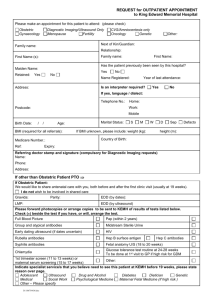
C h 41 Obstetrical Applications for 3D Ultrasonography Wesley Lee, M.D. Dolores Pretorius, M.D. CHAPTER CONTENTS A. INTRODUCTION B. IMPORTANT CONCEPTS FOR VOLUME SONOGRAPHY C. EARLY PREGNANCY EVALUATION USING 3DUS early fetal anatomic evaluation genetic risk assessment nuchal translucency nasal bone assessment frontomaxillary facial angle fetal pelvic angle embryonic volume D. SELECTED 3DUS APPLICATIONS FOR LATER PREGNANCY face eyes and ears metopic suture cleft lip and palate jaw abnormalities brain spina bifida skeletal dysplasia E. TISSUE VASCULARIZATION ASSESSMENT F. FETAL GROWTH AND WEIGHT ESTIMATION G. OTHER CONSIDERATIONS safety issues parental bonding medicolegal issues ultrasound for entertainment H. EMERGING CONCEPTS I. CONCLUSIONS 1 A. INTRODUCTION Three-dimensional ultrasonography (3DUS) can be combined with conventional twodimensional ultrasonography (2DUS) for the evaluation of normal and abnormal fetal anatomy. Development of cost-effective high performance computers and sophisticated image analysis software now makes it practical for 3DUS to be conveniently integrated with standard diagnostic imaging equipment. The previous chapter summarized basic concepts regarding the acquisition and fundamental concepts of ultrasound volume data. This overview will describe how this information can be applied to specific problems during pregnancy. Although 3DUS applications have been described for over two decades, one of our initial challenges was to evaluate their clinical value against a backdrop of emerging technology. In 2005, a literature review of more than 500 related articles suggested that additional diagnostic information was particularly useful for facial anomalies, neural tube defects, and skeletal malformations (1). Other potential benefits involved early pregnancy evaluation, nuchal translucency measurements, weight estimation, fetal lung volumetry, growth evaluation, and possibly maternal fetal bonding. Technical developments, such as spatiotemporal image correlation (STIC) algorithms, were also cited for improving our ability to examine rapid changes in the fetal heart. The following chapter by Dr. DeVore will more closely examine the emerging field of four-dimensional ultrasonography. B. IMPORTANT CONCEPTS FOR VOLUME SONOGRAPHY We have witnessed an impressive refinement of image analysis tools and their migration from dedicated image workstations to notebook computers. This technology permits the examiner to choose among many different visualization techniques with a variety of output display modes as summarized by Dr. Bega’s preceding chapter. In the most cases, volume sonography can be generally considered as an important diagnostic technique that is complementary to conventional 2D imaging. Before specific examples of how 3DUS can be applied to pregnant women are reviewed, we will first describe a few general concepts for how 3DUS can be best applied during pregnancy. 1. Use 2D ultrasonography for an initial diagnostic impression. Health care professionals are classically trained to translate 2D images into volume reconstructions for an improved understanding of spatial relationships and image patterns that suggest congenital abnormalities. Volume sonography provides the examiner with an opportunity to systematically evaluate anatomic structures with less inter-observer dependency, sometimes in ways that are not possible through conventional 2D methods. A preliminary 2D sonographic scan for suspected fetal abnormalities can be very useful and the results can be used to guide the subsequent 3D study. Once an initial differential diagnosis has been generated, the examiner should be able to formulate pending questions about the initial diagnostic impression that may or may not be satisfactorily addressed using 3DUS. If spina bifida is detected, for example, there may be a need to more precisely define the 2 anatomic level of the defect. This information would help the clinician to estimate the risk of problems related to ambulation and bowel or bladder function. In order to better understand the contribution of conventional imaging to 3DUS, Gonçalves and colleagues (2) compared both modalities in a blinded manner for 99 fetuses at a mean menstrual age of 24.4 ± 6.5 weeks. Complete agreement between 2DUS and 3DUS was observed for 90.4% of the findings. Six anomalies were missed by volume sonography, including ventricular septal defects (n=2), interrupted inferior vena cava with azygous continuation (n=1), tetralogy of Fallot (n=1), and cystic adenomatoid malformation (n=1). There were 12 discordant diagnoses between 2D and 3D ultrasonography. When compared to postnatal diagnoses (n=106), the sensitivity and specificity of volume sonography was 92.2% and 76.4%, respectively. However, no significant differences in the diagnostic conformity to neonatal outcomes were found when the 3DUS results were compared to the sensitivity (96.1%) and specificity (72.7%) from 2DUS (p = 0.23). This study concluded that the information provided by 2D ultrasonography is consistent, in most cases, with the diagnostic results from 3DUS. 2. Match the 3DUS technique with a specific clinical question that is being asked. The diagnostic benefit of volume sonography critically depends upon expectations of the examiner and the precise reason why the scan itself is being performed. Although most patients relate to this technology from its ability to display a fetal face for bonding purposes, this is not a recognized medical indication in low-risk pregnancies. In this context, one must recognize that 3DUS has the potential of revealing much more than a fetal face. The fundamental technologies, as described in the preceding chapter, actually represents several different image visualization tools that may or may not apply to the question being asked. They include multi-planar imaging, surface rendering, volume rendering, thick slice scanning, tomographic slices, inversion mode, and 3D Doppler ultrasonography (Figures 1-7). As one example, the maximum intensity projection algorithm might be most appropriate to analyze a possible hemi-vertebra that is suspected on the 2D scan. Complementary display modes, such as multi-planar imaging or the use of parallel tomographic slices, might also offer benefit. By comparison, a surface-rendering algorithm would not expected to provide useful information for bony structures such as cranial sutures or spinal abnormalities. This modality would be better suited for delineation of soft tissue problems such as cleft lip. Some volume analysis software packages allow the examination of volume reconstructions using a combination of different rendering algorithms (Figure 8). Others may use 4DUS for evaluating the status of joint movement of the wrist in a fetus suspected to have arthrogryposis. Hence, the examiner must remember to formulate one or more specific questions that are based on the initial 2D scan in order to choose the most appropriate type of image analysis. 3. Do not underestimate the diagnostic value of 3D multi-planar imaging. Although much emphasis has been placed on volume rendering, one must appreciate how useful it is for an examiner to analyze multi-planar image slices from standardized orthogonal views. In our practices, it is not uncommon that we might use this modality as the initial method of fetal organ evaluation. After standardized orthogonal planes are displayed, it is possible to systematically "march" through a volume of interest in order to better characterize the anatomy. One of the most common applications for this modality will be demonstrated for the fetal face evaluation. From these views, it will also be 3 possible to make a wide variety of quantitative distance, angle, and area measurements as needed. 4. Good two-dimensional imaging is likely to translate to satisfactory threedimensional volume acquisitions. The most useful volume data sets will be acquired when optimal sonographic technique is used in pregnancies where technical factors do not degrade the image. Remember the basics by adjusting scanning parameters such as system gain and acoustic focus. A reasonable goal is to adjust the region of interest in the rendering box so that it fills about two-thirds of the available display screen. Scan from different viewing perspectives for optimal images of the specific region of interest. For example, the fetal spine and overlying skin line should be obtained from a prone fetus, not from the supine position. We are often asked, "Is the sonographer's job at risk if all one needs to do is to place a transducer on the maternal abdomen and push a start button? The answer is emphatically, "NO!" because the likelihood that volume sonography will provide an adequate means for diagnostic interpretation is really dependent on the original quality of the images. The examiner should be able to optimize the image by utilizing the proper probe position while making certain that excessive pressure is not placed on the maternal abdomen. There are several ways to analyze good quality volume data sets if the original acquisition is obtained under optimal conditions. Careful attention should be made for adjusting image depth, acoustic focus, and signal gain at a time when fetal movement is minimal for acquisition of this image data. Both 2D and 3D ultrasonographic techniques, however, are sensitive to the potentially detrimental effects of maternal obesity, fetal movement, early fetal age, presence of maternal abdominal scars, and oligohydramnios. With these caveats in mind, some of the more common diagnostic applications will now be reviewed to further demonstrate basic approaches for using volume sonography during pregnancy. C. EARLY PREGNANCY EVALUATION USING 3DUS Early Fetal Anatomic Evaluation The first trimester 2D scan is mainly performed for dating early pregnancies, confirming cardiac activity, and to measure nuchal translucency as part of risk assessment for aneuploidy. Relatively fewer investigators have used conventional 2D imaging techniques to evaluate anatomic structures of the developing embryo. An important advantage of accurate early diagnosis would include parental reassurance that a major abnormality was not present. Earlier anomaly detection would provide more time for defining pregnancy options, prenatal care, delivery plans, and prognosis. As the field of fetal therapy develops, the earlier diagnosis of certain types of anomalies may even allow treatment at a time when chances for salvaging the fetus may be higher at an earlier stage of disease progression. Several investigators have used 2D endovaginal scans to visualize fetal anatomy before 14 weeks, menstrual age (3-5). First trimester pregnancies can also be evaluated using 3DUS although recent improvements in high frequency probe technology have made it 4 increasingly feasible to visualize cross-sectional and surface anatomy of the embryo (Figure 9). Blaas and co-workers (6) were among the first groups to use 3DUS for volume reconstruction of embryos between 7-10 weeks, menstrual age. They used a customized 7.5 MHz annular array vaginal probe and a VingMed system to trace contours of embryonic brain structures that permitted volume calculations as well. Normal embryonic anatomy has also been studied using 3DUS (7). One investigator threaded a catheter-based 20 MHz ultrasound transducer through the maternal cervix and endometrial cavity to demonstrate the embryonic face, limbs, and brain (8). Benoit et al (9) introduced the term, "sonoembryology" for describing the specific use of volume sonography of the developing fetus. He later demonstrated the evolving changes in embryonic brain development and reported that the optimal time to use 3DUS was between 7-12 weeks (10). Twelve representative images of the rendered volume provided an informative timeline of embryonic brain development (Figure 10). There have also been several related reports of conjoined twins (11-13), spina bifida (14), holoprosencephaly (10, 15-18), sirenomelia (19), and sacrococcygeal teratoma (20). Although the sensitivity of 2DUS for the detection of major fetal anomalies between 11 and 14 weeks has been reported to be approximately 50 percent (21), there are many factors that can affect diagnostic results. They include the population being studied, type of equipment used, examiner experience, exam duration, and the gestational age at which the scan is performed. Unfortunately, no large scale comparative studies have been performed that can clearly define the role of 3DUS for the systematic detection of fetal anomalies during early pregnancy as compared to 2DUS. Technical improvements, such as the development of more sophisticated image analysis tools or the commercial availability of higher frequency transducers, are likely to result in more accurate and earlier diagnoses over time. The best diagnostic technology in the world, however, will not be translated into improved outcome unless clinical management protocols are also capable of taking advantage of this information. How much additional benefit is actually provided by 3DUS over conventional 2DUS during early pregnancy? Michailidis and co-workers (22) compared real-time 2D scans (5 MHz transabdominal and 7 MHz transvaginal probes) to 3DUS (7 MHz transvaginal probe) for early fetal anatomic assessment. The anatomic survey included the head, face, stomach, abdominal wall, kidneys, bladder, spine, and extremities in 159 consecutive women at 12.0 to 13.9 weeks gestation. Two 3D volumes were obtained at the end of the procedure and they were subsequently analyzed for the same anatomic features that were examined using 2DUS. A "complete" anatomic survey was possible in 93.7% of the 2D scans which was a higher visualization rate than 80.5% of fetuses that were satisfactorily examined using 3DUS (p < 0.001). The mean time to perform a 2D scan was 12.2 ± 3.4 minutes (SD) as compared to the greater time it took to acquire and analyze 3D volume datasets for the same information (8.4 ± 1.5 minutes) (p<0.001). They concluded that real-time 2DUS was the best way to examine first trimester embryonic anatomy. Volume sonography provided occasional views that were not possible using 2DUS, was associated with less scanning time, and provided a mechanism where scanned data could be stored for subsequent review. Fauchon (23) recently performed a prospective study where an examiner acquired transabdominal 3DUS of the entire fetus from 273 singleton pregnancies between 11.0 5 and 13.9 weeks, menstrual age. Each dataset was manipulated and analyzed by two independent examiners who were blinded to each other's results. The requirements for sonographic visualization of 12 anatomic structures were strictly defined. Crown-rump length and nuchal translucency were measured with a high degree of agreement between both investigators in 100% and 84.6% of cases, respectively. Negligible clinical differences in either measurement resulted among all three examiners. In this study, a single abdominal 3DUS acquisition of a fetus between 11-13.0 weeks gestation usually provided satisfactory views for both the anatomic survey and nuchal translucency measurement of the embryo. Increasing maternal weight was an important factor that prevented adequate visualization of embryonic anatomy whereas longer crown rump length increased the odds of the examiners being able to identify half of these anatomic characteristics. The aforementioned studies indicate that the entire fetus can usually be satisfactorily screened for an anatomic survey during early pregnancy. Factors such as embryonic position, bladder filling, examiner experience, type of equipment used, menstrual age, limited range of probe movement, transducer frequency, and even maternal obesity can greatly influence the examiner's ability to complete this transvaginal study. The advantages for using a high frequency transvaginal probe to improve image resolution is offset by relatively limited tissue penetration. It also becomes increasingly difficult to capture the entire fetus after approximately 14 weeks, menstrual age. After this time, it may be necessary to acquire more than one volume data sets due to the technical specifications of most mechanical volume probes. Accordingly, one could subsequently attempt volume acquisitions with a lower frequency abdominal probe. More studies are required to characterize the normal appearance and evolution of embryonic structures on the basis of 3DUS. For example, the physiologic mid-gut herniation and its relationship to development of ventral wall defects is well known. This normal finding is typically very prominent in a 10 week fetus (Figure 9). Genetic Risk Assessment Several sonographic markers of genetic risk have included an evaluation of nuchal translucency (NT), nasal bone, frontomaxillary facial angle, fetal pelvic measurements, and embryonic volume. Key questions must be considered before these new techniques are introduced into clinical practice. First, the technique must be relatively simple to perform, affordable, and reproducible among different examiners. Second, the relationship of these measurements to menstrual age must be established. Third, the new marker should be able to distinguish between normal and pathologic pregnancies with good sensitivity and relatively low false positive rate. Fourth, any potential advantages over the use of conventional 2DUS and any technical limitations of the new technique should be described. Nuchal Translucency At least six reports have examined how 3DUS can be used to evaluate nuchal translucency (24-29). Paul et al. (27) studied 40 consecutive uncomplicated pregnancies who underwent first trimester screening for Down syndrome at 11-14 weeks. Nuchal translucency was measured using both transabdominal 2DUS and 3DUS. Two volume data sets were acquired - one that included a mid-sagittal plane and a second one that 6 was obtained from a random initial plane. This detail is important because images that are analyzed from the original plane of acquisition are usually the clearest because they do not require reconstruction. Small, but significant errors can occur if the nuchal translucency thickness is in the range of the ultrasound beam's lateral resolution of 1-2 mm. They found that nuchal translucency thickness could be repeated in 38/40 (95%) of the volumes that were acquired from a sagittal view of the fetus. By contrast, the random volumes yielded only 24/40 embryos with satisfactory nuchal translucency measurements. The mean difference between results from 2DUS and those obtained from reslicing "sagittal" volume datasets was -0.097 mm (95% limits of agreement from 0.481 to 0.675) and 0.225 mm (95% limits of agreement from -0.369 to 0.819) when random volumes were analyzed. Their results underscored the fact that the analysis of 3D volume datasets can be reliably used to replicate nuchal translucency measurements only when the nuchal skin line is also seen on the 2D scan. If visualization of the posterior neck is obscured by acoustic shadowing, one would not expect a well-defined nuchal translucency on the multi-planar reconstruction. Clementschitsch and co-workers (28) also prospectively examined 229 unselected pregnancies to compare the use of 2DUS and 3DUS for NT measurements. Satisfactory nuchal translucency measurements were obtained using 2DUS in 96.8% of cases as compared to 3DUS (98.6% transabdominal). Suboptimal fetal position was the main reason why 2DUS failed to provide satisfactory measurements. In some cases, it was difficult to precisely distinguish between fetal skin and amnion or uterine wall (6.3% for 2DUS, 3.3% for 3DUS). Fetal movement was the main reason for measurement failure using 3DUS. The mean time for either method was similar (9 minutes for 2DUS versus 10 minutes for 3DUS). Finally, the correlation between these measurements was very high (r = 0.97). Both studies suggest that reliable nuchal translucency measurements are feasible with transabdominal 3DUS during the 11-14 week embryo, especially if the original plane of volume acquisition contains a midsagittal view of the embryonic neck. Of course, it would be prudent to follow technical guidelines for 2DUS that are recommended by the Foundation for Fetal Medicine (http://www.fetalmedicine.com/downs/nuchal.htm) or the Nuchal Translucency Quality Review (NTQR, http://www.ntqr.org) programs to assure adequate quality control of these precise measurements. Presently, only the latter program addresses the use of 3DUS for NT measurement. The NTQR guidelines suggest that volume data acquisitions for this purpose are most reliable from a sagittal sweep of the embryonic face. Examiners are also cautioned about the potential limitations of lateral resolution for their ultrasound system. Can reliable NT measurements be obtained from volume data that are not originally acquired from a sagittal plane? Shipp and associates (30) addressed this question by analyzing NT measurements of 29 consecutive fetuses between 11.4 and 13.9 weeks, menstrual age. The 2DUS results were compared to 3D based measurements from a median sagittal plane of the embryonic neck. A sagittal plane was obtained by navigating through 3D multi-planar views using volume data sets that had been initially acquired from a coronal sweep of the embryo. The mean measurement (± SD) between 2DUS (1.7 ± 1.4 mm) was not statistically different from use of a reconstructed sagittal plane (1.8 ± 1.6 mm) (p = 0.4) and these results were highly correlated (r = 0.98, p < 0.001). Their findings suggest that nuchal translucency measurements are feasible from 3D data, 7 despite the original volume was initially acquired from a coronal plane. They also concurred with an earlier report that emphasized the importance of satisfactorily visualizing the neck region using 2DUS before initiating the volume sweep procedure (27). The interpretation and practical implementation of their findings warrant further investigation in a larger group of patients. Furthermore, the study did not consider the skill of the examiner for satisfactory manipulation of these volume data sets in a reproducible manner. Nasal Bone Assessment The fetal nasal bone also has been found to be a sonographic marker of genetic risk. Cicero and co-workers (31) used conventional 2DUS to identify the absence or presence of nasal bone in fetuses with trisomy 21 at 11 to 13 + 6 weeks gestation. The nasal bone was absent in 113 (0.6%) of the 20,165 chromosomally or phenotypically normal fetuses and in 87 (62.1%) of the 140 fetuses with Down syndrome. The inclusion of the nasal bone in first trimester combined screening for trisomy 21 achieved a detection rate of 90% for a false-positive rate of 2.5%. Another 2DUS study (32) observed a much lower rate of absent nasal bone in an unselected (16.7%) and selected (46.7%) population of fetuses between 11 to 13.9 weeks, menstrual age. Since this study did not utilize any formal training or quality assurance program for the detection of nasal bone, Sonek et al. (33) recommended that an ultrasound marker, such as the nasal bone, should not be used in a screening program unless the examiners are adequately trained. In an earlier study, Cicero et al (34) analyzed the ability of 15 sonographers for obtaining satisfactory views of the nasal bone. They found that approximately 80 2D examinations were required to achieve competency for nasal bone assessment during the routine 11-14 week scan. In this context, Malone and colleagues (35) performed nasal bone imaging as a screening tool for aneuploidy in 6,324 of 38,189 patients who were scanned at 10.4 to 13.9 weeks, menstrual age. An acceptable nasal bone image was reported in 76% of cases. Nasal bones were present in 4,779 (99.5%) of this subgroup and absent in 22 fetuses (0.5%). Absence of nasal bones had sensitivity for aneuploidy of only 7.7% with a false positive rate of 0.3% and positive value of 4.5%. They concluded that nasal bone evaluation was not useful for population screening for trisomy 21, possibly because of the difficulty in performing this assessment consistently in a general U.S. population setting. However, one-quarter of these sonographers reported unsatisfactorily visualization of the nasal bone despite specific training in first trimester sonography. These results seemed contrary to their specific implementation of a quality control program to monitor on-going performance of nasal bone sonography. Nonetheless, it is presently unclear as to why the FASTER trial results in the United States did not confirm the utility of nasal bone screening in the United Kingdom. Does 3DUS provide additional diagnostic benefit for nasal bone evaluation during early to mid pregnancy? Rembouskos and co-workers (36) found that a mid-sagittal view was the best original plane of 3D volume acquisition and their results suggested that satisfactory visualization of the nasal bone was optimal when the fetal profile was insonated at about 45 degrees. The likelihood of an adequately visualized nasal bone from a 3D volume dataset was strongly related to the quality of the initial 2D image. Other investigators (37,38) have used 3DUS to document the presence of a gap between the nasal bones during early pregnancy. Peralta (38) used 2DUS and 3DUS to scan 450 fetuses between 11.0 to 13.9 weeks, menstrual age. They found sonographic evidence of this gap in about 8 20 percent of fetuses. Furthermore, in about 40% of these cases, the nasal bone may erroneously be interpreted to be absent in an optimal median sagittal plane. Goncalves and associates (39) used 3DUS to evaluate nasal bones in 26 fetuses with Down syndrome during the second trimester of pregnancy (Figure 11). Rendered facial profile views demonstrated absent nasal bones in 18.9% of cases, of which 90% had Down syndrome for an overall sensitivity of 34.6% and false positive rate of 3.7%. This appearance was associated with a 9.3 fold increased risk for Down syndrome when compared to the normal control group. By comparison, three ossification patterns were demonstrated from coronal views of the rendered face: (1) normally developed, (2) delayed ossification, and (3) absent nasal bones. Sensitivity, false positive rate, and likelihood ratio of absent nasal bones for detecting Down syndrome were 34.6%, 3.7%, and 9.0 (95% CI, 1.3–68.7), respectively. These investigators identified nasal bones with delayed ossification by using this maximum intensity projection algorithm. Similar to findings from 2DUS, the absence of nasal bones was associated with the highest risk of Down syndrome. Delayed nasal bone ossification patterns were associated with a somewhat lower risk for these abnormal fetuses. The sensitivity, false positive rate, and likelihood ratio of delayed ossification for detecting Down syndrome were 42.3%, 22%, and 1.83 (95% CI, 0.8–4.4), respectively. This “hypoplasic” pattern probably reflects shortened nasal bones that have been described using 2DUS (40). Benoit et al. (41) subsequently used the 3D maximum intensity projection algorithm to demonstrate unilateral absence or hypoplasia of nasal bones during the second trimester of pregnancy. An analysis of these nasal bone patterns may improve our ability to identify fetuses at risk for Down syndrome. However, more experience with these methods is required for an unselected patient population before the diagnostic significance of 3DUS can be established for this purpose. Frontomaxillary Facial Angle Frontomaxillary facial angle (FMF) is another sonographic marker of fetal aneuploidy that has been studied in both the first and second trimesters of pregnancy. This measurement is defined as the angle between the upper surface of the upper palate and the frontal bone from a median sagittal view of the fetal face (Figures 12 and 13). Sonek and associates (42) used 3DUS to standardize this measurement, based on the hypothesis that the maxilla is dorsally displaced in relation to the forehead in fetuses with trisomy 21 between 11.0 to 13.9 weeks, menstrual age. The FMF angle was significantly larger in the abnormal group of 100 fetuses with Down syndrome (mean 88.7, range 75.4 – 104 degrees) as compared to 300 chromosomally normal controls (mean 78.1, range 66.6 – 89.5 degrees). This angle was also not significantly associated with NT. Subsequent work by the same group (43) underscored the importance of standardizing the FMF measurement using 3D multi-planar views of the facial profile that includes the tip of the nose and the rectangular shape of the maxillary bone. This approach was used to demonstrate very reproducible results and they were able to prospectively demonstrate that experienced examiners can alternatively measure the FMF angle using 2DUS as well (44). Furthermore, an increased FMF angle in fetuses at 11.0 to 13.9 weeks, menstrual age is increased in cases of trisomy 13 but, only when associated holoprosencephaly is present (45). A prospective study of 782 euploid and 108 fetuses with Down syndrome combined the FMF with biochemical screening tests (46). The inclusion of FMF angle to first-trimester combined screening increased the estimated detection rate from 90 to 94% 9 for a false positive rate of 5%. Molina and co-workers (47) also applied the FMF angle to 150 normal fetuses and 23 fetuses with Down syndrome between 16 – 24 weeks, menstrual age. In the normal group, the FMF angle did not change with menstrual age and the 95 th centile was 88.5. By comparison, the FMF angle was greater than 88.5 degrees in 65.2% of abnormal fetuses and inter-observer analysis indicated that in 95% of cases, the difference in measurements between examiners was less than 5 degrees. Technically, one must differentiate between the bony palate and vomer from a median sagittal view of the facial profile for optimal FMF measurements (Figures 14 and 15). Fetal Pelvic Angle Since the late 1990's, several studies have correlated iliac angles - from a 2D axial view of the fetal pelvis - with the risk of Down syndrome (48-50). Bork and colleagues (50) prospectively scanned 377 singleton fetuses, of which karyotypes were available for only 128 cases. The mean iliac angle for normal fetuses (68.2 ± 15.4 degrees) was significantly lower than observed in abnormal fetuses (98.5 ± 11.3 degrees). A receiver operator curve for their high-risk population identified an optimal cut-off of 90 degrees for a detection rate of 90.9% (5.5% false positive rate). By comparison, Shipp and associates (51) prospectively measured iliac angles for all fetuses undergoing second trimester amniocentesis over a 17-month period. Nineteen fetuses with Down syndrome and 1167 normal controls were scanned with a mean iliac angle was 80.1 ± 19.7 degrees for abnormal cases as opposed to normal controls (63.1 ± 20.3 degrees). The iliac angle was at least 90 degrees in 36.8 percent (7 of 19 fetuses) with Down syndrome and in 12.8% (64 of 500 fetuses) with normal karyotype. Despite their results, it was concluded that the iliac angle alone was not useful in a high-risk population because of the high falsepositive rate of 12.9%. French investigators also found a similar high false positive rate of 20% for use of the iliac angle as a single marker for trisomy 21 (52). Massez and coworkers (53) examined the effect of fetal position on the iliac angle measurement using 2DUS in 695 fetuses during the midtrimester. In euploid fetuses, the mean iliac wing angle was 83.7 degrees in decubitus and 68.7 degrees in the lateral position. In fetuses with trisomy 21, the mean angles were 104.9 and 102.5 degrees, respectively. A relatively high false positive rate of prior studies that utilized 2DUS may have been largely attributed to the complex structure of the fetal pelvis. To address this possibility, Lee et al. (54) used 3DUS to standardize iliac angle measurements from multi-planar views of the fetal pelvis. Thirty-five normal fetuses and 16 fetuses with trisomy 21 were scanned during second trimester amniocentesis. The mean iliac angle for normal fetuses was 79 ± 5.5 degrees, which was significantly less than the abnormal fetuses (87.7 ± 4.9 degrees) (P < 0.001). Intraclass correlation analysis suggested that this technique was reproducible between examiners. For a false-positive rate of 5%, an axial iliac angle threshold of 87 degrees alone correctly classified 56 percent of fetuses with trisomy 21 in this high-risk group. Further studies will be required to improve our understanding of the potential utility for iliac angle measurements for an unselected low-risk population during the second trimester of pregnancy. 10 Embryonic Volume Falcon and colleagues (55) used 2DUS and 3DUS to measure fetal trunk and head volume in 140 chromosomally abnormal fetuses at 11.0 to 13.9 weeks, menstrual age and compared them to 500 normal controls. In 72 fetuses with trisomy 21 and 14 fetuses with Turner syndrome, the CRL for gestation was similar, but the fetal trunk and head volume was about 10–15 percent lower. In fetuses with trisomy 18 (n = 29), trisomy13 (n = 14) and triploidy (n = 11), the deficit in volume was about 45 percent, as compared to crown-rump length, which was lower by less than 15 percent. These results raised the possibility that fetal trunk and head volume measurements may have advantages over 2DUS for the identification of early fetal growth abnormalities. The same research group used similar techniques to show that early asymmetric growth restriction between the trunk and head was characteristic of triploidy, trisomy 13, and trisomy 18 (56). By comparison, the growth abnormalities equally affected the head and abdominal volumes in fetuses with trisomy 21 and Turner syndrome. D. SELECTED 3DUS APPLICATIONS FOR LATER PREGNANCY Several 3D volume analysis tools can be applied to the fetus. Although we are trained to mentally translate 2D images into 3D representations, this traditional approach is limited by the examiner’s prior experience and ability to interpret this information. Furthermore, there are new volume analysis tools that permit us to visualize images in ways that are not possible using conventional methods. Despite these possible advantages, many diagnostic imaging cases can be simply evaluated from using only 2DUS. In some instances, 3DUS offers a complementary approach that may improve diagnostic confidence for the diagnostic impression that is initially based on conventional sonography. We currently use 2DUS for the prenatal detection of most congenital anomalies, with a targeted application of 3DUS to answer specific questions that are raised from the initial diagnostic impression. As more applications for 3DUS are described against an emerging backdrop of technological improvements, the paradigm for how volume sonography is applied to obstetrical practice may also evolve (57). For example, Benacerraf and coworkers (58) have described how 3DUS improved the workflow of clinical practices by the efficient acquisition and review of volume data sets. Although this is not a focus of the current chapter, several investigations have also proposed automating the analysis for data sets for the fetal heart (59-62). Others have reported remote sonographic diagnosis for telemedicine applications, using 3DUS in areas that are remote from the expert consultant (63-66). Volume sonography has also been used to assess fetal urine production in both normal fetuses (67, 68) and after laser surgery for a case of twin-twin transfusion (69). Many scientific articles have been published over the past decade as a result of the ultrasound manufacturing industry’s successful efforts to commercialize 3DUS technology into clinical practice. This process has not only included improved image quality, smaller transducers, and faster computers but, also the development of volume data analysis tools as well. Potential advantages and technical limitations of 3DUS will now be reviewed for selected obstetrical problems. 11 Face The fetal face is important because it can provide diagnostic clues for the presence of isolated abnormalities and genetic syndromes. Although many patients immediately recognize facial features from the surface rendered display, we believe that 3D multiplanar images are often the most helpful for medical diagnosis. However, the most appropriate selection of volume analysis tools critically depends on the question being asked. For example, one would use the maximum intensity projection algorithm to visualize problems with bony structures such as the cranial sutures. Soft tissue clefts might be well visualized with surface rendering. The lips and hard palate could be systematically evaluated by using multi-planar images as well. This modality allows one to use a reference dot to improve their understanding of complex anatomic relationships that are being investigated. Others might want to confirm a specific finding by using a parallel slice display (e.g. tomographic ultrasound imaging, multi-slice, i-Slice) or even thick slice scanning of the fetal lips (e.g. volume contrast imaging). Therefore, one must choose the most appropriate set of volume analysis tools on the basis of the diagnostic questions that are clinically relevant. Many early investigators pointed out the benefits of 3DUS in evaluating the fetal face (7072). Pretorius and associates (73) described their preliminary experiences with visualizing the fetal face and lips using surface rendering and multi-planar views. In a subgroup of fetuses at less than 24 weeks gestation, 3DUS confirmed a normal lip in 93% (58 of 63 cases) as compared with 76% (48 of 63 cases) using 2DUS. At that time, they noted that the 3D images of cleft lip were easier to understand for both the family and clinical colleagues. Merz and colleagues (74) used multi-planar views of the face and found that the facial profile that was obtained by 2DUS represented the true mid-sagittal profile in only 69.6 percent of cases. In the remaining 30.4 percent, the profile view deviated from a true mid-sagittal section by up to 20 degrees in one or two planes. In this series, they found 20 of 25 facial anomalies that were demonstrated using both 2DUS and 3DUS. In the remaining five cases, 3DUS revealed additional anomalies that included two cases of narrow cleft lip as well as single examples of unilateral orbital hypoplasia, cranial ossification defect, and flat facial profile with decreased amniotic fluid volume. Such preliminary observations were quite extraordinary for the level of 3D technological development at that time. It was not until approximately 3 years later that the “electronic scalpel” image segmentation tool became commercially available on desktop computers (75). This tool permits the examiner to selectively remove surrounding voxels that prevent the precise display of volume-rendered structures. One approach initiallty applies 4DUS to confirm recognizable features of the fetal face. The rendered algorithms provided by the equipment vendors are often excellent and provide a rapid acquisition of the face (Figure 16). Movement of the mouth is also easily demonstrated. Acquisition is optimal when the fetal face is acquired from the sagittal or profile view by placing the region of interest box (ROI) directly over the face, with the rendering line just anterior to the nose (Figure 17). The rendering line may be straight or curved to optimize the image. Occasionally it is necessary to increase the threshold knob to take away unwanted echoes, particularly in heavier patients. If the face cannot be positioned in a sagittal orientation, a frontal view (coronal) can be obtained, resulting in a rendered image that displays the profile of the fetus. 12 Static 3DUS acquisitions of the fetus generally provide better resolution than 4DUS acquisitions and are used for diagnostic evaluation. The face can be acquired from any orientation but sagittal and slightly oblique off sagittal are optimal for seeing the rendered face en face. Optimal planes of acquisition for various facial structures are summarized in Table 1. Manipulation of the 3DUS volume should begin with attempting to get the face into a standard, symmetrical orientation. The cursor dot should be placed on a midline structure, preferably the nose or the region in between the orbits. The volumes should be rotated in all three planes until the orbits are symmetrical. It can then be evaluated by moving up and down in parallel slices in each plane. The face can also be displayed using a multi-slice technique that is similar to MRI imaging or computed tomography where parallel slices at discrete intervals are varied to demonstrate the anatomy. In a series of 142 patients, McGahan et al. (76) found that if you started at 3 mm intervals there was minimal manipulation needed to show in the axial plane the orbits, maxilla (primary palate) and mandible on one screen. Finally, Rotten and colleagues (77) have nicely described how 2DUS and 3DUS can be systematically used to evaluate the fetal face Eyes Although there are no published series of cases of abnormal orbits, case reports and images in review articles have been published (78-80). The orbits can be measured from volumes acquired of the face to identify hypotelorism (Figure 18), hypertelorism and microopthalmia. We have found 3DUS very helpful when the orbits are absent or very small (Figure 19). Periorbital masses such as dacrocystocele (81), frontal encephalocele, glioma, hemangioma and teratoma may be difficult to evaluate with 2DUS and 3DUS can be helpful (82-84). Several authors have reported that 3DUS was useful in evaluating these entities and for showing parents the 3D images for counseling (82-84). Ears Fetal ear abnormalities are often associated with aneuploidy (e.g. Trisomy 13,18,21) as well as genetic syndromes such as Treacher-Collins Syndrome, Fraser syndrome, CHARGE association and VACTERL association (85,86). The ears may be small, large, abnormal shape and abnormal position. Although 2DUS can be used to assess the fetal ears, 3DUS has been found to be extremely helpful (Figure 20). Shih et al. (85) evaluated 18 fetuses with abnormal ears and using 3DUS and found the ear shape, ridge pattern and helix development as well as cranial location, axis and orientation of the ear was better recognized on 3DUS compared to 2DUS. Case reports of abnormal ears seen using 3DUS in fetuses with Treacher Collins syndrome have also been reported (87,88). Nomograms for ear length and width measurements obtained with 3DUS have been reported as a potential screening test for aneuploidy (86). 13 Metopic Sutures The metopic suture lies in the midline of the face above the nasal bone and is the space where the frontal bones comes together (Figure 21). Abnormal development of the metopic sutures has been associated with facial dysmorphism, fetal brain malformations, chromosomal defects and genetic syndromes (89). The use of 3DUS to evaluate cranial sutures and fontanelles was first reported in 1994 by Pretorius and Nelson (90). Visualization of normal sutures has been reported in 120 cases by Dikkeboom et al (91) and in 120 patients by Faro et al (92). In general, it is easier to visual the sutures at earlier gestational ages. The metopic sutures have also been evaluated in the first trimester (93,94). Holoprosencephaly is associated with an accelerated development of frontal bones and premature closure of the metopic sutures (93). Similar changes were not observed in fetuses with trisomy 21 (94). Faro and colleagues (95) have also described the presence of a widened metopic suture in fetuses with Aperts syndrome. Chaoui and co-workers (89) later described four patterns of abnormal metopic suture development. The first pattern involved delayed development with a V- or Y-shaped open suture in normal fetuses at 12-16 weeks. A second pattern was a U-shaped open suture. The third pattern was premature closure of the suture in normal fetuses after 32 weeks. The fourth pattern resulted from additional bone between the frontal bones in fetuses with holoprosencephaly and agenesis of the corpus callosum. The other three patterns were observed in fetuses with facial defects involving the orbits, nasal bones, lip, palate and mandible. Cleft Lip and Palate Despite some geographic differences, oral cleft defects are among the most common congenital abnormalities with a prevalence of approximately 2.0 per 1000 births during the mid-trimester of pregnancy (96). One large Norwegian study recently reported 101 fetuses or newborns with facial clefts for 49,314 deliveries. Twelve percent of affected cases were associated with chromosomal abnormalities and 18% were documented with syndromes (97). Cleft lip and palate were probably the main reasons that 3DUS was initially developed for the detection of fetal anomalies. Many papers have been written on the technique and benefits of 3DUS in evaluating the lip and palate. It assists in evaluating the presence, the extent and the appearance for communication with the patient and her family. Subtle deformities can be precisely evaluated using a stationary volume, rather than a moving fetus. Chmait et al. (98) showed that even clefts, thought to be isolated on 2DUS and 3DUS, were found to associated abnormalities at birth in 22% (8/37) of fetuses. Volumes are acquired from static 3DUS volumes to evaluate the lip and palate. Axial acquisitions angled slight upward toward the top of the mouth are optimal for evaluation of the primary and secondary palate. Rendered images of the face are helpful to demonstrate the cleft lip to the family (Figure 22). Multi-planar imaging can be used to evaluate the primary palate and lip. Many of the early articles only used the multi-planar reconstruction to evaluate for cleft lip and palate (99,100). Johnson et al (101) studied 28 fetuses with cleft lip with or without palate and found that 3DUS was able to identify the 14 cleft palate more frequently (19/22) than 2DUS (9/22). They also found that management was changed using 3DUS in that some patients elected to terminate the pregnancy and others elected to carry the pregnancy when they had planned otherwise. In another study, Chmait and co-workers (102) evaluated 53 fetuses with cleft lip with or without cleft palate and found that the diagnostic accuracy was improved for cleft lip to 100% (53/53) using 3DUS vs. 91% (48/53) using 2DUS and or cleft palate it was 89% (47/53) for 3DUS vs 57% (30/53) for 2DUS. An isolated cleft lip is shown in video 3 using both multi-planar and rendered displays. Wang (103) also demonstrated how the use of a parallel image slice display format (“extended imaging”) can also be used to evaluate fetal cleft lip and palate. The rendered display can also be used to evaluate the secondary (hard and soft) palate. Campbell et al. (104) first published the demonstration of the hard palate using a ‘reversed face’ technique. He later wrote an informative editorial discussing issues related to evaluation of the hard palate with various rendering techniques (105). Platt and colleagues (106) described the ‘flipped face’ technique to display the primary (alveolar ridge) and secondary (hard and soft) palate. This view emphasizes the palate with an upright face and viewing from an inferior direction, rather than superiorly (Figures 23 and 24). Faure (107) described a similar technique to display the primary and secondary palate in 100 low-risk fetuses that showed how 3D reconstruction of the fetal palate can be correlated to anatomic specimens. Pilu and co-workers (108) studied 15 normal fetuses and one fetus with cleft lip and palate and showed that the secondary palate could be evaluated if the face was insonated at a 45 degree angle in the sagittal plane; in addition, they showed that the palate could be displayed on both axial and coronal planes (Figures 25 and 26). Faure (109) also found that a 30 degree inclined axial plane appears to be useful for assessing the integrity of the fetal soft palate (Figure 27). These examples serve to demonstrate the versatility of high quality voxel-based images for providing several options for the analysis of fetal anomalies. It is important to remember that scanning artifacts may lead to misinterpretation of these images. For example, Nelson et al. (110) have reported several artifacts related to both 2DUS artifacts being propagated through the volume and new artifacts related to 3D reconstruction, display and scanning. Jaw Abnormalities An evaluation of the median facial profile can be performed using both multiplanar and rendered displays (Figure 28). The face should be rotated into a standard, anatomic orientation so that the face is symmetrical. 3DUS has been shown to be useful in identifying abnormal profiles such as micrognathia (Figure 29), retrognathia, midface hypoplasia and frontal bossing (Figure 30). Lee and co-workers (111) evaluated 9 cases of micrognathia and found that an oblique plane can lead to misinterpretation of a normal chin to be abnormal, that prominent cheeks (e.g. in diabetic mothers) and retrognathia can lead to an overcall of micrognathia. Evaluation of the fetal mandible can provide important diagnostic clues to the presence of genetic syndromes. By mid-2008, the Online Mendelian Inheritance in Man (OMIM) database cited 328 syndromes for micrognathia (small jaw) and 53 syndromes for retrognathja (posteriorly displaced jaw). From a clinical perspective, these jaw 15 abnormalities can also be associated with obstructed airways and problems with feeding after birth. Toward this end, Rotten and co-workers (112) have described an objective approach for the assessment of abnormal jaw size and position using 3DUS. Micrognathia was defined on the basis of a ratio between the mandibular width (MD) to the maxillary width (MX). Both parameters can be measured on an axial plane, caudal to the cranial base, at the level of the maxillary or mandibular tooth buds. From an axial plane, a line was extended posteriorly, one centimeter from the anterior border of the tooth buds. The MD/MX ratio was obtained from these two measurements (Figure 31). Retrognathia was defined by an inferior facial angle (IFA) that resulted from the crossing of two lines (Figure 32): 1. a ‘reference line’, orthogonal to the vertical part of the forehead, drawn at the level of the synostosis of the nasal bones. 2. A ‘profile line’, joining the tip of the mentum and the anterior border of the more protrusive lip. Their results demonstrated that micrognathia and retrognathia can be distinguished by the methods in this paper. The MD/MX ratio assesses mandible size, whereas, the IFA evaluates mandible position. Although it is possible to obtain these measurements using 2DUS, the Authors believed that 3DUS could be applied more easily for this analysis. Such improvements in our ability to more precisely diagnose congenital abnormalities may translate into improved therapeutic approaches and outcome. Brain Three-dimensional ultrasound images of the embryonic brain (6,9) have offered a fascinating insight into normal and abnormal development of the central nervous system. Similar to 2DUS, however, the fetal brain can be poorly visualized as a result of acoustic shadowing from the bony calvarium during the second and third trimester of pregnancy. A successful sonographic study of the brain often relies on the use of transvaginal sonography through a suitable acoustic window such as the anterior fontanelle. Some of the earliest reports on the use of 3DUS for the diagnosis of fetal brain abnormalities included unilateral megalencephaly, hydrocephalus, anencephaly, holoprosencephaly, Dandy-Walker cyst, enlarged cisterna magna, periventricular leukomalacia, agenesis of the corpus callosum, and cerebellar fusion (113-115). Subsequent investigators have described 3DUS with varying degrees of successful visualization for fetal brain evaluation. One important technique for fetal brain evaluation was originally introduced by Timor-Tritsch (116) as the ‘three-horn view”. This view can be used to demonstrate the anterior, posterior, and inferior horns by either 2DUS or 3DUS scans. This 3D technique requires acquisition of a volume dataset, orthogonal multi-planar display of brain structures, and by rotating or tilting the mid-coronal section to the left or right. The examiner is able to navigate through the volume data for an improved understanding of these anatomic relationships for telemedicine, consultative, and teaching purposes (117). Another approach, the transfrontal view, uses the frontal cranial suture as an acoustic window to examine midline cerebral structures with abdominal 16 3DUS (118). This view was easily obtained in 89 percent of 124 healthy fetuses beween 19 to 24 weeks, menstrual age. Anatomic findings were similar to a median sagittal scan through the anterior fontanelle. The trans-frontal approach can also be used to evaluate the fetal facial profile. Correa et al. (119) prospectively scanned 202 fetuses using abdominal 3DUS between 16 and 24 weeks, menstrual age. Acceptable cerebral multiplanar views were satisfactorily viewed by a sonologist who had expertise in neonatal cranial sonography in 92% of cases. The visualization rate for brain structures are summarized for the “3D multi-planar neuroscan” in Table 2. Pilu and colleagues (120) have also presented a very informative review that demonstrates how they use 3DUS to systematically evaluate the fetal brain. As the imaging resolution and visualization software improved, other investigators have examined the fetal brain as well. Roelfsema and colleages (121) applied the VOCAL technique to document median brain volume that increased from 34 mL at 18 weeks to 316 mL at 34 weeks, menstrual age. This represents a nearly 10-fold increase during the second half of pregnancy. Viñals et al. (122) later applied a thick-slice scanning technique (volume contrast imaging) to describe the normal appearance and dimensions of the fetal cerebellar vermis. Paladini et al. (123) found that posterior fossa abnormalities can usually be characterized using 3DUS on the basis of key findings that include upward displacement of the tentorium, counterclockwise rotation, and vermian hypoplasia of the cerebellum. One group has even described how 3DUS findings over time (i.e. 4D ultrasonography or 4DUS) can be used to assess neurobehaviorial movements of the fetus (124). Roeflsema and co-workers (125) described the normal development of the fetal skull base and found that these measurements were reproducible between examiners. In another study, serial volume measurements of the fetal cerebellum were prospectively acquired in 52 normal pregnant women between 20 and 32 weeks, menstrual age (126). These volume measurements were taken every two weeks as a potential tool for fetal growth evaluation. All of these studies demonstrate the evolving applications of 3DUS for fetal brain assessment. In many cases, the diagnostic results from both 2DUS and 3DUS should be complementary to MRI studies of the fetal brain (127). Spina Bifida The prenatal diagnosis of spina bifida has steadily improved as a result of maternal serum alpha-fetoprotein screening and from the widespread use of ultrasonography. Corresponding advances in patient management have greatly reduced mortality, but have had minimal impact on long-term disability from neurological sequalae. This morbidity includes paraplegia, sensory deficits, spinal deformity, bowel dysfunction, and urinary incontinence. Accurate characterization of spina bifida relies on sonographic recognition of disrupted ossification centers and/or overlying skin from transverse and coronal views of the fetal spine. Sonography predicts the clinical severity of open spina bifida because neurological symptoms correlate with the anatomic level of the defect. Kollias et al. (128) reported that two-dimensional ultrasonography (2DUS) estimated the defect to within one vertebral segment in 79% of fetuses with spina bifida. However, one retrospective study of 171 consecutive cases of spina bifida found that only 29% of cases accurately identified the 17 specific upper level of a spinal lesion using 2DUS (129). Other investigators have proposed that 3DUS may be used to further characterize spina bifida (130-133) Optimal views can be generated by manipulation of a virtual cutting plane through a volume reconstruction of the fetal spine. Lee and colleagues (134) has proposed that 3DUS can be used as a semi-quantitative technique for determining the anatomic level of this lesion. Multi-planar views are acquired using a volume probe from an axial sweep of the fetal spine (Figure 33). A coronal view of the lumbar and sacral spine is rendered with a maximum intensity projection (MIP) algorithm that primarily displays the bony spine. An electronic cutting plane is used to display orthogonal views of the volume-rendered spine, beginning at the spinal segment that is contiguous with the last fetal rib. As the examiner moves the cutting plane towards the sacral spine, simultaneous views of the axial spine and over-lying skin line can be visualized. Other 3DUS techniques can be used to directly render the bony and soft tissue defects (Figures 34-35). Spinal defect levels obtained in this manner closely correlate with findings from both 2DUS and postnatal results. Although multi-planar views are generally more informative than rendered views for localizing these defects, their simultaneous use increases the likelihood that a spinal defect will be appropriately analyzed. This approach may improve the characterization of spina bifida by adding diagnostic information that is complementary to the initial assessment by 2DUS. Skeletal Dysplasias Volume sonography offers an important method that allows the examiner to visualize fetal skeletal structures on the basis of a maximum intensity projection (MIP) technique. This software algorithm displays only the most echogenic structures and it is possible to mix varying degrees of volume-rendered soft tissue for the final output display. Pretorius and Nelson were among the first to use 3DUS to visualize cranial sutures and fontanelles (135) as well as the thoracic skeleton (136). The same group later demonstrated the value of stereoscopic imaging for these 3D reconstructions in order to better visualize fetal bony structures (137). One of the earliest applications of 3DUS for a fetal skeletal abnormality was described in a fetus with platylospondylic lethal chondrodysplasia (138). Yanagihara et al (139) subsequently reported early experiences with a specially developed abdominal 3D transducer for visualizing skeletal structures in 42 normal fetuses and in 3 anencephalic fetuses. Garjian and co-workers (140) reported a small series of fetuses with skeletal dysplasia using this technology.The series included camptomelic dysplasia, thanatophoric dysplasia, ostetogenesis imperfecta, arthrogryposis, and short limbed dysplasia. Surface rendering, volume rotation, and multi-planar displays were especially helpful in 3 of 7 cases, when compared to 2DUS. Multi-planar imaging was helpful for displaying a true median facial profile and volume sonography provided a more global assessment of the skeletal anatomy. The MIP technique made it possible to identify scapular hypoplasia in a fetus with campomelic dysplasia. The added depth perception cues and ability to rotate volume data both facilitated increased appreciation of positional limb anomalies as well as improved visualization of the spine. Another series from Cedars-Sinai Hospital further described diagnostic advantages of 3DUS over 2DUS for additional skeletal dysplasias for evaluating fetuses with facial dysmorphism, relative proportion of appendicular skeletal elements, as well as the hands and feet (141). Benoit (142) provided additional examples 18 of the maximum intensity mode for displaying normal skeletal structures, hemivertebrae, cranial sutures, spina bifida, hand digits, and cranial fontanelles (Figures 36-39). Ruano and colleagues (143) have reported the use of a novel technology, 3D helical computed tomography (CT) for the diagnosis of fetal skeletal anomalies between 27 and 36 weeks, menstrual age. There were three cases of achondroplasia, two cases of osteogenesis imperfecta, Type II, and one case of chondrodysplasia punctata. The correct diagnosis was made in four cases using 2DUS. Both 3DUS and 3D helical CT were used to make the correct diagnosis in all cases. However, 3D helical CT provided an advantage of imaging the entire fetus. E. TISSUE VASCULARIZATION ASSESSMENT Tissue Perfusion Using 3D Vascular Flow Indices 3DUS and the VOCAL technique have been combined to estimate organ tissue perfusion using vascular flow indices (4D View, version 7.0, GE Healthcare, Milwaukee, WI). Pairleitner and co-workers (144) first introduced this approach for quantifying the degree of vascularized tissue in adnexal masses. First, the VOCAL technique is used to define a volume of interest that contains both gray-scale (nonvascular) and color voxels (vascular). The fundamental principle is based on the use of histograms to analyze the ratio of colored voxels to gray-scale voxels in the following manner. 1. VI = vascularization index (standardized range 0 – 100) Number of color voxels in relation to total number of voxels Example: 2. Number of color voxels = 1000 Total number of voxels = 5000 VI = 1000/5000 = 0.2 or 20% FI = flow index (standardized range 0 – 100) Average intensity value of color voxels contained in the volume. Example: 3. 500 color voxels have a very high intensity = 80 500 color voxels have a lower intensity = 20 [(500 * 80) + (500*20)] / 1000 total voxels = FI = 0.50 or 50% VFI = vascularization flow index = (VI *FI)/100 Example: VFI = .2 x .5 = .10 or 10% Several investigators have used vascular flow indices to study gynecologic conditions. Pan et al. (145) studied differences in ovarian stromal flow in patients with polycystic ovarian syndrome. The VI, FI, and VFI were significantly higher in affected women 19 compared with women having normal ovaries. Raine-Fenning and associates (146,147) also examined periodic changes in endometrial development and subendometrial vascularity during the normal menstrual cycle and found significantly reduced 3D vascular flow indices in women with unexplained subfertility. Ng and co-workers (148) found significantly higher endometrial and subendometrial vascularity in pregnant patients with a live birth following in-vitro fertilization using frozen thawed-embryo transfer cycles as compared to these women who experienced miscarriage. Others have applied 3D vascular flow indices to the fetal liver (149), brain (150), kidneys (151), and placenta (152). All flow indices significantly increase over time with advancing pregnancy. Merce and colleagues (153) evaluated the reproducibility of placental vascular flow indices on 30 normal singleton pregnancies from 14 to 40 weeks, menstrual age. All 3D power Doppler vascular indices (VI, FI and VFI) showed a correlation greater than 0.85, with a better intra-observer agreement for the flow indices (FI and VFI). They subsequently described increases of placental vascular flow indices over time (154). Power Doppler settings included a PRF 600 Hz; wall filter 40 Hz; and fixed 35 degree field of view, although the overall gain settings were not reported. The FI, reflecting placental flow, increased in a linear and progressive manner as compared to VI (number of placental vessels) that increased up to the 30th week. The VI maintained a plateau up to the 37th week and decreased afterwards. A few salient points are pertinent to this line of investigation. First, these noninvasive Doppler techniques do not measure true tissue perfusion because this technique would require knowledge regarding how fast blood volume moves through tissue. Secondly, the reproducibility of vascular flow indices is dependent on several technical factors such as system gain, pulse repetition frequency, angle of insonation, wall filter settings, and examiner experience. In this regard, the use of vascular flow indices may be more suited towards gynecological imaging, in which the proximity of the ovaries and endometrium to the transvaginal probe almost eliminates the beam path (146,155). By contrast, the use of standardized ultrasound system settings may not satisfactorily compensate for different beam paths between obstetrical scans because of the signal attenuation that results from insonating intervening tissue at various depths (156,157). In order to address some of these concerns, Rubin and associates (158) have introduced the concept of fractional moving blood volume. In this elegant in-vitro experiment, they used power Doppler ultrasonography to detect moving scatterers in a flow tube as a function of successive dilutions of a blood mimicking perfusate. Power Doppler ultrasonography has advantages over color Doppler methods because of its low noise variance, decreased electronic noise, greater dynamic range, and increased sensitivity to the detection of blood flow. The fractional moving blood volume technique normalizes power Doppler measurements to compensate for signal attenuation and insonation depth. These signal intensities can be compared to similar measurements from the center of a large blood vessel that is used to define the highest value for vascular amplitude scanning. These colored voxels are set to a value of 100% and this normalized data compensates for the attenuation of the Doppler signal through tissue. Fractional moving blood volume has also been shown to correlate well with regional blood flow perfusion on the basis of radioactive microspheres in exteriorized fetal lambs that were exposed to experimentally induced asphyxia (159). This technique also appears to be reproducible in the fetal lung during the third trimester of pregnancy (160). Furthermore, fractional moving 20 blood volume has more recently been used to study regional cerebral blood perfusion in third trimester fetuses (161). Interobserver agreement showed a mean difference of -0.2 (SD 2.7) with 95% limits of agreement ranging from -5.6 to 5.2. Statistically significant differences in fractional moving blood volume were also found between cerebellar and complete sagittal planes of the frontal and basal ganglia regions. Future studies will need to address the role of fractional moving blood volume analysis for standardized 3DUS as well. F. FETAL GROWTH AND WEIGHT ESTIMATION Abnormal fetal growth is associated with a significant proportion of newborn babies that develop postnatal complications. Approximately 8.3 percent of babies are born with low birth weight (< 2,500 gm) in the United States (162). These infants can experience a broad range of problems that include respiratory distress syndrome, intraventricular hemorrhage, patent ductus arteriosus, necrotizing entercolitis, and retinopathy of prematurity. Furthermore, the National Center of Vital Statistics also reports that 10 percent of all live-born infants in this country weigh more than 4,000 grams. The most serious complication of fetal macrosomia is shoulder dystocia during delivery, although clavicular fractures, and brachial plexus injuries from birth trauma also occur (163, 164). Contemporary obstetrical practice has heavily relied on a generalized assessment of fetal nutritional status is based on either estimated weight or only a single abdominal circumference measurement. Fetal weight estimation models typically include the abdominal circumference with some combination of head or limb measurements. However, these fetal growth parameters do not emphasize the degree of soft tissue development. This issue is extremely important because there is mounting evidence that indicates an association between low birth weight and health in later adult life. The Barker Hypothesis has stimulated much interest regarding the fetal origins of adult disease (165). This line of investigation proposes that some fetuses will respond differently to an unfavorable intrauterine environment and that malnourished fetuses will generally respond less favorably to these insults. Epidemiologic studies have found that low birth weight infants are at increased risk for decreased longevity as well as the onset of heart disease, diabetes, chronic renal disease, metabolic syndrome, and neurological sequelae in adult life (165-168). Although many of these studies have been based on low birth weight infants, obstetricians are now challenged with the task of separating fetuses that are small, but otherwise normal from these that are truly malnourished. Early identification of malnourished fetuses could potentially be used to guide timely prenatal intervention, to minimize risk of adverse perinatal outcome, and possibly to reduce the development of health problems in later adult life. Nonetheless, is it possible that 3DUS could provide additional fetal size and growth parameters that will ultimately improve our ability to detect and monitor malnourished fetuses? Several studies have described the early use of 3DUS for measuring fetal limb volume that includes soft tissue assessment (169-174). For example, Chang and colleagues (169) investigated the relationship of fetal thigh volume to birth weight. The thigh volume was measured by manually tracing transverse slices of the thigh at 3 mm intervals, a process that usually took 10-15 minutes to complete for each limb. This information was used to derive the best one-parameter regression model in 100 women who delivered at term gestation. They prospectively compared their results in 50 additional Taiwanese 21 subjects against previously published fetal weight estimation models (175-177). Their new model (birth weight = 1080.87350 + 22.447 x thigh volume) gave the most accurate and precise results when the data was expressed as mean percent differences (1.5 ± 5.6 percent) as compared to the methods of Warsof (-4.2 ± 9.4%), Hadlock (-4.8 ± 9.4%), and Thurnau (-19.2 ± 7.0%). Furthermore, they found no significant differences between the inter- and intra- examiner errors of mean differences among 20 of their subjects. Similar results with only fetal arm volume were prospectively obtained (0.35 ± 4.6%), although no reproducibility testing was performed between examiners (Liang, 1997). German investigators (172) subsequently reported new fetal weight estimation models that combined upper arm and thigh volume measurements with BPD and abdominal volume. The multiple parameter model prospectively yielded a mean percentage error of 1.9 ± 7.6%, as compared to results using the Hadlock model (0.8 ± 9.3%). No information was provided about the time necessary to complete these measurements and only intraobserver reproducibility results were reported. Unfortunately, two major technical limitations have prevented the practical application of soft tissue measurements into obstetrical practice. First, limb volume measurements originally required a series of tedious manual traces around the axial limb from one end of the femur to the other. Secondly, soft tissue borders are often difficult to clearly visualize at either end of the long bone shaft due to acoustic shadowing. This inherent limitation of sonographic imaging can make manual tracing of soft tissue borders difficult from overlying dense tissue. Lee and colleagues (178) addressed these technical concerns by introducing the concept of fractional limb volume (Figure 40). A commercially available software product (4D View, version 7.0, GE Healthcare, Milwaukee, WI) can be used to measure fractional limb volume that is based on an analysis of a mid-section of arm or thigh from a volume dataset (Figure 41). The examiner is able to more rapidly measure soft tissue volume in the center of the limb, where the manual tracings around the soft tissue borders are less likely to be obscured by acoustic shadowing. Manual fractional limb volume measurements take approximately 2 minutes to complete and are reproducible between observers throughout a broad range of pregnancy. A prospective validation study of 55 fetuses (range 390 to 5143 gm) found a greater than 2-fold improvement in the percentage of infants having predicted weight within 5% of actual birth weight, when compared to more conventional 2D parameters alone (179). Fractional limb volume has also been successfully applied to individualized fetal growth assessment using the Rossavik fetal growth model (180,181) (Figures 42-43). Normal values for fractional limb volume and the reproducibility of these measurements have now been reported during pregnancy (182). Another study used air displacement plethysmography for newborn infant body composition to determine which prenatal growth parameters had the greatest correlation to percent body fat (183). Fractional thigh volume (TVol) was the most significant predictor of %BF and this parameter explained 46.1% of the variability in %BF. Actual birth weight similarly explained 44.7% of the variation in %BF. By comparison, abdominal circumference and estimated fetal weight accounted for only 24.8% and 30.4% of the variance in %BF, respectively. Skeletal growth parameters, such as FDL (14.2%), HC (7.9%), and BPD (4.0%), contributed the least towards explaining the variance in %BF (Figure 44). If a major goal of prenatal care is to detect malnourished fetuses, the rationale for using single parameters such as AC, or even EFW, to detect and monitor fetal growth abnormalities may require critical re-examination. However, fractional thigh 22 volume still accounts for no more than one half of the variance in neonatal %BF. Other novel fetal soft tissue parameters must be identified and validated to improve our understanding of soft tissue development and, possibly, the subsequent risk for disease in later life. G. OTHER CONSIDERATIONS Safety Issues The two main bioeffects of ultrasound exposure to fetuses are based on the possibility of thermal effects and mechanical cavitation (184). Many professional organizations encourage the prudent use of diagnostic sonography for medically indicated scans by trained healthcare providers during pregnancy (185). Specific emphasis is placed on the examiner for using acoustic power settings that are as low as reasonably achievable for the acquisition of satisfactory diagnostic images (ALARA principle) with the corresponding use of appropriate output display standards (186). A recent review of this topic suggests that exposure to diagnostic ultrasound does not pose a significant health risk to either the expectant mother or her fetus (184). Sheiner and co-workers (187) have performed a prospective, longitudinal study of three commercially available 3D ultrasound systems to examine the mechanical and thermal indices during pregnancy. Mean thermal indices from volume sonography were comparable to corresponding values resulting from conventional 2D ultrasound scans. However, the mechanical indices for volume acquisitions were significantly lower than observed using 2D b-mode ultrasonography. Parental Bonding It has been known for some time the 2DUS imaging increases bonding between parents and fetuses (188-190). As practitioners began using 3DUS, it appeared that there was an even more obvious recognition of the fetus by parents, particularly images of the fetal face and it appeared that there might be increased bonding between parents and their fetus. Many physicians hoped that an increase in bonding might lead to a decrease in abusive behaviors such as child abuse, spousal abuse, maternal smoking and use of drugs and alcohol however no significant data has yet been published. Several studies have now been published looking at bonding between parents and the fetus after observing 3DUS images of their fetus. Certain subsets of patients appear to benefit more from viewing the images and these include prior anomalies or fetal demise, surrogate parents, hospice patients carrying fatal anomalies, infertility and family history of anomalies (191). In a study of 100 patients, Ji and colleagues (192) looked at 50 patients having undergone 2-D ultrasound and 50 patients having undergone 3-D ultrasound. They found that the patients with 3-D ultrasound shared their photographic images with more people (median 27.5) than those who had 2-D ultrasound (median 11.0). In another study by Pretorius et al (193), 189 patients filled out, both before and after 3DUS imaging, a validated questionnaire modified for pregnant parents and found that bonding had increased. Drawings of fetuses made by parents have been evaluated by two different teams of investigators and appeared to increase bonding after undergoing 3DUS (194,195). It was 23 possible to predict which pictures were drawn before and after the 3DUS examination primarily based on uterine context and positioning of the extremities (195). Parents appear to have a more realistic view of their fetus after seeing three-dimensional ultrasound images. The data regarding bonding is however difficult to assess. Rustico et al (196) found that facial expressions and hand-to-mouth movements were twice as likely after 4DUS in 48 patients (44%) compared to 2DUS in 52 patients (27%). The 4DUS group had more women with positive quality, intensity, and global attachment although this was not statistically significant. In addition, fetal structures and movements visualized were similar between the two groups, as the face was visualizing 83% after 2DUS and 81% after 4DUS. Medicolegal Issues A common question regarding medical legal use of 3DUS is related to whether the volumes should be saved. It is clear that much information is within each data volume and the examination of all data is not feasible for all possible planes. Diagnostic images that are derived from volume data should be recorded as single images and saved. It is not mandatory that volume data sets be saved unless there is a need to archive them for research, consultative, or teaching purposes. This strategy is similar to how MRI and computed tomography data are archived and stored in clinical practice. Ultrasound for Entertainment Patients and medical care providers have various opinions regarding whether parents should be allowed to have 3DUS examinations for bonding alone. The question is whether ultrasound examinations are entertainment or reassurance. 3DUS studies are now being formed in commercial venues as well as pregnancy crisis centers after minimal training, often at two weeks. The medical community is concerned about biohazards of diagnostic ultrasound, including the understanding of power output, risk of Doppler to the early embryo, length of time and frequency of scanning as well as misdiagnosis if performed by non-skilled personnel outside the medical environment. Both the Federal Drug Administration and the American Institute of Ultrasound in Medicine have guidelines recommending that diagnostic ultrasound only be used when there is a medical indication. The AIUM strongly discourages the nonmedical use of ultrasound for psychosocial or entertainment purposes. Physicians have varied opinions regarding the use of ultrasound for reassurance. Dr. Peter Doubilet (197) suggested that to ban or condemn the use of ultrasound for entertainment is inconsistent with our acceptance of many other goods and services that provide enjoyment while carrying a small potential risk. Good examples of the computer, microscope and camera were described that were all initially single use devices and only later were used for many different purposes. This Editorial reminds us that we do not forbid airline travel for pregnant women even though there is a cosmic ray related risk. Noting that our societal approach is to warn mothers rather than to dictate actions, he also states that businesses make it clear that entertainment ultrasound is not a diagnostic medical sonogram. 24 H. EMERGING CONCEPTS Future developments for volume sonography will include faster imaging systems with improved detail resolution in both the original plane of volume acquisition as well as reconstructed planes. Ultrasound volume probes will become smaller and may eventually rely on the use of matrix array probes for real-time imaging, particularly of the fetal heart. New software applications will allow us to analyze and quantify volume data in ways that are currently not possible and the efficiency of clinical workflow will also be improved with automated algorithms. It may eventually become practical to interactively explore fourdimensional volume data for the moving fetus within a virtual environment. This type of “virtual ultrasound simulation” would allow improved depth perception and allow joint discussion with colleagues for telemedicine applications, research, and training (198200). I. CONCLUSIONS Volume sonography is an important complementary diagnostic technique to conventional 2D imaging (201). In this chapter, we have presented a perspective of the current medical literature with our extensive experiences in this area. Remember that 3DUS is not just one method, but it is based on a combination of several image visualization tools that must be customized to answer the pertinent clinical questions being asked. This technology can be used to improve diagnostic confidence as part of your problem-solving process. Three-dimensional ultrasonography is still in its infancy as software tools become more sophisticated and as we begin to apply these versatile capabilities for a wide variety of clinical problems. Health care providers should be aware of these emerging capabilities and their potential applications. Key Points 3DUS uses several different types of image analysis techniques that are based on the acquisition, processing, and manipulation of volume pixels (voxels). 2DUS and 3DUS are complementary diagnostic imaging modalities. 2DUS should be used to make an initial diagnostic impression and clinical judgment will determine if there is likely to be a clinical advantage for the application of 3DUS. Match the 3DUS technique with a specific clinical question that is being asked. Do not underestimate the diagnostic value of 3D multi-planar imaging. Good two-dimensional imaging is likely to translate to satisfactory 3D volume acquisitions. 25 References 1. Gonçalves LF, Lee W, Espinoza J, Romero R. Three- and 4-dimensional ultrasound in obstetric practice – does it help? J Ultrasound Med. 2005;24:15991624. 2. Gonçalves LF, Nien JK, Espinoza J, Kusanovic JP, Lee W, Swope B, Soto E, Treadwell MC, Romero R. What does 2-dimensional imaging add to 3- and 4dimensional obstetric ultrasonography. J Ultrasound Med. 2006;25:691-9. 3. Timor-Tritsch IE, Bashiri A, Monteagudo A, Arslan AA. Qualified and trained sonographers in the US can perform early fetal anatomy scans between 11 and 14 weeks. Am J Obstet Gynecol. 2004;191:1247-1252. 4. Souka AP, Pilalis, A, Kavalakis I, Antsaklis P, Papantoniou N, Mesogitis S, Antsaklis A. Screening for major structural abnormalities at the 11- to 14-week ultrasound scan. Am J Obstet Gynecol. 2006;194;393-396. 5. Weiner Z, Goldstein I, Bombard A, Applewhite L, Itzkovits-Eldor J. Screening for structural fetal anomalies during the nuchal translucency ultrasound examination. Am J Obstet Gynecol. 2007;197:181.e1-5. 6. Blaas HG, Eik-Nes SH, Breg S, Torp H. In-vivo three-dimensional ultrasound reconstructions of embryos and early fetuses. Lancet. 1998;352:182-185. 7. Hata T, Aoki S, Manabe A, Hata K, Miyazaki K. Three-dimensional ultrasonography in the first trimester of human pregnancy. Human Reproduction. 1997;12:1800-1804. 8. Hata T, Manabe A, Aoki S, Miyazaki K, Yoshino K, Yamamoto K. Threedimensional intrauterine sonography in the early first-trimester of human pregnancy: preliminary study. Human Reproduction.1998;13:740-743. 9. Benoit B, Hafner T, Kurjak A, Kupesic S, Bekavac I, Bozek T. Three-dimensional sonoembryology. J Perinat Med. 2002;30:63-73. 10. Kim MS, Jeanty P, Turner C, Benoit B. Three-dimensional sonographic evaluations of embryonic brain development. J Ultrasound Med. 2008;27:119-124. 11. Bonilla-Musoles F, Raga F, Bonilla F Jr, Blanes J, Osborne NG. Early diagnosis of conjoined twins using two-dimensional color Doppler and three-dimensional ultrasound. J Natl Med Assoc. 1998;90:552-556. 12. Bega G, Wapner R, Lev-Toaff A, Kuhlman K. Diagnosis of conjoined twins at 10 weeks using three-dimensional ultrasound: a case report. Ultrasound Obstet Gynecol. 2000;16:388-390. 26 13. Kuroda K, Kamei Y, Kozuma S, Kikuchi A, Fujii T, Unno N, Baba K, Taketani Y. Prenatal evaluation of cephalopagus conjoined twins by means of three-dimensional ultrasound at 13 weeks of pregnancy. Ultrasound Obstet Gynecol. 2000;16:264-266. 14. Blaas HG, Blaas K, Eik-Nes SH, Vogt Isaksen C. The detection of spina bifida before 10 gestational weeks using two- and three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2000;16:25-29. 15. Blaas HG, Eik-Ness SH, Vainio T, Vogt Isaksen, C. Alobar holoprosencephaly at 9 weeks gestational age visualized by two- and three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2000;15:62-65. 16. Lee G, Hur YS, Shin JC, Kim SP, Kim SJ. Case Report. Prenatal diagnosis of holoprosencephaly with ethmocephaly via 3-dimensional sonography. J Clin Ultrasound. 2006;36:306-308. 17. Tonni G, Centini G. Three-dimensional first-trimester transvaginal diagnosis of alobar holoprosencephaly associated with omphalocele in a 46,XX fetus. Am J Perinatol. 2006;23:67-69. 18. Tonni G, Ventura A, Centini G, De Felice C. First trimester three-dimensional transvaginal imaging of alobar holoprosencephaly associated with proboscis and hypotelorism (ethmocephaly) in a 46,XX fetus. Congenit Anom (Kyoto). 2008;48: 5155. 19. Van Keirsbilck J, Cannie M, Robrechts C, de Favel T, Dymarkowski S, Van den Bosch T, Van Schoubroeck D. First trimester diagnosis of sirenomelia. Prenat Diagn. 2006;26:684-688. 20. Roman AS, Monteagudo A, Timor-Tritsch I, Rebarber A. First-trimester diagnosis of sacrococcygeal teratoma: the role of three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2004;23:612-614. 21. Souka AP, Pilalis A, Kavalakis I, Antsaklis P, Papantoniou N, Mesogitis S, Antsaklis A. Screening for major structural abnormalities at the 11- to 14-week ultrasound scan. Am J Obstet Gynecol 2006;194:393-6. 22. Michailidis GD, Papageorgiou P, Economides D L. Assessment of fetal anatomy in the first trimester using two- and three-dimensional ultrasound. Br J Radiol. 2002; 75:215-219. 23. Fauchon DEV, Benzie RJ, Wye DA, Cairns DR. What information on fetal anatomy can be provided by a single first-trimester transabdominal three-dimensional sweep? Ultrasound Obstet Gynecol. 2008;31:266-270. 24. Kurjak A, Kupesic S, Ivanciś-Kosuta M. Three-dimensional transvaginal ultrasound improves measurement of nuchal translucency. J Perinat Med.1999; 27:97-102. 27 25. Chung BL, Kim HJ, and Lee KH. The application of three-dimensional ultrasound to nachal translucency measurement in early pregnancy (10-14 weeks): a preliminary study. Ultrasound Obstet Gynecol. 2000;15:122-125. 26. Eppel W, Worda C, Frigo P, Lee A. Three- versus two-dimensional ultrasound for nuchal translucency thickness measurements: comparison of feasibility and levels of agreement. Prenat Diagn. 2001;7:596-601. 27. Paul C, Krampl E, Skentou C, Jurkovic D, Nicolaides KH. Measurement of fetal nuchal translucency thickness by three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2001;18:481-484. 28. Clementschitsch G, Hasenőhrl G, Schaffer H, Steiner H. Comparison between two- and three-dimensional ultrasound measurements of nuchal translucency. Ultrasound Obstet Gynecol. 2001;18:475-480. 29. Worda C, Radner G, Lee A, Eppel W. Three-dimensional ultrasound for nuchal translucency thickness measurements: comparison of transabdominal and transvaginal ultrasound. J Soc Gynecol Investig. 2003;10:361-5. 30. Shipp TD, Bromley B, Benacerraf B. Is 3-dimensional volume sonography an effective alternative method to the standard 2-dimensional technique of measuring the nuchal translucency? Journal of Clinical Ultrasound. 2006;34:118-122. 31. Cicero S, Avgidou K, Rembouskos G, Kagan KO, Nicolaides KH. Nasal bone in first-trimester screening for trisomy 21. Am J Obstet Gynecol. 2006;195:109-114. 32. Prefumo F, Sairam S, Bhide A, Thilaganathan B. First-trimester nuchal translucency, nasal bones, and trisomy 21 in selected and unselected populations. Am J Obstet Gynecol. 2006;194:828-33. 33. Sonek J, Borenstein M, Downing C, McKenna D, Neiger R, Croom C, Genrich T, Nicolaides KH. Frontomaxillary facial angles in screening for trisomy 21 at 14-23 weeks’ gestation. Am J Obstet Gynecol. 2007;197:160.e1-160e5. 34. Cicero S, Dezerega V, Andrade E, Scheier M, Nicolaides KH. Learning curve for sonographic examination of the fetal nasal bone at 11-14 weeks. Ultrasound Obstet Gynecol. 2003;22:135-137. 35. Malone FD, Ball RH, Nyberg DA, Comstock CH, Saade G, Berkowitz RL, Dugoff L, Craigo SD, Carr SR, Wolfe HM, Tripp T, D’Alton ME. First-trimester nasal bone evaluation for aneuploidy in the general population. Am J Obstet Gynecol. 2004; 104:1222-1228. 36. Rembouskos G, Cicero S, Longo D, Vandecruys H, Nicolaides KH. Assessment of the fetal nasal bone at 11-14 weeks of gestation by three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2004;23:232-236. 28 37. Gonçalves LF, Espinoza J, Lee W, Romero R. Letters to the Editor. Should the Frontal bone be visualized in midline sagittal views of the facial profile to assess the fetal nasal bones during the first trimester? Ultrasound Obstet Gynecol. 2005; 25: 9094. 38. Peralta CFA, Falcon O, Wegrzyn P, Faro C, Nicolaides KH. Assessment of the gap between the fetal nasal bones at 11 to 13 + 6 weeks of gestation by threedimensional ultrasound. Ultrasound Obstet Gynecol. 2005;25:464-467. 39. Gonçalves LF, Espinoza J, Lee W, Schoen ML, Devers P, Mazor M, Chaiworapongsa T, DeVore GR, Romero R. Phenotypic characteristics of absent and hypoplastic nasal bones in fetuses with down syndrome – description by 3dimensional ultrasonography and clinical significance. J Ultrasound Med. 2004;23:1619-1627. 40. Cusick W, Shevell T, Duchan LS, Lupinacci CA, Terranova J, Crombleholme WR. Likelihood ratios for fetal trisomy 21 based on nasal bone length in the second trimester: how best to define hypoplasia? Ultrasound Obstet Gynecol. 2007;30:271274. 41. Benoit B, Chaoui R. Three-dimensional ultrasound with maximal mode rendering: a novel technique for the diagnosis of bilateral or unilateral absence or hypoplasia of nasal bones in second-trimester screening for Down syndrome. Ultrasound Obstet Gynecol. 2005;25:9-24. 42. Sonek J, Borenstein M, Dagklis T, Persico N, Nicolaides KH. Frontomaxillary facial angle in fetuses with trisomy 21 at 11 – 136 weeks. Am J Obstet Gynecol 2007;169; 271e1-271e4. 43. Plasencia W, Dagklis T, Sotiriadis A, Borenstein M, Nicolaides KH. Frontomaxillary facial angle at 11 + 0 13 + 6 weeks’ gestation – reproducibility of measurements. Ultrasound Obstet Gynecol. 2007;29:18-21. 44. Borenstein M, Persico N, Kaihura C, Sonek J, Nicolaides KH. Frontomaxillary facial angle in chromosomally normal fetuses at 11 + 0 to 13 + 6 weeks. Ultrasound Obstet Gynecol. 2007;30:737-741. 45. Borenstein M, Persico N, Dagklis T, Faros E, Nicolaides KH. Frontomaxillary facial angle in fetuses with trisomy 13 at 11 + 0 to 13 +6 weeks. Ultrasound Obstet Gyncol. 2007;30:819-823. 46. Borenstein M, Persicu N, Kagan KO, Gazzoni A, Nicolaides KH. Frontomaxillary facial angle in screening for trisomy 21 at 11 + 0 to 13+ 6 weeks. Ultrasound Obstet Gynecol. 2008;32:5-11. 47. Molina F, Persico N, Borenstein M, Sonek J, Nicolaides KH. Frontomaxillary facial angle in trisomy 21 fetuses at 16-24 weeks of gestation. Ultrasound Obstet Gynecol. 2008;31:384-387. 29 48. Kliewer MA, Hertzberg BS, Freed KS, DeLong DM, Kay HH, Jordan SG, PetersBrown TL, NcNaly PJ. Dysmorphologic features of the fetal pelvis in Down syndrome: prenatal sonographic depiction and diagnostic implications of the iliac angle. Radiology.1996;201:681-684. 49. Shipp TD, Bromley B, Lieberman E, Benacerraf BR. The iliac angle as a sonographic marker for down syndrome in second-trimester fetuses,.Obstet Gynecol 1997;89:446-450. 50. Bork MD, Egan JFX, Cusick W, Borgida AF, Winston AC, Rodis JF. Iliac wing angle as a marker for trisomy 21 in the second trimester. Obstet Gynecol 1997;89:734-737. 51. Shipp TD, Bromley B, Lieberman E, Benacerraf BR. The second-trimester fetal iliac angle as a sign of Down’s syndrome. Ultrasound Obstet Gynecol. 1998;12:1518. 52. Grangé G, Thoury A, Dupont J, Pannier E, LeRhun F, Goussot SM, Goffinet F, Cabrol D. Sonographic measurement of the fetal iliac angle cannot be used alone as a marker for trisomy 21. Fetal Diagn Ther. 2000;15:373-374. 53. Massez A, Rypens R, Metens T, Donner C, Avni F. The iliac angle: a sonographic marker of trisomy 21 during the midtrimester: dependency of fetal lying? Eur Radiol. 2003;13:2075-2081. 54. Lee W, Blanckaert K, Bronsteen RA, Huang R, Romero R. Fetal iliac angle measurements by three-dimensional sonography. Ultrasound Obstet Gynecol. 2001; 18:150-154. 55. Falcon O, Peralta CFA, Cavoretto P, Auer M, Nicolaides KH. Fetal trunk and head volume in chromosomally abnormal fetuses at 11 + 0 to 12 + 6 weeks gestation. Ultrasound Obstet Gynecol. 2005;26:517-520. 56. Falcon O, Cavoretto P, Peralta CFA, Csapo B, Nicolaides KH. Fetal head-to-trunk volume ratio in chromosomally abnormal fetuses at 11 + 0 to 13 + 6 weeks of gestation. Ultrasound Obstet Gynecol. 2005;26:755-760. 57. Benacerraf BR, Benson CB, Abuhamad AZ, Copel JA, Abramowicz JS, DeVore GR, Doubilet PM, Lee W, Lev-Toaff AS, Merz E, Nelson TR, O’Neill M, Parsons AK, Platt LD, Pretorius DH, Timor-Tritsch IE. Three- and 4-dimensional ultrasound in obstetrics and gynecology. J Ultrasound Med. 2005;24:1587-1597. This document was developed as part of Consensus Development meeting that was sponsored by the American Institute of Ultrasound in Medicine. 58. Benacerraf BR, Shipp TD, Bromley B. How sonographic tomography will change the face of obstetric sonography. J Ultrasound Med. 2005;24:371-378. 59. Abuhamad A. Automated multiplanar imaging – a novel approach to ultrasonography. J Ultrasound Med. 2004;23:573-576. 30 60. Espinoza J, Kusanovic JP, Goncalves LF, Nien JK, Hassan S, Lee W, Romero R. A novel algorithm for comprehensive fetal echocardiography using 4-dimensional ultrasonography and tomographic imaging. J Ultrasound Med. 2006;25:947-956. 61. Rizzo G, Capponi A, Cavicchioni O, Vendola M, Pietrolucci ME, Arduini D. Application of automated sonography on 4-dimensonal volumes of fetuses with transposition of the great arteries. J Ultrasound Med. 2008;27:771-776. 62. Abuhamad A, Falkensammer P, Reichartseder F, Zhao Y. Automated retrieval of standard diagnostic fetal cardiac ultrasound planes in the second trimester of pregnancy: a prospective evaluation of software. Ultrasound Obstet Gynecol. 2008; 31:30-36. 63. Nelson T, Pretorius DH, Lev-Toaff A, Bega G, Budorick N, Hollenbach K, Needleman L. Feasibility of performing a virtual patient examination using threedimensional ultrasonographic data acquired at remote locations. J Ultrasound Med 2001;20:941-952. 64. Michailidis GD, Simpson JM, Karidas C, Economides DL. Detailed threedimensional fetal echocardiography facilitated by an Internet link. Ultrasound Obstet Gynecol. 2001;18:325-328. 65. Viñals F, Mandujano L, Vargas G, Giuiano A. Prenatal diagnosis of congenital heart disease using four-dimensional spatio-temporal image correlation (STIC) telemedicine via an internet link: a pilot study. Ultrasound Obstet Gynecol. 2005; 25: 25-31. 66. Viñals F, Ascenzo R, Naveas R, Huggon I, Giuliano A. Fetal echocardiography at 11 +0 to 123 +6 weeks using four-dimensional spatiotemporal image correlation telemedicine via an Internet link: a pilot study. Ultrasound Obstet Gynecol. 2008;31:633-8. 67. Lee SM, Park SK, Shim SS, Jun JK, Park JS, Syn HC. Measurement of fetal urine production by three-dimensional ultrasonography in normal pregnancy. Ultrasound Obstet Gynecol. 2007;30:281-286. 68. Peixoto-Filho FM, Sá RA, Lopes LM, Velarde LG, Marchiori E, Ville Y. Threedimensional ultrasound fetal urinary bladder volume measurement: reliability of rotational (VOCAL) technique using different steps of rotation. Arch Gynecol Obstet. 2007;276:345-349. 69. Yamamoto M, Essaoui M, Nasr B, Malek N, Takahashi Y, Moreira R, Ville Y. Three-dimensional sonographic assessment of fetal urine production before and after surgery in twin-to-twin transfusion syndrome. Ultrasound Obstet Gynecol. 2007;30:972-976. 70. Pretorius DH, Nelson TR. Fetal face visualization using three-dimensional ultrasonography. J Ultrasound Med. 1995;14:349-56. 31 71. Devonald KJ, Ellwood DA, Griffiths KA, Kossoff G, Gill RW, Kadi AP, Nash DM, Warren PS, Davis W, Picker R. Volume imaging: three-dimensional appreciation of the fetal head and face. J Ultrasound Med. 1995;14:919-25. 72. Hata T, Yonehara T, Aoki S, Manabe A, Hata K, Miyazaki K. Three-dimensional sonographic visualization of the fetal face. AJR Am J Roentgenol.1998;170:481-3. 73. Pretorius DH, House M, Nelson TR, Hollenbach KA. Evaluation of normal and abnormal lips in fetuses: comparison between three- and two-dimensional sonography. AJR Am J Roentgenol.1995;165:1233-7. 74. Merz E, Weber G, Bahlmann F, Miric-Tesanic D. Application of transvaginal and abdominal three-dimensional ultrasound for the detection or exclusion of malformations of the fetal face. Ultrasound Obstet Gynecol. 1997;9:237-43. 75. Merz E, Miric-Tesanic D, Welter C. Value of the electronic scalpel (cut mode) in the evaluation of the fetal face. Ultrasound Obstet Gynecol. 1997;16:564-8. 76. McGahan M, Ramos G, Landry C, Sowell B, Wolfson T, D'Agostini D, Patino C, Nelson T, Pretorius D. Multislice display of the fetal face using 3-D ultrasound. J Ultrasound Med, in press. 77. Rotten D, Levaillant JM. Two- and three-dimensional sonographic assessment of the fetal face. 1. A systematic analysis of the normal face. Ultrasound Obstet Gynecol. 2004;23:224-231. 78. Sase, M, Hasegawa K, Honda R, Sumie M, Nakata M, Sugino N, Furukawa S. Ultrasonographic findings of facial dysmorphism in Wolf-Hirschhorn Syndrome. Am J Perinatol. 2005;22;99-102. 79. Lee G, Hur S, Shin J, Kim S, Kim S. Prenatal diagnosis of holoprosencephaly with ethmocephaly via 3-dimensional sonography. J Clin Ultrasound. 2006;34:306-8. 80. Tonni G, Ventura A, Centini G, De Felice C. First trimester three-dimensional transvaginal imaging of alobar holoprosencephaly associated with proboscis and hypotelorism (ethmocephaly) in a 46,XX fetus. Congenit Anom. 2008;48:51-5. 81. Chmait RH, Pretorius DH, Hull AD. Picture of the month. Ultrasound Obstet Gynecol. 2002;20:417-418. 82. Chmait R, Pretorius D, Jones M, Hull R, James G, Nelson T, Moore T. Prenatal evaluation of facial clefts with two dimensional and adjunctive three dimensional ultrasonography: A prospective trial. Am J Obstet Gynecol. 2002;187:946-9. 83. Sepulveda W, Wojakowski AB, Elias D, Otaño L, Gutierrez J. Congenital dacryocystocele – prenatal 2- and 3-dimensional sonographic findings. J Ultrasound Med. 2005;24:225-230. 32 84. Petrikovsky BM, Kaplan GP. Fetal dacryocystocele: comparing 2D and 3D imaging – Letter to the Editor. Pediatri Radiol. 2003;33:582-583. 85. Shih JC, Shyu MK, Lee CN, Wu CH, Lin GJ, Hsieh FJ. Antenatal depiction of the fetal ear with three-dimensional ultrasonography. Obstet Gynecol 1998;91:500-505. 86. Chang CH, Chang FM, Yu CH, Liang RI, Ko HC, Chen HY. Fetal ear assessment and prenatal detection of aneuploidy by the quantitative three-dimensional ultrasonography. Ultrasound Med Biol. 2000; 26:743-749. 87. Hsu TY, Hsu JJ, Chang SY, Chang MS. Letters to the Editor – Prenatal threedimensional sonographic images associated with Treacher Collins syndrome. Ultrasound Obstet Gynecol. 2002;19:413-422. 88. Tanaka Y, Miyazaki T, Kanenishi K, Tanaka H, Yanagihara T, Hata T. Antenatal three-dimensional sonographic features of Treacher Collins syndrome. Ultrasound Obstet Gynecol 2002;19:414-5. 89. Chaoui R, Levaillant JM, Benoit B, Faro C, Wegrzyn P, Nicolaides KH. Threedimensional sonographic description of abnormal metopic suture in second- and third-trimester fetuses. Ultrasound Obstet Gynecol 2005;26:761-764. This key article demonstrates congenital anomalies of the metopic sutures using 3DUS that have not been made previously using 2DUS. 90. Pretorius DH, Nelson TR. Prenatal visualization of cranial sutures and fontanelles with three-dimensional ultrasonography. J Ultrasound Med. 1994;13:871-876. 91. Dikkeboom CM, Roelfsema NM, Van Adrichem LNA, Wladimiroff JW. The role of three-dimensional ultrasound in visualizing the fetal cranial sutures and fontanels during the second half of pregnancy. Ultrasound Obstet Gnecol. 2004;24:412-416. 92. Faro C, Benoit B, Wegrzyn P, Chaoui R, Nicolaides KH. Three-dimensional sonographic description of the fetal frontal bones and metopic suture. Ultrasound Obstet Gynecol. 2005;26:618-621. 93. Faro C, Wegrzyn P, Benoit B, Chaoui R, Nicolaides KH. Metopic suture in fetuses with holoprosencephaly at 11 + 0 to 13 + 6 weeks of gestation. Ultrasound Obstet Gynecol. 2006;27:162-166. 94. Faro C, Wegrzyn P, Benoit B, Chaoui R, Nicolaides KH. Metopic suture in fetuses with trisomy 21 at 11 + 0 to 13 + 6 weeks of gestation. Ultrasound Obstet Gynecol. 2006;27:286-289. 95. Faro C, Chaoui R, Wegrzyn P, Levaillant JM, Benoit B, Nicolaides KH. Metopic suture in fetuses with Apert syndrome at 22-27 weeks of gestation. Ultrasound Obstet Gynecol. 2006;27:28-33. 33 96. Sivertsen Å, Wilcox A, Johnson GE, Åbyholm F, Vindenes HA, Lie RT. Prevalence of major anatomic variations in oral clefts. Plast Reconstr Surg. 2008;121:587-595. 97. Offerdal K, Jebens N, Syvertsen T, Blaas HG, Johansen OJ, Eik-Nes SH. Prenatal Ultrasound detection of facial clefts: a prospective study of 49,314 deliveries in a non-selected population in Norway. Ultrasound Obstet Gynecol. 2008;31:639646. 98. Chmait R, Pretorius D, Moore T, Hull A, James G, Nelson T, Jones M. Prenatal detection of associated anomalies in fetuses diagnosed with cleft lip with or without cleft palate in utero. Ultrasound Obstet Gynecol. 2006;27:173-176. 99. Lee W, Kirk JS, Shaheen KW, Romero R, Hodges AN, Comstock CH. Fetal cleft lip and palate detection by three-dimensional ultrasonography. Ultrasound Obstet Gynecol. 2000;16:314-320. 100. Rotten D, Levaillant JM. Two-and three-dimensional sonographic assessment of the fetal face. 2. Analysis of cleft lip, alveolus and palate. Ultrasound Obstet Gynecol. 2004;24:402-411. 101. Johnson DD, Pretorius DH, Budorick NE, Jones MC, Lou KV. Fetal lip and primary palate: three-dimensional versus two-dimensional US. Radiology. 2000;217:236-239. 102. Chmait R, Pretorius D, Jones M, Hull A, James G, Nelson T, Moore T. Prenatal evaluation of facial clefts with two-dimensional and adjunctive three-dimensional ultrasonography. Am J Obstet Gynecol. 2002;187;946-9. 103. Wang LM, Leung KY, Tang M. Prenatal evaluation of facial clefts by threedimensional extended imaging. Prenat Diagn. 2007;27:722-729. 104. Campbell S, Lees C, Moscoso G, Hall P. Ultrasound antenatal diagnosis of cleft palate by a new technique: the 3D ‘reverse face’ view. Ultrasound Obstet Gynecol. 2005;25:12-18. 105. Campbell S. Prenatal ultrasound examination of the secondary palate. Ultrasound Obstet Gynecol. 2007;29:124-7. This Editorial reviews the current state of knowledge regarding visualization of the fetal hard palate. 106. Platt LD, DeVore GR, Pretorius DH. Improving cleft palate/cleft lip antenatal diagnosis by 3-dimensional sonography – the “flipped face” view. J Ultrasound Med. 2006;25:1423-1430. 34 107. Faure JM, Captier G, Bäumler M, Boulot P. Sonographic assessment of normal fetal palate using three-dimensional imaging: a new technique. Ultrasound Obstet Gynecol. 2007;29:159-165. This study describes how 3DUS can be used to examine the normal fetal posterior palate by correlating these images with anatomic specimens. 108. Pilu G, Segata M. A novel technique for visualization of the normal and cleft fetal secondary palate: angled insonation and three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2007;29:166-169. 109. Faure JM, Bãumler M, Boulot P, Bigorre M, Captier G. Prenatal assessment of the normal fetal soft palate by three-dimensional ultrasound examination: is there an objective technique? Ultrasound Obstet Gynecol. 2008;31:652-656. 110. Nelson TR, Pretorius DH, Hull A, Riccabona M, Sklandsky MD, James G. Sources and impact of artifacts on clinical three-dimensional ultrasound imaging. Ultrasound Obstet Gynecol 2000;16:374-383. 111. Lee W, McNie B, Chaiworapongsa T, Conoscenti G, Kalache K, Vettraino IM, Romero R, Comstock CH. Three-dimensional ultrasonographic presentation of micrognathia. J Ultrasound Med. 2002; 21: 775-781. 112. Rotten D, Levaillant JM, Martinez H, Ducou Le Pointe H, Vicaut É. The fetal mandible: a 2D and 3D sonographic approach to the diagnosis of retrognathia and micrognathia. Ultrasound Obstet Gynecol. 2002;19:122-130. The medical literature includes many scientific studies that do not clearly differentiate micrognathia from retrognathia. In this article, Rotten and coworkers describe new ways to characterize these abnormalities by using inferior facial angle and the mandibular to maxillary width ratio. 113. Hafner E, Bock W, Zoder G, Schuchter K, Rosen A, Plattner M. Prenatal diagnosis of unilateral megalencephaly by 2D and 3D ultrasound: a case report. Prenat Diagn. 1999;19:159-62. 114. Hata T, Yanagihara T, Matsumoto M, Hanaoka U, Ueta M, Tanaka Y, Kanenishi K, Kuno A, Yamashiro C, Ohnishi Y, Tanaka H, Hayashi K. Three-dimensional sonographic features of fetal central nervous system anomaly. Acta Obstet Gynecol Scand. 2000;79:635-639. 115. Pooh RK, Pooh KH, Nakagawa Y, Nishida S, Ohno Y. Clinical application of threedimensional ultrasound in fetal brain assessment. Croat Med J. 2000;41:245-251. 116. Timor-Tritsch IE, Monteagudo A, Mayberry P. Three-dimensional ultrasound evaluation of the fetal brain: the three horn view. Ultrasound Obstet Gynecol. 2000; 16:302-306. 35 117. Monteaqudo A, Timor-Tritsch ID, Mayberry P. Three-dimensional transvaginal neurosonography of the fetal brain: “navigating” in the volume scan. Ultrasound Obstet Gynecol. 2000;16:307-313. 118. Visentin A, Pilu G, Falco P, Bovicelli L. The transfrontal view: a new approach to the visualization of the fetal midline cerebral structures. J Ultrasound Med. 2001;20: 329-33. 119. Correa FF, Lara C, Bellver J, Remohi J, Pellicer A, Serra V. Examination of the fetal brain by transabdominal three-dimensional ultrasound: potential for routine neurosonographic studies. Ultrasound Obstet Gynecol. 2006;27:503-508. 120. Pilu G, Ghi T, Carletti A, Segata M, Perolo A, Rizzo. Three-dimensional ultrasound examination of the fetal central nervous system. Ultrasound Obstet Gynecol. 2007; 30:233-245. Dr. Pilu and colleagues provide useful examples of how 3DUS can be systematically applied to the fetal brain evaluation. 121. Roelfsema NM, Hop WCJ, Boito SME, Wladimiroff JW. Three-dimensional sonographic measurement of normal fetal brain volume during the second half of pregnancy. Am J Obstet Gynecol. 2004;190:275-280. 122. Viñals F, Muñoz M, Naveas R, Giuliano A. Transfrontal three-dimensional visualization of midline cerebral structures. Ultrasound Obstet Gynecol. 2007;30:162168. 123. Paladini D, Volpe P. Posterior fossa and vermian morphometry in the characterization of fetal cerebellar abnormalities: a prospective three-dimensional ultrasound study. Ultrasound Obstet Gynecol. 2006;27:482-489. 124. Kurjak A, Miskovic B, Stanojevic M, Amiel-Tison C, Ahmed B, Azumendi G, Vasilj O, Andonotopo W, Turudic T, Salihagic-Kadic A. New scoring system for fetal neurobehavior assessed by three- and four-dimensional sonography. J Perinat Med. 2008; 36: 73-81. 125. Roelfsema NM, Grijseels EW, Hop WC, Wladimiroff JW. Three-dimensional sonography of prenatal skull base development. Ultrasound Obstet Gynecol. 2007;29:372-7. 126. Araujo Júnior E, Pires CR, Nardozza LM, Filho HA, Moron AF. Correlation of the fetal cerebellar volume with other fetal growth indices by three-dimensional ultrasound. J Matern Fetal Neonatal Med. 2007;20:581-587. 127. Sanz-Cortes M, Raga F, Leon JL, Sniderman A, Bonilla-Musoles F. MRI and multiplanar 3D ultrasound compared in the prenatal assessment of enlarged posterior fossa. J. Perinat. Med. 2007;35:422-424. 36 128. Kollias SS, Goldstein RB, Cogen PH, Filly RA. Prenatally detected myelomeningoceles: sonographic accuracy in estimation of the spinal level. Radiology. 1992;185:109-112. 129. Bruner JP, Tulipan N, Dabrowiak ME, Luker KS, Walters K, Burns P, Reed G. Upper level of the spina bifida defect: how good are we? Ultrasound Obstet Gynecol. 2004; 24:612-617. 130. Mueller GM, Weiner CP, Yankowitz J. Three-dimensional ultrasound in the evaluation of fetal head and spine anomalies. Obstet Gynecol 1996;88:372-378. 131. Riccabona M, Johnson D, Pretorius DH, Nelson TR. Three dimensional ultrasound: display modalities in the fetal spine and thorax. Eur J Radiol. 1996;22:141-145. 132. Johnson DD, Pretorius DH, Riccabona M, Budorick N.E, Nelson TR. Threedimensional ultrasound of the fetal spine. Obstet & Gynecol. 1997;89:434-438. 133. Leung KY, Nqai CS, Chan BC, Leung WC, Lee CP, Tang MH. Three-dimensional extended imaging: a new display modality for three-dimensional ultrasound examination. Ultrasound Obstet Gynecol. 2005;26:244-51. 134. Lee W, Chaiworapongsa T, Romero R, Williams R, McNie B, Johnson A, Treadwell M, Comstock CH. A diagnostic approach for the evaluation of spina bifida by three-dimensional ultrasonography. J Ultrasound Med. 2002;21:619-626. Simultaneous examination of 3D multi-planar and rendered views of the fetal spine are very useful for helping the examiner localize the anatomic level of the lesion. This information can be used to counsel parents about what functional disabilities can be expected after birth. 135. Pretorius DH, Nelson TR. Prenatal visualization of cranial sutures and fontanelles with three-dimensional ultrasonography. J Ultrasound Med. 1994;13:871-6. 136. Nelson TR, Pretorius DH. Visualization of the fetal thoracic skeleton with threedimensional sonography: a preliminary report. AJR Am J Roentgenol. 1995;164:1485-8. 137. Nelson TR, Ji EK, Lee JH, Bailey MJ, Pretorius DH. Stereoscopic evaluation of fetal bony structures. J Ultrasound Med. 2008;27:15-24. 138. Steiner H, Spitzer D, Weiss-Wichert PH, Graf AH Staudach A. Three-dimensional ultrasound in prenatal diagnosis of skeletal dysplasia. Prenat Diagn. 1995;15:373373. 139. Yanagihara T, Hata T. Three-dimensional sonographic visualization of fetal skeleton in the second trimester of pregnancy. Gynecol Obstet Invest. 2000;49:12-16. 37 140. Garjian KV, Pretorius DH, Budorick NE, Cantrell CJ, Johnson DD, Nelson TR. Fetal skeletal dysplasia: three-dimensional US – initial experience. Radiology. 2000;214: 717-723 141. Krakow D, Williams J 3rd, Poehl M, Rimoin DL, Platt LD. Use of three-dimensional ultrasound imaging in the diagnosis of prenatal-onset skeletal dysplasias. Ultrasound Obstet Gynecol. 2003;21:467-472. 142. Benoit B. The value of the three-dimensional ultrasonography in the screening of the fetal skeleton. Childs Nerv Sys. 2003;19:403-409. 143. Ruano R, Molho M, Roume J, Ville Y. Prenatal diagnosis of fetal skeletal dysplasias by combining two-dimensional and three-dimensional ultrasound and intrauterine three-dimensional helical computer tomography. Ultrasound Obstet Gynecol. 2004; 24:134-140. 144. Pairleitner H, Steiner H, Hasenoehrl G, Staudach A. Three-dimensional power Doppler sonography: imaging and quantifying blood flow and vascularization. Ultrasound Obstet Gynecol. 1999;14:139-143. This article first described the use of vascular flow indices from 3D power Doppler ultrasonography during pregnancy. 145. Pan HA, Wu MH, Cheng YC, Li CH, Chang FM. Quantification of Doppler signal in polycystic ovary syndrome using three-dimensional power Doppler ultrasonography: a possible new marker for diagnosis. Hum Reprod. 2002;17:201-6. 146. Raine-Fenning NJ, Campbell BK, Clewes JS, Kendall NR, Johnson IR. The interobserver reliability of three-dimensional power Doppler data acquisition within the female pelvis. Ultrasound Obstet Gynecol. 2004;23:501-508. 147. Raine-Fenning NJ, Campbell BK, Kendall NR, Clewes JS, Johnson IR. Endometrial and subendometrial perfusion are impaired in women with unexplained subfertility. Hum Reprod. 2004;19:2605-2614. 148. Ng EHY, Chan CCW, Tang OS, Yeung WSB, Ho PC. Endometrial and subendomentrial vascularity is higher in pregnant patients with livebirth following ART than in those who suffer a miscarriage. Human Reproduction. 2007;22:1134-1141. 149. Chang CH, Yu CH, Ko HC, Chang FM, Chen HY. Assessment of normal fetal liver blood flow using quantitative three-dimensional power Doppler ultrasound. Ultrasound Med Biol. 2003;29:943-949. 150. Chang CH, Yu CH, Ko HC, Chen CL, Chang FM. Three-dimensional power Doppler ultrasound for the assessment of the fetal brain blood flow in normal gestation. Ultrasound Med Biol. 2003;29:1273-1279. 38 151. Chang CH, Tsai PY, Yu CH, Ko HC, Chang FM. Predicting fetal growth restriction with renal volume using 3-D ultrasound: efficacy evaluation. Ultrasound Med Biol 2008;34:533-537. 152. Rizzo G, Capponi A, Cavicchioni O, Vendola M, Arduini D. Placental vascularization measured by three-dimensional power Doppler ultrasound at 11 to 13 + 6 weeks’ gestation in normal and aneuploid fetuses. Ultrasound Obstet Gynecol. 2007;30: 259-262. 153. Mercé LT, Barco MJ, Bau S. Reproducibility of the study of placental vascularization by three-dimensional power Doppler. J Perinat Med. 2004;32:228-233. 154. Mercé LT, Barco MJ, Santiago B, Sanja Kupešić S, Kurjak A. Assessment of placental vascularization by three-dimensional power Doppler “vascular biopsy” in normal pregnancies. Croat Med J. 2005;46:765-771. 155. Raine-Fenning NJ, Campbell BK, Clewes JS, Kendall NR, Johnson IR. The reliability of virtual organ computer-aided analysis (VOCAL) for the semiquantification of ovarian, endometrial and subendometrial perfusion. Ultrasound Obstet Gynecol. 2003;22:633-639. 156. Welsh A. Correspondence. A caution regarding standardization of power Doppler to measure perfusion in placental tissue. Ultrasound Obstet Gynecol. 2008;31:111-114. 157. Welsh AW, Rubin JM, Fowlekes JB, Fisk NM. Standardization of power Doppler quantification of blood flow in the human fetus using the aorta and inferior vena cava. Ultrasound Obstet Gynecol. 2005;26:33-43. 158. Rubin JM, Adler RS, Fowlkes JB, Spratt S, Pallister JE, Chen JF, Carson PL. Fractional moving blood volume: Estimation with power Doppler US. Radiology. 1995;197:183-190. 159. Hernandez-Andrade E, Jansson T, Ley D, Bellander M, Persson M, Lingman G, Maršál K. Validation of fractional moving blood volume measurement with power Doppler ultrasound in an experimental sheep model. Ultrasound Obstet Gynecol. 2004;23:363-368. 160. Hernandez-Andrade, Thuring-Jönsson A, Jansson T, Lingman G, Maršál K. Fractional moving blood volume estimation in the fetal lung using power Doppler ultrasound: a reproducibility study. Ultrasound Obstet Gynecol. 2004; 23: 369-373. 161. Hernandez-Andrade, JT, Figueroa-Diesel H, Rangel-Nava H, Acosta-Rojas R, Gratascós E. Evaluation of fetal regional cerebral blood perfusion using power Doppler ultrasound and the estimation of fractional moving blood volume. Ultrasound Obstet Gynecol. 2007;29:556-561. 39 162. Martin JA, Kung HC, Mathews TJ, Hoyert DL, Strobino DM, Guyer B, Sutton SR. Annual summary of vital statistics: 2006. Pediatrics. 2008;121:788-801. 163. Ventura SJ, Martin JA, Curtin SC, Mathews TJ, Park MM. Births: final data for 1998. Natl Vital Stat Rep. 2000;48:1-100. 164. American College of Obstetricians and Gynecologists. Fetal macrosomia. ACOG Practice Bulletin No. 22, November, 2000. 165. Barker D. The midwife, the coincidence, and the hypothesis. BMJ;327:1428-30, 2003. 166. Reyes L, Manalich R. Long-term consequences of low birth weight. Kidney Int Suppl 2005; 97:S107-11. 167. McMillen IC, Robinson JS. Developmental origins of the metabolic syndrome: prediction, plasticity, and programming. Physiol Review;85:571-633, 2005. 168. Plagemann A. Perinatal nutrition and hormone-dependent programming of food intake. Horm Res;65:83-9, 2006. 169. Chang FM, Liang RI, Ko HC, Yao B.L, Chang CH, Yu CH. Three-dimensional ultrasound-assessed fetal thigh volumetry in predicting birth weight. Obstet Gynecol. 1997;90:331-339. Dr. Chang and colleagues were among the first to describe how volume measurements of the fetal thigh could be used to estimate fetal weight. 170. Lee W, Comstock CH, Kirk JS, Smith RS, Monck JW, Deenadayalu R. Birthweight prediction by three-dimensional ultrasound volumes of the fetal thigh and abdomen. J Ultrasound Med. 1997;16:799-805. 171. Liang RI, Chang FM, Yao BL, Chang CH, Yu CH, Ko HC. Predicting birth weight by fetal upper-arm volume with use of three-dimensional ultrasonography. Am J Obstet Gynecol. 1997;77:632-638. 172. Schild RL, Fimmers R, Hansmann M. Fetal weight estimation by three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2000;16:445-452. 173. Song TB, Moore TR, Lee JY, Kim YH, Kim EK. Fetal weight prediction by thigh volume measurement with three-dimensional ultrasonography, Obstet Gynecol 2000;96:157-161. 174. Patipanawat S, Komwilaisak R, Ratanasiri T. Correlation of weight estimation in large and small fetuses with three-dimensional ultrasonographic volume measurements of the fetal upper-arm and thigh: A preliminary report. J Med Assoc Thai. 2006;89:13-9. 40 175. Warsof SL, Gohari P, Berkowitz RL, Hobbins JC. The estimation of fetal weight by computer-assisted analysis. Am J Obstet Gynecol.1977;128:881-92. 176. Thurnau GR, Tamura RK, Sabbagha R, Depp OR 3rd, Dyer A, Larkin R, Lee T, Laughlin C. A simple estimated fetal weight equation based on real-time ultrasound measurements of fetuses less than thirty-four weeks' gestation. Am J Obstet Gynecol. 1983;145:557-61. 177. Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body, and femur measurements – a prospective study. Am J Obstet Gynecol. 1985;151:333-7. 178. Lee W, Deter RL, Ebersole JD, Huang R, Blanckaert K, Romero R. Birth weight prediction by three-dimensional ultrasonography – fractional limb volume. J Ultrasound Med. 2001;20:1283-1292. This key article introduces the concept of including soft tissue parameters such as fractional thigh volume into fetal weight estimation models during the late third trimester of pregnancy. 179. Lee W, Balasubramaniam M, Deter RL, McNie B, Powell MD, Gonçalves LF, Espinoza J, Romero R. Soft tissue parameters improve the precision of fetal weight estimation. Ultrasound Obstet Gynecol. 2006;28:389. 180. Lee W, Deter RL, McNie B, Gonçalves LF, Espinoza J, Chaiworapongsa T, Romero R. Individualized growth assessment of fetal soft tissue using fractional thigh volume. Ultrasound Obstet Gynecol 2004;24:766-774. Volume parameters, such as fractional limb volume, can also be used for individualized fetal growth assessment. This uses a Rossavik growth model and second trimester growth velocities to predict normal third trimester growth trajectories. The challenge of comparing an individual measurement against a population standard, with its inherent biological variability, is eliminated. 181. Lee W, Deter RL, McNie B, Gonçalves LF, Espinoza J, Chaiworapongsa T, Balasubramaniam M, Romero R. The fetal arm: individualized growth assessment in normal pregnancies. J Ultrasound Med 2005;24:817-828. 182. Lee W, Balasubramaniam M, Deter RL, Hassan SS, Gotsch F, Kusanovic JP, Goncalves LF, Romero R. Fractional limb volume: a soft tissue parameter of fetal body composition. Validation, technical considerations, and normal ranges during pregnancy. Ultrasound Obstet Gynecol, in press. Fractional arm volume (AVol) and fractional thigh volume (TVol) are introduced as new soft tissue parameters of fetal body composition. The reproducibility, methodology, and normal ranges are summarized during pregnancy. 41 183. Lee W, Balasubramaniam M, Deter RL, Hassan SS, Gotsch F, Kusanovic JP, Goncalves LF, Romero R. Fetal growth parameters and birth weight: their relationship to infant body composition. Ultrasound Obstet Gynecol, in press. Fractional thigh volume correlates as well as actual birth weight to percent body fat of the newborn. A lower correlation is seen with estimated fetal weight and fetal abdominal circumference. These results may have significant implications for cases of suspected IUGR, where clinical decisions are based on either estimated fetal weight or abdominal circumference alone. 184. Miller MW, Brayman AA, Abramowicz JS. Obstetric ultrasonography: a biophysical consideration of patient safety – the “rules” have changed. Am J Obstet Gynecol;1998;179:1-11. 185. Abramowicz JS, Kossoff G, Marsal K, Ter Haar G. Safety statement, 2000 (reconfirmed 2003). Ultrasound Obstet Gynecol. 2003; 21:100. 186. Lee W, Garra B. How to interpret the ultrasound output display standard for higher acoustic output diagnostic ultrasound devices – version 2. J Ultrasound Med. 2004; 23: 723-726. 187. Sheiner E, Hackmon R, Shoham-Vardi I, Pombar X, Hussey MJ, Strassner HT, Abramowicz JS. A comparison between acoustic output indices in 2D and 3D/4D ultrasound in obstetrics. Ultrasound Obstet Gynecol. 2007;29:326-328. 188. Campbell S, Reading AE, Cox DN, Sledmere CM, Mooney R, Chudleigh P, Beedle J, Ruddick H. Ultrasound scanning in pregnancy: the short-term psychological effects of early real-time scans. J Psychosomatic Obstet Gynecol. 1982;2:57-61 189. Zechmeister I. Foetal images: the power of visual technology in antenatal care and the implications for women’s reproductive freedom. Health Care Anal. 2001;9:387400. 190. Whynes DK. Receipt of information and women’s attitudes towards ultrasound scanning during pregnancy. Ultrasound Obstet Gynecol. 2002;19:7-12. 191. Pretorius D, Hull A, Newton R, Nelson T, James G. Impact of patient initiated 3dimensional ultrasound examination. Ultrasound Obstet Gynecol. 2000;16s:94. 192. Ji EK, Pretorius DH, Newton R, Uyan K, Hull AD, Hollenbach K, Nelson TR. Effects of ultrasound on maternal-fetal bonding: a comparison of two- and threedimensional imaging. Ultrasound Obstet Gynecol. 2005;25:473-477. 193. Pretorius DH, Gattu S, Ji EK, Hollenbach K, Newton R, Hull A, Carmona S, D’Agostina D, Nelson TR. Preexamination and postexaminiation assessment of parental-fetal bonding in patients undergoing 3-/4-dimensional obstetric ultrasonography. J Ultrasound Med. 2006;25:1411-1421. 42 194. Maier B, Steiner H, Wienerroither, Staudach A. The psychological impact of threedimensional fetal imaging on the fetomaternal relationship. Progress in Obstetric and Gynecological Sonography Series. Kaba K and Jurkovic D (eds), Informa Healthcare, London, 1997. 195. Pretorius DH, Hearon HA, Hollenbach KA, JI EK, Gattu S, Nelson NM, Nelson TM, Chibuk J, Hull AD, Newton RP, Nelson TR. Parental artistic drawing of the fetus before and after 3-/4-dimensional ultrasonography. J Ultrasound Med. 2007;26:301-308. 196. Rustico MA, Mastromatteo C, Grigio M, Maggioni C, Gregori D, Nicolini U. Twodimensional vs. two-plus four-dimensional ultrasound in pregnancy and the effect on maternal emotional status: a randomized study. Ultrasound Obstet Gynecol. 2005; 25:468-472. 197. Doubilet PM. Entertainment ultrasound (Letter to the Editor). J Ultrasound Med. 2005;24:251-254. 198. Groenenberg IAL, Koning AHJ, Galjaard RJ, Steegers EAP, Brezinka C, Van Der Spek PJ. Picture of the Month – A virtual reality rendition of a fetal meningomyelocele at 32 weeks of gestation. Ultrasound Obstet Gynecol 2005;26: 799-801. 199. van den Bosch AE, Koning AHJ, Meijboom FJ, McGhie JS, Simoons ML, van der Spek PJ, Bogers AJ. Dynamic 3D echocardiography in virtual reality. Cardiovasc Ultrasound. 2005;3:1-4. 200. Verwoerd-Dikkeboom CM, Koning AH, van der Spek PJ, Exalto N, Steegers EA. Embryonic staging using a 3D virtual reality system. Hum Reprod.2008;23:14791484. 201. Reddy UM, Filly RA, Copel JA. Prenatal imaging: ultrasonography and magnetic resonance imaging. Obstet Gynecol. 2008;112:145-57. 43