
retrograde
–
What is the purpose?
4. Glial (support cells)
Discuss the two glial cells of the peripheral nervous system
•
Schwann and Satellite
•
Shwann: support and insulate axons by forming myelin. Also act as insulation around axons and
speeding up their signal transmissions.
•
•
Satellite: non-myelinating schwann cell that helps form the supportive capsules around nerve
cell bodies located in the ganglia
•
–
myelin, a substance composed of multiple concentric layers of phospholipid membrane
. A ganglion {cluster or knot} is a collection of nerve cell bodies found outside the CNS.
Ganglia appear as knots or swellings along a nerve. (A cluster of nerve cell bodies inside
the CNS, the equivalent of a peripheral ganglion, is called a nucleus {plural, nuclei}.)
Discuss the four glial cells of the central nervous system
•
microglia, astrocytes, ependymal cells, and the oligodendrocytes
•
Oligodendrocytes: Same as schwann cells, but in the CNS
•
Astrocytes: highly branched CNS glial cells that by some estimates make up about half of
all cells in the brain and come in several subtypes form a functional network by
communicating with one another through gap junctions.
•
•
They are closely associated with the synapses, take up and release chemicals
•
Provide neurons with metabolic substrates for ATP prod.
•
Help maintain homeostasis in CNS EC fluid by taking up K+ and water
•
Ends of astrocytes processes surround blood vessels and become part of
blood/brain barrier q regulates movement of mat’l bet. Blood and EC fluid.
Microglia: not actually neural tissue. Specialized immune cells only residing in CNS.
When activated, remove damaged cells and foreign invaders.
•
•
Not always helpful. Sometimes will release damaging reactive oxygen species
(ROS) that form free radicals. The oxidative stress caused by ROS is believed to
contribute to neurodegenerative diseases, such as amyotrophic lateral sclerosis
(ALS, also known as Lou Gehrig’s disease) when activated
Ependymal Cells: Specialized cells that create a selectively permeable epithelial layer
(ependyma) q seperates fluid compartments of CNS.
•
Ependyma is one source of neural stemcells.
•
All glial cells communicate with neurons and with one another primarily through
chemical signals. Glial-derived growth and trophic (nourishing) factors help
maintain neurons and guide them during repair and development. Glial cells in
turn respond to neurotransmitters and neuromodulators secreted by neurons.
Glial cell function is an active area of neuroscience research, and scientists are
still exploring the roles these important cells play in the nervous system
• Discuss the importance of the Nernst and Goldman-Hodgin-Katz (GHK) Equations
Nernst predicts the membrane potential for a SINGLE ion. The Nernst equation assumes that the cell in
question is freely permeable to only the ion being studied. This is not the usual situation in living cells.
The Nernst equation describes the membrane potential that would result if the membrane were
permeable to only one ion
GHK predicts the membrane potentential using MULTIPLE ions (all ions that can cross the membrane.) The
GHK equation includes membrane permeability values because the permeability of an ion influences its
contribution to the membrane potential. If the membrane is not permeable to a particular ion, that ion does not
affect the membrane potential
• What are the main differences between graded and action potentials?
•
•
Graded Potentials are a reflection of stimulus strength. In the neurons, GPs are depolarization and
hyperpolarization occurring in the dendrites and cell body, as well as near the axon terminals (less freq
tho). The size/amp of these potentials is directly proportional 2 the strength of the trigger event (lg stim
causes strong gp). In the CNS and efferent div, GPs occur as result of chem sign d other neurons
opening chem gated ion chann. GP can also occur when open channels close
Action Potentials Travel long distances. They are very brief, large depolarizations that travel for long
distances through a neuron without losing strength. Their function is rapid signaling over long distances,
such as from your toe to your brain. Na and K move across the membrane during AP. AP do not alter
the conc gradient, wont fire during absolute refractory period, and are conducted *Look at table 8.3
• What are the steps in action potential development (specific)
– How are action potentials propagated?
•
•
•
•
•
•
•
•
•
Step One Resting Membran Potential: The membrane starts at the resting potential of 70mV
Step 2 Depolarizing Stimulus: A stimulus is received by the dendrites of a nerve cell.
Step 3 Reaching Threshold: If the opening is sufficient to drive the interior potential from -70
mV to -55 mV it has reached threshold. Voltage-gated Na+ and K+ channels begin to open
Step 4 Rapid NA+ Entry Depolarizes the Cell: More sodium channels open and sodium ions
rush into the cell membrane as the gates stay open. The sodium influx drives the cell
membrane potential from -55 mV to +30 mV
Step 5 Sodium Channels Close and Potassium Channels Open: Since the potassium
channels are much slower to open, the depolarization has time to be completed.
Step 6 K+ moves from EC Fluid: With the potassium channels open, K+ moves from cell to
extracellular fluid and the membrane begins back to its resting potential of -70 mV.
Step 7 K+ Hyperpolarization: Potassium channels remain open and additional K+ leaves the
cell. Repolarization typically overshoots the resting potential to about -90 mV, hyperpolarizing
the cell and preventing the neuron from receiving another stimulus.
Step 8 Voltage gated K+ channels close and less K+ leaks out of the cell
Step 9 Resting Potential: Potassium and sodium pumps eventually bring the neuron back to 70 mV and can now receive another stimulus.
• Discuss the steps involved in synaptic transmission and inhibition
SYNAPTIC TRANSMISSION
1. An action potential depolarizes the axon terminal.
2. The depolarization opens voltage gated Ca2+ channels, and Ca2+ enters the cell.
3. Calcium entry triggers exocytosis of synaptic vesicle contents.
4. Neurotransmitter diffuses across the synaptic cleft and binds with receptors on the postsynaptic cell.
5. Neurotransmitter binding initiates a response in the postsynaptic cell
SYNAPTIC INHIBITION
•
Know the difference between divergent and convergent neural networks
Divergence: the axon of a presynaptic neuron branches, and its collaterals (branches) synapse on multiple target
neurons
Convergence: when a group of presynaptic neurons provide input to a smaller number of postsynaptic neurons
• What controls the amount of neurotransmitter released?
– How are EPSPs and IPSPs controlled?
Stronger stimuli release larger amts of neurotransmitters; a single AP arriving at axon terminal releases const
amt of NT. Stronger stimuli results in more AP reaching axon terminal more NT release
Excitatory postsynaptic potential ESPS: synaptic potential when it is depolarizing because it makes the cell more
likely to fire an action potential. When more NA+ enters the postsynaptic cell, triggers ESPS
Inhibitory postsynaptic potential ISPS: synaptic potential when it is hyperpolarizing bc hyperpol moves the
membrane potential away from threshold and makes cell less likely to fire an action potential. When more K+
leaves the postsynaptic cell, decreased NA+ enters, or CL- enters, triggers ISPS
• Discuss the importance of glutamate for long-term potentiation
•
Glutamate is key element in potentiation
•
May be related to learning, memory, depression, and mental illness
•
Long-term potentiation and depression
• Discuss the primary differences between the autonomic and somatic nervous systems
Autonomic motor neurons: Controls smooth muscles, cardiac muscles, many glands, adipose tissue
Somatic neurons: control skeletal muscles
Autonomic nervous system: functions are not under voluntary control
Another name for the autonomic division is visceral nervous system because of its control over internal
organs
subdivided into sympathetic and parasympathetic branches
sympathetic: dominates in stressful situations, such as the potential threat from the snake. One
of the most dramatic examples of sympathetic action is the fight-or-flight response, in which the brain triggers
massive simultaneous sympathetic discharge throughout the body
parasympathetic: If you are resting quietly after a meal, the parasympathetic branch is
dominant, taking command of the routine, quiet activities of day-to-day living, such as digestion.
Autonomic system is Important for homeostasis
The ANS differs from the somatic nervous system in that it can stimulate or inhibit its effectors.
The effectors of the somatic nervous system are skeletal muscles, while the ANS innervates cardiac and
smooth muscles and glands.
In the somatic nervous system, the cell bodies of the neurons are in the spinal cord and their
axons extend to the skeletal muscles they innervate.
The ANS consists of a two-neuron chain in which the cell body of the first neuron, the preganglionic
neuron, resides in the spinal cord, and synapses with the second neruon, the postganglionic neuron,
reside within an autonomic ganglion outside the CNS.
The neurotransmitter released by the somatic motor neurons is acetylcholine, which always has an
excitatory effect; the neurotransmitters released by the ANS are epinephrine and acetylcholine, and both may
have either an excitatory or an inhibitory effect.
• What are the links between the endocrine, limbic and autonomic systems?
• Discuss neurotransmitters and targets of pre- and post-ganglionic axons of the PNS
and SNS.
All autonomic pathways (sympathetic and parasympathetic) consist of two neurons in a series (FIG. 11.4). The first
neuron, called the preganglionic neuron, originates in the central nervous system and projects to an autonomic
ganglion outside the CNS.
There, the preganglionic neuron synapses with the second neuron in the pathway, the postganglionic neuron
This neuron has its cell body in the ganglion and projects its axon to the target tissue.
Both sympathetic and parasympathetic preganglionic neurons release acetylcholine (ACh) onto nicotinic
cholinergic receptors (nAChR) on the postganglionic cell
Most postganglionic sympathetic neurons secrete norepinephrine (NE) onto adrenergic receptors on the target
cell.
Most postganglionic parasympathetic neurons secrete acetylcholine onto muscarinic cholinergic receptors
(mAChR) on the target cell.
• Discuss the anatomical features, primary actions, and primary receptors for PNS and
SNS peripheral nerves
PNS: The "rest and digest" system. responsible for:
- slowing the heart rate
- increasing gastric secretions
- emptying the bladder
- emptying the bowel
- focusing the eye for near vision
- constricting the pupil
- contracting bronchial smooth muscle
SNS: has three main functions
1. regulate the cardiovascular system
2. control body temperature
3. Implement the "fight or flight" response.
Receptors:
1. Both sympathetic and parasympathetic
preganglionic neurons release acetylcholine
(ACh) onto nicotinic cholinergic receptors
(nAChR) on the postganglionic cell [p. 252].
2. Most postganglionic sympathetic neurons
secrete norepinephrine (NE) onto adrenergic
receptors on the target cell.
3. Most postganglionic parasympathetic neurons
secrete acetylcholine onto muscarinic
cholinergic receptors (mAChR) on the target cell.
However, there are some exceptions to these
rules. A few sympathetic postganglionic
neurons, such as those that terminate on sweat
glands, secrete ACh rather than norepinephrine.
These neurons are therefore called sympathetic
cholinergic neurons
A small number of autonomic neurons secrete
neither norepinephrine nor acetylcholine and
are known as nonadrenergic, noncholinergic
neurons. Some of the chemicals they use as
neurotransmitters include substance P,
somatostatin, vasoactive intestinal peptide (VIP), adenosine, nitric oxide, and ATP.
The nonadrenergic, noncholinergic neurons are assigned to either the sympathetic or parasympathetic branch
according to where their preganglionic fibers leave the nerve cord. A few autonomic neurons co-secrete more
than one neurotransmitter simultaneously
• What is a neuroeffector junction? How is it different from a model synapse?
The targets of autonomic neurons are smooth muscle, cardiac muscle, many exocrine glands, a few
endocrine glands, lymphoid tissues, the liver, and some adipose tissue.
Neuroeffector junction (recall that targets are also called effectors): The synapse between a
postganglionic autonomic neuron and its target cell
autonomic postganglionic axons end with a series of swollen areas at their distal ends, like beads
spaced out along a string. such swellings are called a varicosity
• Why are actions of norepinephrine relatively slow, and acetylcholine relatively fast?
Takes longer to remove it from synaptic cleft.
• Reuptake into presynaptic terminal and degraded by monoamine oxidase (MAO)
• Some degraded by COMT
• Some diffuses away into blood where it circulates with epinephrine from adrenal medulla
• Describe the steps in somatic-neural coupling
• Excitation-Contraction Coupling
– Know the steps of E-C coupling from binding of acetylcholine to re-sequestration
of calcium at the sarcoplasmic reticulum
An action potential arrives at the axon terminal (of neuron) and voltage-gated Ca2+ channels open
causing an influx of Ca2+ into the axon terminal. [Ca2+ moved]
The influx of Ca2+ into axon terminal causes the exocytosis of ACh (a neurotransmitter: acetylcholine)
into the synaptic cleft.
ACh then binds to receptors on the motor end plate (of muscle cell). If the end plate reaches threshold,
an action potential is propagated on the sarcolemma and down the T tubules.
This causes depolarization of the T tubules and causes the release of Ca2+ from the terminal cisternae of
the sarcoplasmic reticulum.
This movement of Ca2+ into the muscle cell causes Ca2+ to bind to troponin, which moves tropomyosin,
exposing the myosin-binding active sites on G actin.
The myosin heads then form cross bridges to the G actin and immediately pivot toward the M line
causing chemically activated muscle contraction.
ATP binds to myosin heads, causing them to release muscle contraction and recock.
• Discuss differences between the three different muscle fiber types
•
•
Slow-twitch fibers: Rely primarily on oxidative phosphorylation
Fast-twitch fibers
– Develop tension faster
• Split ATP more rapidly
2+
–
–
–
Pump Ca into sarcoplasmic reticulum more rapidly
Fast-twitch glycolytic fibers
• Rely primarily on anaerobic glycolysis
Fast-twitch oxidative-glycolytic fiber: Use oxidative and glycolytic metabolism
–
• What factors affect development of muscular force?
•
Length-tension relationship
•
Muscle fiber recruitment
•
Muscle fiber size
•
Load applied
• What are teleological and mechanistic differences between skeletal and smooth
muscle?
Teleological:
Skeletal muscles can contract without conscious direction, and we can learn a certain degree of conscious
control over some smooth and cardiac muscle.
Skeletal muscles are unique in that they contract only in response to a signal from a somatic motor neuron. They
cannot initiate their own contraction, and their contraction is not influenced directly by hormones
They position and move the skeleton, as their name suggests. usually attached to bones by tendons made of
collagen [p. 80]. The origin of a muscle is the end of the muscle that is attached closest to the trunk or to the
more stationary bone. The insertion of the muscle is the more distal {distantia, distant} or more mobile
attachment
Mechanistic: When the bones attached to a muscle are connected by a flexible joint, contraction of the
muscle moves the skeleton. The muscle is called a flexor if the centers of the connected bones are brought
closer together when the muscle contracts, and the movement is called flexion. The muscle is called an extensor
if the bones move away from each other when the muscle contracts, and the movement is called extension