Fallopian Tubes & Ovaries: Anatomy, Function, & Clinical Significance
advertisement

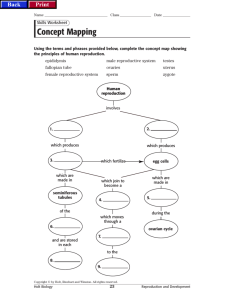
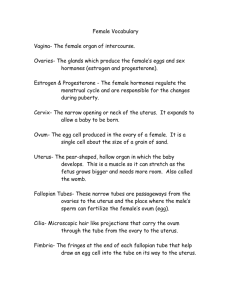
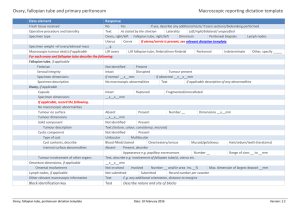
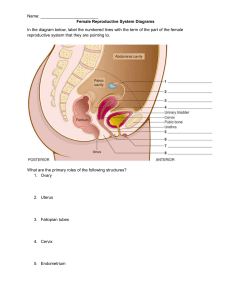
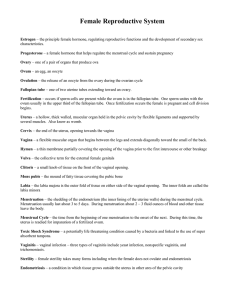
FALLOPIAN TUBES AND OVARIES BY: KSHITIZ SONI 20180179 INTRODUCTION- The fallopian tubes, also known as oviducts, uterine tubes, or salpinges (singular salpinx) are uterine appendages, lined from inside with ciliated simple columnar epithelium, leading from the ovaries of female mammals into the uterus, via the uterotubal junction. They enable the passage of egg cells from the ovaries to the uterus. In non-mammalian vertebrates, the equivalent structures are just called oviducts. STRUCTURE: Its different segments are (lateral near the ovaries to medial near the uterus): the infundibulum with its associated fimbriaenear the ovary, the ampullary region that represents the major portion of the lateral tube, the isthmus the visible medial third segment which is the narrower part of the tube that links to the uterus, and the interstitial (also known as intramural) part that transverses the uterine musculature. The ostium is the point where the tubal canal meets the peritoneal cavity, while the uterine opening of the fallopian tube is the entrance into the uterine cavity, the uterotubal junction. MICROANATOMY A cross-section of a fallopian tube shows four distinct layers, from outer to inner: serosa, subserosa, lamina propria and innermost mucosal. The serosa is derived from visceral peritoneum. Subserosa is composed of loose adventitious tissue, blood vessels, lymphatics, an outer longitudinal and inner circular smooth muscle coats. This layer is responsible for the peristaltic action of the fallopian tubes. Lamina propria is a vascular connective tissue. The inner layer is a single layer of simple columnar epithelium. The columnar cells have microscopic hair-like filaments (cilia) predominately throughout the tube, but are most numerous in the infundibulum and ampulla. Estrogen increases the production of cilia on these cells. Between the ciliated cells are peg cells, which contain apical granules and produce the tubular fluid. This fluid contains nutrients for spermatozoa, oocytes, and zygotes. The secretions also promote capacitation of the sperm by removing glycoproteins and other molecules from the plasma membrane of the sperm. Progesterone increases the number of peg cells, while estrogen increases their height and secretory activity. Tubal fluid flows against the action of the cilia, that is toward the fimbrial end. FERTILISATION The tube allows passage of the egg from the ovary to the uterus. When an oocyte is developing in an ovary, it is encapsulated in a spherical collection of cells known as an ovarian follicle. Just prior to ovulation the primary oocyte completes meiosis I to form the first polar body and a secondary oocyte which is arrested in metaphase of meiosis II. This secondary oocyte is then ovulated. The follicle and the ovary's wall rupture, allowing the secondary oocyte to escape. The secondary oocyte is caught by the fimbriated end and travels to the ampulla of the uterine tube where typically the sperm are met and fertilization occurs; meiosis II is promptly completed. The fertilized ovum, now a zygote, travels towards the uterus aided by activity of tubal cilia and activity of the tubal muscle. The early embryo requires critical development in the fallopian tube. After about five days the new embryo enters the uterine cavity and on about the sixth day implants on the wall of the uterus. The release of an oocyte does not alternate between the two ovaries and seems to be random. After removal of an ovary, the remaining one produces an egg every month. Occasionally the embryo implants into the fallopian tube instead of the uterus, creating an ectopic pregnancy, commonly known as a "tubal pregnancy". Clinical significance Patency testing While a full testing of tubal functions in patients with infertility is not possible, testing of tubal patency is important as tubal obstruction is a major cause of infertility. A hysterosalpingogram, laparoscopy and dye, or HyCoSy (hysterocontrast sonography) will demonstrate that tubes are open. Tubal insufflation is a standard procedure for testing patency. During surgery the condition of the tubes may be inspected and a dye such as methylene blue can be injected into the uterus and shown to pass through the tubes when the cervix is occluded. As tubal disease is often related to Chlamydia infection, testing for Chlamydia antibodies has become a cost -effective screening device for tubal pathology. Inflammation Main article: Salpingitis Salpingitis is inflammation of the fallopian tubes and may be found alone, or be a component of pelvic inflammatory disease (PID). A thickening of the fallopian tube at its narrow portion, due to inflammation, is known as salpingitis isthmica nodosa. Like PID and endometriosis, it may lead to fallopian tube obstruction. Fallopian tube obstruction is associated with infertility and ectopic pregnancy. Cancer Main article: Fallopian tube cancer Fallopian tube cancer, which typically arises from the epithelial lining of the fallopian tube, has historically been considered to be a very rare malignancy. Recent evidence suggests it probably represents a significant portion of what has been classified as ovarian cancer in the past.[5] While tubal cancers may be misdiagnosed as ovarian cancer, it is of little consequence as the treatment of both ovarian and fallopian tube cancer is similar. SURGERY: The surgical removal of a fallopian tube is called a salpingectomy. To remove both tubes is a bilateral salpingectomy. An operation that combines the removal of a fallopian tube with removal of at least one ovary is a salpingo-oophorectomy. An operation to remove a fallopian tube obstruction is called a tuboplasty. The ovary is an organ found in the female reproductive system that produces an ovum. When released, this travels down the fallopian tube into the uterus, where it may become fertilized by a sperm. There is an ovary (from Latin ovarium, meaning 'egg, nut') found on the left and right sides of the body. The ovaries also secrete hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause. It is also an endocrine gland because of the various hormones that it secretes. The ovaries are considered the female gonads.[2] Each ovary is whitish in color and located alongside the lateral wall of the uterus in a region called the ovarian fossa. The ovarian fossa is the region that is bounded by the external iliac arteryand in front of the ureter and the internal iliac artery. This area is about 4 cm x 3 cm x 2 cm in size.[3][4] The ovaries are surrounded by a capsule, and have an outer cortex and an inner medulla. Usually, ovulation occurs in one of the two ovaries releasing an egg each menstrual cycle; however, if there was a case where one ovary was absent or dysfunctional then the other ovary would continue providing eggs to be released without any changes in cycle length or frequency. The side of the ovary closest to the fallopian tube is connected to it by infundibulopelvic ligament,[3] and the other side points downwards attached to the uterus via the ovarian ligament. Other structures and tissues of the ovaries include the hilum. The ovaries lie within the peritoneal cavity, on either side of the uterus, to which they are attached via a fibrous cord called the ovarian ligament. The ovaries are uncovered in the peritoneal cavity but are tethered to the body wall via the suspensory ligament of the ovary which is a posterior extension of the broad ligament of the uterus. The part of the broad ligament of the uterus that covers the ovary is known as the mesovarium.[4] The ovarian pedicle is made up part of the fallopian tube, mesovarium, ovarian ligament, and ovarian blood vessels. The surface of the ovaries is covered with membrane consisting of a lining of simple cuboidal-to-columnar shaped mesothelium. The outermost layer is called the germinal epithelium. The outer layer is the ovarian cortex, consisting of ovarian follicles and stroma in between them. Included in the follicles are the cumulus oophorus, membrana granulosa (and the granulosa cells inside it), corona radiata, zona pellucida, and primary oocyte. Theca of follicle, antrum and liquor folliculi are also contained in the follicle. Also in the cortex is the corpus luteum derived from the follicles. The innermost layer is the ovarian medulla.[7] It can be hard to distinguish between the cortex and medulla, but follicles are usually not found in the medulla. Follicular cells flat epithelial cells that originate from surface epithelium covering the ovary, are surrounded by Granulosa cells - that have changed from flat to cuboidal and proliferated to produce a stratified epithelium At puberty, the ovary begins to secrete increasing levels of hormones. Secondary sex characteristics begin to develop in response to the hormones. The ability to produce eggs and reproduce develops. The ovary changes structure and function beginning at puberty. The ovaries are the site of production and periodical release of egg cells, the female gametes. In the ovaries, the developing egg cells (or oocytes) mature in the fluidfilled follicles. Typically, only one oocyte develops at a time, but others can also mature simultaneously. Follicles are composed of different types and number of cells according to the stage of their maturation, and their size is indicative of the stage of oocyte development. When the oocyte finishes its maturation in the ovary, a surge of luteinizing hormone secreted by the pituitary gland stimulates the release of the oocyte through the rupture of the follicle, a process called ovulation. The follicle remains functional and reorganizes into a corpus luteum, which secretes progesterone in order to prepare the uterus for an eventual implantation of the embryo. At maturity, ovaries secrete estrogen, testosterone, inhibin, and progesterone. In women, fifty percent of testosterone is produced by the ovaries and adrenal glands and released directly into the blood stream.[16] Estrogen is responsible for the appearance of secondary sex characteristics for females at puberty and for the maturation and maintenance of the reproductive organs in their mature functional state. Progesterone prepares the uterus for pregnancy, and the mammary glands for lactation. Progesterone functions with estrogen by promoting menstrual cycle changes in the endometrium THANK YOU KSHITIZ SONI 20180179