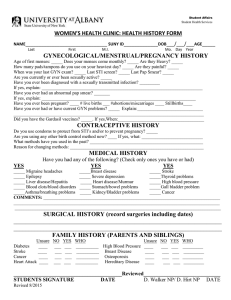
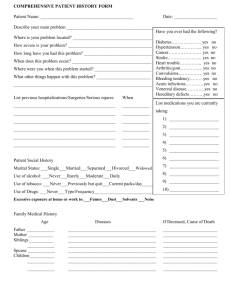
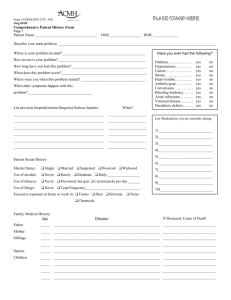
Subjective (S): Identifying Data: Intitals: A.M. Age: 24 Race: Caucasian Gender: Female Marital Status: Single Chief Complaint (CC): Patient states that she “needs her pap and refill on her birth control.” History of Present Illness (HPI): Patient is a health 24 year old white female with no known medical history. Patient has had her first pap smear when she was 19 years old. Previous pap was done in September of 2012 and was normal. She admits to only have one male sexual partner with whom she uses condoms approximately 75% of sexual encounters. Patient states that he is her only lifetime partner. Past Medical History (PMH): · Allergies: NKDA · Current medications: Tri Sprintec, one tab daily · Age/health status: 24 years · Appropriate immunization status: Up to date on all vaccines; Patient would like to receive FLU vaccine today as she receives it yearly. Refuses HPV vaccine. · Previous screening tests result: Normal pap smear in 2012. Patient’s mother was diagnosed with breast cancer at age 41, therefore mammograms are recommended to begin at ate 31. · Dates of illnesses during childhood: N/A · Major adult illnesses: No medical history · Injuries: N/A · Hospitalizations: No hospitalizations. · Surgeries: N/A Family History (FH): Patients father has a history of GERD and gastric ulcers. Mother has a history of breast cancer (diagnosed at age 41), for which she underwent a lumpectomy, radiation therapy and is currently taking an aromatase inhibitor. Patient denies any other major family history. Social History (SH): Patient is a single female who is currently attending school to obtain her Bachelor’s degree in Business. She currently works at Gulf State Park and states that it is a low stress job. Normal diet, exercises rarely. Denies the use of alcohol, tobacco or illicit drugs. Review of Systems (ROS): 1. Constitutional symptoms- Patient denies fatigue, fever, chills, malaise, night sweats, unexplained weight loss or weight gain, loss of appetite, difficulty sleeping. 2. Eyes- Patient denies blurred vision, difficulty focusing, ocular pain, diplopia, scotoma, peripheral visual changes, and dry eyes. Patient states she does wear contacts. Date of last eye exam was August of 2014. 3. Ears, nose, mouth, and throat- Patient denies vertigo, headaches, sinus problems, epistaxis, hoarseness, dental problems, oral lesions, hearing loss or changes, nasal congestion. 4. Cardiovascular- Patient states she rarely exercises. Patient denies any history of heart murmur, chest pain, palpitations, dyspnea, activity intolerance, varicose veins, edema. 5. Respiratory- Patient denies cough, SOB on exertion, difficulty breathing, wheezing, pain on inspiration, exposure to passive smoke, history of respiratory infections, exposure to TB, hemoptysis. Patient states she has never had a chest x-ray. Her last TB skin test was done in January 2012 for work and it was negative. 6. Gastrointestinal- Patient denies dysphagia, reflux, pyrosis, loss of appetite, bloating, nausea, vomiting, diarrhea, constipation, hematemesis, abdominal or epigastric pain, hematochezia, change in bowel habits, food intolerance, flatulence, hemorrhoids. 7. Genitourinary- She denies dysuria, heavy bleeding and incontinence. Date of LMP was 1 week ago. Had first period at age 14, has had regular monlthy periods. Admits to sexual conduct with only one partner. 8. Musculoskeletal- Patient denies joint pain, swelling, muscle pain or cramps, neck pain or stiffness, changes in ROM. 9. Integumentary- states uses sunscreen when in the sun. Denies changes in skin, rash, itching, nail deformity, hair loss, moles, open areas, or bruising. Breast: denies lumps, pain, discharge, or dimpling during self breast exam. 10. Neurologic- Patient denies transient weakness, numbness, muscular weakness, tingling, memory difficulties, involuntary movements or tremors, syncope, stroke, seizures, paresthesias. 11. Psychiatric- Patient denies nightmares, mood changes, anxiety, depression, nervousness, insomnia, suicidal thoughts, exposure to violence, or excessive anger. 12. Endocrine- Patient denies thyroid problems, cold or heat intolerance, polydipsia, polyphagia, polyuria, changes in skin, hair or nail texture, unexplained change in weight, changes in facial or body hair, changes in hat or glove size, use of hormonal therapy. 13. Hematologic/lymphatic- Patient denies unusual bleeding or bruising, lymph node enlargement or tenderness, fatigue, history of anemia, blood transfusions. 14. Allergic/immunologic- Patient denies seasonal allergies, allergy testing, exposure to blood or body fluids, use of steroids, or immunosuppression in self or family. OBJECTIVE DATA (O): 1. Constitutional- VS: Temp- 98.8, BP- 110/67, HR- 68 Height- 5’7”, Weight- 178 lbs; General Appearance: healthy-appearing, well-nourished, and well-developed . Level of Distress: NAD. Ambulation: ambulating normally. 2. Eyes- sclerae white. Conjunctivae pink. Pupils are PERRL, 3 mm bilaterally. Extraocular movements intact. 3. Ear, Nose, Throat- Ears: external appearance normal-no lesions, redness, or swelling; on otoscopic exam tympanic membranes clear. Hearing is intact. Nose: appearance of nose normal with no mucous, inflammation or lesions present. Nares patent. Septum is midline. Mouth: pink, moist mucous membranes. No missing or decayed teeth. Throat: no inflammation or lesions present. Tonsils WNL- no erythema, ulcers, masses, exudate, inflammation. 4. Cardiovascular- S1, S2. Regular rate and rhythm, no murmurs, gallops, or rubs Carotid Arteries: normal pulses bilaterally, no bruits present Pedal Pulses: 2+ bilaterally Extremities: no cyanosis, clubbing, or edema, less than 2 second refill noted 5. Respiratory- Even and unlabored. Clear to auscultation bilaterally without wheezes, rales, or rhonchi. 6. Gastrointestinal- abdomen soft and nontender to palpation, nondistended. Negative Murphy’s sign. No rigidity or guarding, no masses present, BS present in all 4 quadrants 7. Genitourinary- No bladder tenderness upon palpation, no distention noted. External genitalia normal, no gross lesions or lacerations. Vagina shows healthy, pink mucosa, no gross lesions, white discharge noted. Cervix shows no lesions. Wet prep has normal results. 8. Musculoskeletal- Normal ROM, joint stability normal in all extremities, no tenderness to palpation. No scoliosis noted. 9. Integument/lymphatic- Inspection: No scaling, redness or breaks on neck, or arms, or trunk. Skin warm, dry and intact with good skin turgor. General palpation: no skin or subcutaneous tissue masses present, no tenderness, skin turgor normal Lower Extremities: no rash, lesion, or discoloration present Upper Extremities: no rash, lesion, or discoloration present 10. Neurologic- Grossly alert and oriented x3, communication ability within normal limits, attention and concentration normal. Sensation intact to light touch, gait within normal limits 11. Psychiatric- Judgment and insight intact, rate of thoughts normal and logical. Pleasant, calm, and cooperative. Patient appears to be happy/content. 12. Hematologic/immunologic- Lymph nodes not palpable, no tenderness or masses present, no bruising or bleeding noted. Diagnostic Testing: - Pap Smear: Pending - Wet Prep: Normal Assessment (A): 1. Pap Smear V72.31 Routine gynecological exam with pap Patient states that she needs her routine pap smear and after reviewing the patient’s records, it is noted that this is appropriate. Patient is sexually active and on oral contraceptives, therefore pap smears are recommended. 2. Family planning V25.09 Counseling and advice on contraceptive management Patient has requested a refill on her oral contraceptives and has discussed her usage of back up birth control when she occasionally misses a dose of medication. Plan (P): 1. Pap smear was performed with no difficulties. Sample was sent to LabCorp; results pending. Patient is aware that she will receive results in the mail at home. Patient will be contacted by the clinic if it is abnormal. 2. Tri Sprintec, 1 pill PO daily, disp #1, 11 refills; Encourage patient to continue to use a backup form of birth control is OCs are missed. Reiterate the importance of taking this medication as directed and maintaining only one sexual partner. Medication Profile: Tri Sprintec o Indication: Prevention of pregnancy. Treatment of moderate acne vulgaris in females ≥15 yrs of age who have no known contraindication to oral contraceptive therapy, desire oral contraceptive for birth control, and have achieved menarche. o MOA: Combination oral contraceptive; acts by suppressing gonadotropins, primarily inhibiting ovulation, and causing other alterations, including changes in the cervical mucus (increases difficulty of sperm entry into the uterus) and the endometrium (reduces likelihood of implantation). Acne: not established; increases sex hormone-binding globulin and decreases free testosterone. o Dosage: Three different doses in package that are taken in a specific order. Tri-Sprintec (norgestimate and ethinyl estradiol tablets) 0.18 mg/0.035 mg are gray, round, unscored tablets debossed with stylized b on one side and 985 on the other side; 0.215 mg/0.035 mg are light blue, round, unscored tablets debossed with stylized b on one side and 986 on the other side; 0.25 mg/0.035 mg are blue, round, unscored tablets debossed with stylized b on one side and 987 on the other side. o Brand, generic: Tri-Sprintec; norgestimate and ethinyl estradiol o Cost for 3 pharmacies: WalMart ($4); Target ($0); Coastal Pharmacy ($9) o Cost for 30 day supply: Free to $10 Outside testing: Pap Smear, pending Follow up: 1 year and PRN Referral: N/A Patient education: - Oral contraceptives can cause DVTs. Do not smoke while taking OCs, as it increases the risk of DVT. - Certain medications decrease the effectiveness of OCs. If you are placed on a new medication, ensure that interactions are checked. - If you miss a dose, take that dose as soon as possible. If two doses are missed, take two pills immediately, then continue taking one pill daily. If this occurs, use a form of back up birth control for up to 7 days. - The use of OCs do not prevent against the transmission of HIV, AIDS or other STDs - Begin self breast exams on a monthly basis, especially with 1st degree relative history of breast cancer.