SURVEY OF OPHTHALMOLOGY
VOLUME 54 NUMBER 4 JULY–AUGUST 2009
DIAGNOSTIC AND SURGICAL
TECHNIQUES
MARCO ZARBIN AND DAVID CHU, EDITORS
Mitomycin C in Corneal Refractive Surgery
Miguel A. Teus, MD, PhD,1,2 Laura de Benito-Llopis, MD, PhD,1
and Jorge L. Alió, MD, PhD3,4
1
Vissum Madrid, Madrid, Spain; 2Universidad de Alcalá, Madrid, Spain; 3Vissum Alicante, Alicante, Spain;
and 4Universidad Miguel Hernández, Alicante, Spain
Abstract. Mitomycin C has played a deciding role in the current revival of excimer laser surface
ablation techniques. We review the literature regarding mechanism of action of mitomycin C,
histological effects on the cornea, and indications, dose, exposure time, and toxicity of mitomycin C in
corneal refractive surgery. Mitomycin C is an alkylating agent with cytotoxic and antiproliferative effects
that reduces the myofibroblast repopulation after laser surface ablation and, therefore, reduces the risk
of postoperative corneal haze. It is used prophylactically to avoid haze after primary surface ablation
and therapeutically to treat pre-existing haze. There is no definite evidence that establishes an exact
diopter limit or ablation depth at which to apply prophylactic mitomycin C. It is usually applied at
a concentration of 0.2 mg/ml (0.02%) for 12 to 120 seconds over the ablated stroma, although some
studies suggest that lower concentrations (0.01%, 0.002%) could also be effective in preventing haze
when treating low to moderate myopia. This dose of mitomycin C has not been associated with any
clinically relevant epithelial corneal toxicity. Its effect on the endothelium is more controversial: two
studies report a decrease in endothelial cell density, but the majority of reports suggest that the
endothelium is not altered. Regarding mitomycin C’s effect on keratocyte population, although animal
studies report keratocyte depletion after its use, longer follow-up suggested that the initial keratocyte
depletion does not persist over time. (Surv Ophthalmol 54:487--502, 2009. Ó 2009 Elsevier Inc. All
rights reserved.)
Key words. advanced surface ablation excimer laser surface ablation haze laser-assisted
subepithelial keratectomy mitomycin LASEK laser subepithelial keratomileusis mitomycin C MMC photorefractive keratectomy
Laser in situ keratomileusis (LASIK) has become the
most popular corneal refractive surgery procedure
because it provides a rapid postoperative recovery
and less discomfort when compared to photorefractive keratectomy (PRK). Nevertheless, the
possibility of sight-threatening complications associated with the stromal flap in LASIK, and the
development of new surface ablation procedures,
has led to a renewed interest in these techniques.
Surface ablation has become the technique of
choice in patients with thin corneal pachymetry,
those at risk for trauma, and those with corneal
surface problems such as dry eye, recurrent erosion
syndrome, or basement membrane disease,108,153
487
Ó 2009 by Elsevier Inc.
All rights reserved.
0039-6257/09/$--see front matter
doi:10.1016/j.survophthal.2009.04.002
488
Surv Ophthalmol 54 (4) July--August 2009
and it has shown to be safe, effective, and predictable for treating low,29 moderate,154 and high
myopia.32,151
Mitomycin C (MMC) has played a decisive role in
the current revival of surface ablation techniques.
The main complication associated with laser surface
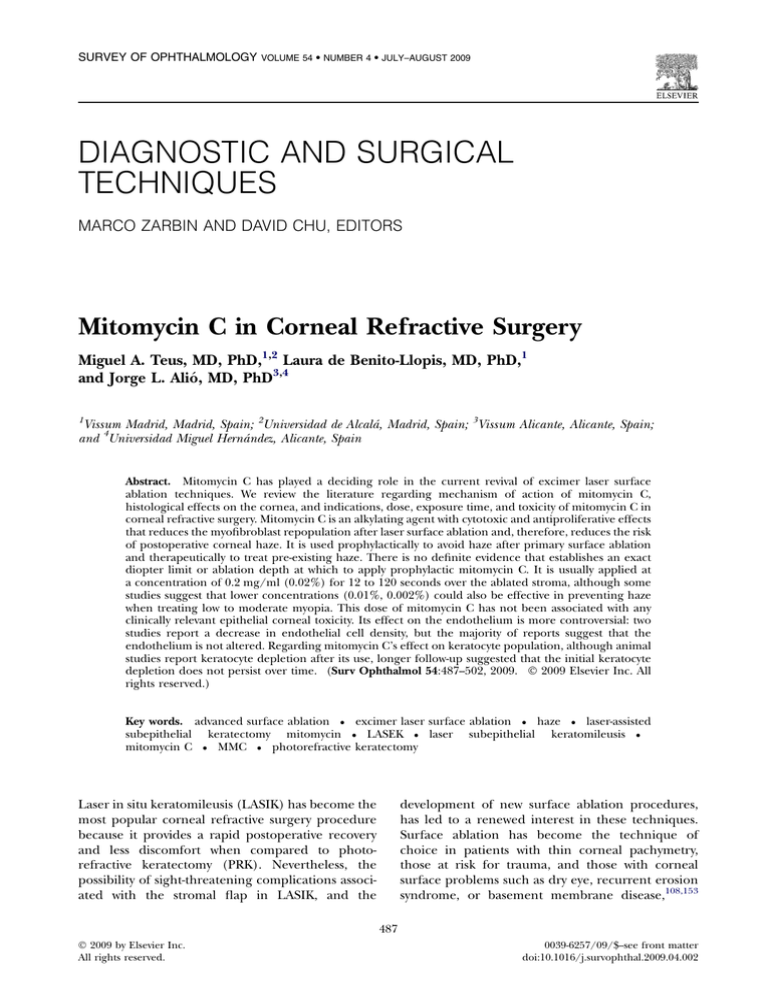
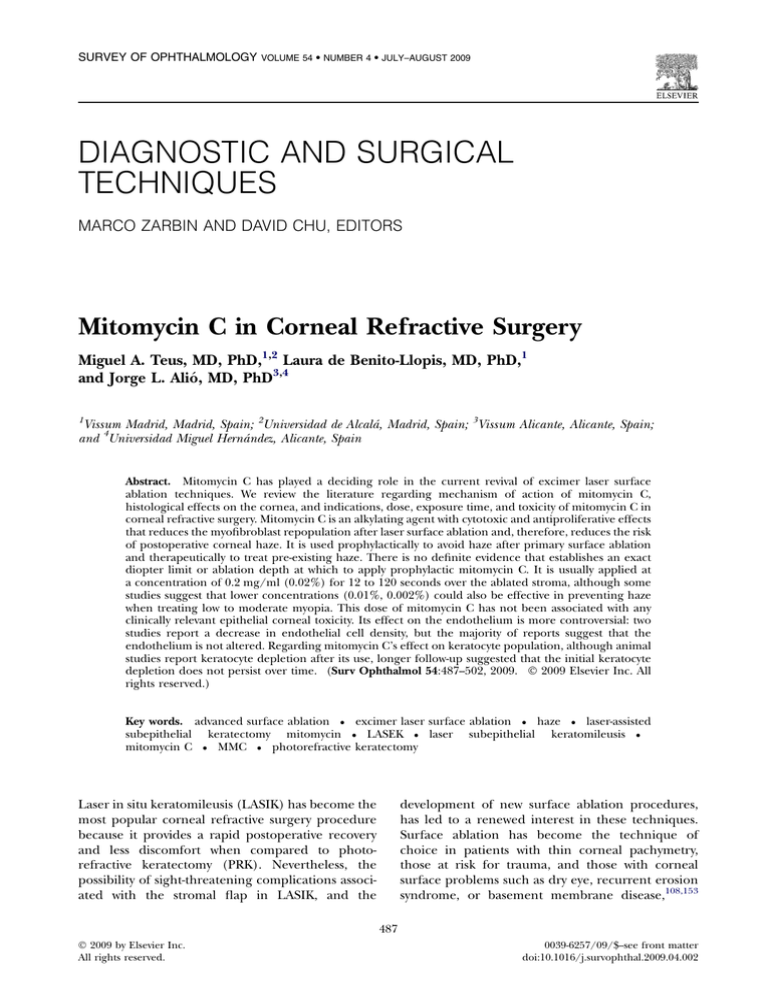
ablation was the loss of corneal transparency—corneal haze—that appeared most frequently associated with deep ablations (Fig. 1).83,96 The efficacy of
the MMC in reducing the incidence of this
complication has led to its widespread use in most
refractive surgery practices. Nevertheless, the mechanism of action of this drug, the optimal dose and
exposure time, the visual and refractive results of
surface ablation techniques using MMC, and the
possible toxicity of this drug remain subjects of
intense debate.
MECHANISM OF ACTION
Mitomycin C was first isolated from cultures of
Streptomyces caespitosus by Hata in 1956.16,139 It acts as
a genotoxic antibiotic because of its alkylating
action: once it becomes activated by enzymes such
as the cytochrome p450 reductase,10,24,26,164 it produces cross-linking of the DNA molecules between
adenine and guanine, thereby blocking DNA
synthesis and secondarily inhibiting cell mitosis,
causing cell cycle arrest.56,94 Although it acts
primarily during the late G1 and S phases, it is
non-cell cycle specific. As a result of its antimitotic
effect, cells with a higher mitotic rate are more
sensitive to its action, and it is widely used
systemically as a chemotherapeutic agent.125,161
Nevertheless, some of the effects of MMC cannot
be explained simply by this antiproliferative mechanism. MMC shows a cytotoxic effect that is not
completely justified by its capacity to bind DNA.127
Fig. 1. Subepithelial corneal haze 3 months after surface
ablation. The arrow points to the corneal haze.
TEUS ET AL
The mechanisms for its cytotoxicity have not been
completely clarified. Many studies have analyzed the
cellular mechanisms activated by MMC that could
explain its cytotoxicity: it produces up-regulation of
the expression of cytokines such as IL-8 and monocyte chemoattractant protein-1 (MCP-1) by the
activation of protein kinases,23 induction of Fasmediated apoptosis24,135 and also apoptosis through
the activation of caspase cascades with mitochondrial dysfunction,70,135 T lymphocytes mediated cell
lysis,25 depletion of intracellular glutathione,48
generation of reactive oxygen radicals,121 and
secondary amplification of the production of tumor
necrosis factor (TNF).119
Another point of debate is the possible long-term
cellular effects of this drug. It is not clear whether
cells repair the DNA damage caused by the MMC81
or whether its effects are permanent. Some studies
with fibroblasts cultures suggest that these cells do
not suffer a permanent inhibition after a single
exposure to MMC114 and that the adjacent nonexposed cells can replace them.27,63
DRUG EFFECTS ON THE CORNEA
Corneal haze is caused by the mechanisms of
corneal wound healing that become activated after
surface ablation and that are different from the
wound healing process observed after LASIK. Epithelial damage and the secondary epithelial-stromal
interaction seem to cause these differences.7,124
During surface ablation, both the deepithelialization
and the laser ablation incite keratocyte apoptosis,36
which is followed by proliferation and migration of
the surrounding keratocytes to repopulate the denuded stroma.124 In response to epithelial derived
cytokines, especially TGFb,58 some keratocytes differentiate into myofibroblasts.36 These cells are the
base of corneal haze, as they scatter more light than
quiescent keratocytes, not only from their nuclei, but
also from their cell bodies and dendritic processes.28,97,98 In addition, they participate in extracellular matrix remodelling, resulting in a denser
and more disorganized extracellular matrix, with
abundant collagen type III, which contributes to the
loss of corneal transparency28,59,97,98 (Figs. 2 and 3).
These stromal healing mechanisms lead to the
formation of a fibrotic and hypercellular scar in the
anterior stroma.28
MMC is useful in laser surface ablation because of
its capacity to interfere with this stromal wound
healing process. MMC is usually applied over the deepithelialized stroma after the laser ablation has
been performed. Animal studies have shown, within
the first hours after its application, a higher rate of
keratocyte apoptosis,144 followed 24 hours after-
489
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
Fig. 2. Confocal microscope image of keratocytes. The
arrows point to the nuclei of the keratocytes; their cell
bodies and dendritic processes are barely seen.
wards by a reduced keratocyte repopulation. Four
weeks later, there is a lower keratocyte and
myofibroblast density and less deposit of collagen
and extracellular matrix, compared to untreated
eyes.70,76,107 These effects in the corneal stroma
result in increased corneal transparency after
surface ablation in animal models. 67,68,167 In
human corneas maintained in vitro, Rajan et al123
also detected a lower keratocyte proliferation after
MMC application, although they did not observe the
initial increase in keratocyte apoptosis.
The initial increase in keratocyte apoptosis is
related to the cytotoxic effect of the MMC, whereas
the antimitotic effect of this drug is responsible for
blocking keratocyte activation and differentiation
into myofibroblasts. This latter mechanism seems
more effective than cytotoxic elimination of the
already differentiated myofibroblasts, as Netto et al
demonstrated in rabbit corneas.107 Sadeghi et al130
had already shown that the concentration of MMC
needed in vitro to achieve its antiproliferative effect
was lower than that to cause cytotoxicity. In fact,
MMC seems more effective as a prophylactic agent,
to prevent haze, than as a therapeutic agent to
eliminate pre-existing haze.86,105 Nevertheless, no
consensus has been reached, and some authors
consider the antimitotic activity the more important
mechanism of action,86,107 while others support that
the cytotoxic effect.143,144
FIRST USES OF MMC IN CORNEAL REFRACTIVE
SURGERY
The first studies of MMC in surface ablation were
performed in animals. Talamo et al150 suggested in
1991 the use of postoperative MMC to modulate the
corneal wound-healing response to surface ablation.
They showed that the application of topical MMC in
rabbit corneas during the 2 weeks after surgery
resulted in less subepithelial collagen deposition.
Schipper et al132 observed that intraoperative 0.04%
MMC for 5 minutes after surface ablation in rabbits
resulted in less scar tissue and lower keratocyte
density.
Majmudar et al85 pioneered its use to treat corneal
scars secondary to refractive procedures. They
applied 0.02% MMC intraoperatively for 2 minutes
and found a clinically significant improvement in
corneal transparency. It was subsequently proposed
as a prophylactic agent to prevent haze formation
after primary surface ablation. Carones et al15 (Table
1) applied MMC after surface ablation to correct
myopia from --6.00 to --10.00 D. They reported less
haze and better predictability of visual results in the
group that received intraoperative MMC compared
to the control group, with no side effects.
Uses of MMC in Corneal Refractive
Surgery
USE OF MMC TO TREAT CORNEAL HAZE
Fig. 3. Confocal microscope image of corneal stroma
with haze after surface ablation. The arrows point to the
nuclei of the myofibroblasts; these cells scatter more light
than quiescent keratocytes, and not only from their nuclei
but also from their cell bodies and dendritic processes.
Intraoperative MMC, along with scraping of the
corneal surface, has shown to be effective in
increasing the transparency of corneas with haze
following previous refractive surgery procedures.85
490
Clinical Studies Comparing Eyes Treated with Surface Ablation without Mitomycin C versus Eyes Treated with Surface Ablation with Intraoperative Mitomycin C
Manuscript
Type
Preop Spherical
Equivalent
(diopters)
MMC
Dose
(%)
MMC
Application
Time
Follow-up
(months)
75 sec
6
Authors
Number
of Eyes
Argento
et al4
30 MMC 28
controls
Retrospective,
comparative
study
MMC:
--5.72 2.82
controls:
--5.81 2.74
0.02
Bedei
et al8
62 MMC 62
controls
O--5.00
0.02
Carones
et al15
30 MMC
30
controls
Prospective,
randomized,
comparative
study
Prospective,
randomized,
comparative
study
MMC:
--7.75 0.86
controls:
--7.79 0.87
(p 5 0.82)
0.02
2 min
Gambato
et al42
36 MMC 36
controls
Prospective,
randomized,
comparative
study
MMC:
--9.40 1.74
controls:
--8.71 1.67
(p 5 0.03)
0.02
2 min
12
6
Mean:18
(range 12-36)
Refractive
Results
Haze
Visual Results
MMC-group: 0%
controls: trace
17.9%, grade 1:
3.6%
(p ! 0.001)
Less haze in
MMC-group
(p 5 0.005)
Efficacy index:
MMC: 0.954
controls: 0.909
(p ! 0.01)
No significant
difference
Better BCVA in
MMC-group
(p 5 0.013)
Haze grade $1:
MMC: 0%
controls: 63%
(p 5 0.01)
Better UCVA
(p # 0.01)
and BCVA
(p # 0.001) in
MMC-group.
Loss of 1-3 lines
of BCVA: MMC:
0% controls:
23.3%
(p 5 0.0006)
UCVA (logMAR):
MMC:
0.4 0.48
controls:
0.5 0.53
(p 5 0.03)
eyes 0.50 D:
MMC: 69.3%
controls:
50%
eyes 0.50D:
MMC: 87%
controls:
47%
Haze grade $1:
MMC: 0%
controls: 20%
Surv Ophthalmol 54 (4) July--August 2009
TABLE 1
No significant
difference
BCVA 5 best-corrected visual acuity; MMC 5 mitomycin C; UCVA 5 uncorrected visual acuity.
TEUS ET AL
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
491
In contrast with the trend to shorten exposure time
and lower dosage when MMC is used prophylactically in primary surface ablation, therapeutic MMC
is generally still applied at the same concentration
(0.02%) and for the same duration (2 minutes) as in
those first studies.120,162 The cytotoxic effect to
produce apoptosis of pre-existing myofibroblasts
seems lower than MMC’s capacity to prevent their
appearance when applied prophylactically. Netto et
al107 showed that 4 weeks after application of 0.02%
MMC for 2 minutes to treat pre-existing haze in
rabbit corneas, myofibroblats could still be detected.
These cells tended to disappear progressively during
the first 6 months after surgery.
The use of MMC in thin corneas (thinner than
500 mm) has been the subject of only one study31 in
which intraoperative MMC did not seem to increase
the risk of postoperative corneal instability with
a follow-up of 15 months. More studies with longer
follow-up are needed to further elucidate the safety
of MMC in thin corneas.
USE OF MMC IN PRIMARY SURFACE ABLATION
PROCEDURES
Several comparative studies have reported less
incidence of haze, and better visual and refractive
outcomes, when using intraoperative MMC during
surface ablation procedures in moderate and high
myopia4,8,42,80 (Table 1). The corneal wound-healing response to laser surface ablation is directly
related to ablation depth.83,96 This was initially the
main limitation for PRK, since treating high refractive defects was associated with a stromal response that caused significant haze and refractive
regression,71 resulting in poorer outcomes as
compared to LASIK.66 The introduction of MMC
has improved the outcomes of surface ablation in
high myopia.4,15,42 A comparison between 114 eyes
treated with laser-assisted subepithelial keratectomy
(LASEK) and 0.02% MMC for 60 seconds and 114
refractive-matched eyes treated with LASIK to
correct a myopic defect of --7.00 D or greater
showed no difference between techniques regarding
safety and efficacy and in UCVA or BSCVA 3 months
after surgery. A trend toward overcorrection was
detected in the LASEK with MMC group, despite the
planned undercorrection of 10%.32
The wound-healing response to the laser ablation
seems to be one of the causes of refractive
regression.71,97 Because the MMC reduces that
response, it causes a tendency to overcorrection
that needs to be compensated for with an appropriate adjustment of the laser nomogram.12,75,79
Although each surgeon should define their own
adjustment based on his/her results, it is advisable
to perform an undercorrection of about 10% of the
preoperative spherical refraction, sometimes higher
depending on patient age and preoperative refractive defect (Carones et al: 10%15; Lacayo et al: 8-15%75; Camellin: 20% in low myopia12; our group:
10% 32). Usually, the cylinder programmed ablation
does not need to be modified.4,75
USE OF MMC IN ADVANCED SURFACE ABLATION
PROCEDURES
The sight-threatening complications associated
with LASIK led to a renewed interest in surface
ablation techniques. New procedures appeared,
aiming to improve outcomes and postoperative
rehabilitation over those of conventional PRK. These
techniques, together with the development of better
excimer laser platforms, were embraced under the
name of Advanced Surface Ablation (ASA).
Mitomycin C has been shown to be effective in
LASEK.4,32 Currently, the criteria to apply MMC
during LASEK are the same as in PRK. However, if
this procedure demonstrates a lower incidence of
haze as compared to conventional mechanical PRK,
MMC may be less necessary. De-epithelialization
with 20% ethanol produces less inflammatory response and delayed keratocyte apoptosis than
manual mechanical deepithelialization in rabbits.18
Clinical studies comparing PRK with mechanical
versus ethanol deepithelialization (in both cases
discarding the epithelium) showed less haze after
ethanol use.13,136 On the other hand, the effect of
replacing the epithelial flap obtained with 20%
ethanol has been studied in animals, showing less
and delayed apoptosis when it was repositioned
compared to no replacement of the flap.78 In
clinical studies, repositioning of the ethanol-obtained epithelial flap has also been associated with
less postoperative haze.137 Two animal studies have
shown that MMC and ethanol applied together are
synergistic, leading to increased keratocyte apoptosis in the anterior stroma69,104 and to a lower
keratocyte density in the anterior stroma 4 weeks
after the surgery.104 If ethanol use during LASEK
produces similar effects as MMC, MMC will not be as
necessary as in conventional PRK.
Regarding the other ASA technique—the epipolisLASIK (epi-LASIK)—the only study comparing this
technique with conventional PRK showed no significant difference in the incidence of haze.113 There
are no specific recommendations yet for MMC use in
epi-LASIK different from those in PRK.88
USE OF MMC DURING SURFACE ABLATION AFTER
OTHER CORNEAL SURGICAL PROCEDURES
Treating residual refractive error with LASIK after
previous corneal surgeries, such as radial keratot-
492
Surv Ophthalmol 54 (4) July--August 2009
omy or penetrating keratoplasty, may result in
problems during the creation of the stromal flap.
Surface ablation avoids these complications, but has
been associated with a higher incidence of haze
than what would have been expected from the
ablation depth.6,87,126 Mitomycin C allows treatment
of these cases with surface ablation, diminishing the
risk of haze.74,102,141,142,168 MMC use has also
extended to complicated LASIK cases (buttonholes
or incomplete LASIK flaps17,77,100,152), even though
some series report low incidence of haze in these
cases.46,138,147,165
Residual refractive errors after LASIK could
benefit from treatment with surface ablation when
an in-the-bed enhancement is not possible. Carones
et al,14 however, reported the development of dense
corneal haze several months after treatment of postLASIK residual refraction with surface ablation.
Even though other series report a much lower
incidence,11,138,159 haze may still appear even with
shallow ablations—Cagil et al11 reported haze with
corrections of --2.00 D or greater—or when treating
residual hyperopia.9 It has been suggested that
surface ablation with MMC in such cases could allow
treatment of these cases while avoiding the risk of
haze.159 Srinivasan et al146 reported good visual and
refractive results when treating residual refraction
from þ0.75 to --2.38 D after LASIK using PRK with
intraoperative MMC, with a tendency to transitory
overcorrection one month postoperatively. We have
noted a tendency to overcorrection, and thus
recommend caution when using surface ablation
with MMC to treat post-LASIK residual refraction.155
For retreatment over a previous surface ablation,
there is no consensus on the need for MMC. Some
authors have performed surface ablation enhancements without MMC and found no increased
incidence of postoperative haze when treating low
residual myopia.1,2,41,118 As a result of the presence
of activated keratocytes at the site of ablation, haze
may appear and cause a decrease in best-corrected
visual acuity.51,129 Therefore, it has been suggested
that MMC would be useful in surface ablation
enhancements.12 There are, however, no studies
addressing the safety of re-applying the drug, and
caution is recommended when using it during
re-treatments.
DOSE AND EXPOSURE TIME IN PRIMARY SURFACE
ABLATION
MMC was initially applied at a concentration of
0.02% for 2 minutes over the ablated stroma.85
Subsequently, when applied prophylactically during
primary surface ablation, the tendency has been to
use a lower dose and a shorter exposure
TEUS ET AL
time.12,107,123,130 Sadeghi et al130 applied MMC on
cultured human keratocytes and reported that its
antiproliferative effect was achieved with much
lower doses than the cytotoxic effect. After a 5minute exposure the lowest concentration that
significantly (O50%) inhibited keratocyte proliferation was 0.05 mg/ml. After that exposure time, the
median inhibitory dose was 0.038 mg/ml (0.0038
%) and the median lethal dose was much higher
than the greatest concentration tested in the study
(0.5 mg/ml [0.05%]).
Netto et al107 applied MMC prophylactically at
two different concentrations (0.02% and 0.002%)
using three different exposure times (12 seconds,
1 minute, 2 minutes) in rabbits. They observed that,
even though 0.02% MMC applied for 2 minutes
achieved the greatest reduction in the postoperative
myofibroblast population, 0.002% MMC applied for
12 seconds was equally effective in preventing
postoperative haze. The difference in the myofibroblast density did not seem to have clinical relevance,
although a larger study might be required to find
a significant difference.
In another study in rabbits, Song et al144
compared the keratocyte apoptosis rate after deepithelialization and application of 0.02% MMC for
15, 30, 60, and 120 seconds and of MMC 0.005%,
0.01%, 0.02% and 0.04% for 2 minutes. They
observed more apoptosis with both greater concentrations and longer exposure times, but the correlation was stronger and statistically significant with
concentration than exposure time.
In human corneas maintained in vitro, Rajan et
al123 applied 0.02% MMC for 1 or 2 minutes after
laser ablation. They observed an initial decrease in
the number of keratocytes in the ablated stroma
similar in the control group and in both MMC-treated
groups. Afterwards, the keratocyte repopulation
started first in the control group, then in the MMC1 minute group, and then in the MMC-2 minutes
group. Four weeks afterwards, the keratocyte density
in the anterior stroma was significantly lower in the
groups that received MMC, with lower density
associated with longer exposure times.
There are only three clinical studies using MMC
at a lower concentration than 0.02%. Camellin12
reported his results using just a ‘‘brushstroke’’ of
0.01% MMC after LASEK in 86 eyes compared to
100 control eyes. He detected less haze in the MMC
group, although the incidence was low in both
groups. Thornton et al156 retrospectively reviewed
the outcomes after LASEK of 83 eyes treated with
0.002% MMC (for 45 to 120 seconds) versus 92
control, non-MMC eyes. They found significantly
less haze in the MMC-treated group. However, haze
in 0.002% MMC-treated eyes that received ablation
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
493
for more than --9.00 D showed a bimodal response
over time, peaking 1 month after the surgery and
again 1 to 2 years afterwards. They also reported
some cases of dense haze in high myopes treated
with low-dose MMC. A retrospective review by the
same authors157 analyzed 126 eyes treated with
0.002% MMC versus 95 eyes treated with 0.02%
MMC. They found less haze in the 0.02% MMC
group, especially in the subgroups of high myopia
(more than --6 D) and deep ablation (more than 75
mm) and reported some cases of moderate to severe
haze in the group that received 0.002% MMC. As
mentioned previously, Sadeghi et al showed that the
median inhibitory dose of the MMC on cultured
human keratocytes is 0.038 mg/ml (0.0038%),
almost twice the concentration applied in the eyes
that received 0.002% MMC.157
Therefore, 0.02% MMC still seems to be the most
effective option for high myopia.157 More studies are
needed to establish the efficacy of lower concentrations for moderate myopia.
Based on the study by Netto et al, 107 and because
there is a lack of other evidence to establish the
optimal exposure time, the tendency has been to
shorten exposure times in order to reduce the side
effects of the MMC. The drug is usually applied for
12 seconds to 1 minute, depending on the ablation
depth.4,75,80,156 Animal studies by Song et al143,144
suggest, however, that changes in the exposure time
have less impact on the absorption of MMC by the
cornea and aqueous humor than changes in
concentration.
The factor most clearly related to development
corneal haze is ablation depth.83,96 Individual and
ethnic factors,149 however, may result in different
corneal wound-healing responses in two patients
receiving the same surgery, and other extrinsic
factors, such as the exposure to ultraviolet radiation,101,148 can modulate that response. Therefore,
there is no established ablation depth under which
there is no risk for haze. When treating myopia,
some authors suggest applying prophylactic MMC
when ablation exceeds a certain number of diopters
(such as --6.00D107), a particular ablation depth (50
mm,32 75 mm,75 or 100 mm93), or when the ablation
depth/corneal thickness ratio is equal to or higher
than 0.18.83,93
Surface ablation is less popular for the treatment
of hyperopia because LASIK obtains better results.145,160 Some reports, however, suggest that
ASA procedures could be safe, effective, and predictable in these eyes.5,112 No study has defined
the indications for using prophylactic MMC in
hyperopic ASA. The incidence of haze after hyperopic surface ablation seems to be higher than
after myopic ablation,111 and although haze after
hyperopic ablation is located at the mid-periphery
of the cornea, it leads to important refractive
regression. Therefore, it is probably advisable to
use MMC even with low hyperopic corrections12
until further comparative studies become available.
PREPARATION AND APPLICATION OF THE
MITOMYCIN C
The MMC dilution may be prepared as follows:
5 ml of balanced salt solution (BSS) or distilled
water are added to 2 mg of MMC, to obtain
a 0.4 mg/ml dilution of MMC. Using an insulin
syringe, we take 0.5 ml of this solution and we add
0.5 ml of BSS or distilled water, thus obtaining 1 ml
with 0.2 mg of MMC—that is, an MMC concentration of 0.2 mg/ml (0.02%).
There are several ways of applying the MMC over
the ablated stroma.12,57,65 The easiest way to avoid
leakage of the MMC to the peripheral cornea or the
limbus is to use a round cellulose sponge approximately 7--9 mm in diameter. This is soaked in the
MMC solution and placed carefully over the ablated
stroma. This technique results in the release of
a reproducible amount of MMC.65 Jain et al proposed
the use of a ring instead of a complete disk, in order to
diminish the exposure of the central cornea to the
MMC,57 and reported good results.86 A small piece of
a cellulose sponge soaked in the MMC solution may
be used to apply a brushstroke of MMC over the
ablated stroma.12
Adverse Effects on the Cornea
The complications associated with MMC in pterygium and glaucoma surgeries3,35,40,92 have not been
reported in refractive surgery. Mitomycin C may cause
vascular endothelial injury140 and, secondarily, tissue
necrosis.80 While the tissues in contact with MMC
during pterygium and glaucoma surgeries are richly
vascularized and may be damaged through that
ischemic mechanism, the avascular cornea is not
affected. When applied to the cornea, MMC could
potentially damage all three main corneal cell types
by direct citotoxicity: epithelial (differentiated epithelium and limbal cells), stromal (keratocytes), and
endothelial cells. Only the first two have substantial
mitotic activity. Because cells with a higher mitotic
rate are more sensitive to the MMC, the epithelium
and the keratocytes would be expected to be
more susceptible to MMC toxicity than the
endothelium.166
EFFECT ON THE CORNEAL EPITHELIUM
Animal studies have shown variable results regarding the effect of MMC in the corneal epithe-
494
Surv Ophthalmol 54 (4) July--August 2009
TEUS ET AL
lium. Chang21 reported a dose-dependant delay in
re-epithelialization after application of 0.01% and
0.02% MMC for 2 minutes, but another study in
rabbits76 did not find any re-epithelialization delay
associated with MMC.
Rajan et al 123 applied 0.02% MMC for 1 and
2 minutes on human corneas in vitro. They found
a delay in the latency until the re-epithelialization
started that was dependant on the duration of the
application of the MMC, but no difference in the
epithelial migration rate (once the re-epithelialization began) between the group that received MMC
for 1 minute compared to controls. They observed
a statistically significant delay until the corneal
epithelialization was complete in the group that
received MMC for 2 minutes.
Despite these experimental observations, clinical
studies suggest a lack of relevant epithelial toxicity
(Table 2). In addition, studies of repeated topical
application of MMC to treat ocular surface neoplasias, where the drug also contacts the limbus, do
not show epithelial changes, thus suggesting the
absence of limbal toxicity.64 There has been only
one report of epithelial corneal toxicity after
application of 0.02% MMC intraoperatively for
2 minutes, a case of persistent punctate keratitis.73
When used prophylactically, the MMC is currently
applied for a shorter time.4,75,80 Given the results of
Rajan et al,123 those short exposure times could
explain why corneal epithelial complications are
rarely seen after MMC use during surface ablation.
There is another aspect of the possible epithelial
toxicity of MMC that has not been thoroughly
studied: the effect on the development of epithelial
hyperplasia. Epithelial hyperplasia has been described following surface ablantion,28,47,84 especially
with small optical zones (#5 mm) and deeper
ablations, where the change in dioptric power at
the edge of the ablation zone is more abrupt.45,50
The epithelium reacts to stromal loss with hypertrophy of the cells of the basal layer and, if this
hypertrophy does not result in a smooth corneal
surface, epithelial hyperplasia develops.28,34 As the
epithelium plays an important role in determining
the dioptric power of the total cornea,44,82 this
epithelial hyperplasia is thought to be one cause of
refractive regression after surface ablation.84 Another study97 using confocal microscopy on human
corneas after surface ablation found no epithelial
hyperplasia and no relation between postoperative
epithelial thickness and refractive regression. They
did detect an increment in stromal thickness related
to postoperative regression.
A change in the pattern of epithelial hyperplasia
associated with the use of MMC could be a subtle
sign of its epithelial toxicity. Rajan et al,123 using
human corneas in vitro, found a normal epithelial
thickness and morphology 1 month after the
application of 0.02% MMC for 1 minute when
compared to the control group, but the epithelial
layer was less differentiated and significantly thinner
in the group that received 0.02% MMC for
2 minutes. These differences might have disappeared with longer follow-up. Chen et al22 applied
0.02% MMC for 20--30 seconds after epi-LASIK and
found that, 1 week postoperatively, the number of
basal cells with normal morphology was greater in
the control group that did not receive MMC, but
they did not find any differences in subsequent
examinations. The number of apical cells with
normal morphology was only slightly higher in the
control group in examinations 2 weeks, 1 month,
TABLE 2
Clinical Studies Reporting The Effect of Mitomycin C (MMC) on the Corneal Epithelium after Surface Ablation
MMC
Dose (%)
MMC
Application
Time
Authors
Number of Eyes
Manuscript Type
Argento et al4
30 MMC-treated
28 controls
86 MMC-treated
100 controls
30 MMC-treated
30 controls
36 MMC-treated
36 controls
1
Retrospective,
comparative study
Prospective, nonrandomized,
comparative study
Prospective, randomized,
comparative study
Prospective, randomized,
comparative study
Case report
0.02
75 sec
0.01
Brushstroke
0.02
30 sec
0.02
2 min
0.02
2 min
52 MMC-treated
52 controls
1,011
35
Prospective, randomized,
comparative study
Retrospective case series
Retrospective case series
0.02
45 sec
0.02
0.02
30 sec - 2 min
2 min
Camellin12
Carones et al15
Gambato et al42
Kymionis et al73
Leccisotti79
Lee et al80
Vigo et al162
Effect on the
Epithelium
No difference in
re-epithelialization
No difference in
re-epithelialization
No difference in
re-epithelialization
No difference in
re-epithelialization
Persistent punctate
keratitis
No difference in
re-epithelialization
Delay in 2 eyes
No epithelial toxicity
reported
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
495
and 6 months after the surgery. In a group of 64
eyes, we found a statistically significant increase in
central corneal thickness from 1 to 3 months after
surface ablation, with no significant difference in
the corneal thickness increase between the group
that received intraoperative MMC and the group
that did not receive MMC (Teus MA et al. Effect of
mitomycin C on epithelial hyperplasia after LASEK.
EVER meeting, Portoroz, Slovenia, October 3--6,
2007). More studies with longer follow-up measuring epithelial and stromal thicknesses after surface
ablation would help define whether the MMC
interferes with the normal pattern of corneal
regrowth seen after laser surface ablation.
keep their capacity to activate and proliferate in
response to a corneal trauma.
MMC has been shown to reduce haze associated
with ultraviolet B (UV-B) irradiation after surface
ablation in rabbits.68 Irradiation alone causes
cellular toxicity and reduces cell growth in cultures
of porcine corneal fibroblasts, effects that are
enhanced when MMC was applied before the UV-B
irradiation.19 This observation has led to the
recommendation that UV-B protection be used in
eyes treated with surface ablation and intraoperative
MMC until the synergistic effect of MMC and UV-B
on long-term keratocyte population is clarified.
The keratocyte density that a cornea needs to
maintain to keep its normal function is not known,
nor whether a depletion of keratocytes would carry
a higher risk of long-term corneal instability.
Whether MMC effects on the stromal population
could facilitate post-surface ablation ectasia or
corneal melting is not known, although no case of
ectasia or corneal melting after surface ablation with
MMC has yet been reported.
EFFECT ON THE CORNEAL STROMA
Keratocytes constitute the second cell type exposed to the MMC. It is in fact the cytotoxic and
antiproliferative effects of the MMC on the corneal
stromal cellularity that produce its capacity to
reduce haze, since it inhibits its activation, proliferation and differentiation into myofibroblasts.20,67,68,76,107,167 This antimitotic effect has led
to concern over a possible long-term depletion of
keratocyte population.36,106,107
The long-term effect of the laser ablation itself on
stromal population is itself controversial. Studies
disagree: some find a similar or higher postoperative
keratocyte density28,39,95,97,124 whereas others have
reported a decreased stromal population37,38,54 after
surface ablation with no adjunctive MMC.
The few studies using intraoperative MMC also
report contradictory results (Table 3). All reporting
keratocyte depletion are animal or laboratory
studies and all have a short follow-up (1 to 3
months). Those animal and human studies with
longer follow-up (6 months or more) demonstrate
that, after the initial depletion, the keratocytes
proliferate, and no significant decrease in their
density is found 6 to 12 months after the use of
MMC. Midena et al90 detected keratocyte depletion
5 years after surface ablation compared to preoperative levels, regardless of whether MMC was
used. The keratocytes of the posterior cornea do not
seem to be altered by the use of MMC.42,123
Qazi et al122 reported a case of late dense haze
that developed after uncomplicated primary surface
ablation with prophylactic MMC performed 17
months previously. We have also observed late
corneal scarring that developed following epithelial
trauma 1 year after LASEK with intraoperative
0.02% MMC for 1 minute. These two cases and the
observations made by Gambato et al suggest that
stromal cellularity does not significantly suffer from
permanent MMC effect and that the keratocytes
EFFECT ON THE CORNEAL ENDOTHELIUM
The third corneal cell type exposed to the MMC
in corneal refractive surgery is the endothelium.
Endothelium has the least mitotic activity in normal
conditions as a result of contact inhibition and the
presence in the aqueous humor of inhibitory
factors.61,62,134 Torres et al158 and Song et al143,144
detected the presence of MMC in the aqueous
humor after its application over the de-epithelialized cornea in animal models, suggesting that the
drug contacts the posterior stromal layers and the
endothelium. This raises the question of potential
deep corneal toxicity. Direct exposure of the
endothelium to the MMC at the concentrations
used on the ocular surface would rapidly cause
endothelial damage.53,89,110 Fortunately, apart from
accidentally instillation of MMC into the anterior
chamber during glaucoma filtering surgery, such
concentrations do not reach the endothelium, as
the concentration of MMC detected in the anterior
chamber after its application over the deepithelialized cornea is much lower.143,144,158 McDermott et
al89 and Garweg et al43 showed that direct application of MMC (on human corneas maintained in
vitro89 and on endothelial cell cultures43) at
concentrations of 100 mg/ml (0.01%) or lower did
not result in endothelial toxicity, whereas application of 200 mg/ml (0.02%) MMC rapidly induced
edema with marked ultrastructural changes. Torres
et al158 and Song et al143,144 measured MMC
concentration in the aqueous humor after application of 0.02% MMC for 2 minutes and found an
Non-decreased compared
to eyes without MMC
5 years
2 min
0.02
3 years
2 min
0.02
6 months
5 min
0.02
1 month
1 min, 2 min
0.02
36
56
Gambato et al42
Midena et al90
Human study
20
Xu et al167
Human study
Prospective, randomized,
comparative study
Prospective, randomized,
comparative study
Prospective, randomized,
comparative study
Prospective, randomized,
comparative study
16
Rajan et al123
Animal study (rabbits)
182
Netto et al107
Laboratory study
(human corneas in vitro)
Animal study (rabbits)
1 month
12 sec--2 min
0.002, 0.02
3 months
2 min
0.02
Prospective, randomized,
comparative study
Prospective, randomized,
comparative study
Animal study (rabbits)
18
Manuscript Type
Type of Study
Authors
Kim et al68
Last Follow-up
MMC
Application
Time
MMC
Dose (%)
Number of Eyes
Receiving MMC
Studies Reporting the Effect of Mitomycin C (MMC) on the Keratocytes
TABLE 3
Non-decreased
aqueous humor concentration much lower than
0.002%. Nevertheless, this small concentration has
been shown to cause cross-linking and doublestrand breaks of corneal endothelial DNA in goat
corneas.128
The possible long-term effects of these changes
on human corneas in vivo are still controversial,
since two recent studies suggest a decrease in
corneal endothelial cell density, whereas the majority of them report no endothelial change at all
(Table 4).115 In fact, there have been no reports of
corneal edema after the usual dose and exposure
time of intraoperative MMC in surface ablation. The
only case of corneal edema after MMC application
in refractive surgery occurred in a patient after
repeated postoperative topical application of
MMC.117 Garweg et al43 had shown that MMC
cytotoxicity appeared if the exposure was maintained chronically for 7 days, even with low
concentrations, which could explain the case of
corneal edema.117
Chang21 applied 0.01% and 0.02% MMC for
2 minutes in rabbit corneas and reported a dosedependent transient edema and a decrease in
endothelial cell density. The fact that the rabbit
corneal endothelium has continuous mitotic activity,60 unlike human endothelium, may have led to
a higher sensitivity of the rabbit endothelium to the
antimitotic action of the MMC.
Among the human studies, Morales et al99 found
significant cell loss in the MMC group (nine eyes),
compared to the control group (nine eyes).
However, the high standard deviation of endothelial
cell counts make results in studies with few patients
difficult to interpret, because the probability of
having cases with extreme counts (too low or too
high) in a given group is high. There are two main
ways to decrease the uncertainty: decrease the
standard deviation (i.e., increase the reproducibility
of the measurement) or increase the number of
cases studied. Most human studies that include
a large number of patients do not detect that
endothelial cell decrease (Table 4), and two of
them30,80 actually found a statistically significant
increase in the endothelial cell density 3 to 6
months after surgery. This increase may have
resulted from the cessation of contact lens wear.116
Another explanation may be the change in corneal
magnification after laser ablation. The decrease in
the keratometric values after myopic laser ablation
profiles would produce a decrease in the magnification of the image of the endothelial cells obtained
by specular microscopy.55 The cells would consequently appear smaller than in the preoperative
picture and would thus be counted erroneously as
being more numerous.
Time and
dose-dependant
decrease
Time-dependant
decrease
Non-decreased
TEUS ET AL
Decreased
Surv Ophthalmol 54 (4) July--August 2009
Keratocyte Density
at Last Follow-up
496
Clinical Studies Reporting the Effect of Mitomycin C (MMC) on the Corneal Endothelium after Its Application over the Cornea
Number of Eyes
(patients)
Authors
De Benito-Llopis et al30
48 (24)
Diakonis et al33
15 (15)
Gambato et al42
36 (36)
Goldsberry et al49
16 (8)
Leccisotti79
52 (52)
Lee et al80
359
Morales et al99
9 (9)
Nassaralla et al102
Nassiri et al103
22 (14)
76 (48)
Wallau et al163
44 (44)
Zhao et al
169
174 (89)
Manuscript Type
Prospective, nonrandomized,
comparative study
Prospective, randomized,
comparative study
Prospective, randomized,
comparative study
Prospective case series
Prospective, randomized,
comparative study
Retrospective case series
Prospective, randomized,
comparative study
Prospective case series
Prospective, nonrandomized,
comparative study
Prospective, randomized,
comparative study
Prospective case series
MMC
Dose (%)
MMC
Application
Time
Follow-up
(months)
Endothelial
Cell Density
Endothelial Cell
Morphology
Clinically
Evident
Corneal
Edema
0.02
30 sec
3
Non-decreased
n.a.
No
0.02
15 sec
12
Non-decreased
Unchanged
No
0.02
2 min
n.a.
Unchanged
No
0.02
12 sec
Non-decreased
Unchanged
No
0.02
45 sec
Mean: 12
(range 12--36)
Mean: 18
(range 12--24)
12
Non-decreased
n.a.
No
0.02
30 sec--2 min
0.02
Non-decreased
Unchanged
No
30 sec
3 (96 eyes
followed up
to 6 months)
3
Decreased
n.a.
No
0.02
0.02
2 min
10--50 sec
6
6
Non-decreased
Decreased
n.a.
n.a.
No
No
0.002
1 min
6
Non-decreased
Unchanged
No
0.02
15 sec
6
Non-decreased
Unchanged
No
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
TABLE 4
497
498
Surv Ophthalmol 54 (4) July--August 2009
The lack of clinically evident endothelial toxicity
and the mentioned studies (Table 4) suggest that
one application of MMC at the low concentration
used in refractive surgery is probably insufficient to
produce a significant cytotoxic effect in the endothelium. Long-term studies are still needed to
further establish its safety.
EFFECT ON THE CILIARY BODY AND THE
INTRAOCULAR PRESSURE
Several studies have suggested a cytotoxic effect of
topical MMC on the ciliary body when applied
transsclerally, and such cytotoxicity might be involved in the postoperative hypotony that may
appear after its use in glaucoma surgery.52,91,109,131,133 Only one recent study analyzes
this effect after applying MMC over the ablated
cornea. Kymionis et al72 applied 0.02% MMC during
2 minutes in 20 rabbit corneas previously treated
with a 7-mm deep surface ablation. The contralateral
eyes served as controls. They did not find differences in the intraocular pressure between eyes
treated with MMC and the fellow eyes up to 3
months postoperatively. They also did not find any
difference between preoperative and postoperative
intraocular pressure. Optic and electronic microscopy did not show morphological changes in the
ciliary body. These results suggest that the amount
of MMC that enters the anterior chamber and gets
in contact with the ciliary body is insufficient to
cause toxicity.72
Conclusions
Evidence 1 clinical trials are clearly needed to
definitely establish the efficacy and safety of the use
of MMC in corneal refractive surgery. Nevertheless,
the current available evidence supports the use of
this drug in surface ablation procedures.
Mitomycin C has shown to decrease the incidence
of haze after surface ablation refractive surgery. Its
use allows treatment with surface ablation not only
of low and moderate myopia, but also of high
myopia with similar visual and refractive results as
LASIK. There is a trend toward reduced dosage and
exposure time of MMC; several studies suggest that
even low concentrations over short times are
effective in reducing the risk of haze. Some studies,
however, suggest that lower concentrations
(0.002%) may not be adequate to prevent haze
after surface ablation for high myopia. More longterm clinical studies are needed to establish the
efficacy of lower concentrations to avoid haze in
moderate myopia. There is not enough evidence to
establish the criteria for the use of prophylactic
TEUS ET AL
MMC in hyperopic ablations. The usual intraoperative dose of 0.02% MMC has not been associated
with any clinically relevant corneal toxicity. More
studies are needed to evaluate the effect of this drug
on postoperative corneal epithelial hyperplasia and
stromal regrowth. Long-term depletion of keratocyte population after MMC application is controversial, and its consequences to corneal stability still
needs to be analyzed. Human studies are needed to
confirm the lack of toxicity to the ciliary body and of
effect on the postoperative intraocular pressure, as
suggested by animal studies.
Method of Literature Search
Articles regarding mitomycin C were identified
through a multistage systematic approach. First, we
conducted a computerized search of the Medline
database using PubMed (www.pubmed.com). Last
search was performed in September 2008. A
comprehensive search was made using the terms:
haze, excimer laser surface ablation, advanced surface
ablation, photorefractive keratectomy, PRK, laser-assisted
subepithelial keratectomy, laser subepithelial keratomileusis, LASEK, epipolis LASIK, epi-LASIK, LASIK, laser in
situ keratomileusis and all of those terms followed by
‘‘AND’’ and the following: mitomycin, mitomycin-C,
MMC, alkylating agent, MMC toxicity. Second, all
entries were critically reviewed and those considered
to be of significance were used, including those
written in English, Spanish, and French, and also
those from the non-English literature if an English
abstract was available. Next, we reviewed the
reference section of each article, to detect other
studies not captured by the Medline search. Once
these articles were critically reviewed, they were
included if they were considered to add additional
data or to refute previous information.
References
1. Alió JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of
photorefractive keratectomy for myopia of less than --6
diopters. Am J Ophthalmol. 2008;145:29--36
2. Alió JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of
photorefractive keratectomy for myopia of more than --6
diopters. Am J Ophthalmol. 2008;145:37--45
3. Anand N, Arora S, Clowes M. Mitomycin C augmented
glaucoma surgery: evolution of filtering bleb avascularity,
transconjunctival oozing and leaks. Br J Ophthalmol. 2006;
92:175--80
4. Argento C, Cosentino MJ, Ganly M. Comparison of laser
epithelial keratomileusis with and without the use of
mitomycin C. J Refract Surg. 2006;22:782--6
5. Autrata R, Rehurek J. Laser-assisted subepithelial keratectomy and pohotorefractive keratectomy for the correction
of hyperopia: results of a 2-year follow-up. J Cataract
Refract Surg. 2003;29:2105--14
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
499
6. Azar DT, Tuli S, Benson RA, Hardten DR. Photorefractive
keratectomy for residual myopia after radial keratotomy.
PRK after RK Study Group. J Cataract Refract Surg. 1998;
24:303--11
7. Baldwin HC, Marshall J. Growth factors in corneal wound
healing following refractive surgery: a review. Acta Ophthalmol Scand. 2002;80:238--47
8. Bedei A, Marabotti A, Giannecchini I, et al. Photorefractive
keratectomy in high myopic defects with or without
intraoperative mitomycin C: 1-year results. Eur J Ophthalmol. 2006;16:229--34
9. Beerthuizen JJG, Siebelt E. Surface ablation after laser in
situ keratomileusis: retreatment on the flap. J Cataract
Refract Surg. 2007;33:1376--80
10. Bligh HF, Bartoszek A, Robson CN, et al. Activation of
mitomycin C by NADPH:cytochrome p-450 reductase.
Cancer Res. 1990;50:7789--92
11. Cagil N, Aydin B, Ozturk S, Hasiripi H. Effectiveness of
laser-assisted subepithelial keratectomy to treat residual
refractive errors after laser in situ keratomileusis. J Cataract
Refract Surg. 2007;33:642--7
12. Camellin M. Laser epithelial keratomileusis with mitomycin
C: indications and limits. J Refract Surg. 2004;20:S693--8
13. Carones F, Fiore T, Brancato R. Mechanical vs alcohol
epithelial removal during photorefractive keratectomy. J
Refract Surg. 1999;15:556--62
14. Carones F, Vigo L, Carones A, Brancato R. Evaluation of
photorefractive keratectomy retreatments after regressed
myopic laser in situ keratomileusis. Ophthalmology. 2001;
108:1732--7
15. Carones F, Vigo L, Scandola E, Vacchini L. Evaluation of
the prophylactic use of mitomycin-C to inhibit haze
formation after photorefractive keratectomy. J Cataract
Refract Surg. 2002;28:2088--95
16. Chabner BA, Ryan DP, Paz-Ares L, et al. Antineoplastic
agents, in Hardman JG, Limbrid LE, Goodman Gilman A.
The Pharmacological Basis of Therapeutics. New York,
McGraw Hill, 2001. ed 10; pp 1389--459.
17. Chalita MR, Roth AS, Krueger RR. Wavefront-guided
surface ablation with prophylactic use of mitomycin C
after a buttonhole laser in situ keratomileusis flap. J Refract
Surg. 2004;20:176--81
18. Chang SW, Chou SF, Chuang JL. Mechanical corneal
epithelium scraping and ethanol treatment up-regulate
cytokine gene expression differently in rabbit cornea. J
Refract Surg. 2008;24:150--9
19. Chang SW, Chou SF, Chuang JL. Mitomycin C potentiates
ultraviolet-related cytotoxicity in corneal fibroblasts. Cornea. 2008;27:686--92
20. Chang SW. Corneal keratocyte apoptosis following topical
intraoperative mitomycin C in rabbits. J Refract Surg. 2005;
21:446--53
21. Chang SW. Early corneal edema following topical
application of mitomycin-C. J Cataract Refract Surg. 2004;
30:1742--50
22. Chen WL, Chang HW, Hu FR. In vivo confocal microscopic
evaluation of corneal wound healing after epi-LASIK.
Invest Ophthalmol Vis Sci. 2008;49:2416--23
23. Chou SF, Chang SW, Chuang JL. Mitomycin C upregulates
IL-8 y MCP-1 chemokine expression via mitogen-activated
protein kinases in corneal fibroblasts. Invest Ophthalmol
Vis Sci. 2007;48:2009--16
24. Crowston JG, Chang LH, Constable PH, et al. Apoptosis
gene expression and death receptor signalling in mitomycin-C-treated human tenon capsule fibroblasts. Invest
Ophthalmol Vis Sci. 2002;43:692--9
25. Crowston JG, Chang LH, Daniels JT, et al. T lymphocyte
mediated lysis of mitomycin C treated Tenon’s capsule
fibroblasts. Br J Ophthalmol. 2004;88:399--405
26. Cummings J, Spanswick VJ, Tomasz M, Smyth JF.
Enzymology of mitomycin C metabolic activation in
tumour tissue: implications for enzyme-directed bioreductive drug development. Biochem Pharmacol. 1998;56:
405--14
27. Daniels JT, Occleston NL, Crowston JG, Khaw PT. Effects of
antimetabolite induced cellular growth arrest on fibroblastfibroblast interactions. Exp Eye Res. 1999;69:117--27
28. Dawson DG, Edelhauser HF, Grossniklaus HE. Long-term
histopathologic findings in human corneal wounds after
refractive surgical procedures. Am J Ophthalmol. 2005;139:
168--78
29. De Benito-Llopis L, Teus M, Sánchez-Pina JM, Hernández-Verdejo JL. Comparison between LASEK and LASIK
for the correction of low myopia. J Refract Surg. 2007;23:
139--45
30. De Benito-Llopis L, Teus MA, Ortega M. Effect of
mitomycin C on the corneal endothelium during excimer
laser surface ablation. J Cataract Refract Surg. 2007;33:
1009--13
31. De Benito-Llopis L, Teus MA, Sánchez-Pina JM, Fuentes I.
Stability of LASEK with and without mitomycin-C performed to correct myopia in thin corneas. A 15-month
follow-up. Am J Ophthalmol. 2008;145:807--12
32. De Benito-Llopis L, Teus MA, Sánchez-Pina JM. Comparison between LASEK with MMC and LASIK for the
correction of high myopia (--7.00 to --13.75 D). J Refract
Surg. 2008;24:516--23
33. Diakonis VF, Pallikaris A, Kymionis GD, Markomanolakis MM.
Alterations in endothelial cell density after photorefractive
keratectomy with adjuvant mitomycin. Am J Ophthalmol.
2007;144:99--103
34. Dillon EC, Eagle RC Jr, Laibson PR. Compensatory
epithelial hyperplasia in human corneal disease. Ophthalmic Surg. 1992;23(11):729--32
35. Dougherty PJ, Hardten DR, Lindstrom RL. Corneoscleral
melt after pterygium surgery using a single intraoperative
application of mitomycin-C. Cornea. 1996;15:537--40
36. Dupps WJ, Wilson SE. Biomechanics and wound healing in
the cornea. Exp Eye Res. 2006;83:709--20
37. Erie JC, Patel SV, McLaren JW, et al. Corneal keratocyte
deficits after photorefractive keratectomy and laser in situ
keratomileusis. Am J Opththalmol. 2006;141:799--809
38. Erie JC, Patel SV, McLaren JW, et al. Keratocyte density in
the human cornea after photorefractive keratectomy. Arch
Ophthalmol. 2003;121:770--6
39. Frueh BE, Cadez R, Bohnke M. In vivo confocal microscopy
after photorefractive keratectomy in humans. A prospective, long-term study. Arch Ophthalmol. 1998;116:1425--31
40. Fujitani A, Hayasaka S, Shibuya Y, Noda S. Corneoscleral
ulceration and corneal perforation after pterygium excision and topical mitomycin-C therapy. Ophthalmologica.
1993;207:162--4
41. Gabler B, von Mohrenfels CW, Herrmann W, et al. Laserassisted subepithelial keratectomy enhancement of
residual myopia after primary myopic LASEK: six-month
results in 10 eyes. J Cataract Refract Surg. 2003;29:1260--6
42. Gambato C, Ghirlando A, Moretto E, et al. Mitomycin C
modulation of corneal wound healing after photorefractive
keratectomy in highly myopic eyes. Ophthalmology. 2005;
112:208--19
43. Garweg JG, Wegmann-Burns M, Goldblum D. Effects of
daunorubicin, mitomycin C, azathioprine and cyclosporine
A on human retinal pigmented epithelial, corneal endothelial and conjunctival cell lines. Graefe’s Arch Clin Exp
Ophthalmol. 2006;244:382--9
44. Gatinel D, Racine L, Hoang-Xuan T. Contribution of the
corneal epithelium to anterior corneal topography in
patients having myopic photorefractive keratectomy.
J Cataract Refract Surg. 2007;33:1860--5
45. Gauthier CA, Holden BA, Epstein D, et al. Factors affecting
epithelial hyperplasia after photorefractive keratectomy.
J Cataract Refract Surg. 1997;23:1042--50
46. Gimbel HV, Stoll SB. Photorefractive keratectomy with
customized segmental ablation to correct irregular astigmatism after laser in situ keratomileusis. J Refract Surg.
2001;17:S229--32
47. Gipson IK. Corneal epithelial and stromal reactions to
excimer laser photorefractive keratectomy. I. Concerns
500
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
Surv Ophthalmol 54 (4) July--August 2009
regarding the response of the corneal epithelium to
excimer laser ablation. Arch Ophthalmol. 1990;108(11):
1539--40
Goeptar AR, Groot EJ, Scheerens H, et al. Cytotoxicity of
mitomycin C and adriamycin in freshly isolated rat
hepatocytes: the role of cytochrome p450. Cancer Res.
1994;54:2411--8
Goldsberry DH, Epstein RJ, Majmudar PA, et al. Effect of
mitomycin C on the corneal endothelium when used for
corneal subepithelial haze prophylaxis following photorefractive keratectomy. J Refract Surg. 2007;23:724--7
Hamberg-Nystrom H, Gauthier CA, Holden BA, et al. A
comparative study of epithelial hyperplasia after PRK:
Summit versus VISX in the same patient. Acta Ophthalmol
Scand. 1996;74(3):228--31
Haw WW, Manche EE. Excimer laser retreatment of
residual myopia following photoastigmatic refractive keratectomy for compound myopic astigmatism. J Cataract
Refract Surg. 2000;26:660--7
Heaps RS, Nordlund JR, Gonzalez-Fernandez F, et al.
Ultrastructural changes in rabbit ciliary body after extraocular mitomycin C. Invest Ophthalmol Vis Sci. 1998;39:
1971--5
Hernández-Galilea E, Sanchez F, Guzman K, et al. Effect of
mitomycin C on corneal endothelium cells. In vitro study.
Arch Soc Esp Oftalmol. 2000;75:515--21
Herrman WA, Muecke M, Koller M, et al. Keratocyte
density in the retroablation area after LASEK for the
correction of myopia. Graefe’s Arch Clin Exp Ophthalmol.
2007;245:426--30
Isager P, Hjortdal JO, Ehlers N. Magnification changes in
specular microscopy after corneal refractive surgery. Acta
Ophthalmol Scand. 1999;77:391--3
Islaih M, Halstead BW, Kadura IA, et al. Relationships
between genomic, cell cycle, and mutagenic responses of
TK6 cells exposed to DNA damaging chemicals. Mutat Res.
2005;578:100--16
Jain S, McCally RL, Connolly PJ, Azar DT. Mitomycin C
reduces corneal light scattering after excimer keratectomy.
Cornea. 2001;20:45--9
Jester JV, Ho-Chang J. Modulation of cultured corneal
keratocyte phenotype by growth factors /cytokines control
in vitro contractility and extracellular matrix contraction.
Exp Eye Res. 2003;77:581--92
Jester JV, Petroll WM, Cavanagh HD. Corneal stromal
wound healing in refractive surgery: the role of myofibroblasts. Prog Retin Eye Res. 1999;18:311--56
Joyce NC, Navon SE, Roy S, Zieske JD. Expression of cell
cycle-associated proteins in human and rabbit corneal
endothelium in situ. Invest Ophthalmol Vis Sci. 1996;37:
1566--75
Joyce NC. Cell cycle status in human corneal endothelium.
Exp Eye Res. 2005;81:629--38
Joyce NC. Proliferative capacity of the corneal endothelium. Prog Ret Eye Res. 2003;22:359--89
Khaw PT, Doyle JW, Sherwood MB, et al. Prolonged
localized tissue effects from 5-minute exposures to fluorouracil and mitomycin C. Arch Ophthalmol. 1993;111:263--7
Khong JJ, Muecke J. Complications of mitomycin C therapy
in 100 eyes with ocular surface neoplasia. Br J Ophthalmol.
2006;90:819--22
Khoury JM, Farah T, El-Haibi CP, Noureddin BN. Corneal
light shield as a delivery system for standardized application of mitomycin C in excimer surface ablation. J Refract
Surg. 2007;23:716--9
Kim JK, Kim SS, Lee HK, et al. Laser in situ keratomileusis
versus laser-assisted subepithelial keratectomy for the
correction of high myopia. J Cataract Refract Surg. 2004;
30:1405--11
Kim TI, Lee SY, Pak JH, et al. Mitomycin C, ceramide, and
5-fluorouracil inhibit corneal haze and apoptosis after PRK.
Cornea. 2006;25:55--60
Kim TI, Pak JH, Lee SY, Tchah H. Mitomycin C-induced
reduction of keratocytes and fibroblasts after photor-
TEUS ET AL
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
83.
84.
85.
86.
87.
88.
89.
90.
efractive keratectomy. Invest Ophthalmol Vis Sci. 2004;45:
2978--84
Kim TI, Tchah H, Cho EH, Kook MS. Evaluation for safety of
cultured corneal fibroblasts with cotreatment of alcohol and
mitomycin C. Invest Ophthalmol Vis Sci. 2004;45:86--92
Kim TI, Tchah H, Lee SA, et al. Apoptosis in keratocytes
caused by mitomycin C. Invest Ophthalmol Vis Sci. 2003;
44:1912--7
Kremer I, Kaplan A, Novikov I, Blumenthal M. Patterns of
late corneal scarring after photorefractive keratectomy in
high and severe myopia. Ophthalmology. 1999;106:467--73
Kymionis GD, Diakonis VF, Charisis S, et al. Effects of
topical mitomycin C on the ciliary body and intraocular
pressure after PRK: an experimental study. J Refract Surg.
2008;24:633--8
Kymionis GD, Tsiklis NS, Ginis H, et al. Dry eye after
photorefractive keratectomy with adjuvant mitomycin C.
J Refract Surg. 2006;22:511--3
La Tegola MG, Alessio G, Sborgia C. Topographic
customized photorefractive keratectomy for regular and
irregular astigmatism after penetrating keratoplasty using
the LIGI CIPTA/LaserSight Platform. J Refract Surg. 2007;
23:681--93
Lacayo GO 3rd, Majmudar PA. How and when to use
mitomycin-C in refractive surgery. Curr Opin Ophthalmol.
2005;16:256--9
Lai YH, Wang HZ, Lin CP, Chang SJ. Mitomycin C alters
corneal stromal wound healing and corneal haze in rabbits
after argon-fluoride excimer laser photorefractive keratectomy. J Ocul Pharmacol Ther. 2004;20:129--38
Lane HA, Swale JA, Majmudar PA. Prophylactic use of
mitomycin-C in the management of a buttonholed LASIK
flap. J Cataract Refract Surg. 2003;29:390--2
Laube T, Wissing S, Tehis C, et al. Decreased keratocyte
death after laser-assisted subepithelial keratectomy and
photorefractive keratectomy in rabbits. J Cataract Refract
Surg. 2004;30:1998--2004
Leccisotti A. Mitomycin C in photorefractive keratectomy:
effect on epithelialization and predictability. Cornea. 2008;
27:288--91
Lee DH, Chung HS, Jeon Y, et al. Photorefractive
keratectomy with intraoperative mitomycin-C application.
J Cataract Refract Surg. 2005;31:2293--8
Lee YJ, Park SJ, Ciccone SL, et al. An in vivo analysis of
MMC-induced DNA damage and its repair. Carcinogenesis.
2006;27:446--53
Legeais JM, Mayer F, Saragoussi JJ, et al. The optical power
of the corneal epithelium In vivo evaluation. J Fr
Ophtalmol. 1997;20(3):207--12
Lin N, Yee SB, Mitra S, et al. Prediction of corneal haze
using an ablation depth/corneal thickness ratio after laser
epithelial keratomileusis. J Refract Surg. 2004;20:797--802
Lohmann CP, Reischl U, Marshall J. Regression and epithelial
hyperplasia after myopic photorefractive keratectomy in
a human cornea. J Cataract Refract Surg. 1999;25:712--5
Majmudar PA, Forstot SL, Dennis RF, et al. Topical
mitomycin C for subepithelial fibrosis after refractive
corneal surgery. Ophthalmology. 2000;107:89--94
Maldonado MJ. Intraoperative MMC after excimer laser
surgery for myopia. Ophthalmology. 2002;109:826--8
Maloney RK, Chan WK, Steinert R, et al. A multicenter trial
of photorefractive keratectomy for residual myopia after
previous ocular surgery. Summit Therapeutic Refractive
Study Group. Ophthalmology. 1995;102:1578--9
Matsumoto JC, Chu YSR. Epi-LASIK update: overview of
techniques and patient management. Int Ophthalmol Clin.
2006;46:105--15
McDermott ML, Wang J, Shin DH. Mitomycin and the
human corneal endothelium. Arch Ophthalmol. 1994;112:
533--7
Midena E, Gambato C, Miotto S, et al. Long-term effects on
corneal keratocytes of mitomycin C during photorefractive
keratectomy: a randomized contralateral eye confocal
microscopy study. J Refract Surg. 2007;23:S1011--4
MITOMYCIN C IN CORNEAL REFRACTIVE SURGERY
501
91. Mietz H, Addicks K, Diestelhorst M, Krieglstein GK.
Extraocular application of mitomycin C in a rabbit model:
cytotoxic effects on the ciliary body and epithelium.
Ophthalmic Surg. 1994;25:240--4
92. Mietz H, Roters S, Krieglstein GK. Bullous keratopathy as
a complication of trabeculectomy with mitomycin C.
Graefes Arch Clin Exp Ophthalmol. 2005;243(12):1284--7
93. Mirza MA, Qazi MA, Pepose JS. Treatment of dense
subepithelial corneal haze after laser-assisted subepithelial
keratectomy. J Cataract Refract Surg. 2004;30:709--14
94. Mladenov E, Tsaneva I, Anachkova B. Activation of the S
phase DNA damage checkpoint by mitomycin C. J Cell
Physiol. 2007;211:468--76
95. Moilanen JA, Vesaluoma MH, Muller LJ, Tervo TM. Longterm corneal morphology after PRK by in vivo confocal
microscopy. Invest Ophthalmol Vis Sci. 2003;44:1064--9
96. Moller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV.
Corneal haze development after PRK is regulated by
volume of stromal tissue removal. Cornea. 1998;17:
627--639
97. Moller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV.
Stromal wound healing explains refractive instability and
haze development after photorefractive keratectomy. A 1year confocal microscopic study. Ophthalmology. 2000;107:
1235--45
98. Moller-Pedersen T. Keratocyte reflectivity and corneal haze.
Exp Eye Res. 2004;78:553--60
99. Morales AJ, Zadok D, Mora-Retana R, et al. Intraoperative
mitomycin and corneal endothelium after photorefractive
keratectomy. Am J Ophthalmol. 2006;142:400--4
100. Müller LT, Candal EM, Epstein RJ, et al. Transepithelial
phototherapeutic keratectomy/photorefractive keratectomy with adjunctive mitomycin-C for complicated LASIK
flaps. J Cataract Refract Surg. 2005;31:291--6
101. Nagy ZZ, Hiscott P, Seitz B, et al. Clinical and morphological response to UV-B irradiation after excimer laser
photorefractive keratectomy. Surv Ophthalmol. 1997;42:
S64--76
102. Nassaralla BA, McLeod SD, Nassaralla JJ. Prophylactic
mitomycin C to inhibit corneal haze after residual
myopia following radial keratotomy. J Refract Surg.
2007;23:226--32
103. Nassiri N, Farahangiz S, Rahnavardi M, et al. Corneal
endothelial cell injury induced by mitomycin-C in photorefractive keratectomy: nonrandomized controlled trial.
J Cataract Refract Surg. 2008;34:902--8
104. Netto MV, Barreto J, Santo R, et al. Synergistic effect of
ethanol and mitomycin C on corneal stroma. J Refract
Surg. 2008;24:626--32
105. Netto MV, Chalita MR, Krueger RR. Corneal haze
following PRK with mitomycin C as a retreatment versus
prophylactic use in the contralateral eye. J Refract Surg.
2007;23:96--8
106. Netto MV, Mohan RR, Ambrosio R, et al. Wound healing in
the cornea. A review of refractive surgery complications
and new prospects for therapy. Cornea. 2005;24:509--22
107. Netto MV, Mohan RR, Sinha S, et al. Effect of prophylactic
and therapeutic mitomycin C on corneal apoptosis, cellular
proliferation, haze, and long-term keratocyte density in
rabbits. J Refract Surg. 2006;22:562--74
108. Netto MV, Wilson SE. Indications for excimer laser surface
ablation. J Refract Surg. 2005;21:734--41
109. Nuyts RM, Felten PC, Pels E, et al. Histopathologic effects
of mitomycin C after trabeculectomy in human glaucomatous eyes with persistent hypotony. Am J Ophthalmol.
1994;118:225--37
110. Nuyts RM, Pels E, Greve EL. The effects of 5-fluorouracil
and mitomycin C on the corneal endothelium. Curr Eye
Res. 1992;11:565--70
111. O’Brart DP, Patsoura E, Jaycock P, et al. Excimer laser
photorefractive keratectomy for hyperopia: 7.5-year followup. J Cataract Refract Surg. 2005;31:1104--13
112. O’Brart DPS, Mellington F, Jones S, Marshall J. Laser
epithelial keratomileusis for the correction of hyperopia
using a 7.0-mm optical zone with the Schwind ESIRIS laser.
J Refract Surg. 2007;23:343--54
O’Doherty M, Kirwan C, O’Keeffe M, O’Doherty J. Postoperative pain following epi-LASIK, LASEK, and PRK for
myopia. J Refract Surg. 2007;23:133--8
Occleston NL, Daniels JT, Tarnuzzer RW, et al. Single
exposures to antiproliferatives: long-term effects on ocular
fibroblast wound-healing behaviour. Invest Ophthalmol Vis
Sci. 1997;38:1998--2007
Panda A, Peer J, Aggarwal A, et al. Effect of topical
mitomycin C on corneal endothelium. Am J Ophthalmol.
2008;145:635--8
Perez-Santonja JJ, Sahla HF, Alio JL. Evaluation of
endothelial cells changes one year after excimer laser in
situ keratomileusis. Arch Ophthalmol. 1997;115:841--6
Pfister RR. Permanent corneal edema resulting from the
treatment of PTK corneal haze with mitomycin: a case
report. Cornea. 2004;23:744--7
Pietilä J, Mäkinen P, Uusitalo H. Repeated photorefractive
keratectomy for undercorrection and regression. J Refract
Surg. 2002;18:155--61
Pogrebniak HW, Matthews W, Pass HI. Chemotherapy
amplifies production of tumor necrosis factor. Surgery.
1991;110:231--7
Porges Y, Beh-Haim O, Hirsh A, Levinger S. Phototherapeutic keratectomy with mitomycin C for corneal haze
following photorefractive keratectomy for myopia. J Refract
Surg. 2003;19:40--3
Pritsos CA, Sartorelli AC. Generation of reactive oxygen
radicals through bioactivation of mitomycin antibiotics.
Cancer Res. 1986;46:3528--32
Qazi MA, Johnson TW, Pepose JS. Development of lateonset subepithelial corneal haze after laser-assisted subepithelial keratectomy with prophylactic intraoperative
mitomycin-C. Case report and literature review. J Cataract
Refract Surg. 2006;32:1573--8
Rajan MS, O’Brart DPS, Patmore A, Marshall J. Cellular effects
of mitomycin-C on human corneas after photorefractive
keratectomy. J Cataract Refract Surg. 2006;32:1741--7
Rajan MS, Watters W, Patmore A, Marshall J. In vitro
human corneal model to investigate stromal epithelial
interactions following refractive surgery. J Cataract Refract
Surg. 2005;31:1789--801
Rang HP, Dale MM. Quimioterapia anticancerı́gena, in
Rang HP, Dale MM. Farmacologı́a. Madrid, Churchill
Livingstone, 1995. ed 2; pp 846--70.
Ribeiro JC, McDonald MB, Lemos MM, et al. Excimer laser
photorefractive keratectomy after radial keratotomy.
J Refract Surg. 1995;11:165--9
Rockwell S, Kim SY. Cytotoxic potential of monoalkylation
products between mitomycins and DNA: studies of
decarbamoyl mitomycin C in wild-type and repair-deficient
cell lines. Oncol Res. 1995;7:39--47
Roh DS, Cook AL, Rhee SS, et al. DNA cross-linking,
double-strand breaks and apoptosis in corneal endothelial
cells after a single exposure to mitomycin-C. Invest
Ophthalmol Vis Sci. 2008;49(11):4837--43
Rozsı́val P, Feuermannová A. Retreatment after photorefractive keratectomy for low myopia. Ophthalmology.
1998;105:1189--92
Sadeghi HM, Seitz B, Hayashi S, et al. In vitro effects of
mitomycin C on human keratocytes. J Refract Surg. 1998;
14:534--40
Sari A, Onol M, Ozdek S, et al. Effect of mitomycin C on
ciliary body and intraocular pressure with various application depths: an experimental study. Clin Experiment
Ophthalmol. 2005;33:169--75
Schipper I, Suppelt C, Gebbers JO. Mitomycin C reduces
scar formation after excimer laser (193 nm) photorefractive keratectomy in rabbits. Eye. 1997;11:649--55
Schraermeyer U, Diestelhorst M, Bieker A, et al. Morphologic proof of the toxicity of mitomycin C on the ciliary
body in relation to different application methods. Graefes
Arch Clin Exp Ophthalmol. 1999;237:593--600
113.
114.
115.
116.
117.
118.
119.
120.
121.
122.
123.
124.
125.
126.
127.
128.
129.
130.
131.
132.
133.
502
Surv Ophthalmol 54 (4) July--August 2009
134. Senoo T, Joyce NC. Cell cycle kinetics in corneal
endothelium from old and young donors. Invest Ophthalmol Vis Sci. 2000;41:660--7
135. Seong GJ, Park C, Kim CY, et al. Mitomycin-C induces the
apoptosis of human Tenon’s capsule fibroblast by activation of c-Jun N-terminal kinase 1 and caspase-3 protease.
Invest Ophthalmol Vis Sci. 2005;46:3545--52
136. Shah S, Doyle SJ, Chatterjee A, et al. Comparison of 18%
ethanol and mechanical debridement for epithelial removal before photorefractive keratectomy. J Refract Surg.
1998;14:S212--4
137. Shah S, Sarhan ARS, Doyle SJ, et al. The epithelial flap for
photorefractive keratectomy. Br J Ophthalmol. 2001;85:393--6
138. Shaikh NM, Wee CE, Kaufman SC. The safety and efficacy
of photorefractive keratectomy after laser in situ keratomileusis. J Refract Surg. 2005;21:353--8
139. Skolnick AC, Grimmett MR. Management of pterygium. In
Krachmer JH, Mannis MJ, Holland EJ (eds): Cornea.
Philadelphia, PA, Elsevier Mosby, ed 2. 2005, pp. 1873--92
140. Smith S, D’Amore PA, Dreyer EB. Comparative toxicity of
mitomycin C and 5-fluorouracil in vitro. Am J Ophthalmol.
1994;118:332--7
141. Solomon R, Donnenfeld ED, Perry HD. Photorefractive
keratectomy with mitomycin C for the management of
a LASIK flap complication following a penetrating keratoplasty. Cornea. 2004;20:403--5
142. Solomon R, Donnenfeld ED, Thimons J, et al. Hyperopic
photorefractive keratectomy with adjunctive topical mitomycin C for refractive error after penetrating keratoplasty
for keratoconus. Eye Contact Lens. 2004;30:156--8
143. Song JS, Kim JH, Yang M, et al. Concentrations of
mitomycin C in rabbit corneal tissue and aqueous humor
after topical administration. Cornea. 2006;25:S20--3
144. Song JS, Kim JH, Yang M, et al. Mitomycin C concentration in
cornea and aqueous humor and apoptosis in the stroma after
topical Mitomycin-C application. Effects of Mitomycin-C
application time and concentration. Cornea. 2007;26:461--7
145. Spadea L, Sabetti L, D’Alessandri L, Balestrazzi E. Photorefractive keratectomy and LASIK for the correction of
hyperopia: 2-year follow-up. J Refract Surg. 2006;22:131--6
146. Srinivasan S, Drake A, Herzig S. Photorefractive keratectomy with 0.02% mitomycin C for treatment of residual
refractive errors after LASIK. J Refract Surg. 2008;24:S64--7
147. Steinert RF, Ashrafzadeh A, Hersh PS. Results of phototherapeutic keratectomy in the management of flap striae
after LASIK. Ophthalmology. 2004;111:740--6
148. Stojanovic A, Nitter TA. Correlation between ultraviolet
radiation level and the incidence of late-onset corneal haze
after photorefractive keratectomy. J Cataract Refract Surg.
2001;27:404--10
149. Tabbara KF, El-Sheikh HF, Sharara NA, Aabed B. Corneal
haze among blue eyes and brown eyes after photorefractive
keratectomy. Ophthalmology. 1999;106:2210--5
150. Talamo JH, Gollamudi S, Green WR, et al. Modulation of
corneal wound healing after excimer laser keratomileusis
using topical mitomycin C and steroids. Arch Ophthalmol.
1991;109:1141--6
151. Taneri S, Feit R, Azar DT. Safety, efficacy and stability
indices of LASEK correction in moderate myopia and
astigmatism. J Cataract Refract Surg. 2004;30:2130--7
152. Taneri S, Koch JM, Melki SA, Azar DT. Mitomycin-C assisted
photorefractive keratectomy in the treatment of button-
TEUS ET AL
153.
154.
155.
156.
157.
158.
159.
160.
161.
162.
163.
164.
165.
166.
167.
168.
169.
holed laser in situ keratomileusis flaps associated with
epithelial ingrowth. J Cataract Refract Surg. 2005;31:2026--30
Taneri S, Zieske JD, Azar DT. Evolution, techniques,
clinical outcomes and pathophysiology of LASEK: Review
of the literature. Surv Ophthalmol. 2004;49(6):576--602
Teus MA, de Benito-Llopis L, Sánchez-Pina JM. LASEK
versus LASIK for the correction of moderate myopia.
Optom Vis Sci. 2007;84:605--10
Teus MA, de Benito-Llopis L. LASEK with MMC to treat
post-LASIK myopic regression. J Cataract Refract Surg.
2007;33:1674--5
Thornton I, Puri A, Xu M, Krueger RR. Low-dose
mitomycin C as a prophylaxis for corneal haze in myopic
surface ablation. Am J Ophthalmol. 2007;144:673--81
Thornton I, Xu M, Krueger RR. Comparison of standard
(0.02%) and low dose (0.002%) mitomycin C in the
prevention of corneal haze following surface ablation for
myopia. J Refract Surg. 2008;24:S68--76
Torres RM, Merayo-Lloves J, Daya SM, et al. Presence of
mitomycin-C in the anterior chamber after photorefractive
keratectomy. J Cataract Refract Surg. 2006;32:67--71
Trattler W, Salz JJ. Surface ablation over LASIK flaps. Int
Ophthalmol Clin. 2006;46:117--22
Varley GA, Huang D, Rapuano CJ, et al. LASIK for
hyperopia, hyperopic astigmatism, and mixed astigmatism.
A report by the American Academy of Ophthalmology.
Ophthalmology. 2004;111:1604--17
Verweij J, Pinedo HM. Mitomycin C: mechanism of action,
usefulness and limitations. Anticancer Drugs. 1990;1:5--13
Vigo L, Scandola E, Carones F. Scraping and mitomycin C
to treat haze and regression after photorefractive keratectomy for myopia. J Refract Surg. 2003;19:449--54
Wallau AD, Campos M. Photorefractive keratectomy with
mitomycin C versus LASIK in custom surgeries for myopia:
a bilateral prospective randomized clinical trial. J Refract
Surg. 2008;24:326--36
Wang SL, Han JF, He XY, et al. Genetic variation of human
cytochrome p450 reductase as a potential biomarker for
mitomycin C-induced cytotoxicity. Drug Metab Dispos.
2007;35:176--9
Weisenthal RW, Salz J, Sugar A, et al. Photorefractive
keratectomy for treatment of flap complications in laser in
situ keratomileusis. Cornea. 2003;22:399--404
Wu KY, Hong SJ, Huang HT, et al. Toxic effects of
mitomycin-C on cultured corneal keratocytes and endothelial cells. J Ocul Pharmacol Ther. 1999;15:401--11
Xu H, Liu S, Xia X, et al. Mitomycin C reduces haze
formation in rabbits after excimer laser photorefractive
keratectomy. J Refract Surg. 2001;17:342--9
Yee RW, Yee SB. Update on laser subepithelial keratectomy
(LASEK). Curr Opin Ophthalmol. 2004;15:333--41
Zhao LQ, Wei RL, Ma XY, Zhu H. Effect of intraoperative
mitomycin-C on healthy corneal endothelium after laserassisted subepithelial keratectomy. J Cataract Refract Surg.
2008;34:1715--9
The authors reported no proprietary or commercial interest in
any product mentioned or concept discussed in this article.
Reprint address: Dr Laura de Benito-Llopis, Vissum Madrid,
Santa Hortensia 58, 28002 Madrid, Spain. E-mail: lbenito@
vissum.com.