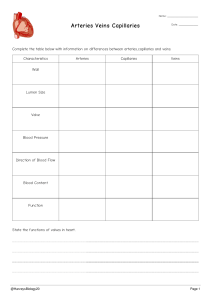
In the end of the lecture you will be able to : -differentiate between veins and arteries in their structure and function -venous and arterial blood flow direction and their mechanism -lymphatic system function , structure and related organs -changes in structure and function of peripheral vascular system during developmental stages . -do holistic assessment for your patient -common disease that affect peripheral vascular system -Health Promotion and Patient Teaching STRUCTURE AND FUNCTION : ARTERIES Arteries The function of the arteries is to supply oxygen and essential nutrients to the cells. The heart pumps freshly oxygenated blood through the arteries to all body tissues Which makes this a high-pressure system. The artery walls are strong, tough, and tense to withstand pressure demands. Arteries contain : elastic fibers :which allow their walls to stretch with systole and recoil with diastole. muscle fibers (vascular smooth muscle [VSM]), which control the amount of blood delivered to the tissues. The VSM contracts or dilates, which changes the diameter of the arteries to control the rate of blood flow. Each heartbeat creates a pressure wave, which makes the arteries expand and then recoil . It is the recoil that propels blood through like a wave which called pulse, you can feel it only at body sites where the artery lies close to the skin and over a bone. The following arteries are accessible to examination. Arteries in the Arm : Three sites Brachial (major):runs in the biceps-triceps furrow of the upper arm and surfaces at the antecubital fossa in the elbow medial to the biceps tendon Superficial and deep palmar arches : Radial : lies just medial to the radius at the wrist Ulnar: in the same relation to the ulna, but it is deeper and often difficult to feel. Legs – Four Locations Femoral (major): passes under the inguinal , travels down the thigh. At the lower thigh it courses posteriorly Popliteal: behind knee devides to : 1- The anterior tibial artery >>Dorsalis pedis: dorsum foot; lateral extensor tendon 2-Posterior tibial: behind medial malleolus ankle >>> plantar arteries in the foot VEINS The course of the veins is parallel to the arteries, but the direction of flow is opposite ,the veins absorb CO2 and waste products from the periphery and carry them back to the heart. The body has more veins, and they lie closer to the skin surface Veins in the Arm Each arm has two sets of veins: superficial and deep. The superficial veins are in the subcutaneous tissue and are responsible for most of the venous return. Veins in the Leg : The legs have three types of veins 1. The deep veins run alongside the deep arteries and conduct most of the venous return from the legs. These are the femoral and popliteal veins. 2. The superficial veins are the great and small saphenous veins. The great saphenous vein, inside the leg, starts at the medial side of the dorsum of the foot. The small saphenous vein, outside the leg, starts on the lateral side of the dorsum of the foot **Blood flows from the superficial veins into the deep leg veins 3. Perforators (not illustrated) Connect superficial (saphenous) system with deep system . They also have one way valves that route blood from the superficial into the deep veins and prevent reflux to the superficial veins. Unlike the arteries, veins are a low-pressure system. Because they do not have a pump to generate their blood flow, they need a mechanism to keep blood moving . 1. the contracting skeletal muscles that milk the blood proximally 2. the pressure gradient caused by breathing, in which inspiration makes the thoracic pressure decrease and the abdominal pressure increase. 3. the intraluminal valves, which ensure unidirectional flow(semilunar pocket) *In the legs this mechanism is called the calf pump or peripheral heart. -capacitance vessels. Efficient venous return depends on contracting skeletal muscles, competent valves in the veins, and a patent lumen. Problems with any of these three elements lead to venous stasis LYMPHATICS The lymphatics form a completely separate vessel system that retrieves excess fluid and plasma proteins from the interstitial spaces and returns them to the bloodstream. Without lymphatic drainage, fluid would build up in the interstitial spaces and produce edema. The vessels converge and drain into two main trunks, which empty into the venous system at the subclavian veins : 1. The right lymphatic duct empties into the right subclavian vein. It drains the right side of the head and neck, right arm, right side of the thorax, right lung and pleura, right side of the heart, and right upper section of the liver. 2. The thoracic duct drains the rest of the body. It empties into the left subclavian vein. The lymphatic system functions (1) conserve fluid and plasma proteins that leak out of the capillaries (2) form a major part of the immune system that defends the body against disease (3) absorb lipids from the small intestine. The immune system is a complicated network of organs and cells that work together to protect the body. It detects and eliminates foreign pathogens, both those that come in from the environment and those arising from inside (abnormal or mutant cells). It accomplishes this by phagocytosis (digestion) of the substances by neutrophils and monocytes/macrophages and by production of specific antibodies or specific immune responses by the lymphocytes. The lymphatic vessels have a unique structure. Lymphatic capillaries start as microscopic openended tubes, which siphon interstitial fluid. The capillaries converge to form vessels and drain into larger ones. The vessels have valves; therefore flow is one way from the tissue spaces into the bloodstream. The many valves make the vessels look beaded. The flow of lymph is slow compared with that of the blood. Lymph flow is propelled by contraction of the skeletal muscles, by pressure changes secondary to breathing, and by contraction of the vessel walls themselves. Lymph nodes are small, oval clumps of lymphatic tissue located at intervals along the vessels. Most nodes are arranged in groups, both deep and superficial, in the body. Nodes filter the fluid before it is returned to the bloodstream and filter out microorganisms that could be harmful to the body. The pathogens are exposed to B and T lymphocytes in the lymph nodes, and these mount an antigen-specific response to eliminate the pathogens. With local inflammation the nodes in that area become swollen and tender. The superficial groups of nodes are accessible to inspection and palpation and give clues to the status of the lymphatic system. 1. Cervical nodes drain the head and neck 2. Axillary nodes drain the breast and upper arm 3. The epitrochlear node is in the antecubital fossa and drains the hand and lower arm. 4. The inguinal nodes in the groin drain most of the lymph of the lower extremity, the external genitalia, and the anterior abdominal wall. RELATED ORGANS The spleen, tonsils, and thymus aid the lymphatic system (Fig. 21.7). 1. The spleen :left upper quadrant of the abdomen. It has four functions: (1) to destroy old red blood cells; (2) produce antibodies (3) to store red blood cells (4) to filter microorganisms from the blood. The tonsils (palatine, pharyngeal, and lingual) are located at the entrance to the respiratory and gastrointestinal tracts and respond to local inflammation. The thymus is the flat, pink-gray gland located in the superior mediastinum behind the sternum and in front of the aorta. It is relatively large in the fetus and young child and atrophies after puberty. It is important in developing the T lymphocytes of the immune system in children. The B lymphocytes originate in the bone marrow and mature in the lymphoid tissue. DEVELOPMENTAL COMPETENCE Infants and Children the excessive antigen stimulation in children causes the early rapid growth. Lymph nodes are relatively large in children, and the superficial ones often are palpable even when the child is healthy. The Pregnant Woman Hormonal changes cause vasodilation and the resulting drop in blood pressure ,The growing uterus obstructs drainage of the iliac veins and the inferior vena cava. This condition causes low blood flow and increases venous pressure. This in turn causes dependent edema, varicosities in the legs and vulva, and hemorrhoids. The Aging Adult Peripheral blood vessels grow more rigid with age, termed arteriosclerosis. This condition produces the rise in systolic blood pressure Aging produces a progressive enlargement of the intramuscular calf veins. Prolonged bed rest, prolonged immobilization, and heart failure increase the risk for deep vein thrombosis (DVT) and subsequent pulmonary embolism Loss of lymphatic tissue leads to fewer numbers of lymph nodes in older people and to a decrease in the size of remaining nodes. CULTURE AND GENETICS For environmental factors, cigarette smoking is a particularly strong risk factor for all persons with PAD, as are diabetes and hypertension. Other risk factors are elevated levels of total cholesterol and obesity. In the Heart and Soul Study examining risk factors by gender, data showed that depression was the strongest risk factor in women for PAD Common or Concerning Symptoms : 1. Leg pain or cramps 2. Skin changes on arms or legs (Cold, numbness, pallor in legs, hair loss) 3. Swelling in arms or legs 4. Lymph node enlargement 5. Medications 6. Smoking history Examination of the arms and legs includes peripheral vascular characteristics , the skin , musculoskeletal findings, and neurologic findings Room temperature should be about 22° C (72° F) and draftless to prevent vasodilation or vasoconstriction. Use inspection and palpation. Compare your findings with the opposite extremity. Equipment Needed Occasionally need: Paper tape measure Tourniquet or blood pressure cuff Stethoscope Doppler ultrasonic probe inspect and then turn the person's hands over, noting color of skin and nail beds; temperature, texture, and turgor of skin; and the presence of any lesions, edema, or clubbing. check capillary refill an index of peripheral perfusion and cardiac output Consider it normal if the color returns in less than 1 or 2 seconds . The two arms should be symmetric in size (note edema) Note the presence of any scars on hands and arms. Palpate both radial pulses, noting rate, rhythm, elasticity of vessel wall, and equal force Grade the force (amplitude) on a 3-point scale: 3+, Increased, full, bounding (HTN , HYPERTHYRODISM) 2+, Normal 1+, Weak (PAD) 0, Absent Check the epitrochlear lymph nodes :These nodes normally are not palpable. The modified Allen test : is used to evaluate the adequacy of both ulnar and radial artey Adequate circulation is suggested by a palmar blush, a return to the normal color of the hand in less than 7 seconds noting skin color, hair distribution, venous pattern, size (swelling or atrophy), and any skin lesions or ulcers. The venous pattern :normally is flat and barely visible Both legs should be symmetric in size without any swelling or atrophy. If the lower legs look asymmetric or if DVT is suspected If lymphedema is suspected, measure also at the ankle, distal calf, knee, and thigh. skin discoloration, skin ulcers, or gangrene, note the size and the exact location. Palpate for temperature along the legs down to the feet, comparing symmetric spots The skin should be warm and equal bilaterally. Assess calf for pain : Calf pain is not specific for DVT because it occurs also with superficial phlebitis, Achilles tendinitis, gastrocnemius and plantar muscle injury, and lumbosacral disorders. Palpate the inguinal lymph nodes. It is not unusual to find palpable nodes that are small (1cm or less), movable, and nontender. Palpate these peripheral arteries in both legs: femoral, popliteal, dorsalis pedis, and posterior tibial. Grade the force on the three-point scale noting the pulse tap under your fingertips. If this pulse is weak or diminished, auscultate the site for a bruit A bruit occurs with turbulent blood flow, indicating partial occlusion In adults older than 45 years, occasionally either the dorsalis pedis or the posterior tibial pulse may be hard to find, but not both on the same foot. Check for pretibial edema :Firmly depress the skin over the tibia or the medial malleolus for 5 seconds and. Normally your finger should leave no indentation , although a pit commonly is seen if the person has been standing all day or is pregnant. Bilateral, dependent pitting edema occurs with heart failure, diabetic neuropathy, and hepatic cirrhosis Unilateral edema occurs with occlusion of a deep vein. Unilateral or bilateral edema occurs with lymphatic obstruction. If pitting edema is present, grade it on the following scale: 1+, Mild pitting, slight indentation, no perceptible swelling of the leg 2+, Moderate pitting, indentation subsides rapidly 3+, Deep pitting, indentation remains for a short time, leg looks swollen 4+, Very deep pitting, indentation lasts a long time, leg is grossly swollen and distorted Ankle circumference is more reliable using a nonstretchable tape at a point 7 cm proximal to the midpoint of the medial malleolus. Because peripheral edema is a common clinical sign in a great number of conditions, it is important to detect true changes in the most accurate way available Ask the person to stand up so you can assess the venous system. Note any visible, dilated, and tortuous veins. If varicose veins are present, ask if they cause pain, swelling, fatigue, cramping. If you suspect an arterial deficit, raise the legs about 30 cm for about 30 seconds to drain off venous blood The skin color now reflects only the contribution of arterial blood. A light skinned person's feet normally look a little pale but still should be pink. A dark-skinned person's feet are more difficult to evaluate, but the soles should reveal extreme color change. Now have the person sit up with the legs over the side of the table (Fig. 21.22, A). Compare the color of both feet. Note the time it takes for color to return to the feet—the normal time is10 seconds or less. Note also the time it takesfor the superficial veins around the feet to fill Compare the two legs, note the time required for: Return of the pinkness; normally within 10s. Filling of the veins; normally within 15s Unusual rubor (dusky redness) after 1 min Dependent rubor (deep blue-red color) occurs with severe arterial insufficiency (Fig. 21.22, B). Chronic hypoxia produces loss of vasomotor tone and pooling of blood in the veins. Delayed venous filling occurs with arterial insufficiency. Test the lower legs for strength and sensation : Motor loss occurs with severe arterial deficit. You can map out the course and connection of varicose veins by transmitting pressure waves along the blood- filled veins. With the patient standing, place your palpating fingers gently on a vein, and with your other hand below it, compress the vein sharply. Feel for the pressure wave transmitted to the fingers of your upper hand. A palpable pressure wave indicates that the two parts of the vein are connected. Raynaud Phenomenon Episodes of abrupt, progressive tricolor change of the fingers in response to cold, vibration, or stress: (1) white (pallor) in top figure from sympathetic mediated vasoconstriction and resulting deficit in supply (2) blue (cyanosis) in lower figure from slight relaxation of the spasm that allows a slow trickle of blood through the capillaries and increased oxygen extraction of hemoglobin; (3) finally red (rubor) in heel of hand caused by return of blood into the dilated capillary bed or reactive hyperemia. May have cold, numbness, or pain along with pallor or cyanosis stage; then burning, throbbing pain, swelling along with rubor. Avoidance of cold is the most effective therapy; when episodes do occur, rewarm hands by donning gloves, rubbing in warm water, or using chemical rewarmers. After rewarming, a typical attack lasts 15 to 20 minutes. It is important to avoid smoking, sympathomimetic drugs, certain drugs for migraine headaches and for attention deficit/ hyperactivity disorder.24 Lymphedema Lymphedema is the accumulation of protein-rich fluid in the interstitial spaces of the arm following breast surgery or treatment. It results from axillary lymph node removal, radiation therapy, fibrosis, or inflammation. Acute lymphedema (within first 18 months) is reversible with treatment if no tissue damage has occurred. Chronic lymphedema is more difficult, and can lead to pain, disfigurement, mobility dysfunction, difficulty fitting into clothing, increased weight of arm making it hard to do daily activities, negative body image, and a constant emotional reminder of cancer Risk factors of lymphedema include : 1- Age 2- obesity 3- extent of axillary surgery 4- axillary radiation 5- infection Objective data include: unilateral swelling (compared to baseline pre-surgical measurement), measurement of arm volume, nonpitting brawny edema, overlying skin indurated . 3 types : 1. Chronic Arterial Insufficiency (Arterial (Ischemic) Ulcer) 2. Chronic Venous Insufficiency (Venous (Stasis) Ulcer) 3. Neuropathic Ulcer (diabetic) ARTERIAL (ISCHEMIC) ULCER Buildup of fatty plaques on intima (atherosclerosis) plus hardening, calcification of arterial wall (arteriosclerosis). S: Deep muscle pain in calf or foot, claudication (pain with walking); pain worsens with leg elevation; pain at rest indicates worsening of condition. O: Coolness in only one foot or leg, pallor, elevational pallor, and dependent rubor; diminished pulses; systolic bruits; signs of malnutrition (thin, shiny skin; thick-ridged Nails : atrophy of muscles); distal gangrene. Ulcers occur at toes, metatarsal heads, heels, and lateral ankle and are characterized by pale ischemic base, well-defined edges, and no bleeding; they look dry and punched out. Arterial ulcers are more common in those with smoking, diabetes, hyperlipidemia, and hypertension. VENOUS (STASIS) ULCER After acute DVT or chronic incompetent valves in deep veins. Venous ulcers account for 80% of lower leg ulcers. S : Aching pain in calf or lower leg, worse at end of day, worse with prolonged standing or sitting; pain lessens with leg elevation. Itching with stasis , dermatitis. O : Lower leg edema that does not resolve with diuretic therapy. Firm, brawny edema; coarse, thickened skin; pulses normal; brown pigment discoloration , petechiae , dermatitis. Venous stasis causes increased venous pressure, which then causes red blood cells (RBCs) to leak out of veins and into skin. RBCs break down to hemosiderin (iron deposits), which are brown pigment deposits , Borders are irregular , Venous ulcers are shallow and may contain granulation tissue. A weepy, pruritic stasis dermatitis may be present. Ulcers occur at medial malleolus and tibia; characterized by bleeding, uneven edges. DIABETIC Peripheral diabetic ulcer has its pathogenesis in sensory neuropathy with loss of protective sensation, autonomic neuropathy with decreased sweating and dry skin, and motor neuropathy with foot deformity. Symptoms include : numbness tingling, pain, weakness, loss of balance, falling, allodynia. Signs include : decreased reflexes, loss of proprioception, loss of vibration sensation, small muscle wasting, loss of warm and cold sensation and pinprick, decreased reflexes, poor blood flow, and cold feet. 1. Chronic Venous Disease (Superficial Varicose Veins) 2. Acute Venous Disease (Deep Vein Thrombophlebitis) SUPERFICIAL VARICOSE VEINS leg veins have dilated as a result of chronic increased venous pressure (obesity, multiple pregnancies) and incompetent valves that permit reflux of blood back toward leg instead of forward toward heart. Varicose veins are 3 times more common in women than men. Older age increases risk as a result of thinning of elastic lamina of veins and degeneration of vascular smooth muscle. Size ranges from 1 mm to 1 cm in diameter; color ranges from red to blue or purple. S: Aching, heaviness in calf, easy fatigability, restless legs, burning, throbbing, cramping. O: Dilated, tortuous veins. New varicosities sit on surface of muscle or bone; older ones are deep and feel spongy. DEEP VEIN THROMBOPHLEBITIS A deep vein is occluded by a thrombus, causing inflammation, blocked venous return, and edema. Virchow triad is the classic 3 factors that promote thrombogenesis: 1. stasis, 2. hypercoagulability, 3. endothelial dysfunction. Cause may be : prolonged bed rest, history of varicose veins, trauma, infection, cancer, obesity, immobility, heart failure, or the use of estrogen hormone S: Sudden onset of intense, sharp, deep muscle pain. O: Increased warmth; swelling (to compare swelling, observe usual shoe size as in above photo); redness; dependent cyanosis is mild or may be absent; tender to palpation; apply Wells criteria 1. Occlusions 2. Aneurysms Occlusions in arteries are caused by atherosclerosis, which is the chronic gradual buildup of (in order) fatty streaks, fibroid plaque, calcification of the vessel wall, and thrombus formation. This reduces blood flow with vital oxygen and nutrients. Risk factors for atherosclerosis include obesity, cigarette smoking, hypertension, diabetes mellitus, elevated serum cholesterol, sedentary lifestyle, and family history of hyperlipidemia. An aneurysm is a sac formed by dilation in the artery wall. Atherosclerosis weakens the middle layer (media) of the vessel wall. This stretches the inner and outer layers (intima and adventitia), the effect of blood pressure creates the balloon enlargement. The most common site is : the aorta the most common cause is atherosclerosis. The incidence increases rapidly in men older than 55 years and women older than 70 years; the overall occurrence is 4 to 5 times more frequent in men. The Doppler Ultrasonic Probe Use this device to detect a weak peripheral pulse, to monitor blood pressure in infants or children, or to measure a low blood pressure or blood pressure in a lower extremity Normal ABI is 0.90 - 1.30 because ankle pressure is slightly higher than brachial <.89 - >0.60 : mild PAD <.59 - >0.40: moderate PAD <.39: severe PAD Wells and others have combined findings into a simple scoring system. These criteria separate patients into groups of low, moderate, or high probability of DVT score of 0 or less = Low probability of DVT Score of 1 or 2 = moderate probability 2 points or more = high probability of DVT Description It is invasive procedure involves visualization of arteries, the most common site for an arteriogram is the femoral artery. Arterial catheters are positioned with a guide wire that is used to advance the catheter to a special location in the arterial tree. Because the arterial catheter is radiopaque, movement of catheter is noted with fluoroscopy. Purposes 1. Observe blood flow 2. Detect any lesion 3. Diagnosed of kidney or liver lesion 4. Introduction of chemotherapeutic drugs 5. Introduction of drugs to stop bleeding 6. Remove atherosclerotic plaques HEALTH PROMOTION AND PATIENT TEACHING Become familiar with the teaching points listed here, and adapt them for each patient's age and condition (e.g., heart failure, diabetes, obesity, PAD, arthritis) Foot care First, check your feet often • Look for red spots, sensitive areas, discoloration, cuts, blisters, and ingrown toenails. Use a mirror to check the bottoms of your feet. If you have diabetes, check your feet every day. • Wash your feet regularly, especially between your toes. Dry feet carefully after a shower or bath; gently slide a towel between each toe. • Keep toenails trimmed straight across, filed at the edges. • Wear clean socks every day. • Sit down and rotate your ankles in one direction, then the other, or try writing the alphabet from A to Z! • If you cannot walk far, put your feet up when sitting or lying down, stretching, wiggling toes. Having a gentle foot massage also helps. • If sitting a long time, stand up and move around every half hour or hour. • If you find yourself crossing your legs when sitting, uncross them often. • Measure your feet toward the end of the day, when feet may be the largest. • If you have one foot larger than the other, buy shoes that fit the larger one. • Choose shoes so that the ball of the foot fits comfortably into the widest part of the shoe and toes are not crowded. • Keep in mind that low-heeled shoes are safer and less damaging to the toes than are high-heeled shoes. • Use mild soap and mild skin lotion. • Avoid adding oils or bubble bath to the bath; it makes the feet and tub very slippery. SUMMARY CHECKLIST: PERIPHERAL VASCULAR EXAMINATION 1. Inspect arms for color, size, any lesions. 2. Palpate pulses: radial, brachial. 3. Check epitrochlear node. 4. Inspect legs for color, size, any lesions, trophic skin changes. 5. Palpate temperature of feet and legs. 6. Palpate inguinal nodes. 7. Palpate pulses: femoral, popliteal, posterior tibial, dorsalis pedis. 8. Touch sole of foot with microfilament.