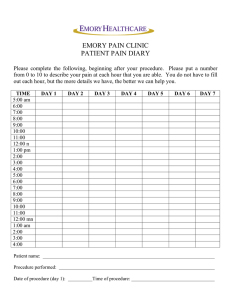
Pain Consult | 2013
advertisement

Inside This Issue Tag-Teaming Chronic Headache p6 Improving Ablation for SI Joint Pain p8 Opioid Complications: More than Just Abuse p 12 Research Snapshots and Clinical Trials pp 14, 16 Pain Consult D E PA R T M E N T O F PA I N M A N A G E M E N T | 2 0 1 3 mild Procedure Minimally Invasive Approach to Lumbar Spinal Stenosis p3 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) Dear Colleague, At Cleveland Clinic, we recognize the central role that innovation plays in meeting our nation’s growing imperative to deliver greater healthcare value — that is, better patient outcomes without higher overall costs. I’m pleased that this issue of our Department of Pain Management’s Pain Consult is full of examples of that kind of innovation. Take the story on page 8 featuring the work of Jianguo Cheng, MD, PhD, in developing a simple yet ingenious tool to improve radiofrequency ablation (RFA) for sacroiliac joint pain. Faced with the need to precisely place seven or eight needle electrodes for the procedure, Dr. Cheng designed a small plastic template to quickly and reliably guide placement of the electrodes. The result has been a two-thirds reduction in procedure length, a 90 percent reduction in patients’ X-ray exposure and greater patient comfort. In other words, markedly improved healthcare value. Other stories spotlight additional examples of innovation in our department. The cover story touches on Cleveland Clinic’s contributions to early clinical testing of the minimally invasive mild® procedure for lumbar spinal stenosis and the encouraging results we’ve achieved to date. And the “Research SnapVKRWVµVHFWLRQRQSDJHSURÀOHVVHYHUDORIRXUVWDII·VUHVHDUFKLQLWLDWLYHVLQ areas ranging from cooled RFA for painful bone tumors to ultraprecise spinal cord stimulation for lower extremity pain. Our ethic of innovation extends beyond procedures, devices and research. For example, the story on page 6 illustrates how patients with chronic headache VWDQGWREHQHÀWIURP&OHYHODQG&OLQLF·VVLQJXODUPRGHORIFROODERUDWLRQEHWZHHQ our department’s pain medicine experts and the headache specialists in Cleveland Clinic’s Neurological Institute. And the story on page 10 examines how a number of our pain specialists are bringing complementary and alternative medicine to bear for increasing numbers of patients with chronic pain. The quest for value in our changing healthcare landscape depends increasingly on this ethic of innovation. It also depends on a commitment to sharing successes in innovation with our colleagues across the nation in a multidisciplinary fashion. That is the spirit in which we bring you this Pain Consult newsletter. ,KRSH\RXÀQGLWVWLPXODWLQJDQG,XUJH\RXWRFRQWDFWPHRUP\FROOHDJXHV who are featured in these pages with your feedback and thoughts. Richard W. Rosenquist, MD Chairman, Department of Pain Management rosenqr@ccf.org | 216.445.8388 2 On the Cover: Nagy Mekhail, MD, PhD (foreground), performs the mild procedure in a patient with lumbar spinal stenosis. clevelandclinic.org/painmanagement 2013 | Pain Consult Cleveland Clinic Procedure, Intense Satisfaction Minimally Invasive Approach to Lumbar Spinal Stenosis Relieves Pain and Increases Mobility P atients with moderate to severe lumbar spinal stenosis (LSS) often can’t stand longer than a few minutes or walk more than a few hundred feet without developing severe pain. This VLJQLÀFDQWO\OLPLWVWKHLUDFWLYL ties and quality of life. Until a few years ago, the only treatment options available for patients with LSS were conservative therapies or open spine surgery. Continued next page i 3 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) For patients who don’t respond to con- Patients with moderate to severe LSS may The mild procedure offers a new treat- servative treatment and are unable or be candidates for mild if they complain of ment option for these patients. “With unwilling to undergo open spine surgery, neurogenic claudication and if MRI shows more than 10,000 baby boomers turning Cleveland Clinic’s Department of Pain WKDWDWKLFNHQHGOLJDPHQWXPÁDYXPQRW 65 every day, more and more patients Management now offers a novel X-ray- a bulging disk, is the major cause of the are seeking innovative treatments such guided percutaneous outpatient treatment spinal stenosis, Dr. Mekhail says. as mild to stay active and maintain their called mild®, which stands for minimally invasive lumbar decompression. C A N FA L L S H O R T M I N I M A L LY I N V A S I V E , “The mild procedure decreases pain Nonsurgical treatment for LSS includes M A X I M A L LY Q U I C K R E C O V E R Y and increases mobility while maintain- NSAIDs, physical therapy and/or epidural The mild procedure is performed under ing the structural integrity of the spine,” LQMHFWLRQVWRUHOLHYHLQÁDPPDWLRQDQG deep sedation through a 1-cm incision. The says Nagy Mekhail, MD, PhD, Director swelling. These treatments are effective in clinician uses a special sculpting tool that of Evidence-Based Medicine in the only a small percentage of patients, and glides through a portal with a diameter of 5 Department of Pain Management. WKHLUFKDQFHVRIHIÀFDF\GHFUHDVHZLWKWKH mm, about the size of a pen cap, to go be- The average age of patients presenting with duration of LSS. If they do work, the effect tween the bones, scrape out the ligaments may not be sustained, and they need to and widen the spinal canal to reduce nerve the mild procedure in July 2012, and a be repeated. compression (see images below). X-ray number of private insurers cover it as well. “Epidural steroid injections tend to have LSS is 73 years. Medicare began covering W H O ’ S A C A N D I D AT E ? LSS may be due to a bulging disk and/or hypertrophy of the ligamentum limited effectiveness because LSS pain LVLVFKHPLFUDWKHUWKDQLQÁDPPDWRU\LQ origin, as in radicular pain due to a herniated lumbar disk,” Dr. Mekhail explains. ÁDYXPZKLFKOLQHVWKHEDFNRIWKH spinal canal. Narrowing of the spinal 6RPHSDWLHQWVZKRKDYH/66FDQEHQHÀW canal causes nerve compression. When from open spine surgery, in which the someone with LSS stands or walks, the laminae are removed to relieve pressure on spinal canal narrows even more, caus- the spinal nerves. However, not all patients ing neurogenic claudication, or low back are candidates for open spine surgery, and leg pain that is relieved with sitting especially since surgery and anesthesia or bending forward. carry a higher risk in the older patients who account for the bulk of LSS cases. 4 quality of life,” Dr. Mekhail says. TRADITIONAL OPTIONS ÁXRURVFRS\DQGUHSHDWHGLQMHFWLRQRIFRQ trast material into the epidural space are used to assess positioning and assist with visualization throughout the procedure. Because the architecture of the spine remains intact, spinal mechanics are not disrupted and patients typically recover quickly. They are discharged home after a couple of hours and are able to begin ZDONLQJZLWKLQWKHÀUVWKRXUVDIWHU the procedure. Patients are encouraged to walk regularly and/or participate in physical therapy following the procedure. Radiographic views of a spine before (left) and after (right) the mild procedure. Widening of the spinal canal decompresses nerves, relieving chronic pain from lumbar spinal stenosis. 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic ENCOURAGING AND E N D U R I N G R E S U LT S Results with mild to date have been PATIENTS PLEASED WITH QUALITY-OF-LIFE PAYOFFS encouraging. Dr. Mekhail and colleagues recently published one-year outcomes Enthusiastic testimonials are common among patients who have had the mild among dozens of patients who under- SURFHGXUHIRU/66+HUHDUHSURÀOHVRIVHYHUDOSDWLHQWVZKRXQGHUZHQWWKH went the mild procedure (see Suggested procedure in Cleveland Clinic’s Department of Pain Management. Reading). Highlights include: • No major device- or procedure-related complications •6LJQLÀFDQWUHGXFWLRQLQSDLQDW one-year follow-up • Improvement in physical functionality and mobility as measured by change (before vs. after procedure) in walking distance and standing time • Decreased disability secondary to neurogenic claudication Results are no less impressive at the individual patient level, as illustrated in the sidebar. “Patients are able to get back to more normal lives and the activities they enjoy — everything from grocery shopSLQJWRJROÀQJµ'U0HNKDLOQRWHV Frances Robinson, 70, had the procedure in January 2012. She had previously received epidural injections to control her LSS-related pain, but the effectiveness would eventually wear off. “I couldn’t walk too far or I would get pain down my OHJDQGZRXOGKDYHWRVWRSµVKHVD\V6KHDOVRFRXOGQ·WVWDQGORQJHUWKDQÀYH or six minutes without having to sit or lie down. Since the procedure, Mrs. Robinson has been able to run errands and do FKRUHVDURXQGWKHKRXVHWKDWKDGEHFRPHLQFUHDVLQJO\GLIÀFXOW2QDUHFHQW WULSWR)ORULGDVKHZDVDEOHWRHQMR\ZDWHUDHURELFVVKRSDWÁHDPDUNHWVDQG outlet stores, and comfortably walk on the beach with her husband for 40 to 50 minutes at a time. “I call the mild procedure my miracle,” Mrs. Robinson says. “I would certainly advise others to consider this procedure, as it made such a big difference to my life.” Michael O’Malley, 71, used to experience LSS-related pain that “felt like an electric shock that started at the hip and went all the way down to the knee.” That pain is a distant memory since he underwent the mild procedure in November 2012. Despite unrelated hip pain for which he is seeking treatment, Mr. O’Malley has been regularly walking a quarter of a mile a day for exercise. He says he was impressed that mild was done on an outpatient basis and he To refer an LSS patient for evaluation for was able to get back to his normal activities so quickly. “The procedure was the mild procedure, call 216.444.9114. amazing, especially the fact that you could go to the hospital at 8 a.m. and be back home by 4 p.m. The doctors and everyone there were excellent. I walked the same day I had the procedure.” Nagy Youssef, 67,DRQHWLPHLQWHUQDWLRQDOOHYHOWUDFNDQGÀHOGDWKOHWHIURP (J\SWFRXOGZDONQRIDUWKHUWKDQIHHWDQGKDGWRVLWDIWHUÀYHPLQXWHVRI VWDQGLQJZKHQKHÀUVWVDZ'U0HNKDLOIRU/66UHODWHGSDLQ7KHSDLQIRUFHG 0U<RXVVHIWRVLJQLÀFDQWO\VFDOHEDFNKLVZRUNFRDFKLQJ(J\SWLDQWUDFNDQG ÀHOGWHDPV+HZDVDOVRXQDEOHWRPHQWRUKLVJUDQGFKLOGUHQLQWKHLUDWKOHWLF SUGGESTED READING pursuits or grocery shop with his wife. Mekhail N, Costandi S, Abraham B, ´7KHEDFNSDLQGHFUHDVHGVLJQLÀFDQWO\DIWHUWKHmild procedure, and I can now Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stand for more than 30 minutes and walk four miles,” says Mr. Youssef, who stenosis following percutaneous decompres- was known as Nagui Assad when he competed in the Olympics in the 1970s sion. Pain Pract. 2012;12(6):417-425. and ’80s. He’s now back at work as a coach, active with his grandchildren and Mekhail N, Vallejo R, Coleman M, Benya- once again able to help his wife with shopping. min RM. Long-term results of percutaneous lumbar decompression mild® for spinal stenosis. Pain Pract. 2012;12(3):184-193. “I feel that my life clock has been wound back to before the year 2000, when the pain started,” Mr. Youssef says. 5 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) Collaboration Brings a Full Spread of Options for Chronic Headache // FEATURING SUMIT KATYAL, MD, and STEWART TEPPER, MD // For patients with refractory chronic headache, pain relief often is all about treatment options — having enough of them and having access to the expertise to deploy them wisely. Cleveland Clinic’s Department of Pain nerve blocks — medial branch blocks, Dr. Katyal for interventional procedures Management includes several pain atlantoaxial (or C1-2) blocks, spheno- or for diagnostic support in especially challenging cases. specialists with expertise in headache palatine ganglion (SPG) blocks, occipital and atypical facial pain. They are a key nerve blocks and others — depending resource in an extensive and multidis- on the source and type of headache. ciplinary array of treatment options Many can alleviate headaches in some Cleveland Clinic offers to patients who patients for six months or more. suffer from refractory chronic headache, sided headache, which Dr. Tepper says usually signals one of three headache types, one of which is cervicogenic head- He also sometimes performs blocks in ache. “The best way to diagnose cervi- conjunction with radiofrequency abla- cogenic headache is to do a block of the tion. In some cases, good response to C1-2 nerve roots,” he says. “So I may D U A L H E A D A C H E / PA I N M E D I C I N E a couple of diagnostic nerve blocks can refer a patient with one-sided headache EXPERTISE predict long-term response to ablation to Dr. Katyal for a diagnostic block. If the or identify good candidates for stimula- headache is stopped cold by the block tor placement. but then returns when the block wears be it migraine, cluster headache or other forms of primary or secondary headache. “We provide a number of interventions to give patients long-term relief from headache pain they may have suffered with for years,” says Sumit Katyal, MD, a member of the Department of Pain Management who is one of a handful of U.S. SK\VLFLDQVERDUGFHUWLÀHGLQERWKSDLQ medicine and headache medicine. Those interventions include: • Specialized nerve blocks • Injection of botulinum toxin and other medications • Radiofrequency ablation C A L I B R AT I N G C A R E W I T H A TEAM OF HEADACHE EXPERTS In those types of cases, Dr. Katyal and off, and if this process can be repeated, we can then diagnose cervicogenic headache and manage it accordingly.” his Department of Pain Management col- S P E C I A L I Z AT I O N M AT T E R S leagues work closely with the headache This type of close cooperation between specialists in the Headache and Facial headache specialists and pain special- Pain Clinic in Cleveland Clinic’s Neurological Center for Pain. Stewart Tepper, MD, is one of those headache specialists. “There’s a lot of consultation and collaboration between ists is not possible at most institutions. “We’re fortunate to have the Headache and Facial Pain Clinic,” says Dr. Katyal. “Many hospitals don’t have a department dedicated to headache medicine, so the neurologists in our headache clinic headache patients are seen by general • Epidural blood patches and the Department of Pain Manage- QHXURORJLVWV+DYLQJERDUGFHUWLÀHG • Stimulator implantation ment,” he says. While Dr. Tepper and Many additional options exist within these categories. For instance, Dr. 6 Take the example of continuous one- Katyal performs a host of different his colleagues provide comprehensive evaluative, diagnostic and medical management services for headache patients, they often refer patients to headache specialists can make a big difference for patients by allowing for more comprehensive and specialized care. Dr. Tepper and his colleagues see headache patients exclusively.” 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic A M U LT I T U D E O F O P T I O N S F O R C H R O N I C H E A D A C H E S U F F E R E R S Department of Pain Management • Interventional management – Radiofrequency ablation – Epidural blood patches – Specialized nerve blocks Headache and Facial Pain Clinic SPG, occipital nerve, others) • Evaluation/diagnosis and medical management by headache specialists IMATCH Program day-hospital program •(YDOXDWLRQRIGLIÀFXOWFDVHVZLWK – Medication injections Chronic Pain Rehab Program • Interdisciplinary – Stimulator implantation (medial branch, atlantoaxial, • Day-hospital program Headache and Facial Pain Clinic) Alcohol and Drug Recovery Center • Inpatient/outpatient Center for Neurological Restoration • Deep brain stimulation for patients with for patients with head- programs for patients and other stimulation medication overuse/ ache refractory to other whose headache has an modalities habituation issues and/ interventions; uses addictive component or medical/psychiatric UHKDELOLWDWLRQGHWR[LÀ comorbidities cation, mobilization Dr. Tepper likewise notes that many pain take care of the whole person by address- medicine physicians do not provide the ing comorbid psychiatric or medical issues “We refer patients and solicit opinions across these various areas all the time,” headache interventions that the Depart- along with the chronic headache,” Dr. says Dr. Tepper. “There is a lot of cross- ment of Pain Management does, because Tepper explains. It is one of only two day- fertilization.” of the technically advanced procedures hospital programs of its kind in the nation. required. “Beyond that,” he adds, “for headache patients in whom additional medications, blocks, stimulators or other procedures are not going to help, there is a very rich smorgasbord of other options at Cleveland Clinic.” As outlined in the diagram above, these include: • The IMATCH (Interdisciplinary Method for Assessment and Treatment of Chronic Headache) Program, a three-week dayhospital program in which patients receive IV infusions and are seen by neurologists, • The Chronic Pain Rehabilitation ProJUDPDWZRWRÀYHZHHNGD\KRVSLWDO program that focuses on rehabilitation WKHUDS\GHWR[LÀFDWLRQDQGPRELOL]DWLRQ “There are very few intensive outpatient pain rehab programs like this in the country,” Dr. Tepper says. • The Alcohol and Drug Recovery Center, MORE OPTIONS THAN MANY REALIZE This richness of available treatment options is something Dr. Katyal hopes physicians become more aware of. “I’m not sure primary care specialists know about the many interventional approaches that can be effective for chronic headache,” he says. “Their paWLHQWVZLWKFKURQLFKHDGDFKHFDQEHQHÀW for patients whose headache has an ad- from many options that might not be diction component. available in their local community.” • The Center for Neurological Restoration, psychologists, internists and physical which offers deep brain stimulation or therapists. “The aim is to wean patients implantation of other stimulators requir- off any overuse headache medications and ing neurosurgery expertise. Dr. Katyal can be contacted at 216.444.3134 or katyals@ccf.org. 7 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) Better Ablation for SI Joint Pain: Template for Precise Needle Placement Shortens Procedure, Reduces X-ray Exposure // FEATURING JIANGUO CHENG, MD, PHD // Sometimes the best innovations are the simplest. Consider the small plastic template that Jianguo Cheng, MD, PhD, developed to guide the precise placement of needle electrodes during radiofrequency ablation (RFA) procedures to treat sacroiliac (SI) joint pain. The template, which is made of a Over the years, four different RFA SAVING TIME AND material similar to the cover of a watch modalities have been developed, with ENSURING PRECISION face, has resulted in: varying levels of clinical complexity and The template that Dr. Cheng developed is • A two-thirds reduction in procedure length, improving patient comfort and saving time for the clinician • A 90 percent decrease in patients’ X-ray exposure ´7KLVLVDPHGLFDOÀUVWµVD\V'U&KHQJ Professor of Anesthesiology and Director of Cleveland Clinic’s Pain Medicine designed with eight holes spaced exactly 1 cm apart, with two small radiopaque the clinician to place seven or eight nee- metal marks embedded in the template dle electrodes that are exactly parallel as guides (see images on page 9). to one another, optimally spaced exactly 1 cm apart. This precise placement causes a geographic lesion between the electrodes, which can be very effective in targeted SI nerve ablation. This simple yet highly utilitarian design ensures that once the clinician numbs the patient’s skin and places the template under X-ray guidance, all the electrodes can be aligned perfectly Fellowship Program in the Department Traditionally, it takes a skilled clinician parallel, ensuring that the geographic of Pain Management. “The template about 45 minutes, with continual X-ray lesions will be made in the desired is effective, practical, easy to use and guidance, to precisely place the needles spots. inexpensive to produce.” for this procedure. R A D I O F R E Q U E N C Y A B L AT I O N T O T R E AT S I J O I N T PA I N Low back pain is a major clinical problem, with up to one-third of cases attributable to the SI joint. Over the past decade, RFA of the nerves supplying the SI joint has evolved as an effective treatment. Heat generated by radiofrequency electrical pulses is delivered through needles placed in the patient’s body to ablate, in a controlled fashion, the SI 8 equipment needs. The bipolar RFA approach used at Cleveland Clinic requires nerves that are conducting the pain. 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic Use of the template has shortened the procedure from 45 to about 15 minutes. “Once you determine the position of the template, you can almost automatically determine the right position for abdomen, which can be an uncomfortable position for those with SI joint pain. the needle electrodes, so you can place PAT E N T P E N D I N G them more precisely and more quickly,” :KHQ'U&KHQJÀUVWKDGWKHLGHDIRU says Dr. Cheng. Indeed, use of the tem- the template, he drew a diagram with evidence that there will be demand for Meanwhile, Dr. Cheng has informal plate has shortened the procedure from measurements, from which designers the template, which can be sterilized and 45 to about 15 minutes and allows just in Cleveland Clinic’s Department of Bio- reused. “We have 10 of the templates DFRXSOHRI;UD\H[SRVXUHVWRVXIÀFH medical Engineering created the model. for use in our practice,” he says. “Our instead of the continual X-ray exposures Dr. Cheng is now working with Cleve- attending physicians have found it an required in the past. land Clinic’s technology commercializa- easy-to-learn and very useful tool — and tion arm, Cleveland Clinic Innovations, all our graduating fellows want to keep on a patent application. Future research one when they leave.” With the template, even a less experienced clinician can complete the procedure in 20 minutes. The result: The patient spends less time lying on his or her will focus on medical device outcomes and comparative analyses of the four Dr. Cheng can be reached at RFA approaches. 216.445.9572 or chengj@ccf.org. 9 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) CAM Therapies for Chronic Pain: With Minimal Risk, There’s Little Reason Not to Try Them Early // FEATURING HONG SHEN, MD, and WILLIAM WELCHES, DO, PHD // It’s no secret: Patients with chronic pain will return to physicians again and again in search of an inWHUYHQWLRQWKDWFRPEDWVWKHLUSDLQDQGVLJQLÀFDQWO\LPSURYHVWKHLUIXQFWLRQLQJ$IWHUPXOWLSOHVWUDWHJLHV fail to provide that relief, more than a few patients and their providers will turn to complementary and alternative medicine (CAM) therapies. They’re not without reason to do so, Dr. Shen concurs. “With opioids, you studies demonstrate its effectiveness, DVHYLGHQFHVXSSRUWVWKHHIÀFDF\RI have to worry about addiction,” she says. Dr. Shen notes. The NIH’s National acupuncture, dietary changes and/or “With NSAIDs, you have to worry about Center for Complementary and Alterna- osteopathic manipulation therapy for cardiac, GI and kidney damage. With tive Medicine features the most rigorous many types of chronic pain. The ques- other medications, you have to worry VFLHQWLÀFÀQGLQJVRQLWV´*HWWKH)DFWVµ tion may be why so many patients about other side effects.” website (nccam.nih.gov/health/acupunc- and providers wait so long. ture/acupuncture-for-pain.htm). “Most of my patients have tried almost COMPLEMENT FOR MANY OVERCOMING SKEPTICISM — everything when they come to my of- A much safer alternative, she notes, is A N D M A N A G I N G E X P E C TAT I O N S ÀFHµREVHUYHV+RQJ6KHQ0'DSK\V acupuncture, which can relieve muscu- Dr. Shen initially was skeptical. “I was iatrist in Cleveland Clinic’s Department loskeletal pain, headaches, neck pain, trained in China, and I didn’t believe it. of Pain Management with an interest low back pain, myofascial pain and joint Stick a needle in someone to help their in CAM therapies. She’s one of sev- pain. For about 10 percent of patients, pain? Initially I used acupuncture to treat eral physicians in the department who Dr. Shen combines acupuncture with patients who failed all conventional treat- integrate a wide range of traditional and other therapies such as pain medication ments. I didn’t have any other options, alternative strategies, each employed or trigger point injections. so I tried acupuncture. Then I saw the appropriately to optimize the chances amazing results.” RIVLJQLÀFDQWUHOLHIIURPFKURQLFSDLQ Between 70 and 80 percent of patients report initial results good enough to Dr. Welches reports little reluctance Another such physician is William continue acupuncture, says Dr. Welches, among physicians. “It’s remarkable — Welches, DO, PhD, who encourages DFHUWLÀHGPHGLFDODFXSXQFWXULVW)RU even surgeons refer patients to me for that reason, acupuncture should be acupuncture. It’s widely accepted.” referring physicians to consider CAM strategies sooner to spare patients the tried fairly early in almost all patients adverse effects of some pain medica- with chronic pain, he adds. “There are tions. “It’s not that medications cannot no side effects, it’s easy to do and it’s be useful sometimes,” says Dr. Welches, relatively inexpensive compared with “but physicians are using them all the medicine and procedures.” time, and too often we fail to seriously investigate the alternatives.” 10 ACUPUNCTURE: A SAFE, EFFECTIVE Still, patients must have realistic expectations about insurance coverage — Dr. Shen estimates only about 25 percent of insurers in Ohio reimburse for acupuncture — and the number of treatment Not only is acupuncture safer than most sessions required. “Many people think other interventions, but more and more they can come for one or two sessions,” 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic she says, “but usually they need more than 10, based on the national studies.” Some patients require ongoing periodic treatment as well. A ROLE FOR DIET TOO The Department of Pain Management also offers dietary interventions and supplementation. “It amazes me that diet and exercise are considered complementary to mainstream medicine,” Dr. :HOFKHVVD\V+HFLWHVWKHDQWLLQÁDPPD tory diet — modeled after the Mediterranean diet and rich in vegetables, fruit and seafood — as an example. “I’m not sure how this got labeled as complementary. ,WKDVWKHDGGLWLRQDOEHQHÀWRIEHLQJWKH healthiest diet there is — the one we all should be following.” But Dr. Welches cautions that patient expectations are important here as well. “I tell my patients that the diet I’m putting them on is rigorous and a hard one to follow.” For some patients, Dr. Shen recommends nutritional supplements in conjunction with physical exercise, such as gluFRVDPLQHDQGÀVKRLOSURGXFWVWRWUHDW chronic osteoarthritis joint pain. O S T E O PAT H I C M A N I P U L AT I O N T H E R A P Y Dr. Welches also practices osteopathic manipulation therapy (OMT), which he says is about alignment, with muscles playing a central role. OMT aims to “open up” interconnected muscles, bones, nerves, blood and other systems as part of a holistic approach to treating the patient. OMT works by optimizing KRZRQHV\VWHPÁRZVLQWRDQRWKHUXQ encumbered by pain or misalignment. do up above — it’s not going to last,” It can be frustrating for patients, as they Dr. Welches says, citing the intercon- don’t always get the results they want. It nectedness of the musculoskeletal system is critical that we engage patients in their between the neck and lower back. own recovery. Usually we have to sit down In rare instances, Dr. Welches cannot recommend OMT because he cannot identify a musculoskeletal source of chronic pain. But about 99 percent of patients make appropriate candidates, he says. A PAT H T O E M P O W E R M E N T No matter what the intervention, patients with chronic pain need to make a daily commitment to lead a healthy lifestyle. “For instance, I start out evaluating a pa- “That’s the leading edge in pain manage- tient with neck pain by looking at the lower ment,” Dr. Welches observes. “We realize back,” he explains. “If the patient’s stance we’ve created a healthcare system that is cockeyed, it doesn’t matter what I encourages the patient to remain passive. with patients to explain what is required of them and what it is we are doing.” Dr. Welches sees patients at Cleveland Clinic’s Euclid and South Pointe hospitals; he can be reached at 216.692.8813 or welchew@ccf.org. Dr. Shen sees patients at Cleveland Clinic’s Lutheran Hospital and Westlake Medical Campus; she can be reached at 440.312.7246 or shenh@ccf.org. 11 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) Complications of Opioid Therapy: More to the Story than Abuse and Addiction // BY BENJAMIN ABRAHAM, MD // 2QHRIP\SDLQPHGLFLQHPHQWRUVRQFHVDLG´7KHÁLJKWWLPHDQGODQGLQJDUHDVLPSRUWDQWDVWKHWDNHRIIµ How true for opioid therapy. Too often, pain management specialists are seeing new patients who have DOUHDG\´WDNHQRIIµRQRSLRLGWKHUDS\ZLWKRXWDÁLJKWSODQ7KH\KDYHQRHVWDEOLVKHGJRDOVVRWKH\GRQ·W know how to determine if the therapy is working. They have no idea when the therapy should end or how they will “land.” Some have no understanding of the challenges they may encounter along the way. A M U LT I T U D E O F P O T E N T I A L E F F E C T S the dosage or discontinue opioid therapy Because these symptoms can be at- Of course, one of the biggest challenges when possible, such as for patients with WULEXWHGWRYDULRXVFDXVHVLW·VGLIÀFXOW with opioid therapy is risk of abuse nonmalignant pain. to pinpoint whether they are caused by and addiction. In the past decade, the $QGURJHQGHÀFLHQF\ One study of number of deaths from painkillers, including opioids, has quadrupled to nearly 15,000 per year in the United States. (See “Opioid Management: How WR+DUQHVVWKH%HQHÀWVZLWK)HZHURI the Harms” on page 8 of the 2012 issue of Pain Consult at clevelandclinic.org/ painconsult2012.) cancer survivors found that 90 percent of men taking opioids had hypogonadism, compared with 40 percent of those not taking opioids.1 But opioid-induced DQGURJHQGHÀFLHQF\23,$'LVDQLVVXH for both men and women. Symptoms include erectile dysfunction, reduced opioids and how soon they may follow opioid initiation. However, we know it can take about one month after stopping opioid use for testosterone and estrogen to reset and for changes such as weight gain and erectile dysfunction to begin to reverse. Reversing changes like reduced bone density may take longer. OLELGRIDWLJXHKRWÁDVKHVPHQVWUXDO If discontinuing opioid use is not pre- But abuse and addiction aren’t the only irregularities, low energy, weight gain ferred, treatment can include androgen concerns. Opioid therapy can cause other and depression. And OPIAD can lead replacement therapy, although androgen unwelcome side effects, some of which to more serious complications, such replacement in women sometimes brings are detailed below. as infertility and osteoporosis. other medical concerns. Immunosuppression. For more than a century, studies have shown opioids’ ability to weaken the immune system. OPIOID-INDUCED SIDE EFFECTS AND POTENTIAL TREATMENTS SIDE EFFECT POTENTIAL TREATMENT Immunosuppression Reduce opioid dose or discontinue $QGURJHQGHÀFLHQF\ Testosterone replacement therapy every opioid user. Constipation Stool softeners and laxatives; methylnaltrexone for severe cases With no tried-and-true method for Hyperalgesia Reduce opioid dose; rotate to methadone Depression Reduce opioid dose; antidepressants The function and activity of antibodies and T cells decrease immediately after exposure to opioids. While it may not EHFRPHFOLQLFDOO\VLJQLÀFDQWXQWLO\HDUV later, immune function declines in boosting immune function, the best way 12 to manage this side effect is to reduce 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic dose. Centers for Disease Control and Prevention data show that prescription opioids were involved in 14,800 overdose deaths in 2008 — more than the deaths from cocaine and heroin overdose combined. That’s why Cleveland Clinic’s Department of Pain Management prescribes opioids Constipation. Constipation can set in morphine and NMDA receptor antagonist quickly, after only a day or two of opioid that actually reverses opioid-induced use. Prevalence varies by study, from 15 hyperalgesia. Methadone brings its own to 90 percent of patients.2 Effects can challenges, however. Its dosage is dif- range from uncomfortable hemorrhoids ÀFXOWWRDGMXVWDQGLWFRPHVZLWKVLJQLÀ to life-threatening bowel obstruction. cant side effects, including risk of heart only when other treatments and analgesics have proven ineffective. At that time, we establish expectations and set goals for each patient and then actively monitor them. Post-discharge follow-ups are standard procedure. Together with refer- arrhythmia and respiratory depression. ring physicians and colleagues through- laxatives are effective management tools. Depression. Studies show that about side effects of opioid therapy before they For more severe cases, most often in 10 percent of patients using opioids cause major complications. patients with long-term opioid use, there develop some kind of depression. Again, is methylnaltrexone. This mu-opioid LWLVGLIÀFXOWWROLQNRSLRLGXVHGLUHFWO\WR Dr. Abraham, a specialist in the Depart- receptor antagonist acts locally in the GI this effect because depression can occur ment of Pain Management, sees patients tract, selectively reversing opioid-induced for other reasons. If a patient cannot be at Marymount Hospital and Elyria Fam- constipation without reversing pain relief. transitioned off opioids, antidepressants ily Health Center. His specialty interests Methylnaltrexone is administered as a are standard adjunctive therapy. include interventional pain manage- For the most part, stool softeners and subcutaneous injection in two doses. Once it relieves the severe constipation and removes bowel obstruction, the patient can resume using stool softeners C O M P L I C AT I O N S N O T L I M I T E D T O L O N G -T E R M U S E Notably, these conditions are not limited out Cleveland Clinic, we work to head off ment for back and neck pain, pain from failed back surgery, abdominal pain, vertebral compression fracture and peripheral neuropathy. He can be reached and laxatives. to patients with long-term opioid use or Hyperalgesia. Evidence of increased even those who have been using opioids pain resulting from opioid use has for a short time. Many effects begin to REFERENCES been observed since the 19th century. RFFXULPPHGLDWHO\³ZLWKLQÀYHPLQXWHV 1. Rajagopal A, Vassilopoulou-Sellin R, for some instances of hyperalgesia. And Palmer JL, Kaur G, Bruera E. Symptomatic symptom is relatively unstudied, partly they can occur even with properly man- hypogonadism in male survivors of cancer EHFDXVHSDLQLVGLIÀFXOWWRTXDQWLI\ aged therapeutic doses. In general, the way to manage opioid- The rate of drug overdose in the United induced hyperalgesia is to reduce the 2. Panchal SJ, Muller-Schwefe P, Wurzelmann States has more than tripled since 1990. JI. Opioid-induced bowel dysfunction: preva- dosage or rotate to another opioid, such Current estimates suggest that more than as methadone. Methadone is a synthetic 100 people per day die from drug over- However, the onset and severity of the overuse. They can occur in all patients, at 216.587.8830 or abrahab@ccf.org. with chronic exposure to opioids. Cancer. 2004;100:851-858. lence, pathophysiology and burden. Int J Clin Pract. 2007;61:1181-1187. 13 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) Research Snapshots 3URÀOHVRIQRWDEOHLQYHVWLJDWLRQVXQGHUZD\LQWKH'HSDUWPHQWRI3DLQ0DQDJHPHQW Cooled RFA: New Option for Painful Metastatic Bone Tumors A new radiofrequency ablation (RFA) technique uses a bipolar water-cooled Nagy Mekhail, MD, PhD analog scale as well as decreased dis- heating. Internal cooling eliminates the ability and improved function, with an 80 pain related to tissue charring that is common with con- percent improvement in Pain Disability metastatic bone ventional RFA. Transmission of RF waves Index score. Improvements were main- tumors when such ceases in charred tissue, limiting the size tained at two- and six-month follow-up. pain is unresponsive to conventional of the intervertebral lesion. The bipolar methods. Clinical experience with cooled tip on the OsteoCool device localizes RFA (OsteoCool® RF Ablation System) heating within cortical bone, eliminating at Cleveland Clinic shows local disease the need for a grounding pad and reduc- control, marked pain reduction and ing risk of damage to surrounding tissue. quality-of-life improvements from a single treatment, says Nagy Mekhail, MD, PhD. Up to 30 percent of patients with “The lesion created by water-cooled RFA is spherical and extends beyond the probe tip on both sides,” says Dr. Mekhail. “It metastatic bone tumors do not respond is eight times greater by volume than the to palliative measures involving radiation thermal RFA lesion produced by a similar- therapy, chemotherapy, surgical excision length probe. A large spherical lesion can or conventional RFA. Most RFA systems effectively ablate the metastatic tumor were designed for use in soft tissue, and the free nerve endings that are caus- employing a monopolar technology. They ing the pain.” do not perform consistently in bone because bone is not a good conductor of electrical energy and heat. The current from the single probe tip takes the path of least resistance to a grounding pad on the patient’s leg, explains Dr. Mekhail, The treatment is performed on an outpatient basis. Patients who have vertebral fracture as a tumor complication can undergo kyphoplasty in conjunction with cooled RFA. Enrollment in a study to test the Osteo&RROV\VWHP·VHIÀFDF\DQGVDIHW\LQ patients with spinal metastases will begin at Cleveland Clinic soon, says Dr. Mekhail. Precise Method of Spinal Cord Stimulation Promises Better Control of Lower Extremity Pain Though spinal cord stimulation has been used to treat chronic pain since the 1970s, it often fails to control lower Samuel Samuel, MD extremity pain because of the dif- ÀFXOW\RIWDUJHWLQJWKHVSHFLÀFDQDWRPLF sites involved. Dorsal root ganglion (DRG) stimulation is emerging as an option with the ability to more precisely stimulate ana- Director of Evidence-Based Medicine in To date, 11 patients have been treated the Department of Pain Management. tomic targets implicated in chronic pain with the OsteoCool system at Cleveland — even in the lower extremities. So says “Ideally, we’d like to produce a big lesion by burning the tumor and the surrounding trabecular bone,” he says. “Ablating WKHIUHHQHUYHÀEHUVFDQDOOHYLDWHSDLQ caused by vertebral body metastases.” Current RFA systems produce lesions 14 ance, increasing the radius of effective RFA probe to treat Clinic and the University of Washington Samuel Samuel, MD, a pain specialist in Seattle. Three patients who presented leading a study of DRG stimulation in with severe low back pain despite opioid the Department of Pain Management. therapy — two with metastatic breast cancer to the L3 vertebral body, and one with vertebral metastasis secondary to prostate cancer — have been treated FRQÀQHGWRWKHDFWLYHWLS$QLQWHUQDOO\ at Cleveland Clinic. All achieved a 75 cooled RFA probe lowers tissue imped- percent reduction in pain on the visual Patients with lower extremity pain, such as neuropathy or postlaminectomy syndrome (failed back surgery syndrome), appear to be the best candidates for DRG stimulation, which has been in clinical 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic use in Europe for the past few years. pain with or without back pain in the The current DoD study in rats is testing Single-center pilot studies and case stud- multicenter clinical trial. The principal safety, analgesic effects and anti-toler- ies have been conducted in the United investigators at Cleveland Clinic are Dr. ance effects, as well as the longevity and States, in preparation for a multicenter Samuel and Nagy Mekhail, MD, PhD. stability of the cells once transplanted. trial for which Cleveland Clinic is enroll- To refer a patient for enrollment, call ing patients. 216.636.0103. The DRG is located within the spinal Analgesic Cell Therapy Could Be a Game-Changer in Chronic Pain foramen and contains cell bodies of the primary neurons. “We are just beginning to understand the DRG’s function pain signal,” says Dr. Samuel. “The DRG receives information from the extremities or the trunk and conveys it to the brain, complex structure.” Discrete stimulation of one side or one level of the spinal column is sometimes hard to achieve with conventional spinal patients with intractable neuropathic pain, patients with cancer pain could someday land Clinic could If the stem cell therapy is found to be way chronic pain Jianguo Cheng, MD, PhD promise,” says Dr. Cheng. In addition to be good candidates for this therapy. cally change the diminishes the pain signal depending can be tested in humans, initial results from animal studies have shown great underway at Clevesomeday dramati- DFWLQJDVDJDWHNHHSHU,WPDJQLÀHVRU on the information it gets. It’s a highly over many years before this approach Stem cell research and its mechanism for modulating the “While many more studies are needed is treated and decrease the potential for prescription drug abuse. The research is in the early stages of testing whether mesenchymal stem cells, after safe and effective, potential advantages include: • Therapeutic alternative — This approach promises the ability to treat intractable neuropathic pain in patients who don’t respond to prescription opioids. • Fewer side effects — Patients who opt cord stimulation, which may explain being harvested from a patient’s bone mar- for analgesic cell therapy could avoid the some treatment failures with convention- URZDQGUHSURJUDPPHGLQWRFKURPDIÀQ side effects of exogenous opioids, such al stimulation. Preferentially targeting the primary sensory neurons responsible for like cells, can provide relief from chronic as respiratory depression, immunocom- intractable pain when they are transplanted promise, disruption or depression of en- chronic pain in the lower extremities — back into the same patient. which DRG stimulation makes possible The endogenous opioids that are gener- — can improve the outcomes obtained DWHGIURPWKHVHGLIIHUHQWLDWHGFKURPDIÀQ docrine functions, constipation, vomiting and itching. • Decreased abuse — Endogenous with neuromodulation. like cells have powerful analgesic effects. “For instance, we can precisely stimulate In fact, they have the potential to treat as an alternative to highly addictive nerve injury-induced pain that usually prescription opioids, which cause more doesn’t respond to exogenous opioids deaths than car accidents and are often such as morphine and its derivatives, diverted for illegal use. the left thigh or the right foot if needed,” explains Dr. Samuel. “The advantage is the ability to stimulate one or two levels of the spinal column, and one or both sides.” Candidates for DRG stimulation undergo a trial stimulation period of up to two weeks. If they experience 50 percent or greater improvement in pain, electrical leads and contacts are placed permanently using a minimally invasive epidural approach, and the leads are attached according to Jianguo Cheng, MD, PhD, principal investigator of the Department of Defense (DoD)-funded study and Professor and Director of Cleveland Clinic’s embryonic stem cells, once the mesenchymal stem cells are differentiated into FKURPDIÀQOLNHFHOOVWKH\FDQ·WJURZRU divide, so tumor risk is not an issue. Dr. Cheng and his collaborator, Tingyu If found to be viable, analgesic cell Qu, MD, PhD, from the University of Illinois at Chicago, developed the patentpending technology to differentiate the performed on an outpatient basis. DXWRORJRXVVWHPFHOOVLQWRFKURPDIÀQOLNH patients with chronic intractable leg • Reprogrammed stem cells — Unlike Pain Medicine Fellowship Program. to a neurostimulator. The procedure is Cleveland Clinic seeks to enroll 20 opioids from analgesic cell therapy serve cells. Initial animal studies have already demonstrated the feasibility of transplanting the cells for pain relief. therapy has the potential to be a gamechanger. As stated in the DoD’s assessment of the grant application, “This approach to pain management is very innovative and, if successful, could have a tremendous impact on the way that chronic pain is treated.” 15 Cleveland Clinic Pain Consult | 2013 216.444.PAIN (7246) Ongoing Pain Management Trials: Is Your Patient a Candidate? Cleveland Clinic’s Department of Pain Management is enrolling patients in a range of ongoing clinical studies. To refer a patient for possible enrollment, call 216.636.0103. C U R R E N T C L I N I C A L T R I A L S I N T H E D E PA R T M E N T O F PA I N M A N A G E M E N T Study Name PI Key Inclusion Criteria* Major Exclusion Criteria* Controlled, Two-Arm, Parallel-Group, Randomized Withdrawal Study to Assess the Safety and (IÀFDF\RI+\GURPRU phone HCl Delivered by Intrathecal Administration Using a Programmable Implantable Pump Nagy Mekhail, MD, PhD • Age 18-75 • History of dependence on opiates, stimulants, alcohol or benzodiazepines in prior year Prospective, Randomized, Multicenter, Controlled Clinical Trial to Assess WKH6DIHW\DQG(IÀFDF\ of the Spinal Modulation Axium™ Neurostimulator System in the Treatment of Chronic Pain (ACCURATE Trial) Samuel Samuel, MD, and Nagy Mekhail, MD, PhD &OLQLFDOGLDJQRVLVRIFKURQLFSDLQIRUPR • Presently on intrathecal pain medication and has or is eligible for SynchroMed® II pump implantation • Metastatic cancer to spinal canal or known CNS contraindication to intrathecal therapy • Active implanted device that would interfere with intrathecal pump • Pain in head/neck region, central pain synGURPHVRUDQ\RWKHUSDLQXQOLNHO\WREHQHÀW from intrathecal administration • Age 22-75 • Chronic intractable pain of lower extremity for PR • Diagnosis of failed back surgery syndrome, complex regional pain syndrome or peripheral neuropathy • Any of the following in past 30 days: escalating or changing pain condition, corticosteroid therapy at intended stimulation site, unstable pain med dosages • Previous failure of spinal cord stimulation • Minimum average VAS > 60 mm in lower extremity • Pain only within a cervical distribution • Inadequate pain relief from at least two drugs from different classes • Active implantable device, other indwelling device, or need for MRI or diathermy • Stable neurologic function for past 30 days • Coagulation disorder • Radiofrequency treatment within past 3 mo • Cancer diagnosis in past 2 yr Prospective, Multicenter, Randomized, DoubleBlinded, Partial Crossover Study to Assess the 6DIHW\DQG(IÀFDF\RI the Bioness® Stimulator Neuromodulation System in Treatment for Patients with Chronic Pain of Peripheral Nerve Origin Nagy Mekhail, MD, PhD Phase 4 Multicenter, Open-Label Pilot Study of Pregabalin and Prediction of Treatment Response in Patients with Postherpetic Neuralgia Daniel Leizman, MD $JH • Severe intractable chronic pain of peripheral nerve origin associated with post-traumatic/postsurgical QHXUDOJLDIRUPR • Ability to tolerate skin surface stimulation (TENS) :RUVWFKURQLFSDLQOHYHOLQSULRUKRXUV on NRS for Pain • Implanted demand-type cardiac pacemaker/ GHÀEULOODWRURURWKHUPHWDOLPSODQWLQDUHDRI planned implantation • Bleeding disorder or active anticoagulation that cannot be stopped for a few days for implantation 7UHDWPHQWZLWKVWDEOHGRVHRISDLQPHGVIRU wk before screening and ability to maintain dosage from randomization to 3-mo follow-up $JH • Pain for > 3 mo after healing of herpes zoster skin rash • Other severe pain that may confound assessment of postherpetic neuralgia (PHN) pain • Neurolytic or neurosurgical therapy for PHN 6FRUHRQ156IRU3DLQDWVFUHHQLQJDQG baseline • Failure or intolerance of pregabalin or gabapentin therapy • Completion of at least four pain diaries within past GD\VZLWKDYHUDJHSDLQVFRUH • Any clinically unstable cardiovascular, hematologic, autoimmune, endocrine, renal, hepatic, retinal or GI disease • Malignancy in past 5 yr Functional Capacity Evaluation of Patients Undergoing Lumbar Spinal Cord Stimulation Therapy 16 Daniel Leizman, MD $JH • Diagnosis of chronic back pain with radicular lower limb pain extension and successful completion of a spinal cord stimulator trial *Complete inclusion and exclusion criteria to be covered at time of referral. Pregnancy, breastfeeding and potential to become pregnant are exclusion criteria for most of these trials. 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic &OHYHODQG&OLQLF·V3DLQ0DQDJHPHQW6\PSRVLXP Heads to Las Vegas in February 2014 More than 250 physicians and other providers from 40 states and 12 nations brought themselves up to date on the full spectrum of pain medicine at Cleveland Clinic’s 15th Annual Pain Management Symposium, held in Sarasota, Fla., this past February. Now course organizers are busy planning decisions,” says Richard Rosenquist, While many attendees are specialists for the 16th Annual Pain Management MD, Chairman of Cleveland Clinic’s in anesthesiology or pain management, Symposium, to be held Feb. 15-19, Department of Pain Management and attendees this year came from nearly one of the faculty members for the 20 different specialties, with sizable 2013 symposium. contingents from rehabilitation medicine, 2014, at Caesars Palace in Las Vegas. 7KHFRPSUHKHQVLYHÀYHGD\FRXUVH internal medicine and family practice. provides in-depth reviews and analyses Content is presented by approximately of most major aspects of contemporary 40 renowned experts in pain manage- pain medicine. This year’s topic catego- ment. About half the faculty comes from ries ranged from emerging technologies Cleveland Clinic and half from other to controversies in pain medicine and leading U.S. and international medi- ment Symposium to learn about the from evidence-based spine pain care to cal centers. The 2013 faculty included latest advances in pain medicine and risk management in pain medicine. Ad- experts from Sweden and the United how healthcare reform is changing our ditional program sections were devoted Kingdom. The agenda is a diverse mix of practices,” advises Dr. Rosenquist. to imaging techniques and updates on traditional lectures with problem-based headache management. learning discussions, cadaver workshops For 2014 symposium details and regis- on novel interventional techniques, and tration info, email cmeregistration@ live-model workshops for training in ccf.org or visit ccfcme.org/pain14. “This course tackles provocative issues in pain medicine and challenges attendees to examine the basis for their medical The course is designated for CME credit for physicians and CE credit for nurses. “Plan to attend the 2014 Pain Manage- ultrasonography-guided injections and peripheral nerve blocks. 17 Pain Consult | 2013 Cleveland Clinic 216.444.PAIN (7246) Department of Pain Management at a Glance 30 Physicians 127,303 Patient visits (2012) 20 42,394 Locations in NE Ohio Procedures (2012) And we act fast when needed: 37% of our 2012 procedures were acute. A N E D U C AT I O N P O W E R H O U S E 10 30-40 Fellows per year Residents per year Launched optional two-year pain medicine fellowship in 2012 A RESOURCE FOR RESE ARCH $1.13 million in Department of Defense research funding in 2012, and $150,000 internal funding for research S O U G H T O U T F R O M A FA R 932 patients in 2012 came from out of state or out of the country FILLING THE CARE G AP IN THE WAKE OF 2012 “ PILL MILL BILL” 2012 saw a 15% surge in our new-patient volume after passage of Ohio HB93, which tightened standards for operation of pain clinics and opioid distribution. Scores of Ohio providers stopped prescribing opioids, so many of their patients on opioids turned to Cleveland Clinic. Department of Pain Management staff met with these patients to optimize their care plans. REGIONAL GROW TH SPURT 18 Clinic expansions are underway in 2013 for our locations at main campus and Fairview Hospital. The volume of our Regional Pain Management practice continues to grow: • 74,408 total visits in 2010 • 75,865 in 2011 • 81,529 in 2012 2013 | Pain Consult clevelandclinic.org/painmanagement Cleveland Clinic New Staff The Department of Pain Management welcomes new specialists: Daniel Callahan, MD Adam Kramer, MD Specialty interests: Interventional pain management (injection therapy, medication management), electromyography, autonomic disorders Specialty interests: Spine pain, complex regional pain syndrome, chronic pain in athletes, abdominal pain, headaches Location: South Pointe Hospital 216.491.6433 callahd@ccf.org Location: Medina Hospital 330.721.5700 kramera@ccf.org Our pain management specialists are available at 20 locations across Northeast Ohio. For a complete list of physicians and their locations, visit clevelandclinic.org /painmanagement. Same-Day Appointments Cleveland Clinic now offers same-day appointments to help your patients get the care they need, right away. If patients call our same-day appointment line, 216.444.CARE (2273), they can be seen, in most cases, by a physician that day. When patients call before noon, we’ll offer them a same-day appointment; when they call after noon, we’ll offer an appointment for the next day. 5HFHLYH7KLV1HZVOHWWHU Electronically Want to receive future issues of Pain Consult electronically? Just log on to clevelandclinic.org /chronicpainnews to receive future issues in your email inbox. DEPARTMENT OF PAIN MANAGEMENT CHAIRMAN Richard W. Rosenquist, MD M A N A G ING EDITO R Glenn Campbell ART DIRECTOR Michael Viars MARKETING MANAGER Laura Vasile P H O TO G RAPH Y Cleveland Clinic Center for Medical Art & Photography 19 The Cleveland Clinic Foundation 9500 Euclid Ave./AC311 Cleveland, OH 44195 RESOURCES FOR PHYSICIANS Referring Physician Hotline 855.REFER.123 (855.733.3712) Hospital Transfers 800.553.5056 On the Web at:FOHYHODQGFOLQLFRUJUHIHU 6WD\FRQQHFWHGZLWKXVRQ« $ERXW&OHYHODQG&OLQLF Referring Physician Center and Hotline Cleveland Clinic’s Referring Physician Center has established a 24/7 hotline — 855.REFER.123 (855.733.3712) — to streamline access to our array of medical services. Contact the Referring Physician Hotline for information on our cliniFDOVSHFLDOWLHVDQGVHUYLFHVWRVFKHGXOHDQGFRQÀUPSDWLHQW appointments, for assistance in resolving service-related issues, and to connect with Cleveland Clinic specialists. Physician Directory View all Cleveland Clinic staff online at clevelandclinic.org /staff. Track Your Patient’s Care Online DrConnect is a secure online service providing realtime information about the treatment your patients receive at Cleveland Clinic. Establish a DrConnect account at clevelandclinic.org/drconnect. Critical Care Transport Worldwide &OHYHODQG&OLQLF·VFULWLFDOFDUHWUDQVSRUWWHDPVDQGÁHHW of vehicles are available to serve patients across the globe. Cleveland Clinic is an integrated healthcare delivery system with local, national and international reach. At Cleveland Clinic, more than 3,000 physicians and researchers represent 120 medical specialties and subVSHFLDOWLHV:HDUHDQRQSURÀWDFDGHPLFPHGLFDOFHQWHU with a main campus, eight community hospitals, more than 75 northern Ohio outpatient locations (including 16 full-service family health centers), Cleveland Clinic Florida, Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas, Cleveland Clinic Canada, Sheikh Khalifa Medical City and Cleveland Clinic Abu Dhabi. • To arrange for a critical care transfer, call 216.448.7000 or 866.547.1467 (see clevelandclinic.org /criticalcaretransport). In 2013, Cleveland Clinic was ranked one of America’s top 4 hospitals in U.S. News & World Report’s “America’s Best Hospitals” survey. The survey ranks Cleveland Clinic among the nation’s top 10 hospitals in 14 specialty areas, and the top in heart care for the 19th consecutive year. Clinical Trials We offer thousands of clinical trials for qualifying patients. Visit clevelandclinic.org /clinicaltrials. • For STEMI (ST elevated myocardial infarction), acute stroke, ICH (intracerebral hemorrhage), SAH (subarachnoid hemorrhage) or aortic syndrome transfers, call 877.379.CODE (2633). Outcomes Data View clinical Outcomes books from all Cleveland Clinic institutes at clevelandclinic.org /outcomes. CME Opportunities: Live and Online The Cleveland Clinic Center for Continuing Education’s website offers convenient, complimentary learning opportunities. Visit ccfcme.org to learn more, and use Cleveland Clinic’s myCME portal (available on the site) to manage your CME credits. Executive Education Cleveland Clinic has two education programs for healthcare executive leaders — the Executive Visitors’ Program and the two-week Samson Global Leadership Academy immersion program. Visit clevelandclinic.org /executiveeducation. 13-PAI-127 24/7 Referrals