CHRONIC URTICARIA: THE ANSWER WAS IN THE STOOL
advertisement
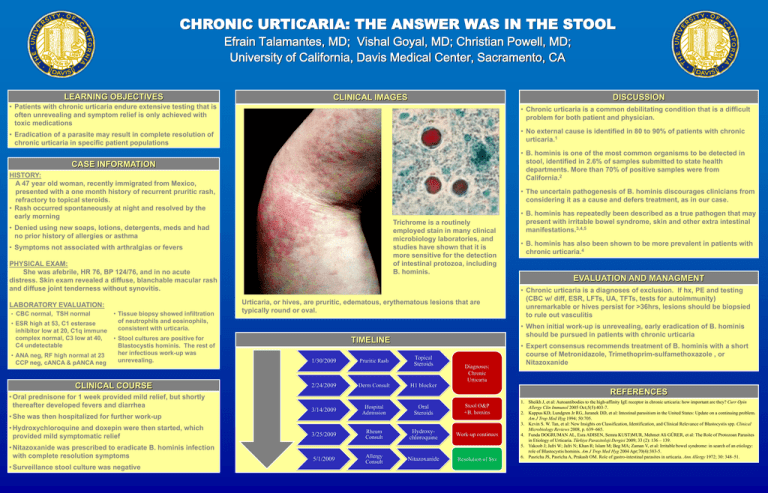
CHRONIC URTICARIA: THE ANSWER WAS IN THE STOOL Efrain Talamantes, MD; Vishal Goyal, MD; Christian Powell, MD; University of California, Davis Medical Center, Sacramento, CA LEARNING OBJECTIVES DISCUSSION CLINICAL IMAGES • Patients with chronic urticaria endure extensive testing that is often unrevealing and symptom relief is only achieved with toxic medications • Chronic urticaria is a common debilitating condition that is a difficult problem for both patient and physician. • Eradication of a parasite may result in complete resolution of chronic urticaria in specific patient populations • No external cause is identified in 80 to 90% of patients with chronic urticaria.1 • B. hominis is one of the most common organisms to be detected in stool, identified in 2.6% of samples submitted to state health departments. More than 70% of positive samples were from California.2 CASE INFORMATION HISTORY: A 47 year old woman, recently immigrated from Mexico, presented with a one month history of recurrent pruritic rash, refractory to topical steroids. • Rash occurred spontaneously at night and resolved by the early morning • The uncertain pathogenesis of B. hominis discourages clinicians from considering it as a cause and defers treatment, as in our case. Trichrome is a routinely employed stain in many clinical microbiology laboratories, and studies have shown that it is more sensitive for the detection of intestinal protozoa, including B. hominis. • Denied using new soaps, lotions, detergents, meds and had no prior history of allergies or asthma • Symptoms not associated with arthralgias or fevers PHYSICAL EXAM: She was afebrile, HR 76, BP 124/76, and in no acute distress. Skin exam revealed a diffuse, blanchable macular rash and diffuse joint tenderness without synovitis. LABORATORY EVALUATION: • CBC normal, TSH normal • ESR high at 53, C1 esterase inhibitor low at 20, C1q immune complex normal, C3 low at 40, C4 undetectable • ANA neg, RF high normal at 23 CCP neg, cANCA & pANCA neg • Tissue biopsy showed infiltration of neutrophils and eosinophils, consistent with urticaria. • Stool cultures are positive for Blastocystis hominis. The rest of her infectious work-up was unrevealing. CLINICAL COURSE • Oral prednisone for 1 week provided mild relief, but shortly thereafter developed fevers and diarrhea • She was then hospitalized for further work-up • Hydroxychloroquine and doxepin were then started, which provided mild symptomatic relief • Nitazoxanide was prescribed to eradicate B. hominis infection with complete resolution symptoms • Surveillance stool culture was negative Urticaria, or hives, are pruritic, edematous, erythematous lesions that are typically round or oval. 2/24/2009 Pruritic Rash Derm Consult • B. hominis has also been shown to be more prevalent in patients with chronic urticaria.4 EVALUATION AND MANAGMENT • Chronic urticaria is a diagnoses of exclusion. If hx, PE and testing (CBC w/ diff, ESR, LFTs, UA, TFTs, tests for autoimmunity) unremarkable or hives persist for >36hrs, lesions should be biopsied to rule out vasculitis • When initial work-up is unrevealing, early eradication of B. hominis should be pursued in patients with chronic urticaria TIMELINE 1/30/2009 • B. hominis has repeatedly been described as a true pathogen that may present with irritable bowel syndrome, skin and other extra intestinal manifestations.3,4,5 Topical Steroids Diagnoses: Chronic Urticaria • Expert consensus recommends treatment of B. hominis with a short course of Metronidazole, Trimethoprim-sulfamethoxazole , or Nitazoxanide H1 blocker REFERENCES 3/14/2009 Hospital Admission Oral Steroids Stool O&P +B. homins 3/25/2009 Rheum Consult Hydroxychloroquine Work-up continues 5/1/2009 Allergy Consult Nitazoxanide Resolution of Sxs 1. Sheikh J, et al: Autoantibodies to the high-affinity IgE receptor in chronic urticaria: how important are they? Curr Opin Allergy Clin Immunol 2005 Oct;5(5):403-7. 2. Kappus KD, Lundgren Jr RG, Juranek DD, et al: Intestinal parasitism in the United States: Update on a continuing problem. Am J Trop Med Hyg 1994; 50:705. 3. Kevin S. W. Tan, et al: New Insights on Classification, Identification, and Clinical Relevance of Blastocystis spp. Clinical Microbiology Reviews 2008, p. 639–665. 4. Funda DOGRUMAN AL, Esra ADISEN, Semra KUST)MUR, Mehmet Ali GÜRER, et al: The Role of Protozoan Parasites in Etiology of Urticaria. Türkiye Parazitoloji Dergisi 2009; 33 (2): 136 – 139. 5. Yakoob J; Jafri W; Jafri N; Khan R; Islam M; Beg MA; Zaman V, et al: Irritable bowel syndrome: in search of an etiology: role of Blastocystis hominis. Am J Trop Med Hyg 2004 Apr;70(4):383-5. 6. Pasricha JS, Pasricha A, Prakash OM. Role of gastro-intestinal parasites in urticaria. Ann Allergy 1972; 30: 348–51.