LUMBAR SPINE IMAGING Normal Variants, Imaging Pitfalls, and
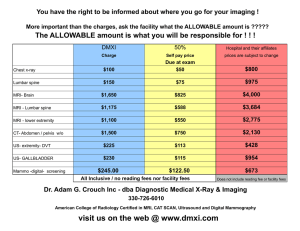
advertisement

LUMBAR SPINE IMAGING Normal Variants, Imaging Pitfalls, and Artifacts Radiologic Clinics of North America - Volume 38, Issue 6 (November 2000) - Copyright © 2000 W. B. Saunders Company DOI: 10.1016/S0033-8389%2808%2970004-6 IMAGING OF LOW BACK PAIN I LUMBAR SPINE IMAGING Normal Variants, Imaging Pitfalls, and Artifacts Jamshid Tehranzadeh 1 MD Carol Andrews 2 MD Edward Wong 1 MD Department of Radiological Sciences, University of California Irvine (JT, EW), Orange Department of Radiological Sciences, and Spinal Injection Service, University of California Los Angeles (CA), Los Angeles, California 1 2 Address reprint requests to Jamshid Tehranzadeh, MD Department of Radiological Sciences University of California, Irvine Medical Center 101 The City Drive Orange, CA 92868-3298 e-mail: jtehranz@uci.edu Correct interpretation of images requires sound knowledge of normal spine and being cognizant of normal variants, pitfalls, and artifacts. Definition of normal depends on the imaging modality (CT or MR imaging) and the particulars of each patient. Different MR imaging sequences may create different challenges in interpretation of the same anatomic structures. Finally, patients occasionally may have benign static conditions that mimic the imaging appearance of a lesion.[117] DEVELOPMENT OF THE BONY SPINAL COLUMN Development of the spinal column begins in the 4th week of gestation, when cells of the sclerotomes surround the spinal cord and notochord. These cells form a mesenchymal column, which retains its segmental origin, and its blocks are separated by areas of less density.[102] This process is followed by the proliferation and condensation of the sclerotomal segments and their extension into subjacent intersegmental tissue, binding the caudal half of one sclerotome to the cephalic half of the superior one. The vertebral body is intersegmental in origin.[117] Anomalies may develop during the intersegmental process of the vertebral bodies. Asymmetric fusion of the sclerotomal segment may lead to hemivertebra. Symmetric abnormalities in intersegmentation probably lead to either an increase or a decrease in the individual's number of vertebrae. Normal segmentation of the spine should not be mistaken for fracture (Figs. 1 (Figure Not Available) 2 (Figure Not Available) 3 ) or vice versa.[117] Figure 1. (Figure Not Available) Normal sacral segmentation. Axial CT scan of the sacrum in an 8-year-old boy shows normal segmentation. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535570; with permission.) Figure 2. (Figure Not Available) Normal segmentation of the vertebra. Axial CT of the lumbar spine in an 18-month-old boy. These separate ossification centers will coalesce later to create a solid vertebra. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 3. Old fracture of superior articular process simulating segmentation. A, Axial and B, coronal CT scan reconstruction of lumbosacral spine (L5 to S1) showing fragmentation of right superior articular process of S1 (arrows) mimicking segmentation. Spinal dysraphism (Figs. 4 and 5) is a general term collectively referring to congenital anomalies of the pediatric spine. Spinal dysraphism occurs during the first 8.5 weeks of development of life, which is called the embryonic period. [32] Figure 4a. Figure 4b. Butterfly vertebra. Midsagittal T2-weighted image (TR = 5000, TE = 45) in a 20-month-old girl with spinal dysraphism. A, The cartilaginous bright area at the center of body of L3 (arrow) may be misleading on this image. B, It is more obvious on the coronal T2-weighted image (6066/67) and C, the axial T2-weighted image (6100/34). D, The axial CT scan and E, the coronal CT scan reconstruction. (Courtesy of Sherri Birchansky, Miami, FL.) Figure 5. Spinal dysraphism with hemivertebra and butterfly vertebra of lumbosacral spine. Sclerotic response of facet joint on concave side of scoliosis. The intervertebral disk is mesenchymal in origin and is derived from the tissue between the cephalic and caudal portions of the original sclerotome. This tissue does not proliferate like the cephalic and caudal portions of the sclerotome. Rather, it fills the space in between what eventually becomes two precartilaginous vertebral bodies. Although the portion of the notochord in the region of the vertebral body regresses, the portion in the region of the intervertebral disk persists and enlarges. When the persistent notochord later undergoes mucoid degeneration, it becomes the nucleus pulposus and is surrounded by the circular fibers of the annulus fibrosus.[117] Spinal dysraphism refers to imperfect fusion of midline mesenchymal, neural, and bony structures and it may appear in several forms. Spina bifida refers to defective closure of the bony encasement of the cord through which neural elements may or may not protrude. Spina bifida cystica refers to a skin-covered defect. Spina bifida aperta, which includes meningocele, myelocele, and meningomyelocele, refers to a non-skin-covered defect. Spina bifida occulta is a normal variant in which the failure of bony fusion is not associated with protrusion of neural structures.[32] [81] [117] DEVELOPMENT OF THE SPINAL CORD Development of the spinal cord begins in the 3rd week of fetal life, when the ectodermal layer thickens, giving rise to the neural plate. This is followed by neurulation. The neural plate is formed and the neural folds fuse at the midline to form the neural tube. Fusion occurs first in the cervical region and then progresses irregularly in the cephalic and caudal directions.[37] [122] The position of the spinal cord changes with age. The vertebral canal and dura lengthen to a greater degree than the spinal cord. It results in the terminal end of the spinal cord being shifted to a higher level. The spinal cord ends at approximately L1 to L3 at birth. Because of the disproportionate growth between the spinal cord and vertebral canal, the spinal nerves course obliquely from their origin to exit at the correct vertebral level.[117] NORMAL IMAGING CHANGES DURING SPINAL GROWTH The intervertebral disk undergoes marked anatomic change with age. The nucleus pulposus, in infancy, is a slightly flattened spheroid of clear gel and the disks are prominent. The typical appearance of the normal adult disk is intermediate to low signal on T1-weighted image and high signal on T2-weighted image reflecting the high water content and long relaxation times of the disk compared with adjacent bone marrow.[27] [133] The disk water content decreases radially from the central nucleus to the annulus and is seen as a progressive decline both in signal on T2weighted image and in volume with aging. The transition between nucleus and annulus is relatively sharp in a young disk and becomes less distinct with aging and degeneration. A horizontal central linear focus of decreased signal intensity representing a denser fibrous collection is found in the nucleus pulposus, which becomes more prominent with aging. This dark line, which is called the intranuclear cleft (Fig. 6) (Figure Not Available) , could represent a fibrous remnant of the notochord[86] or an embryonic fissure separating sclerotomes in the perichondral disk.[27] This should be distinguished from truncation artifacts. Truncation artifacts are thin, uniform, and located midway between the vertebral end plate. Intranuclear clefts are less distinct and less irregular.[14] Absence of this cleft might be a secondary sign of disk space infection in the proper clinical setting.[74] Figure 6. (Figure Not Available) Normal intranuclear cleft of intervertebral disks. Sagittal T2-weighted image (3,000/96) in a 38year-old woman shows normal horizontal dark signal line (arrows) inside the bright nuclear disk substance. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) In infants and children, the marrow signal is low intensity because of prominent hematopoietic activity. During the first month of life the vertebral bodies show hypointense signal on T1weighted images, except for the linear hyperintensity along the course of the basivertebral vein. On T2-weighted images, marrow appears hypointense. Between 1 and 6 months of age there is an increase in vertebral marrow signal intensity on T1-weighted images, which progresses from the end plates centrally, with relative isointensity of vertebral bodies and cartilage achieved at approximately 7 months. Normal vertebral marrow and cartilage may enhance somewhat with administration of contrast agent.[74] SIGNIFICANCE OF MARROW CHANGES Prevalent hematopoietic red marrow in infants and children is replaced by yellow marrow in adult life (Fig. 7) (Figure Not Available) . Normal adult marrow appears as bright signal on T1-weighted images with a less bright signal on T2-weighted images (T2 appearance may vary according to the pulse sequence). In myeloproliferative diseases, myelofibrosis (Fig. 8) , anemia, and hypoxemia caused by such conditions as morbid obesity and pickwickian syndrome, congenital cyanotic heart disease, and chronic obstructive pulmonary disease, and in patients with AIDS (Fig. 9) (Figure Not Available) , there is a reconversion of yellow marrow to red marrow, which shows low signal intensity on both T1- and T2-weighted images.[39] [66] This process can occur in women of reproductive age secondary to physiologic anemia[75] and anemia of any cause, including infiltrative marrow disorders, where normally dormant vertebral marrow is seen to undergo compensatory hematopoiesis. Short-tau inversion recovery (STIR) and fat-saturation sequences are particularly sensitive to abnormal marrow changes. Figure 7. (Figure Not Available) Evolution of hematopoietic to fatty marrow in a growing skeleton. A, Sagittal T1-weighted image (850/23) of the spine in a 4-month-old infant showing hematopoietic low signal marrow. Note prominent disks at infancy. B, Sagittal T1-weighted image (650/19) of the spine in a 6-year-old boy showing intermediate to low signal intensity in bone marrow, indicating partial fatty replacement of hematopoietic marrow. C, Sagittal T1-weighted image (400/19) of the spine in a 29-year-old woman showing further fatty replacement of bone marrow. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 8. Myelofibrosis. Sagittal T1-weighted image (TR 500, TE 14) demonstrates the diffuse low intensity signal of the vertebral body marrow that is only slightly higher than the adjacent disks in this 55-year-old male with myelofibrosis. Figure 9. (Figure Not Available) Dark marrow. Parasagittal T1-weighted gradient-echo image of thoracic spine in a 30-year-old man with AIDS showing diffuse low signal intensity of bone marrow. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Marrow of low signal intensity on T1-weighted images may be mistaken for diffuse tumor involvement.[28] [74] If edema or necrosis is present, as in the case of many neoplasms, it shows increased signal intensity on T2-weighted images. Some spinal tumors, however, are mostly fibrotic and appear hypointense on T2-weighted images.[74] A further confusing matter is the fact that on fat-suppressed T2-weighted images or STIR images, hematopoietic marrow may appear relatively hyperintense, mimicking a tumor. Further distinction between tumor and hematopoietic marrow can be made by comparing the vertebral body signal intensity with that of the intervertebral disk. With hematopoietic marrow, the vertebral bodies have a higher signal intensity than the adjacent disk on T1-weighted images. This relationship is reversed in neoplasm, where the disk has higher signal intensity compared with the vertebral body on T1-weighted images. This has been termed the hyperintense disk sign.[19] The hyperintense disk sign is not always specific. The disks may become hyperintense relative to the vertebral body in cases of iron overload or severe anemia when hyperplastic marrow is present.[74] In equivocal cases, gadolinium can be administered before the acquisition of T1-weighted images. The disks are noticeably hypointense adjacent to the enhancing neoplasm. The contrast is even more evident on fat-suppressed images.[74] It is important always to compare contrast-enhanced images with non-contrast-enhanced images of the same pulse sequence (e.g., nonenhanced T1-weighted images with enhanced T1-weighted images). Fatty vertebral bone marrow is normally present later in life. The MR imaging characteristics of fatty marrow are bright on T1- weighted images and moderately dark on T2-weighted images. The signal intensity is decreased on T1-weighted images with fat suppression. Although diffuse fatty marrow normally is identified as age related, focal vertebral body fat may be mistaken for benign and malignant tumors and hemangioma. Increased marrow signal can also occur following radiation therapy,[89] [90] [92] [127] where fatty marrow is sharply demarcated along the extent of the radiation port (Fig. 10) (Figure Not Available) . The actual appearance of vertebral body signal alterations after radiation therapy is variable, and is dependent on the dose of radiation and time elapsed.[90] These fatty changes could be seen as soon as 9 days following completion of radiotherapy with a radiation dose of at least 800 rad (8 Gy)[90] and could remain unchanged for more than 10 years.[89] The use of fat-suppressed images may be helpful, because tumor should not change in appearance. The use of gadolinium may be confusing because postradiation fibrosis has a variable pattern of enhancement. Figure 10. (Figure Not Available) Fatty marrow changes after radiation therapy. Parasagittal proton density (900/12) image of lumbosacral spine in a patient with rectal carcinoma who received radiation with a port extending from L5 to sacrum and coccyx. Note bright signal (fatty changes) at L5 and sacral levels. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) DIFFERENTIATION OF COMPRESSION FRACTURE FROM PATHOLOGIC FRACTURE ON MR IMAGING The dilemma of differentiating osteoporotic compression fractures from pathologic fractures is frequently encountered in elderly patients, especially elderly women. Sacral insufficiency fractures may mimic malignant lesions (Fig. 11) .[4] [36] [134] In the first 3 to 6 months following the fracture, both benign and malignant fractures have increased water content and are dark on T1weighted images and bright on fat-saturated T2-weighted images or STIR images. On fatsaturated T1-weighted images both enhance with gadolinium. If additional lesions are not demonstrated on a nuclear bone scan, it is difficult to distinguish benign from malignant fractures.[11] Figure 11. Sacral insufficiency fractures masquerading as metastasis in a 59-year-old female. A, Coronal T-1 weighted image (450/12) shows focal area of low signal in the sacrum adjacent to left SI joint suggesting metastasis (open arrow). Proved to be stress fracture on biopsy. Note a second stress fracture on the right sacrum (arrowheads). B, Posterior view of Tc-99m methylene diphosphonate bone scan shows more uptake on the left sacrum (arrowheads). When the marrow signal is normal, the lesion may characterize an old process. If the marrow is abnormal, however, it may represent either a new (acute) fracture, tumor, or metastasis. It is important to decide whether the lesion is focal and caused by a neoplasm or a lesion in the end plate, which may represent a traumatic fracture. If the lesion extends into the pedicle or affects several levels (multiple foci) in the spine, it is most likely caused by metastatic disease. If this differentiation cannot be made on the basis of MR imaging, a plain film, CT, or possibly a bone scan may be helpful. If there is a clinical concern, a follow-up imaging study or a bone biopsy may be performed. In a recent study by Palmer et al,[84] who compared 107 benign with 45 malignant collapses of vertebral bodies, the presence of a linear fracture line parallel to the superior end plate was both sensitive and specific for benign vertebral collapse and it was demonstrated to have the highest negative predictive value for malignant collapse. In the same study, extraosseous soft tissue extension and convex cortical contours were found to be highly specific but insensitive for malignant collapse. Intravertebral fluid and angulated retropulsed cortical fragments were highly specific but insensitive for benign collapse. In this study, pedicle involvement, gadolinium enhancement pattern, and the degree of preserved intravertebral fat were found not helpful. Bauer et al[6] have used diffusion imaging in making the distinction between malignant and acute benign vertebral body compression fractures. A metastatic compression fracture is brighter on diffusion images than an osteoporotic compression fracture. The following provides pearls that may help in this differentiation. In general, pathologic cause is suggested when there is evidence of adjacent osseous metastases, when there is involvement of the posterior element, and when cortical destruction and associated soft tissue mass are present. Individual cases can be difficult, particularly when there is an acute fracture present resulting in diffuse signal alteration involving the entire vertebra.[115] Marrow heterogeneity is another variant of normal that could be mistaken for a pathologic condition. Normal marrow heterogeneity is usually caused by bright foci of increased signal on T1-weighted images, whereas neoplastic marrow heterogeneity is often characterized by foci of low signal intensity on T1-weighted images. Heterogeneous signal intensity of the vertebral body bone marrow may also be seen in metastatic disease, multiple myeloma, Waldenstrom's macroglobulinemia, or other infiltrative conditions.[79] [80] Marrow heterogeneity is more conspicuous on high field-strength MR imaging systems and in older adults.[74] [91] Clinical information and other laboratory findings or even bone biopsy may be necessary to reach the diagnosis. SIGNIFICANCE OF FOCAL BRIGHT MARROW IN VERTEBRAE Focal bright marrow in the vertebral body may represent veins; focal fat; end plate fat, such as that in Modic type II degeneration; or hemangiomas (Fig. 12) (Figure Not Available) . Generally, the presence of a focal bright spot in the T1-weighted image indicates a benign process. The only exception is the rare appearance of metastatic melanoma. Vertebral hemangiomas are bright on T1-weighted images because of the fat interspersed within the trabeculae of the hemangioma.[51] [95] They have decreased signal intensity on fat-saturated T1- and T2-weighted images. Hemangioma may even present as isointense foci on T1-weighted images. On CT, the vertebral hemangioma has a typical polka dot appearance within a low-density area (Fig. 13) (Figure Not Available) . Other lesions in the spine, such as metastases or myeloma, may be mistaken for hemangioma (Fig. 14) (Figure Not Available) .[51] Sometimes, a small polka dot pattern is seen as a result of localized hypertrophied struts.[51] [69] For example, osteoporosis may sometimes be associated with apparent hypertrophy of trabeculae and may mimic a hemangioma. Osteoporosis usually presents a similar appearance at multiple levels, whereas a hemangioma most commonly involves only a single level. It may, on occasion, be difficult to differentiate these two entities.[52] The polka dot pattern in hemangioma is symmetric and homogeneous, whereas those in myeloma and metastasis often have inhomogeneous and asymmetric aggregations of bone trabeculae. Figure 12. (Figure Not Available) Hemangioma of thoracic spine. Axial CT of thoracic vertebra shows radiating polka dot appearance indicating vertebral body hemangioma. (From Helms CA, Volger JB III, Hardy DC: CT of the lumbar spine: Normal variants and pitfalls. Radiographics 7:447-463, 1987; with permission.) Figure 13. (Figure Not Available) Focal vertebral body hemangioma. Axial CT of spine shows focal lytic lesion with polkadot appearance inside indicating focal hemangioma. (From Major NM, Helms CA: Normal variants and pitfalls in CT of the lumber spine. Contemp Diagn Radiol 16:1-6, 1993; with permission.) Figure 14. (Figure Not Available) Myeloma of the spine. Axial CT of the spine showing lytic lesion of the vertebral body mimicking hemangioma. However, this does not have the typical polkadot appearance of hemangioma. (From Helms CA, Volger JB III, Hardy DC: CT of the lumbar spine: Normal variants and pitfalls. Radiographics 7:447-463, 1987; with permission.) Occasionally, lipid rests are found in the spine (Fig. 15) . They present as bright foci on T1weighted images.[50] Another cause of bright foci on T1-weighted images (Fig. 16) is the basivertebral venous complex (Fig. 17) (Figure Not Available) , which has a horizontal striated appearance with a predilection for fat along its course.[74] Figure 15. Focal fatty degeneration of vertebral marrow in a 78-year-old man with ankylosing spondylitis. Sagittal T1-weighted image (500/10) shows focal fatty marrow degeneration with squaring of vertebrae. Note bright signals in the intervertebral disk due to paradoxical effect of intradiscal ossification. Figure 16. Basivertebral plexus. A, Sagittal T1-weighted (TR 500, TE 14) scan demonstrates the flow void of the basivertebral vein (as linear low signal) and the surrounding fat (as globular high signal intensity) located in the central region of the vertebral body. B, Sagittal T2-weighted (TR 4000, TE 112) scan shows the decrease in marrow signal as the fatty marrow signal is suppressed. The continued high signal in the immediate region of the plexus most likely represents vessels with slower flow adjacent to the high-flow signal void. Figure 17. (Figure Not Available) Basivertebral vein. Axial CT scan of the lumbar spine shows normal basivertebral vein (open arrowhead). (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) VERTEBRAL BODIES AND VERTEBRAL END PLATES Hemivertebrae may be found throughout the spinal column, and they may be fused with adjacent vertebrae.[74] Other congenital anomalies include butterfly vertebra (see Fig. 4) . Sacrococcygeal elements may be of varied number and size.[74] Schmorl's nodes (Fig. 18) (Figure Not Available) represent disk material herniated into the vertebral end plate and are enhanced on MR imaging.[109] They may be mistaken for a metastasis. Metastasis can be differentiated from a Schmorl's node based on the typical location of the latter adjacent to the disk space and by its well-defined sclerotic border surrounding a zone of variable lucency.[69] Few Schmorl's nodes become symptomatic. Vascularization may be a normal healing process for intraosseous cartilaginous hernias and is not necessarily accompanied by back pain. Enhancing Schmorl's nodes (Fig. 19) , however, were larger and more often accompanied by bone marrow edema in patients with back pain than in those without.[109] Deep Schmorl's node (Fig. 20) and tunneling Schmorl's node of lumbar vertebra have been reported.[67] In tunneling Schmorl's node, there are communicating superior and inferior Schmorl's nodes, creating a longitudinal tunnel through the vertebral body. Limbus vertebra also represents a herniation of disk material into the adjacent end plate, through the extrusion of nucleus pulposus that typically occurs at an anterior oblique angle, resulting in isolation of a corner of the vertebral body. This wedge-shaped fragment retains normal marrow elements and signal (Fig. 21) . In Scheuermann's disease (juvenile kyphosis), abnormal softening of the end plates leads to development of multilevel Schmorl's nodes and vertebral compression (Fig. 22) (Figure Not Available) . Rarely, a notochordal remnant tissue may create an osteolytic change in a vertebral body that should be distinguished from chordoma. Figure 18. (Figure Not Available) Schmorl's node. Axial CT of the lumbar spine shows a Schmorl's node (arrow). Schmorl's node represents focal herniation of the intervertebral disk into the end plate. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 19. Enhancing Schmorl's node. A, Sagittal T1-weighted (TR 600, TE 14) scan demonstrates the low signal node extending from the disk space directly into the vertebral body. B, Sagittal T2-weighted scan (TR 2000, TE 100) shows the bright extruded cartilage. C, Sagittal T1-weighted scan (TR 600, TE 14) with fat suppression following contrast administration demonstrates rimlike enhancement while the center of this large node remains low signal intensity. Figure 20. Deep Schmorl's node. CT sagittal reconstruction scan of lumbar spine shows deep Schmorl's node (arrowheads) penetrating two thirds of L5 vertebral body. The intervertebral disk is narrowed at this level. Figure 21. Limbus vertebra. A, Sagittal T1-weighted scan (TR 466, TE 16) demonstrates high signal intensity in the triangular anterosuperior end plate of L3, representing the residua from a remote herniation of disk material through the end plate at an oblique angle, resulting in isolation of this small fragment of bone containing normal fatty marrow. B, Sagittal T2-weighted (TR 3650, TE 112) image confirms the normal fatty marrow signal within the fragment, comparable to the adjacent vertebral body. Figure 22. (Figure Not Available) Scheuermann's disease. Parasagittal T1-weighted image (650/19) in a 34-year-old man shows multiple thoracolumbar Schmorl's nodes indicating Scheuermann's disease. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Occasionally, it is difficult to number the vertebral bodies on axial images (Fig. 23) . One method is to refer to a reference image in which numbered lines, corresponding to the axial images, are superimposed on either a CT scout film or an MR sagittal image. If the patient has moved between the time of the scout film and the axial images, however, the vertebral body level may be misinterpreted. In the lumbar spine, anomalies of fusion can lead to assigning incorrect vertebral body levels. Transitional vertebrae occur with partial or complete lumbarization of a sacral vertebra or partial or complete sacralization of a lumbar vertebra. Transitional vertebrae can lead to mistakes in assigning vertebral body levels to lesions in the lumbosacral spine, including the bodies themselves or the intervertebral disks.[49] Figure 23. Pitfall in identification of normal spine segmentation. A, Sagittal T1-weighted scan (TR 510, TE 14) suggests lumbar segment configuration of five lumbar segments. B, Anteroposterior radiograph demonstrates six non-rib-bearing lumbar-type vertebral bodies (rather than the five suggested on MR image). Mirowitz [74] makes several recommendations for determining the correct level in an MR image of the spine. With a large field-of-view MR imaging body coil, one may localize vertebral bodies on surface coil images by placing an external marker (vitamin E capsule) over a particular vertebral body and then using an electronic cursor.[119] The right renal artery interposed between the crus of the diaphragm and the inferior vena cava on parasagittal images can indicate the L1-L2 disk level 86% of the time.[88] Some sources consider this method unreliable.[48] It is important to state in a report how one has numbered the vertebrae. Review of an anteroposterior radiograph is necessary to confirm which vertebral body corresponds to the findings by MR imaging. Lap-belt injuries in children tend to occur in the midlumbar area because of their unique anthropomorphic characteristics. Children have a higher center of gravity than adults, a larger head size relative to body length, and incompletely developed iliac crests. These factors cause hyperflexion of the midlumbar spine and riding up of the lap-belt above the pelvis, leading to spinal and visceral injury. Spinal fractures in restrained children tend to occur in the midlumbar area, tend to be oriented in an axial plane, and may be missed on transaxial images. Transaxial imaging may also fail to detect dislocations in the axial plane.[116] Spiral CT, with sagittal and coronal reformatted images, may prevent this potential pitfall. In restrained pediatric trauma patients undergoing CT imaging of the abdomen and pelvis, one might consider obtaining the entire examination in spiral mode, allowing sagittal and coronal reconstructions. The intravertebral vacuum cleft seen on radiographs in avascular necrosis (Kummell's disease) may not be seen on MR images because of the relative insensitivity of MR imaging to small air collections.[74] Occasionally, paradoxic signal alterations may be seen.[70] Images that initially show a signal void from air later show increased signal on T2-weighted images. This is because of fluid in the vacuum cleft accumulating in the supine position, which can mimic infection or neoplasm.[74] VERTEBRAL END PLATES Degenerative diskogenic vertebral changes can be noted on the end plates bordering the intervertebral disks (also called Modic I to III). There are three phases of degenerative disease on MR imaging of the spine.[28] [78] Type I results in decreased signal intensity on T1-weighted images and increased signal intensity on T2-weighted images (Fig. 24) , and there is increased signal intensity with gadolinium. These changes are caused by edema or granulation tissue.[57] [97] [104] It is not easy to distinguish this type of degenerative disease from infection. Type II changes are secondary to fatty change with increased signal intensity on T1-weighted images and mildly increased (less than T1) signal intensity on T2-weighted images (Fig. 25) (Figure Not Available) . [74] Type III changes result from sclerosis and lead to hypointensity on all sequences (Fig. 26) (Figure Not Available) . These changes are distinguished from more serious conditions by serial examinations or by the presence of associated disk degeneration or disk protrusion.[74] Figure 24. Type I end plate changes (edema). A, Parasagittal T1-weighted image (583/19) of the lumbar spine shows eroded L45 end plate with low signal intensity and narrowed disk, suggesting marrow edema or infection. B, Parasagittal T2-weighted image (3,000/96) shows bright signal at L4-L5 end plate with disk narrowing and end plate erosion, suggesting marrow edema or infection. Figure 25. (Figure Not Available) Type II end plate changes (fatty degeneration). A, Sagittal T1-weighted image (650/19) of the lumbar spine shows bright signal intensity of end plates at L5 to S1 level representing fatty degeneration. B, Sagittal T2-weighted image (3,000/96) of the lumbar spine shows the fatty changes at the end plate representing intermediate signal intensity. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 26. (Figure Not Available) Type III end plate changes (sclerosis). A, Sagittal T1-weighted image (650/19) of the lumbar spine in a patient with spondylolysis and spondylolisthesis. Diskogenic end plate sclerosis at the L5 to S1 end plate represents type III (sclerotic) marrow changes. B, Sagittal T2-weighted image (3,000/96) of the lumbar spine. The sclerotic end plate changes at the L5 to S1 level remain with low signal intensity. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) SUMMARY OF MARROW CHANGES AT END PLATES The three phases of degenerative disease on MR imaging of the spine are: 1. Type I: Edema. Decreased signal intensity on T1-weighted images and increased signal intensity on T2-weighted images 2. Type II: Fatty changes. Increased signal intensity on T1-weighted images and increased (but less than T1) signal intensity on T2-weighted images 3. Type III: Sclerotic changes. Decreased signal intensity on T1- and T2-weighted images There are a multitude of other vertebral pathologic conditions with overlapping features. Occasionally, conditions as diverse as vertebral neoplasm, infection, avascular necrosis, Paget's disease, and fracture are difficult to distinguish.[108] Tuberculosis or coccidiomycosis commonly spares the adjacent disk.[1] This may lead one to diagnose neoplasm, especially if there is an associated soft tissue mass. Vertebral osteomyelitis typically involves two contiguous vertebral bodies and the intervertebral disk. Type I degenerative marrow signal intensity changes parallel those of osteomyelitis. These marrow changes may also enhance after gadolinium injection. Enhancement of the central portion of the degenerated disk has also been reported.[97] The disk, however, is usually decreased in signal intensity on T2-weighted images in the setting of degenerative disk disease, helping to differentiate it from diskitis.[24] Many disease processes, such as metastatic disease, and low-grade pyogenic infections, such as brucellosis, fungal infections, and sarcoidosis, have imaging findings similar to those of tuberculosis of the spine. Characteristic features of brucellar spondylitis include gas within the disk, minimal associated paraspinal soft tissue mass, absence of gibbus deformity, and predilection for the lower lumbar spine.[128] Pathologic spine fractures are characterized by marrow replacement and decreased vertebral body height.[74] There may be enhancement after gadolinium in both insufficiency and pathologic fractures.[79] [80] There may be enlargement of the intervertebral disk adjacent to a fractured vertebra and increased signal intensity on T2-weighted images. These changes reflect increased disk hydration in an effort to occupy the volume lost by a vertebral compression fracture.[74] THE INTERVERTEBRAL DISK The intervertebral disk changes in size with aging. It is prominent during infancy[133] (see Fig. 7A) (Figure Not Available) and decreases in volume with age. The intervertebral disk also has changing signal characteristics. Normally the disk is of decreased signal intensity on T1-weighted images and increased signal intensity on T2-weighted images. There is loss of signal on T2weighted images with disk degeneration caused by loss of hydration and alteration in the connective tissue components of the disk. These changes are accentuated in sequences with long echo times, such as T2-weighted gradient echo imaging or fast spin echo sequences.[74] Disk degeneration occurs in older individuals but may also be seen in children.[118] Degenerative changes do not always correlate with symptoms[58] and may be seen in asymptomatic patients. Septic diskitis is associated with decreased disk space; however, in tuberculous and fungal infections the intervertebral disk is preserved in the early stages of the disease (Fig. 27) . Figure 27. Coccidiomycosis Spondylitis. Intervertebral disk preservation in a 20-year-old man with disseminated coccidioidomycosis of the spine. Sagittal T2-weighted image (3000/96) of lumbar spine shows dark signal in L4 and sacral bone due to osteomyelitis. Note relative preservation of disk spaces. Grenier et al[45] suggest the nuclear gas collections within the disk could be identified because of their contrast with the disk on short TR/TE sequences. The identification of vacuum phenomenon when it lies close to the cortical end plates, however, is more difficult. Differentiation of calcifications in the disk from vacuum phenomenon with MR imaging depends on the distribution of calcium within the voxels. Dense calcification creates the same signal void as gas, but most of these types of calcifications have a nodular configuration, unlike vacuum phenomena. When calcium deposition is widespread in the disk, the decreased signal is not perceptible.[45] Rarely, the presence of air in the intervertebral disk may be a sign of infection; such findings have been described in spinal brucellosis.[128] Intervertebral disks may undergo signal change in processes other than degeneration or infection. Ankylosing spondylitis affects the axial skeleton with an osteitis of the end plate corners resulting in bright signal on T2 and squaring of the vertebral bodies. This same inflammatory process affects the adjacent disk with bright T2 signal in the anterior disk as well (Fig. 28) . Figure 28. Ankylosing spondylitis. A, Sagittal T1-weighted scan (TR 600, TE 14) in a 35-year-old male with recent low back pain. Note the "squared" configuration of the vertebral bodies as well as the increased signal in the anterior corners of several vertebral bodies. B, Sagittal T2-weighted (TR 2000, TE 100) scan demonstrates the persistent high signal in these same areas suggesting the presence of vascularized fibrous tissue, consistent with the osteitis seen in ankylosing spondylitis (shiny corner sign). Note the increased intradiskal signal at L1 and L2 suggestive of fibrovascular ingrowth into the disk substance. C, Axial proton density (TR 2000, TE 40) scan confirms the bilateral sacroiliac joint fusion. POSTERIOR ELEMENTS Spina bifida occulta results from incomplete fusion of the posterior elements. This is a common entity in the sacral spine and may be considered a normal variant. Other variants include neoarthrosis between the transverse processes of L5 and S1, often associated with transitional vertebra. There may also be variations in the diameter of the spinal canal. Spinal canal narrowing can occur when congenitally short pedicles are present.[65] Congenital hypoplasia or absence of pedicle or pars interarticularis on one side (Fig. 29) creates stress reaction or marrow edema (Fig. 30) and eventually sclerosis on the contralateral side (Fig. 31) . Bilateral defects in the pars interarticularis (spondylolysis) or fracture in the lamina (Figs. 32 (Figure Not Available) and 33) can result in vertebral subluxation (spondylolisthesis) (Fig. 34) . This may not be evident on axial MR images.[44] On CT, axial views are diagnostic for spondylolysis; otherwise, one should refer to the sagittally reconstructed images. Often, one can identify spondylolisthesis on the scout images. On MR images, these defects are best appreciated on the sagittal and parasagittal images (see Fig. 33) . These defects are also identifiable on contiguous axial imaging and may appear as a double facet (see Fig. 32) (Figure Not Available) . Fibrovascular tissue occupying the defect may enhance with contrast. A false diagnosis of spondylolisthesis can occur with partial volume averaging of facet osteophytes.[61] In addition, sclerosis involving the pars may also give the false appearance of a defect.[61] [63] Figure 29. Congenital absence of lumbar pedicle. A, Axial CT scan of L3 vertebra in a 6-year-old girl. CT scan of L3 vertebra shows congenital absence of left L3 pedicle with partial hypoplasia of left lamina. B, Left parasagittal reconstruction CT shows absence of L3 pedicle. (Courtesy of Sherri Birchansky, Miami, FL.) Figure 30. Unilateral spondylolysis of lumbosacral spine in a 15-year-old boy with contralateral marrow edema. A, Left parasagittal T1-weighted scan (400/11) shows left lateral pars interarticularis defect (arrow). B, Right parasagittal T2-weighted scan (4800/140) shows focal increased signal due to marrow edema in the right pedicle (arrow) secondary to stress. (Courtesy of Sherri Birchansky, Miami, FL.) Figure 31. Dense pedicle and lamina secondary to laminar defect on the opposite side. A, Plain radiograph shows dense pedicle of lumbar spine on the right side. B, Axial CT scan shows defect in left lamina (arrowhead) and secondary reactive sclerotic changes of right pedicle and lamina. (Courtesy of Marnix vanHolsbeek, Detroit, MI.) Figure 32. (Figure Not Available) Spondylolysis and spondylolisthesis of L5 to S1. A, Axial CT at L5 vertebral body shows bilateral pars interarticularis (isthmus) defects (solid arrows). It should not be mistaken for facet joints (open arrows). Note that the spinal canal size is not narrowed in true spondylolysis. B, Sagittal reconstruction CT of L5 to S1 shows isthmus defect (arrowheads) with grade I spondylolisthesis. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 33. Pars intra-articularis defect. A, Axial T1-weighted (TR 600, TE 14) image shows the double facet sign of the right pars defect with evidence of a small amount of fluid within the defect itself on axial T2-weighted (TR 5000, TE 112) scan (B). C, Axial T1-weighted image (TR 600, TE 14) with fat suppression following intravenous injection of gadolinium demonstrates enhancement in the more ventral of the two linear bands. Figure 34. Spondylolysis and spondylolisthesis. A, Parasagittal T2-weighted image (3,000/96) shows pars interarticularis defect at the L5 to S1 level (arrow) with grade I spondylolisthesis. B, Axial T1-weighted image (700/14) at the L5 to S1 level shows spondylolysis. Note the canal size is not decreased. Rather, it seems larger than normal. DIFFERENTIATION OF DEGENERATIVE SUBLUXATION FROM SPONDYLOLISTHESIS In a degenerative subluxation, so-called pseudospondylolisthesis, the canal depth is usually decreased (Fig. 35) (Figure Not Available) . In spondylolytic spondylolisthesis, however, because of the pars interarticularis defect, there is preservation of the canal depth (see Figs. 32 (Figure Not Available) 33 34 ), but there is narrowing of the neural foramen on sagittal views.[121] Figure 35. (Figure Not Available) Degenerative pseudospondylolisthesis at L4-5. A, Parasagittal T2-weighted image (3,000/96). In this case, subluxation of L4 over L5 is related to facet arthritis and ligamentous laxity and not to pars interarticularis defect. Note that spinal canal is consequently narrowed. Thickening of ligamenta flava is also noted. B, Axial multiplanar gradient-echo (316/17) image shows that subluxation has resulted in small spinal canal. Subluxation in pseudospondylolisthesis is related to degenerative process and not to pars interarticularis defect. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) PARASPINAL SOFT TISSUES Inferior lumbar space hernias can simulate paravertebral mass lesions.[40] Paraspinal soft tissue inflammatory processes can simulate neoplastic lesions in this region. Tuberculosis is certainly known to simulate neoplasm. Pseudotumors comprised of reactive inflammatory tissue are sometimes seen with chronic vertebral subluxation.[112] A bulky osteophyte may mimic a paraspinous mass on MR imaging. Comparison with radiographs quickly clarifies the source of the psoas pseudomass (Fig. 36) . Bony callus following fracture may create neoarthrosis (Fig. 37) . Figure 36. Osteophyte masquerading as a psoas mass. A, Axial T1-weighted image (TR 600, TE 14) at L1-L2 in a 45-year-old male presenting two months following posterior fusion with continued back pain. The right psoas is markedly wasted and displayed by a smooth rounded mass (arrowheads) that seems to arise in or near the adjacent vertebral body. B, Axial T2- weighted image (TR 2000, TE 100) demonstrated intermediate signal intensity, suggesting a possible mass lesion. C, Postoperative radiograph confirms this mass to be a mature osteophyte (arrowheads). Figure 37. Osteophyte pseudoarthrosis. Hypertrophic osteophyte and bony callus creating pseudoarthrosis in a 24-year-old man with previous right sacral fracture. A, Plain radiograph of lumbosacral spine may mimic appearance of hemisacralization of L5 vertebra on the right side. Note evidence of old fracture of sacrum on the right side. B, Axial CT scan at L5-S1 level shows pseudoarthrosis of merging osteophytes at L5-S1 level. Note sclerotic line indicating healed sacral fracture (arrowhead). (Courtesy of Henry Pribram, Orange, CA.) Normal paravertebral soft tissues can be mistaken for masses.[33] One example is a prominent ascending lumbar vein. These are of intermediate signal intensity, similar to that of the soft tissue, because of slow flow within the vein. Flow-sensitive gradient echo imaging is helpful in confirming the presence of flowing (moving) blood. EXTRADURAL SPACE The basivertebral vein appears dark on T1-weighted images and bright on T2-weighted images (see Figs. 16 and 17) (Figure Not Available) . A focal prominence of the basivertebral vein may simulate a small disk herniation on sagittal or transaxial images. Because the venous plexus enhances with gadolinium, further confusion with a mass may occur.[38] Lumbar veins at the periphery of the spine should not be confused with a basivertebral vein. Basivertebral veins are noted on midsagittal images, whereas lumbar veins are at the periphery of the vertebral bodies (Fig. 38) (Figure Not Available) . A prominent epidural venous plexus may simulate a herniated disk[17] [35] [85] or arteriovenous malformation. Relative increased signal intensity on T1- and T2weighted images can be observed in these veins because of slow flow and second echo rephasing.[74] On CT examination, the basivertebral vein within the bony column should not be mistaken for a lytic lesion (see Fig. 18) (Figure Not Available) . The basivertebral plexus has distinct margins. Occasionally, a small amount of calcification may be seen within the plexus, and in some instances a calcific spur can be seen protruding posteriorly from the plexus. Venous channels may simulate fractures (Fig. 39) (Figure Not Available) and vice versa. Venous channels present as linear lucent lines, identified exclusively in the midportion of the vertebral body and extending to the basivertebral plexus.[69] Figure 38. (Figure Not Available) Normal lumbar vessels. Lateral parasagittal T1-weighted image (510/15) shows normal lumbar vessels that hug the periphery of vertebral bodies. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 39. (Figure Not Available) Venous channels. Axial CT scan of the thoracic vertebra shows normal intrasomatic venous channels (arrowheads). (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) EPIDURAL SOFT TISSUES The ligamentum flavum has increased signal intensity on T1-weighted images compared with other ligamentous structures. This is because of the heavy concentration of elastin.[74] Ligamentous ossification is usually associated with decreased signal intensity on all sequences and may be difficult to distinguish from ligamentous hypertrophy, but there may be increased signal intensity on T1-weighted images because of marrow fat.[44] [45] [82] [83] [101] [110] [129] When axial forces are applied to the spine, the ligamentum flavum may appear to bulge.[82] Focal globular calcifications can give the appearance of a mass, similar to a synovial cyst.[45] Figure 40 (Figure Not Available) shows an air-filled calcified synovial cyst on both CT and MR imaging. The air resulting from vacuum phenomena from a degenerative disk or facet joint may diffuse into the epidural space and be a source of diagnostic pitfall (Fig. 41) . Figure 40. (Figure Not Available) Calcified synovial cyst with vacuum air in the facet joint and in the cyst. A, Axial CT scan of the lumbar spine showing calcified synovial cyst filled with air that has leaked from degenerative facet arthrosis on the right side. B, Axial T1-weighted MR image of the lumbar spine showing calcified synovial cyst with air presenting as low-signal-intensity mass. Right facet arthrosis shows low signal from sclerosis and presence of air in the facet joint. (Courtesy of Clyde Helms, Durham, NC.) (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 41. Vacuum air in intervertebral disk and inside spinal canal. Axial CT scan of L5 to S1 level shows volume averaging of a degenerated intervertebral disk and vertebral end plate with vacuum air inside the disk and in the right anterior epidural space (arrow). A redundant or prominent posterior longitudinal ligament may resemble a vertebral osteophyte.[101] This is most likely to occur on gradient echo images when the ligament is calcified.[74] On CT examination, the presence of a dividing cleft between the vertebral body and a calcified posterior longitudinal ligament can differentiate this condition from a bony ridge arising from the vertebral end plate. Epidural masses may be simulated by hypertrophy of the posterior elements[44] or by synovial cysts arising from the facet joints and projecting into the spinal canal.[60] Filum lipoma is a normal variant that exhibits a string of intradural fatty tissue at several levels (Fig. 42) (Figure Not Available) . Paraspinal fatty replacement is seen in paraplegia, quadriplegia, or chronic disuse.[74] Paraspinal lipomatosis is seen in cases undergoing chronic steroid treatment, in adrenal tumors, or in cases of adrenal hyperplasia.[40] Figure 42. (Figure Not Available) Filum lipoma. A, Axial T1-weighted image (650/14) at body of L4 vertebra shows small focal fatty bright area that extends at multiple levels superiorly and inferiorly, indicating filum lipoma (arrow). Note normal thin layer of epidural fat. B, Axial T1-weighted image (650/14) at L5 to S1 level shows extension of the filum lipoma (arrow) down to sacral level. Note increased amount of epidural fat at L5 to S1 level. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Epidural lipomatosis (Fig. 43) is an unusual condition. Patients with rheumatoid arthritis, systemic lupus erythematosus, asthma, and dermatomyositis, and transplant recipients have all been reported to develop epidural lipomatosis after undergoing steroid therapy. Although the result of neurologic examination may be normal, patients with epidural lipomatosis usually present with weakness (72% of cases); decreased sensation or reflexes (50%); and mild back pain. Epidural lipomatosis can be diagnosed easily as homogeneous high signal intensity of epidural fat on T1weighted images. Findings on myelography may be normal. On CT, the increased epidural fat usually manifests posterior to the dura matter and may compress the cord anteriorly.[43] Figure 43. Epidural lipomatosis. A, Sagittal T1-weighted image shows excessive fat (bright signal) in epidural space anterior and posterior to dural sac. B, Axial T1-weighted image shows that the normally round dural sac has a clover or V-shaped appearance. (Courtesy of Henry Pribram, Orange, CA.) NEUROFORAMINA The dorsal root ganglia may enhance after the administration of gadolinium.[15] [22] [97] Synovial cysts may extend into the neuroforamina or spinal canal.[97] SPINAL CORD The thecal sac has a variable caudal termination. Usually, it ends at the level of the second sacral vertebra; however, in many individuals it terminates at higher levels,[7] such as L5. The spinal subarachnoid space varies in prominence. Cystic dilation of the thecal sac can be seen, especially in the lower lumbar and sacral areas.[74] Sacral meningeal cysts are rarely associated with neurologic symptoms.[26] Prominence of the subarachnoid space can be seen in patients with spinal cord atrophy, simulating an arachnoid cyst,[107] and in patients with a tethered cord. Tarlov cysts may mimic an expansile lesion or even metastasis (Fig. 44) (Figure Not Available) . Figure 44. (Figure Not Available) Tarlov cysts simulating tumor or metastasis. Axial CT scan of lumbar spine shows Tarlov cysts simulating tumor or metastasis. (Courtesy of Clyde Helms, Durham, NC.) (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) The conus medullaris is usually at L1 but may be at T12 or L3. Early in development the conus is low lying, ascending with maturity.[87] [124] On sagittal images, the exact location of the conus can be difficult to determine because of clustering of the proximal cauda equina nerve roots,[74] [87] [94] [124] and this may be mistaken for an intradural mass on axial images.[74] Clustering of the nerve roots may be caused by spinal stenosis or arachnoiditis. [94] Scoliosis can present difficulties in spinal imaging because the spine comes into and out of the plane of imaging (Fig. 45) (Figure Not Available) . The spine is imaged segmentally. It is also subject to partial volume averaging effects.[74] Mirowitz and Shady[75] recommend imaging the spine by reformatting sagittal images along oblique or curved planes, allowing continuous visualization of the spinal cord; alternatively, a coronal image may be obtained. Figure 45. (Figure Not Available) Scoliosis. Parasagittal T2-weighted image (4,400/112) shows upper lumbar region close to midline and lower lumbar area more lateral, close to neural foramina, indicating scoliosis at this level. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) SPINAL NERVES AND GANGLIA There are numerous variations of the spinal nerve roots and associated ganglia. The dorsal root may be larger in size than the corresponding ventral roots, and there may be duplication of the dorsal root ganglia at the lumbar and upper sacral levels. The L5 through S4 ganglia are located in the spinal canal and not the neural foramen. Some ganglia, usually sacrococcygeal, are located in the dural sac.[7] A filum lipoma may be seen at several levels parallel to the cauda equina (see Fig. 42) (Figure Not Available) . Conjoined nerve roots (Fig. 46) may simulate disk herniation. These conjoined nerve roots can be seen to divide on consecutive images.[74] Figure 46. Conjoined nerve root. A, Myelogram of lumbar spine (prone position) shows L4 and L5 nerve roots exiting together under the pedicle of L4 vertebra on the right side, so-called conjoined nerve root (open arrows). Note conjoined L5 and S1 nerve roots on the left side. B, Axial CT postmyelogram shows double nerve root on the left side (arrows). (Courtesy of Clyde Helms, Durham, NC.) THE POSTOPERATIVE SPINE Postoperative Changes Postoperative changes include spondylolisthesis, central stenosis, foraminal stenosis, arachnoiditis, infection, hemorrhage, nerve injury, epidural fibrosis, recurrent disk herniation, and pseudomeningocoele. Chemonucleolysis Chymopapain injection for chemonucleolysis results in characteristic changes on MR imaging. The treated disk has a very low signal intensity on T2-weighted images[73] and decreased height. [64] Decreased signal intensity can be seen 2 weeks following treatment, with a return to baseline appearance approximately 2 years later, as a result of scar formation.[64] Diskectomy Diffuse decreased signal intensity of the disk is usually observed after diskectomy[74] and increased signal intensity on T2-weighted images within the posterior disk margin. In the immediate postoperative period, this is caused by fluid at the site of disk curettage.[93] This is later replaced by granulation tissue, which undergoes enhancement after contrast.[74] This is distinguished from postoperative diskitis, where there is increased disk signal intensity on T2weighted images and enhancement of the adjacent vertebral end plates.[9] Comparison with previous studies should be made, because similar changes can be seen with type I degenerative changes in the vertebral end plates.[74] In the immediate postoperative period, the configuration of the interspace may be identical to its preoperative appearance for at least 1 month postsurgery. Between 2 and 6 months following surgery, false-positive appearance decreases.[9] [10] [93] The appearance of apparent herniated disk material results from the presence of postoperative edema or hemorrhage.[74] As a result, the use of MR imaging in detecting residual disk material in the immediate postoperative period is limited but is important as a baseline study. Bone Marrow Transplantation In individuals who have undergone bone marrow transplantation, decreased marrow signal intensity on T1-weighted images occurs.[74] Like other discrete high signal foci, this may mimic infection or neoplasm. Persistent Appearance of Pseudoherniation Following Surgery Patients with relief following surgery may have imaging evidence of persistent herniation in the immediate postoperative period in 20% of cases. This is because early on there are changes, such as granulomatous reactions, that may mimic disk protrusion but in fact are a pseudoherniation. In 10% of postoperative patients, postenhancement images may still be abnormal. End plate changes are also slow to resolve despite the fact that the patient did well.[125] Pseudodisk Appearance The conditions that may produce a pseudodisk appearance include scar, osteophyte, posterior longitudinal ligament calcification, spondylolisthesis, conjoined nerve root, neuroma, schwannoma, Tarlov cyst, synovial cyst (see Fig. 41) , epidural abscess, and epidural hematoma. Tarlov cyst may simulate an expansile lesion or intracanalicular metastasis (see Fig. 44) (Figure Not Available) . Long after spinal surgery, epidural soft tissue masses are frequently seen; these may represent herniated disk material, granulation tissue, fibrosis, or a combination of these.[74] There are certain general principles that may aid in distinguishing these entities. There are exceptions to each of these principles, however, and the patient's clinical condition must be taken fully into account before arriving at any conclusion. On T2-weighted images, granulation tissue and fibrosis usually are of greater signal intensity than herniated disk material,[74] but extruded disk fragments may appear hyperintense on T2-weighted images, similar to inflammatory tissue.[17] Mature fibrosis may develop decreasing signal intensity on T2-weighted images because of the declining proportion of extracellular space.[18] Herniated disk fragments are usually associated with mass effect, whereas epidural fibrosis either does not or is characterized by retraction of adjacent tissues.[74] Mass effect, however, can be associated with epidural granulation tissue or fibrosis.[57] [75] [96] Because disk material is avascular, it does not enhance, whereas postoperative inflammatory tissue is very vascular and enhances prominently.[74] Enhancement of herniated disk material can occur if MR imaging is delayed 20 minutes or more following the administration of gadolinium.[57] [97] Areas of epidural fibrosis have been known to enhance up to 20 years following surgery.[96] Enhancement is most intense in the 9 months following surgery and declines thereafter[41] and may lead to confusion with recurrent disk herniation. Subtle enhancement of epidural fibrosis may be recognized by using contrast-enhanced T1-weighted images with fat suppression.[8] [75] Region-of-interest measurements can be obtained and compared with the precontrast scan. Noncontrast scans should always precede contrast scans because failure to do so may lead to serious errors of diagnosis.[74] Summary: How to Differentiate Scar from Recurrent Disk Following injection of the contrast agent, scar tissue reveals homogeneous enhancement (Fig. 47) (Figure Not Available) , whereas the recurrent disk shows peripheral enhancement (Fig. 48) . The anterior scar remains vascular and enhances for many years. The posterior scar becomes fibrotic, and after a few months there is diminished enhancement. Scar consistently enhances, causing retraction of the thecal sac, and may even show mass effect or may be contiguous with the disk space. Figure 47. (Figure Not Available) Postoperative scar. A, Postoperative axial T1-weighted image (700/14) without gadolinium shows a low-signal focal area (arrowheads) near the left lateral nerve root mimicking a recurrent disk protrusion. B, Axial T1weighted image (700/14) post-gadolinium shows enhancement of low-signal area indicating postoperative scar tissue. Note enlarged left nerve root ganglion as a result of edema. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 48. Recurrent disk herniation. A, Noncontrast axial T1-weighted image (700/14) MRI at the T12 to L1 disk level shows focal abnormal low signal mass at the epidural space. B, Axial T1-weighted image (800/11) post-gadolinium injection shows peripheral enhancement around the recurrent disk herniation at the T12 to L1 level. Although scar may be noted in the nonoperated spine surrounding disk herniation, it is more likely seen in the operated spine; surgical curettage site; the intervertebral disk in diffuse, spotty, or linear form; and in type I end plate changes. The recurrent disk does not enhance within 20 minutes postinjection, and it is expected to enhance on delayed images. It is important that imaging is done within 20 minutes of injection. In general, all disks, whether operated or not operated, are surrounded by some scar. Imaging differentiation of scar from recurrent disk has improved from 83% (CT myelogram) in 1983 to almost 100% in 1993 with high-resolution enhanced MR imaging. Failure of Differentiation of Disk from Scar This may be the result in part from partial volume averaging (e.g., a small amount of disk or a large amount of scar); vascularization of the disk; and delay in imaging following contrast injection. Postoperative Epidural and Paraspinal Soft Tissue Changes There may be a postoperative pseudomeningocoele. If fat packing is performed at the operative site, collections of fat are seen within the epidural space.[93] This can simulate the T1 shortening effects of methemoglobin within an epidural hematoma.[74] Gelfoam or methylmethacrylate may result in heterogeneous signal intensity and simulate an abscess[93] at the laminectomy site.[74] The paraspinal musculature has an abnormal postoperative appearance. Air within the tissues shows a signal void (Fig. 49) . Increased signal intensity on T2-weighted images resulting from edema and hemorrhage may be noted. Not only does the postoperative paraspinal musculature appear distorted in the postoperative state, it may also show abnormal contrast enhancement.[93] Figure 49. Air as a signal void. Transaxial T2-weighted scan (TR 4300, TE 98) at L4-L5 obtained two days following a laminectomy shows the retained air (arrow) within surgical place in the operative bed. This artifact occurs at the tissue-air interface as a signal void. Myelography Retained iophendylate (Pantopaque) in patients who have undergone previous myelography presents as increased signal intensity on T1-weighted images because of the lipid composition of iophendylate.[74] This may simulate intradural lesions, such as lipomas, hemorrhage, or dermoid.[5] [13] [46] [47] [59] [72] [111] Chemical shift misregistration may surround the retained iophendylate because of its lipid composition.[74] Retained iophendylate is hypointense to cerebrospinal fluid (CSF) on gradient echo imaging and may simulate intradural and extradural lesions, magnetic susceptibility, or flow artifact.[59] IMAGING ARTIFACTS MR Imaging Artifact Caused by Nonuniform Magnetic Field Artifacts occur when the read frequency gradient cannot create an orderly change in the magnetic field.[114] Tissue Interfaces Bone-tissue interfaces cause variation in the magnetic field, which can change the frequency of tissue signal. In the spine, magnetic susceptibility variation occurs within the trabecular bone. This causes rapid dephasing of the signal and a mottled hypointense appearance on gradient echo scan. A T1-weighted spin echo image of bone appears brighter than a gradient echo image because it is much less sensitive to magnetic field inhomogeneities. Incomplete Fat Saturation An air-fat interface causes variation in the magnetic field, which causes lipid protons to have a Larmour frequency that does not match that of the saturation pulse. The lipid appears bright. Ferromagnetic Artifact Ferromagnetic artifact is caused by the large magnetic susceptibility of ferromagnetic material. Magnetic susceptibility is the ratio of intensity of magnetization produced in a substance to the intensity of the applied external magnetic field.[23] [53] This large magnetic susceptibility causes gross local static magnetic field inhomogeneities.[53] This kind of artifact results in spatial and signal distortion displayed along the frequency-encoding axis, usually presenting as a signal void associated with peripheral signal hyperintensity.[74] Stainless steel produces severe artifact compared with titanium (Fig. 50) (Figure Not Available) .[76] Ferromagnetic artifact is greater with gradient echo imaging than it is with both conventional and fast spin echo imaging. It is also worse with reduced-bandwidth imaging,[53] large voxel sizes, long echo times, and high-fieldstrength magnets.[22] [130] Apart from causing artifacts, ferromagnetic objects can be hazardous during MR imaging examination and should be removed, if possible. A number of nonremovable metallic objects, however, are still encountered. Spinal fixation rods are a common problem. Others may be shrapnel or inferior vena cava filters. Nonferrous devices can cause similar artifacts through the generation of eddy currents.[34] [71] [103] [123] On CT examination, metallic artifact results in a beam-hardening phenomenon causing image deterioration. Figure 50. (Figure Not Available) Magnetization susceptibility artifact. Parasagittal T1-weighted image of the lumbar spine (510/15) shows metallic artifact caused by spine fusion. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Chemical Shift Chemical shift is the difference in Larmour frequency of hydrogen nuclei bound into a different chemical compound.[53] Chemical shift misregistration artifact is caused by differences in precessional frequencies of fat and water protons, causing an artifactual shift in signal intensity along fat-water interfaces in the frequency-encoding direction of an image.[74] This causes spatial mismapping of one of the two, fat or water, in an MR image.[3] [12] [25] [29] [113] [106] Because MR imaging systems are tuned to the frequency of water, fat is mismapped on the image (Fig. 51) .[53] Misregistration artifact increases with reduced-bandwidth imaging and high-field-strength magnets.[53] [74] Fat-suppression methods can be combined with reduced bandwidth to decrease chemical shift misregistration artifact. The diskovertebral junction represents a fat-water interface. Chemical shift misregistration can cause an artifactual shift in signal intensity from one vertebral end plate to the opposite end plate on sagittal images of the spine.[29] The posterior longitudinal ligament can be obscured by chemical shift misregistration, suggesting a tear.[57] This problem can be avoided by swapping phase and frequency axes. Figure 51. Chemical shift artifact. A, Sagittal T1-weighted image (TR 500, TE 14) demonstrates a discrete rounded low-intensity fluid collection behind the S3 segment of the sacrum with a rudimentary connection to the thecal sac, representing a Tarlov cyst. B, Sagittal T2-weighted scan (TR 4000, TE 112) demonstrates increased signal intensity within the fluid collection. Immediately dorsal to the Tarlov cyst a low-intensity signal creates a thin shell over a portion of the cyst. This results from chemical shift artifact in the frequency direction, where the fluid content of the cyst is immediately adjacent to the epidural fat. Tissue contrast within bone marrow, which contains both fat and water, can be improved by exploiting the chemical shift effect. The technique is called phase-contrast imaging.[126] Red marrow looks dark in an out-of-phase contrast gradient echo image, because the fat and water signals nearly cancel. If the normal red and yellow marrow are replaced by cellular infiltrate with high water content, however, as seen in leukemic infiltration or metastatic disease, this results in minimal signal change on a proton density out-of-phase gradient echo image when compared with the in-phase imaging.[42] Zebra-Stripe Artifact Local variations in magnetic field are much more noticeable in gradient echo images than in spin echo images. For example, zebra stripe artifacts can be seen at the borders of large field-of-view gradient echo images. This is because of spatially dependent phase variations caused by inhomogeneity of the static magnetic field. Such phase variations become more significant at locations far from the center of the magnet.[42] Motion Artifact This can cause artifactually increased or decreased signal intensity.[74] Motion artifact occurs in the phase-encoding direction and can lead to blurring or ghosting of structures (Fig. 52) . [53] [74] Blurring may occur in any direction, causing spatial dispersion of signal.[31] [123] Blurring occurs when an object changes location between phase-encoding views.[55] The signal of the structure is displayed over its range of motion, causing decreased edge definition.[2] [62] [99] Ghost artifact (Figs. 53 and 54) is structured noise [62] caused by periodic signal intensity or phase shift variations.[2] [62] [99] With a constant frequency of the periodicity, the effect is to display copies or ghosts across the phase-encoding axis. Ghost artifact (see Figs. 53 and 54) propagates across the entire image.[53] With a variable frequency of periodic motion, there is mismapped signal along the phaseencoding axis appearing as streak artifact.[55] [99] In the thoracolumbar region, motion artifact results from respiratory motion and vascular pulsations from the heart and aorta. Motion artifacts are expressed along the phase-encoding axis of an image, which in the spine is usually anteroposterior.[74] [123] The two generally available CSF motion-compensation methods are CSFgated acquisition and gradient rephasing. CSF gating refers to the synchronization of pulsatile CSF motion with MR imaging data acquisition; this is usually accomplished with the use of peripheral pulse or electrocardiographic gating. Gradient rephasing is a general term referring to the use of imaging gradients to rephase motion-dependent phase shifts.[100] On CT examination, motion misregistration artifact can lead to significant deterioration on reconstructed images and may be misleading on axial images. Figure 52. Motion artifact. A, Sagittal T1-weighted (TR 416, TE 10) scan of the lumbosacral junction exhibits a single air-filled loop of bowel in the presacral region. B, Sagittal T1-weighted (TR 400, TE 16) scan of the same area obtained 20 minutes later demonstrates the motion artifact resulting from a peristaltic wave from the previously air-filled bowel loop. Figure 53. Motion artifact. Sagittal T1-weighted image (TR 600, TE 11) demonstrates the ghosting artifact related to misregistration related to the pulsation of the aorta. This occurs in the phase-encoding direction, which is superior-inferior in this image. Figure 54. Motion artifact. Sagittal T2-weighted scan (TR 3500, TE 112) demonstrates an artifact in the phase-encoding direction (superior to inferior) from the rhythmic motion of the diaphragm during respiration. Vascular Artifact In the normal patient, the aorta has fast pulsatile laminar arterial flow. Multiple ghost images of this flow create a complex multilayered horizontal band artifact, often referred to as phase shift within the image. This artifact becomes more prominent when a contrast agent is administered unless the ghost artifacts are minimized with inferior and superior saturation pulses, which prevent contrast media from exaggerating the vascular artifacts from flowing blood. CSF Pulsation Artifact Pulsatile motion of CSF (up and down the spinal canal) can cause ghost images propagating parallel to the phase-encoding direction (Figs. 55 (Figure Not Available) and 56) (Figure Not Available) and may mimic a vascular malformation. Figure 55. (Figure Not Available) Cerebrospinal fluid flow void artifact simulating AVM. Parasagittal fat-saturated FSE T2weighted image (3,000/96) shows serpiginous black artifacts (arrows) in cerebrospinal fluid (CSF) representing CSF flow artifact simulating AVM. Angiogram proved normal. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Figure 56. (Figure Not Available) Cerebrospinal fluid flow void artifact. Axial fat-saturated FSE T2-weighted image (3,466/108) shows a ring of focal, small black signal artifacts in the bright CSF, palisading around the spinal cord. These represent CSF flow artifacts. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Motion artifact can be reduced by respiratory gating,[31] [74] [123] pseudogating, breath-hold technique, and restraints.[31] [123] In addition, presaturation bands can be positioned over moving structures.[30] [113] [123] Last, sagittal images can be acquired with the phase-encoding gradient aligned along the craniocaudal direction to prevent motion artifacts traversing the spinal canal.[56] The CSF signal may vary depending on the location of CSF in the spinal canal. In cases of spinal stenosis, the free flow of CSF above the level of stenosis creates mild loss of signal, whereas below the level of stenosis stagnation of CSF results in a brighter signal intensity of CSF (Fig. 57) (Figure Not Available) .[99] Figure 57. (Figure Not Available) Cerebrospinal fluid signal variation related to slow CSF flow. Sagittal T2-weighted MR image (4,400/112) of lumbosacral spine shows very bright signal of CSF at sacral region because of decreased CSF flow there. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Paradoxic enhancement results in flow-related increased signal intensity. Because routine pulse sequences use multiple repetitions at an interval that does not allow complete recovery of longitudinal magnetization, the net signal from stationary spins is less than if complete recovery of magnetization were allowed. The flowing spins from outside the imaging volume have not been exposed to radiofrequency excitation pulses, so that their full magnetization leads to a greater signal intensity than stationary spins.[53] Moving spins are saturated, then quickly replaced by inflowing fully magnetized spins.[30] There is a greater signal intensity of moving fluids than stationary tissue in an image.[2] [20] [62] [99] Flow-related enhancement causes signal gain for both blood and CSF. Flow-related enhancement is most conspicuous on short TR and short TE images because of the hypointensity of stationary CSF on this sequence. Under these conditions, flow-related enhancement may mimic extramedullary pathology and reduce CSF cord contrast.[98] To avoid paradoxic enhancement, one should apply upstream presaturation pulses. Partial Volume Averaging Partial volume averaging occurs when two structures or an anatomic interface with different signal intensities are included within the same voxel.[20] [123] This leads to an averaging of signal intensity within the voxel.[20] Artifactually increased or decreased signal intensity may obscure or simulate pathology (Figs. 58 and 59) (Figure Not Available) . The results of partial volume averaging may cause the appearance of pseudomasses or may decrease the visibility of objects of low inherent tissue contrast.[123] Partial volume averaging is more likely with increased slice thickness and interslice gaps[20] ; selecting a thinner slice reduces the amount of artifact present. Decreasing the voxel size also is of help.[53] Partial volume averaging between the vertebral body and intervertebral disk may simulate vertebral marrow replacement, and vice versa.[18] The scoliotic spine is subject to increased partial volume effects.[74] On CT examination, partial volume averaging results in an image that has the average density of two different adjacent structures (see Fig. 58) . Figure 58. Partial volume averaging of intervertebral disk and bony vertebral body. Axial CT scan of lumbar vertebral end plate shows low density of body because of volume averaging with the disk. Figure 59. (Figure Not Available) Partial volume-averaging artifact. Axial T1-weighted image (525/12) shows a band of bright signal intensity projecting over the right pedicle and lamina of the lumbar spine (arrows), representing partial volume averaging of paraspinal fat at adjacent sections. (From Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570; with permission.) Artifact Secondary to Protocol Error Saturation Artifact. Saturation artifact may occur when angled images of the lumbar intervertebral disks are obtained. In patients with accentuated lumbar lordosis, oblique slices may overlap posteriorly. This artifact occurs when tissue adjacent to the primary slice being evaluated is partially excited. This incomplete excitation remains when the next tissue slice is stimulated by radiofrequency pulse. This artifact is sometimes referred to as crosstalk or coherence. This results in saturation effects, represented as a series of linear areas of decreased signal intensity overlying the posterior paraspinal soft tissues. This artifact may even obscure intraspinal lesions. A less acute oblique angle or transaxial images can solve this problem (Fig. 60) .[74] Figure 60. Saturation artifact. Transaxial T1-weighted images (TR 800, TE 12) A, at L4-5, and B, at L5-S1 demonstrate band-like signal loss resulting from slice acquisition overlap. C, The midline sagittal T2-weighted (TR 3200, TE 96) localizer demonstrates the overlap of adjacent slices resulting in the signal loss. Radiofrequency Interface Artifact. Static electricity from an electric blanket or other electrical appliance leads to an artifact. This artifact may also be seen with poor humidity control. It results in bandlike or "moire" patterned artifact across the entire image (Fig. 61) . Figure 61. Radiofrequency interface artifact. A, Sagittal T1-weighted image (TR 500, TE 28) and B, axial T1-weighted image (TR 500, TE 28) display a moire-like pattern resulting from the receiver coil receiving extraneous data. The improper data came from poor humidity control in a portable scanner trailer. Shading Artifact. Radiofrequency fields fall off rapidly away from the coil, causing gradual image loss of brightness. Radiofrequency Leak. This involves leakage of radiowaves from the transmitter to the receiver through the center of the image parallel to the phase-encoding direction (Fig. 62) . Figure 62. Radiofrequency leak. This sagittal T1-weighted image (TR 500, TE 10) obtained in a magnetic resonance suite with a leaky door seal exhibits a vertical streak related to the poor seal. The artifact represents a band of fluctuating intensity in the phase-encoding direction, which is superior-inferior in this image (arrowheads). Aliasing. Aliasing, or wraparound artifact, results from excitation of tissue outside the field of view, with a mismapping of the resulting signal into the field of view.[74] The signal is misplaced into the opposite side of the image.[31] [62] [123] Aliasing occurs when the field of view is smaller than the dimensions of the object being imaged in that selected plane.[53] This causes an error during analog-to-digital conversion of the MR imaging signal.[20] Undersampling of the out-of-view tissue occurs and, as a result, high-frequency signal is digitized to low-frequency components of opposite-phase polarity.[53] [62] When a small field of view is selected, oversampling techniques available on current scanners can reduce the incidence of this artifact. Aliasing artifact occurs on the slice selection and the phase-encode direction (in two-dimensional acquisitions) and the slice partition direction (for three-dimensional acquisitions).[120] [131] With aliasing, images of the upper spine can be represented on images of the lower spine.[74] Obviously, this has the potential to obscure lesions of the spine and adjacent tissues. The aliasing artifact can be avoided by increasing the field of view and phase-encoding steps. Truncation Artifact (Gibbs Phenomenon). This is seen at high-tissue-contrast interfaces, such as the discovertebral junction and CSF-cord interface.[14] [77] This artifact presents as a linear focus of alternating high and low signal intensity that propagates along the phase-encoding direction from both sides of a high-contrast interface. These signal intensity changes diminish in amplitude with increasing distance from the highcontrast interface (Fig. 63) .[53] Truncation artifacts are caused by the inability of two-dimensional Fourier transformation to reproduce signal intensity changes at high-contrast interfaces accurately.[14] [16] [21] [68] [132] There is a resultant fluctuating underestimation and overestimation of true signal intensity. Truncation artifact may result in a syrinx-like artifact most commonly seen in the cervical spine. This artifact is the result of the summation of overshoot and undershoot signal intensity changes from the high-contrast spinal cord-CSF interface.[16] [21] [68] Underestimation of signal intensity in the center of the cord on T1-weighted images and overestimation on T2weighted images results in a hyperintense and hypointense signal traversing the cord in the craniocaudal direction on sagittal images. The pseudosyrinx artifact is similar in appearance to a true syrinx on T1- and T2-weighted images. Truncation artifact can be reduced by decreasing the pixel size (by either increasing the number of phase-encoding steps or by decreasing the field of view); switching the phase- and frequency-encoding directions; filtering raw data before image reconstruction; or using alternative methods of image reconstruction.[16] [21] [68] [132] Figure 63. Truncation (Gibbs) artifact. Sagittal T1-weighted image (TR 500, TE 10) shows the alternating hypointense and hyperintense bands parallel to the sharp interface between the subcutaneous fat and the underlying musculature. This artifact results from failure of the two-dimensional Fourier transformation to accurately reproduce the signal intensity. Note that the intensity of the repetitive pattern decreases as it moves further away from the sharp interface. Other Artifacts Flair Sometimes an unusual bright artifact is produced because of unexplained technical reasons. Incomplete Fat Saturation at Edge of a Large Field of View In a large field of the spine, fat in vertebrae may not be suppressed at the top edge of the field. In this area, water being saturated instead of fat causes loss of signal from the spinal cord. ACKNOWLEDGMENTS The authors thank Mrs. E. Trent for her assistance in preparation of this manuscript. References 1. Ahmadi J, Bajaj A, Destian S, et al: Spinal tuberculosis: Atypical observations at MR imaging. Radiology 189:489-493, 1993 Abstract 2. Axel L, Summers RM, Kressel HY, et al: Respiratory effects in two-dimensional Fourier transform MR imaging. Radiology 160:795-801, 1986 Abstract 3. Babcock EE, Brateman L, Weinreb JC, et al: Edge artifacts in MR images: Chemical shift effect. J Comput Assist Tomogr 9:252-257, 1985 Abstract 4. Baker LL, Goodman SB, Perkash I, et al: Benign versus pathologic compression fractures of vertebral bodies: Assessment with conventional spin-echo, chemical-shift, and STIR MR imaging. Radiology 174:495-502, 1990 5. Barsi P, Kenez J, Varallyay G, et al: Unusual origin of free subarachnoid fat drops: A ruptured spinal dermoid rumour. Neuroradiology 34:343-344, 1992 Citation 6. Bauer A, Stabler A, Bruning R, et al: Diffusion weighted MR imaging of bone marrow: Differentiation of benign versus pathologic compression fractures. Radiology 207:349-356, 1998 7. Bergman RA, Thompson SA, Afifi AK, et al: Compendium of Human Anatomic Variation: Text, Atlas and World Literature. Baltimore, Urban & Schwarzenberg, 1988 8. Bobman SA, Atlas SW, Listerud J, et al: Postoperative lumbar spine: Contrast-enhanced chemical shift MR imaging. Radiology 179:557-562, 1991 Abstract 9. Boden SD, Davis DO, Dina TS, et al: Contrastenhanced MR imaging performed after successful lumbar disc surgery: Prospective study. Radiology 182:59-64, 1992 Abstract 10. Boden SD, Davis DO, Dina TS, et al: Postoperative discitis: Distinguishing early MR findings from normal postoperative disc space changes. Radiology 184:765-771, 1992 Abstract 11. Bradley WC: Use of contrast in MR imaging of lumbar spine. Magn Reson Imaging Clin North Am 7:439-457, 1999 12. Brateman L: Chemical shift imaging: A review. AJR Am J Roentgenol 146:971-980, 1986 Abstract 13. Braun IF, Malko JA, Davis PC, et al: The behavior of pantopaque on MR: In vivo and in vitro analyses. AJNR Am J Neuroradiol 7:997-1001, 1986 Abstract 14. Breger RK, Czervionke LF, Kass EG, et al: Truncation artifact in MR images of the intervertebral disc. AJNR Am J Neuroradiol 9:825-828, 1988 Abstract 15. Breger RK, Williams AL, Daniels DL, et al: Contrast enhancement in spinal MR imaging. AJNR Am J Neuroradiol 10:633-637, 1989 16. Bronskill MJ, McVeigh ER, Kucharczyk W, et al: Syrinx-like artifacts on MR images of the spinal cord. Radiology 166:485-488, 1988 Abstract 17. Bundschuh CV, Modic MT, Ross JS, et al: Epidural fibrosis and recurrent disc herniation in the lumbar spine: MR imaging assessment. AJR Am J Roentgenol 150:923-932, 1988 Abstract 18. Bundschuh CV, Stein L, Slusser JH, et al: Distinguishing between scar and recurrent herniated disc in postoperative patients: Value of contrast-enhanced CT and MR imaging. AJNR Am J Neuroradiol 11:949958, 1990 Abstract 19. Castillo M, Malko JA, Hoffman JC Jr: The bright intervertebral disc: An indirect sign of abnormal spinal bone marrow on T1-weighted MR images. AJNR Am J Neuroradiol 11:23-26, 1990 Abstract 20. Clark JA II, Kelly WM: Common artifacts encountered in magnetic resonance imaging. Radiol Clin North Am 26:893-920, 1988 Abstract 21. Czervionke LF, Czervionkc JM, Daniels DL, et al: Characteristic features of MR truncation artifacts. AJNR Am J Neuroradiol 9:815-824, 1988 22. Czervionke LF, Daniels DL, Ho PSP, et al: Cervical neural foramina: Correlative anatomic and MR imaging study. Radiology 169:753-759, 1988 Abstract 23. Czervionke LF, Daniels DL, Wehrli FW, et al: Magnetic susceptibility artifacts in gradient-recalled echo MR imaging. AJNR Am J Neuroradiol 9:1149-1155, 1988 Abstract 24. Dagirmanjian A, Schils J, McHenry MC: MR imaging of spinal infections. Magn Reson Imaging Clin North Am 7:525-538, 1999 25. Daniels DL, Kneeland JB, Shimakawa A, et al: MR imaging of the optic nerve and sheath: Correcting the chemical shift misregistration effect. AJNR Am J Neuroradiol 7:249-253, 1986 Abstract 26. Davis SW, Levy LM, LeBihan DJ, et al: Sacral meningeal cysts: Evaluation with MR imaging. Radiology 187:445-448, 1993 27. DeLaPaz RI: Physical basis and anatomic correlates of MR signal in the spinal cord. In Enzmann DR, DeLaPaz RL (eds): Magnetic Resonance of the Spine. St. Louis, Mosby Yearbook, 1990, 108-129 28. de Roos A, Kressel H, Spritzer C, et al: MR imaging of marrow changes adjacent to end plates in degenerative lumbar disc disease. AJR Am J Roentgenol 149:531-534, 1987 Abstract 29. Dwyer AJ, Knop RH, Hoult DJ: Frequency shift artifacts in MR imaging. J Comput Assist Tomogr 9:16-18, 1985 Abstract 30. Edelman RR, Rubin JB, Buxton RB: Flow. In Edelman RR, Hesselink JR (eds): Clinical Magnetic Resonance Imaging. Philadelphia, WB Saunders, 1990, pp 109-182 31. Edelman R, Shellock FG, Ahladis J: Practical MRI for the technologist and imaging specialist. In Edelman RR, Hesselink J (eds): Clinical Magnetic Resonance Imaging. Philadelphia, WB Saunders, 1990, pp 39-67 32. Egelhoff JC: MR imaging of congenital anomalies of the pediatric spine. Magn Reson Clin Imaging North Am 7:459-479, 1999 33. Ellis JH, Martel W, Lillie JH, et al: Magnetic resonance imaging of the normal craniovertebral junction. Spine 16:105-111, 1991 Abstract 34. Farahani K, Sinha U, Sinha S, et al: Effect of field strength on susceptibility artifacts in magnetic resonance imaging. Comput Med Imaging Graph 14:409-413, 1990 Abstract 35. Flannigan BD, Lufkin RB, McGlade C, et al: MR imaging of the cervical spine: Neurovascular anatomy. AJR Am J Roentgenol 148:785-790, 1987 Abstract 36. Frager D, Elkin C, Swerdlow M, et al: Subacute osteoporotic compression fracture: Misleading magnetic resonance appearance. Skeletal Radiol 17:123-126, 1988 Abstract 37. Geelen JAG, Langman J: Closure of the neural tube in the cephalic region of the mouse embryo. Anat Rec 189:625-640, 1977 Citation 38. Gelber ND, Ragland RL, Knorr JR: Gd-DTPA enhanced MRI of cervical anterior epidural venous plexus. J Comput Assist Tomogr 16:760-763, 1992 Abstract 39. Geremia GF, McCluney KW, Adler SS, et al: The magnetic resonance hypointense spine of AIDS. J Comput Assist Tomogr 14:785-789, 1990 Abstract 40. Glickstein MF, Miller WT, Dalinka MK, et al: Paraspinal lipomatosis: A benign mass. Radiology 163:79-80, 1987 Abstract 41. Glickstein MF, Sussman SK, et al: Time-dependent scar enhancement in magnetic resonance imaging of the postoperative lumbar spine. Skeletal Radiol 20:333-337, 1991 Abstract 42. Goldman A, Chien D, Edelman RR: Image artifacts in fast magnetic resonance imaging. Top Magn Reson Imaging 4:35-45, 1992 Abstract 43. Grenier FG, Takhtani D: Neuroradiology case of the day: Extradural lipomatosis. Radiographics 19:1397-1400, 1999 44. Grenier N, Greselle J-F, Vital J-M, et al: Normal and disrupted lumbar longitudinal ligaments: Correlative MR and anatomic study. Radiology 171:197-205, 1989 Abstract 45. Grenier N, Grossman RI, Schiebler ML, et al: Degenerative lumbar disc disease: Pitfalls and usefulness of MR imaging in detection of vacuum phenomenon. Radiology 164:861-865, 1987 Abstract 46. Gupta RK, Jena A, Kumar S: Iophendylate or spillage from epidermoid: A diagnostic dilemma on cranial MR imaging. Magn Reson Imaging 7:293-295, 1989 Abstract 47. Hackney DB, Grossman RI, Zimmerman RA, et al: MR characteristics of iophendylate (Pantopaque). J Comput Assist Tomogr 10:401-403, 1986 Abstract 48. Hahn PY, Strobel JJ, Hahn FJ: Verification of lumbar vertebral bodies: Response to letter to editor. Radiology 185:616, 1992 49. Hahn PY, Strobel JJ, Hahn FJ: Verification of lurnbosacral segments on MR images: Identification of transitional vertebrae. Radiology 182:580-581, 1992 Abstract 50. Hajek PC, Baker LL, Goobar JE, et al: Focal fat deposition in axial bone marrow: MR characteristics. Radiology 162:245-249, 1987 Abstract 51. Helms CA, Volger JB III, Genant HK: Characteristic CT manifestations of uncommon spinal disorders. Orthop Clin North Am 16:445-459, 1985 Abstract 52. Helms CA, Volger JB III, Hardy DC: CT of the lumbar spine: Normal variants and pitfalls. Radiographics 7:447-463, 1987 Abstract 53. Hendrick RE, Russ PD, Simon JM: MRI: Principles and Artifacts. New York, Raven Press, 1993 54. Henkelman RM, Bronskill MJ: Artifacts in magnetic resonance imaging. Rev Magn Reson Med 2:1-126, 1987 55. Hinks RS, Quencer RM: Motion artifacts in brain and spine MR. Radiol Clin North Am 26:737-753, 1988 Abstract 56. Holtas SL, Plewes DB, Simon JH, et al: Technical aspects on magnetic resonance imaging of the spine at 1.5 tesla. Acta Radiol 28:375-381, 1987 Abstract 57. Hueftle MG, Modic MT, Ross JS, et al: Lumbar spine: Postoperative MR imaging with Gd-DTPA. Radiology 167:817-824, 1988 Abstract 58. Isherwood I, Prendergast DJ, Hickey DS, et al: Quantitative analysis of intervertebral disc structure. Acta Radiol Suppl 369:492-495, 1986 Abstract 59. Jack CR Jr, Gehring DO, Ehman R-L, et al: Cerebrospinal fluid-iophendylate contrast on gradient-echo MR images. Radiology 169:561-563, 1988 Abstract 60. Jackson DE Jr, Atlas SW, Mani JR, et al: Intraspinal synovial cysts: MR imaging. Radiology 170:527530, 1989 Abstract 61. Jinkins JR, Matthes JC, Sener RN, et al: Spondylolysis, spondylolisthesis, and associated nerve root entrapment in the lumbosacral spine: MR evaluation. AJR Am J Roentgenol 159:799-803, 1992 Abstract 62. Johnson 1989 BA, Kelly WM: Common MRI artifacts: An overview (concluded). MRI Decisions 3:26-32, 63. Johnson DW, Farnum GN, Latchaw RE, et al: MR imaging of the pars interarticularis. AJR Am J Roentgenol 152:327-332, 1989 Abstract 64. Kato F, Mimatsu K, Kawakami N, et al: Changes seen on magnetic resonance imaging in the intervertebral disc space after chemonucleolysis: A hypothesis concerning regeneration of the disc after chemonucleolysis. Neuroradiology 34:267-270, 1992 Abstract 65. Keats TE, Lusted LB: Atlas of Roentgenographic Measurement, ed 5. Chicago, Year Book Medical Publishers, 1985 66. LeBlanc AD, Schonfeld E, Schneider VS, et al: The spine: Changes in T2 relaxation times from disuse. Radiology 169:105-107, 1988 Abstract 67. Leibner ED, Floman Y: Tunnelling Schmorl's node. Skeletal Radiol 27:225-227, 1998 Citation 68. Levy LM, DiChiro G, Brooks RA, et al: Spinal cord artifacts from truncation errors during MR imaging. Radiology 166:479-483, 1988 Abstract 69. Major NM, Helms CA: Normal variants and pitfalls in CT of the lumbar spine. Contemp Diagn Radiol 16:1-6, 1993 70. Malghem J, Maldague B, Labaisse M-A, et al: Intravertebral vacuum cleft: Changes in content after supine positioning. Radiology 187:483-487, 1993 Abstract 71. Malko JA, Hoffman JC, Jarrett PJ: Eddy-current-induced artifacts caused by an MR-compatible halo device. Radiology 173:563-564, 1989 Abstract 72. Mamourian AC, Briggs RW: Appearance of Pantopaque on MR images. Radiology 158:457-460, 1986 Abstract 73. Masaryk TJ, Boumphrey F, Modic MT, et al: Effects of chemonucleolysis demonstrated by MR imaging. J Comput Assist Tomogr 10:917-923, 1986 Abstract 74. Mirowitz SA: Pitfalls, Variants and Artifacts in Body MR Imaging. St Louis, Mosby-Year Book, 1996 75. Mirowitz SA, Shady KL: Gadopentetate dimeglumine-enhanced MR imaging of the postoperative lumbar spine: Comparison of fat-suppressed and conventional T1-weighted images. AJR Am J Roentgenol 159:385-389, 1992 Abstract 76. Mirvis SE, Geisler F, Joslyn JN, et al: Use of titanium wire in cervical spine fixation as a means to reduce MR artifacts. AJNR Am J Neuroradiol 9:1229-1231, 1988 Abstract 77. Modic MT, Masaryk TJ, Ross JS, et al: Imaging of degenerative disc disease. Radiology 168:177-186, 1988 Citation 78. Modic MT, Steinberg PM, Ross JS, et al: Degenerative disc disease: Assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193-199, 1988 79. Moulopoulos LA, Dimopoulos MA, Varma DGK, et al: Waldenstrom macroglobulinemia: MR imaging of the spine and CT of the abdomen and pelvis. Radiology 188:669-673, 1993 Abstract 80. Moulopoulos LA, Varma DGK, Dimopoulos MA: Multiple myeloma: Spinal MR imaging in patients with untreated newly diagnosed disease. Radiology 185:833-840, 1992 Abstract 81. Naidich TP, Zimmerman RA, McLone DQ, et al: Congenital anomalies of the spine and spinal cord. In Atlas SW (ed): Magnetic Resonance Imaging of the Brain and Spine, ed 2. Philadelphia, Lippincott-Raven, 1996, pp 1265-1337 82. Nowicki BH, Yu S, Reinartz J, et al: Effect of axial loading on neural foramina and nerve roots in the lumbar spine. Radiology 176:433-437, 1990 Abstract 83. Otake S, Matsuo M, Nishizawa S, et al: Ossification of the posterior longitudinal ligament: MR evaluation. AJNR Am J Neuroradiol 13:159-167, 1992 Abstract 84. Palmer WE, Suri R, Kattapuram SV: Benign versus malignant vertebral collapse: Value of a fracture line on MR images [abstract]. Presented at the 85th Scientific Assembly and Annual Meeting of RSNA. Chicago, November 28-December 1999, p 293 85. Parizel PM, Rodesch G, Baleriaux D, et al: Gd-DTPA-enhanced MR in thoracic disc herniations. Neuroradiology 1:75-79, 1989 Abstract 86. Pech P, Haughton VM: Lumbar intervertebral disc: Correlative MR and anatomic study. Radiology 156:699-701, 1985 Abstract 87. Raghavan N, Barkovich AJ, Edwards M, et al: MR imaging in the tethered spinal cord syndrome. AJR Am J Roentgenol 152:843-852, 1989 Abstract 88. Ralston MD, Dykes TA, Applebaum BL: Verification of lumbar vertebral bodies [letter]. Radiology 185:615-616, 1992 Citation 89. Ramsey RG, Zacharias CE: MR imaging of the spine after radiation therapy: Easily recognizable effect. AJNR Am J Neuroradiol 6:247-251, 1995 90. Remedios PA, Colletti PM, Raval JK, et al: Magnetic resonance imaging of bone after radiation. Magn Reson Imaging 6:301-304, 1988 Abstract 91. Ricci C, Cova M, Kang YS, et al: Normal age-related patterns of cellular and fatty bone marrow distribution in the axial skeleton: MR imaging study. Radiology 177:83-88, 1990 Abstract 92. Rosenthal DI, Hayes CW, Rosen B, et al: Fatty replacement of spinal bone marrow due to radiation: Demonstration by dual energy quantitative CT and MR imaging. J Comput Assist Tomogr 13:463-465, 1989 Abstract 93. Ross JS, Masaryk TJ, Modic MT, et al: Lumbar spine: Postoperative assessment with surface-coil MR imaging. Radiology 164:851-860, 1987 Abstract 94. Ross JS, Masaryk TJ, Modic MT, et al: MR imaging of lumbar arachnoiditis. AJR Am J Roentgenol 149:1025-1032, 1987 Abstract 95. Ross JS, Masaryk TJ, Modic MT, et al: Vertebral hemangiomas: MR imaging. Radiology 165:165-169, 1987 Abstract 96. Ross JS, Masaryk TJ, Schrader M, et al: MR imaging of the postoperative lumbar spine: Assessment with gadopentetate dimeglumine. AJNR Am J Neuroradiol 11:711-776, 1990 97. Ross JS, Modic MT, Masaryk TJ, et al: Assessment of extradural degenerative disease with Gd-DTPAenhanced MR imaging: Correlation with surgical and pathologic findings. AJNR Am J Neuroradiol 10:1243-1249, 1989 Abstract 98. Rubin JB: Basic principles of CSF flow. In Enzmann DR, DeLaPaz RL, Rubin JB (eds): Magnetic Resonance of the Spine. St Louis, CV Mosby, 1990, pp 1-63 99. Rubin JB, Enzmann DR: Harmonic modulation of proton MR precessional phase by pulsatile motion: Origin of spinal CSF flow phenomena. AJNR Am J Neuroradiol 8:307-318, 1987 Citation 100. Rubin JB, Wright A, Enzmann DR: Lumbar spine: Motion compensation for cerebral fluid on MR Imaging. Radiology 166:225-231, 1988 Abstract 101. Russell 102. Sadler EJ: Cervical disc disease. Radiology 177:313-325, 1990 Citation TW: Langman's Medical Embryology, ed 6. Baltimore, William & Wilkins, 1990 103. Schick RM, Wismer GL, Davis KR: Magnetic susceptibility effects secondary to out-of-plane air in fast MR scanning. AJNR Am J Neuroradiol 9:439-442, 1988 Abstract 104. Sether LA, Yu S: Intervertebral disc: Normal age-related changes in MR signal intensity. Radiology 177:385-388, 1990 Abstract 105. Siffring PA, Forrest TS, Frick P: Hernias of the inferior lumbar space: Diagnosis with US. Radiology 170:190, 1989 Citation 106. Simon JH, Szurnowski J, Totterman S, et al: Fat-suppression MR imaging of the orbit. AJNR Am J Neuroradiol 19:961-968, 1988 Abstract 107. Sklar E, Quencer RM, Green BA, et al: Acquired spinal subarachnoid cysts: Evaluation with MR, CT myelography, and intraoperative sonography. AJR Am J Roentgenol 153:1057-1064, 1989 Abstract 108. Smith AS, Weinstein MA, Mizushima A, et al: MR imaging characteristics of tuberculous spondylitis vs. vertebral osteomyelitis. AJR Am J Roentgenol 153:399-405, 1989 Abstract 109. Stabler A, Bellan M, Weiss M, et al: MR imaging of enhancing intraosseous disc herniation (Schmorl's node). AJR Am J Roentgenol 168:933-938, 1997 Abstract 110. Sugimura H, Kakitsubata Y, Suzuki Y, et al: MRI of ossification of ligamenture flavurn. J Comput Assist Tomogr 16:73-76, 1992 Abstract 111. Suojanen J, Wang AM, Winston KR: Pantopaque mimicking spinal lipoma: MR pitfall. J Comput Assist Tomogr 12:346-348, 1988 Abstract 112. Sze G, Brant-Zawadzki MN, Wilson CR, et al: Pseudotumor of the craniovertebral junction associated with chronic subluxation: MR imaging studies. Radiology 161:391-394, 1986 Abstract 113. Szumowski J, Simon JM: Proton chemical shift imaging. In Stark DD, Bradley WG Jr (eds): Magnetic Resonance Imaging, ed 2. St Louis, CV Mosby, 1991, pp 471-521 114. Taber KH, Herrick RC, Weathers SW, et al: Pitfalls and artifacts encountered in clinical MR imaging of the spine. Radiographics 18:1499-1521, 1988 115. Tan SB, Kpzak JA, Mawad MB: The limitation of magnetic resonance imaging in the diagnosis of pathologic vertebral fractures. Spine 16:919-923, 1991 Abstract 116. Taylor GA, Eggli KD: Lap-belt injuries of the lumbar spine in children: A pitfall in CT diagnosis. AJR Am J Roentgenol 150:1355-1358, 1988 Abstract 117. Tehranzadeh J, Rappard G, Anavim A, et al: Spinal computed tomography and magnetic resonance imaging. In Shirkhoda A (ed): Variants and Pitfalls in Body Imaging. Philadelphia, Lippincott, Williams and Wilkins, 1999, pp 535-570 118. Tertti MO, Salminen JJ, Paajanen HEK, et al: Low-back pain and disc degeneration in children: A casecontrol MR imaging study. Radiology 180:503-507, 1991 Abstract 119. Tien R, Newton TH, Dillon WP, et al: A simple method for spinal localization in MR imaging. AJNR Am J Neuroradiol 10:1232, 1989 Citation 120. Tsuruda JS, Norman D, Dillon W, et al: Three-dimensional gradient-recalled MR imaging as a screening tool for the diagnosis of cervical radiculopathy. AJR Am J Roentgenol 154:375-383, 1990 Abstract 121. Ulmer JL, Elster AD, Mathews VP, et al: Distinction between degenerative and isthmic spondylolisthesis on sagittal MR images: Importance of increased anteroposterior diameter of the spinal canal (wide canal sign). AJR Am J Roentgenol 163:411-416, 1994 Abstract 122. Waterman RE: Topographical changes along the neural fold associated with neurolatism in the hamster and the mouse. Am J Anat 146:151-171, 1976 Abstract 123. Wesbey G, Edelman RR, Harris R: Artifacts in MR imaging: Description, causes, and solutions. In Edelman RR, Hesselink JR (eds): Clinical Magnetic Resonance Imaging. Philadelphia, WB Saunders, 1990, pp 74-108 124. Wilson DA, Prince JR: MR imaging determination of the location of the normal conus medullaris throughout childhood. AJNR Am J Neuroradiol 10:259-262, 1989 Abstract 125. Winkler ML, Modic MT: MRI of the spine. Presented at the Magnetic Resonance Imaging National Symposium, Las Vegas, Nevada, 1997 126. Wismer G, Rosen B, Buston B, et al: Chemical shift imaging of bone marrow preliminary experience. AJR Am J Roentgenol 165:1031-1037, 1985 Abstract 127. Yankelevitz DF, Henschke CI, Knapp PH, et al: Effect of radiation therapy on thoracic and lumbar bone marrow: Evaluation with MR imaging. AJR Am J Roentgenol 157:87-92, 1991 Abstract 128. Yao DC, Sartoris DJ: Musculoskeletal tuberculosis. Radiol Clin North Am 33:679-689, 1995 Abstract 129. Yomashita Y, Takahashi M, Matsuno Y, et al: Spinal cord compression due to ossification of ligaments: MR imaging. Radiology 175:843-848, 1990 Abstract 130. Young IR, Cox IJ, Bryant DJ, et al: The benefits of increasing spatial resolution as a means of reducing artifacts due to field inhomogeneities. Magn Reson Imaging 6:585-590, 1988 Abstract 131. Yousem DM, Atlas SW, Goldberg HI: Degenerative narrowing of cervical spine neural foramina. AJR Am J Roentgenol 156:1229-1236, 1991 132. Yousern DM, Janick PA, Atlas SW, et al: Pseudoatrophy of the cervical portion of the spinal cord on MR images: A manifestation of the truncation artifact? AJNR Am J Neuroradiol 11:373-377, 1990 Abstract 133. Yu S, Haughton VM, Ho PSP, et al: Progressive and regressive changes in the nucleus pulposus: II. The adult. Radiology 169:93-97, 1988 Abstract 134. Yuh WTC, Zachar CK, Barloon TJ, et al: Vertebral compression fractures: Distinction between benign and malignant causes with MR imaging. Radiology 172:215-218, 1989 Abstract