CROSS-SECTIONAL ECHO IN PDA/Sahn and Allen
dimensional technique for evaluating congenital heart disease.
Circulation 57: 503, 1978
7. Weyman A, Wann S, Feigenbaum H, Dillon J: Mechanism of
abnormal septal motion in patients with right ventricular
8.
9.
10.
l
.
12.
343
Med 63: 41, 1977
13. Matsumoto M, Matsuo H, Nagata S, Hamanaka Y, Fujita T,
Kawashima V, Nimura Y, Abe H: Visualization of Ebstein's
anomaly of the tricuspid valve by two-dimensional and standard echocardiography. Circulation 53: 69, 1976
14. Hirschklau M, Sahn D, Hagan A, Williams D, Friedman W:
Cross-sectional echocardiography: Ebstein's anomaly. Am J
Cardiol 40: 400, 1977
15. Lev M, Liberthson R, Joseph R, Seten C, Kunske R, Eckner F,
Miller R: The pathologic anatomy of Ebstein's disease. Arch
Pathol 90: 334, 1970
16. Lieppe W, Scallion R, Behar V, Kisslo J: Two-dimensional
echocardiographic findings in atrial septal defect. Circulation
56: 447, 1977
17. Lieppe W, Behar V, Scallion R, Kisslo J: Detection of tricuspid
regurgitation with two-dimensional echocardiography and
peripheral vein injections. Circulation 57: 128, 1978
volume overload: A cross-sectional echocardiographic study.
Circulation 54: 179, 1976
Milner S, Meyer R, Venables A, Korfhagen J, Kaplan S:
Mitral and tricuspid valve closure in congenital heart disease.
Circulation 53: 513, 1976
Lundstrom N: Echocardiography in the diagnosis of Ebstein's
anomaly of the tricuspid valve. Circulation 47: 597, 1973
Farooki Z, Henry J, Green E: Echocardiographic spectrum of
Ebstein's anomaly of the tricuspid valve. Circulation 53: 63,
1976
Kotler MN: Tricuspid valve in Ebstein's anomaly. Circulation
49: 194, 1974
Meyer R: Echocardiography in congenital heart disease. Am J
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Real-time Cross-sectional Echocardiographic
Imaging and Measurement
of the Patent Ductus Arteriosus
in Infants and Children
DAVID J. SAHN, M.D.,
AND
HUGH D. ALLEN, M.D.
SUMMARY While echocardiography has been used to noninvasively document indirect effects on the heart of left-to-right
shunting through a patent ductus arteriosus, no noninvasive technique has been developed to image the duct itself. In this
study, 35 sequential studies were performed on 28 patients with a mechanical sector scanner to image the distal pulmonary
artery and its bifurcation by scanning along the axis of the right ventricular outflow tract. Cross-sectional imaging, just
superior to the take-off of the right pulmonary artery, provided visualization of the patent ductus as a distal continuation of
the pulmonary artery connecting to the descending aorta. Ductal visualization by cross-sectional echo was validated by
saline echo contrast observations of right-to-left and left-to-right shunting through the duct in 14 patients, by surgical observations in 11, angiographic observations in 13 and autopsy observations in three. Angiographic size of the ductus arteriosus,
whether constricted or widely patent, tortuous or straight, was predicted correctly and echo/angiographic correlations for
smallest inner ductal dimension were excellent (r 0.97). This study provides a method for and validates the direct imaging
of the ductus arteriosus and suggests that cross-sectional echocardiography can accurately predict ductal contour and quantitative ductal cross-sectional size noninvasively.
=
PATENT DUCTUS ARTERIOSUS, a common
condition in pediatric patients, has recently assumed
major importance as a life-threatening disease of
small premature infants, who now survive due to advances in neonatology. -4 While in an older child, the
classical physical findings of ductus arteriosus and the
minimal risk of surgery have at times obviated the
need for compulsory catheterization before ductal
ligation, atypical physical findings and the presence of
concomitant respiratory disease in premature infants
have often created problems of ductal identification,
as well as problems in determining which infants
might benefit by ductal closure.
From the Department of Pediatrics, University of Arizona
Health Sciences Center, Tucson, Arizona.
Address for reprints: David J. Sahn, M.D., Department of
Pediatrics, University of Arizona Health Sciences Center, Tucson,
Arizona 85724.
Received November 21, 1977; revision accepted March 23, 1978.
Echocardiography has achieved importance in
assessing the hemodynamics of ductal shunting by
demonstrating quantitative left atrial enlargement
and/or left ventricular enlargement in premature infants, and has been most important when serially
applied to the same infant throughout his course.58
Nonetheless, many of the M-mode echocardiographic
features can be mimicked by sepsis,8 hypoglycemia,
hypervolumia or severe anemia in premature infants,
and are nonspecific for ductal shunting. Recently, concern has been expressed over the failure to identify infants who have ductal shunting without an audibly
detectable murmur.9 In order to aid in the detection
and serial followup of these infants, our laboratory
recently developed an arterial saline echo contrast
technique for identification of left-to-right shunting
patent ductus arteriosus.'0 Unfortunately, this latter
technique requires the presence of an umbilical
arterial catheter above the level of the diaphragm,
344
CIRCULATION
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
identifies only left-to-right shunting patent ductus
arteriosus and cannot demonstrate a balanced or
right-to-left shunt through an equally large ductus.
None of the available noninvasive techniques directly
demonstrate the anatomy of the area of concern - the
ductus itself. Rapid identification of the infant who
can benefit from a ductal closure is becoming increasingly important, in view of the potential of using
prostaglandin inhibitors to noninvasively induce ductal constriction. Additionally, while echocardiographic indices of left atrial size have been of
assistance in following medical manipulation of the
patent ductus, these measures are affected by other
hemodynamic changes8 and are nonspecific and indirect indicators of ductal patency. As such, the need
has not been met for a specific technique to follow
noninvasively the effects of these drugs on the ductus."1' 12 Accordingly, we have applied a high frequency portable real-time cross-sectional echocardiographic system to the identification and direct
measurement of the ductus arteriosus and the
visualization of right-to-left and left-to-right shunting
through the ductus using saline contrast echocardiographic techniques.'3
Methods
Patient Population
Thirty-five serial cross-sectional echocardiographic
studies were performed on 28 patients, five of whom
underwent postoperative cross-sectional echocardiographic examinations as well. Patients could Se
subdivided into four groups:
Group A
Group A consisted of three infants with hypoplastic
left heart syndrome proven by autopsy as well as confirmed premortem by cardiac catheterization in
one. The infants had a mean age of 5 days (range 1
to 6 days) and a mean weight of 3,010 g (range
2,910-3,245 g). They were all initially evaluated
by single crystal echo within the first week of life,
the oldest surviving five and one-half weeks. Crosssectional echocardiograms were performed in the
week before death on all infants and the inner ductus
diameter was compared to postmortem measurements.
Group B
Group B consisted of 13 premature infants whose
mean age at study was 2.2 days (range 22 hours-14
days). Mean weight in Group B infants was 1,557 g
(range 625-1,870 g). In each, the cross-sectional
echocardiogram was performed at the first initial
suspicion of a ductus identified by the neonatologist,
either by increasing pulses, precordial activity or the
presence of a murmur compatible with a ductus
arteriosus. Nine of these infants with indwelling umbilical arterial catheters had ductus presence and
shunting confirmed by visualization of shunting on the
M-mode suprasternal contrast echo.'0 This was also
confirmed on the cross-sectional echocardiogram in
VOL 58, No 2, AUGUST 1978
real-time by saline contrast passing through the duct
from the aortic end to the pulmonary artery end after
descending aortic contrast injection. Two of the
patients had right-to-left ductal shunting, visualized
after peripheral venous contrast injections with echo
contrast material passing from the duct, right-to-left,
into the descending aorta. Six infants subsequently underwent operative ductal ligation because of unremitting congestive heart failure and had their ductus confirmed at surgery. Three of these infants underwent
cross-sectional echocardiography in the postoperative
period. As such, only one infant of the 13 did not have
ductal patency verified by contrast'0 or by surgical
observation. This infant had a continuous murmur
and bounding pulses at the time of his echo.
Group C
Eight older patients, with an uncomplicated ductus
arteriosus (mean age 3.2 years, range 4 months-7
years) (mean weight 14.7 kg, range 3.8-23.2 kg), underwent ductal imaging by cross-sectional echocardiography on the day before cardiac catheterization to
provide angiographic/echocardiographic correlations.
Five of these subsequently underwent elective ductal
ligations. Two patients had echo saline contrast
studies performed in the catheterization laboratory for
verification of ductal identification and one had a
postoperative cross-sectional echo study.
Group D
Four additional infants with catheterization-proven
coarctation of the aorta undergoing aortography
before coarctectomy were selected for study to provide
visualization of the juxtaductal area. They had a mean
weight of 2.3 kg, range 1.8-3.1 kg, and were studied
between 3 weeks-41/2 months of age, mean age 42
days. All had spontaneously closed ductus, both by
echo and by angiography, and therefore provided
verification of the spontaneously closed duct.
Control Group
Cross-sectional echocardiograms were then
reviewed retrospectively from 125 children (age 1
day-16 years) who had been proven angiographically
not to have a ductus arteriosus. Their two-dimensional
echoes had been performed before the development of
our ductus examination technique and were reviewed
in an attempt to identify false positives. In only 45 of
these patients had the scanning procedure included
visualization of the juxtaductal area, and so the comprehensively evaluated control group actually consisted of 45 patients.
Methods
Unsedated patients were studied in the supine position with a real-time cross-sectional echocardiographic system, a 300 mechanical sector scanner
(the Smith Kline Ekosector 1), using a 3½/2MHz or a 5
MHz transducer, both focused at 4 cm to provide
maximal lateral resolution in the area of greatest in-
345
CROSS-SECTIONAL ECHO IN PDA/Sahn and Allen
Ant
R +~~ L
Post
-R. Ventricle
_N
-.7-
-Aorta
I L. Pulmonary Art.
R.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
a
uava /Netf
sup. vena e,%-.,c,..-
I1
xl---
__,_
-' \Patent Ductus
Arteriosus
Aorta
A
,4~Desc.
P. Pulmonary Art.
Pulmonary Veins
i
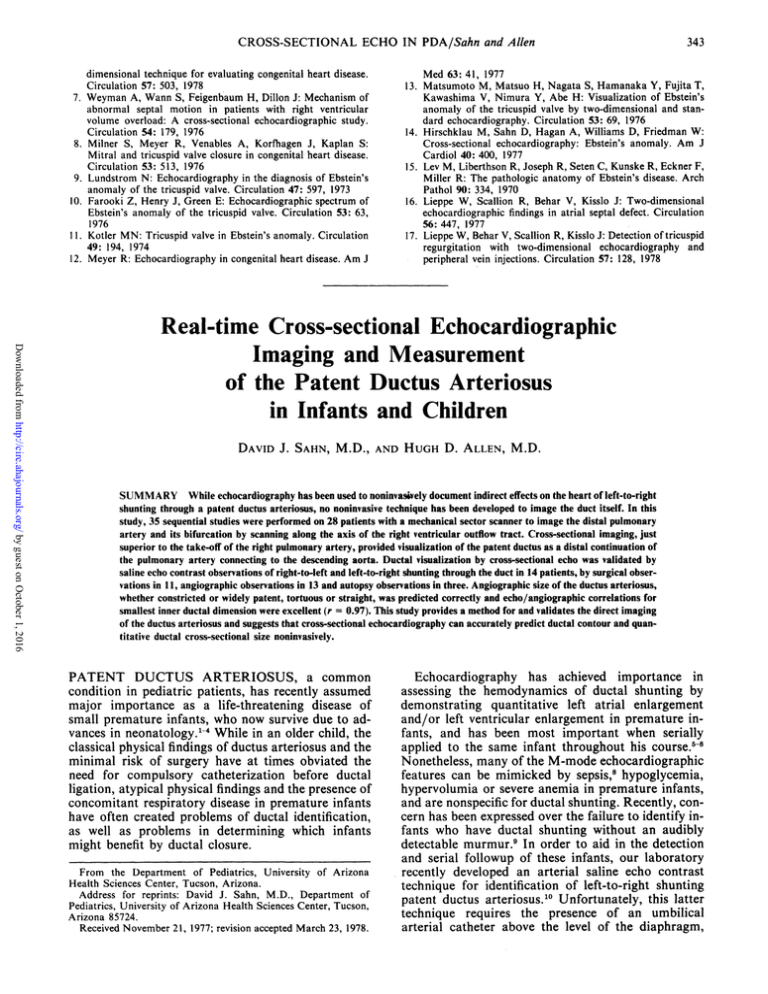
FIGURE 1. Schematic drawing of the anatomy of the right ventricular outflow tract plane. The great
arteries (aorta and pulmonary artery) are cut along the plane of the right ventricular outflow tract and
viewed as if one were standing at the patient's feet and looking at the heart from below. The orientation of
the image and of all the echoes in this paper are as shown in the compass. R right; L left;
Ant = anterior; Post posterior; Sup = superior; Art = artery; Desc = descending.
=
=
terest. The transducer oscillates at 30 cycles/sec,
producing a 30° sector scan with 120 lines per frame
and a frame rate of 30 full frames per second with high
line density over the limited area of interest. A three
lead ECG was recorded simultaneously for timing
purposes on all examinations. The system is portable
and has a self-contained videotape recorder which
records, without an intervening video camera, direct
image information in analog format which is replayed
on the oscilloscope of the instrument itself. This
provides for discrete frame-by-frame analysis without
loss of resolution due to optical conversion to video
format. Problems arise in illustrating all the crosssectional observations with selected still frames. As
usual, the videotapes and movies of the examinations
are more convincing than the illustrations provided in
this paper.
A generous amount of airless contact gel was placed
on the chest. Next, the transducer was placed lightly
on the left precordium in the third intercostal space
and directed along the line of the left ventricular outflow tract to scan the long axis of the aorta. The plane
of scanning was gradually rotated toward the left
shoulder and the transducer was tilted somewhat
superiorly to scan a more superiorly directed plane
along the line of the right ventricular outflow tract to
image the pulmonary artery wrapping around the aorta, the distal main pulmonary artery and the bifurcation of the pulmonary artery into its right and left
branches'4, 15 (figs. 1 and 2). As the transducer was
Normal Great Vessel
Orientation
Ant
A>PV
IN
I
I..
FIGURE 2. Echo still frame shows imaging of the distal
main pulmonary artery (MPA) and the origin of the left
pulmonary artery (LPA) in a normal patient. The back wall
of the pulmonary artery at the point of bifurcation is well
seen. R
right; L left; Ant anterior; Post posterior;
P V pulmonary valve; AO aorta.
=
=
=
L
R
Pst
Pc
VOL 58, No 2, AUGUST 1978
CI RCULATION
346
F
B
AAnt
R +L
Post
iI
!.- -Z..
A
MPA
AORPA A
AO
oLPA
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
a
PA
PDA
DESC AO
FIGURE 3. Two stillframe echo images show identification of patent ductus arteriosus (PDA). From the
scan plane of the main pulmonary artery (MPA) and its bifurcation (panel A, left) the scan plane is rotated
slightly superiorly to the plane of the duct us arteriosus (panel B, right). R = right; L left; Ant - anterior;
Post posterior; AO aorta, RPA right pulmonary artery; LPA = left pulmonary artery; DESC
A O descending aorta.
=
=
=
rotated superiorly from this position, the ductus arteriosus was most often visualized as a distal continuation
of the pulmonary artery space continuing posteriorly
to the echo image of the descending aorta. The duct
usually continued in the curvature of the main
pulmonary artery posteriorly with a gradual angle
superiorly and toward the right (fig. 3). When ductal
visualization was achieved, fine reject and damping
controls and overall gain of the instrument were adjusted to provide minimal background noise while imaging what was felt to be the ductal endothelium and
the smallest inner ductal dimension. The studies were
recorded in real-time and were evaluated by two
observers in real-time, in slow motion and using
frame-by-frame analysis on the analog videotape
recorder as well as on Super 8 mm motion picture film
and Polaroid stills. Measurements of ductal size
(smallest inner echo dimension) were performed using
the calibration standard on the two-dimensional echo
image. Little variation of ductal size with the phase of
the cardiac cycle was apparent on our images.
Nevertheless, all measurements were made during
mid-diastole.
With regard to the mechanical sector scanner examination of premature infants, we initially approached this examination with great trepidation,
since on the only previous occasion when we were
forced to use this technique (a 600 g premature infant
with tricuspid atresia) the mechanical sector scanner
produced reddening of the infant's chest and minor
abrasions on the precordium. This experience
suggested that we should accomplish this examination
with essentially little or no transducer contact to the
infants' chest, while the weight of a light mechanical
transducer was supported by the examiner's hand. As
a result, no significant mechanical abrasion or vibration was transmitted to the infants during the performance of this study, with the exception of minimal
reddening of the examined area after the sector scan
was performed. No complications occurred.
Contrast Echocardiographic Techniques
In nine Group B premature infants, as well as two
older children in the catheterization laboratory, saline
contrast verification of ductal shunting was obtained
by injection of saline into the descending aorta, an
arterial saline contrast technique as previously
described.10 16 In the premature infants, during the
sector scan echocardiogram, three consecutive 1 cc
boluses of sterile D5 in ¼h normal saline were hand injected rapidly into the umbilical-aortic catheter using
a 5 cc syringe while the ductus was imaged at high reject, low gain and images recorded on the videotape
recorder. Contrast injections were identified vocally
by the word "'inject" recorded on the audio channel.
These sequences were then reviewed in slow motion at
the bedside. After performance of the arterial saline
contrast study, the catheter was pulled down into the
descending aorta well below the level of the renal
arteries.
In the two older patients, cardiac catheters which
had been passed through the ductus into the aorta
were flushed with 5 cc of sterile heparinized saline and
a contrast echo similarly recorded.
Four premature infants with severe respiratory distress syndrome and cross-sectionally identified patent
ductuses underwent venous saline contrast injections
as well."6 In three of these patients, the venous injection was adequate (contrast eventually was visualized
within the pulmonary artery).
CROSS-SECTIONAL ECHO IN PDA/Sahn and Allen
347
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Angiographic Techniques
Autopsy Observations
Standard biplane cineangiograms were performed
in the eight patients undergoing cardiac catheterization with a clinical diagnosis of patent ductus
arteriosus. Seventy-six percent Renografin was injected into the juxtaductal aorta through catheters
which had been passed antegrade through the ductus
from the pulmonary artery and cineangiograms
recorded in AP and lateral or left and right anterior
oblique views. The catheter size was recorded and the
catheter image through the ductus was then used for
calibration to allow quantitative ductal measurements
from the angiograms. Since the catheter was passing
through the duct, it was subject to the same magnification as the duct itself. For measurement, ductal contours were then traced from the angiographic frames
along with the catheter dimensions. The smallest inner
ductal diameter was measured at the narrowest point
along the ductal silhouette on either the PA, lateral or
left anterior oblique angiogram, whichever showed the
ductus most clearly. In the infants with coarctation
(Group D), all had actually closed the ductus at the
time of catheterization, as confirmed by angiography.
The three infants with hypoplastic left heart (Group
A) and one of the infants with postoperative ligation
of a ductus arteriosus who had a postoperative crosssectional echocardiogram were examined postmortem. The position of the ductal ligature was the
only gross observation made in the premature infant
after ligation. In the other three infants with
hypoplastic left heart syndrome, the ductus was
opened longitudinally and the length of ductal circumference was measured with a millimeter ruler at
the smallest circumference. This was then divided by ir
to provide an estimate of the smallest inner ductal
diameter during life.
Surgical Observations
Because our primary interest was measuring ductal
luminal diameter and because the narrowest point was
often difficult to identify externally, surgical obser-
vations consisted only of verification of patency of the
ductus. No other surgical grading was attempted.
PDA Hypoplast ic
Left Heart
Ant
R+L
Post
AO DESC
PV
MN
-14
_S11 MPAS
fI WEE
may
Ad
_
AO5
r
-PDA
TAA
FIGURE 4. Patent ductus arteriosus (C PDA) and
hypoplastic left heart syndrome. A diminutive ctorta is seen.
The large pulmonary artery (MPA) di-stal to th e pulmonary
valve (PV) is well-seen and its connection to th e descending
aorta (DESC AO) by large PDA is imaged in ithis echocardiographic still frame. R
right; L
left; An t - anterior;
=
Post
arch.
=
posterior;
AO
aorta;
TAA
trans
verse aortic
Results
Group A: Ductal Imaging in Group A Hypoplastic Left Heart Syndrome
It is pertinent to review the appearance of the ductus arteriosus in hypoplastic left heart syndrome, since
the duct is almost always large and should be easily
imaged as a distal continuation of the pulmonary
artery. Figure 4 shows the echocardiographic
appearance of the ductus arteriosus in one of these infants. Historically, this female baby was quite important with regard to our study of ductal imaging. After
an initial evaluation where she demonstrated findings
compatible with complete mitral and aortic atresia
and extremely hypoplastic left ventricle by M-mode
echo, she survived for three weeks. It was apparent
that she was ductus-dependent for her systemic blood
flow and, by definition, must have had a large patent
ductus arteriosus. The identification of her ductus
represented our first successful ductal imaging and
suggested to us that the ductus could be visualized as a
direct distal continuation of the main pulmonary
artery. Ductus were imaged in all three of the infants
in Group A who had hypoplastic left heart syndrome.
Ductal dimensions in this group were 5 mm in two and
6 mm in the third. At autopsy, ductus dimension estimated in the three infants was 4.5 mm in one, 5 mm
in the second and 6 mm in the third. No infant later
requiring a ductus ligation had a ductal dimension less
than 3 mm.
Group B: Ductal
ImaginginGroupB-Prematurelnfants
Of the 13 infants studied to detect ductus arteriosus,
the duct could be visualized in all, with images similar
to that shown in figure 3, panel B (representing large
unconstricted ducts) or in figure 5, a constricted patent
ductus arteriosus. Ductal diameter ranged between 1.5
mm and 4.7 mm in the premature infant group. The
infants could be subcategorized, since only eight had
clinically large ductus at the time of echo, based on
pulmonary edema on x-rays, requirements for
prolonged ventilatory support, increased left atrial
diameter on M-mode echos and the requirement for
digitalis and fluid restriction. Left atrial/aortic ratio
for the large ducts was 1.33 ± 0.05 (SEM) compared to
1.03 + 0.04 (SEM) in the small ducts (P < 0.01). Mean
~-~ ~~ 8~ 2
VOL 58, No 2, AUGUST 1978
CIRCULATION
348
Ligated PDA
2 days post-op
Constricted PDA
Ant
vMMPA
lcm
L
% 1-*
PDkwmwPA
N%l
DescAo
DESC AO
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
FIGURE 5. A constricted patent duct us arteriosus (PDA) is
imaged in a premature infant. The dotted line shows the area
of measurement of smallest inner ductal dimension.
A 0 aorta; MPA main pulmonary artery; DESC
=
AO = descending aorta.
FIGURE 7. Imaging of the area of the patent ductus
arteriosus (PDA) after ligation shows a decrease in ductal
dimension as well as the position of the ligature. R = right;
L left; Ant anterior; Post posterior.
=
1.6r
1.4
1.2
0
0-4
1.0
0
6:
0.8
4:
0.6
=
Y= 1 .09 X +0 . 74
R=+O . 64
PSO.001
SEE=O. 1 1
04
0.2
0
0
0.5
1.0
1.5
2.0
2.5
3.0
3.5
4.0
4.5
PDA SIZE (MM)
FIGURE 6. Inner dimension of the patent ductus arteriosus (PDA) in millimeters (abscissa) is related to left
atrial/aortic ratio (LA/A 0 ratio) on the ordinate, both as measured on the initial echo in each of the 13
premature infants in group B. SEE the standard error of the estimate for the regression relationship shown
by the equation.
349
CROSS-SECTIONAL ECHO IN PDA/Sahn and Allen
patent ductus arteriosus size was 3.9 0.02 mm in the
group with large ducts compared to 2.4 ± 0.02 mm in
the group with small ducts (P < 0.01). However, left
atrial/aortic ratio correlated poorly with patent duc= 0.64) (fig 6). The linear
relationship in figure 6 shows much scatter and little
predictive ability. Nonetheless, the extrapolation to 0
mm ductal lumen occurred at a left atrial/aortic ratio
of 0.74.6' 8 Six of the infants subsequently required
ligation and postoperative echoes were obtained in
three of these infants (fig. 7). The position of the
ligature could be imaged echocardiographically in all
three infants, with minimal ductal lumens proximal
and distal to the point of ductal obliteration.
tus arteriosus size (r
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Group B: Contrast Studies
Nine of the infants had indwelling arterial catheters
placed above the diaphragm at the level of T6 at the
time of study. In all nine, the ductal visualizations
could be verified by seeing contrast material passing
from the descending aorta directly through the duct
into the pulmonary artery. Four of the infants had
peripheral IVs in place and had venous contrast
studies performed. Contrast material initially
appeared in the pulmonary artery successfully in
three; and, in two, a right-to-left shunt was seen with
contrast passing through the duct into the descending
aorta. Both of the infants who had right-to-left shunts
detected had clinically small ductus and significant
hyaline membrane disease with respirator dependency
at the time of the study. Figure 8 was derived from one
of the infants who had a bidirectional shunt through a
small patent ductus arteriosus proven by both arterial
and venous contrast studies. In figure 8, the ductus is
seen in panel A followed by left-to-right filling of the
ductus after an arterial contrast study (panel B). In
panel C, the same image is shown after peripheral
venous contrast injection filling the pulmonary artery
and the ductus. In later frames, contrast appeared in
the descending aorta. These two positive peripheral
venous injections represent the first successful
echocardiographic technique for identifying right-toleft ductal shunts. No temporal artery-descending aortic blood gas comparisons were available in the infants
to document or assess the magnitude of the right-toleft shunting.
Group C
Ductal visualizations were achieved successfully in
all eight of the older children studied before cardiac
catheterization. The inner dimension of the ductus
could be measured in all. Figure 9 shows the
angio/echo comparison of a patient with a large unconstricted ductus arteriosus which measured ap-
~~AntB
L
~~~~
A
-
R
PA
Post
AOt
icmjI
PV
~PDA
Vt
A
DESC AO
DESC MAOB
C
PA
--a&I
1
LA-
-PDA
-
DESC AO
__
-I
FIGURE 8. Imaging of a small ductus is visualized in panel A, left. Contrast opacification coming through
the duct us and into the pulmonary artery (PA ) is seen in the still frame panel B, after saline injection into the
descending aorta (DESC A 0). In panel C, contrast is visualized in the main pulmonary artery and in the patent ductus after peripheral venous saline contrast injection. All were derived from the same infant.
R
=
righ t,
L
left;
Ant
ductus arteriosus; LA
=
=
anterior; Post
left atrium.
=
posterior;
A 0
=
aorta; PV=
pulmonary valve;
PDA
=
patent
VOL 58, No 2, AUGUST 1978
CI RCULATION
350)
FI GURE 9. Echo still frame (right) and lateral angiocardiogram (left) are shown from a group C patient
with a large patent ductus arteriosus (PDA). The lateral plane angiocardiogram has been turned on its side
to approxinmate the orientation of the echo image. Actually, the echo image visualizes the structures in a
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
transverse
DESC
rather than
AO
a
lateral plane. R
descending
aorta; MPA
right; L = left; Ant = anterior;
pulmonary artery.
Post
=
posterior;
A 0
=
aorta;
main
proximately 7 mm inner dimension. Figure 10 shows
similar images in a patient with a constricted small patent ductus arteriosus (2.5 mm) which was minimally
larger than the diameter of a 7 French catheter shown
passing through it. Figure 11 shows the regression
analysis of echo vs angiographic dimension and
verifies that echo can quantitatively predict the
smallest inner ductal dimension quite reliably
(r - 0.97) with minimal overestimation of the smaller
ducts, as shown, suggested by the regression analysis
and its intercept. We believe this minimal overestimation represents some lack of endocardial visualization
because of echo dropout. Previous work from our lab
suggested a similar overestimation by echo of the
lumen size in supravalvar aortic stenosis.'7 This potential dropout may be substantiated by the approximate
I mm residual lumen apparent on the post-ligation
echoes in Group B. Nonetheless, the experience
verifies the quantitative accuracy of ductal imaging.
The two saline contrast injections during cardiac
catheterization in Group C patients visualized left-toright shunting through the ductal structure on echo.
Group D
Figure 12 demonstrates the visualization of the juxtaductal area of the descending aorta in an infant with
coarctation showing the configuration of a proven
spontaneously closed ductus and its orientation in
comparison to the shelf of the coarctation coming off
the back wall of the desending aorta. Images similar
to this were obtained in the other three infants in this
group and again verify that we are indeed imaging the
spontaneously closed ductus and the juxtaductal area
of the descending aorta.
Control Group
As stated in the Methods section, subsequent to the
specifically studied in this protocol, we reviewed
cross-sectional echocardiograms, retrospectively,
group
Ant
R+L
VMPA
AO
St
rPDA
*DESC AO
I~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~....
FI GURE 10. Lateral plane angiogeardiogram and echocardiographic still frame are shown from a patient
stricted patent ductus arteriosus (PDA). AO = aorta; MPA = main pulmonary artery; DESC AO =
descending
aorta.
CROSS-SECTIONAL ECHO IN PDA/Sahn and Allen
PDA SMALLEST INNER DIAMETER
8-
E
2
a
0
.
7
65-
z
4-
a)
a)
3-
2
2-
R = +0.96
SEE = 0.4mm
Y = 1.24X-1.4mm
aDownloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
1
2
3
5
4
6
7
8
PDA Diameter ECHO in mm
FI GURE 11. Echocardiographic (abscissa) vs angiographic
(ordinate) correlation for the measurement ofsmallest inner
dimension in mm is shown for the eight patients in group C.
Correlation coefficient (R), standard error of the estimate
(SEE) and the regression equation (IY) are shown.
from 125 children who had undergone echocardiography of the great arteries before cardiac
catheterization, and who subsequently were shown on
aortography or levophase angiography, if no other
Closed PDA
Coarctation
K It/ MPA
AO
Si
Ant
L
RPost
YtPoi nt of
Obliteration
-ASC AO
DESC AO
COARCT
FIGURE 12. A constricted (closed) patent ductus
arteriosus (PDA ) is visualized in a patient with aj]uxtaductal
coarctation (COA R CT). The coarctation itself is imaged as
a shelf between the ascending aorta (ASC AO) and the
descending aortas (DESC AO). R= right; L = left,
Ant anterior; Post posterior; AO aorta; MPA
main pulmonary artery.
=
=
35 1
shunts existed, not to have a patent ductus arteriosus.
In only 45 of these did the scan of the great arteries include the distal main pulmonary artery and views of
the descending aorta which were suitable for assessing
that the ductal area had been imaged. As such, of the
125 patients, only 45 were acceptable for this
retrospective evaluation. In 10 of the 45, images
suggesting a spontaneously closed ductus were obtained (all were infants under 7 months of age). In 34
of the 45 adequate examinations, no ductal structure
was imaged at all. In the last of these adequate examinations, however, actual ductal patency was
suggested and the examination would have been read
as a blind false positive for a small patent ductus
arteriosus if presented to us during the prospective
study. The angiogram of the infant in question, who
had a ventricular septal defect, showed a large ductus
diverticulum. The aortogram of the same infant did
not demonstrate a left-to-right patent ductus
arteriosus; this represents the single known false
positive for ductal imaging. The potential for echo
dropout producing false positive examinations, and
our inability to distinguish between a patent ductus
arteriosus less than 1.5 mm vs a closed patent ductus
arteriosus, are both problems further discussed in the
next section.
Discussion
The ability to image a ductus at all rests with the
lateral resolution of the instrument at the depth in
question. An examination of the individual echo lines
on our images suggests that in most patients, the ductal lumen continues the overall curvature of the
pulmonary artery posteriorly and slightly to the right,
passing around the aorta. Therefore, the ductus is
oriented almost parallel to the incident sound beam.
The smearing across of echoes from the bright back
walls of the pulmonary artery after its bifurcation
could completely obscure the ductal lumen and actually appears to do so when the gain is set too high or
the reject too low. Once, having imaged the area of the
ductus, echoes of the structure must be obtained at
varying gain and reject in an attempt to visualize not
only its outer contour but also its endothelial surfaces.
Having achieved direct ductal visualization, the
present study further established the quantitative accuracy of ductal imaging techniques and the ability of
the method to image both right-to-left and left-toright ductal shunts. In closely examining the results of
the ductal imaging studies in older children, it became
obvious that, once again, ductal images must be obtained at varying gains and rejects in an attempt to
produce the fine echoes within the ductal lumen at the
very time they appear. Overdamped echoes probably
demonstrate only the outer contour of the ductus
because of endothelial dropout and will overestimate
the angiographic size of the ductus, while underdamped studies may obscure the ductus completely.
The problem of endothelial dropout caused by overdamping probably accounts for overestimation of
those smaller ducts which might have been completely
missed at higher gain settings. Nonetheless, in view of
352
CIRCULATION
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
the lateral resolution characteristics of the instrument
in question, using a transducer focused at 4 cm, we
believe that ductus lying at a depth of between 3-7 mm
from the chest wall can probably be imaged with our
3.5 MHz system if they are greater than 1.5 mm in
diameter. Theoretically, our present technique cannot
distinguish between a lumen size of less than 1.5 mm
and a completely closed duct. Dynamic focusing and
higher frequencies in future instrumentation may
further alleviate this resolution limitation. While wide
angle (70-90°) sector scan instruments have recently
become available, high line density with good line
resolution over the limited juxtaductal region is required for accurate ductal imaging.
The direct but noninvasive detection of ductal
patency, as demonstrated in our study, can be applied
to pediatric cardiology in several important circumstances, some of which parallel the patient groups
that we studied. In the older child, the presence of the
duct itself probably warrants a surgical ligation.18
Many of these children with classical findings for ductus arteriosus may undergo ductal ligation without
cardiac catheterization. Catheterization is then
reserved for two groups of patients, those with
atypical physical findings where confusion may arise
between this lesion and venous hums, aorticopulmonary windows or coronary arteriovenous
malformations, or those patients in whom pulmonary
vascular resistance must be assessed. Since older
children may represent a group in which ductal imaging is at times difficult to obtain because the structure
is too small and far away, the inability to detect a ductus arteriosus on echo may not clarify the situation or
avoid the need for cardiac catheterization. Nonetheless, a detectable ductus imaged adequately by this
method may obviate the need for a catheterization in
some of these patients.
In children who have a patent ductus coexisting
with other forms of congenital heart disease, the
assessment of ductal patency by this technique may
also be quite important. In children with large ventricular septal defects, the murmur of the ventricular
septal defect may mask the associated presence of a
patent ductus arteriosus. Identification of concomitant large ductus arteriosus provides the opportunity
to significantly improve cardiovascular status, without
cardiopulmonary bypass, by performing ductal ligation early in some of these children. At cardiac
catheterization, the demonstration of the ductal shunt
itself in the presence of a ventricular septal defect requires an aortogram. Aortography can most often be
achieved by entering the aorta through the ventricular
septal defect from the right ventricle, but occasionally,
ruling out a large concomitant ductus requires a
retrograde left heart study, prolonging the cardiac
catheterization and entailing an added risk.19
Other infants with cyanotic forms of congenital
heart disease secondary to right ventricular inflow or
outflow tract obstruction may be ductus-dependent for
their pulmonary blood flow. Emergency cardiac
catheterization and possibly an infusion of prostaglandin E, if there are signs of decreasing ductal patency,
VOL 58, No 2, AUGUST 1978
are indicated for these babies.20 In these forms of
cyanotic heart disease, the duct is usually a smaller
structure and more tortuous in direction. Nonetheless,
we have recently encountered three infants (two with
pulmonary atresia and one with tricuspid atresia) in
whom ductal patency could be determined by our
technique. In one of these infants, the duct was imaged
quite well from the suprasternal notch.2'
While the surgical mortality of bedside ductal ligation performed in the nursery in premature infants
appears to be quite low, and initial reports suggest the
safety of producing noninvasive ductal constriction
with inhibitors of prostaglandin El synthetase, the
success of, for instance, indomethacin administration
in various reports appears to vary with patient selection.22 A reliable indicator for the selection of infants
who can benefit from medical therapy or ductal
closure still remains to be delineated.23 We believe that
the early diagnosis of ductal patency and images of
ductal contour using our technique may hold
prognostic significance. Figure 13 shows inner ductal
dimensions in our 13 premature infants related to their
subsequent course. Ductal dimensions were measured
at the time of initial study when the suspicion-of a ductus first arose. As shown, the infants who later required ductal ligation had a mean ductal dimension of
4.2 ± 0.2 mm. Those who subsequently had spontaneous closure had a mean ductal dimension of
2.6 ± 0.2 mm (P < 0.01). Further, as a corollary of
the difference in size, those requiring ligation appeared
to have unconstricted or uniform ducts, whereas those
with smaller inner duct dimensions had a duct which
appeared somewhat constricted in cross-sectional
visualization. No infant later requiring ligation had a
ductal dimension less than 3 mm on his initial echo,
and all with ductal dimensions below this had spontaneous closure of their duct detected clinically within
five days.
In -the face of the increasingly widespread administration of prostaglandin inhibitors to premature
infants, and in view of infants in all series who have on
clinical grounds experienced partial or incomplete
closure or only temporary closure", 12, 19 after indomethacin administration, it would be important to
demonstrate the actual effect on the ductus of the drug
administration in serial fashion. We believe that a
comprehensive approach to the evaluation of the
effects of prostaglandin inhibitors, which includes
direct assessment of ductal contour or size, as has
recently been achieved in animals,24 is an essential
precursor of the wide clinical application of these
compounds in humans.
Our study has demonstrated for the first time that
real-time cross-sectional echocardiography can be
used to provide direct imaging of the ductus arteriosus
in order to estimate its size and contour. From our
study it appears that in premature infants, inner ductal
dimension as well as contour on initial echo has
prognostic significance which may be quite important
in planning medical or surgical management. Ductus
imaging alone or in combination with echo contrast
techniques will be important not only for verification
CROSS-SECTIONAL ECHO IN PDA/Sahn and Allen
353
PDA IMAGING IN PREMATURE INFANNTS
r6 T
I
S
0
ooo I
4
0
Li
<
Lii
a
C
3
00 00
0
s-i
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
-J
'C
2
K1
OL>
(
1
REQUIRED LIGATION
PONTANE>JUSLY CLOSED
N=7
NUB
MEAN WGT L557
195
OMS
FIGURE 13. Individual patient values (open circles) and the group means (closed circles) ± one standard
(bars) are visualized for the six group B infants whose ducts required ligation compared to those who
subsequently experienced spontaneous closure. Mean inner ductal dimensions in mm between the two
groups were statistically different (P < 0.01) between the two groups. See text for discussion.
error
of the ductus existing in isolation, but also for patent
ductus in conjunction with other forms of congenital
heart disease where identification of the patent ductus
arteriosus is of major consequence and where it is
sometimes difficult to achieve without aortography.
References
1. Neal WA, Bessinger FB Jr., Hunt CE, Lucas R: Patent ductus
arteriosus complicating respiratory distress syndrome. J
Pediatr 86: 127, 1975
2. Zachman RD, Steinmetz GP, Botham RJ, Graven SN,
Ledbetter MK: Incidence and treatment of the patent ductus
arteriosus in the ill premature neonate. Am Heart J 87: 697,
1974
3. Siassi B, Emmanouilides GC, Cleveland RJ, Hirose F: Patent
ductus arteriosus complicating prolonged assisted ventilation in
respiratory distress syndrome. J Pediatr 74: 11, 1969
4. Kitterman JA, Edmunds LH, Gregory GA, Heymann MA,
Tooley WH, Rudolph AM: Patent ductus arteriosus in
premature infants: incidence, relation to pulmonary disease and
management. N Engl J Med 287: 473, 1972
5. Baylen RB, Meyer RA, Kaplan S, Ringenburg WE, Korfhagen
J: The critically ill premature infant with patent ductus
an echocardiographic
arteriosus and pulmonary disease
assessment. J Pediatr 86: 423, 1975
6. Silverman NH, Lewis AB, Heymann MA, Rudolph AM:
Echocardiographic assessment of ductus arteriosus shunt in
premature infants. Circulation 50: 821, 1975
7. Goldberg SJ, Allen HD, Sahn DJ: Pediatric and adolescent
echocardiography: a handbook. Chicago, Year Book Medical
Publishers, Inc, 1975, pp 77-80
-
8. Sahn DJ, Vaucher Y, Williams WE, Allen HD, Goldberg SJ,
Friedman WF: Echocardiographic detection of large left-toright shunts and cardiomyopathies in infants and children. Am
J Cardiol 38: 73, 1976
9. Thibeault DW, Emmanouilides GC, Nelson RJ, Lachman RS,
Rosengart RM, Oh W: Patent ductus arteriosus complicating
the respiratory distress syndrome in preterm infants. J Pediatr
86: 120, 1975
10. Allen HD, Sahn DJ, Goldberg SJ: A new serial contrast
technique for assessment of left-to-right shunting patent ductus
arteriosus in the neonate. Am J Cardiol 41: 288, 1978
11. Friedman WF, Hirschklau MJ, Printz MP, Pitlick PT,
Kirkpatrick SE: Pharmacologic closure of patent ductus
arteriosus in premature infants. N Engl J Med 295: 526, 1976
12. Heymann MA, Rudolph AM, Silverman NH: Closure of the
ductus arteriosus in premature infants by inhibition of
prostaglandin synthesis. N Engl J Med 295: 530, 1976
13. Gramiak R, Shalpe M, Kramer DH: Ultrasound cardiography
contrast studies in anatomy and function. Radiology 92: 939,
1969
14. Sahn DJ, Terry R, O'Rourke R, Leopold G, Friedman WF:
Multiple crystal cross-sectional echocardiography in the
diagnosis of cyanotic congenital heart disease. Circulation 50:
230, 1974
15. Henry WL, Maron BJ, Griffith JM, Redwood DR, Epstein SE:
Differential diagnosis of anomalies of the great arteries by realtime two-dimensional echocardiography. Circulation 51: 283,
1975
16. Sahn DJ, Allen HD, Mason M, Goldberg SJ: The utility of
contrast echocardiographic techniques in the care of critically
ill infants with cardiac and pulmonary disease. Circulation 56:
959, 1977
17. Williams DE, Sahn DJ, Friedman WF: Cross-sectional
354
18.
19.
20.
21.
CI RCULATION
echocardiographic localization of the sites of left ventricular
outflow tract obstruction. Am J Cardiol 37: 250, 1976
Ziegler RF: Patent ductus arteriosus. In Heart Disease in Infants, Children and Adolescents, edited by Moss AJ, Adams
FH. Baltimore, The Williams & Wilkins Co, 1968, p 338
Stanger P, Heymann MA, Tarnoff H, Kaufman J, Rudolph
AM: Complications of cardiac catheterizations in neonates, infants and children: a three-year study. Circulation 55: 95, 1974
Olley PM, Coceani F, Bodach E: E-type prostaglandins - a
new emergency therapy for certain cyanotic congenital heart
malformations. Circulation 53: 728, 1976
Sahn DJ, Allen HD, McDonald G, Goldberg SJ: Real-time
VOL 58, No 2, AUGUST 1978
cross-sectional echocardiographic diagnosis of coarctation of
the aorta: a prospective study of echocardiographicangiographic correlations. Circulation 56: 762, 1977
22. Neal WA, Kyle JM, Mullett MD: Failure of indomethacin
therapy to induce closure of patent ductus arteriosus in
premature infants with respiratory distress syndrome. J Pediatr
91: 621, 1977
23. Gersony WM: Commentary: Patent ductus arteriosus and the
respiratory distress syndrome - a perspective. J Pediatr 91:
624, 1977
24. Kirkpatrick SC, Printz MT, Friedman WF: Prostaglandins and
the fetal ductus arteriosus. (abstr) Pediatr Res 11: 394, 1977
Models of Congenital Heart Disease
in Fetal Lambs
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
NOEL H. FISHMAN, M.D., ROBERT B. HOF, M.D., ABRAHAM M. RUDOLPH, M.D.,
AND MICHAEL A. HEYMANN, M.D.
SUMMARY Intracardiac flow patterns were chronically altered by partially obstructing left ventricular (LV) inflow or
outflow in midgestational fetal lambs. Physiological measurements of the fetal circulation were made serially through indwelling catheters and the use of radioactive microspheres.
With LV inflow obstruction, mean LV output (LVO) decreased to 30% of control (P < 0.01). Within seven days, the
LV/right ventricular (RV) weight ratio decreased to 70% of control (P < 0.01), and the mean LV/RV chamber volume
decreased to less than one-half of control (P < 0.001), simulating an early form of the hypoplastic left heart syndrome.
With LV outflow obstruction, mean LVO decreased to 64% of control (P < 0.05). Mean LV/RV wall thickness doubled
(P < 0.0001) and mean LV/RV chamber volume decreased to less than one-half of control (P < 0.0001). Within four to ten
days after increasing LV afterload, a large increase in LV mass occurred, which was demonstrated by morphometric
analysis to be due to hyperplasia of ventricular myocytes. LV chamber volume decreased somewhat, simulating moderately
severe congenital aortic stenosis. Over the long term (30-36 days), the mean LV/RV weight ratio decreased and the LV
chamber was nearly obliterated, simulating very severe congenital aortic stenosis.
The results suggest that by varying preload and afterload in both ventricles of the fetus, various forms of congenital heart
disease may be simulated.
IT IS NOT KNOWN WHY the massive ventricular
enlargement associated with severe congenital aortic
or pulmonic stenosis cannot be duplicated experimentally in postnatal animals,' nor why the structure of
blood vessels is altered in fetuses with congenital heart
disease.2' I Improved understanding of early adaptation to a mechanical cardiovascular lesion should
come from development of fetal animal models in
which myocardial and vascular structure and function
as well as circulatory reflexes can be measured.
The possibility that non-genetic models of congenital heart disease could be induced in fetuses was
suggested by the observations of pathologists4 and experimental embryologists.5' 6 Lev et al.4 noted that the
hypoplastic left heart syndrome in human fetuses is
From the Departments of Surgery and Pediatrics, University of
California, San Francisco, San Francisco, California.
Supported by NIH grant HL 15798 and AHA grant 73-827.
Presented in part at the Philadelphia Academy of Surgery, as the
Samuel D. Gross Prize lecture, November 7, 1977.
Address for reprints: Noel H. Fishman, M.D., Department of
Surgery, University of California, San Francisco, California 94143.
Received January 27, 1978; revision accepted April 17, 1978.
often associated with premature closure of the
foramen ovale, and postulated that a decreased venous
return was responsible for arrest of the left ventricle in
those cases. Hahr et al.5 induced various forms of the
hypoplastic left heart syndrome in chick embryos by
obstructing flow through the left atrioventricular canal
with a tiny nylon plug. Subsequently, Shapiro et al.7
showed that constriction of the pulmonary artery
leads to marked thickening of the right ventricular
(RV) wall in the fetal lamb.
We selected the fetal lamb as the experimental
animal in which to attempt to induce models of congenital heart disease for several reasons. Fetal lambs
and humans are similar in weight and have similar
blood pressures, oxygen tensions, ventricular stroke
volumes, and internal distribution of blood flows at
corresponding stages of gestation.8 It is possible to
operate on lamb fetuses without precipitating abortion,9 10 and physiological measurements of circulatory function can be made in utero for days or
even weeks under normal physiological conditions
through indwelling catheters.9 11
A great deal of data has been accumulated from
chronically catheterized fetal lambs concerning nor-
Real-time cross-sectional echocardiographic imaging and measurement of the patent
ductus arteriosus in infants and children.
D J Sahn and H D Allen
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Circulation. 1978;58:343-354
doi: 10.1161/01.CIR.58.2.343
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1978 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/58/2/343
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/