Anatomy Lab
advertisement

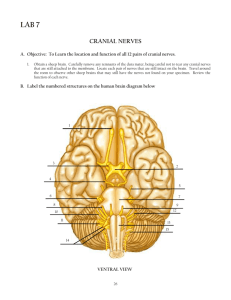
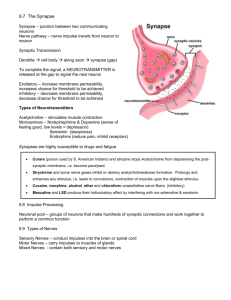
AP1, Lab 8 - Central Nervous System The 12 Pairs of Cranial Nerves # I II III IV V Name Olfactory Optic Oculomotor Trochlear Trigeminal VI VII Abducens Facial VIII IX Vestibulocochlear Glossopharyngeal X Vagus XI Accessory XII Hypoglossal Function Sensory impulses from nose for sense of smell Sensory impulses from eye for vision Motor impulses to eye muscles for movements of the eyes Motor impulses to eye muscles for movements of the eyes Sensory impulses info from face, scalp, and teeth; Motor impulses to temporal and masseter muscles for closing the mandible as when chewing Motor impulses to eye muscles for abduction of the eyes Sensory impulses from some taste buds of tongue; Motor impulses to muscles controlling facial expressions like frowning, smiling, etc. Sensory impulses from ear for senses of both sound and balance Sensory impulses from throat and some taste buds at the back of the tongue (salty); Motor impulses to muscles of throat for swallowing and to salivary glands Sensory impulses from throat, larynx, thoracic and abdominal organs; Motor impulses to stimulate digestive organs, to slow heart rate, to cough, and to swallow. Motor impulses to trapezius and sternocleidomastoid muscles of the neck and upper shoulder for shoulder movements and movements of the head. Motor impulses to muscles of the tongue for most tongue movements. MNEMONIC DEVICES for Names of Cranial nerves: On occasion, our trusty truck acts funny - very good vehicle anyhow Or: Oh, Oh, Oh—To Touch And Feel Very Good Velvet, A-H! MNEMONIC DEVICE for Sensory, Motor, or Both: Some say Marry Money, but my brother says Big Business makes money Or: Some Say Marilyn Monroe, But My Brother Says Brigitte Bardot, My, My! Revised 8/20/14 1 Visual learning: The figure below is especially useful to visual learners: There are 12 pairs of cranial nerves in humans. Their Roman numeral designations and names are: I Olfactory II Optic III Oculomotor IV Trochlear V Trigeminal VI Abducens VII Facial VIII Vestibulocochlear (auditory) IX Glossopharyngeal X Vagus XI Accessory (spinal accessory) XII Hypoglossal The cranial nerves mostly innervate structures in the head and neck. The cartoon codes for at least one major functional innervation of each cranial nerve. This drawing is based on one done by Beatrice Humphris, R.N. published in Nursing 1984. http://www.sci.uidaho.edu/med532/cranialnervebackgroundinfo.html Revised 8/20/14 2 12 pairs of cranial nerves are associated with the ventral aspect of the brain. —The first 2 pairs attach to the forebrain, the rest originate from the brainstem. **Note: The Intermediate nerve included in the diagram above is actually the smaller root of the facial nerve (VII). Most images do not illustrate it separately. This one just happens to do so. Revised 8/20/14 3 Test Your Cranial Nerves Now that you know the names and functions of the cranial nerves, let's test them. These tests will help you understand how the cranial nerves work. These tests are not meant to be a "clinical examination" of the cranial nerves. You will need to get a partner to help...both of you can serve as the experimenter (tester) and the subject. Record your observations of what your partner does and says. Olfactory Nerve (I): sensory for smell Gather some items with distinctive smells (for example, cloves, lemon, chocolate or coffee). Have your partner smell the items one at a time with each nostril. Have your partner record what the item is and the strength of the odor. Now you be the one who smells the items...have your partner use different smells for you. Optic Nerve (II): sensory for sight Use an eye chart (a "Snellen Chart") and have your partner try to read the lines at various distances away from the chart. Cranial nerves III, IV and VI are tested together. They each control muscles involved with eye movement. In addition, the oculomotor also functions in pupil dilation. Oculomotor Nerve (III), Trochlear Nerve (IV) and Abducens Nerve (VI): Motor These three nerves control eye movement and pupil diameter. Hold up a finger in front of your partner. Tell your partner to hold his or her head still and to follow your finger, then move your finger up and down, right and left. Do your partner's eyes follow your fingers? Check the pupillary response (oculomotor nerve): look at the diameter of your partner's eyes in dim light and also in bright light. Check for differences in the sizes of the right and left pupils. Trigeminal Nerve (V): sensory for touch/pain in face motor for chewing (mastication) The trigeminal nerve has both sensory and motor functions. To test the motor part of the nerve, tell your partner to close his or her jaws as if he or she was biting down on a piece of gum. Temporal and masseter muscles of the face should have equal strength To test the sensory part of the trigeminal nerve, lightly touch various parts of your partner's face with piece of cotton or a blunt object. Be careful not to touch your partner's eyes. Although much of the mouth and teeth are innervated by the trigeminal nerve, don't put anything into your subject's mouth. Revised 8/20/14 4 Facial Nerve (VII) Sensory for taste on anterior 2/3 of tongue and salivary glands. Sensory from external auditory meatus and ear drum but NOT sensory from inner ear for hearing. Motor for controlling muscles used in facial expression The motor part of the facial nerve can be tested by asking your partner to smile or frown or make funny faces. Lack of symmetry when smiling or frowning may indicate damage to this nerve or a portion of the motor cortex – might indicate a stroke. The sensory part of the facial nerve is responsible for taste on the front part of the tongue. You could try a few drops of sweet or salty water on this part of the tongue and see if your partner can taste it. Vestibulocochlear Nerve (VIII): Sensory for sound and balance The vestibulocochlear nerve is a branching nerve. The cochlear nerve is responsible for hearing and the vestibular controls balance. Hearing: Have your partner cover one ear and close his or her eyes. Stand about 2 feet from the subject and whisper a word with 2 distinct syllables, like mailman, or football and observe for difficulties distinguishing words. You may also determine the distance at which he or she can hear the ticking of a clock or stopwatch. Balance: Test for balance by having the subject stand with his feet close together and eyes closed. The subject may sway a little, but should not fall. Cranial nerves IX and X can be tested together since they both serve to innervate the pharynx. Glossopharyngeal Nerve (IX): Sensory for taste on the posterior 1/3 of the tongue and conveying information from the tongue, tonsils and pharynx Motor for swallowing Have your partner drink some water and observe the swallowing reflex. Also the glossopharyngeal nerve is responsible for taste on the back part of the tongue. You could try a few drops of salty (or sugar) water on this part of the tongue and see if your partner can taste it. Vagus Nerve (X): Sensory from throat, larynx, thoracic and abdominal organs Motor for swallowing, esophagus and to stimulate stomach and intestines (digestion). Motor to slow HR. Have the subject speak or cough. Her voice should be clear and strong. Cough should be strong. Subject should have a strong gag reflex. Spinal Accessory Nerve (XI): Motor to control the sternocleidomastoid and trapezius muscles involved in head movement Put your hands on your partner’s shoulders from the back. As you apply slight resistance, have him shrug his shoulders upward. Contraction should be symmetrical. Now place one hand on one side of your partner's jaw. Tell your partner to move his or her head toward your hand while you apply slight resistance. Repeat on the opposite side. Strength in the sternocleidomastoid should be symmetrical. Hypoglossal Nerve (XII): Motor for tongue movement Have your partner stick out his or her tongue and move it side to side. Check for symmetry. Revised 8/20/14 5 DO YOU KNOW……? Which cranial nerve is the largest? _______________________________ Which cranial nerves are responsible for eye movements? ______________ What does "abducens" refer to? _________________________________ Which cranial nerves carry gustatory (taste) information? ______________ Which cranial nerve is the longest? _______________________________ Which nerve or nerves are involved in: Rotating the head? _________________________________________ Smelling a flower? _________________________________________ Raising the eyelids, pupillary constriction? ________________________ Slowing the heart rate? _____________________________________ Increasing motility of the digestive tract? _______________________ Bell’s Palsy? ______________________________________________ Chewing food? ____________________________________________ Listening to music? _________________________________________ Seasickness? _____________________________________________ Secretion of saliva? ________________________________________ Sensation of taste? ________________________________________ Rolling the eyes? (3 nerves)__________________________________ Feeling a toothache? _______________________________________ Reading a newspaper? ______________________________________ Purely sensory in function? __________________________________ Revised 8/20/14 6 Revised 8/20/14 7 PAIN HOW THE BODY BLOCKS PAIN The Medical community has observed that a person can block or reduce the amount of perceived pain. Over time there have been many theories of the physiology of this phenomenon. The current theory states: the brain, in response to pain, will activate analgesic systems in the brainstem. These in turn will relay pain-suppressing signals to the spinal cord to release endogenous opioids such as ENDORPHINS and ENKEPHALINS. These create IPSPs to cancel out EPSPs (Substance P) produced by the pain receptors. HOW MEDICATIONS BLOCK PAIN: ASPIRIN and IBUPROFEN inhibit prostaglandin activity thereby reducing inflammation and pain. ACETAMINOPHEN (Tylenol) blocks pain but not inflammation by inhibiting activation of the COX enzyme. NSAIDS are anti-inflammatory in a variety of ways; often as COX2 inhibitors NARCOTICS such as morphine, Demerol, and heroin reduce pain by mimicking the effects of endorphins and enkephalins. HOW A T.E.N.S. UNIT BLOCKS PAIN TENS = Transcutaneous Electrical Nerve Stimulation Every day, ordinary afferent sensory impulses enter the spinal cord at the posterior horns of the gray matter. Here they must pass through synapses before traveling up to the brain via ascending tracts of the spinal cord. Pain messages follow the same pathway. Applying continuous or repetitive stimulation through the skin of an appropriate area using TENS ‘annoys’ the brain with a flood of sensory input. In response, the brain increases the frequency of impulses down the spinal cord to create IPSPs to “block” both the incoming messages from the skin as well as the pain messages. Electrical stimulation of nerves using TENS also stimulates the release of endorphins so that fewer pain generating impulses reach the brain, so pain is not felt or at least is felt less. Revised 8/20/14 8 REFERRED PAIN A painful sensation felt in a region of the body that is not the origin of the stimuli. Usually, it’s a painful sensation of visceral origin felt in a somatic region of the body that is not the origin of the stimuli. Examples: 1. Heart attack – the origin of the impulses is the heart muscle but the pain is often felt in the upper chest, left side of the mandible, and on the medial surface of L arm. 2. Gallbladder and Liver – often felt at the top of the R shoulder. 3. Kidney, Ureters, and Urinary Bladder – often felt in the lower back, groin, or scrotum. 4. Appendix – often felt near the umbilicus Happens because the visceral sensory neurons and somatic sensory neurons converge on the same ascending tracts of the spinal cord. When messages arrive on these tracts the brain can’t always distinguish between the two points of origin. PHANTOM LIMB PAIN and HYPERALGESIA The sensation of pain experienced in a body part you no longer have – a missing foot, leg, arm, etc. The brain receives no sensory information from the missing limb to inhibit pain sensations. If an action potential is initiated anywhere along the neuronal pathway from the severed limb, the idea of pain will be projected back to the missing limb even though the limb is not there. Hyperalgesia is pain amplification and is common in amputations. In order to reduce this hyperalgesia during amputations, epidural anesthetics (in addition to general anesthesia) are used to block neurotransmission in the spinal cord and thus prevent the spinal cord from “learning” hyperalgesia. Revised 8/20/14 9 Dissection of Cow Brain with Dura Mater Use images from the dissection manuals in lab and your knowledge of the brain to identify the following. Recall the functions of those with an *. Your group will be evaluated on the quality of your dissection. FOLLOW INSTRUCTIONS CAREFULLY. 1. Glove up – your choice of latex or polyethylene. 2. Safety – practice caution with the knives and other implements. 3. Housekeeping (Your mother does not work here, kindly clean up after yourself) – Don’t put pieces of tissue in the sink. If you notice, there is no garbage disposal. At the end of lab, we will put brains back in the bag. Don’t get “slime” on the brain models. When you are finished, wash everything and return it where you found it. 4. Open your bag and rinse away as much preservative as possible. Observe the dull white DURA MATER covering the surface of the brain. 5. The two, large fatty masses dangling from the anterior and inferior surface are the tissues that were behind the eyes. Find the two OPTIC NERVES in these and then cut the fatty mass off. 6. Use scissors to cut away the superior 90% of the DURA MATER. Leave the bottom portion intact as it will contain the pituitary gland. The ARACHNOID LAYER will come off with the dura mater leaving only the PIA MATER on the surface of the brain. 7. Observe the LONGITUDINAL and TRANSVERSE FISSURES containing DURAL SINUSES as you remove the dura mater. What occurs at your dural sinuses? _______________ 1. Identify the following externally visible structures while the brain is still whole. No cutting necessary. CEREBRUM L and R CEREBRAL HEMISPHERES Various SULCI & GYRI OLFACTORY BULBS and OLFACTORY TRACTS. This is CRANIAL NERVE #1 carrying sensory messages to the brain for the sense of smell. Observe the delicate PIA MATER anchoring blood vessels to the cerebrum mostly in the sulci. These vessels are dark brown/black in color. CEREBELLUM OPTIC NERVES and OPTIC CHIASMA. Cut the optic nerves (cranial nerve #2) and other motor nerves as far out as you can clearly see them to get rid of those dangling lumps of fatty tissue that were located behind the eyes. Pituitary gland - usually appears as a nodule or “lump” approximately ¼ inch in diameter on the ventral side of the brain.) TRIGEMINAL NERVES - The lateral edges of the dura mater containing the pituitary gland also contain the large trigeminal nerves (cranial nerve #5). Cut the nerves near the dura mater to leave stumps on the lateral walls of the pons. Remove the dura mater containing any branches of this nerve but do not remove the pituitary gland. Revised 8/20/14 10 OCULOMOTOR NERVES – Gently lift the pituitary gland from its anterior edge while looking for the oculomotor nerves (cranial nerve #3) to be raised with the dura mater and the pituitary gland. Go ahead and remove the dura mater and pituitary gland. The stumps of the oculomotor nerves will either be lying on the midbrain, projecting forward or they will have torn loose and be attached to the dura mater above the pituitary gland. BRAIN STEM Spinal cord – function? Medulla Oblongata – functions? Pons – functions? **Confirm identifications of everything up to this point with your instructor. 2. Bisect the brain on the mid-sagittal plane along the longitudinal fissure all the way through the brain stem. Make one clean, straight cut all the way through. Try to cut as precisely in the middle as possible. Identify the following. Corpus Callosum and Fornix– recall function? Thalamus – recall functions? Hypothalamus – recall functions? Lateral ventricles - Use your metal probe to separate the corpus callosum and the fornix in order to see better into the lateral ventricles. The corpus callosum will be the roof and the fornix will be the floor of each ventricle. Third ventricle – Look above the thalamus but below the fornix. Choroid plexus - specialized capillaries for production of CSF. They are delicate and dark brown in color similar to the vessels on the surface of the cerebrum. Use your forceps to gently reach deep into the posterior portion of a lateral ventricle and pull some of this out. You might also find some in the 3rd and 4th ventricles. Cerebral aqueduct – passageway for CSF to flow from 3rd to 4th ventricle. Fourth ventricle – space between the cerebellum and spinal cord. 3. Locate your thalamus again. Put the two hemispheres back together and perform a coronal section such that your cut passes through the thalamus. Hold the two posterior portions together and view them from the anterior side. Identify the following: Cerebral white matter Cerebral cortex - The term “cortex” refers to the outer layer of any structure. On the cow brain it’s the darker, more superficial layer that borders the white matter and follows the contour of the sulci. The majority of the synapses of the brain are found in the cortex. Corpus callosum Lateral ventricles Fornix Third ventricle Thalamus Revised 8/20/14 11