12601150_Visuals.ppt (946.5Kb)
advertisement

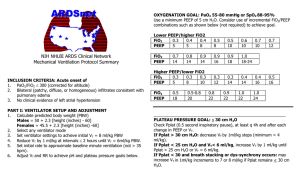
Optimising Ventilation Using a Simple Model of Ventilated ARDS Lung Geoffrey M Shaw1, J. Geoffrey Chase2, Toshinori Yuta2, Beverley Horn2 and Christopher E Hann2 1Univ of Otago, Christchurch School of Medicine and Health Sciences 2 Univ of Canterbury, Dept of Mechanical Engineering, Centre for Bio-Engineering Introduction • Mechanical ventilation is a “bread and butter” therapy in critical care • It is well known that a properly or well ventilated patient has an increased likelihood of improved outcome • However, selecting optimal settings, such as PEEP and tidal volume are difficult • Especially, as these settings can change regularly as patient condition evolves, particularly in ARDS • Hence, a method of monitoring and capturing these changes and then optimising ventilation would offer significant clinical benefit. Models offer the opportunity to both monitor and optimise ventilated patient status for better outcomes Model Basics • • • Collapsed Peak Volume Abnormal End Exp. Volume • Tidal • Volume Clinical Tradeoff: Maximise gas exchange and minimise risk of damage (e.g. tidal volume and PEEP “within reason”) Inspiretory Pressure • Volume Goal = capture critically ill patient behaviour Healthy region is kept inflated under PEEP Most of volume change occurs in abnormal region Recruitment and Derecruitment (R/D) is the fundamental mechanism of volume change Healthy PEEP Pressure Peak Pressure Requirement: Simple model to determine the recruitment status of a patient and thus the pressure, volume changes for various PEEP and tidal volume settings/choices More Detail • Compartments with different superimposed pressure • Lung units – cluster of alveoli and distal airways Model Number of Units • Recruitment is described by Threshold Opening Pressure (TOP) • Derecruitment is described by Threshold Closing Pressure (TCP) • Skewed normal distribution • Unique to a patient and condition TCP TOP Pressure Results • True lung PV curve with associated threshold pressure distributions PEEP • Unique distributions for different levels of PEEP are found Clinical Application • Optimisation of ventilation – Parameter identification = patient specific model – Simulation to determine effect of settings on PV curve – Optimise ventilator settings as desired Clinical Application • Optimisation of ventilator treatment – Reduces recovery time – Detect over-inflation • Up-to-minute condition specific result – Result immediately applicable – Unique to patient and condition • Provides continuous patient monitoring • Simple GUI based system could be readily put on a PDA Clinical Application • Data requirements: – Pressure and flow (volume) data at different PEEP values (2 minimum, 3 preferred = current and +/- 2-5 cmH2O • Data acquisition: – – – – Obtain data directly from ventilator Patient kept on ventilator No additional tests, i.e. CT, MRI Fully/Semi automatic data acquisition, simulation, and analysis • Similar data can be used for full validation study GUI Lung parameters Resulting PV curve Alternative settings Summary • Simplified model of mechanics captures fundamental characteristics • Shows a potential to be a clinical tool to: – Estimate and track state of disease – Provide continuous monitoring – Provide objective optimal ventilator settings • Minimum interference to the patient and staff Any Questions?