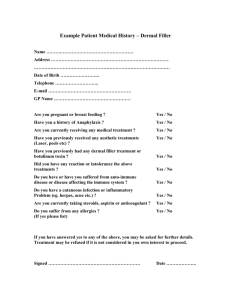
Case Study 2: Hyaluronic Acid Outline Structure Tissue and Cell distribution Biological Function Sources Biomedical Applications Structure & Function HA is a non-sulphated GAG and is composed of repeating polymeric disaccharides of D-glucuronic acid and N-acetyl-D-glucosamine linked by a glucuronidic β (1→3) bond. • forms H-bonds with H2 O molecules • helps maintain hydration of skin Tissue and Cell distribution In humans, HA is most abundant in the skin, accounting for 50% of the total body HA, the vitreous of the eye, the umbilical cord, and synovial fluid, but it is also present in all tissues and fluids of the body, such as skeletal tissues, heart valves, the lung, the aorta, the prostate, tunica albuginea, corpora cavernosa and corpus spongiosum of the penis. Biological Function hydration, lubrication of joints, a space filling capacity, and the framework through which cells migrate regulates several aspects of tissue repair, including activation of inflammatory cells to enhance immune response and the response to injury of fibroblasts and epithelial cells. provides the framework for blood vessel formation and fibroblast migration, that may be involved in tumor progression. Sources Biomedical Applications Biomedical Applications In tissue engineering. Chemical crosslinking of HA combines desirable biological and mechanical properties, even for bone or cartilage tissue engineering. Moreover, crosslinking extends the HA degradation process in vivo and provides long-term stability. Crosslinking HA at various densities has been used for multiple applications including orthopedics, cardiovascular medicine, and dermatology. Biomedical Applications As a dermal filler. To address age-related changes in skin quality and appearance, several treatments have been proposed. They may be classified based on their composition with primary ingredients such as collagen (bovine, porcine, or human), animal or synthetic hyaluronic acid, poly-L-lactic acid, calcium hydroxyapatite, polymethyl methacrylate, and polyacrylamide gel. Biomedical Applications HA as dermal filler and some of the commercially available products Material Hyaluronic acid Brand name Description Duration Restylene® Crosslinked HA (20 mg/mL) Temporary 6–12 months Prelane® Crosslinked HA (20 mg/mL) Temporary 6–12 months Juvéderm™ Crosslinked HA (24 mg/mL) Temporary up to 12 months Elevess® Crosslinked HA (28 mg/mL) Temporary months Hylaform® Crosslinked HA (5 mg/mL) Temporary 3–6 months Biodegradability Biodegradable Biomedical Applications In osteoarthritis treatment. After damage or aging, synovial fluid cannot provide the required viscoelastic response to compression and tangential forces arising in everyday life, allowing cartilage-cartilage contact and increasing wear of the joint surface. Intra-articular treatment with HA and hylans (uncrosslinked HA and crosslinked HA, respectively) has recently been accepted as a common therapy for reducing pain associated with OA. Currently, products such as Hyalgan® (HA), Orthovisc® (HA) and Synvisc® (hylan GF 20) are available as viscosupplements for intra-synovial injection in osteoarthritis treatment References Fakhari, A. & Berkland, C. (2013). Applications and Emerging Trends of Hyaluronic Acid in Tissue Engineering, as a Dermal Filler, and in Osteoarthritis Treatment. Acta Biomater. 2013 Jul; 9(7): 7081–7092. <10.1016/j.actbio.2013.03.005> Papakonstantinou, E., Roth, M. & Karakiulakis, G. (2012). Hyaluronic acid: A key molecule in skin aging. Dermato-Endocrinology 4:3, 253–258; July–December 2012; © 2012 Landes Bioscience. <http://dx.doi.org/10.4161/derm.21923>