460
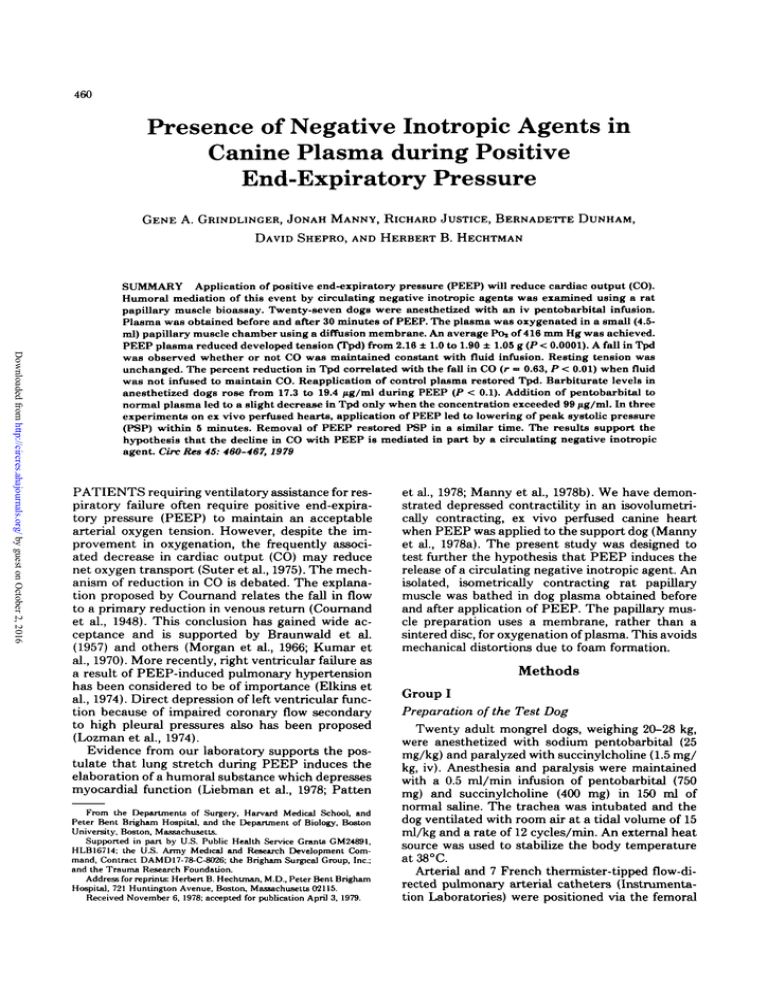
Presence of Negative Inotropic Agents in
Canine Plasma during Positive
End-Expiratory Pressure
GENE A. GRINDLINGER, JONAH MANNY, RICHARD JUSTICE, BERNADETTE DUNHAM,
DAVID SHEPRO, AND HERBERT B. HECHTMAN
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
SUMMARY Application of positive end-expiratory pressure (PEEP) will reduce cardiac output (CO).
Humoral mediation of this event by circulating negative inotropic agents was examined using a rat
papillary muscle bioassay. Twenty-seven dogs were anesthetized with an iv pentobarbital infusion.
Plasma was obtained before and after 30 minutes of PEEP. The plasma was oxygenated in a small (4.5ml) papillary muscle chamber using a diffusion membrane. An average POi of 416 mm Hg was achieved.
PEEP plasma reduced developed tension (Tpd) from 2.18 ± 1.0 to 1.90 ± 1.05 g (P < 0.0001). A fall in Tpd
was observed whether or not CO was maintained constant with fluid infusion. Resting tension was
unchanged. The percent reduction in Tpd correlated with the fall in CO (r •= 0.63, P < 0.01) when fluid
was not infused to maintain CO. Reapplication of control plasma restored Tpd. Barbiturate levels in
anesthetized dogs rose from 17.3 to 19.4 /ig/ml during PEEP (P < 0.1). Addition of pentobarbital to
normal plasma led to a slight decrease in Tpd only when the concentration exceeded 99 /ig/ml. In three
experiments on ex vivo perfused hearts, application of PEEP led to lowering of peak systolic pressure
(PSP) within 5 minutes. Removal of PEEP restored PSP in a similar time. The results support the
hypothesis that the decline in CO with PEEP is mediated in part by a circulating negative inotropic
agent. Ore Res 45: 460-467, 1979
PATIENTS requiring ventilatory assistance for respiratory failure often require positive end-expiratory pressure (PEEP) to maintain an acceptable
arterial oxygen tension. However, despite the improvement in oxygenation, the frequently associated decrease in cardiac output (CO) may reduce
net oxygen transport (Suter et al., 1975). The mechanism of reduction in CO is debated. The explanation proposed by Cournand relates the fall in flow
to a primary reduction in venous return (Cournand
et al., 1948). This conclusion has gained wide acceptance and is supported by Braunwald et al.
(1957) and others (Morgan et al., 1966; Kumar et
al., 1970). More recently, right ventricular failure as
a result of PEEP-induced pulmonary hypertension
has been considered to be of importance (Elkins et
al., 1974). Direct depression of left ventricular function because of impaired coronary flow secondary
to high pleural pressures also has been proposed
(Lozman et al., 1974).
Evidence from our laboratory supports the postulate that lung stretch during PEEP induces the
elaboration of a humoral substance which depresses
myocardial function (Liebman et al., 1978; Patten
From the Departments of Surgery, Harvard Medical School, and
Peter Bent Brigham Hospital, and the Department of Biology, Boston
University, Boston, Massachusetts.
Supported in part by U.S. Public Health Service Grants GM24891,
HLB16714; the U.S. Army Medical and Research Development Command, Contract DAMD17-78-C-8026; the Brigham Surgical Group, Inc.;
and the Trauma Research Foundation.
Address for reprints: Herbert B. Hechtman, M.D., Peter Bent Brigham
Hospital, 721 Huntington Avenue, Boston, Massachusetts 02115.
Received November 6, 1978; accepted for publication April 3, 1979.
et al., 1978; Manny et al., 1978b). We have demonstrated depressed contractility in an isovolumetrically contracting, ex vivo perfused canine heart
when PEEP was applied to the support dog (Manny
et al., 1978a). The present study was designed to
test further the hypothesis that PEEP induces the
release of a circulating negative inotropic agent. An
isolated, isometrically contracting rat papillary
muscle was bathed in dog plasma obtained before
and after application of PEEP. The papillary muscle preparation uses a membrane, rather than a
sintered disc, for oxygenation of plasma. This avoids
mechanical distortions due to foam formation.
Methods
Group I
Preparation of the Test Dog
Twenty adult mongrel dogs, weighing 20-28 kg,
were anesthetized with sodium pentobarbital (25
mg/kg) and paralyzed with succinylcholine (1.5 mg/
kg, iv). Anesthesia and paralysis were maintained
with a 0.5 ml/min infusion of pentobarbital (750
mg) and succinylcholine (400 mg) in 150 ml of
normal saline. The trachea was intubated and the
dog ventilated with room air at a tidal volume of 15
ml/kg and a rate of 12 cycles/min. An external heat
source was used to stabilize the body temperature
at38°C.
Arterial and 7 French thermister-tipped flow-directed pulmonary arterial catheters (Instrumentation Laboratories) were positioned via the femoral
NEGATIVE INOTROPISM AND PEEP/Grindlinger et al.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
vessels. Mean systemic and pulmonary arterial,
mean pulmonary arterial wedge, and mean central
venous pressures were measured with strain gauge
transducers (Bentley, model 800). The pulse was
monitored using the arterial wave form (HewlettPackard, model 78203C), and CO was determined
in triplicate by the thermodilution technique (Instrumentation Laboratory, model 601). Arterial
blood gases and pH were measured with standard
Clark and Severinghaus electrodes (Instrumentation Laboratory, model 813), and hemoglobin and
percent saturation were measured spectrophotometrically (Instrumentation Laboratory, model
282), using extinction coefficients specific for dog
blood. Base excess was derived from the SiggaardAnderson Nomogram (Siggaard-Anderson, 1963).
After 30 minutes of ventilation at 0 cm H2O endexpiratory pressure (O-EEP) or at 15 cm H2O
PEEP, hemodynamics, blood gases, and pH were
measured. Twenty milliliters of arterial blood were
drawn into a heparinized plastic syringe. The blood
was centrifuged at 2500 rpm and 25 °C for 20 minutes (Sorvall, model GLC) and the plasma separated. The papillary muscle assay was started immediately.
Papillary Muscle Assay
The posterior left ventricular papillary muscle
from Sprague Dawley rats, weighing an average of
225 g, was used. The heart was removed after
decapitation and the papillary muscle rapidly excised and immersed in a solution that had been
equilibrated with 95% O2 and 5% CO2. The composition of this solution (meq/liter) was: Na + , 146; K+
3.6; Ca2+, 4.5; Mg2*, 2.5; PO/", 1.4; SO,2", 2.5; Cl",
130; and HC0 3 , 25. Glucose concentration was 10.2
mM/liter. The final pH was adjusted to 7.40 by
adding small quantities of sodium bicarbonate.
The papillary muscle length averaged 8.31 ± 2.13
mm (mean ± SD) with a range of 5.42-9.72 mm. The
calculated mean cross-sectional area was 1.37 ± 0.43
mm2. The muscle was suspended vertically in a 4.5ml Plexiglas chamber using stainless steel spring
clamps. The tendonous end was attached to the
rigid arm of an isometric force transducer (Harvard
Apparatus, model 363). The mural end was attached
to the movable arm of a dial micrometer (Micrometric Instrument Co.). The chamber was mounted
on a Delrin block which housed a rotating magnet
and variable speed motor (Instech Laboratories,
models 450/055 and 1055). A 1.25-cm diameter well
in the base of the chamber contained a magnetic
stirring bar which was used to ensure adequate
mixing of the chamber fluid. A port at the bottom
of the well allowed rapid filling and emptying of the
chamber (Fig. 1).
Continual oxygenation of the electrolyte solution
or test plasma was accomplished by diffusion. A
Silastic membrane, 0.178 mm thick (Dow Corning),
was glued with Silicone adhesive sealant (Dow
Corning) onto the grooved inner face of two oppos-
461
FIGURE 1 A schematic diagram of the papillary muscle
system is shown. The stippled rectangle is the force
transducer. A rigid hook used to mount the tendonous
end of the papillary muscle projects from the transducer.
The lower movable arm used to fix the mural end of the
muscle is connected to a dial micrometer, a = Silastic
membrane, b = electrode, c = gas inflow port, d = gas
outflow port, e = stirring bar, f= drain port, g = rotating
magnet.
ing chamber walls. The total surface area available
for diffusion was 500 mm2. Inlet and outlet ports in
both walls allowed continuous flow of 95% and 5%
CO2.
Stainless steel field-stimulating electrodes of
17.3-mm2 cross-sectional area were mounted parallel to the longitudinal axis of the muscle. A 4.5-msec
rectangular pulse (Grass Instrument Co., model
S44), set just at suprathreshold voltage, was delivered once every 5 seconds. The stimulus voltage
was increased periodically 5-fold to ensure that
developed tension was not limited by excitation
characteristics. The amplified signal of the force
transducer was continuously displayed on an oscilloscope (Hewlett-Packard, model 78304A). Recordings were made every 15 minutes using a light beam
recorder with a frequency response flat to 500 Hz
(Hewlett-Packard, model 4888A), and the following
variables were measured: peak developed tension,
Tpd; resting tension, Tr; time-to-peak tension,
TPT; and relaxation time (i.e., time for tension to
fall one-half of developed tension), RT )/2 . All experiments were conducted at 26.2 ± 0.52°C.
After a 60-minute period of equilibration, lengthtension curves were constructed by progressively
increasing length of the isometrically contracting
muscle. The length was then set so that Tpd was at
the apex of the curve. Only those preparations
462
CIRCULATION RESEARCH
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
which remained stable during the equilibration period were used (20 of 23). Test plasma was preoxygenated in a second chamber. The electrolyte solution was drained rapidly and the test plasma
added to the muscle chamber between contractions.
Plasma was tested in the following sequence: 0EEP, PEEP, 0-EEP. The two O-EEP samples were
drawn at the same time. Each plasma sample was
allowed to bathe the muscle for 1 hour. Small
aliquots were removed at 30-minute intervals to
measure P02, PCO2, and pH.
Barbiturate concentrations in 0-EEP and PEEP
plasma were determined in seven experiments by
UV absorption (Goldbaum, 1948). Experiments
then were conducted to assess the influence of
barbiturates on contractility. Plasma was obtained
from nonanesthetized dogs and was used to bathe
a series of four papillary muscles. Pentobarbital
sodium (Nembutal, Abbott Laboratories) was
added to the test chamber in increments to achieve
a concentration range of 9-200 /ng/ml. The papillary
muscle was equilibrated with each barbiturate concentration for 30 minutes. Records were obtained
at 15-minute intervals. After exposure to the highest
concentration, the chamber was emptied rapidly
and refilled with oxygenated plasma without barbiturate.
Group II
Preparation of the Test Dog and Papillary
Muscle Assay
Another group of experiments was conducted
first, to test the effect of PEEP when CO was held
constant and second, to test the effect of the removal of PEEP on the negative inotropism.
Seven adult mongrel dogs and the corresponding
papillary muscles were prepared in a manner similar
to that of group I. During ventilation at 15 cm H2O
PEEP, balanced salt solution was infused to maintain the CO at O-EEPi levels. After removal of
PEEP, the dog again was ventilated at 0 cm H2O
end-expiratory pressure, (O-EEP2). After 30 minutes of ventilation at O-EEPi, PEEP, or O-EEP2
hemodynamics, blood gases and pH were measured,
and plasma was obtained from 20 ml of arterial
blood. Plasma was tested in the following sequence:
O-EEP,, PEEP, O-EEP2, O-EEP,. The two O-EEP,
samples were obtained at the same time. Each
plasma sample was allowed to bathe the muscle for
1 hour. Small aliquots were removed at 30-minute
intervals to measure P02, PCO2, and pH.
Three improvements were made in the design of
the papillary muscle bioassay apparatus used in
group II experiments. First, the chamber was modified to provide a greater surface area per volume of
plasma for gas exchange. Second, the stainless steel
electrodes were redesigned. Each electrode was
pressed onto the tinned terminal of an insulated
nylon-tip jack, fitted with an outer threaded metal
shell (H.H. Smith Co., model 1501). Two opposing
VOL. 45, No. 4, OCTOBER 1979
chamber walls were drilled and tapped to accommodate the electrodes. This allowed precise positioning of the electrodes in the horizontal plane
relative to the muscle. Finally, the isometric force
transducer was mounted on a screw jack (Ealing,
model 22-9435) which allowed longitudinal positioning of the muscle relative to the electrodes.
Ex Vivo Perfused Hearts
Three isolated hearts undergoing coronary perfusion from a support dog at a fixed rate of 1.4 ml/
min-g heart were studied to examine the rate of
appearance and disappearance of the negative inotropic effect. The details of this temperature-controlled, paced, isovolumetrically contracting preparation have been reported previously (Manny et al.,
1978a). In the current experiments, the left ventricular balloon was filled with 30 ml saline, which
corresponded to a diastolic pressure of 6.6 mm Hg
(strain gauge transducer, Bentley, model 800). Perfusion pressure measured at the aortic arch of the
isolated heart was 92 mm Hg. The changes in left
ventricular peak systolic pressure in the isolated
heart and mean arterial pressure in the support dog
were recorded after 15 cm H2O PEEP was applied
or removed from the support dog.
The transit delay for the passage of substances
from the lungs of the support dog to the aortic arch
of the isolated heart was determined by injecting
indocyanine green dye into the pulmonary artery of
the support dog. At the same time, blood sampling
was started from the aortic arch of the isolated
heart. Blood was withdrawn at a constant rate of
20 ml/min through a cuvette densitometer (Gilson,
model DTL). The mean transit time, derived from
the concentration-time curve of the dye, varied
from 28 to 39 seconds.
Data are presented as the mean ± SD. Probability
is based on Student's paired t-test.
Results
Group I
The application of 15 cm H2O PEEP resulted in
hemodynamic changes similar to those reported in
the past (Table 1) (Liebman et al., 1978; Patten et
al., 1978; Manny et al., 1978a, 1978b). CO and mean
arterial pressure decreased (P < 0.001), whereas
central venous and pulmonary arterial wedge pressure increased (P < 0.01, P < 0.001). Pulse rate fell
from 174 ± 14 to 159 ± 15 (P < 0.01). Blood gases
were unchanged, but pH decreased by 0.07 units (P
< 0.05), and the base excess fell from —5 to —9 meq/
liter (P < 0.005) (Table 1).
Papillary Muscle
After addition of PEEP plasma to the papillary
muscle, Tpd decreased in 18 of 20 experiments
(Table 2). After 1 hour, Tpd had declined from an
average of 1.73 ± 0.75 to 1.47 ± 0.79 g (P < 0.0001)
NEGATIVE INOTROPISM AND PEF.P/Grindlinger et al.
463
TABLE 1 Hemodynamic, Blood Gas, and Acid-Base Response to
15 cm H2O PEEP
Responses in group I
0-EEP
3.47 ± 0.72
144 ± 17
5±3
CO (liter/min)
MAP (mm Hg)
PAWP (mm Hg)
CVP (mm Hg)
P (mirT1)
Po, (mm Hg)
Pcoj (mm Hg)
pH
BE (meq/liter)
:
4 ±2
174 ± 14
85 ± 10
33.7 ±4.1
7.34 ± 0.05
PEEP
P
1.87 ± 0.82
124 ± 18
< 0.001
< 0.001
< 0.001
< 0.001
<0.01
NS
NS
<0.05
< 0.005
11±3
11 ± 3
159 ± 15
93 ± 14
35.8 ± 9.7
7.27 ± 0.07
-9 ± 3
-5 ±3
Results are expressed as mean ± ED.
MAP — mean arterial pressure; PAWP — pulmonary arterial wedge pressure; CVP — central venous pressure; P
pulse; BE — base excess; and NS — not significant.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
in 19 of the 20 experiments in which CO also declined. In the one dog in which CO rose during
PEEP, there was an increase in Tpd. This experiment was excluded from the statistical analysis of
the change in Tpd, since the PEEP plasma would
not have been expected to exert a negative inotropic
effect. Reapplication of O-EEP plasma led to a slow
restoration in Tpd. Only after 1 hour did the Tpd
exceed the level attained during exposure to PEEP
plasma (P < 0.001).
Barbiturate
In six of seven experiments, PEEP plasma contained higher concentrations of pentobarbital than
O-EEP (Table 3). The average increase was 2.1 /ig/
ml (P < 0.1). The addition of pentobarbital to
normal plasma yielded a slight decrease in Tpd at
99 jug/ml (Fig. 2). This concentration was over three
times the highest concentration measured during
PEEP. Even at 200 jug/ml, only 9% depression in
TABLE 2 Changes in Developed Tension (g) during Exposure to
OEEP, PEEP,
and 0-EEP Plasma
Changes in group I at
0-EEP
PEEP
0-EEP
15 min
30 min
45 min
60 mm
1.66 ± 0.75
1.34 ± 0.56
1.31 ± 0.66
1.66 ± 0.66
1.40 ± 0.71
1.48 ± 0.75
1.65 ± 0.67
1.46 ± 0.76
1.60 ± 0.76
1.73 ± 0.75
1.47 ± 0.79
1.66 ± 0.75
Results are expressed as mean ± SD.
Following application of PEEP plasma, RTi /2 fell
from 0.18 ± 0.03 to 0.15 ± 0.03 seconds (P < 0.001).
Reintroduction of O-EEP plasma did not restore
this value to baseline. PEEP plasma did not alter
Tr or TPT.
The diffusion membrane in the muscle chamber
provided good exchange of gases. The average P02
was 391 ± 78 mm Hg; Pco^, 34 ± 7 mm Hg; and pH,
7.41 ± 0.07. There were no differences between 0EEP and PEEP plasmas.
TABLE 3 Plasma Levels of Pentobarbital before
(OEEP) and during 15 cm H2O PEEP
Experiment no.
4
5
6
8
10
11
12
Mean
SD
0-EEP Oig/ml)
PEEP (MK/ml)
14.5
26.5
21.5
14.3
17.0
18.0
12.0
30.0
24.2
15.4
14.5
18.7
21.0
17.3
19.4
9.5
5.5
6.2
P<0.1
Tpd was observed, compared with a 14% depression
with PEEP plasma.
Group II
Maintenance of Constant Flow
Infusion of balanced salt solution during PEEP
resulted in maintenance of CO at levels equivalent
to O-EEP, (Table 4). Mean arterial pressure decreased slightly (P < 0.01), whereas central venous
and pulmonary arterial wedge pressures increased
(P < 0.001, P < 0.001). Pulse rate fell, but not
significantly, from 145 ± 15 to 135 ± 9. Blood gases
were unchanged, but pH decreased by 0.08 unit (P
< 0.005), and the base excess fell from —1 to —4
meq/liter (P < 0.001). Thirty minutes after removal
of PEEP (O-EEP2), hemodynamics returned to 0EEPi levels. Blood gases were unchanged, but pH
rose by 0.03 unit and the base excess rose from —4
to-3.
Papillary Muscle
After addition of PEEP plasma to the papillary
muscle, Tpd decreased in seven of seven experiments. After 1 hour, Tpd had declined from an
CIRCULATION RESEARCH
464
VOL. 45, No. 4, OCTOBER
1979
fication in the chamber dimensions provides a
greater surface area per volume of plasma for gas
exchange. This results in a higher average Po 2 of
519 ± 41 mm Hg compared with group I. Pco 2 and
pH were comparable to group I (35.4 ± 4.3, 7.39 ±
0.08).
to
100
Ex Vivo Heart
Within 15-20 seconds after application of PEEP
to the support dog, there was a 10- to 20-mm Hg
fall in mean arterial blood pressure. Soon after, a
transient increase in peak systolic pressure (PSP)
in the isolated heart was observed. This was followed by a decline in PSP, which reached a minimum in 3-5 minutes (Fig. 3). After removal of
PEEP, recovery of PSP took 5-10 minutes.
200
PENTOBARBITAL, pg/ml
2 Addition ofpentobarbital to normal plasma
led to a slight decrease in Tpd at concentrations above
99 \ig/ml. After testing with the highest barbiturate
concentrations, reapplication of normal plasma restored
Tpd. The data represent the means of data from four
papillary muscle experiments.
FIGURE
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
Discussion
The reduction in CO that attends the use of
PEEP usually is attributed to mechanical events.
The most prominent of these events is an increase
in pleural pressure, which is thought to impede
venous return (Suter et al., 1975). Such mechanisms
are likely to be operative under many circumstances
but need not always be invoked to explain flow
reductions with PEEP. Thus, the application of 15
cm H2O PEEP to a series of animals whose chest
average of 3.04 ± 0.60 to 2.86 ± 0.70 g (P < 0.05)
(Table 5). Application of O-EEP2 plasma restored
Tpd after 60 minutes to 3.11 g (P < 0.001). Reapplication of O-EEPi plasma maintained Tpd at a
level equivalent to O-EEP2 and significantly higher
than PEEP (P < 0.005).
Following addition of PEEP plasma, RT, /2 fell
TABLE
4 Hemodynamic, Blood Gas, and Acid-Base Response to 15 cm H2O PEEP
Responses in group II
0-EEP,
CO (liter/min)
MAP (mm Hg)
PAWP (mm Hg)
CVP (mm Hg)
P (miir1)
POj ( m m Hg)
PCO2 (mm Hg)
pH
BE (meq/liter)
3.65 ± 0.77
144 ± 7
7 ± 2.4
5 ± 3.5
145 ± 15
107 ± 16
32.8 ± 3.5
7.41 ± 0.04
-1 ± 3
P
PEEP
P
0-EEP,
NS
3.74 ± 1.01
137 ± 7
14 ± 2.7
13 ± 4.8
135 ± 9
105 ± 11
40.0 ± 7.7
7.33 ± 0.03
-4± 3
NS
NS
<0.01
< 0.005
NS
NS
NS
NS
NS
3.99 ± 0.76
138 ± 10
9 ±2.7
8 ±3.8
135 ± 7
102 ± 13
35.4 ± 6.0
7.36 ± 0.03
-3 ±2
<0.01
< 0.001
< 0.001
NS
NS
NS
< 0.005
< 0.001
P is probability of a difference between adjacent columns NS — not significant.
slightly from 0.18 ± 0.05 to 0.16 ± 0.03 seconds (P
< 0.05). Neither O-EEP2 plasma nor reintroduction
of O-EEPi plasma could restore this value to baseline. PEEP plasma did not alter Tr or TPT.
Modification in electrode design, positioning, and
additional experience with the preparation enabled
us to achieve consistently higher values for Tpd in
the experiments of group II than in group I. Modi-
walls had been excised and in which pleural pressure remained constant led to dramatic falls in CO
(Liebman et al., 1978). Further, the flow reduction
was greater than in closed-chested animals treated
with PEEP (Manny et al., 1978b). This was not due
to right ventricular failure, since elevation of the
pulmonary artery pressure during O-EEP in these
open-chested dogs to levels equivalent to PEEP did
TABLE 5 Changes in Developed Tension (g) during Exposure to 0-EEP\,
PEEP, and 0EEP2 Plasma
Change B in group II at
15 mm
0-EEP,
PEEP
O-EEP2
0-EEP,
2.96 ±
2.96 ±
2.98 ±
3.07 ±
0.74
0.74
0.91
0.94
30 min
45 min
60 min
3.00 ± 0.81
2.93 ± 0.72
3.01 ± 0.87
3.09 ± 0.93
3.04 ± 0.66
2.90 ± 0.72
3.09 ± 1.03
3.10 ±0.79
3.04 ± 0.66
2.86 ± 0.76
3.11 ±0.95
3.10 ± 0.81
NEGATIVE INOTROPISM AND
PEEP-O-EEP
TIME (minutes)
FIGURE 3 The typical course of change in PSP in the
isolated heart (balloon volume of 30 ml) is illustrated in
one preparation when PEEP was applied (O-EEP —>
PEEP) and in another when PEEP was removed (PEEP
—> O-EEP). The mean transit delay due to the coronary
perfusion circuit ranged between 28 and 39 seconds.
These values were not subtracted from the abcissa.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
not lead to a fall in CO (Liebman et al., 1978).
Reduction in left ventricular contractility during
PEEP was suggested by a rising left ventricular
filling pressure despite a falling CO (Liebman et al.,
1978; Manny et al., 1978b). Strong support for humoral mediation of this event was provided by a
series of cross-circulation experiments in which application of PEEP to one animal led to decreasing
CO in both (Patten et al., 1978). This humoral
hypothesis was strengthened by a series of studies
on ex vivo perfused isolated hearts (Manny et al.,
1978a). When PEEP was applied to the support dog
that provided coronary flow to the heart, there was
a decrease in contractility. This fall in contractility
still was observed after infusions were given to the
support dog to prevent the PEEP-induced reduction in CO. The event that appeared to stimulate
release of a negative inotropic agent or cause a
reduction in levels of a positive inotropic agent was
lung stretch, since when PEEP was applied, but the
functional residual capacity was kept constant, the
isolated heart was not depressed. Since the lungs
are active metabolic organs, capable of elaborating
and metabolizing a variety of vasoactive substances
(Said et al. 1975; Heineman et al., 1977), it is reasonable to postulate that lung stretch can alter
pulmonary metabolic activity such that there is a
resultant depression in cardiac contractility. It also
could be argued that lung stretch acts via a neural
arc (possibly vagal) causing release of substances at
a site distant from the lung.
This study demonstrates that plasma from a
PEEP-treated dog will exert a negative inotropic
effect on rat papillary muscle. The decrease in
contractility is based on a reduction of Tpd at
constant preloads. This negative inotropic effect
was reversed following replacement of PEEP
plasma with O-EEP i or O-EEP2 plasma.
Papillary Muscle Characteristics
The newly developed papillary muscle bioassay
system is ideally suited for testing small volumes of
PEEP/Grindlingeretal.
465
plasma. Substitution of a membrane oxygenator for
the usual sintered disc system or bubble oxygenator
eliminates mechanical distortions induced by
plasma foam. Our most recent experience has indicated that a plasma P02 above 500 mm Hg may be
obtained routinely after 10-15 minutes of equilibration.
The findings of a reduced Tpd with PEEP plasma
is consistent with a negative inotropic effect but
also may be related to an alteration in excitation,
excitation-contraction coupling, contraction, and
relaxation processes. We found no evidence that
the threshold for excitation was influenced by
PEEP plasma. Increasing the stimulation voltage
5-fold did not reverse the depression in Tpd. Since
stimulating frequency was far below the physiological rate, it is unlikely that the refractory period
played a role. These considerations make it probable that Tpd was independent of the characteristics
of stimulation.
The observed fall in Tpd was not related to
variations in parallel elastic compliance since Tr
was unchanged. Further, these experiments were
conducted near the apex of the length-tension
curve, where small changes in Tr would not be
expected to influence Tpd significantly (Sonnenblick and Skelton, 1971). It is possible that an
increase in series compliance could account for the
fall in Tpd (Hill, 1951). However, this event should
also delay the occurrence of peak tension (Sonnenblick, 1964). Our observation was that TPT was
either unchanged or reduced.
Changes in the active state may be related to
temperature (Edman et al., 1974), oxygenation (Tyberg et al., 1970), or acid-base (Johannsson and
Nilsson, 1975) characteristics of the bathing medium. These were held constant and are therefore
not likely to be related to the fall in Tpd. It is
possible that lactate levels rose in the support dog
secondary to a PEEP-induced fall in the CO of
group I or redistribution of flow in group II (Manny
et al., 1979). We did not measure lactate but did
observe a significant decrease in base excess. Lactate ion will reduce contractility (Gimeno et al.,
1966) but only in the presence of acidosis. In the
absence of acidosis, lactate will increase Tpd by
prolonging the duration of the active state, despite
a small reduction in contractility parameters (Pannier and Weyne, 1970). We observed a slight and
nonsignificant reduction in TPT, which is inconsistent with a lactate effect. Furthermore, in group
II dogs in which CO was maintained constant during PEEP, Tpd fell despite only modest decreases
in base excess.
Finally, a barbiturate infusion was used for anesthesia. The metabolism of this known myocardial
depressant could have been decreased during the
low flow state that accompanies PEEP. The measured barbiturate levels did indeed rise, although
only slightly. The highest levels found were below
those reported to decrease cardiac contractility
CIRCULATION RESEARCH
466
(Naylor and Szeto, 1972; Buccino et al., 1967). In
addition, a reduction in Tpd was not observed until
barbiturate levels, substantially higher than those
measured in dog plasma, were achieved. Further,
barbiturates prolong relaxation time when Tpd is
depressed (Nayler and Szeto, 1972). We observed
that RTi/2 did not increase following exposure to
PEEP plasma.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
In Vivo Negative Inotropic Effects
These considerations make it likely that PEEP
plasma contains a negative inotropic agent (or reduced levels of a positive inotropic agent). The
decrease in contractility is not caused by changes
in P02, pH,- temperature, lactate, or barbiturate.
This negative inotropic effect of PEEP has been
demonstrated previously in intact, as well as in ex
vivo perfused hearts (Patten et al., 1978; Manny et
al., 1978a). The present study does not demonstrate
an in vivo decrease in contractility, since no direct
measurements of contractility parameters, such as
end-systolic or end-diastolic fiber length, were
made. However, the inference that negative inotropism did occur in vivo is supported by the direct
relationship between the in vivo percent decrease
in CO and the in vitro percent decrease in Tpd (Fig.
4). The equation describing the least square fit of
this relationship is % fall Tpd = 36% fall CO - 0.19.
It is possible, but not proven by our data, that these
are causally related events. If the latter is true,
then, in theory, the slope of 36% is an approximation
of the contribution of decreased contractility in
reducing CO. The fact that the agent may be destroyed partially by plasma during the hour of in
vitro testing at room temperature makes this estimate of the role of contractility a possible underestimate.
Studies on the ex vivo perfused heart indicate
that the negative inotropic effect appears and disappears within minutes (Fig. 3). Application of
PEEP leads, at first, to an increase and, eventually,
a net decrease in contractility. Removal of PEEP is
followed by restoration of contractility and a tran-
VOL. 45, No. 4, OCTOBER
1979
sient positive inotropic effect. These events are
consistent with a combination of positive and negative inotropic influences. Thus, the hypotension
occurring immediately after PEEP is likely to have
stimulated the sympathoadrenal system. In previous studies, bleeding the support animal, used to
perfuse the isolated heart to achieve a CO and
arterial pressure equivalent to values observed during PEEP, led to an increase in PSP (Manny et al.,
1978a). In other experiments, preventing the PEEPinduced decline in flow and pressure with volume
infusions led to significant falls in PSP.
The delayed recovery of Tpd after the reapplication of O-EEP plasma to the papillary muscle,
compared with the rapid restoration of PSP in the
perfused heart, is consistent with the presence of a
negative inotropic agent. It would be expected that
the capacity for metabolism of a newly formed
agent might be reduced in vitro. Any negative inotropic agent still attached to the cellular membrane
after exchange of plasmas might require spontaneous degradation for inactivation.
The negative inotropic agent has not been characterized chemically. The fact that arterial levels of
the prostaglandin, PGF2,,, and its metabolite, 15keto-13,14 dihydro—PGF^, were not changed by
PEEP (Manny et al., 1978a) does not exclude the
action of other prostaglandins. These lipids are
attractive mediators, since lung stretch will alter
the pulmonary processing and metabolism of these
agents (Berry et al., 1971). Further, many of the
prostaglandins are vasoactive (Lee, 1976), and at
least one of them is thought to possess negative
inotropic properties (Fitzpatrick et al., 1978). It
remains possible that nonlipid agents may be involved. For example, several peptides have been
found in the effluent of lungs following mechanical
stimulation (Said et al., 1975; Berry et al., 1971).
Further, the lungs recently have been shown to
secrete plasminogen activator in response to pressure breathing and PEEP (McLoughlin et al., 1978).
Whether the release mechanisms for the negative
inotropic agent share common properties with vasoactive substances is unknown. The resolution of
these questions requires further study.
References
20
40
60
80
100
DECREASE IN CO (X)
FIGURE 4 There is a direct relationship between the
percent fall in CO induced by PEEP and the percent
decrease in developed tension (Tpd).
Berry EM, Edmunds JF, Wyllie JH (1971) Release of prostaglandin Ej and unidentified factors from ventilated lungs. Br
J Surg 58: 189-193
Braunwald E, Binion JT, Morgan WL Jr, Samoff SJ (1957)
Alterations in central blood volume and cardiac output induced by positive-pressure breathing and counteracted by
metaraminol. Circ Res 5: 670-675
Buccino RA, Sonnenblick EH, Spann JF, Friedman WF, Braunwald E (1967) Interaction between changes in the intensity
and duration of active state in the characterization of inotropic
stimuli in heart muscle. Circ Res 21: 857-867
Cournand A, Motley ML, Werko L, Richards DW (1948) Physiological studies of the effect of intermittent positive-pressure
breathing on cardiac output in man. Am J Physiol 152: 162174
Edman KAP, Maitiazzi A, Nilsson E (1974) The influence of
NEGATIVE INOTROPISM AND PEEP/Grindlinger et al.
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
temperature on the force-velocity relationship of rabbit papillary muscle. Acta Physiol Scand 90: 750-756
Elkins RC, Peyton MD, Hinshaw LB, Greenfield NJ (1974)
Clinical hemodynamic and respiratory responses to graded
positive end-expiratory pressure. Surg Forum 25: 226-229
Fitzpatrick TM, Alter I, Corey EJ, Ramwell PW, Rose JC, Kot
PA (1978) Cardiovascular responses to PGL; (prostacyclin) in
the dog. Circ Res 42: 192-194
Gimeno AC, Gimeno MF, Savino EA, Bedners AS (1966) Effects
of glucose, pyruvate, lactate, and starvation on contractility of
isolated rat atria. Proc Soc Exp Biol Med 123: 875-880
Goldbaum LR (1948) An ultraviolet spectrophotometric procedure for the determination of barbiturates. J Pharmacol Exp
Ther 94: 68-75
Heinemann HO, Ryan JW, Ryan US (1977) Is the lung a paraendocrine organ? Am J Med 63: 595-603
Hill AV (1951) Effect of series compliance on tension development in a muscle twitch. Proc R Soc Lond [Biol] 138: 325329
Johannsson M, Nilsson E (1975) Acid-base changes and excitation-contraction coupling in rabbit myocardium. I. Effects on
isometric tension development at different contraction frequencies. Acta Physiol Scand 93: 295-309
Kumar A, Falke KF, Geffin B, Aldredge CR, Laver MB, Lowenstein E, Pontoppidan H (1970) Continuous positive-pressure
ventilation in acute respiratory failure. N Engl J Med
283(suppl 26): 1430-1436
Lee JB (1976) Prostaglandins and blood pressure control. Am J
Med 61: 681-695
Liebman PR, Patten MT, Manny J, Hechtman HB (1978) The
mechanism of depressed cardiac output on positive end-expiratory pressure (PEEP). Surgery 83: 595-598
Lozman J, Powers SR, Older T, Dutton RC, Roy RJ, English M,
Marco D, Eckert C (1974) Correlation of pulmonary wedge
and left artnal pressures. Arch Surg 109: 270-277
Manny J, Grindlinger G, Mathe A, Hechtman HB (1978a) Positive end-expiratory pressure, lung stretch, and decreased myocardial contractility. Surgery 84: 127-133
467
Manny J, Patten MT, Liebman PR, Hechtman HB (1978b) The
association of lung distension, PEEP, and biventricular failure.
Ann Surg 187: 151-159
Manny J, Justice RE, Hechtman HB (1979) Abnormalities in
organ blood flow and its distribution during PEEP. Surgery
85: 425-432
McLoughlin GA, Manny J, Grindlinger GA, Hechtman HB
(1978) Induction of fibrinolytic activity by pressure breathing.
Surg Forum 29: 201-203
Morgan BC, Martin WE, Horenbein TF, Crawford EW, Untheroth WG (1966) Hemodynamic effects of intermittent positivepressure respiration. Anesthesiology 27: 584-590
Nayler WG, Szeto NJ (1972) Effect of sodium pentobarbital on
calcium in mammalian heart muscle. Am J Physiol 22:(Suppl
2): 339-344
Pannier JL, Weyne J (1970) The influence of lactate on the
contractile properties of papillary heart muscle. Arch Int
Physiol Biochim 78: 101-110
Patten MT, Liebman PR, Manny J, Shepro D, Hechtman HB
(1978) Humorally mediated alterations in cardiac performance
as a consequence of positive end-expiratory pressure. Surgery
84: 201-205
Said SI, Mutt V, Noshida T, Hara N (1975) Vasoactive polypeptides from normal lung. Chest 67: 44S
Siggaard-Anderson O (1963) Blood acid-base alignment nomogram. Scand J Clin Lab Invest 15: 211-217
Sonnenblick EH (1964) Series elastic and contractile elements
in heart muscle: Changes in muscle length. Am J Physiol 207:
1330-1338
Sonnenblick EH, Skelton CC (1971) Myocardial energetics:
Basic principles and clinical implications. N Engl J Med 285:
668-675
Suter P, Fairley B, Isenberg M (1975) Optimum end-expiratory
airway pressure in patients with acute pulmonary failure. N
Engl J Med 292: 284-289
Tyberg JV, Yeatman LA, Parmley WW, Urschel CW, Sonnenblick EH (1970) Effects of hypoxia on mechanics of cardiac
contraction. Am J Physiol 218(Suppl 6): 1780-1788
Presence of negative inotropic agents in canine plasma during positive end-expiratory
pressure.
G A Grindlinger, J Manny, R Justice, B Dunham, D Shepro and H B Hechtman
Downloaded from http://circres.ahajournals.org/ by guest on October 2, 2016
Circ Res. 1979;45:460-467
doi: 10.1161/01.RES.45.4.460
Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1979 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7330. Online ISSN: 1524-4571
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circres.ahajournals.org/content/45/4/460
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further information
about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation Research is online at:
http://circres.ahajournals.org//subscriptions/