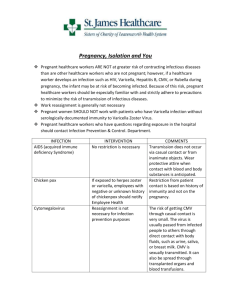
Running head: VARICELLA ZOSTER Infectious Disease: Varicella Zoster Rebecca E. Johnson Sullivan University BIO201: Medical Microbiology Professor: Joelle Robinson, MS June 7, 2020 VARICELLA ZOSTER 1 Abstract Varicella-zoster virus is known to be a common human pathogen, primarily observed in children, that causes varicella, more commonly known as “chickenpox”. Once infected with the virus individuals develop a febrile, pruritic rash, which evolves into pustules that will subsequently rupture and crust over. The duration of illness typically lasts four to seven days from the onset of symptoms. Once recovered, the virus establishes latency within the sensory nerve ganglia. Varicella-zoster can reactivate years later, most often in those over the age 50, as herpes zoster, also commonly known as “shingles”. Although both manifestations of the virus are uncomfortable and can have complications, the prognosis is favorable with most making a full recovery once the illness has run its course. “Chickenpox” and “shingles” were once very common diagnosis’s in the healthcare setting; fortunately, modern science and research have yielded a vaccine for both, minimizing the prevalence in today’s society. VARICELLA ZOSTER 2 Varicella Zoster Introduction Varicella Zoster Virus (VZV) is a highly contagious pathogen, found around the globe and exclusively present in humans. Varicella Zoster virus is the primary cause of varicella, commonly known as chicken pox. Persons whom have contracted VZV and develop chickenpox are found to have highly favorable outcomes with minimal or zero complications outside the typical manifestation of headache and fever that is accompanied by a pruritic (itching) rash that evolves to pustules (small bumps on the skin that contain fluid or pus) and/or vesicles (small, fluid-filled sacs that can appear on your skin) that rupture either spontaneously or by scratching, crusting over in the end stages of the illness (Zander & Farver, 2016, p. 260). Duration of illness is known to be on average four to seven days, with the majority of cases being observed in children. Once recovered, the virus lies dormant in the sensory ganglia and can later manifest as herpes zoster, more commonly known as shingles. Precipitates of manifestation are still being identified but the occurrence of a herpes zoster outbreak has been linked to unusual amounts of stress. Shingles outbreaks present clinically as prodromal (the period between the emergence of initial symptoms and the appearance of skin involvement) discomfort or pain for up to five days before the appearance of skin lesions that are also known to be quite painful. The duration of a shingles outbreak is much longer by comparison, with the ruptured and subsequently encrusted vesicles remaining for two to four weeks and the postherpatic (after a herpes type epidose) neuralgia (pain) associated lasting months in some cases. (Watson, Gershon, & Oxman, 2017, p. 26) Laboratory Identification and Pathogen characteristics According to a report published in Clinical Microbiology Reviews (Arvin, 1996, p. 361) the Varicella Zoster virion consists of a nucleocapsid (shell) surrounding a core that contains a linear, doublestranded DNA genome. Additionally, a protein tegument separates the capsid from the lipid envelope, that incorporates the major viral glycoproteins.The DNA of VZV consists of an estimated 125,000 base pairs, with at least 69 open reading frames (ORFs). The viral DNA is arranged in long and short unique segments with terminal repeat regions. Most full-length VZV DNA consists of two predominant isomers, although four isomeric forms are possible. Disease VARICELLA ZOSTER 3 Primary infection with Varicella Zoster is known to be contracted by way of airborne transmission of inoculated saliva/respiratory secretions that can become aerosolized when couching or sneezing, as well as direct contact with the fluid of ruptured vesicles. Chickenpox is most contagious during prodrome and early stages of the eruption, more specifically 48 hours before the first skin lesions appear and up until the final lesions have crusted. The incubation period for VZV is generally 7-21 days, historically most prevalent in children. (Zander & Farver, 2016, p. 261). Symptoms of Chickenpox include a febrile, vesicular-pustular, pruritic rash often accompanied by a headache and general malaise. It is further noted that, within just a few hours, the rash may present with lesions in all stages of development (see figure 1), including macules, papules, vesicles, pustules, and scabs. ("Varicella-zoster virus (VZV)," 2019). The appearance of new lesions usually ceases by the fifth day, with the majority crusting by the sixth day, and most crusts disappearing in less than 20 days from onset of illness (Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School, 2019). Herpes Zoster is the product of the reactivation of latent Varicella Zoster virus from the sensory ganglia. Herpes zoster acts by inflaming the sensory root ganglia, the skin of the associated dermatome (an area of skin that is supplied by a single spinal nerve). In some cases, the posterior and anterior horns of the gray matter, meninges, as well as the dorsal and ventral roots may become involved (Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School, 2019). Shingles outbreaks are often noted to initiate with discomfort or pain known as a prodromal period (the period between the emergence of initial symptoms and the appearance of skin involvement) burning, itching, tingling, stinging or numbness for up to five days before the eruption of unilateral fluid-filled vesicles that are also known to be quite painful. Shingles lesions physically manifest as a dermatomal rash (see figure 3) described as maculopapular, meaning a rash that contains both macules, flat discolored areas of the skin, and papules, small raised bumps. The maculopapules evolve into vesicles, pustules, and scabs that are painful and unilateral in location ("Varicella-zoster virus (VZV)," 2019). Diagnosis and Treatment Diagnosis is primarily made through physically assessment by a healthcare professional following the presentation of symptoms indicative of Varicella Zoster as discussed previously in this text. VARICELLA ZOSTER 4 Although additional diagnostic studies are not required in the routine management of either chickenpox or shingles, other findings consistent with the diagnosis will include blood specimen analysis, exudate cultures, as well as the use imaging for diagnosing suspected complications such as x-ray, magnetic resonance imaging (MRI) scan or a magnetic resonance angiogram (MRA). Laboratory analysis of blood specimens may reveal an elevation in the white blood cell (WBC) count in immunocompromised hosts and will reflect the nature of the immune compromise. Additionally, liver enzymes may be elevated in chickenpox, as the virus is circulated throughout the body via the bloodstream, which passes through the liver. It is believed that transient hepatitis likely occurs in most healthy individuals with primary VZV infection, but extensive viral replication in the liver, with widespread hepatocellular destruction due to virus-induced cell lysis, is a potential complication of progressive varicella, resulting in acute hepatic failure (Arvin, 1996, p. 361). It is further noted that vesicular lesions can be cultured, however, it has been determined that the virus does not survive well in transport media, even when preservative measures such as placing the container with the specimen is placed on ice have been attempted. Thus, retrieval of the virus in cell culture is of limited success and should only be performed by experienced clinicians. Polymerase chain reaction (PCR) detection of viral DNA is found to be the most sensitive and specific diagnostic for both chickenpox and shingles. Salivary specimens are found to be an excellent source of viral DNA when attempting to detect VZV by way of PCR ("Varicella-zoster virus (VZV)," 2019). Routine management of neither chickenpox or shingles requires diagnostic imaging studies, however, if complications arise they may be necessary. Complications of chickenpox may cause, in a low number of cases, a syndrome of cerebellar ataxia (inability to coordinate balance, gait, extremity and eye movements) or in rare cases, encephalitis (inflammation of the brain) (“Varicella-zoster virus (VZV)," 2019). In Herpes Zoster patients, granulomatous arteritis (also know as Temporal arteritis or Horton’s Disease), a chronic vascular disease of unknown origin occurring in the elderly, characterized by granulomatous inflammation in the wall of medium-size and large arteries, can occur after the infection has resolved. In both of the aforementioned circumstances, the use of a magnetic resonance imaging (MRI) scan or a magnetic resonance angiogram (MRA) would be of value in delineating pathology. (Watson, Gershon, & Oxman, 2017, p. 78-83) Radiographic imaging of the chest (chest x-ray) VARICELLA ZOSTER 5 is commonly used to assess for pneumonia in adults, most especially pregnant women, who exhibit classic dermatologic presentation of chickenpox (“Varicella-zoster virus (VZV)," 2019). Treatment for the primary VZV infection of chickenpox in children is typically limited to symptom management may include relief of itching with wet compresses and colloidal oatmeal baths may help or, in more severe cases of itching, the use of systemic antihistamines such as diphenhydramine, loratadine, cetirizine or hydroxyzine. Prevention of scratching is of high priority as it predisposes patients to secondary bacterial infections. It is also recommended that patients bathe regularly, change into clean underclothes frequently, practice more frequent hand hygiene and keep fingernails trimmed shorten length. It is not recommended to use antiseptics unless the lesions become infected, furthermore, bacterial superinfections are treated with antibiotics. Patients are considered contagious and should not return to school or work until the final lesions have crusted and dried. Immunocompromised patients and those at risk of severe disease or complication may be treated with antiviral medications such as acyclovir, famciclovir or valacyclovir (Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School, 2019). Treatment of herpes zoster should start as soon as possible, ideally during the prodrome, and is found to be less effective if initiated less than 72 hours from the time skin lesions appear. As with the treatment of varicella, treatment is primarily limited to symptom management for relief of itching by using wet compresses and colloidal oatmeal baths and in more severe cases of itching, the use of systemic antihistamines such as diphenhydramine, loratadine, cetirizine or hydroxyzine. Treatment with antiviral medications such as acyclovir, famciclovir or valacyclovir is common practice (Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School, 2019). Postherpetic neuralgia is almost always present and can be difficult to manage. Pharmaceutical interventions include the use of gabapentin, pregabalin, cyclic antidepressants, topical capsaicin or lidocaine ointment, and botulinum toxin injection. It is also not uncommon for opioid analgesics to be used in the plan of treatment. As with chickenpox, it is recommended that patients bathe regularly, change into clean underclothes frequently, practice more frequent hand hygiene and keep fingernails trimmed shorten length to mitigate the risk of bacterial infection at the lesion sites. VARICELLA ZOSTER 6 Prevention Varivax was licensed by the Food and Drug Administration in 1995 in the United States for use as a vaccine to prevent Varicella Zosta. This live attenuated varicella vaccine was developed by Merck & Co., Inc. induced protection against household exposure with an efficacy rate of more than 95% in an initial placebo-controlled study when administered to more than 7,000 children and more than 1,600 healthy susceptible adults during pre-licensure clinical trials (Arvin, 1996, p. 375). Present day, it is recommended that all healthy children and susceptible adults receive 2 doses of live-attenuated varicella vaccine. Children should receive the first vaccine at 12 months and the second at 4 years of age. Persons age 7–18 years whom have no evidence of immunity should receive 2 doses of varicella vaccine, with the 2nd dose given 3 months after the first dose in children aged 7–12 years; adolescents 13 years and older, including adults should receive the second dose at least 4 weeks after the first dose, noting that the minimum interval for both age groups is 4 weeks (Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School, 2019). As a result of the call to promote public health and use of Varivax, the incidence of varicella has decreased dramatically in the United States since it first became available in 1995. According to American Academy of Pediatrics’ Red Book (Kimberlin DW, Brady MT, Jackson MA, Long SS, eds., 2018) based on pre-vaccine disease rates, estimates suggest that the vaccination program prevents 3.5 million cases of varicella, 9,000 hospitalizations and 100 deaths each year. A staggering comparison to the early 1990s when the highest rate of varicella was reported in preschool-aged children and where it is documented that an average of 4 million people contracted varicella, 8,000 to 18,000 were hospitalized, and 100 to 150 died yearly (Jennifer Hamborsky, Kroger, & Wolfe, 2015, p. 353-376). Although infection with VZV provides lifelong protection for most, those infected are now burdened with the latency of herpes zoster. As the Varicella Zoster vaccine has proven to have great efficacy, research has shifted to prevention of herpes zoster. Scientists have developed 2 zoster vaccines, one being a recombinant vaccine, the other a live-attenuated vaccine. The recombinant vaccine is the preferred zoster vaccine as it provides better, longer-lasting protection than the live-attenuated vaccine. The recombinant vaccine is indicated for adults 50 years and older, regardless of whether they have had episodes of herpes zoster or have previously received a live-attenuated zoster vaccine. The recombinant VARICELLA ZOSTER 7 vaccine is administered in 2 doses, given 2 to 6 months apart and at least 2 months after the administration of a live-attenuated vaccine. The efficacy of the recombinant vaccine in immunocompromised patients is still unknown at this time. In 2017, Shingrix, a recombinant, adjuvanted (a pharmacological or immunological agent that improves the immune response of a vaccine) vaccine was licensed for prevention of zoster and post-herpetic neuralgia as a two-dose series for adults 50 years of age and older. Shingrix is recommended by the Centers for Disease Control and Prevention (CDC) as the preferred shingles vaccine. The live-attenuated vaccine is similar to the varicella vaccine but contains a larger amount of the attenuated virus. In 2006, Zostavax vaccine was licensed by the Food and Drug Administration (FDA)for the prevention of zoster and was recommended for all individuals beginning at 60 years of age. As mentioned above, it consists of the same Oka strain used in the Varivax, however, one dose of Zostavax contains approximately 14 times more virus (plaque-forming units) than that found in Varivax. In 2011, the FDA licensed Zostavax for those age 50 through 59 years for prevention of Herpes Zoster, although routine use for this age group was not recommended for this vaccine. Use of the live-attenuated vaccine is contraindicated in immunocompromised patients. Carriers, Transmission, and Epidemiology Carriers for the Varicella Zoster Virus are those who have contracted the illness and are in prodromal or active stages of illness.VZV is highly contagious and spreads easily from person to person, primarily through direct contact with persons in prodromal or active stages of illness to persons who have not previously had the disease or been vaccinated. It is of note that chickenpox can result in another case of chickenpox but will not result in shingles if one is exposed. Conversely, exposure to active shingles can result in a susceptible (without acquired immunity or vaccination) individual contracting chickenpox, but cannot cause shingles. As previously discussed, transmission of VZV is possible though either direct contact with an actively infected person or via airborne route. Transmission of inoculated saliva/respiratory secretions can become aerosolized when couching or sneezing, as well as direct contact with the fluid of ruptured vesicles. Varicella zoster, in its primary infection form, infects the mucosa of the oropharynx, where the initial round of virus replication takes place, resulting in the appearance of disseminated vesicles that VARICELLA ZOSTER 8 cover the trunk of the body and to a lesser extent, the extremities (see figure 2). Chickenpox is most contagious during prodrome and early stages of the eruption, more specifically 48 hours before the first skin lesions appear and up until the final lesions have crusted, on average, six days after the first lesions appear (Zander & Farver, 2016, p. 261). Shingles is the reactivation of latent virus from a sensory ganglion. Precipitants, also known as triggers, for reactivation of the virus are not well defined and remain unclear at this time. It is known that immunocompromised individuals are more susceptible to recurrent herpes zoster episodes due to their weakened immunity. As previously discussed, exposure to an active chickenpox infection will not result in contracting shingle, however, persons experiencing an episode of active shingles can infect in a susceptible individual with chickenpox, but cannot transmit shingles (Arvin, 1996, p. 372). The epidemiology of VZV infections is evolving with the discovery, implementation and success of vaccines. The use of these vaccines for both chickenpox and shingles (two different vaccines) has proven to drastically decrease the incidence of both diseases. The two dose administration schedule for the Varicella Zoster vaccine, the overall incidence of disease has decreased dramatically, although it is yet to be determined if waning immunity in young adults who received the chickenpox vaccine will be observed. Historically, a spike in chickenpox illness occurred in late winter and into early spring; however, after the introduction of routine vaccination, the epidemiology has changed and cases are now quite uncommon. Comparatively, the introduction of a shingles vaccine for use individuals over the age 50 years has decreased the incidence of disease by 50% ("Varicella-zoster virus (VZV)," 2019). Although shingles can recur, it is extremely uncommon in immunocompetent hosts, while immunocompromised patients with HIV/AIDS can have multiple episodes of shingles for reasons that are not yet entirely clear. Seasonal variations are not observed in the study of episodic shingles. Prevalence, Target population, susceptibility The prevalence of chickenpox, its incidences and associated complications has plummeted since licensure of a vaccine in 1995. A stark contract to just years before when chickenpox occurred in children at a rate that was nearly in line with the US birthrate. Still, some adults did not receive the vaccination and remain susceptible to the primary infection. Then remains the population of generations who have acquired immunity having been infected with Varicella Zoster during childhood, before the vaccine was VARICELLA ZOSTER 9 available. Those individuals remain at risk for episodic shingles and are strongly urged by healthcare professionals to receive vaccination against Herpes Zoster. Shingles increases in incidence in individuals with Advancing age and the incident os shingles are proportionally related with approximately 1 million cases occurring annually in the United States in persons older that 50 years of age ("Varicella-zoster virus (VZV)," 2019). Target populations include those previously discussed at length with the primary infection being acquired by susceptible individuals exposed to those excreting VZV in either the prodromal stages immediately prior to the development of the rash or during active stages of infection. Shingles being the reactivation of latent Varicella Zoster virus from its dormant stages within the sensory ganglia ("Varicellazoster virus (VZV)," 2019). In regard to susceptibility, immunocompromised hosts are most at risk for contracting both chickenpox and episodic shingles occurrences, as well as the associated complications of each disease. Of great concern in immunocompromised individuals, dissemination to involve organ systems is paramount. In some instances, immunocompromised patients can develop chronic VZV reactivation, which persists unless immunosuppressive therapy is reduced or antiviral therapy is used; AIDS patients being particularly susceptible to this complication. Cutaneous dissemination, defined as the appearance of lesions outside of the primary dermatome, is due to viremia (the virus entering the bloodstream), occurring in 10 to 40% of immunocompromised patients with herpes zoster and is indicative of possible visceral dissemination. Dissemination following VZV reactivation can result in pneumonia, hepatitis, encephalitis, and disseminated intravascular coagulopathy (the inability coagulate or form clots). Furthermore, VZV reactivation in high-risk patients, most especially bone marrow transplant recipients, may manifest atypical non-localized herpes zoster (see figure 4) resulting in increased clusters of lesions not associated with the location of latency within the sensory ganglia (Gross & Doerr, 2006, p. 26). This diffuse vesicular rash is indistinguishable clinically from varicella and has a higher mortality rate than localized herpes zoster. Episodes of severe or fatal VZV reactivation, manifesting as a “sepsis-like syndrome” or as central nervous system disease, absent of cutaneous lesions, have also been reported. Herpes zoster is an early clinical indicator of underlying HIV infection in known high-risk populations, increasing their risk for progressive, disseminated, or chronic VZV reactivation. Although extremely rare VARICELLA ZOSTER 10 except in patients with AIDS, progressive central nervous system infections have been documented in relation to VZV reactivation (Arvin, 1996, p. 372). Pregnant women in their second and third trimesters are at increased risk for complications if infected with Varicella Zoster. The primary concern is in regard to the development of pneumonia. Rarely, Varicella has been documented to complicate pregnancy, this is attributed to most adults having already acquired immunity. In a study conducted of 30,000 pregnancies, the incidence was 0.7 per 1,000 women. In rare cases, maternal varicella in early gestation results in the congenital varicella syndrome (CVS). Congenital varicella syndrome consist of skin lesions in dermatomal distribution, neurologic defects, eye diseases, and skeletal anomalies, with approximately 30% of infants born with these lesions documented to have not the first months of life. The diagnosis of CVS should be conformed by the appearance of maternal varicella, presence of typical clinical symptoms as indicated above, as well as laboratory confirmation of in utero varicella-zoster virus (VZV) infection. In the documented infants exhibiting the outlined diagnostic criteria, intrauterine VZV-infection has been confirmed in approximately 60% of cases. It is suggested that passive immunization may reduce the risk of fetal infection, however, there is no evidence that it can prevent fetal viremia (Arvin, 1996, p. 369). Current Research Medical research is ongoing and with regard to shingles, has two primary goals. The first of which is to develop drugs to fight the disease when it is present, as well as prevent and/or treat its subsequent complications. Secondly, research continues in an effort to understand the disease more completely in effort to prevent it, most specifically in those at higher risk. Achieving these goals are not without obstacles as much more information is needed to understand the unique intricacies of Herpes Zoster. There is still a wealth of information that remains unknown about VZV and its effects, most intriguingly, how it becomes latent in nerve cells, it's precipitants, and how reactivation leads to postherpetic neuralgia and other complications. The National Institute of Neurological Disorders and Stroke (NINDS) seeks out fundamental knowledge about the brain and nervous system, in an effort to use that knowledge to reduce the burden of neurological disease. The NINDS is a constituent of the National Institutes of Health, the global leader in support of biomedical research. The NINDS funds and conducts research on a wide range of neurological disorders, including shingles, to better understand their causes, VARICELLA ZOSTER 11 develop and improve ways to diagnosis, treat, and prevent those disorders. The NINDS currently supports research on the interplay between the viral proteins and virus defense mechanisms in neurons in efforts to better understand why VZV establishes latency uniquely in neurons and not other cell types. Additional studies are aimed at examining why and how VZV travels along sensory nerve fibers, and the role it plays in latency, as well as viral reactivation. Scientists hope to one day identify the molecular mechanisms that regulate the expression of latent viral genes, in hopes that may lead to developing targeted therapies to prevent reactivation. Lastly, research is underway in regard to postherpetic neuralgia that includes studies in animal models of the same condition, with the goal of better understanding the cellular changes that lead to persistent pain. These studies and research efforts my lead researchers on path to future targets in the way of improved vaccines, new pharmaceutical therapies, or even gene therapies (National Institute of Neurological Disorders and Stroke National Institutes of Health, 2015, p. 16). Conclusion In conclusion, although Varicella Zoster Virus is still present in todays society, the development and implementation of vaccinations for chickenpox has drastically reduced the prevalence of a disease that was once know to be as common as the occurrence of child birth per annum. Staggering figures given that in the early 1990s it is documented that an average of 4 million people contracted varicella, 8,000 to 18,000 were hospitalized, and 100 to 150 died yearly (Jennifer Hamborsky, Kroger, & Wolfe, 2015, p. 353-376). The successes and efficacy of the Varicella vaccine has paved the way for future generations to be spared the suffering of the subsequent reactivation of VZV, resulting in the much more painful Herpes Zoster that also has a much longer duration of illness. Those generations who had not received a vaccine prior to contracting VZV are now armed with options to prevent reactivating and potential Herpes Zoster episodes. As research continues and the population continues to age, it seems hopeful that Varicella Zoster may one day be eradicated, thereby eradicating Herpes Zoster as well. VARICELLA ZOSTER 12 Literature Cited: see references above Figure 2 (below): (Informatics & Berger, 2020, p. 34) Figure 1 (above): (Kimberlin DW, Brady MT, Jackson MA, Long SS, eds., 2018) Figure 4 (above): (Gross & Doerr, 2006, p. 26) Figure 3 (above): (Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School, 2019) VARICELLA ZOSTER 13 References: Zander, D. S., & Farver, C. F. (2016). Pulmonary pathology E-book: A volume in foundations in diagnostic pathology series [Google Books] (2nd ed. pages 260-263). Watson, C. P., Gershon, A. A., & Oxman, M. N. (2017). Herpes zoster: Postherpetic neuralgia and other complications: Focus on treatment and prevention [Googel Books]. Varicella-zoster virus (VZV). (2019, January 19). Retrieved from https:// www.infectiousdiseaseadvisor.com/home/decision-support-in-medicine/infectious-diseases/ varicella-zoster-virus-vzv/ Kenneth M. Kaye , MD, Brigham and Women’s Hospital, Harvard Medical School. (2019, October). Chickenpox - Infectious diseases - Merck manuals professional edition. Retrieved from https:// www.merckmanuals.com/professional/infectious-diseases/herpesviruses/chickenpox National Institute of Neurological Disorders and Stroke National Institutes of Health. (2015). Shingles: Hope through research. Bethesda, MA: Office of Communications and Public Liaison NIH Publication No. 15-307 May 2015. Kimberlin DW, Brady MT, Jackson MA, Long SS, eds. (2018). American Academy of Pediatrics. Varicella-Zoster Virus Infections. In: Red Book: 2018 Report of the Committee on Infectious Diseases (31st ed. pages 869-883). Gross, G., & Doerr, H. W. (2006). Herpes zoster: Recent aspects of diagnosis and control. CA: Karger Medical and Scientific Publishers. Jennifer Hamborsky, M., Kroger, A., & Wolfe, C. (2015). Epidemiology and prevention of vaccinepreventable diseases: The pink book (13th ed. Pages 353-376). Public Health Foundation. Informatics, G., & Berger, S. (2020). Varicella-zoster: Global status (2020 ed.). Los Angeles, CA: GIDEON Informatics.