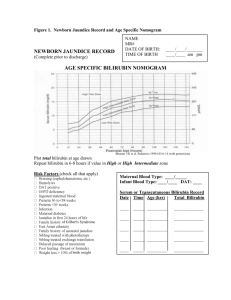
Jaundice is the visible manifestation of increased level of bilirubin in the body. It is not a disease rather a symptom of diseases. In adults sclera appears jaundiced when serum bilirubin exceeds 2 mg/dl. However it is difficult to see sclera in newborn due to difficulty in opening eye. But in new born it is very easy to see jaundice in skin. Important problem in the 1st week of life Almost all neonates (60% Term and 80% Preterm) will have bilirubin > 5 mg/dl in the 1st week of life and become visibly jaundiced, vast majority being benign Some of the term babies (8 to 9%) have levels exceeding 15 mg/dl in 1st 7 days of life. High bilirubin level is toxic to the developing CNS A women who delivered at home presented on her 5th postpartum day at pediatric OPD complaining that her baby looked yellow. Hyperbilirubinemia in the first week of life is usually of the indirect variety. 1. Appearing at birth or within 24 hours of age › Hemolytic disease of newborn › Infections: intrauterine viral, bacterial; malaria › G-6PD deficiency 2. Appearing between 24-72 hours of life › Physiological › Sepsis neonatorum › Polycythemia › Concealed hemorrhages: cephalhematoma, subarachnoid bleed, IVH. › Increased enterohepatic circulation 3. Appearing after 72 hrs and within 1st week a) Sepsis neonatorum (4th - 7th days) b) Syphilis c) Toxoplasmosis 4. Jaundice appearing after1 week a) Prolonged direct Jaundice › Neonatal hepatitis (common) › Extrahepatic biliary atresia › Breast milk jaundice › Metabolic disorders › Intrahepatic biliary atresia › Amino acid toxicity › Inspissated bile syndrome (uncommon) Jaundice appearing after1 week contd… b) Prolonged Indirect Jaundice › Criggler Najjar Syndrome › Breast milk jaundice › Hypothyroidism › Pyloric stenosis › Ongoing hemolysis, malaria On history, the baby started turning yellow on his 2nd day. The baby was a full term male child delivered at home. Baby is currently 120 hours old. There was no history of any maternal illness during pregnancy. Delivery was uneventful. Baby immediately cried after birth and was immediately breastfed. Baby passed meconium on his first day. Urine is normal with no staining of nappies. Stool also is normal in colour. On past history, there was no H/O history of malaria during pregnancy. On family history, there was no H/O of jaundice, liver disease. Previous sibling had no history of neonatal jaundice. Baby was well looking, feeding well, vitals were normal, temperature was normal. There were no rashes and petechiae in the body. Baby weighed 3 kg. Icterus was present. Pallor was Absent. On abdominal examination no organomegaly was present. Chest was clear and CVS examination was normal. 1. 2. Dermal staining (By karmer) progresses from head to toe › Examined in good day light skin of forehead, chest, abdomen, thigh, legs, palms, and soles › Blanched with digital pressure and the underlying color of the skin and subcutaneous tissue should be noted. Transcutaneus bilirubinometer In new born babies bilirubin metabolism is immature which results in the occurrence of hyperbilirubinemia in the first few days of life. Also there is increased bilirubin load on the hepatic cell due to physiological polycythemia. Immaturity could be at various steps of bilirubin metabolism like: Defective uptake from plasma into liver cell Defective conjugation Decreased excretion Increased entero-hepatic circulation First appears between hours of age Maximum intensity seen on 4-5th day in term and 7th day in preterm neonates Does not exceed 15 mg/dl Clinically undetectable after 14 days. No treatment is required but baby should be observed closely for signs of worsening jaundice. Presence of any of the following signs denotes that the jaundice is pathological. Clinical jaundice detected before 24 hours of age Rise in serum total bilirubin by more than 5 mg/dl/ day (>5mg/dl on first day , 10 mg/dl on second day and 12- 13 mg/dl thereafter in term babies) Serum bilirubin more than 15 mg/dl Clinical jaundice persisting beyond 14 days of life Clay/white colored stool and/or dark urine staining the nappy yellow Direct bilirubin >2 mg/dl at any time Treatment is required in the form of phototherapy or exchange blood transfusion. One should investigate to find the cause of pathological jaundice. Clinical Jaundice Measure Billirubin > 12 mg/dl and infant < 24 hr old < 12 mg/dl and infant > 24 hr old Follow bilirubin level Coomb’s test Positive Identify antibody Rh, ABO etc Negative Direct bilirubin Direct bilirubin > 2 mg/dl < 2 mg/dl Consider Hepatitis Intrauterine,viral,or Toxoplasmatic inf. Hematocrit Biliary obstr. Sepsis Galactosemia Cholestasis Normal or low Hemochromatosis High (Polycythemia) Normal or Low RBC morphology Reticulocyte Count NORMAL Enclosed hemorrhage Increased enterohep. circ. Breast milk, Hypothyroidism, Crigler-Najjar syndrome Infant of diabetic mother RDS, Asphyxia Infections, Drugs(eg novobiocin), galactosemia ABNORMAL Spherocytosis Elliptocytosis etc. ABO Incompatibility Red cell enzyme def Alpha thallasemia Drugs(eg penicillin Investigations were done. Serum total bilirubin was found to be 10 mg/dl. The baby was diagnosed as a case of physiological Jaundice. Parents were counseled. The baby was discharge and kept on follow up for serial analysis of Bilirubin level. 1. 2. 3. 4. Bhutani V.K., Johnson Lois H., Keren Ron Diagnosis and management of hyperbilirubinemia in term neonates for a safer first week, Pediatric clinic of North America, Common issues and concerns in Newborn Nursery, Part II Aug 2004, vol 5, No. 4 Gowen CW Jr. Anemia and hyperbilirubinemia. In: Kliegman R. Nelson Essentials of Pediatrics. 5th ed. Philadelphia, Pa.: Elsevier Saunders; 2006:318. Paul Vinod K, Deorari Ashok K, Agrawal Ramesh et all, Newborn infants, Ghai Essential Pediatrics, 2009, 147-51 Internet