MERSCOV
advertisement

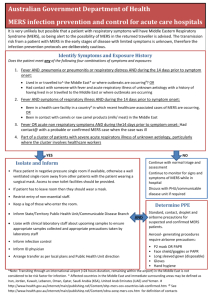
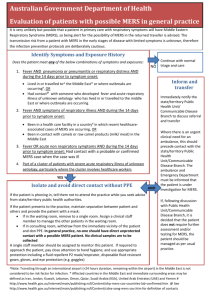
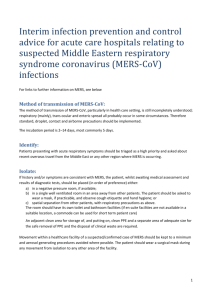
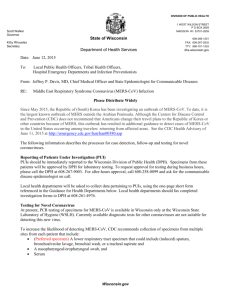
ADRIAN MARK NO known effective treatment or preventive vaccines ● From 2012- 2018, 37 patients reported direct or indirect contact with dromedaries in Saudi Arabia (33 cases), Oman (2 cases), the United Arab Emirates (one case) and Malaysia (one case; contact with dromedary was in Saudi Arabia). nd 2 Jan 2018 ● ● ● ● 55 year old male who resides in Malaysia, traveled as a member of a pilgrimage group to KSA from 13-23 December 2017. The case reported a history of exposure to dromedary camels (drinking unpasteurized camel milk and direct contact with a camel) while visiting a camel farm in Riyadh on 20 December 2017. The case developed symptoms on 24 December, was treated and hospitalized in Malaysia. 1st case in 2014. 2nd case in Jan 2018. Epidemiology ● Between 2012 and 30 June 2018, 2229 laboratory confirmed cases of Middle East respiratory syndromecoronavirus (MERS-CoV) infection were reported to WHO, ● 83% of whom were reported by the Kingdom of Saudi Arabia . ● ● ● ● In total, cases have been reported from 27 countries in the Middle East, North Africa, Europe, the United States of America, and Asia To date, 791 individuals have died (crude CFR 35.5%). 21% of the 2228 cases were reported to have no or mild symptoms, while 46% had severe disease or died. Overall, 18.6% of the cases reported to date are health care workers HUMAN TO HUMAN TRANSMISSION IN HEALTHCARE FACILITY IS COMMON! ● ● ● ● ● On 20th May 2015, the Republic of Korea notified WHO of the first laboratoryconfirmed case of MERS-CoV. • The index case had recently travelled to the Kingdom of Saudi Arabia (KSA), Qatar, the UAE and Bahrain. The source of his infection remains unknown. • The second case was his wife, the third was his hospital roommate, the fourth was the daughter of the roommate, the fifth was a healthcare professional who treated the first patient, and so on. According to the WHO, the rapid spread of the disease in South Korea was because of - among other things - a lack of awareness among the public and healthcare workers about MERS, crowded hospitals and emergency rooms, visitation by too many friends and family members and the practice of 'doctor shopping', or seeking care in multiple hospitals. • In this outbreak, transmission of MERS-CoV has been strongly associated with health care settings. 14% cases are health care professionals Clinical Features About 3 to 4 out of every 10 people reported with MERS have died. ● MERS can affect anyone. ● MERS patients have ranged in age from younger than 1 to 99 years old. ● The groups at highest risk for developing MERSCoV are: ● • Infants/Children ● • Elderly ● • People with immune system problems ● • Chronic Heart, Lung and Kidney problems ● • Pregnant women ● • People with Diabetes 3 CASE DEFINITIONS FOR PUI MERSCOV CASE DEFINITIONS (a) PUI (Patient Under Investigation ) MERS CoV 1)A person with an acute respiratory infection, which may include history of fever and cough ● ● 2) and indications of pulmonary parenchymal disease, based on clinical or radiological evidence of consolidation, 3)who requires admission ( mod to severe )to hospital 4) who within 14 days before onset of symptoms has history of residing in/travel to the Middle East/other affected countries with active transmission where human infections reported and in countries where MERS‐CoV is known to be circulating in dromedary camels” CASE DEFINITIONS (b) PUI (Patient Under Investigation ) MERS CoV Individuals with acute respiratory illness of any degree of severity who, within 14 days before onset of illness, had any of the following exposure: i.close physical contact with a confirmed/probable case of an ill MERS‐CoV patient ii.a healthcare facility in a country within 2 months of the last laboratory confirmed case of hospital‐associated MERS‐CoV infections have been reported; iii.direct contact with dromedary camels or consumption or exposure to dromedary camel products (raw meat, unpasteurized milk, urine) in countries where MERS‐CoV is known to be circulating in dromedary camel Close physical contact 1.Health care associated exposure -providing direct care for MERS‐CoV patients/visiting patients/staying in the same close environment 3.Working together in close proximity or sharing the same classroom environment 4.Traveling together in any kind of conveyance 5.Household contact CASE DEFINITIONS (c) PUI (Patient Under Investigation ) MERS CoV ● A person with an acute respiratory infection, which may include history of fever and cough and indications of pulmonary parenchymal disease, based on clinical or radiological evidence of consolidation, who requires admission to hospital AND Part of a cluster of patients with SARI of unknown aetiology in which MERS-COV is being evaluated , In consultation with state and local health departments in Malaysia” Probable Case 1)A person with a febrile acute respiratory illness with clinical, radiological, or histopathological evidence of pulmonary parenchymal disease (e.g.pneumonia or Acute Respiratory Distress Syndrome); AND 2)MERS-CoV test is unavailable/negative (on single inadequate specimen*) or inconclusive** AND i) ii) direct epidemiologic-link with confirmed case OR direct contact with dromedary camels or consumption or exposure to dromedary camel products (raw meat, unpasteurized milk, urine) in countries where MERS‐CoV is known to be circulating in dromedary camel OR iii) with hx of residing in/ travelling to countries with active transmission in last 14 days *Inadequate specimen = NP swab without LRT specimen/sample of poor quality/taken too late in course of illness **Inconclusive test = positive screening test without confirmation/positive serological assay Confirmed Case: ● A person with laboratory confirmation of infection with the MERS-CoV Step 1 ● ● Patient comes to ED with symptoms of respiratory infection ( fever, cough, runny nose, sorethroat, shortness of breath) IF NO = NOT PUI MERCOV Step 2 ● Any POSITIVE history of : 1) Travelling/residing middle east/countries with MERSCOV ● ● ● ● 2) Hx of visiting camel farm / direct contact with camel 3) Hx of drinking unpasteurised camel milk/ urine / raw meat 4) Hx of being in contact with a probable or confirmed case of MERS COV IF NO = NOT PUI MERSCOV Step 3 ● Is it within 14 days prior to onset of symptoms? ● If more than 14days ; MERSCOV Unlikely Step 4 ● ● Any evidence of lung parenchymal disease, either clinical ( pneumonia/ hypoxia/ tachypnoea/ ARDS) ) or chest xray finding of consolidation? IF NO ( lungs clear, xray normal, clinically comfortable on room air) = Not PUI MERCOV STEP 5 ● Assess Severity IF 1 YES IS CONSIDERED MODERATE TO SEVERE ILLNESS AND NEEDS ADMISSION IF ALL NO, MILD ILLNESS Clinical Assessment of Severity STEP 6 ● ● IF Severity Mild, Not considered PUI MERSCOV However if severity Mild, with contact with camels or confirmed cases of MERCOV, To admit ward as PUI MERCOV. Step 7 ● 1) Hx of Respiratory symptoms = Yes ● 2) Hx of travel to middle east/camel = Yes ● 3) Hx within 14 days prior to onset = Yes ● 4) Evidence of lung parenchymal disease = Yes ● 5) Severity Mod/Severe = PUI MERSCOV and Admit ● ● ● 6) Severity Mild ( NO contact with camels or confirmed cases) = Not PUI MERSCOV, discharge with advice 7) Severity Mild ( Contact with camels or confirmed cases) = Admit as PUI MERSCOV Step 8 ● Severity Mild ( NO contact with camels or confirmed cases) = Not PUI MERSCOV, discharge with home assessment tool ● No need to be notified ● No need throat swab ● Treast as outpatient assessment eg, URTI, or ILI with tamiflu ● TCA stat if worsening symptoms ● Provide clinic contact number for patients to contact if symptoms worsen Step 9 ( Mild Symptoms) ● Contact patient daily for 72 hours, to enquire health status and condition ● If well, can be discharged. ● If worsens, for patient to seek medical attention. Step 10: For PUI MERSCOV Immediate referral for admission Notify immediately if at OPD If at ED notify in ward Initial management PUI Mers CoV (OPD/ED) Initial management PUI Mers CoV (OPD/ED) Management of PUI Mers CoV in ward Respiratory Specimens Lower respiratory tract specimens has better yield 1. Sputum - Deep cough sputum 2. Broncheoalveolar lavage, tracheal aspirate, pleural fluid 3. If collection of lower tract specimens is not possible a combined nasopharyngeal and oropharyngeal swabs may be collected Also pls request for influenza PCR/IF /sputum culture & sensitivity Respiratory Specimens Positive result Lower respiratory tract specimens has better yield •Send second sample for 1. Sputum - Deep cough sputum 2. Broncheoalveolar lavage, tracheal aspirate, pleural fluid 3. If collection of lower tract specimens is not possible a combined nasopharyngeal and oropharyngeal swabs may be collected confirmation •Repeat test every 2-4 days until 2 consecutive negative test at least 24 hours apart Negative result • If highly suspicious, repeat sample every 4 days until negative till 14 days Also pls request for influenza PCR/IF /sputum culture & sensitivity MERS-CoV Infection: Management Of Close Contacts To A Probable / Confirmed Case Asymptomatic ● Hand-out / pamphlet about MERS-CoV ● ● ● Mild symptoms ● ● Home Assessment Tool 14 days surveillance (i.e. from the date of last exposure ● ● no restriction of movement ● HOME SURVEILLANCE RESTRICTION on his / her daily movement. hand-out / pamphlet about MERS-CoV infection modified Home Assessment Tool -To conduct 14 days surveillance (i.e. from the date of last exposure To send the diagnostic specimen INFECTION CONTROL ● ● ● 1) MERS: SCREENING AND TRIAGING • A special area should be set up for PUI of MERS, to which he / she can come directly. The PUI should be managed by a dedicated team where possible. ● Clinical triage - rapid case identification of patients at risk ● • Spatial separation of at least 1m between patients in the waiting rooms ● • Provide resources for performing hand hygiene (alcohol hand rub bottles made available) ● • Offer surgical mask (not N95 mask) if patient able to tolerate (not tachypneic, not hypoxic) ● • Adequate environmental ventilation and environmental cleaning at waiting and triage areas 2) Designated Pathway ● ● From ED Decontamination room, need to have assigned pathway ( designated lift) for direct admission to negative pressure room Need to establish designated portable xray machine ● ● Personal Protective Equipment (PPE) (Standard And Droplets Precaution) In addition to Standard Precautions, all individuals (visitors and healthcare workers), when in close contact (within 1 metre) or upon entering the room or cubicle of patients, should always wear: ● A 3 ply surgical mask ● Eye protection (i.e. goggles or a face shield) ● A clean, non-sterile, long-sleeved gown ● Nonsterile Gloves ● ● Use dedicated equipment (e.g. stethoscopes, blood pressure cuffs and thermometers) PPE When Performing Aerosol-Generating Procedures (Standard And Airborne Precautions) – Wear N95 ● ● ● • An aerosol-generating procedure (AGP) is defined as any medical procedure that can induce the production of aerosols of various sizes, including small (< 5 μm) particles. The aerosol-generating procedures include: ● Intubation - the strongest evidence for needing airborne precaution ● Manual ventilation ● Non-invasive ventilation (e.g., BiPAP, BPAP) – avoid if possible ● Tracheostomy insertion ● Bronchoscopy ● Sputum induction ● Nebulization (some recent guidelines disqualified this as AGP) ● • Airborne precaution also recommended when taking oropharyngeal/ nasopharyngeal swab 3) Isolation Rooms In descending order of preference: i. Negative pressure single room en-suite bath (if available within the health care facility) ii. Single room (nursed with door closed) and en-suite bath iii. Single room ( IF No negative pressure room in ICU for intubated cases, need to be ventilated in ward with designated nurse) VISITOR POLICY ● ● ● • Limit the number of family members and visitors in contact with a probable or confirmed case MERS infection. • Family members and visitors who may come into contact with a patient should be limited to those essential for patient support and should be trained on the risk of transmission and on the use of the same infection control precautions as HCWs who are providing routine care. THANK YOU