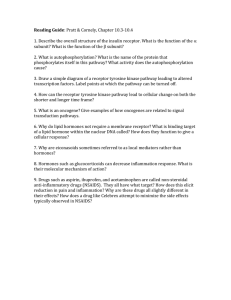
Drug Discovery & Safety: Cancer Molecular Mechanisms Course
advertisement

Introduction Course – Drug Discovery and Safety - Introduction to the Msc intro course on DDS: Molecular mechanisms involved in cancer - G-protein coupled receptors as drug targets in cancer - Drug design and synthesis - Big data on drug discovery - Understanding computation network and cellular dynamics through - Understanding drug action - A systems microscopy approach to cancer drug discovery and drug safety assessment - Safety assessment of candidate drugs - A pipeline spanning in vitro to in vivo animal models for preclinical cancer research Introduction Course – Drug Discovery and Safety 1. Introduction to the MSc intro course on Drug Discovery and Safety: Molecular mechanisms involved in cancer. Study objectives: - Overview of research at the division DDS: from cancer biology to drug discovery and drug safety. - Knowledge of the hallmarks of cancer. - Knowledge of the complex multicellular nature of cancer. - Insight in the concepts of cancer initiation, growth, progression, metastasis. Discovery of drug targets and lead with the desired therapeutic effect and minimal adverse reactions: It’s not just pharma, but more concepts where companies are connected to. - Identify drug targets and leads through phenotypic screening for the discovery of anticancer drugs. - Establish novel safety and efficacy concepts related to the early phases of drug discovery and development. - Understand pharmacological modulation of drug targets at the molecular level. Binding of receptors: how strong, where is the binding? Etc. for a better insight of the drug target and potential new drug. - Use computational techniques for pharmacological interaction and quantitative systems biology modelling. Cell observatory: imaging, RNAi interference, drug screening, target discovery, cell signalling, GPCRs-kinases, medicinal chemistry, computational biology, cheminformatics. Establish concepts for drug discovery cycle: 1. Drug target discovery: screens. 2. Computational chemical biology. What fits in the binding pocket?: structure 3. Drug discovery of compounds and synthesizing to fit in site: assays. 4. Molecular pharmacology, 5. Drug safety. when you find something you need to know if it’s safe and can we better quantify compounds if they are safe. 6. Computational modelling. Cancer development is a multi-step process: cancer is very complex: it also takes a long time to develop. In the lab we look at the simple processes. Normal tissue with mutation, not aggressive, but with more mutations it will be aggressive distribution to other tissues. Every tumor has another set of several events that take place before there is tumor formation, the time of these steps differ from each sort of cancer. Normal initiated mild moderate severe CIS cancer. What are the mutations witch determine which steps will occur? Development and progression steps in cancer: - initiation: suppression of DNA damage response allows cells to accumulated mutated DNA. Critical in tumor development. - Progression: growth advantage: pro-proliferation/anti-apoptosis genes activated and or anti-proliferation/pro-apoptosis genes inactivated. Better performance than their neighbour genes. - Metastasis: invasion of cells into neighbouring tissues and infiltration in blood vessels. Survival of disseminated cells in the niche of distant target organs: metastasis, most people will die because of this. To prevent metastasis: as early as possible, because its very difficult to treat it when there are different metastasis on multiple sites. How do you get from a normal cell to a cell that is really a cancer cell: Genetic alterations and cell consequences – retention or loss of cells: (A mutation is not per se bad for a cell, it does not necessary affect the function of a protein.) Second genetic alteration: possible accumulation of a mutation. In this way you can think of series of events that lead in the end to this aggressive tumor cell. So various forms and accumulation can eventually lead to tumor formation. Crucial mutations for cancer development: they often co-occur. (Proto) oncogene: proto onco (on) - Normally mediates positive signals to growth or survival (inhibition of apoptosis and activation of mitosis). - Activation occurs in cancer where a proto-oncogene (normal functioning gene in a cell) becomes a oncogene (over-inhibition of apoptosis and over-activation of mitosis). (Mutant) tumor suppressor: tumor suppressor mutant tumor suppressor (off) - Normally mediates negative control over cell growth or survival (activation of apoptosis and inhibition of mitosis). So as a sort of balance. - Inactivation occurs in cancer. - Mutations found in syndromes causing enhanced susceptibility to cancer (permanently inactivated tumor suppression with no apoptosis or mitosis). Tumor: upregulation (mutation) of proto oncogenes, where there is an over inhibition of apoptosis and there is overstimulation of mitosis. An oncogene does not give any signals anymore. In colon cancer (long process), these steps are very common. Multistep carcinogenesis: stages in the evolution of colon cancer: Normal cell (chromosome 5q loss or mutation) increased cell growth adenoma 1 (ras mutation) adenoma 2 (chromosome 18 loss or mutation, DCC tumor suppressor) adenoma 3 (p53 tumor suppressor) carcinoma (other chromosome loss) metastasis. With all the work that has been done and the available technology: much better knowledge about all the mutations and molecules that are involved in cell proliferation and cell death and cell survival cancer genome landscape. Every individual has his own type of cancer with different types of mutations (not every breast cancer for instance is the same). -/+ 140 genes altered by mutations in different pathways that can initiate cancer. In different types of cancer: there is a different number of altered genes. for example: in long cancer there are 163 mutations that have been seen, while in breast cancer this is much less. So not all cancer arises or develop in the background of the same number of mutation Also, not every type of cancer has the same amount of mutations per tumor (and these alterations are different per tumor). Some cancer types: a lot of mutations (non-synonymous: mutation will lead to different amino acid so you alter the function of the protein). Cancer develops in the background of a different set of mutations. So, there are more types treatments needed. You have to develop a better target therapy for all these different types of cancer. You also have, for example, long cancer that can give rise because of different things: smoking or genetic. Smokers: continuously exposed to mutagens, these alter the mutations. You also see the variations in the number of mutations between these two types of cancer. Types of DNA modifications in different tumors: Indels: insertions/deletions. SBS: single basepair substitutions, most seen in different tumors: one amino acid that is changing. In different types of tumors: you see different alterations and you see also a different number of alterations. When you look into these different sets of tumor samples, you can also see in the different types of individual cancers, that you have different driver mutations that are distributed. And we still do not know a lot of these driver mutations that are occurring. So in some types of cancer you have more oncogene mutations, whilst in other you have much more tumor suppressor gene mutations. These140 genes are based on a knowledge that we have on what we think how genes are involved in cell proliferation (based on current knowledge). What do these genes do in the cell biology: they can be relevant in cell proliferation (ras mutation). All these oncogenes and tumor suppressor genes are involved in normal signalling pathways that define cell proliferation. So, in fact, it’s all about understanding the individual role of these genes in the cell biology. And based on that, also define, maybe other candidate drug targets. How can you define candidate drug targets? Look at hallmarks of cancer. Mutations are altering the signalling pathways: The hallmarks of cancer: strategies for cancer therapy: critical for development and progression of cancer: to identify candidate drug targets. Hallmark Genome instability and mutation PARP inhibitors Resisting cell death Pro-apoptotic BH3 mimetics Deregulation cellular energetics Aerobic glycolysis inhibitors Sustaining proliferative signalling: escape EGFR inhibitors killing by T-cells. Evading growth suppressors Cyclin-dependent kinase inhibitors Avoiding immune destruction Immune activating anti-CTLA4 mAb Enabling replicative immortality Telomerase inhibitors Tumor promoting inflammation Selective anti-inflammatory drugs Activating invasion and metastasis Inhibitors HGF/c-Met Inducing angiogenesis Inhibitors VEGF signaling Focus on sustaining proliferative signalling; in this lecture. Dive into these genome sequencing dataset. What type of mutations do we actually se: a lot of ras mutations, mutations in EGFR or overexpression, these are all kinases and involved in proliferative signalling. If you know look at these candidate genes: there are even some available candidate genes that are inhibited or mutated in these cell lines. These gene mutations are mutations that you typically see in proliferative signalling. Many of those are kinases, there are many kinases (over 500), they all have a different kinase family that has a different role in the proliferative signalling Getting insight of what the kinases are doing in the different hallmarks of cancer. There are > 500 protein kinase genes. - Receptor tyrosine kinases (subclass o tyrosine kinase): recognize a ligand, extracellular domain that binds the ligand is different and selective (extracellular domain is different for all of these receptor tyrosine kinases), ligand is extracellular is responsible for activation, intracellular is kinase part and this activates a pathway. For some RTKs we now that they are important in cancer, but for some RTKs we don’t know this. We don’t know all the information yet. For many of these receptors, the pharmaceutical industry already developed some inhibitors. These have been used or have been approved in the clinic for various types of cancer. These already reached the clinic. Only small cell permeable compounds can pass the cell membrane, so you want to develop a selective antibody for specific type of receptor. The antibodies recognize particular domain of extracellular region and interact with this region, receptor activation can thereby be prevented. Small inhibitors interact with the intracellular domain. EGFR in breast cancer patients: do the set of higher expression of EGFR, do they actually have sooner a reoccurrence of cancer. So high EGFR: higher relapse of your disease, so your overall survival basically drops. Based on the EGFR expression at the time that the tumor was taken out of the patient. If you have high EGFR at that stage, than you have sooner relapse of the cancer. Also, you will die sooner. So you would say from this: possibly in breast cancer EGFR receptor possible target to inhibit. Target the EGFR receptor. EGFR family has 4 partners, these partners can dimerize and all these dimers that have been formed result in different ligands. These ligands can bind to different receptors. If you stimulate the EGF receptor, than you will activate downstream signalling. Then you get into a large cascade of signalling events, with many kinases that have been activated and also ras pathway activation. If ras gets activated, then you get activation of transcription factors and these will activate target genes. these target genes will define what will actually happen with the cell (promote survival and aggressiveness: growth, inhibit apoptosis etc.). so if you block the EGF receptor, then you will inhibit all of these events and you will prevent all these cell biology and this will be perfect. You actually want to use EGFR inhibitors: to block one of the hallmarks (sustaining proliferative signalling) and the target is the hallmark. You have different approaches: Strategies to target the EGF-receptor: EGF inhibitors to block the sustaining proliferative signalling. - Inhibition through direct antibody binding: antibody binds to the IV site, which lays closest to the cell membrane and closest to tyrosine kinase. Have been used a lot. Are the functional? If you test them now in vivo: if you use cisplatin alone: tumor increases its size. If you use combination with EGFR and cisplatin you reduce the tumor size, so they are effective in cancer treatment. So for this type you need a combination with another cancer drug, you can use them also alone. - Inhibition through dimerization inhibition: antibody binding to the dimerization site which is the II site. - Targeting for intracellular drug delivery: antibody with drug (DM1) binds to the IV site, causes internalization through endocytosis and intracellular release of the drug (DM1). - Targeting through recruitment of cytotoxic effector cells: cytotoxic effector cell binds with bi-specific/tri-specific antibody. - Inhibition of tyrosine kinase activity: small molecule (tyrosine kinase inhibitor) binds to tyrosine kinase intracellular. Only use of small molecules: target the domain specifically of EGFR receptor and block kinase activity and downstream signalling. - Inhibition through HSP90 inhibition and consequent proteasomal degradation: HSP90 inhibitor inhibitors HSP 90 and this leads to proteasomal degradation. What approach can you only use for non-receptor tyrosine or serine kinases: small molecules and not the antibody approach, because antibodies have a limitation to not be able to reach receptors in the cytosol that are sort of masked. One of the key pathways of RTKs: the phospho inositide kinase signalling pathway: whereby the receptor binds PI3kanes, this mediates the formation of PIP3, and binds other kinases that then become active and these kinases, when they are active, they phosphorylate other molecules that then tell the cell to stay alive and keep on proliferating. If these downstream pathways are critical than you can say that PI3k or PIP3 should also be candidate oncogenes and are mutated in cancer. Many types of cancer that regulate this pathway are mutated or overexpressed in cancer. So you can also inhibit these genes, so indeed industry made for these types inhibitors (but they are not in clinic yet). At some point you have a pallet of small molecule inhibitors for kinases that are important in the process that allows you to pick your candidate kinase inhibitor depending on the oncogene activation that is present in the tumor = personalized medicine in the treatment of cancer. Perfect to inhibit the EGFR receptor, but the problem is that the cancer themselves are resistant to the inhibitor. There is a variability in how tumors correspond to a particular drug. But you still want to kill the tumor. Can we define inhibitors that allow to kill the tumor? Look at the inhibitor library and targets. Library to screen the sensitivity of the cell lines. You don’t want that these inhibitors are toxic for normal cell lines. Maybe you need to target multiple hallmarks in one time to have the best effect, we try to understand this in the lab. 2. G protein coupled receptors as drug targets in cancer Study objectives: - Ability to define the roles G protein-coupled receptors (GPCRs) play in the various stages of cancer development. - Ability to describe relevant signalling pathways that link GPCRs and cancer. - Basic knowledge which anti-cancer drugs on the market target GPCRs Big difference between the number of potential proteins and the number of targets for marketed drugs (200-250). We only have a scratch of surface of what is possible. Receptors (GPCR’s) are currently the most used drug targets (45%). Other drug targets are enzymes (28%), hormones and factors (11%), DNA (2%), nuclear receptors (2%), ion channels (5%), and the rest of the drug targets (7%) is unknown. GPCR’s: receptor classical view: binding domain is intracellular at the 7 alfa helices (loops) domain. These helices determine the formation of the receptor. The G-protein coupling domain is extracellular and contains a Cterminus. Receptors – the classical view: - Targets for classic neurotransmitters and hormones: biogenic amines: (nor)adrenaline (beta receptors), dopamine (5 dopamine receptors), histamine, acetylcholine, etc. - Communication with alfa-subunit of G-proteins: o Alpha S: stimulates adenylate cyclase. o Alpha I: inhibits adenylate cyclase. o Alpha q/11: o Alpha 12/13: - Activation of classic effector enzymes: so it is a second messenger. o Adenylate cyclase: second messenger. o Phospholipase C. GPCR classes: A. Rhodopsin: biggest class. B. Secretin and adhesion: second biggest class. C. Metabotropic glutamate, GABA: second biggest class. D. Pheromone (not human). E. Cyclic AMP (not human). Putative GPCRs: frizzled family. Structural diversity in GPCRs: in the human we will only talk about the class A, B, C and frizzled family. Class A: for example M2 mAChR: we know the most of this receptor class. Class B: for example CRF1: big N-terminus where ligands can bind, mainly endogens. Class C: for example GABA2: on the outside Venus flight trap domain: when ligand binds, ligand will get stuck in receptor. They operate together as dimers. Class A is the biggest so it’s the most relevant for cancer. GPCR summary (textbook view on GPCRs): - Membrane proteins with 7 transmembrane domains (7 TM). - Main class is class A. o Many embers are physiological targets for neurotransmitters and hormones. - G-proteins interface between receptor and effector proteins inside the cell. GPCR (not so much in textbooks: a newer view): - Other receptor classes have emerged: class B and C and frizzled, based on sequence and structural differences. o A (rhodopsin ~500). o B (secretin and adhesion ~30). o C (~glutamate/GABA 20). - Novel functions have been discovered. o Transmission factors in viral infection. o Control of food intake and processing. o Role in growth, differentiation and proliferation. - Part of larger protein complex with spatio-temporal aspects. - Alternative messaging. Cancer receptors: - Virally encoded oncogenes: o All chemokine like receptors: mini proteins of 80 amino acids. o KSHC (= HHV8) GPCR (= ORF74). o Human CMV genes (US27, 28, 33, 78). - - - Endogenous receptors: o Classic ones: neurotensin, endothelin-1, bradykinin, somatostatin, GnRH, chemokines (CXCR4), etc. o New ones: metastatin, lipids, adenosine, proteinase activated receptor (PAR-1 and -2), and more. Endogenous receptors with somatic mutations: with somatic mutations the receptor is super active. o E.g., TSH receptor. Also communicate via beta gamma-subunits of G-proteins. Activate alternative signalling pathways: o Rho/Ras/RAF. o MEK ~ MAP kinase. o SEK/JNK. o Hippo. GPCRs are involved in all sorts of cancer and in all stages of cancer: Primary tumor: how they react on inflammation and immune tolerance, how they proliferate and survive: there are several receptors who interact with these stages. Angiogenesis is also a process where receptors are connected with. Later invasion and metastasis takes place where also receptors take part of. GPCR in cancer summary: - GPCRs: o Oncogenic: they cause the cancer. o Oncomodulatory: they help the cancer, by reducing it or by enlarging it. Depending on the goal in the cancer that you are studying. - In different stages of cancer. o Immune response o Proliferation and survival o Angiogenesis o Metastasis and invasion o Resisting cell death GPCR signalling in cancer: the alpha subunits, all together, switch on or switch off certain pathways in GPCR signalling. During metastasis you have the viral(v)GPCR oncogene and the CXR4 receptor, activation of these receptors by metastasis can lead to several events: cytokine secretion (paracrine neoplasia), nuclear events, protein synthesis, survival, or active remodeling (migration). Viral GPCR: US28 is an oncogenic viral GPCR (causes infection): Crypts are getting bigger, and villi is getting smaller. Tissues is getting altered. Chemokine receptor CXCR4: Can be activated by ligands (it is a chemokine). Altogether, the receptor can activate at least three pathways (Hippo/PI3K/EGFR). The expression of the CXCR4 receptor is much higher in cancer tissue, than in the normal corresponding tissue. You can also use this for: using the receptor as a body marker. If the receptor expression is high, then you are not in the best shape. Can be used to treat cancers, but the timeline to discover the right drug: Mimicking a cancer cell: you can see actually what the cancer cell does. Adenosine A3 receptor: Only the adenosine A3 receptor: reduced extravastated cancer cells and an enhanced permeability. Antagonist adenosine A3 receptor: PSB-10: more extravastated cancer cells and not significant change in permeability, so much more cancer cell present who are entering the blood circulation. Which GPCRs? - Many GPCRs play a role in cancer: but their role may differ (note well: different stages). - Some GPCR drugs are on the market or in clinical trials: o Plerixafor (AMD3100, CXCR4 – chemo sensitization). o CF101/102 (adenosine A3 receptor – liver cancer). o (Pan)somatostatin ligands (octreotide, lanreotide – tumor imaging). o GNRH receptor agonists (buserelin, leuprolide – prostate cancer). Hippo pathway: new pathway that is linked to GPCR-pathways The Hippo pathway and human cancer: in all cases a regulator of cell growth. - The hippo pathway is an evolutionary conserved regulator of tumor growth. - The hippo pathway controls multiple cellular functions that are central to tumorigenesis, including proliferation and apoptosis. - Hippo pathway mutations in mice and flies give rise to tumors. - Hippo pathway activity seems to be frequently deregulated in different human cancers but most hippo pathway genes are not commonly mutated. Molecular events such as sensitivity to the mechanical properties of tumors and crosstalk with other cancer pathways might cause hippo pathway deregulation in human cancers. Hippo ON: normally (no growth factors): ideal situation. Phosphorylation of YAP: YAP is staying in the cytosol and cannot transfer to the nucleus. Leads to no proliferation. One type of receptor is coupled by AC via Gs, then YAP gets phosphorylated and YAP stays in the cytosol. Hippo OFF (growth factor action): ligands (growth factor) binds to the EGF/IGF receptor (RTK) and ligands bind to the LPA receptor (GPCR) No more phosphorylation of YAP, YAP transfers into the nucleus. Leads to proliferation. Some receptors turn Hippo OFF by G-proteins, cause transfer of YAP into nucleus. There are a lot hippo pathway ligands who can be blocked so that the Hippo stays ON, that YAP will be phosphorylated and that the proliferation will be stopped. All these several ligands bind to different GPCR’s. Overall conclusions: - GPCRs play an important role in all stages of cancer progression, while using ‘cancer specific’ pathways: e.g. Hippo. - GPCRs as oncogenes and oncomodulators: o Endogenous: both wild type and with somatic mutations. o Exogenous: mainly of viral origin. - GPCRs are obvious drug targets: o CXCR4 antagonist and GnRH agonists on the market. o Other ligands for a variety of receptors in the cancer development. 3. Drug design and synthesis Study objectives: - Ability to identify the most important properties of a lead compound. - Ability to evaluate, based on a given dataset, which compound would perform best as preclinical drug candidate. - Ability to evaluate a synthetic route in the context of hit-to-lead optimization and suggest a superior strategy, taking into account the variability and feasibility of the synthesis. Medicinal chemistry: Chemistry, pharmacology and informatics together, a repeating circle. We want to design novel concepts which can be used to develop novel drugs (by big pharmaceuticals). Target ID and validation hit generation (synthesis) lead gen and optimization preclinical animal studies phase 1: safety phase 2: efficacy safety phase 3: efficacy safety FDA review and approval. In the drug discovery pipeline, where is the chemistry? At the beginning: target ID validation and hit generation (High throughput screening). At the middle: lead gen and optimization and pre-clinical animal studies (lead optimization and upscaling. And at the end: FDA review and approval (industrial production). HTS: screening of thousands two million of compounds on a target to identify a hit molecule. Hit to lead: Hit generation and lead gen and optimization. Lead optimization: Lead gen and optimization and pre-clinical animal studies. Hit to lead: what are we improving? Drug target interaction to form a drug target complex. There will be an equilibrium between no binding and maximal binding. [D] x [T] / [DT] = Kd = koff / kon (as low as possible, so a strong binding). When [T] = [DT] (the half is bound and the other half is not bound) Kd = D = Ki. D + T DT: speed (M/s) = [D][T]kon D + T DT: speed (M/s) = [DT]koff - - Affinity: Kd or Ki = drug concentration (L) that gives a 50% occupancy of the target at equilibrium < 100 nM. So, it is the concentration in which we have the same amount of free receptor, and the same amount of the bound drug. In that case the dissociation constant of RL is the same as Kd. And the lower the better. Residence time: RT or Koff (RT = 1/koff) = lifetime of the drug target complex optimum residence time validation. Potency (EC50): drug concentration that elicits 50% of the maximal physiological response. Efficacy (Emax): maximal physiological response. Ligand efficiency (LE) > 0.29 What are we aiming for? - Hit affinity/activity around 1 uM lead < 100 nM. - Kinetics: depends on target and desired effect. So, there are no guidelines for the kinetics. Residence Time (RT) is different for different targets. Most of the times there is an optimum, we have to study this. What do we do: to determine this optimum: - Addition of chains/fragments (growing and merging). - Scaffold optimization. You need to have the same properties, but you do can change the … Optimize hit compound: a lot of molecules and we look at them to see what is the best. We build Structure Activity Relationships (SAR). Then we try to draw a correlation between the physical chemical properties of those substituents and see how they change the affinity. What it looks like: - Addition of chains/fragments (growing and merging) (fragment growing) - Scaffold optimization (changing the core of the molecule). What do we really do? - Synthesize a series of compounds. - Generate bioassay data: with SAR/SKR. - Draft structure activity/affinity relationship. Synthesis: What do we want? - Choose strategy based on: o Diversity. o Complexity. o Amount (both number and quantity). o Ease of synthesis. o Ease of variation. o Cost of building blocks. o Etc… Retrosynthetic analyses: for example; synthesis of Dendrobine: - Moving backwards to simpler molecules (until reaching commercially/readily available starting materials). Powerful tool: systematic way. Only problem with this approach: difficult to diversify, because the synthesis is tailored for this specific structure (consequence of retrosynthetic analysis). More difficult to make series of derivatives. You need different R-groups. - Commercial building blocks. TOS: - Addition of chains/fragments (based on Retro). Scaffold optimization. Parallel synthesis: efficient introduction of diversity (aka good (retro)synthetic planning). - Keep adding groups and try different routes. - Scaffold for diversity (to make as many as possible). Synthetic plan should introduce diversity (decorations, substituents, etc.) in the last step(s). you make a scaffold and in the last steps you add all the structural differences. You save a lot of steps of work (this is an ideal case). For example: adenosine A1 receptor antagonists: one synthetic plan per type of modification if you can’t add all the things in 1 time. Lead optimization: fine tuning of physical, chemical and pharmacological properties of lead compounds (with a high affinity): the aim is to produce a preclinical drug candidate that can be tested. What is important: to predict those things, therefore you need metrics: they are needed that help predict the pharmacological properties. - Fine tuning: o Solubility. o Lipophilicity. o Acidity (pKa). o Bioavailability (during in vivo tests). o Metabolism/clearance (during in vivo tests). o Toxicity and off target effects. - Metrics: o Drug like (rule of 5: MW < 500, H-bond donors < 5, H-bond acceptors < 10, log P < 5). −𝑅𝑇 ln(𝐾𝑖) o Ligand efficiency > 0.29 : 𝐿𝐸 = = binding per (non-H) atom. 𝑁 N = number of non-H atoms (how efficiently your drug binds). LE relates to drug likeness. o MW = 500 and Ki = 10 nM (or < 100 nM) LE = 0.29 (or > 0.29). 1st case: Capadenoson derivatives. Capadenoson: - Developed by Bayer, suggested for treatment of angina pectoris and atrial fibrillation. - High affinity and selectivity for the adenosine A1 receptor. But for the other adenosine receptors, its very selective. - Good drug-like properties: o MW= 520 o clogP = 5 o LE = 0.35 - Problem: no effect in patients for reducing heart rate in patients with atrial fibrillation in phase 2a clinical trials. But the other factors seemed totally fine, so did we miss something? Did we overlooked the medicinal chemistry? There was only looked at the affinity, and not at how long the effect exists, so: Goal: make RT longer than 28 minutes. GPCR drugs with improved efficacy or safety: analysed for binding kinetics. - Better efficacy/longer residence time: o Histamine H1 receptor – long acting antagonist (desloratadine, allergies e.g. hay fever). o Muscarinic M3 receptor – selective antagonist (tiopropium, COPD). - Better safety/shorter residence time, safer because of shorter action (less side effects).: o Dopamine D2 receptor – short acting antagonist (Quetiapine, schizophrenia). - But, this was all shown in retrospect. can we do this in a prospective manner, can we integrate it in drug design? To safe time and money. Goal before (to make RT of Capadenoson longer than 28 minutes): structure affinity and kinetic relationships: for kinetics this was unknown. So synthesis! Synthesis was pretty straightforward. Biological results were of more importance. You need a halogen on you aromatic ring to have a higher RT, you can compete with other molecules. Para > ortho ~ meta CL > I > Br > F for RT. F > Cl ~ Br > I for kon. F binds faster. Electronic substituents on phenyl are the most important. Correlate physical or chemical properties of substituents: rationalization (Craig plot). It’s a very simple plot: plots two substituent properties against each other. Rationalization: docking study: the best compound docks in the receptor. Side view: - Double anchoring: - “usual” interaction at amino acid residues: Top view: - Solvent exposed: no amino acid residues that interact with it. - Halogen substituent: Compare the drug like properties with the molecule you want to make better: Lead selection: ligand metrics. You always have to put lipophilicity at the right side of the compound: - For same LE, some compounds with higher clogP have shorter RT. - Lowest clogP has shortest RT, but highest clogP does not have longest RT. Summary 1st case: - Organic synthesis quite straightforward, based on previously described experiments. - Focus on establishing SKR: o Organic chemistry: enables the rest. o Molecular pharmacology. o Computational study. 2nd case: an affinity-based probe for the adenosine A2a receptor. Probe = to detect something: selectively labelling a receptor (in this case by click conjugation). Aim of the project: design and synthesize: - High affinity ligand. - Irreversible ligand. - Irreversible probe. Summary 2nd case: - Organic synthesis more challenging, reactive intermediates/products. - Focus on producing a tool compound: o Molecular pharmacology. o Mutation study. o Computational study. Conclusions – take home messages: - Organic synthesis in hit to lead optimization is a tool: o Reach target molecule efficiently as possible. o Bring in diversity (series of analogues). - It is tightly dependent on fundamental advances in the field of organic synthesis (methodology). - A synthetic medicinal chemist has to be polyvalent; his areas of expertise must include: o Organic synthesis: reactions of molecules. o Physical chemistry: physical properties/interactions of molecules. o Molecular pharmacology: bioassays, mechanisms of drug action. Conclusions for the exam: - Chemical properties and bioassay are intertwined: o Draft a simple SAR/SKR. o Suggest next step. o Predict affinity/kinetic profile. - Synthetic planning is paramount. o Evaluate practicality of synthetic route. o Suggest an improved route. 4. Big data on Drug Discovery Study objectives: - Ability to define the concept 'big data' in the drug discovery context. - Knowledge of how data is stored in SQL databases and how to use publically accessible databases for drug discovery (ChEMBL, uniprot). Knowledge of what is a QSAR, how to train a QSAR model and to judge its performance, and how data is described with which QSAR models are trained. Knowledge of multiple sequence alignment procedures and apply it to proteins. Ability to perform a simple dimensionality reduction using PCA What is big data? Big data in cheminformatics and big data in bioinformatics. - Generic term for data so large/complex that traditional processing methods are insufficient: high volume, high velocity, high variety. - For example: OV chip card traveller data, or Facebook user interaction data. If every company is a big data company, than … … every research project can profit from big data. Big data in cheminformatics: typically 10 – 100 molecules are made in a project. It is chemistry data applied in computational modeling. Chemistry data and doing machine learning for example or predicting how well a molecule binds. Cheminformatics: similarity principle. - 10^8 molecules have been synthesized. This is what we know. - 10^33 – 10^60 Lipinski drug like molecules estimated [1 – 3]: this is for molecules up to 36 heavy atoms. This is what we theoretically could know. So, can we not use computers to virtually make all possible molecules? The size of the scale is the problem. We are now at 17 heavy atoms, this gives you 10^11 potential molecules. If we draw this on a scale, then we find out that there should be around 10^33 molecules possible. Big data in bioinformatics: studies sequences (DNA/proteins). Bioinformatics is about sequences, only interested in sequences and the alignment of them. - Aligning sequences. - Looking for motifs/mutations/single nucleotide polymorphisms. - Large scale mutations in cancer. Why chem-/bioinformatics? Before you do something, look at what already has been done. Look at it differently! Data usage enables use of previously published research. Big data in drug discovery: 1. Gathering data and storing data: a. Literature. b. Databases. 2. Using data (cheminformatics): a. Transferring to computer readable format. b. Models/predictions. 3. Using data (bioinformatics): a. Sequence alignment. b. Sequence analysis. c. Application examples. Gathering data and storing data: Gathering data: - Previously: reading papers and lab journals. - Not very efficient, and not very big data. How can we get the information in literature out? With the use of a database, namely ChEMBL. We make a molecule and test it, than we make another one that is slightly different. You do this several times and then you send the information to an article. This doesn’t work. ChEMBL: there are people who actually read all the papers, they extract the target where the paper is about, they extract the molecules, and they put it in a table in a database. Over 13 million bioactivity data points are now free available!!! ChEMBL: people hired to read the papers for them, take out the proteins and molecules and put this in a database. A database can be read by a computer. This covers the medicinal chemistry. You will find a link to the papers who have been working on this target. This is going to be useful for research in later phases. But ChEMBL is not perfect: Escape DB: combines data from ChEMBL and PubChem (high quality). How do we make this information digital? Storing data. Sequel database: structured query language. You store your data in separate tables that are linked. Then it is efficient. This is how a database works; the separate tables work with each other and tell something about each other. And it is smaller in size, which also is flexible. Take home message: Large public repositories of data have started to appear online enabling data driven research: - Bioactivity data: ChEMBL/PubChem Bioassay/ExCape/BindingDB. - Chemical data: UniChem/PubChem Compounds. - Protein data. - Patent data.: UniProt/cBioportal - Pathway data: SureChEMBL. - Pathway data: Reactome/WikiPathways. How do you find the right data for you project? Using data (cheminformatics): how can we learn thing from the data? Two flavours of computational chemical biology: - Statistical modeling: in the introduction. We look at what is done in the past and then we use that to make predictions for the future. o QSAR models. o BIG data analysis. o Random Forests. - Structural modeling: not in the introduction! o Docking and storing. o Crystal structure based. Similar compounds have similar properties: use for model predictions. If a molecule looks similar to another molecule, chances are that this molecule does something similar. This is trivial, but we need this to make certain assumptions. Take home message molecular similarity: - In cheminformatics methods rely on the similarity principle which states that ‘similar molecules are expected to have similar bioactivities’. - A comparable principle exists for protein targets. Similar proteins are expected to interact with similar molecules. How does a computer read chemistry: - Descriptors, describe molecules. - Physiochemical properties. For instance: MW, LogP, hydrogen bond donors, hydrogen bond acceptors, polar surface area. But we need something that is more specific, focused, who can describe molecules better. So therefore, we use fingerprints: ‘digitize’ chemical structures. With Fingerprints we make high quality molecules. Bitstring: from zero to 1 million and when something is present it gets a 1 or when its absent it gets a 0. Just bits. Each molecule leads to a 0 or 1 which means on or off, this leads to a lot of puzzle pieces whereby molecules can be read. It is a simple concept: is it there or is it there not? But if you do it for large number of molecules you will find statistics. You can actively search for molecules with certain criteria. Take home messages descriptors: - Computers read chemistry by translating the structure into ‘descriptors’ that describe some characteristic of the molecule. - Characteristics can be very general (e.g. AlogP, a measure for lipophilicity) or more specific (e.g. a bit of a fingerprint that represents the presence of a substructure). o The fingerprints allows for better models as they can better capture a (sub)Structure-Activity Relationship How does a computer compare chemistry? Tanimoto similarity coefficient: defines similarity. 𝑐 There is however a size bias, but this is relatively small: 𝑆𝑖𝑚𝑖𝑙𝑎𝑟𝑖𝑡𝑦𝐴𝐵 = 𝑎+𝑏+𝑐 A = bits only in A, b = bits only in B, c = bits in both A and B. So: similarity = bits in both (A+B) / (bits in A + bits in B + bits in both (A+B)) So: A B: 3 / (3+4+3) = 3/10 = 0.3 Take home message molecular similarity: - A similarity coefficient is used to compare the bit strings of molecules and quantify similarity (express similarity as a single number). - The most commonly used is the Tanimoto coefficient (sometimes also called Jaccard index). o Others include Cosine and Tversky. Two techniques commonly used: - Principal Component Analysis (PCA): reducing data to what really matters: dimensionality reduction technique (simplify data view). - Quantitative Structure-Activity Relationship (QSAR): technique to relate an effect (e.g. affinity) to molecular structure, to understand why compounds bind and predict untested compounds *Principal Component Analysis (PCA): reducing data to what really matters: dimensionality reduction technique (simplify data view). Dimensional reduction: conversion to distance matrices (coloured, heat map). Take home message: Principal Component Analysis: - Used to reduce information in large datasets. - Instead of looking at a lot of variables, dimensionality is reduced to for instance 2 / 3. - The further dots are in 2D the more dissimilar they are, the closer the more similar. - Very useful for molecules or proteins! *QSAR: understand why compounds bind and predict untested compounds. With the use of machine learning. However, you need some information to build on. Machine learning can explain activity on the A1 receptor. Measured versus modeled plot. Take home messages: Quantitative Structure-Activity Relationship: - QSAR is a method to have a computer predict how well a molecule will bind. - If a descriptor occurs commonly in active molecules and never in inactives, QSAR can explain activity based on this feature (e.g. fingerprint bit). - QSAR requires that you already know molecules that do bind (training set). - QSAR requires ‘training of a model’ to understand how features determine activity. - After training a QSAR model can be ‘validated’ to see if the models predict activity of compounds you have tested. - Subsequently a model can be ‘applied’ to predict activity of compounds you have NOT yet tested. Then you get a measured versus modelled plot: it tells us Using data (bioinformatics). How can we learn things from the data? Its all about scoring, about things how often they are occurring. If they are next to each other: high score, if there is a gap: lower score, and if there is a miss alignment: much lower score. Sequence alignment: - Important to determine similarity of sequences. - Assumption is that similar sequences indicate similar proteins. - In turn similar proteins indicate a similar function. An alignment is scored. Alignment: points Gap: min points (cheap) Mis alignment: more min points (costly) The quality of your alignment depends on how good your scoring is. BLOcks SUBstitutoin (BLOSSUM) matrix: Use to make an alignment. Every amino acid is tested next to each other and scored, the one with the highest score is kept. If an amino acid is less frequently occurring or when high impact residues are aligned correctly, this increases the score. When they are aligned incorrectly, this will decrease the score. Example: We have two sequences: CALHP and CLLHL and a GAP leads to a -10 point penalty. Everything is sampled and scored, and then you look at the best one. So the quality of your alignment depends on your gaps and on which matrix you use. This is how bioinformatics works and where they start and do everything else. *Take home messages: Alignment: - Understand what a scoring matrix is and how it is used to judge an alignment: for example the BLOSUM matrix. - Understand why aligning two very different amino acids leads to a penalty. - Understanding why two similar amino acids that occur very rare leads to a higher score. Understanding why a gap leads to a penalty (-10): introducing gaps in the sequences can allow an alignment algorithm to match more terms than a gap-less alignment can. Minimizing gaps in an alignment is important to create a useful alignment, too many gaps can cause an alignment to become meaningless. Gap penalties are used to adjust alignment scores based on the number and length of gaps. Application example. 5. Understanding network and cellular dynamics through computation Outline: - Introduction networks and modeling: o Terminology o Why modeling - Modeling chemical reaction networks: o Model formulation o Model analysis - Using network models for drug discovery. Study objectives: - Knowledge of terminology and concepts used in ODE model formulation and analysis (e.g., variables, parameters, equilibria, stability, null clines, bifurcations). - Ability to create a simple ODE model from a 'cartoon' model and vice versa. - Ability to interpret ODE analysis output and sketch examples of expected output. - Knowledge of how ODE models can be exploited to find the best targets for therapy. Types of models that we make fall into categories, we are interested in the dynamic changes (changes over time) in the system. We take differential equations and spatial (cell based) models into account. Application areas: - Drug safety prediction and mechanistic understanding of toxicity. - Tumor growth/metastasis and role of immune system in tumor destruction Introduction networks: In the past: simple and linear in a straightforward manner, people thought it was quite simple. but currently: non-linear with many feedback and many players involved. Because of all these positive (self-stimulation) or negative feedbacks, it is very difficult to predict what will happen. The feedbacks make it difficult to see what is happening over time. Cartoon network models: - Based on verbal description. - Nodes describe molecular species. - Arrow describe molecular interaction (formation, degradation, regulation). Disadvantage of cartoon models: quite uncertain how this cartoon model will behave over time (it is not a quantitative description). Main drawback of cartoon models (not a quantitative description): uncertainty of model behaviour: Mathematical network models: Modeling: ordinary differential equations (ODEs): describe changes over time (dynamics), to describe all arrows in cartoon models as quantitative reaction rates (this is also a drawback). So you describe the dynamics. You become more quantitative (advantage), but a disadvantage is that you have to know what exactly the quantity is of all the reactions that are occurring (this is difficult). Why modeling? - Removes uncertainty of cartoon model behaviour. - Formalizes a hypothesis and then you test/simulate if this makes sence. - Explain complex system behaviour based on individual components. This is a major advantage. By describing you get complex behaviour of the system as a whole and this is hard to see if you look at all the single players together. - Reveal inconsistencies in cartoon models refine hypothesis test experimentally cycle of experimental work. Mechanistic versus descriptive models: Mechanistic: most interested in. - Describe mechanism underlying observed behaviour. For example: oscillations and the mechanism underlying this. - Leads to understanding of why the system behaves as it does. - Problem: multiple mechanisms could lead to similar behaviour: strong conclusion on which mechanisms cannot explain data. Assumptions are not always true. There are more mechanisms that can explain the same data and explain the same behaviour. Descriptive/phenomenological models: describes a phenomenon. - Summarizes data. It describes without going into the mechanism that is causing it. - Less powerful, but can still be used for prediction. Example: NF-kB pathway (transcription factor): - Regulates cell division, inflammation and apoptosis. - In absence of stimuli: inhibition by protein IkB. - Extracellular stimuli (e.g. hormones) IkB decrease. - Activation of NF-kB response + negative feedback to terminate response. NF-kB oscillations: sketch of experimentally observed behaviours: Negative feedback can lead to oscillations. When modeling the NF-kB pathway: a simple model with one form of protein IkB cannot reproduces observed dynamics, so distinct isoforms of protein IkB have to be included into the model. Then comparing modeling data to experimental data: If there is a good match: then you have a good expanded model of the pathway. More looking into the different isoforms: looking at knock out of the proteins. Than compare the experiment and the model data with each other to see if there is a good match. By doing all this experimental work and modeling work: - Strong feedback by IkB-alpha allows for fast turning off of response. - IkB-beta and IkB-epsilon reduce oscillations. - Demonstrated by combination of modeling and experimental work. To pinpoint the role of the different players in the system. Example: unfolded protein response: - UPR: response to protein folding stress in endoplasmic reticulum. - In absence of stress, chaperones (BIP) bind three sensors. Summary introduction to modeling: - Cartoon models versus mathematica models. - Why modeling? - Example of UPR: modeling generated. Chemical reaction networks: How can we go from a cartoon network to a quantitative description? Write all the possible reactions down in a row. Variables and parameters: State variables: can vary over time. - Concentration or abundance of modelled molecular species that you want to include in the model. - Can vary over time. Parameters: do not vary over time. - Characterizes environmental effects and interactions: values are fixed over studies time scale. - E.g.: degradation rate, maximal expression rate. - Convention in biology: parameters are positive (important). Usually makes sense: formation rate cannot be negative, degradation rate must always be negative so we always write a minus before this parameter, because the parameter itself will be positive. Reaction rates: we need to know this to predict changes over time, we need to know the rate (speed) of the reaction. Reaction rate depends on: - Concentrations of the molecular species (reactants) that are involved in the reaction. - Environmental conditions (temperature, pH). If rate is known, reactions can be described as Ordinary Differential Equations (ODEs). ODE assumptions: reaction rates are approximated. 1. Well mixed environment (all the reactions can occur) rates considered independent of position in space. But: spatial structure in cells. This could be taken up in a model. In some cases it is important to give then two variables of a specie. 2. Many molecules are present can be described as continuous rather than discrete. But: some processes rely on only dozens (few) molecules. Law of mass action: Reaction rate is proportional to the product of the concentrations of the reactants: Reaction Rate XP k1[X] A+BC k2[A][B] D+D k3[D]2 A k[S]0 = k K, k1, k2, k3: (mass-action) rate constants Kinetic order X: 1 A&B: 1 D: 2 0 Derive equations: derive from reaction rates. Write as differential equation: the more a you have, the faster the degradation will go. Summary transform cartoon to ODE: How can we go from a cartoon network to a quantitative description? Chemical reaction network describing all the individual reaction rates assumptions ODE. How to analyse ODEs? 1. Analytical/symbolic solution. 2. Numerical simulation. 3. Model analysis. 1. Analytical solution: in some cases ODEs can be solved analytically, to write down a concentration directly as function of time: a(t). parameters are considered to be positive, so only positive values for k: - da/dt = -ka. a(t) = De^(-kt) Exponential decay function. D is the initial concentration. A will deplete over time because there is no formation. In the end the result will be the same (in the beginning the dropping however differs). Network models: many different players so you need special ways to analyse systems. 1. Analyse by computer simulation: - In silico experiments: how does the system behave? - Predict system behaviour over time for given dontions. - Use numerical simulations in software packages (e.g., matlab, mathematics, R). 2. Mathematical model analysis: Study asymptotic behaviour: Behaviour of the model in the long rung (e.g., steady state, oscillations). Steady state: often, models in the long run arrive at a persistent state. Alternatively, oscillations or chaotic behaviour. Transient: the time course from initial to asymptotic state. Why does the system behave as it does? - Sophisticated mathematical techniques. - Reveals non-intuitive connection between model structure and behavior. Numerical simulations: - Approximation of solution for one initial condition, rather than having the exact solution. - Time step determines accuracy of solution. The smaller the time steps, the better the approximation to a true solution. With the computer you can do this very very well. Asymptotic behaviour and transient behaviour: Asymptotic behaviour: - Behaviour of the model in the long run. You are interested in what will happen after a long time. - Steady state: often, models in the long run arrive at a persistent state. From that they will not change anymore. - Alternatively, oscillations or chaotic behaviour. These oscillations will be stable. Chaotic behaviour is very chaotic and this will happen forever (not seen very much). Transient: - The time course from initial to asymptotic state. Steady states/equilibria: which will occur over the long run (asymptotic). da/dt = k0 – k1a What will happen in the long run? a will be at steady state a* if production equals decay: find a* by solving equation da/dt = 0. When we have set the parameters, than we will now what will happen to a in the end. K0 – k1a* = 0 K0 = k1a* A* = k0/k1 - Here, the steady state is approached independent of the initial condition. If you start at low values of a, it will increase until the steady state is reached. If you start at high values of a, it will decrease until the steady state is reached. This is called a stable steady state, but in general this is not the case: - In general, steady states can be stable or non-stable. Summary model analysis (1): - Exceptionally, analytical solution can be derived. - Numerical simulations. - Mathematical analysis: steady states and phase plane analysis. Allosteric inhibition: dS1/dt = k1 – k3S1 – k5S1. dS2/dt = k2 – k4S2 + k5S2. Example: cooperative allosteric inhibition: N: the number of molecules that can bind to S1 (or S2, etc.). First: model simulation over time: Both S1 and S2 increase at first together. You can also plot this differently, in a phase portrait. Concentration s1 versus concentration S2, in this plot you draw the trajectory. You lose the information of time, but you do see the relation of the variables better. You can draw multiple of the trajectories. Than you get a ‘spiraling’ to the equilibrium, this is called a stable spiral. We can also draw nullclines, nullclines are the turning points of the trajectories: - At the S1 nullcline only S2 changes vertical. - At the S2 nullcline only S1 changes horizontal. - Intersection of nullclines equilibria. There are two nullclines here, because there are also 2 variables (every variable has a nullcline). Where the nullclines intercept: no changes of S1 or S2 equilibrium. How do we calculate these null-clines (if we have a ODE)? By putting each equation to 0: - S1-nullcline: ds1/dt = 0. - S2-nullclinie: ds2/dt = 0. Than you fill in parameter values and then you can draw the line in the phase portraits, this can also be done by a computer program. The advantage of this equation when all the parameters are still there, you can see what happens to the null-cline when the parameter changes: you can see the effect of the parameters on the null-clines. Vector field: can also be drawn into the phase portraits. - Gives direction at specific point in phase portrait. - Can be determined manually or with software. Software can used to determine/calculate the vector field, once you pinpoint the parameters to specific values and also once often see it manually by looking at the equations. At the null-cline: change of direction. Mono/bistability: more than one equilibrium. Mutual inhibition: Parameters can be symmetric and asymmetric. Mutual inhibition and no formation from S1 to S2. There can be different values for n, it can be a symmetric or asymmetric simulation. Monostable system: S2 wins independent of initial condition (S2 inhibits the most, n1 >2). Independent on where you start you always end up where there is only S2 left. If you make the inhibition more symmetric: then you will get an equilibrium around the middle. Then, you have a balanced inhibition. They intercept at multiple positions. Now you see that it depends on where you start to what equilibrium you will go. If it goes specifically to S1 or S2: this equilibrium is called the basin of attraction. In the middle it is called separatrix, where the two basins are separated. This can also be a very irregular shape, for instance a complex model. Bi-stable system: depending on initial condition, either S1 or S2 wins. You cannot go to the equilibrium in the middle, because either S1 or S2 wins. Bi-stability: - Unstable steady state: only maintained if there is no perturbation at all, only if you put it exactly at the middle and there is no fluctuation (in biological systems this will never happen). - Important rule: two stable equilibria there must always be divided an unstable equilibrium (two separate to other to equilibria into two stable equilibria). - Bi-stability can occur if positive feedback and nonlinear interactions. In the mutual inhibition case, the positive feedback in this system is Non linearity is caused by this non allosteric inhibition. If you remove it, you will not have such a bi-stable system. Model behaviour of the system depends on the parameters that you have chosen. Model behaviour depends on parameters that: Vary parameters and study changes of long term behaviour: Bifurcation diagram: Plot steady state as a function of a parameter overview of ‘structural’ changes that occur. Hysteresis: resulted by a differentiation in a cell. Bi-stability can lead to a switch. Transition between states at different thresholds hysteresis. If there is noise in the system (random fluctuations), than you can switch. If you are far from it, than the noise will not be enough. Irreversible switch: system can become trapped in a state. Differentiation in a cell which cant go back. Hysteresis: - Transition between states at different thresholds. - Hysteresis: system has memory of current state. Irreversible switch: system can become trapped in a state. Summary model analysis (3): - Multiple equilibria can be present. - Parameter change can lead to structural change of model behaviour (bifurcation). - Bi-stability can explain switching behaviour. Parameter fitting: - Some parameters can be measured directly, e.g., degradation rates from half-life observations. - Other parameters are estimated by ‘calibrating’ the model to experimental data: model fitting. You need measurements and the predictions of the model (on a continuous line), than you compare the predictions and measurements, than: - Residuals (sum of squared errors) are minimized during fitting using optimization algorithms (to find the best parameters to define the dataset). Uncertainties: How certain are model parameters? E.g., parameters may depend on each other. Different strategies: - Generate artificial data can parameters be retrieved when fitting the model to artificial data? - Find range estimates for parameters (95% confidence intervals) e.g. by ‘bootstrapping’. Summary fitting and uncertainty: - Difficult: parameter estimation. - Important to know their uncertainty. Exam: - Ability to explain concepts/terminology (e.g., parameters/variables, equilibria). - Translate simple example of verbal model into ODE or vice versa. - Interpret graphs like bifurcation plots/phase portraits (or draw examples). o Bifurcation plots: https://www.youtube.com/results?search_query=interpret+bifurcation+plots o Phase portraits: https://www.youtube.com/watch?v=dpbRUQ-5YWc Quite new territory: not much work has been done. Using models to predict good drug targets: Network modeling in drug target discovery: Understanding of network dynamics which network players are critical (and compare these players). Once a model is validated: 1. Describe ‘healthy’ and ‘pathological’ state. 2. Simulate the effect of drugs on critical players. Simulate effet of drug: - First describe both healthy and pathological state. - Next simulate effect of drug administration. - Variant, e.g.: cronotherapy: optimal dosing scheme (dosing scheme that can change over time) e.g. related to circadian clock. To give a drug early in the morning or late at night, this can be investigated in the model. Predicting drug targets: in a more formal way: - Where are the drugs in network models? Drugs affect parameters. - Insensitive parameters have little effect, even if they could be altered with therapy. - Sensitivity analysis: study effect of small parameter changes on response of critical variable. - Insensitive parameters have little effect, even if they could be altered with therapy than it would still not have an effect. You really need a sensitive parameter to find the drug target. - Potential problem: bifurcations can alter the complete dynamic behaviour (than a sensitivity analysis would be very difficult), e.g., an oscillation disappears. Example ErbB/Akt signalling: - Signalling pathway for regulation of proliferation, migration, apoptosis. - In cancer, the four ErbB receptors/ligands often are overexpressed or mutated. - Limited clinical activity of antibodies against receptors. Sensitivity of Akt phosphorylation: ErbB3 receptor is the most sensitive one for this particular stimulus (one of the receptors that was not tackled yet, it was seen as a unimportant receptor) developed antibody against ErB3 and demonstrated effectivity in vitro and in mouse model. Summary modeling in drug discovery: - Validated model effect of drug can be simulated. - Find critical network players potential drug targets. Summary network models: - ODE models of networks: o Formulation and analysis: o Understand dynamics of network. o Understand structural changes of behavior. - ‘sensitive’ network players potential drug targets. Exam: - Ability to explain concepts/terminology (e.g., parameters/variables, equilibria). - Translate simple example of verbal model into ODE or vice versa. - Interpret graphs like bifurcation plots/phase portraits (or draw examples). 6. Understanding drug action Study objectives: - Ability to recognize and apply the concepts of ligand affinity, binding kinetics, potency and efficacy. - Ability to recognize and apply the concepts of agonism, antagonism and inverse agonism. Receptor pharmacology and signal transduction. First: target selection (identification) and then: Receptor pharmacology: Lead (compound) discovery, medicinal chemistry (pre-clinical study) and in vitro studies (clinical study phase I-III). Later: in vivo studies (approval) and clinical trials and therapeutics (marketing and postmarketing study/re-examination). In vivo: drug-receptor interaction. Important questions: - Does the drug reach the site of action? - Does the drug bind the target (occupancy)? - Is there an on-target pharmacological effect? Receptor pharmacology: how to characterize ligand binding? Understanding drug action: drug action is all about mathematics, but you can also use Graphpad Prism. Mathematics of receptor-ligand interactions: Normally: [L] + [R] [LR] Equilibrium: kon [L] [R] = koff [RL] Equilibrium dissociation constant (affinity): Kd = koff/kon = [L] [R] / [RL] The number of binding sites is finite, so [R] + [LR] = Bmax When: 𝐾𝐷 = [𝐿]∗[𝑅] Than: [𝐿𝑅] = and 𝐵𝑚𝑎𝑥 = [𝑅] + [𝐿𝑅] [𝐿𝑅] 𝐵𝑚𝑎𝑥 ∗[𝐿] [𝐿]+𝐾𝐷 [𝐿𝑅] So: 𝑟𝑒𝑐𝑒𝑝𝑡𝑜𝑟 𝑜𝑐𝑐𝑢𝑝𝑎𝑛𝑐𝑦 = 𝜌𝐿 = 𝐵 𝑚𝑎𝑥 [𝐿] = [𝐿]+𝐾 𝐷 How to measure [RL]? By radioligand binding studies: - Label L to yield a marker, L*: radioactive fluorescent, etc. o Ideal L*: stable titrated, high affinity (Kd ~ 1 nM), low non-specific binding, optimal kinetics (temperature). - Distinguish L* R from L*: o Through separation (e.g. filtration). o Without separation (e.g. SPA). - Measure [L*R]: o [3H], [35S]: liquid scintillation counter. o [125I]: gamma counter. Saturation experiment: - Radioligand affinity and number of binding sites: this type of experiment is often done once at the start of a project: Saturation experiment (II): saturation binding parameters of an adenosine A1 receptor antagonist [3H]DPCPX on various cell membranes: comparable Kd values and different Bmax values (under same conditions). Displacement experiment (I): affinities of unlabelled compounds (agonist(CCPA) and antagonist(DPCPX)). Displacement experiment (II): - Linear transformation: Hill plot. - Hill slope (nH): type of receptor ligand interaction (stoichiometry). - IC50 value: depicts ligand affinity. Agonist versus antagonist binding: a receptor system can be depicted as a balance between active (Ra) and inactive (Ri) receptors: [Ri] [Ra] - Antagonist: no effect. - Agonist: effect to the active state. - Inverse agonist: effect to the inactive state. Example: antagonist radioligand (e.g. [3H]DPCPX]: But what happens if we use an agonist radioligand? Displacement experiment: Cheng-Prusoff equation: 𝐾𝑖 = 𝐼𝐶50 1+ [𝐿] 𝐾𝐷 Transform assay dependent IC50 value to assay independent Ki value. IC50: affinity displacer. Kd: affinity [L*] [L]: concentration L* Association and dissociation: radioligand association and dissociation rates. Resulting binding parameters of [3H]DPCPX kinetic association and dissociation assays. Kd comparable to Kd from saturation experiment: - If performed under the same conditions. - If equilibrium was reached for saturation assays. Summary – receptor binding: - For radioligand binding studies one needs a ‘toolbox’ consisting of: o Cells (highly) expressing the target of interest. o A (suitable) labelled ligand. o Competing ligands of interest. - Radioligand binding studies generate: o Equilibrium: Kd, Bmax, IC50, nH values and calculate Ki values. o Kinetic: kobs or koff values and calculate kon or Kd values. Signal transduction: how to characterize functional effects? How to measure a functional effect? - Upon drug binding to the target an (intra) cellular response is generated dependent on the drug’s affinity and efficacy. - Depending on the type of target (e.g. membrane receptor, enzyme, ion channel, transporter etc.) many different functional readouts can be used. - Functional effects can be determined and quantified from in vitro, in vivo and ex vivo experiments. In vitro assays - functional assays: for instance: G-protein activation, 2nd messengers (e.g. cAMP), reporter gene (transcription) and phenotypic assays (cellular respns). Potency and efficacy – background: Drug potency depends on: - Drug factors: affinity and efficacy. - System factors: receptor number and coupling effects. Compound classification: based on intrinsic activity/efficacy (in vitro): - Full agonist: 100% functional effect. - Partial agonist: for instance 50% functional effect. - (neutral) agonist: 0% functional effect. - Partial inverse agonist: for instance -20% functional effect. - Full inverse agonist for instance -60% functional effect. Like said before: a receptor system can be depicted as a balance between active (Ra) and inactive (Ri) receptors: [Ri] [Ra] - Antagonist: no effect on equilibrium. - Agonist: effect to the active state: equilibrium lays to the [Ra] site. - Inverse agonist: effect to the inactive state: equilibrium lays to the [Ri] site. Antagonism: - Antagonism can affect the agonist dose-response curve (DRC) in three ways: o Competitive antagonist: shift of the agonist DRC to the right: same functional effect, but a higher EC50. o Non-competitive antagonist: o Agonist plus irreversible antagonist: - This depends on type of agonist, antagonist, and sensitivity of tissue used. Competitive antagonism: - Lineair transformation Schild-plot. - Slope: mode of antagonism. - pA2 value: antagonist affinity. Antagonist potency (IC50): can be determined from antagonist DRC in presence of agonist. Summary – functional assays: - for functional studies one needs a ‘toolbox’ consisting of: o Cells expressing the target of interest. o Full (endogenous) agonist for reference. o Read out of e.g., 2nd messenger (kit-assay), enzyme activity, protein transcription, cellular response (label free). - Functional studies generate: o Insight in type of ligand, unlike receptor binding assays. o EC50 and Emax values for agonists. o IC50 values for antagonists. Study objectives: - Understand how drug action is quantified: affinity (Ki or Kd), potency (EC50 or IC50) and efficacy (Emax). - Understand how ligand affinity can be measured. - Understand how a drug can be classified as a (partial/inverse) agonist or antagonist. - Understand how agonist and antagonist efficacy and/or potency can be measured. 7. A systems microscopy approach to cancer drug discovery and drug safety assessment To design experiments: use microscopy to do some systems biology. Study objectives: - Knowledge on microscopy techniques, reagents and experimental models for high content screening applied to cancer and drug-induced liver injury (DILI). Insight into experimental and analytical pipelines of an image-based screening. Ability to design a simple functional assay for screening applied to cancer and DILI. Ability to extract relevant phenotypic information from images. All the cells have different functions: they are actually different systems. We use microscopy to understand systems and how they differentiate in those different shaping states. Cells carry many essential functions: different types of cells with different functions in the body, they are kind of systems. Use microscopy to know which kind of systems. Many human genes for basic functions of life remain to be discovered. With microscopy and fluorescence we can identify the different stages of the cell cycle. Only 100 genes with a demonstrated function in mitosis while expected that more tan 1000 genes should play a role. With the imaging we can already understand a lot of the cell cycle process. What is phenotypic difference? Systems microscopy: advanced image based screening techniques for systems biology. Why do we do that? There are different developments in microscopy, we can target different proteins and detect this with the microscope. Recent developments in light microscopy: - Versatile fluorescent probes; - Cell microarray platforms; - Automated fluorescence microscopy; - Quantitative image analysis; - Automated data mining. Systems microscopy: a new research strategy, which facilitates systems biology analyses of living cells. systems microscopy: - From focused studies aimed at quantitatively elucidating detailed molecular mechanisms within specific cellular sub-systems. - To genome-wide RNAi/gRNA screens exploring the comprehensive networking of cellular processes, with the number of parameters recorded ranging from several to hundreds. Light microscopy Light microscopy concepts: Multiple colour FPs: Multicolour live labelling: Fluorescence image of a living HeLA expressing fluorescent protein based markers that highlight different structures: actin (cyan), endoplasmic reticulum (green), Golgi (yellow), mitochondria (orange) and peroxisomes (red). For instance: to track back every neuron in a brain slice. Basics of High throughput fluorescence microscopy: Multi colouring imaging in 2d 3d or in animal, you have FRED microscopy (used in high content screening more and more), FRAP microscopy (handy to understand dynamic of proteins), FCS (to difficult for now). Sample preparation on well plate, plat on microscope, than imaging, is it fixed or is it live? How many samples per well? This needs to be analysed and the data can be put in a model. (Live)-cell imaging: choose the right technique. Fluorescence techniques in live cell imaging: https://www.leica-microsystems.com/science-lab/topics/basics-in-microscopy/ High-throughput fluorescence: Multicolor, 2D/3D and time lapse microscopy Using green fluorescence proteins (basic): looking at substructures. Why invasions moving so fast in tumor cells? Multicolor: e.g. matrix adhesions turnover and actin dynamics. 2D: e.g. cell migration. 3D: e.g. tumor cell invasion. Time lapse: e.g. amoeboid cell movement visualized with two-photon microscopy in the primary tumor of a mouse. First technique: cell migration and invasion in cancer progression. Substructures with green fluorescence. You can also look at actin dynamic with N0chery. You can see how cell(population) will move all around and together, if they make interaction or not. We can analyse migrating cells in animals and in tumor tissues (with mouse models). FRAP (fluorescence recovery after photo bleaching) microscopy Protein turnover (to understand the dynamic of proteins). You look in time at the recovery and you look at 1 protein: the bleached site is dark and when it recovers fast in the dark region, it means that the protein is very mobile. So you first bleach some areas and then you look at how fast those black areas get there fluorescence back (recovery), if this is really fast, than you have a very mobile protein. This will also help to understand certain processes, dynamics in structures for instance. If a protein is very stable you can see this back at the recovery, because then the protein is not very mobile and the protein is also very stable at the structure. You can use this for high content screening. FRET (fluorescence resonance energy transfer imaging) microscopy (we will push this forward in the lab) Spatio-temporal dynamics of intracellular signalling: very powerful: identification of individual cells and identify signalling pathways. To understand signalling pathways of a single cell (phosphorylation cascades activated by a kind of growth factor). You have a donor (for instance CFP), you excite this donor with wavelengths. And if the acceptor and donor are close to each other, you have energy transfer from the donor to the acceptor. Emission of YFP if they are close to each other. this is especially developed for kinases. Intramolecular FRED, you can visualize live in your cells the activity of your kinases. Then, you can follow the signalling cascades in your cells. Now, you have a lot of available intramolecular FRET biosensors for cancer research. These are also more and more used by the pharma industry. FRET sensors for apoptosis, caspase activation, importantly for cancer progression: Akt and Erk. You can also follow the metabolism of the cell using FRET biosensos. Image based systems biology We use different omics to understand a certain system. Understanding of image based -transcriptomics (transcriptors and RNA and expression of genes), -proteomics (map expression of proteins in certain systems), -metabolomics, or monitoring of signal transduction. Image based omics enable us to viusalize live or not at the cellular level what these different oms are. Image based transcriptomics: Use image analysis to recognize the expression level of certain genes at the single cell level (with fluorescent probes). Outline of image-based transcriptomics using bDNA sm-FISH: cultivate cells and experiment in 384 well plates branched DNA single-molecule fluorescence in situ hybridization detect single transcript molecules and organelles quantify transcripts in thousands of single cells. Image based proteomics; looking at protein expression: Biochemical perturbations signal transduction gene expression protein expression (BAC/CRIPR/Cas 9 technology). We can visualize this with the BAC technology. BAC technology: insert in cells under endogenous promoter certain proteins and visualize this under the microscope. You can see the translation of your protein. really live proteomics. Novel assays for high-content screens: You can see live the translation of your protein. really live proteomics. Image based metabolomics (FRET): Use of inserted sensors. When glucose is inserted in the medium, the FRET signal increases (in this case you have decay of FRET). You have this for many many sensors. You look at cells that are migrating. So what is the metabolic signature of your system? Image based monitoring of signal transduction (FRET) (to see the signal transduction live in cells): even more powerful FRET technology. To visualize live phosphorylation cascades. Activated by a kind of growth factor (e.g. a sort of kinase). You have also FRET bio sensors for this. Inserting growth signal you can see that FRET is activated. Now the do it in 3D and animal, so you understand a sort of system. Fluorescent probes available for all kind of applications/functional assays: HCS pipeline: from sample preparation to hit calling. The way we do it or pharma companies do it. We screen different type of libraries. High throughput screening: HTS is a method that uses automation and large dataset processing to quickly assay the biological or biochemical activity of large numbers of compounds, proteins or genes. - Small molecule libraries. - Protein libraries. - siRNA (functional genomics)/shRNA libraries.: knock down of proteins, look at the phenotype and this can tell something about these proteins. - cDNA libraries: by overexpressing genes, discover new compound to inhibit a certain pathway. - chemical compound library: identify new compounds to block a certain pathway. pharma companies use this. Delineating gene functions, discovering new drugs and assessing compound safety. Screen pipeline: optimization of exposure and knockdown, what si the best set up to image, what kind of microscopy do you need to use, image processing is also very time consuming. Once you have developed your assay then you can do your screen, normally with automation you can do this in weeks or in a month. Afterwards there is data analysis to define hits of new compounds, this is also time consuming, you have many images and you need to process your data. It is time consuming to define hits for compounds. Data analysis: this is what is time consuming. Segmentation process is also heavy and needs to be optimized every time. If you have a good segmentation, than you only have to script in R your data input. Cancer drug discovery: computer tutorial: identification of anti-(proliferative)-cancer drug. Hallmarks of cancer: uncontrolled cell proliferation (typical for cancer progression). Explanation why you have tumor evolving. MAPK signalling cascade in cancer progression. Crucial kinases that are involved: those are kinase signalling cascade. One of those kinases is Erk (studied a lot in cancer research). Fact: Erk activity controls cell proliferation in breast cancer progression. - What type of image based screen could you design to discover an anti-proliferative compound? FRET analysis in order to see if Erk is activated or not. Cell proliferation inhibition with cell number, you stain nuclei and you plate your cells on day 1, control situation should end up so far. - What type of image-base screen could you think of to discover specifically an ERK inhibitor? (which reduces cell proliferation). FRET biosensor which reports to you kinase activity, when it is active you have a high FRET signal. If you use your compound library, you have compounds with high or low FRET and low cell number. In highly proliferative cells, you have highly present Erk. This is what you want to do in your cells with image based screens. ERK biosensor for signalling dynamics (for ERK activity). When Erk is active, it gets phosphorylated and it interacts with its substrate (growth signal) and you get a high FRET signal. FRET signal for Erk: EGF simulation so high FET levels, you can visualize your kinase activity. Screening for Erk-mediated cell proliferation inhibition. You use different compound concentrations from low to high and you visualize when the FRET signal decreases, than you have a compound for Erk inhibitor. This is intramolecular FRET. The way the sensor is designed, is with one donor and one acceptor for the FRET. Drug Safety assessment: Cells that are exposed to toxic compounds, the organelles will response to this (especially the mitochondria, ER, nucleus and Golgi will react when there is a stress response). And the way how they react to certain concentrations of the compound, you have a biological outcome which can be cell survival or cell death. So you have different classical responses to cell injury: - Concepts of cellular signalling (post translational modification; including phosphorylation and ubiquitination). - Protein injury (endoplasmic reticulum: unfolded protein response). - Oxidative stress/inflammation (cytokine and xenobiotic: NFkappaB and Nrf2). Adaptive stress responses and drug induced liver injury (DILI). Different stress responses. When its is switched on you get less ATP and more reactive species, you have different outcomes (necrosis, autophagy, apoptosis, or differentiation, this is called cell fate). KEAP1/NRF2 antioxidant stress response: Key proteins involved: keap1, Nrf2. Nrf2 translocation from cytoplasm to nucleus. Fact: the KEAP1/Nrf2 antioxidant stress response pathway is triggered during DILI. - What type of image based screen would you design to unravel the signalling networks that control the KEAP1/Nrf2 pathway? o How to experimentally visualize this stress response? Visualisation by GFP protein and we can see how the stress response can be triggered with microscopy. o How to discover new regulators of this specific pathway? Screen with library of siRNA’s and you visualize the stress response and you knock down a lot of genes (whatever you want), and you see if the stress response is modified, than you identify the main regulators. You visualize live cefotaxime expression. If you have all the individual data: Integration of image based “omics” for data modeling. RNAi screening (genes/phenotype) Quantitative in vivo imaging (biophysics) (proteins/localization Modeling/validation (networks/molecular mechanism) interaction) 8. Safety assessment of candidate drugs Study objectives: - Knowledge on the terminology of the different types of adverse drug reactions. - Ability to explain how cellular stress response pathways can determine the switch from adaptation to adversity. Ability to explain the strategies and application domain of fluorescent protein reporter cell models that represent cellular stress response pathways. Ability to define the different applications of imaging-based compound screens and RNAi screens to understand the biology of adverse drug reactions. Background of adverse drug reactions: Early in pre-clinical development of drugs. Optimize target with good pharmacokinetic properties needs to be safe. How can you know this early in drug development? Medicines (drug compounds) and unwanted side effects. - Un wanted side effects of drugs (Adverse Drugs Reactions [ADR] are an important problem). - 5% hospital admissions are due to ADR. That is a quite large proportion. - 6.7% of patients in the hospital develop ADR (in the clinic). This can be of any kind, severe and little things. - Classes of drugs that cause ADR: anticancer drugs (a lot of ADR: hair loss), immunosuppressive (more susceptible for inflammation), antibiotics. - ADR is also an important cause of the failure of drug development. Some drugs cause for more unwanted side effects than other drugs, for example you have more ADR with anti-cancer drugs than with paracetamol. These adverse drug reactions you already want to discover in the pre-clinical phase. Because if you are already on the market, you will lose a lot of money (if you find ADR in that phase). Therefore, you want to invest millions of money into models. The drug discovery pipeline: 10,000 compounds in drug discovery phase, 250 compounds in pre-clinical phase, 5 compounds in clinical trials to 1 FDA approved drug. This pipeline duration is about 15 to 20 years. Success rate of drug development is really pore, you want to increase this. There are reasons for why this is pore. 11% of all tested drugs fails. One of the reasons is that the problem is in the pharmacokinetic property of the drugs. You need drugs with better kinetic properties, later they designed drugs in this proper way. Nowadays, the biggest problems are clinical safety and toxicity. We have to spend time on this, and find novel tools for the safety assessment. Mostly the toxicity arises in the liver. Adverse effects of drugs due to liver toxicity and steps: a lot of drugs. You still have drugs on this list that you can use, but still have a warning when you take an overdose for example. The liver is an important target organ where you see these side effects are appearing and we still don’t know what actually the cause is. All these drugs were tested in animals and entered the clinic and the toxicity was not seen in in vivo models. There is something in the human situation where we need a better understanding of. We need to make predictions about long term safety. Reasons of drug attrition: Risk benefit ratio: determines if a drug can get to the market. - Man – understanding of pathophysiology is faulty. - Efficacy – no significant effect on a clinical disease process. - Toxicity – long term safety is still totally unpredictable. - Bioavailability and half-life – half-life cannot be predicted, only guessed. - Metabolism – drug/drug interactions; parent or metabolite. Solutions to reduce high drug attrition rates: - Improve our ability to explore and understand human disease processes. - Better target identification and validation. - Improve the predictive power of toxicology: develop in vivo models that are closer to the human situation that allows us to predict the possible onset of liver toxcitiy in humans and therefore prevent the development of compounds that are toxic and have to be removed from the market. - Achieve a more precise drug metabolism and pharmacokinetics (DMPK) assessment. Classification of mechanisms of toxicity: if you have a chemical structure, how can it affect your cells? Toxicity Definition Example On target or mechanism Toxicity due to modulation Statins, EGFR inhibitors related toxicity of the primary pharmacological target (e.g. Receptor, enzyme) In the same tissue or not Off target pharmacology Adverse effects resulting Terfenadine and hERG from interaction of drug with channel effects (in cardiac targets other than intended cells) therapeutic target Hypersensitivity and Hypersensitivity refers to Penicillin (antibiotitcs) immunological reactions undesirable (damaging, discomfort producing, fatal) reactions produces by the normal immune system Bio activation to reactive The biological Acetaminophen intermediates transformation of a drug in (paracetamol) toxic metabolite, which often results in organ or tissue-specific toxicity Idiosyncratic toxicities: its Rare toxicities that are Nevirapine, isoniazid popping up, but we cant thought to represent unique predict it. 1 in 10000 susceptibility of affected individuals will cause toxicity individuals From drug exposure to toxicity: Interaction with molecule in the cell: molecular intitiation event. This can be with a protein, or a lipid where this compound binds to. These responses can be acute: high doses and in few days high severity in your tissue. Mid term: develop hepatology with prolonged treatment, due to longer drug exposure. Long term: cancer of course, you take a drug now, it develops dna damage and in 40 years you have cancer. These compounds are screened out. What is happening in the cell, what is monitored and what can be used to identify drug toxicity? Adaptive stress response pathways and adversity From drug exposure to adversity: You have a drug and at some point you have toxicity. In the past: they exposed animals, cut of the tissues and looked at cellular toxicity. For instance accumulation of fatty acids in the liver. So we don’t know how it was caused, only that something happened. We want to dive into the cellular level what is happening, what are the responses in that cell? Adverse Outcome Pathways (AOP) concept: Stress response pathways that cope with the cellular injury. Normal physiological responses: cellular adaptive … that are switched on. Then there is a balance between trying to repair the cell and between dying at some point. If the last one occurs, you have all signalling programs that cause this cell death. Can we use this information to predict certain side effects? Standard: use of test animals: In vitro model systems for safety testing: Usage of something different than a test animal: you need something that is cheap, efficient and predictable. How far is a cell line sufficient predictive for what in an organ will happen? In vitro model systems for safety testing: Use these models to predict toxicity. In lab, very simple: (tumor) cell lines. The models, test many compounds with many concentrations. When it gets complexed you have less throughput (less material available). What are the stress responses that take place, and can we connect them to use them for prediction. Switch from adaptation to adversity by cellular stress response pathways Drug induced toxicity: from adaptation to adversity: first adaptation but with a higher compound concentration this will lead to adversity (cell death). - Oxidative stress. - ER stress. - Etc. When two pathways or more are connected, than a lower compound concentration will lead to cell death. Is there a relation between concentration and activation of pathway and onset of cell death? Adaptation: trying to adapt to a normal situation, when you need to adapt more (when there is more compound concentration), suddenly there is a knock out, wich is adversity (you can no longer adapt, the cell will die). This is may true for oxidative stress, but this is also the cause during ER stress. When there are two pathways activated by a compound, than the situation is much worse. And there will be knockout even faster. If there are multiple pathways activated, it gets much more sensitive. We want to know how these pathways are regulated. What are the critical genes that regulate this pathway and is there susceptibility? Then we also want to understand this in the context of all these different models. Is it representative what is happening in a human cell, when it is exposed to drugs? How do we take this approach: For instance if there is dna damage, a signal and pathway are activated and then you can repair. Pathways of toxicity high content imaging platform: The concept: All the damage at specific points have specific pathways to recover those damages. But also maybe injury in the cell can cause changes in the structure of these components. In the lab we build cellines that have reporters for these pathways. So that you can see under the microscope if a pathway is being altered or that a structure is changing. Than we can learn how a chemical will react with a cell and if this will be in the end be predictive. We have bacterial artefisial chromosomes, which contain pieces of the human genome. In one piece you have 1 gene containing the reporter. We use this construct to insert a combination with GFP. We integrate GFP at the N or C terminus (normally C-terminus), we can use this for localization. We integrate this in HEPG2 cellines and then make stable linces (clones) and see if it contains the construct and can we activate a pathway and do we see GFP lighting up and is it located where it should be located? BAC GFP trans genomics for reporter cell generation: BAC (150 kbp) transfection + G418 selection for stable integration in HEpG2 cells integration of GFP sequence in gene exon. From 1 construct we have 10 or 15 subclones and in the end we use 1 of these subclones for further studies, but this is quite labor intensive. In the liver it possible to incorporate this. Reporters can say something about the kind of damage and about the severity of this damage: Oxidative stress reporter, unfolded proteins stress response reporter, inflammatory response reporter, DNA damage reporter, mitochondrial morphological reporter, ER morphological reporter, and more reporters. There are more than 50 different candidate reporter cell lines. With image acquisition you can see the dynamics of these reporters. A quantitative manner for quantitative analysis is image analysis and with informatics you can see what is actually happening. Quantitative single cell data to classify compounds in these reporters. We have now more than 50 of these reporter cell line. What type of reporter can we use now to better predict things? We do this in the cell observatory Future: knowledge of biology and knowledge in how to work with the data. High content screening at the cell observatory: - Lab automation: to capture information from the images (24 well plates, over night we analyse this every hour for an entire plate, than we can follow the dynamics). - (intelligent) imaging. - Image analysis. - Data visualization. - Data mining. - Assay development. The image acquisition – analysis pipeline: to extract information from individual cells and from every individual cells we get quantitative information about the reporter activity. Then we use R to extract the information from all the data. The power is now to combine biological information with ifnormatics to extract that information and to say important things in the end. Image acquisition: laser scanning confocals image storage and management image analysis: CellProfiler and ImageJ (loading and metadata nuclear segmentation nuclear identification cell identification cytosol identification nuclei tracking) automated processing and analysis: R: - Nuclei tracking. - Single cell feature correction. - Time responses. - Feature correction bar plots. - Feature correction x-y plots. - Population feature correction. We are building these reporters in the content of the key toxicity pathways. To recognize with a sensor that when you have oxidative stress, than often a downstream (transcription) factor gets activated, this will activate the gene transcription and these genes will recover the toxicity. This is typically the way it works. Any kind of stress: you have these sensors. There is already a lot known, we know what the regulator, transcription factor and target gene for these pathways is (and is described). We can use this existing knowledge. Key toxicity pathways Oxidative stress Regulators Keap1 Transcription Nrf2 Factors Targets Srxn1 ER stress ATF4/XBP1 Inflammation IkBa NFkB DNA damage 53BP1 P53 CHOP/BiP ICAM1 P21/MDM2 Can we use transcriptomics data? Transcriptomics data: changes in the expression of genes: toxicogenomics. We use the data to see what type of biological pathway is being affected. And for each affected pathway you get a p-value (a statistical score). All the pathways that are being affected, in the figure you see blue and the bluer means the more affected. You see that first of all that not all pathways are being affected. Only particular pathways are being affected. These dili compounds have a specific response that triggers a certain network. The aim now to dive into these networks and see if there are molecules that we can use that are not yet part of the set that we had and introduce components of these pathways in reporters as well. This is what we are still working on. Now you can do with high throughput methods, at what concentration you will activate a certain pathway. at the dose response you can see the sensitivity, if it is not activated after that time point anymore than you have reached the “ceiling” of the activation. You don’t want to be near that “ceiling” because that is scary of course. The transcription factors are typically in the nucleus. We want to identify the intensity of the GFP. How will we use these reporters to say something about drug exposure and to unravel the signallers that control these pathways. If all the individual pathways detect what they should detect. We need to find the mode of action so we need to discriminate. So we exposed all our reporters to compounds that are specific for a particular pathway (or at least this is what we anticipated). For different compounds in the dose response you see that a certain compounds is primarily activated. You want to take this information and plot it in such a way that you can easily see a discrimination. So the compound that is causing a certain stress is clustered together for the reporter that belongs to the type of stress. We can identify pathways if we see that there is a perturbation, that would allows to predict a certain mode of action. Clustering analysis: In a dataset you can actually see if there are compunds that would activate certain genes. this would be reflected for its stress pathway. we can then say to pick the top 10 compounds that gives the highest induction, you do this for 3 pathways. Let’s see if the same compound activate the pathways and reporters. test all compounds in reporter lines for 24 hour exposure. We can pick up these responses in our HepG2 models. How can we apply this? Safety assessment using stress response reporters: Pilot drug safety screen of DILI assessment: can we determine the cellular stress response caused by DILI compounds with our cellular stress response? ~ 150 DILI related drugs: - Severe DILI. - Non severe DILI. - Non DILI. Monitor compounds and see if there is induction for your reporter with live cell imaging. Some of the compounds have similar strong responses with model so you are close to the ceiling of the response. Interestingly, you can also see first activation but than it moves back again this is a particular pharmacological effect. There are multiple markers for each of the readout. You hope to see a nice dose response in the reporter activation. We have this information of all the reporters, all the cell lines and for all the compounds. We also have reference compounds and they seem to show no treatment (but they are reference, so we expect this). We also screen reference compounds to see if we expect what we would see. The clustering of a lot of compounds (hierarchical clustering > 180 compound responses): than we can cluster compounds that have a similar effect on the cell biology in the stress response. This allows us to learn something about the mechanism and where do they have an effect in the cell. We need to extend the set of reporters to start clustering to make a distinction between less, normal, and more severe dili. To rebuilt the platform we can make stronger predictions. This is all in 2D. Maybe in a more differentiative stage we can pick up repsonses that we would otherwise not would pick up (in the 3D). If you have hepG2 cells on a plastic plate you have 2D cultures, but if you plate them on a certain gel, you get 3D speroids and they stop proliferating. In 2D you don’t have these structures. In 3D we see structures appearing, subsequently we see differentiation in these structures (formation of the bionucleur structures). All the reporters form these structures in 3D. we can culture these reporter bionuclear formation for 4 weeks to track exposures. We than see actually stress response activation in these reporters (so we use these reporter systems in 3D). Advantages if we culture them up to a few weeks, we can to repeated exposures. This is how pateints are being treated (you can see the effect of multiple exposures on the pathway activation in these 3D differentiated systems). We tested them for control compound and we can pick up reporter activity for these molecules in stress pathways after repeated dosing. How can we understand these pathways better in itself? There are genes that regulate these networks and who define if you get a proper activation or not. That maybe fine whether you are more susceptible to injury because this pathway cannot be effected effectively and therefore you cannot protect yourself sufficiently. There are multiple ways how these networks are regulated. So there is an entire set of genes that regulates the activity of signalling programs. We saw that for kinases with crosstalk. Complex networks require regulation. Do we see an activation of the DILI pathway when we analyse the DILI compounds. This pathway is in physiology highly important: Activation of the Nrf2 response by intrinsic hepatotoxic drugs correlates with suppression of NF-kB actiation and sensitizes toward TNF-alpha induced cytotoxicity. How does this work: Keap1/Nrf2 antioxidant response pathway. normally: translation of Nrf2, that directly binds to Keap1 and Keap1 will ubiquitinate Nrf2 then Nrf2 will be degraded by the proteasome and there is no longer Nrf2. This half life of Nrf2 is 10 minutes, so the turnover is continuous. If you have ROS from durgs, they modify the residues of Keap1 so you switch the pathway, in this condition Keap1 can no longer ubiquitinate Nrf2 and you get a stabilization of Nrf2, because of the high turnover it can no longer be degraded so it transfers to the nucleus and targets cell defense genes. importantly, we can make nice dose response curves for this. CDDO-me to identify novel regulators of the pathway. are there components that are involved in the pathway somewhere else? Is there something known about regulation? There already have been identified kinases that can phosphorylate Nrf2 and thereby modelate the activation of the molecule. This is called post translational modification, this is ohosphrylation and ubiquitinalion. miRNA can also target the messengers of Nrf2 and this will affect the translation process. There are also other transcription factors that have to work with Nrf2 to allow efficient transcription of target genes. in the cytosole Nrf2 can also bind parters that will define its activity. So there are various players known that can modelate this network. We want to know if there are additional molecules that we can try to identify who also regulate this pathway for the understanding of the regulation of this Nrf2 pathway. For this we use RNAi screening (to identify NRf2 pathway modulators). We have siRNA libraries that contain: kinases, phosphatases, transcription factors, epigenetic regulators. In the screen we used CDDO: Phase 1(primary screen): siRNA knockdown (if we knockdown these genes, do we see an modulation), smartpool mix in Srxn1-GFP cells for 72 hours in 96 well format. Phase 2(primary screen): exposure of Srxn1-GFP cells to CDDO-Me 30 nM, fix after 7 hours for 7 or 24 hours and can we identify now when genes are knockddowned if they enhance the response or if they block the response? This would only work if we would have nice controls. This genes have to be dependent on Nrf2. Srxn1-GFP reporter is as expected dependent on Keap1 and Nrf2. z-score (sort of p-value): statistical value about the effect of a knockdown. If it is really negative, than you inhibit the reporter activity, if it is really positive than you enahce the response. We use this condition in the screen. So using this screening set up we can identify genes that modelate the pathway. these screens are with smart pool mixes (set of 4 individual siRNA’s), maybe 1 of these 4 is casuing a faulty effect. We used thes 4 single siRNA’s and then we asked the question: if 2 out of those 4 give the same effect we believe that it is a 2 effect. And if its only 1 out of 4 we say it can be true, but there is a likelihood that it is not true. We do these experiments in the context of DILI: if we identify the genes, can we find polymorphisms to see if some genes are more susceptible. If we take all the suppressor genes (genes upon knockdown who enhance the response, but in normal conditions damp the response). Same genes have same effect on same compounds. For the enhancer genes, the effect on other drugs have the same effect. We identified a set of genes that regulate the NRf2 pathway no matter what compound you use. We can complement this information, the genes will fit in the network. Next step: what is their role and where are the localised. To translate hepg2 cells into in vivo situations. By moving away of morphological to mechanistic understanding and applying this in reporter system, we can learn something about the effect of candidate drugs and how the networks are regulated. 9. A pipeline spanning in vitro to in vivo animal models for preclinical cancer research Description of 3 example how we use this pipeline in the lab to indenitfy gene/proteins that can be certain targets. Study objectives: - Knowledge of the general approaches used in DDS for identification of candidate cancer drug targets. - Insight in the advantages and limitations of the different models used in the cancer drug target discovery pipeline in DDS. Drug target discovery. To discover molecule pathways were a drug can target on. How do we find concepts and processes where drugs can act on. How cancer cells are able to migrate. Tumor cells are very plastic, they can move very easily and they can easily switch to another and different way to growth further. In the lab at the cell observatory we use a pipeline, for high content screening, contianing: lab automation, (intelligent) imaging, assay development, data mining, image analysis, and data visualization. Translate genes in in vivo models and how they correlate with patients. Most interested in: how do cells move in a 3D context, when they are within an extracellular matrix? And how they move and crawl into blood vessels for instance. We pipet tumor cells into an extracellular matrix and then we make arrays of small mini tumors, here you can look in 3D into the cells (tumor spheroids). Look at actin site with GFP marks. Robotics automatic way to look at cell migration in 3D. SYK in RA and lymphoid malignancies. Syk is a kinase in the context of diseases of the immune system. So that glucocides and lymphosides become cancer. Syk works downstream of b-cell receptor, leads to proliferation or differentiation. So often present in cancer. Syk inh: - Non Hodgkin lymphoma. - Chronic lymphocytic leukemia. - Rheumatoid arthritis. Syk knockdown: cells are no longer able to migrate. Zebrafish embryos (not ethical considered as animal, animal model we use in this assay): assay of mm zebrafish embryo with blood vessel system. Inject labelled tumor cells in embryo, follow with automated imaging, and we follow the growth of the tumor. We can do 100 of embryos in 1 experiment. How far do the tumor cells grow in the embryo? With increasing aggressiveness. We knockdown syk, there is a drop in ability to move. Next validation step: before we put this in a mouse model, is this relevant for prostate cancer? Why would we invest in this? If we look at large datasets. The more aggressive the prostate cancer, the more syk protein expression. based on this we move to the next phase, the mouse model. Syk knockdown, we block ability to grow. The experiment is effective. Can we use inhibitors, to prevent metastasis and can we say that there are already inhibitors available that are now in the clinics for other diseases that we could also use for prostate cancer? Two stories on how we find genes that control the metastasis of breast cancer genes? First story: integrins. Integrins are the feet of our cells (for the cellular movement in the matrix). Integrins cross the cellular membrane and they touch the extracellular matrix and the intracellular … integrins are all clustered in this extracellular matrix. They interact with fibrin. Integrins important for growth of tumors, if you block integrins, and if you combine this with radio/chemo therapy the tumor shrinks. There are also models in types of cancers where if you knockout the beta 1 integrins, there is more progression of the tumor. So even if integrins are important for growth, in some conditions they also inhibit the metastasis. Sometimes when you block the beta 1 integrin, they don’t stop to move, they just move in another way. There are some (breast) cancer cells who don’t care if you knockdown the beta 1 integrin or they are so much affected that they stop growing and don’t move anymore. In triple negative breast cancer (they don’t have the targets that available drugs target, so they are very difficult to cure). Those breast cancers, normally they move with branches, but when you block the beta 1 integrin they move as single cells. And in some cancers, we see the growth effect and in others we don’t. We move now from the in vitro to the in vivo zebrafish. If we look at the single cell level, this is more effective for our in vivo model. Now we look at a mouse model (for the proper context), human or mouse breast cancer cells and we put his in the breast tissue of mouse. If we look at the growth of the tumors, the wild type tumors grow really big and beta 1 integrin knock down tumors grow really small. So this is what we actually already reported. However, if we look at the ability to metastasize, the movement (to for instance the lungs), and you look at the beta 1 integrin, the metastasis is much more increased if you remove this integrin. The cadherins (the hands, that keep the cells together): there seems to be crosstalk between the integrins and the cadherins (between the feet and the hands). When you remove the beta 1 integrin, there is a drop in E-cadherin (transcriptional regulation of E-cadherin by beta 1 integrins), they basically loose their hands. So also downregulation of beta 1 integrins leads to decreased E-cadherin surface expression. If you knockdown the beta 1 integrin, there is an increase in metastasis and if you then restore the expression of E-cadherin, metastasis goes down again: downregulation of E-cadherin required for enhanced metastastic capacity upon beta 1 integrin depletion. This is also the reason why these cells are so highly metastatic. We force these cells to go into the EMT, the epithelius mensymal transition. So how do we know if the screened genes and proteins are really important is where we look at. Second story: SRPK1 kinase. This kinase has two lobes, it interacts and regulates spliceosome factor and thereby it regulates splicing and mRNA export. This kinase is identified by phagokinetic track assay (phenotypic cell migration screen). This is used for screens, trying to find important genes for the ability of breast cancer cells to move. And one of these screens is SRPK1. Normally it forms nice tracks, if you knockdown SRPK1 it doesn’t move and just stays there. So SRPK1 is important for migration identification. All the measured parameters tell something if they move and how they move, do they move single cell or chaotic or linear. We look at all these ratios. SRPK1 was one kinase that was identified in this screening. We screen by using SMARTpool deconvoltion (very effective): you look at siRNA’s individually, do we see the same phenotype? If there is a validation, this is a good confirmation. Then we used random cell migration: 2D surface, we look at the cells moving to the 2D surface and when you look at them, how fast and how much do they move? This tells us something about a quantitative fashion. Why do they stay and sit at the same place when you knockdown SRPK1. Why is this? Zoom in at cell matrix adhesions, they are highly dynamic. If they are completely static, the cells are unable to move. So they need to be able to dynamically regulate the adhesions. So if you knockdown SRPK1 the adhesion goes down and it can no longer move. This was enough for 3D assays and for zebrafish in vivo. Then we went into the mouse in vivo with the same experiment. You look at breast cancer in it natural content. If you look at growth of the tumors, this is not really affected by the knockdown of SRPK1. If you look at metastisis, this is affected. Metastasis of cancer is the most deadly part of cancer: the spread and resistance of cancer. 3D models to look at the tumors: to mimic the actual physiology. But we use a combination of simple systems (like a well plate with tumor cells), because the simple tumor cell plate is easier to work with. Blocking integrins will not stop the tumor growth, the tumor cells will find another way to grow. This is due to its plasticity.