Continuous Negative Extrathoracic Pressure and Positive End
advertisement

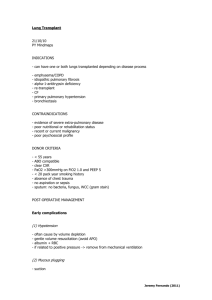
laboratory and animal investigations Continuous Negative Extrathoracic Pressure and Positive End-Expiratory Pressure* A Comparative Study in Escherichia coli Endotoxin-Treated Neonatal Piglets Thomas G. Mundie, PhD; Kuuleialoha Finn, PhD; Venkataraman Ralaraman, MRRS; Sneha Sood, MD; and David Easa, MD Recent clinical studies have suggested that improve¬ pulmonary gas exchange with the use of continuous negative extrathoracic pressure (CNEP) in conjunction with intermittent mandatory ventilation ment in (IMV) may be due to increased pulmonary blood flow. Accordingly, we investigated the effects of CNEP vs positive end-expiratory pressure (PEEP) in ventilated neonatal piglets after Escherichia coli endotoxin was administered to induce pulmonary hypertension. Two experimental groups of piglets with six in each, were subjected to three 30-min alternating periods.6 cm H20 CNEP with 6 cm H20 PEEP, beginning 2 h after endotoxin infusion. End-expiratory lung volume (EELV) increased similarly from baseline (13 ±2 mL/kg) with both CNEP (28 ± 2 mL/kg) and PEEP (29 ± 2 mL/kg). In addition, the increase in PaC>2 from baseline with CNEP (106 ± 9 to 135 ± 7 mm Hg) was similar to that with PEEP (114 ±11 to 132 ±6 mm Hg). Further, no differences were found in dynamic lung compliance, EELV, lung resistance, blood gas indexes, or hemodynamics, includ¬ Administered either by continuous negative extrathoracic pressure (CNEP) or positive end-ex¬ ^** piratory pressure (PEEP), end-expiratory pressure is used in conjunction with mechanical ventilation to normal lung volume. In addi¬ surface area for gas exchange, restoration of lung volume with end-expiratory pres¬ sure decreases pulmonary vascular resistance (PVR) restore and maintain tion to increasing the *From the Department of Clinical Investigation Tripler Army Medical Center (Dr. Mundie), and Department of Pediatrics Medical Center for Women and Children John A. Kapiolani Burns School of Medicine (Drs. Finn, Balaraman, Sood, and Easa), Honolulu. Supported by the US Army Health Services Command and Ka¬ Medical Center for Women and Children. The opinions piolani or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense. Manuscript received September 20, 1993; revision accepted May 6, 1994. Kapiolani Medical Center, Reprint requests: Dr. Easa, Punahou St., Honolulu, HI 96826 1319 ing transmural pulmonary artery pressure and pulmo¬ nary vascular resistance between CNEP and PEEP. With transpulmonary pressure and transrespiratory pres¬ sure equal, CNEP in tandem with IMV is physiologi¬ cally equivalent to PEEP and IMV. (Chest 1995; 107:249-55) Cdyn=dynamic lung compliance; CNEP=continuous neg¬ ative extrathoracic pressure; CO=cardiac output; EELV=end-expiratory lung volume; Fl02=fraction of in¬ spired oxygen; IMV=intermittent mandatory ventilation; MAP=mean arterial pressure; Ptp=transpulmonary pres¬ sure; Ptr=transrespiratory pressure; PAP=pulmonary ar¬ tery pressure; PAPtm=transmural PAP; Pao=airway open¬ ing pressure; PEEP=positive end-expiratory prsesure; Pes=esophageal pressure; PVR=pulmonary vascular resis¬ tance; Rl= lung resistance; SVR=systemic vascular resis¬ tance; Vt= tidal volume; ZEEP=zero end-expiratory pres¬ sure negative extrathoracic pressure; end-expiratory lung volume; pulmonary hypertension Key words: continuous to stinting of extra-alveolar pulmonary blood vessels.1 However, recent reports of improvement in oxygenation after substituting CNEP for PEEP in due mechanically ventilated infants with pulmonary dis¬ have suggested that there may be some intrin¬ sic differences between the two modes of distending pressure.2"4 Proposed mechanisms include a more uniform lung expansion as well as improvement in pulmonary blood flow with CNEP.2"4 Other clinical reports of using CNEP in infants and children also have suggested or demonstrated improvement in pulmonary blood flow.5"7 Experimental evidence for pulmonary hemodynamic differences between CNEP and PEEP has been reported by Adams et al, 8 who showed that when referenced to atmospheric pressure, pulmonary artery pressure (PAP) decreases in spontaneously breathing piglets subjected to .8 cm H20 CNEP as compared with +8 cm H20 PEEP. We recently reported on the pulmonary function ease CHEST /107 /1 / JANUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 249 fluid-filled esophageal catheter was placed into the lower third of the esophagus for measurement of esophageal pressure (Pes). Catheter placement was validated using the occlusion technique of Beardsmore et al.13 Vascular catheters were inserted as previously described.9,11,12 A femoral artery catheter was used for blood sampling and mea¬ surement of mean arterial pressure (MAP), while a femoral vein catheter was used for infusion of normal saline solution, 100 mL/kg/d. A thermodilution catheter measured PAP, pulmonary arterial wedge pressure and was used for CO determination. Fi¬ nally, a right atrial catheter was used to inject cold dextrose for CO determinations and to monitor central venous pressure (CVP). The PVR and systemic vascular resistance (SVR) were calculated using standard formulas.11 All vascular pressures were reported as transmural by subtracting end-expiratory Pes. Lung mechanics were calculated and monitored throughout the experiment as previously described.9,12 In summary, respira¬ tory flow was measured with a low dead space pneumotachometer (Hans Rudolph, 8131, Kansas City, Mo). The flow signal was electronically integrated to obtain tidal volume (Vt) and minute ventilation. In order to provide a measure of pressure across the lung, we measured Ptp at end-expiration, calculated as the difference between airway opening pressure (Pao), measured just proximal to the endotracheal tube, and Pes. Similarly, in order to provide a measure of pressure across the lung at end-inspiration, Ptr was calculated as the difference between Paw and body sur¬ face pressure at end-inspiration.9 Values for Vt, dynamic lung compliance (Cdyn), and lung resistance (Rl) were calculated from the mean of five breaths. The EELV was measured using the helium dilution technique (Equilibrated Bio Systems, Melville, and hemodynamics of anesthetized neonatal piglets; these piglets were ventilated, had lung lavage with saline solution, and were treated with either incre¬ mental CNEP or PEEP. No differences were found in any parameter with the exception of EELV at certain distending pressures.9 In that study, among the effects of saline lavage were significant increases in both cardiac output (CO) and transmural pulmo¬ nary artery pressure (PAPtm), although the increase in PAPtm was only modest. Since pulmonary hyper¬ tension is a common and serious disorder of the newborn infant,10 an accurate understanding of the effects of various ventilator strategies designed to restore EELV on pulmonary hemodynamics is es¬ sential. Thus, we were interested in comparing the effects of CNEP and PEEP in an animal model of acute lung injury associated with a more severe form of pulmonary hypertension. In this study, an infusion of Escherichia coli endotoxin was utilized to induce pulmonary hypertension in two groups of piglets subsequently treated with alternating periods of CNEP and PEEP. We hypothesized that at equiva¬ lent transpulmonary pressure (Ptp) and transrespiratory pressure (Ptr), there would be no differences in the effects of CNEP and PEEP on PAPtm and PVR. Materials Animal Preparation and Methods This study was approved by the Institutional Animal Use and Tripler Army Medical Center and was in compliance with the Animal Welfare Act. Eighteen neonatal piglets of either sex, 6 to 11 days old, weighing 2.6 ±0.5 kg, were anesthetized with pentobarbital as previously described.1112 Af¬ ter intubation with a 3.0- to 4.0-mm cuffed endotracheal tube, the lungs were slowly inflated once with 100 mL of air to reduce the effects of pulmonary atelectasis and to standardize lung inflation history. Mechanical ventilation was initiated at baseline settings: Care Committee of peak inspiratory pressure, 12 to 14 cm H2O; PEEP, 0 cm H2O; rate, 35 to 45 breaths per minute; inspiratory time, 0.35 s; and fraction of inspired oxygen (FI02), 0-21. An end-tidal CO2 mon¬ itor was used during animal preparation to maintain PaCC>2 be¬ tween 35 and 45 mm Hg by adjusting ventilator settings. An 8F Surgery NY). Experimental Design The experimental design is shown in Figure 1. After instru¬ mentation and 30 min of stabilization, piglets were treated with pancuronium, 0.1 mg/kg (Astra Pharmaceutical Products, Westborough, Mass) prior to taking control values. Paralysis was maintained throughout with intermittent doses of pancuronium. Next, E coli endotoxin, 12 Mg/kg (Serotype 055:B5, Sigma Chemical Co., St. Louis) was administered intravenously over 30 min. For the piglets, an FI02 of 0.5 was maintained for the remainder of the experiment. Following endotoxin administra¬ tion, they were observed for a 2-h period before application of distending pressure (CNEP or PEEP) in order to avoid the early phase of endotoxin-induced pulmonary hypertension character¬ ized by wide fluctuations in PAP (Fig 2). At that time, two experimental groups of piglets were exposed to three periods of 6 cm H20 distending pressure, either CNEP-PEEP-CNEP (n=6) or PEEP-CNEP-PEEP (n=6). A third group (zero end-expiratory Sick Control CNEP-PEEP-CNEP PEEP-CNEP-PEEP ZEEP-ZEEP-ZEEP 12 jjg/kg Endotoxin 1.>- -60 -30 -1.1.1- 30 60 90 120 150 180 210 240 Time (min) Figure 1. Experimental design. After piglets were instrumented on ZEEP, initial measurements were taken (Control), followed by endotoxin infusion. Two hours later, measurements were repeated (sick), followed by one of three sequences. Two experimental groups (each n 6) were subjected to alternat¬ ing sequences of distending pressure with -6 cm H20 CNEP or +6 cm H20 PEEP, while a third con¬ trol group (n=6) continued on ZEEP. = 250 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 CNEP and PEEP in E coli Endotoxin-Treated Neonatal Piglets (Mundie et al) Figure 2. Effects of endotoxin in ZEEP control group. Mean values for pulmonary function and he¬ modynamics in ZEEP control group (n=6) during and 4 h after endotoxin infusion (solid rectangles). For clarity, standard error bars have been omitted. Values for Cdyn given in milliliters per centimeter of water; Pa02 values given in millimeters of mercury; CO PVR and SVR values given in millimeters of mercury /liters per minute per kilogram. pressure ([ZEEP], control; n=6) was maintained on ZEEP through¬ the experiment. We kept Vt constant by adjusting peak in¬ spiratory pressure settings on the positive-pressure ventilator. were Hemodynamic and pulmonary function measurements taken every 30 min in the two experimental groups and every 15 min in the ZEEP control group. The ZEEP control group was out monitored more frequently to accurately describe the effects of endotoxin. The CNEP was administered in a body-enclosed two- compartment negative-pressure chamber.4,12,14 Data Analysis The experimental design allowed us to compare the effects of 6 cm H20 PEEP with -6 cm H20 CNEP using within group (one-way analysis of variance for repeated measures) and betweenIn group (two-way analysis of variance) statistical comparisons. addition, the effects of CNEP or PEEP in endotoxin-treated pig¬ lets were compared with the ZEEP control group by two-way was used for multi¬ analysis of variance. Duncan's post hoc test at p<0.05. Data ple comparisons. The level of significance was set in figures and tables are expressed as mean ± SEM. Statistical analysis was performed using a computer software package (NCSS, Kaysville, Utah). When no differences were found between respective data sets, Time (hr) Time (hr) results presented later on represent a combined mean ± SEM from all three periods of CNEP or PEEP taken from both exper¬ imental groups or all three periods in the ZEEP control group. Results Effects of Endotoxin Figure 2 shows a composite of the pulmonary function and hemodynamic responses to E coli endotoxin in ZEEP control piglets. Data were col¬ lected at Control, during endotoxin infusion, and for 4 subsequent hours. During and immediately after the endotoxin infusion (time, 0.5 h), there was a de¬ crease in Cdyn, EELV, PaO2, pH, and CO and an increase in Rl, transmural MAP, PAPtm, SVR, and PVR. During a period lasting 1 h following endotoxin administration, either stabilization or an improve¬ ment in the parameters occurred, except for pH which continued to decrease. From 1 h after endo¬ toxin infusion (time, 1.5 h), Rl, blood gas indexes, and CHEST /107 /1 / JANUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 251 o . oCM -5 x 350 CNEP-PEEP-CNEP PEEP-CNEP-PEEP 300-1 a Control ^4 250 ^ 2.5 H rr > 200 Q. 21 150 o E O 100 1.5 50 250 J 1 35 ^200 4 30 H 25 E > _j UJ UJ 150 O 100 15 o 10 50 Sick Period 1 Period 2 Period 3 Figure 4. Values for PVR and CO before endotoxin infusion Control 5 160-, 140 w (Control), after endotoxin infusion (sick), and after three 30-min periods (periods 1 to 3) in the 3 study groups. Values are mean ± SEM. Asterisks represent values different from ZEEP control group (p<0.05). Values for PVR given in millimeters of mercu¬ ry/liters per minute per kilogram. of three 30-min periods of exposure to alternating distending pressure with CNEP or PEEP, or in the ZEEP control group (Fig 1, 3, 4, Table 1). With appropriate adjustments in peak inspiratory H 120 O °^ 4 20 10080 60 Control Sick Period 1 Period 2 Period 3 Figure 3. Cdyn, EELV, and Pa02 before endotoxin infusion (Control), after endotoxin infusion (sick), and after three 30-min periods (periods 1 to 3) in the 3 study groups. Control values were taken in an FI02 setting of 0.21; piglets were then maintained at an FI02 setting of 0.5 for the remainder of the experiment. Val¬ ues are mean ± SEM. Asterisks represent values different from ZEEP control group (p <0.05); Pa02 values given in millimeters of mercury. hemodynamic parameters began to worsen. The ex¬ perimental sequences with CNEP and PEEP were started 2 h after endotoxin infusion (time, 2.5 h). Ventilator Variables-Indexes of Gas Exchange The data sampling periods are described as fol¬ lows: control, representing sampling after surgery and stabilization prior to endotoxin infusion; sick, representing sampling 2 h after endotoxin infusion; periods 1,2, and 3, representing data taken after each pressure (ZEEP control, 23.5 ± 1.0 cm H20; CNEP, 20.2 ±0.6 cm H20; PEEP, 26.4 ±0.4 cm H20), Vt remained constant during the experimental periods of alternating distending pressure (ZEEP control, 10.3 ±0.3 mL/kg; CNEP, 9.9 ±0.3 mL/kg; PEEP, 9.9 ± 0.3 mL/kg). Values for Ptp are reported only at end-expiration and for Ptr, only at end-inspiration. In the ZEEP control group, Ptp was 0, while Ptr increased significantly from Control (13.3 ±0.9 cm H20) after endotoxin infusion (23.8 ±1.6 cm H20), then remained unchanged for the remaining 4 h. In the experimental groups, Ptp was 0 until subjected to distending pressure with CNEP (3.0 ±0.1 cm H20) or PEEP (3.2 ±0.2 cm H20). The Ptr increased sim¬ ilarly after endotoxin infusion (before distending pressure), as in the ZEEP control group. However, unlike the ZEEP control group, Ptr increased further during CNEP (26.2 ±0.6 cm H20) and PEEP (26.4 ±0.4 cm H20). No differences were found in Table 1.Transmural Pulmonary Artery Pressure in Three CNEP-PEEP-CNEP (n=6) PEEP-CNEP-PEEP (n=6) ZEEP-ZEEP-ZEEP (n=6) Groups of Piglets Treated With Endotoxin* Control Sick Period 1 Period 2 Period 3 17±lf 18±0f 16±lf 34 ±2 32±3 34±2 27±lt 27±2f 25±lf 25±3f 34±3 30±3 24±2f 24±2f 27±3f *Values are mean ± SEM. No differences were found among groups, f Values different from respective sick period measurement (p<0.05). 252 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 CNEP and PEEP in E coli Endotoxin-Treated Neonatal Piglets (Mundie et al) either Ptp or Ptr between experimental groups at any point; as expected, some differences were found be¬ tween experimental groups as compared with the ZEEP control group. Blood pH was similar in the experimental groups at Control, decreased after en¬ dotoxin infusion, but remained stable during CNEP (7.29 ±0.01) and PEEP (7.29 ±0.01). No differences in pH were found between experimental groups. However, pH was lower in the ZEEP control group during periods 1 to 3 (7.18 ±0.03), as compared with the experimental groups. The PaC02 levels increased from control values in all groups after endotoxin in¬ fusion, remained stable in the ZEEP control group, but decreased with CNEP (36 ± 1 mm Hg) and PEEP (36 ± 1 mm Hg). There were no differences in PaC02 between groups. The Pa02 data in Figure 3 showed no differences between experimental groups; there were differences between experimental groups and the ZEEP control group during periods 1 to 3. Pulmonary Function The results in this and the following section sum¬ only differences between and within groups during periods 1 to 3 when piglets were subjected to CNEP and PEEP. In addition to Pa02, Figure 3 shows changes in Cdyn and EELV. There were no between or within group differences found in EELV or Cdyn in the experimental groups during periods 1 to 3. Further, no differences in Cdyn were found between experimental and ZEEP control groups. However, EELV was significantly increased in the marize experimental groups at 6 cm H20 distending pres¬ sure (periods 1 to 3), as compared with the ZEEP control groups. Changes in Rl were more variable (data not shown); no differences were found between any groups. Hemodynamic Parameters Figure 4 shows changes in PVR and CO. There were no between or within group differences found with these parameters in the experimental groups during periods 1 to 3. The only difference found be¬ tween experimental and ZEEP control piglets was with PVR during period 2; both experimental groups had lower values than the ZEEP control group. There were no differences between groups in either PAPtm (Table 1), SVR, transmural MAP, or heart rate (data not shown). Discussion Our previous study9 and the results of the present investigation suggest that from a physiologic point of view, there is no difference between CNEP in tandem with IMV and PEEP with IMV when Ptp and Ptr are equivalent. Both CNEP and PEEP increased EELV equally, resulting in similar reductions in PAP and PVR and increases in Pa02. This study offered the opportunity to explore potential differences in these forms of ventilation in an animal model char¬ acterized by endotoxin-induced pulmonary hyper¬ tension. In addition to the degree of pulmonary hy¬ pertension, other differences in endotoxin effect, such as decreased CO, were seen in contrast to the effects after lavage of the lung with saline solution.9 Our findings are in accord with previous conclusions re¬ garding negative pressure lung inflation utilizing a body-enclosed device.15"17 The situation may be dif¬ ferent from a physiologic point of view when the negative pressure device used is limited to the chest, as with a cuirass appliance, since this local application of negative pressure may create a pressure gradient to encourage venous return and preserve CO.817 The use of CNEP in various respiratory disorders has been supported by the belief that CNEP is more physiologic than PEEP. In contrast to PEEP, which transmits pressure from the proximal airway, CNEP would seem to more closely approximate the me¬ chanical effects of normal respiration. The combi¬ nation of an internally applied positive and exter¬ nally applied negative pressure may more evenly distribute the applied forces across both airways and peripheral lung tissue, leading to uniform lung expansion.3 However, this potential advantage of negative pressure has not been confirmed physiolog¬ ically. Another rationale for the use of extrathoracic negative pressure originated from the notion that lung inflation with negative pressure has a beneficial effect on pulmonary blood flow dynamics. In general, it was concluded that lung inflation with negative pressure reduced PVR, while lung inflation with pressure increased PVR.18"21 These studies utilized exteriorized1819 or isolated lungs20'21 and various experimental setups to compare the static effects of positive- and negative-pressure inflation of the lung at varying lung volumes and Ptp. Rather than reflecting differences between negative- and positive-pressure lung inflation, these results may have been due to differences in experimental condi¬ tions.119,22 Whereas the positive-pressure lung infla¬ tion setup included the vascular perfusion system at the same atmospheric pressure,18"20 this system was located outside of the chamber with negative-pres¬ sure inflation.2021 With negative-pressure lung infla¬ tion, the pressure surrounding the lung was decreased by a suction device connected to the enclosed cham¬ ber housing the excised lung. Since the perfusion setup was located outside the chamber, the driving pressure in the pulmonary circulation and the trans¬ mural pressure across the pulmonary microvasculature both increased, favoring increased blood flow. Including the perfusion system within the negative- positive CHEST /107 /1 / JANUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 253 pressure chamber has been shown to result in iden¬ tical effects on pulmonary hemodynamics to those obtained with positive-pressure inflation.22 Thus, some of the confusion regarding the effects of positive- vs negative-pressure lung inflation may have originated from the failure to properly refer¬ ence vascular and airway pressures.15'23 Since the lung is composed of two compartments, one poten¬ tially filled with air and the other with blood, the reporting of any vascular pressure must take into account the changing positive or negative ambient fusion. Both -6 cm H20 CNEP and 6 cm H20 PEEP similarly increased EELV and Pa02 due to the ben¬ eficial effects of distending pressure. Since both forms of therapy were equally effective, the use of either CNEP or PEEP may be considered for any individ¬ ual clinical situation. However, in contrast to PEEP, the administration of CNEP currently requires the use of cumbersome equipment that limits access to patient care. We feel that further studies with CNEP should be focused on improving the design of the CNEP equipment as well as on issues of clinical util¬ pressure ity. generated by our experimental interven¬ tions.1'9'23 Failure to account for this effect may lead to erroneous conclusions.9'23 For example, comparing CNEP with PEEP after lung lavage with saline solution, PAP was similar only when reported as PAPtm, while uncorrected values (referenced to at¬ mospheric pressure) were different at the higher distending pressures studied.9 Similarly in this study, all pressure measurements were reported as trans¬ mural by subtracting end-expiratory Pes. Although we did not specifically confirm the relationship of Pes to pleural pressure, other studies have shown a good correlation, even with increased lung volume.24 Also, as previously described,9 we used Ptp and Ptr to compare more accurately the effects of negative and positive pressure interventions. This was accom¬ plished by subtracting Pes from Pao at end-expira¬ tion as a measure of pressure across the lung at endexpiration (Ptp); subtracting body surface pressure from Pao at end-inspiration was a measure of pres¬ sure across the lung at end-inspiration (Ptr). By per¬ forming these calculations, it is evident that driving pressure can be expressed as a positive number with both positive- and negative-pressure lung inflation.15 A striking effect of endotoxin was the reproducible biphasic elevation in PAPtm seen during the 4-h pe¬ riod. This was considerably greater in magnitude than that induced by lung lavage with saline solution (PAP in mm Hg, low 20s).9 Indeed, the elevation in PAP demonstrated at the time of the sick period measurements (PAP in mm Hg, low to mid 30s) was even greater than after exposure to a hypoxic gas mixture (FIo2,0.15 [PAP in mm Hg, high 20s]).11 The other hemodynamic and pulmonary function effects of endotoxin demonstrated in this study were consis¬ tent with previous studies in swine.25"29 These are due to the direct effects of endotoxin and the stimulation or the release of numerous cellular and humoral mediators, making it an accepted model of adult respiratory distress syndrome 30 In summary, our results show that by properly referencing pressures, CNEP or PEEP in tandem with IMV results in equivalent effects on pulmonary function and hemodynamics in piglets with pulmo¬ nary hypertension secondary to E coli endotoxin in¬ 254 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 ACKNOWLEDGMENTS: The authors thank David P. Southall, MD, MRCP, and Martin P. Samuels, MB, MRCP, for their help¬ ful suggestions and advice in designing this study, Glenn Hashiro, MS, and Wayne Takenaka, RRT, for technical assistance, and Kenneth T. Nakamura, MD, and Susan Pelke, RN, for preparing and reviewing this manuscript. References 1 Mead J, Whittenberger JL. Lung inflation and hemodynamics. In: Handbook of physiology. Section 3, vol. 1, Circulation. Washington, DC: American Physiological Society, 1964; 477-86 2 Cvetnic WG, Cunningham MD, Sills JH, Gluck L. Reintroduction of continuous negative pressure ventilation in neonates: two-year experience. Pediatr Pulmonol 1990; 8:245-53 3 Cvetnic WG, Shoptaugh M, Sills JH. Intermittent mandatory ventilation with continuous negative pressure compared with positive end-expiratory pressure for neonatal hypoxemia. J Perinatol 1992; 12:316-24 4 Samuels MP, Southall DP. Negative extrathoracic pressure in the treatment of respiratory failure in infants and young chil¬ dren. BMJ 1989; 299:1253-57 5 Sanyal SK, Avery TL, Thapar MK, Hughes WT, Harris KS. Continuous negative chest-wall pressure therapy for assisting ventilation in older children with progressive respiratory in¬ sufficiency. Acta Pediatr Scand 1977; 66:451-56 6 Penny DJ, Hayek Z, Redington AN. The effects of positive and negative extrathoracic pressure ventilation on pulmonary blood flow after the total cavopulmonary shunt procedure. Int J Car¬ diol 1991; 30:128-30 7 Raine J, Samuels MP, Mok Q, Shinebourne EA, Southall DP. Negative extrathoracic pressure ventilation for phrenic nerve palsy after paediatric cardiac surgery. Br Heart J 1992; 67:308-11 8 Adams JA, Osivich H, Goldberg RN, Suguihara C, Bancalari E. Hemodynamic effects of continuous negative extrathoracic pressure and continuous positive airway pressure in piglets with normal lungs. Biol Neonate 1992; 62:69-75 9 Easa D, Mundie TG, Finn KC, Hashiro G, Balaraman V. Con¬ tinuous negative extrathoracic pressure vs. positive end-expi¬ ratory pressure in piglets after saline lung lavage. Pediatr Pul¬ monol. Pediatr Pulmonol 1994; 17:161-68 10 Walsh-Sukys MC. Persistent pulmonary hypertension of the newborn. Clin Perinatol 1993; 20:127-43 11 Easa D, Uyehara CFT, Stevens EL, Finn KC, Balaraman V, Sim H. Pancuronium does not alter the hemodynamic status of piglets after normoxia or hypoxia. Pediatr Res 1993; 33:365-72 12 Easa D, Mundie TG, Finn KC, Balaraman V, Stevens E, Tak¬ enaka W, et al. The effects of reversing the sequence of distending pressure sequences in the neonatal piglet. Pediatr Pulmonol 1994; 17:97-105 13 Beardsmore CS, Helms P, Stocks J, Hatch DJ, Silverman M. Improved esophageal balloon techniques for use in infants. J CNEP and PEEP in E coli Endotoxin-Treated Neonatal Piglets (Mundie et al) Appl Physiol 1980; 49:735-42 14 Scotka J, Takenaka W, Malmstrom-Okita J, Smith MB, Mundie T, Easa D. Evaluation of the operational capabilities of a new extrathoracic negative pressure device for use in newborn in¬ fants. Neonatal Intensive Care 1992; 5:36-40 15 Maloney JV, Whittenberger JL. Clinical implications of pres¬ sures used in the body respirator. Am J Med Sci 1951; 221:425-30 16 Beck GJ, Seanor HE, Barach AL, Gates D. Effects of pressure breathing on venous pressure; a comparative study of positive pressure applied to the upper respiratory passageway and negative pressure to the body of normal individuals. Am J Med Sci 1952; 224:169-74 17 Lockhat D, Langleben D, Zidulka A. Hemodynamic differ¬ ences between continual positive and two types of negative pressure ventilation. Am Rev 18 Roos Respir Dis 1992; 146:677-80 A, Thomas LJ Jr, Nagel EL, Prommas DC. Pulmonary vascular resistance as determined by lung inflation and vascu¬ lar pressures. J Appl Physiol 1961; 16:77-84 19 20 21 Whittenberger JL, McGregor M, Berglund E, Borst HG. Influence of state of inflation of the lung on pulmonary vascu¬ lar resistance. J Appl Physiol 1960; 15:878-82 Burton AC, Patel DJ. Effect on pulmonary vascular resistance of inflation of the rabbit lungs. J Appl Physiol 1958; 12:239-46 Thomas LJ, Griffo ZJ, Roos A. Effect of negative-pressure in¬ flation of the lung on pulmonary vascular resistance. J Appl Physiol 1961; 16:451-56 22 Permutt S, Howell JBL, Proctor DF, Riley RL. Effect of lung inflation on static pressure-volume characteristics of pulmonary vessels. J Appl Physiol 1961; 16:64-70 23 Qvist J, Pontoppidan H, Wilson RS, Lowenstein E, Laver MB. Hemodynamic responses to mechanical ventilation with PEEP: the effect of hypervolemia. Anesthesiology 1975; 42:45-55 24 Wohl ME, Turner J, Mead J. Static volume-pressure curves of dog lungs-in vivo and in vitro. J Appl Physiol 1968; 24:348-54 25 Schrauwen E, Houvenaghel A. Hemodynamic evaluation of endotoxic shock in anesthetized piglets: antagonism of endog¬ enous vasoactive substances. Circ Shock 1985; 16:19-28 26 Schranz D, Huth RG, Stopfkuchen H, Jungst BK. The effect of nif edipine alone or combined with low dose acetylsalicylic acid endotoxin-induced pulmonary hypertension in the piglet. Intensive Care Med 1988; 14:595-601 Kristensen J, Modig J. Ringer's acetate and dextran-70 with or without hypertonic saline in endotoxin-induced shock in pigs. Crit Care Med 1990; 18:1261-68 Siebeck M, Weipert J, Keser C, Kohl J, Spannagl M, Machleidt W, et al. A triazolodiazepine platelet activating factor receptor antagonist (WEB 2086) reduces pulmonary dysfunction during endotoxin shock in swine. J Trauma 1991; 31:942-50 Weitzberg E, Rudehill A, Lundberg JM. Nitric oxide inhalation attenuates pulmonary hypertension and improves gas exchange in endotoxin shock. Euro J Pharamcol 1993; 233:85-94 Brigham KL, Meyrick B. Endotoxin and lung injury. Am Rev on 27 28 29 30 Respir Dis 1986; 133:913-27 CHEST /107 /1 / JANUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/ on 10/01/2016 255