A new study on liver injury caused by Chinese herbal medicines: substantial data, questionable conclusions
The study
A recent study by Melchart and co-authors [1] analysed the incidence of liver injuries occurring in an
TCM hospital in Kötzting, Germany from 1994 to 2015. Included were patients treated with Chinese herbal therapy whose liver enzyme ALT (alanine aminotransferase) at the time of admission was within the normal range. Just before discharge, the liver function was checked again. An elevation of
ALT up to 5 times the upper norm was considered as an adaptive phenomenon of the liver, and a higher increase was interpreted as liver injury. The average treatment time was 19.5 days due to the duration of inpatient stay. The association of liver injury with the Chinese medicines was assessed using the internationally accepted RUCAM (or CIOMS) scale.
21,740 patient cases were evaluated. An ALT elevation above the normal range was observed in
3.93% of cases, and liver injury with an at least 5-fold ALT elevation occurred in 26 patients (0.12%).
In 8 out of these 26 patients, the authors stated a "probable" association with Chinese herbs, in 16 cases a "possible" association, and in 2 cases they excluded a causality. Bupleuri Radix (chai hu) and
Scutellariae Radix (huang qin) particularly stand out, as they were involved in 7 of the "probable" or
"possible" cases, in 6 of which both were involved simultaneously.
In their analysis, the authors supposed a known hepatotoxicity for a number of herbs („associated with potential liver injury as evidenced from the scientific literature “) which were involved in the cases, namely Bombyx batryticatus (jiang can), Dictamni cortex (bai xian pi), Ephedrae herba (ma
huang), Glycyrrhizae radix (gan cao), Polygoni multiflori caulis (shou wu teng), Polygoni multiflori radix (he shou wu), Polygoni cuspidati rhizoma (hu zhang), Psoraleae fructus (bu gu zhi), Puerariae radix (ge gen), Rhei radix et rhizoma (da huang), Sennae folium* (fan xie ye) and Toosendan fructus*
(chuan lian zi).
*Name has been adjusted to the current nomenclature.
Commentary
This study provides valuable, unprecedented data for assessing the potential risk of Chinese herbinduced liver injury, characterised by the following features:
the prospective design
the high number of 21,470 included patients which allows a valid estimate of the incidence of liver injuries in non-predisposed patients within a limited period of time (19.5 days on average)
the prior authentication and testing for contamination of the herbs used
reference to European conditions by exclusion of prohibited substances, the most toxic medicinals which are uncommon in this area, and the use of excessively high doses
and last but not least, full transparency regarding all components of the herbal formulas and the calculation of the RUCAM scores.
This is thanks to the authors. An important signal is that relevant liver injury caused by Chinese herbs
- at least under the conditions of the study - rarely occurs, and after the discontinuation of therapy, usually regresses uneventfully. However, with regard to the interpretation of the results, some comments and corrections to the study appear to be appropriate.
In evaluating the causality between certain herbs and an observed liver injury, the extent to which hepatotoxicity is already considered proven for these herbs is a key point. Known hepatotoxicity leads to an increase of 1 to 2 points in the probability of a causality concerning the RUCAM score used in the study. These points often make the difference between a "possible" and a "probable" association or if one herb or another is suspected of being the causative agent. If an assumption is made without sufficient evidence, one runs the risk of confirming prejudices and reproducing misconceptions. Frequent repetitions do not make statements more true. In addition, evidence of causality assignment can only rely on "probable" or "very probable" associations to avoid misjudgements. "Possible" associations may have a supportive role or may draw attention to certain herbs, but they can not establish evidence.
For several herbs, which were suspected of being hepatotoxic in the study, these reservations are relevant. The most striking example is Glycyrrhizae radix. This is the herb most commonly used in
Chinese medicine which is contained in approximately 50% of herbal formulas. If a formula is suspected of liver toxicity, then Glycyrrhizae radix is automatically involved in about half of the cases.
The same also applies to other herbs commonly used in Chinese medicine such as Atractylodis macrocephalae rhizoma or Angelica sinensis radix. Therefore, the suspicion is justified only if the involvement of a herb in liver injury is significantly higher than its average frequency of use.
Reservation should be used when a particular herb is involved that commonly is prescribed together with a potentially hepatotoxic agent, because both substances are indicated for certain diseases or their effects complement each other. Here, the frequent involvement of a herb can create a wrong picture.
In a previous smaller study from the Kötzting hospital [2], Glycyrrhizae radix and Atractylodis macrocephalae rhizoma stood out significantly as ingredients of herbal formulas associated with liver enzyme elevations. The authors had described these results as possibly due to chance or to confounding factors, since these herbs had not previously been reported as hepatotoxic in the literature. In the current study, Glycyrrhizae radix and Atractylodis macrocephalae rhizoma are involved in only 2 out of 9 cases as being "probably" associated with liver injury, whereupon the inclusion criterion is not based on a 2-fold, but on a more than 5-fold elevation of ALT above upper norm. Nevertheless, a suspected hepatotoxicity for Glycyrrhizae radix in the present study is stated because this property is assumed as being established.
One contributing author repeatedly stressed a hepatotoxicity of Glycyrrhizae radix (gan cao) as having been documented in the literature [3-5] which increased the likelihood of it being associated with liver injury in the present study according to the RUCAM test by 2 points. This assessment is based on two poorly documented case reports within a single publication from Hong Kong [6]. One of these two case reports is sufficient for Teschke and co-authors [3, 5] to establish the hepatotoxicity of three herbs simultaneously, which is hard to reconcile with the laws of logic. The rationale was that the hepatotoxicity of the herbs should be apparently known, but references are not provided by either the authors of the case reports or by Teschke et al. A complete account of the ingredients used in the herbal formulas was missing, as well as the authentication of the herbs or testing for contaminants. The accepted and widely used procedure for assessing the causality of drug-related liver injury is the RUCAM (or CIOMS) test [7]. The scores cited by Teschke et al. [3] for the RUCAM tests are fictitious; the tests were not performed. A recalculation resulted in a RUCAM score of 2 or 3 instead of "6 to 8" for the herbs in question, so that the causality is "unlikely" or even "possible" [8].
Thus, these case reports are not appropriate for establishing hepatotoxicity. There is no evidence of hepatotoxicity relating to Glycyrrhizae radix.
Another case is Bombyx batryticatus. Here too, without legitimacy, the authors claim hepatotoxicity as being known. In many larger case compilations of liver injury, this medicine is missing [9-19]. In the
publication by B. Shaw [20], Bombyx batryticatus was present, as an ingredient of the complex formulas, in just 2 out of 40 patients with a liver reaction likely or possibly related to Chinese herbal therapy, without it being cause for suggesting a suspected hepatotoxicity. The review by Tu et al. [21] gives a detailed report on the side effects of Bombyx batryticatus, with no mention of liver toxicity. If you search for "Bombyx" and "(liver injury or hepatotoxicity)" in Pub Med, you will find 3 publications that describe a hepatoprotective property of this herb. The work by Teschke et al. [22], which in turn relies merely on the unsuitable Hong Kong case study [6], stands alone in asserting a potential hepatotoxicity.
For a valid causality assessment, clear evidence for the assumption of a "known" hepatotoxicity is required. Herbal medicines, especially those from TCM, involve a particular challenge: they are rarely used as single herbs. In multicomponent herbal formulas, it is difficult to blame a particular ingredient for the reaction. The identity of the herbs must be ensured, since mistakes or deliberate adulterations do occur. Furthermore, contamination due to impurities, undesirable substances or conventional drugs must be excluded. The way in which a herb is prepared or pre-treated, which is often done just to reduce toxicity, can also play a crucial role [9]. Therefore, one cannot unconditionally apply study results from another therapeutic system (e.g., Kampo, Ayurveda) which uses a different method of preparation, to TCM.
The conditions for evidence are fulfilled by only a few herbs. For polygoni multiflori radix (he shou
wu), they are beyond doubt. It is often used as a single herb, too. Among the numerous case reports, authentication or testing for contaminants was partially carried out. For Dictamni cortex (bai xian pi), there are only a few cases of it being used as a single herb [23, 24]. However, it is striking that this herb is significantly more probable to be involved in liver injury than its frequency of use accounts for.
Other herbs with insufficiently documented evidence, which are considered potentially hepatotoxic in the study, are: Sennae folium, Polygoni cuspidati rhizoma, Polygoni multiflori caulis, Pueraria radix and Rhei radix et rhizoma. For example, with Puerariae radix: Teschke et al. [22] cited a reference dealing with two cases of hepatitis due to the juice of Puerariae lobatae radix from Korea [25]. An authentication of the preparations was not documented. The phytochemical composition of the juice cannot be equated with that of a decoction from the dried herb as it is used in the context of Chinese medicine. The RUCAM tests which were carried out, each with a high score of 10 [25], are not credible since the differential diagnosis is incomplete and the documentation of the quo ante hepatotoxicity is not sufficiently substantiated.
The updated RUCAM test assigns two points for hepatotoxicity if it is listed in the product characteristic, and one point if there is only evidence in the literature [7]. A product characteristic is missing for raw herbs. TCM finished products with a single herb as the active ingredient exist only as an exception. For the assured, albeit very rare, hepatotoxicity of Polygoni multiflori radix (he shou
wu), 2 points can be applied analogously. For other herbs that are mentioned in publications, but for which there is no clear evidence, a rating with a quo-ante score of "1" is appropriate: this applies for
Ephedrae herba, Toosendan fructus, Bupleuri radix and Scutellariae radix. For the remaining herbs mentioned in the study, no valid references have been documented which would justify one point.
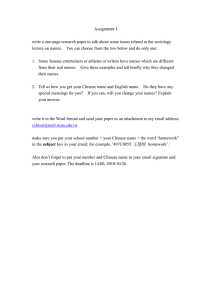
In several cases, this approach leads to an amendment of the RUCAM assessment (Table 1). Of the 9 study cases whose association with Chinese medicine should be "probable", only 4 remain: cases 3,
12, 14 and 19.2; each with a RUCAM score of 6. This "probable" association applies to the entire herbal formula and can only be applied to a single herb if not more than one ingredient of the formula is suspected of being hepatotoxic. This is true for case no. 12, where only Toosendan fructus with a score of "1" justifies a RUCAM score of 6 for a "probable" association. The RUCAM test states
that if other substances are eligible as an alternative cause, "2" points should be deducted [7]. If 2 or more herbs with a pre-existing suspicion of hepatotoxicity are involved, then, if you want to break down the causality to the individual herbs, these 2 points should be subtracted. Then, a "probable" causality can no longer be assumed for these single herbs.
Case no.
RUCAM score formula, acc. to publication
RUCAM score Rezeptur, revised
Association with formula
Involvement of so-called "suspected herbs":
Bupleuri Rx. (RUCAM, herb)
Scutellariae Rx. (RUCAM, herb)
Ephedrae Hb. (RUCAM, herb)
Toosendan Fr. (RUCAM, herb)
3 4
7
6 pr
6
5 po x (4) x (3) x (4) x (4)
12 14 17 18 19(1) 19(2) 24
7
6 pr
7
6 pr
6
5 po
6
5 po
6
5 po
7
6 pr
6
5 po x (3) x (3) x (3) x (4) x (3) x (4) x (3) x (3) x (3) x (4) x (3) x (6) x (4) x (3)
Table 1: Compilation of cases for which the publication, using the RUCAM score, claims a "probable" association of the liver injuries with the respective formula, and revision of the RUCAM scores (red). For the association with individual herbs, corrected RUCAM scores were also given (red). RUCAM score ≤0 =
“excluded”, 1-2 = "unlikely", 3-5 = "possible" (po), 6-8 = "probable" (pr),> 8 = "highly probable". Herbs contained in the formulas which are without any suspicion of hepatotoxicity are omitted.
Bupleuri radix and Scutellariae baicalensis Radix deserve special consideration. There is an abundance of cases of hepatotoxicity in Kampo medicine for formulas containing these substances.
Mostly often, both herbs are used simultaneously, e.g. in the formula sho-saiko-to. In Chinese medicine, however, liver injury due to these herbs is scarcely known [26]. Kampo herbs are not simply comparable to those of Chinese medicine. For Bupleuri radix, the species Bupleurum falcatum is used in Kampo medicine [27]. In Chinese medicine, the species B. chinense or B. scorzonerifolium are officinal [28]. In Japan, standard formulas are predominantly used as granules. Alcohol is also applied for extraction [27], which means that the composition of the extracts is not comparable to that of decoctions from Chinese medicine. As to acute toxicity testing, an ethanol extract was more toxic to the liver than an aqueous extract [29].
Within Chinese medicine, there have been only sporadic case reports with inadequate causality criteria [30, 31] in which these herbs appeared. For the first time, the present study documents several cases with formulas containing Bupleuri radix and Scutellariae radix associated with liver injury, where testing for identity and contamination was done. In the 4 cases remaining as
"probable" after revision, Bupleuri radix is involved twice and Scutellariae radix three times. In case
3, where both herbs are involved, Ephedrae herba appears as an alternative causative agent, and in case 14 (without Bupleuri radix), the potential causative agent Toosendan fructus is present. A clear assignment to Bupleuri radix or Scutellariae radix is therefore not possible here. In case 19.2, only these two herbs are present with a potential quo-ante suspicion. Of particular importance here is the patient's rechallenge by a formula (19.2), which again contained both of these herbs, but only 3 other herbs (Curcumae longae rhizoma, Curcumae radix and Mori ramulus), which were given in the first formula and for which no reasonable suspicion exists. In addition, it is peculiarly striking how many cases with a “possible” causality these two herbs were involved in.
Based on this new data quality, one has to reassess the hepatotoxicity of Bupleuri radix and
Scutellariae baicalensis radix. Either one herb or the other, or both herbs together, should be
considered to be potentially hepatotoxic. However, a definite allocation of causality to one or the other herb does not appear to be feasible without reservation according to the current level of evidence. When using either one of these herbs, one must be prepared for the very rare possibility of an idiosyncratic (unpredictable) reaction.
A re-evaluation also seems appropriate for Toosendan fructus. So far, a possible hepatotoxicity only applied in the case of overdose [32]. Now, the herb is implicated in two out of four cases with a probable association; in case 12, without any other suspected herbs included in the formula.
Apparently, hepatotoxicity can also occur in the normal dose range. Unfortunately, dosages are not detailed in this study. However, if there is a dose-dependency, it may be an intrinsic hepatotoxicity that could be controlled by limiting the dosage.
For a reassessment of Ephedrae herba, the results of the study are not sufficient. This herb is involved in case 3 in which Bupleuri radix and Scutellariae radix are present, so a clear assignment is not possible. The same applies to case 7 and the first formula in case 19 (19.1), for which the association is merely "possible"; in case 20, Bupleuri radix was used simultaneously. The limited number of hepatotoxicity cases involving Ephedra herba documented in the literature must be weighed against the million-fold uses of the herb, especially in the years previous to 2004. However, with the cases from the present study, this herb shifts into the upper range of a "possible" hepatotoxicity.
Conclusion
The study contains unprecedented data quality for assessing the hepatotoxic risk of Chinese herbal medicines. However, many of the evaluations made in the publication do not hold up. The potential hepatotoxicity of Bupleuri radix or Scutellariae baicalensis radix, or of a combination of both drugs together in the context of Chinese medicine must be deemed adequately secured although a further differentiation currently is not possible. Toosendan fructus, at standard dosages, also appears to be possibly hepatotoxic even though the dosages were not explicitly reported in the respective cases of the study. The possible liver injury caused by Polygoni multiflori radix has already been confirmed, and the study provides no additional support on this. Toxicity cases involving this herb seem to be less common in Western countries than in Asia.
Overall, liver injuries caused by Chinese herbal medicine are very rare and their prognosis, if recognized early enough, is generally uneventful. For a duration of use longer than 19.5 days, as in the present study, the incidence might be higher. If liver reactions associated with Chinese herbal therapy occur, it is advisable to carry out a full differential diagnostic procedure [33] to either confirm or disprove the causality, so that the evidence regarding Chinese herbs and their actual hepatotoxic risks increases. This applies not only to the Kötzting hospital, but in every case. The
Centre for Safety of Chinese Herbal Medicines, CTCA (Centrum für Therapiesicherheit in der
Chinesischen Arzneitherapie) in Berlin is an appropriate address for dealing with this matter.
Literature:
1. Melchart D, Hager S, Albrecht S, Dai J, Weidenhammer W and Teschke R. Herbal Traditional
Chinese Medicine and suspected liver injury: A prospective study. World J Hepatol 2017;9:1141-1157
2. Melchart D, Linde K, Hager S, et al. Monitoring of liver enzymes in patients treated with traditional
Chinese drugs. Complement Ther Med 1999;7:208-216
3. Teschke R, Zhang L, Long H, et al. Traditional Chinese Medicine and herbal hepatotoxicity: a tabular compilation of reported cases. Ann Hepatol 2015;14:7-19
4. Teschke R, Wolff A, Frenzel C and Schulze J. Review article: herbal hepatotoxicity - an update on traditional Chinese medicine preparations. Aliment Pharmacol Ther 2014;40:32-50
5. Teschke R, Larrey D, Melchart D and Danan G. Traditional Chinese Medicine (TCM) and herbal hepatotoxicity: RUCAM and the role of novel diagnostic biomarkers such as MicroRNAs. Medicines
2016;3:18
6. Yuen MF, Tam S, Fung J, et al. Traditional Chinese medicine causing hepatotoxicity in patients with chronic hepatitis B infection: a 1-year prospective study. Aliment Pharmacol Ther 2006;24:1179-1186
7. Danan G, Teschke R. RUCAM in drug and herb induced liver injury: The update. Int J Mol Sci
2015;17:E14
8. Wiebrecht A. Dubious pseudoscience – on the alleged hepatotoxicity of Chinese herbal medicines. www.ctca.de/index.php/en/news/dubious-pseudoscience-on-the-alleged-hepatotoxicity-of-chineseherbal-medicines
9. Teo DC, Ng PS, Tan SH, et al. Drug-induced liver injury associated with Complementary and
Alternative Medicine: a review of adverse event reports in an Asian community from 2009 to 2014.
BMC Complement Altern Med 2016;16:192
10. Chen YF, Cai HD. [Investigation of liver damage associated with Chinese medicines] (Chinese).
Yaowu Buliang Fanying Zazhi 1999;1:27-32
11. Li XY, Li CQ, Zhang ZM, et al. [Study on traditional Chinese medicine-induced liver injury: from theory to clinical analysis] (Chinese). Zhuanhua Yixue Zazhi 2015;4:244-249
12. Chau TN, Cheung WI, Ngan T, et al. Causality assessment of herb-induced liver injury using multidisciplinary approach and Roussel Uclaf Causality Assessment Method (RUCAM). Clin Toxicol
2011;49:34-39
13. Lee WJ, Kim HW, Lee HY and Son CG. Systematic review on herb-induced liver injury in Korea.
Food Chem Toxicol 2015;84:47-54
14. Ma X, Peng JH and Hu YY. Chinese Herbal Medicine-induced Liver Injury. J Clin Transl Hepatol
2014;2:170-175
15. Peng XL, Li CS and Cui SZ. [Biometrical analysis on liver injury caused by traditional Chinese herbs]
(Chinese). Shizhen Guoyi Guoyao 1999;10:392-393
16. Pittler MH, Ernst E. Systematic review: hepatotoxic events associated with herbal medicinal products. Aliment Pharmacol Ther 2003;18:451-471
17. Zhang P, Ye Y, Yang X and Jiao Y. Systematic review on Chinese herbal medicine induced liver injury. Evid Based Complement Alternat Med 2016;2016:3560812
18. Zhao P, Wang C, Liu W and Wang F. Acute liver failure associated with traditional Chinese medicine: report of 30 cases from seven tertiary hospitals in China. Crit Care Med 2014;42:e296-299
19. Wang XJ, Xu LP and Wang M. [Hepatotoxicity caused by commonly used Chinese medicinal herbs and compound preparations] (Chinese). Shoudu Yike Daxue Xuebao 2007;28:220-224
20. Shaw BJ. Aspects of Chinese herbal medicine with relation to their hepatotoxicity. A thesis submitted to King's College London for the degree of Doctor of Philosophy. School of Biomedical and
Health Sciences, King's College London & Royal Botanical Gardens, Kew, 2007
21. Tu YD, Yu XP. [The clinical use of Bambusa textilis in lung diseases and its side effects] (Chinese).
Shanghai Zhongyiyao Zazhi 2012;46:64-66
22. Teschke R. Traditional Chinese Medicine induced liver injury. J Clin Translat Hepatol 2014;2:80-94
23. Lee JH, Lee HY, Koh KC, et al. [Drug induced liver disease caused by ingestion of Dictamnus
dasycarpus] (Korean). Korean J Gastroenterol 1998;31:251-257
24. Jang JS, Seo EG, Han C, et al. [Four cases of toxic liver injury associated with Dictamnus dasycarpus] (Korean). Korean J Hepatol 2008;14:206-212
25. Kim SY, Yim HJ, Ahn JH, et al. [Two cases of toxic hepatitis caused by arrowroot juice] (Korean).
Korean J Hepatol 2009;15:504-509
26. Wu SX, Sun HF, Yang XH, et al. ["Re-evaluation upon suspected event" is an approach for postmarketing clinical study: lessons from adverse drug events related to Bupleuri Radix preparations]
(Chinese). Zhongguo Zhongyao Zazhi 2014;39:2983-2988
27. Japanese Pharmacopoeia (JP XVI). English Version. 16th ed. Tokyo: Pharmaceutical and Medical
Device Regulatory Science Society of Japan, 2012
28. Chinese Pharmacopoeia Commission. Pharmacopoeia of the Peoples Republic of China (English version). Vol. I. Beijing, China: China Medical Science Press, 2015
29. Liu YM, Liu XM and Pan RL. [Research progress on toxic effects of Radix bupleuri] (Chinese).
Zhong Chengyao 2012;34:1148-1151
30. Lee CH, Wang JD and Chen PC. Risk of liver injury associated with Chinese herbal products containing Radix bupleuri in 639,779 Patients with Hepatitis B virus infection. PLoS One
2011;6:e16064
31. Melchardt T, Magnes T, Weiss L, et al. Liver toxicity during temozolomide chemotherapy caused by Chinese herbs. BMC Complement Altern Med 2014;14:115
32. Bensky D, Clavey S and Stöger E. Chinese Herbal Medicine. Materia Medica. 3 rd ed. Seattle, WA:
Eastland Press, 2004
33. Center for Safety of Chinese Herbal Therapy (CTCA). Website: www.ctca.de
. A report schedule is available there.