Renal Physiology: Kidney Function, GFR, and Hormonal Control
advertisement

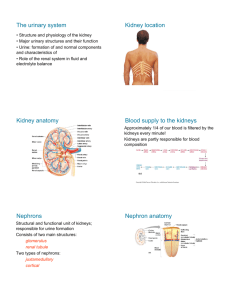
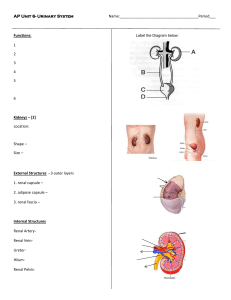
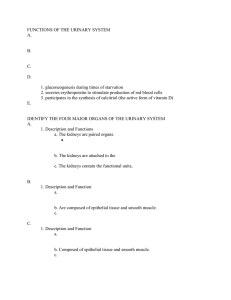
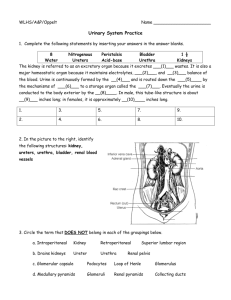
Renal Physiology By Dr. Sadat A. Aziz The Urinary system: The urinary system consists of • Two kidneys • Two ureters • The urinary bladder • Urethra. The formation of urine is the function of the kidneys, and the rest of the system is responsible for elimination of the urine. Main functions of the kidneys: 1.Excretion of metabolic wastes like creatinine and uric acid before being accumulated to toxic levels. 2. Regulation of the blood volume 3. Maintenance of water-salt balance 4. Maintenance of acid-base balance 5. Secretion of some biologically active molecules such as erythropoietin Renal vasculature: • The kidneys receive about 25% of the cardiac output. • Blood enters each kidney via the renal artery then it divides into 1. Afferent arterioles which deliver blood to the glomerular capillaries. 2. Efferent arterioles which drain blood from the glomerular capillaries. • deliver blood to the peritubular capillaries • then into small veins • finally into the renal vein. The nephrons: they are the functional units of the kidneys. Each kidney contains approximately 1 million nephrons. A nephron consists of: 1. Renal corpuscle: which is the site where the blood plasma is filtered, consisting of a glomerular capillary network which is surrounded by the bowman`s capsule. 2. Renal tubule which is made of a single epithelial layer that process the filtrate to urine via process of reabsorption and secretion. a. Proximal convoluted tubule b. The loop of Henle which is a U-shaped tube consisting of a thin descending limb, thin ascending limb and thick ascending limb c. The distal convoluted tubule d. Collecting ducts Nephrons functions: Nephrons have three main functions which include; glomerular filtration, tubular reabsorption and secretion. I. Glomerular filtration: • It is a process in which water and some solutes in the blood plasma pass from the capillaries of the glomerulus into the capsular space of the nephron Permeation of solutes through glomerular capillaries depend on: 1. the solute`s size: Molecules with a molecular weight less than 6 kDa can be filtered freely. However, molecules with a molecular weight more than 70 kDa are impermeable. 2. The solute`s charge: Negatively charged solutes are less likely to be filtered than neutral or positively charged molecules due to the negative charges of the filtration barriers. II. Tubular reabsorption: It is the process of reclaiming of water and solutes from the tubular fluid and returning them to the blood. There is a tight coupling between sodium (Na+) and water reabsorption which is called isosmotic reabsorption. III. Tubular Secretion It is a process in which the renal tubule extracts chemicals from the capillary blood and secretes them into the tubular fluid. it serves two purposes: 1. Waste removal 2. Acid-base balance Glomerular Filtration Rate (GFR): It is the amount of filtrate that can be formed per minute of time by the two kidneys. • Normally about 150-180 L/day which is about 50 to 60 times higher than the amount of blood plasma in the body. However, about 99% of the filtrate can be reabsorbed and only 1 to 2 L (per day) of filtrate is excreted as urine. Urine Volume: An average adult produces 1 to 2 L of urine per day. Diuresis or polyuria: An increase in the urine output to more than 2 L/day, is called diuresis or polyuria. Causes of polyuria: 1. An increase in the volume of fluid intake 2. Some drugs can increase urine output such as furosemide. 3. Chronic diseases such as diabetes. a. Diabetes mellitus b. Gestational diabetes c. Diabetes insipidus d. Renal diabetes Oliguria: it is a reduction in the urine output to less than 500 mL/day. Anuria: it is a clinical condition which is characterised by a reduction in the urine volume to less than 100 mL/day. • Low output can result from 1. Kidney disease 2. Dehydration 3. Circulatory shock 4. Prostate enlargement • If urine output drops to less than 400 mL/day, the body cannot maintain a safe, low concentration of wastes in the blood plasma which leads to development of a condition Known as azotaemia. Renin–Angiotensin System • In response to reduced blood volume and blood pressure, the juxtaglomerular cells secrete an enzyme which is called renin into the blood. • Renin stimulates conversion of angiotensinogen to angiotensin I, then angiotensin converting enzyme (ACE) converts angiotensin I to angiotensin II. • Angiotensin II affects renal physiology in three main ways: 1. It decreases the glomerular filtration rate by causing vasoconstriction of the afferent arterioles. 2. It enhances reabsorption of Na, Cl, and water in the proximal convoluted tubule. 3. It stimulates the adrenal cortex to release aldosterone. HORMONES THAT INFLUENCE REABSORPTION OF WATER 1. Aldosterone: • It is secreted by the adrenal cortex in response to a high blood potassium level, to a low blood sodium level, or to a decrease in blood pressure (hypotension). • When aldosterone stimulates the reabsorption of Na ions, water follows from the filtrate back to the blood. • This helps maintain normal blood volume and blood pressure. 2. Atrial natriuretic peptide: • It is released by the atria of the heart in response to high blood pressure (hypertension) • In turn it stimulates a reduction in the sodium ions reabsorption by the kidneys • which is followed by increasing the excretion of water and lowering the blood volume and blood pressure. 3. Antidiuretic hormone (ADH): • Antidiuretic hormone (ADH or vasopressin) is released by the posterior pituitary gland in response to reduced volume of water in the blood and hypotension. • It regulates facultative water reabsorption by the distal convoluted tubules and throughout the collecting ducts. • This helps maintain normal blood volume and blood pressure. • Hyposecretion of ADH leads to development of a condition which is known as Diabetes insipidus that characterised by a reduction in the water reabsorb and followed by an increase in the volume of urine.