Appendicitis
advertisement

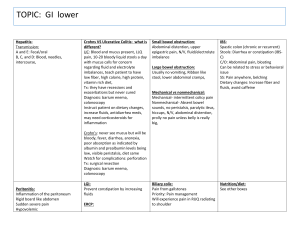
Appendicitis Definition: Is an acute inflammation of the appendix Causes: The lumen of the appendix is quite small, making it liable to incomplete emptying or obstruction which can lead to infection. Kinking of the appendix or obstruction by fecaliths (hardened feces) or foreign bodies also may trigger the acute inflammatory response. Incidence: Occurs most commonly in teen-agers and young adults between the ages of 10 and 30 years. Male are affected more commonly than females. Signs and symptoms: Typically begins with acute abdominal pain that come in waves. The pain typically starts in the epigastric or umbilical region. But gradually become localized in the right lower quadrant of the abdomen. Localization of McBurney's point (halfway between the umbilicus and the anterior spine of the ileum). The pain is intermittent at first but typically becomes steady and severs over a short period. Nausea, anorexia, and vomiting. Rebound tenderness. The person with appendicitis is noted to be lying side or back with knee flexed in an attempt to decrease muscle strain on the abdominal wall. Elevation of temperature in the range of 38o to 40oC, accompanied by an elevation in WBCs count. Diagnosis: A diagnosis of appendicitis is based on classic signs and symptoms and white blood cell count of 10.000 to 15.000/mm3. Medical treatment: When appendicitis is suspected, the patient is allowed: Nothing by mouth. Administer IV fluids as ordered If tolerated advise the patient to maintain semifowler’s position. A cold pack to the abdomen may be ordered. Laxatives, enemas and heat applications should never be given for patient with suspected or known appendicitis. If the appendix is inflamed, heat or laxative may cause it to rupture. Once the diagnosis of appendicitis is confirmed and surgery is scheduled, administer opioid analgesics and antibiotic . Surgical management If rupture has not occurred, immediate surgical treatment is indicated. With a ruptured appendix, surgery may be delayed 6 to 8 hours while antibiotics and intravenous fluids are given. Nursing management 1. Assessment (before urgery): The patient's chief complaint is usually pain. Assess the location, severity, onset, duration, precipitating factors, and alleviating measures in relation to the pain. In the past medical history, note previous abdominal distress, chronic illnesses, and surgeries. Record allergies and medications as well. Record the presence of nausea and vomiting. Significant data in the physical examination are temperature; abdominal pain, distention, and tenderness; and the presence and characteristics of bowel sounds. Postoperative care: Postoperatively, the patient receives antibiotics, intravenous fluids and possible gastrointestinal decompression. Assist the patient in turning, coughing, and deep breathing to promote expansion of the lung. Incentive spirometery also can be useful. Show the patient how to splint the incision during deep breathing. Early ambulation is usually ordered to reduce the risk of postoperative complications. Assess the abdominal wound for redness, swelling and drainage. Provide wound care as ordered or according to agency policy. If there no complication, the patient is usually discharged in a few days. Normal activities can be resumed in 2-3 weeks.