Journal of Neuroimmunology 144 (2003) 53 – 60
www.elsevier.com/locate/jneuroim
Acute and chronic stress exert opposing effects on antibody
responses associated with changes in stress hormone regulation
of T-lymphocyte reactivity
Dafne M. Silberman, Miriam R. Wald, Ana Marı́a Genaro *
Centro de Estudios Farmacológicos y Botánicos, Serrano 669, 3rd floor, CP 1414, Capital Federal, Buenos Aires, Argentina
Received 9 May 2003; received in revised form 7 August 2003; accepted 18 August 2003
Abstract
Here we show that stress exerts a differential effect on T-cell-dependent antibody production. IgG production is augmented after acute
stress and impaired in a chronic situation. We found catecholamines and corticosterone levels were increased in acute situations although they
were not modified after prolonged stress conditions. However, lymphocyte sensitivity to corticosterone and catecholamines was altered under
stress conditions. These results point out the role of the adrenal’s hormones as mediators of the differential effects of stress on the immune
response providing the basis for a functional significance of stress hormone receptors on lymphocytes.
D 2003 Elsevier B.V. All rights reserved.
Keywords: Stress; Antibody production; Catecholamines; Corticosterone; Glucocorticoids
1. Introduction
Stress has long been associated with an altered homeostatic state of the organism including behavioral, endocrine
and immunological changes. The impact of stressor exposure
on the development of an immune response depends on a
variety of factors such as the duration and type of immunological challenge (McEwen, 1998). Thus, it has been
reported that acute stress enhances, whereas chronic stress
suppresses the immune function (Dhabhar and McEwen,
1997; Millan et al., 1996; Dhabhar and McEwen, 1999).
Several studies have reported that stress exposure induces
changes in cellular and humoral immunity in laboratory
animals and have provided a focus for investigating stressinduced immune compromise. Exposure of rodents to acute
stress has been shown to increase mitogen-induced T-cell
proliferation (Bauer et al., 2001; Lysle et al., 1990), T-celldependent delayed-type hypersensitivity response (Dhabhar
and McEwen, 1996) and both the T-cell-dependent and
independent antibody production (Millan et al., 1996; OkiAbbreviations: HPA, hypothalamic-pituitary-adrenal; CMS, chronic
mild stress; ANS, autonomous nervous system; GC, glucocorticoids.
* Corresponding author. Tel.: +54-11-4855-7194; fax: +54-11-48562751.
E-mail address: genaro@cefybo.edu.ar (A.M. Genaro).
0165-5728/$ - see front matter D 2003 Elsevier B.V. All rights reserved.
doi:10.1016/j.jneuroim.2003.08.031
mura et al., 1986). However, other authors found a decrease
in response to a T-cell-dependent antigen related to acute
exposure to footshock depending on the severity of the
stressor and according to the temporal proximity to immunization when the stressor was applied (Zalcman and Anisman, 1993; Zalcman et al., 1988; Laudenslager et al., 1988;
Fleshner et al., 1996; Millan et al., 1996). On the other hand,
chronic stress exposure led to a disruption of cellular
immunity (Dhabhar and McEwen, 1997; Kusnecov and
Rabin, 1993), a reduced mitogen-induced T-cell proliferation
(Silberman et al., 2002), a poor T-cell-dependent antibody
response (Fukui et al., 1997; Tournier et al., 2001) and a
disruption of cytokine secretion (Zhang et al., 1998). The
mechanisms by which these alterations occur have not been
fully elucidated. The immune system itself responds to
pathogens or other antigens with an allostatic form of its
own. At the same time, other allostatic systems, such as the
hypothalamic-pituitary-adrenal (HPA) axis and the autonomous nervous system (ANS), interfere with the immune
system (Elenkov et al., 2000; Roszman and Brooks, 1997).
Cells of the immune system, like cells of other organ
systems, express receptors for hormones and neurotransmitters (Roszman and Brooks, 1997). Triggering of these
receptors results in the modulation of the immune reactivity.
Glucocorticoids (GCs) have profound effects over the immune system development and function (Munck and Guyre,
54
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
1991). On the other hand, strong evidence has been accumulated indicating the participation of the ANS in the
modulation of lymphocyte activity via specific receptors that
in turn regulate intracellular signals, such as cyclic nucleotides levels (Elenkov et al., 2000). Moreover, it has been
suggested that an inadequate communication between the
neuroendocrine and the immune system may contribute to
the pathophysiology of disorders associated with an immune
alteration (Kavelaars et al., 2000). Numerous studies have
shown that stress, through the activation of the ANS and the
HPA axis, can be immunosuppressive and hence detrimental
to health. In particular, GC stress hormones are regarded
widely as being immunosuppressive and are used clinically
as anti-inflammatory agents. However, the established view
that GCs are immunosuppressive may not accurately describe the effects of physiological levels of endogenous GCs
on in vivo immune function. Many of the older studies that
reported immunosuppressive effects of GCs involved the
administration of high pharmacological doses of synthetic
GCs such as dexamethasone. In fact, physiological levels of
endogenous GCs can have important positive effects on
various aspects of the immune response. Regarding acquired
immunity, a number of in vivo processes related to T-cell
function are facilitated (Wilckens and De Rijk, 1997). Less is
known about the role that endogenous GCs might play in
mediating B-cell function and antibody production. Although some studies have found a positive correlation
between endogenous stress-induced GCs increases and antibody production (Moynihan et al., 1994), other experiments have yielded a negative correlation between
endogenous GC levels and splenic antibody-producing cells
(Del Rey et al., 1984). In addition, administration of GCs has
been reported to either increase (Tuchinda et al., 1972) or
have no effect (Fleshner et al., 1996) on plasma antibody
levels.
It seems relevant to distinguish between acute and
chronic stress effects and the particular interaction between
the immune system and the HPA and ANS in both situations. The aim of the present study was to investigate the
effect of acute versus chronic stress in the generation of an
in vivo specific antibody response. Moreover, we examined
the catecholamines and corticosterone levels and their effect
on lymphocyte reactivity in both acute and chronic stress
conditions. Finally, the potential role of endogenous corticoids and catecholamines on the antibody production in stress
conditions is discussed.
2. Materials and methods
2.1. Drugs
Con A, epinephrine, corticosterone and anti-mouse
monoclonal antibodies were purchased from Sigma. [3H]Thymidine ([3H]-tdR) (20 Ci/mmol) were purchased from
New England Nuclear (NEN), Life Science products.
Other materials were obtained from standard commercial
sources.
2.2. Mice
Inbred female BALB/c mice were purchased from the
Instituto Nacional de Tecnologı́a Agropecuaria (INTA). All
animals were between 60 and 100 days of age. Animals
were housed on a 12-h light/dark cycle under controlled
temperatures (18 – 22 C) and were cared in accordance
with the principles and guidelines of the Guide for the
Care and Use of Laboratory Animals, US National Research Council, 1996. All animals were sacrificed by
decapitation.
2.3. Stress protocol
Animals were randomly assigned to experimental groups:
non-stressed (Control, n = 30), acute stressed (Acute, 2h restraint exposure, n = 30) or chronically stressed (CMS,
subjected to chronic mild stress for 6 weeks, n = 30, or for 1
to 6 weeks, n = 36). Restraint was performed by placing each
animal in a well-ventilated polypropylene tube (2.8-cm
diameter 11.5-cm length) for 2 h starting at 10.00 AM.
Animals were not physically compressed and did not experience pain. In chronic stress experiments, animals were
subjected to the CMS model slightly modified from that
previously used in mice by Monleon et al. (1995). The stress
scheme consisted of: one 16-h period of water deprivation;
two periods of continuous overnight illumination; two periods (7 and 17 h) of 45j cage tilt; one 17-h period in a soiled
cage (100 ml water in sawdust bedding); one period (8 h) of
food deprivation; one 17-h period of paired housing (animals
are always housed in the same pairs, but the location
alternates between the home cages of each member of the
pair). The stressors were scheduled throughout the week, in a
similar manner to that previously described (Monleon et al.,
1995). Acute animals were kept in their home cages for 15
min following stress and then sacrificed. Chronic animals
were left undisturbed in their home cages 18 h prior to
sacrifice.
2.4. Immunizations
Acute animals were kept in their home cages for 15 min
following stress and chronic animals were left undisturbed
in their home cages 18 h prior to immunization. Sheep red
blood cells (SRBC) were used as immunogen to evaluate
T-cell-dependent humoral response and lipopolysaccharide
(LPS) was used to determinate T-cell-independent humoral
response. For SRBC response, mice (n = 12) were intraperitoneally (i.p.) immunized on day 0 and boosted on day
11 with 0.2 ml of 2.5% SBRC in saline. Blood samples
were collected for antibody determination on day 10
(primary response) and on day 18 (secondary response).
For LPS, each mouse (n = 12) received an i.p. injection of
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
10 Ag LPS in 0.1 ml saline and blood samples were
collected on day 10. Mice injected with vehicle were used
as controls.
55
epinephrine or corticosterone, each at concentrations ranging from 1 10 9 M to 1 10 5 M.
2.8. Catecholamines assay
2.5. Antibody titers
Serum obtained from retroorbital blood samples was
stored at 20 jC until assayed. Quantitative enzyme-linked
immunoadsorbent assay (ELISA) was performed to determine SRBC-specific and LPS-specific antibodies. Briefly,
96 well plates (Maxisorp immunoplates, Nunc) were coated
overnight with SRBC membranes (10 Ag/ml) or LPS (2 Ag/
ml). Dilutions of sera were added and incubated 2 h at room
temperature, plates were washed, and samples were incubated with a goat IgG anti-mouse IgM or IgG phosphatase
alkaline conjugated and p-nitrophenylphosphatase as substrate for developing coloration that was read at 405 nm.
Reactions were considered positive when optical density
(O.D.) values were above the mean value plus 2 S.D. of
normal sera (sera from non-immunized and/or vehicle
injected mice that gave non-statistical differences among
them).
2.6. Cell suspensions and culture conditions
Spleen lymphoid cell suspensions from control and stress
exposed mice were obtained as previously described (Silberman et al., 2002). Briefly, spleens were removed and
disrupted through a 1-mm metal mesh, and cell suspension
was filtered through a 10-Am nylon mesh. The suspension
was depleted of non-lymphoid cells after centrifugation over
Ficoll/Hypaque. After three washes in RPMI 1640, cells
were re-suspended in RPMI 1640 supplemented with 10%
of batched-tested non-stimulatory fetal calf serum, 2 mM
glutamine, 100 U/ml of penicillin, 100 Ag/ml of streptomycin and 50 AM h-mercaptoethanol.
2.7. Mitogen assay
Proliferation was determined by culturing 2 105 cells
per well in 96-well plates in 0.150 ml triplicate aliquots in
supplemented medium. Aliquots of 50 Al of Con A were
added to the microcultures to yield the optimal mitogen
concentration (2 Ag/ml) according to previous dose – response curves. In control cultures, stimulants were replaced
by 50 Al of culture medium. Then cells were cultured at 37
jC in a 5% CO2 atmosphere for different periods. Mitogenic
activity was measured by adding 1 ACi [3H]-thymidine per
well for the last 18-h period of culture. Thymidine incorporation was measured by scintillation counting after retention over GF/C glass-fiber filters (Whatman) of the acidinsoluble macromolecular fraction. Mitogen-stimulated cells
displayed the expected proliferation kinetic, with a peak of
proliferation at the third day of culture. To analyze the
influence of catecholamine and/or corticosterone on the
proliferative response, co-incubation was carried out with
Catecholamine concentrations were determined in spleen
samples from animals under different experimental conditions by the fluorometric assay described by Laverty and
Taylor (1968). Briefly, spleens were homogenized in 12.5%
sodium sulfite, 10% EDTA in 0.4 N percloric acid. After 24
h at 4 jC, homogenates were centrifuged at 5000 rpm for 10
min. Supernatants were brought to pH 8.2 and seeded in a
pre-washed alumina column. Eluates were oxidized with
iodine in an alkaline medium. The fluorescence was
recorded at 375 nm in a spectrofluorometer using an
excitation source of 325 nm.
2.9. Corticosterone determination
To avoid fluctuations on plasma cortisone levels due to
circadian rhythmus, animals were bled at 12.00 AM on the
day of the sacrifice. Blood from animals under different
experimental conditions was collected on ice in 0.25 M
EGTA and separated in a refrigerated centrifuge. Plasma
was stored at 80 jC until assay was performed. Corticosterone levels were determined using a highly sensitive
double antibody radioimmunoassay kits (ICN Biomedical).
2.10. Statistical analysis
Student’s t-test for unpaired values was used to determine
the level of significance for normally distributed data.
Group differences were tested by one-way analysis of
variance (ANOVA). Proliferation data were analyzed by
two-way ANOVA with fixed factors for experimental
groups and hormone concentrations. When multiple comparisons were necessary after ANOVA, the Student – Newman – Keuls test was applied. Antibody production data
were not normally distributed, so the non-parametric statistic Kruskal – Wallis test was performed, post hoc analysis
was carried out using the Dunn’s Multiple Comparison test.
Differences between means were considered significant if
p V 0.05.
3. Results
3.1. Acute stress enhanced whereas chronic stress
impaired IgG antibody production after T-dependent
antigen immunization
To investigate whether stress exposure was associated
with changes in antibody production, we examined the
humoral response to SRBC—a thymus-dependent antigen—in non-exposed (control), acute and 6-week-chronic
mild stress-exposed mice (to be referred to as ‘‘Acute’’ and
56
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
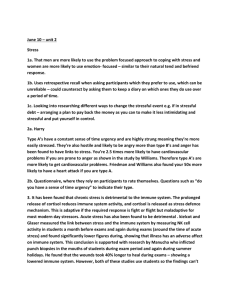
‘‘CMS’’, respectively). We found that the anti-SRBC IgM
primary response (day 10) was not significantly different
(KWs = 0.5528, n.s.) between Acute, CMS and control
animals (Fig. 1, panel A). In contrast, anti-SRBC IgG
primary titers were significantly different between groups
(KWs = 21.26, p < 0.0001). Antibodies production was significantly ( p < 0.05) higher in Acute animals and significantly ( p < 0.05) lower in CMS mice than those found in
controls (Fig. 1, panel B). On day 18, after the first
immunization and one booster injection (secondary response), titers of anti-SRBC IgM secondary response were
similar in controls, Acute and CMS animals (KWs =
0.6721, n.s.) (Fig. 1, panel C). However, stress treatment
induced a significant difference in anti-SRBC IgG production (KWs = 21.1, p < 0.0001). Thus, a significant ( p <
0.05) increase in anti-SRBC IgG production was found
.
Fig. 1. Antibody titers following SRBC and LPS immunization in control and stress exposed mice. Control (5), 2-h Acute ( ) and 6-week CMS (E) exposed
mice were immunized with SRBC, 2.5% in saline (panels A and B), and boosted on day 11 with 2.5% of SRBC in saline (panels C and D) or immunized with
LPS (10 Ag in saline) (panel E). Serum was collected on day 10 (panels A, B and E) or on day 18 (panels C and D) and assayed for the presence of IgM (panels
A, C and E) or IgG (panels B and D) by ELISA. The curves shown are representative of eight experiments performed by duplicate. Each experiment was
performed with one or two sera of each experimental condition. Dotted line represents the OD values + 2 S.D. of normal sera.
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
when animals were submitted to acute stress immediately
before the first antigen challenge (Fig. 1, panel D) regardless the acute stress was administered before the booster
(data not shown). On the contrary, when acute stress was
not administered before the first challenge, no effect was
found, not even in those animals submitted to acute stress
before the booster (data not shown). On the other hand,
anti-SRBC IgG production on day 18 was dramatically
diminished in CMS mice ( p < 0.05) (Fig. 1, panel D). To
confirm that stress affects predominantly the T-cell function, we evaluated the humoral response after a thymusindependent antigen (LPS) challenge. As shown in Fig. 1
(panel E), no significant differences (KWs = 5.098, n.s.)
were found in the anti-LPS titers among Acute, CMS and
control mice.
3.2. Exposure to acute but not chronic stress-induced
changes in catecholamine and corticosterone levels
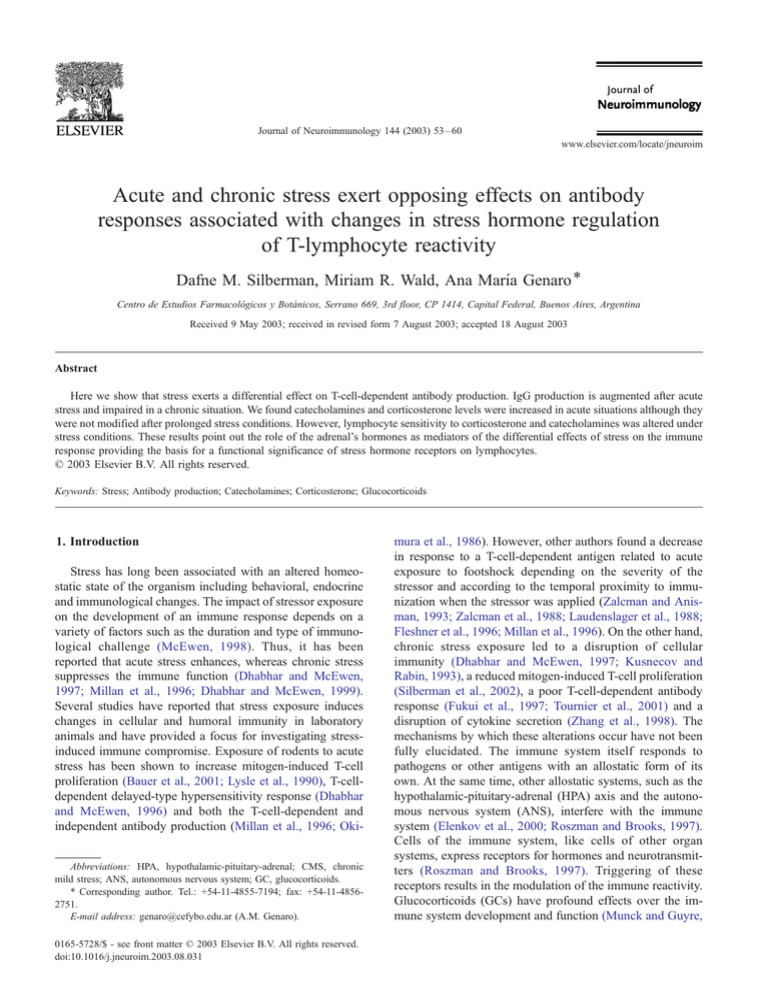
In an attempt to investigate the participation of catecholamines and corticosterone in the disruption of T-cell-dependent antibody response, we evaluate these hormone levels
after stress exposure. As expected, acute stress induced a
significant increase in serum corticosterone level and in the
splenic catecholamine content. However, no significant
variations in hormone levels between controls and 6-week
57
CMS-exposed mice were found (Fig. 2, panel A). It seems
that hormonal levels were adapted following long-lasting
chronic stress exposure. Indeed, we have observed an
increase in serum corticosterone and catecholamine levels
during the first 3 weeks of CMS exposure returning later to
basal values (Fig. 2, panel B).
3.3. Lymphocytes from mice exposed to acute and chronic
stress exhibited changes in stress hormones sensitivity
We analyzed the effect of corticosterone and catecholamines on lymphocyte reactivity. Fig. 3 shows the effect of
catecholamines (panel A) and corticosterone (panel B) on
mitogen-induced T-cell proliferation. Addition of high concentrations of epinephrine to the cultures resulted in an
inhibition of Con A-induced proliferation of control lymphocytes. A biphasic effect was observed in lymphocytes
from Acute mice (stimulatory for low concentrations and
inhibitory for high ones). However, an inhibitory effect
respect to control was induced on lymphocytes from CMS
mice at all the concentrations of epinephrine tested. Twoway ANOVA revealed that epinephrine significantly altered
mitogen-induced T-cell proliferation ( F[4,75] = 25.11,
p < 0.0001) depending on catecholamine concentrations.
Significant stress effect ( F[2,75] = 58.81, p < 0.0001) was
observed for proliferation when cells were incubated with
Fig. 2. Catecholamines and corticosterone levels in control and stress exposed animals. Control (open bars), Acute (dashed bars) and CMS (dark bars) exposed
mice were killed at 12.00 AM and plasma and spleen were collected in order to determine corticosterone levels and catecholamine content, respectively. Panel
A shows the results obtained from control, 2-h acute and 6-week CMS-exposed mice. Panel B shows the results for control and 1- to 6-week CMS-exposed
mice. Data shown represents the mean F S.E.M. of six animal of each group. *p < 0.05 with respect to the corresponding control value. **p < 0.01 with respect
to the corresponding control value.
58
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
proliferation of CMS cells with respect to the inhibition
observed for control cells (Fig. 3, panel A). On the other
hand, the addition of corticosterone resulted in a dosedependent modulation of the proliferative response from
control, Acute and CMS mice. Two-way ANOVA revealed
that corticosterone significantly influence Con A-induced Tcell proliferation ( F[4,75] = 138.6, p < 0.0001) dependent on
the steroid concentration. Significant stress effect was observed for T-cell proliferation under these conditions
( F[2,75] = 75.35, p < 0.0001). Moreover, there was a statistically significant interaction between group and steroid
concentration ( F[8,75] = 3.7080, p < 0.0001). Post hoc analysis revealed that lymphocytes from stressed groups
exhibited changes in corticosterone effects compared to
the control group. The stimulatory effect observed when
low concentrations of corticosterone were added to cell
culture was significantly greater on Acute lymphocyte
proliferation. In contrast, the stimulatory effect was significantly lower on lymphocytes from CMS mice compared to
that found in controls (Fig. 3, panel B). In addition, the
inhibitory effect of mitogen-induced T-cell proliferation
observed when high concentrations of corticosterone were
added to the culture was lower on acute lymphocytes and
higher on CMS lymphocytes compared to the effect
obtained on control lymphocyte proliferation (Fig. 3, panel
B). It is important to note that, according to our previous
results, basal Con A-induced proliferation was decreased in
lymphocytes from animals exposed to CMS. No significant
differences were observed in the basal proliferation of
lymphocytes from acute animals respect to non-exposed
lymphocytes (legend, Fig. 3).
Fig. 3. Effect of epinephrine and corticosterone on Con A induced T-cell
proliferative response. Con A-stimulated T cells from Control (5), 2-h
Acute ( ) and 6-week CMS-exposed mice (E) were co-incubated with the
indicated concentrations of epinephrine (panel A) and corticosterone (panel
B). After 3 days of culture 3H-thymidine incorporation was determined.
Results are expressed as a percentage of proliferation in the absence of
epinephrine or corticosterone (basal proliferation). Values for basal
proliferation were 34,654 F 5233 dpm for non-exposed cells, 42,615 F
5789 dpm for acute-exposed cells and 18,045 F 2024 dpm for CMSexposed cells. Neither of both hormones affected unstimulated cells. Data
showed represent the mean F S.E.M. of six independent experiments of
triplicate cultures performed with one animal of each experimental
condition. *p < 0.05 with respect to the corresponding control value.
**p < 0.01 with respect to the corresponding control value.
.
exogenous epinephrine. Moreover, a significant interaction
between group and hormone concentration was observed
( F[8,75] = 25.11, p = 0.0371). Post hoc analysis revealed
that lymphocytes from both acute and chronic stress groups
exhibited an altered sensitivity to epinephrine effect compared to cells from control group. Thus, low concentrations
of epinephrine added to Acute cell culture induced a
significant stimulation of mitogen-induced T-cell proliferation. This effect is not observed on normal stimulated cells.
However, the addition of epinephrine to lymphocytes cultures resulted in a significantly higher inhibition on the
4. Discussion
Many studies have suggested that stress has profound
effects on immune functions (McEwen, 1998). The consequences of the physiological stress response are generally
adaptive in the short run, but can be damaging when stress is
chronic and long lasting (Dhabhar and McEwen, 1997,
1999; Millan et al., 1996). It has been known for some
time that stress and emotions are associated with neurochemical and hormonal changes that in turn influence the
reactivity of cells of the immune system (Maier et al., 1994).
Activation of both the HPA axis and the sympatheticadrenal-medullar axis plays a key role in the response to
psychological stress (Elenkov et al., 2000; Maier et al.,
1994). The present work was undertaken to investigate the
effect of acute and chronic stress exposure on the antibody
production and the participation of catecholamines and
glucocorticoids as mediators of stress on the immune
response. A 2-h restrain treatment was used as an acute
stress model. For chronic stress, we choose the CMS model.
This is a heterotypic model that implicates a chronic low
grade stress offering a reasonable approximation to the
diverse stresses of daily life. In this sense, we believe that
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
CMS model offers a more realistic simulation of the
biological effects of chronic stress than chronic homotypic
stress model.
The results indicated that humoral response to a T-celldependent antigen but not to a T-cell-independent antigen
is increased after acute stress exposure. In contrast, chronic
stress had an immunosupressive effect on IgG production
indicating an impaired isotype switching without affecting
IgM production. This impairment was not only due to a
delay in the kinetics of IgG production, since a rise in the
antibody titer was not observed afterwards (followed out to
2-week post-secondary challenge, data not shown). However, other mechanisms such us poor accessory function,
cytokine production and co-stimulation could be implicated. Taken together, these findings would suggest that stress
is affecting mainly the T-dependent humoral response.
These results are in agreement with our previous findings
showing an impaired T-cell proliferative response in CMS
mice (Silberman et al., 2002). Several studies have indicated an alteration of the antibody response to immunization in the context of chronic stress. Thus, poorer antibody
response to hepatitis B or influenza vaccine has been
observed in family caregivers of Alzheimer patients as
well as others experiencing severe stress (Glaser et al.,
1998; Jabaaij et al., 1996; Kiecolt-Glaser et al., 1996).
Evidence for a decreased antibody production and impaired isotype switching in response to immunization with
a thymus-dependent antigen has been reported in a genetic
model of stress (Murray et al., 2001). Likewise, it was
shown that chronic restraint stress induced severe disruption of the functional ability of lymphocyte to proliferate
and to produce cytokines and antibody titers against
tetanus toxin (Tournier et al., 2001). Concerning to acute
stress, evidence for enhanced immune function after exposure to footshock proximal to the induction phase of the
immune reaction has been reported (Wood et al., 1993). In
addition, Millan et al. (1996) found that short restraint
stress (2 h over 2 consecutive days) enhanced the primary
serum T-cell-dependent antibody response to SRBC. However, other authors found a decrease in response to a Tcell-dependent antigen related to acute exposure to footshock (Laudenslager et al., 1988; Fleshner et al., 1996).
These contradictory results can be explained by the fact
that the response of the immune system to stress depends
on several factors such as the intensity and/or the duration
of the stress, the antigenic challenge and the temporal
proximity to immunization when the stressor is applied
(Zalcman and Anisman, 1993; Zalcman et al., 1988;
Millan et al., 1996). Regarding the role of catecholamines
and corticosterone in stress effects, we found that their
levels were increased in acute situations but they were not
modified after prolonged stress periods. Previously, we
observed no significant variations in corticosterone and
catecholamine levels between control and 8-week CMSexposed animals (Ayelli-Edgar et al., 2003). These results
agree with those obtained by Azpiroz et al. (1999), who
59
did not observe differences neither in hypothalamic nor in
hippocampal norepinephrine levels as well as serum corticosterone concentration in animals under CMS conditions. These data suggest that there might be an adrenal
(cortical or medullar) activation after acute stress but
hormonal levels were adapted after long-lasting stress
exposure. In fact, the habituation of the HPA axis after
prolonged stress situations has been described (Mizoguchi
et al., 2001). Indeed, we have observed an increase in
serum corticosterone and catecholamine levels during the
first 2 weeks of CMS exposure that return to basal values
after 3 weeks. On the other hand, lymphocyte sensitivity to
the stress hormones effect is also altered. The hormone’s
stimulatory effect was increased under an acute situation,
whereas the inhibitory effect was augmented under a
chronic stress scheme remarking the functional significance of lymphocyte stress hormone receptors. Bauer et
al. (2001) demonstrated a rapid change in steroid sensitivity that occurs at the levels of splenocyte during stress
exposure. Actually, there is a renewed interest in the
physiological role that adrenal GCs play in regulating the
in vivo immune response. This renewed interest stems
from an emerging realization that the established view that
GCs are generally immunosuppressive may not accurately
describe the effects of physiological levels of endogenous
GCs on in vivo immune function. In fact, it has been
demonstrated that endogenous GCs play an important
regulatory role in the optimal in vivo production of antibodies (Fleshner et al., 1996). Moreover, Dhabhar and
McEwen (1999) showed that low doses and acute administration of corticosterone and epinephrine produce
immuno-enhancement. In contrast, high doses of stress
hormones or its chronic administration induces immunosuppression. The possibility that early increments of these
hormone levels may be contributing to induce long-lasting
changes in catecholamines and corticosterone lymphocytes
sensitivity is under study.
Summarizing, to our knowledge, the present study is the
first experimental evidence that points out that stress exerts
a differential effect on T-cell-dependent antibody production
affecting, mainly, the IgG isotype switching. Whereas IgG
production is augmented by acute stress exposure, it is
impaired in a chronic condition. Catecholamines and corticosterone exert either a stimulatory or an inhibitory effect on
lymphocyte reactivity depending on the concentration tested. Acute stress induced an enhancement of lymphocyte’s
sensitivity to the stimulatory effect of stress hormones,
whereas chronic stress increased lymphocyte’s sensitivity
to the inhibitory effect of these hormones. These findings
suggest an important role for adrenal hormone receptors on
lymphocytes and indicate a physiological and adaptive
mechanism through which epinephrine and corticosterone
could act as mediators for the differential effects of stress on
the immune system. Since stress is a common aspect of
modern life and it participates in the etiology of many
diseases, the emerging results of these studies will be
60
D.M. Silberman et al. / Journal of Neuroimmunology 144 (2003) 53–60
helpful to improve and develop new and more efficient
biomedical treatments.
Acknowledgements
This work was supported by grant PIP 0543/98 from
CONICET. The authors wish to thank Daniel Gonzalez and
Eduardo Nieves for their invaluable help in the animal stress
model and Marı́a Rosa Gonzalez Murano for the technical
assistance.
References
Ayelli-Edgar, V., Silberman, D.M., Cremaschi, G., Zieher, L.M., Genaro,
A.M., 2003. Altered lymphocyte catecholamine reactivity in mice subjected to chronic mild stress. Biochem. Pharmacol. 65, 15 – 23.
Azpiroz, A., Fano, E., Garmendia, L., Arregi, A., Cacho, R., Beitia, G.,
Brain, P.F., 1999. Effects of chronic mild stress (CMS) and imipramine
administration, on spleen mononuclear cell proliferative response, serum corticosterone level and brain norepinephrine content in male mice.
Psychoneuroendocrinology 24, 345 – 361.
Bauer, M.E., Perks, P., Lightman, S.L., Shanks, N., 2001. Restraint stress is
associated with changes in glucocorticoid immunoregulation. Physiol.
Behav. 73, 525 – 532.
Del Rey, A., Besedovsky, H., Sorkin, E., 1984. Endogenous blood levels of
corticosterone control the immunologic cell mass and B cell activity in
mice. J. Immunol. 133, 572 – 575.
Dhabhar, F.S., McEwen, B.J., 1996. Stress-induced enhancement of antigen-specific cell-mediated immunity. J. Immunol. 156, 2608 – 2615.
Dhabhar, F.S., McEwen, B.J., 1997. Acute stress enhances while chronic
stress suppresses immune function ‘‘in vivo’’: a potential role for leukocyte trafficking. Brain Behav. Immun. 11, 286 – 306.
Dhabhar, F.S., McEwen, B.J., 1999. Enhancing versus suppressive effects of stress hormones on skin immune function. Proc. Natl. Acad.
Sci. U. S. A. 96, 1059 – 1064.
Elenkov, I.J., Wilder, R.L., Chrousos, G.P., Vizi, E.S., 2000. The symphathetic nerve—an integrative interface between two supersystem: the
brain and the immune system. Pharmacol. Rev. 52, 595 – 638.
Fleshner, M., Brennan, F.X., Nguyen, K., Watkins, L.R., Maier, S.F., 1996.
RU-486 blocks differentially suppressive effect of stress on in vivo antiKLH immunoglobulin response. Am. J. Physiol. 271, R1344 – R1352.
Fukui, Y., Sudo, N., Yu, X.-N., Nukina, H., Sogawa, H., Kubo, C., 1997.
The restraint stress-induced reduction in lymphocyte cell number in
lymphoid organs correlates with the suppression of in vivo antibody
production. J. Neuroimmunol. 44, 33 – 42.
Glaser, R., Kiecolt-Glaser, J.K., Malarkey, W.B., Sheridan, J.F., 1998. The
influence of psychological stress on the immune response to vaccines.
Ann. N.Y. Acad. Sci. 840, 649 – 655.
Jabaaij, L., van Hattum, J., Vingerhoets, J.J., Oostveen, F.G., Duivenvoorden, H.J., Baillieux, R.E., 1996. Modulation of immune response to
rDNA hepatitis B vaccination by psychological stress. J. Psychosom.
Res. 41, 129 – 137.
Kavelaars, A., Kuis, W., Knook, L., Sinnema, G., Heijen, C.J., 2000. Disturbed neuroendocrine – immune interactions in chronic fatigue syndrome. J. Clin. Endocrinol. Metab. 85, 692 – 696.
Kiecolt-Glaser, J.K., Glaser, R., Gravenstein, S., Malarkey, W.B., Sheridan,
J., 1996. Chronic stress alters the immune response to influenza virus
vaccine in older adults. Proc. Natl. Acad. Sci. U. S. A. 93, 3043 – 3047.
Kusnecov, A.W., Rabin, B.S., 1993. Inescapable footshock exposure differentially alters anti- and mitogen-stimulated spleen cell proliferation in
rats. J. Neuroimmunol. 44, 33 – 42.
Laudenslager, M.L., Fleshner, M., Hofstadter, P., Held, P.E., Simons, L.,
Maier, S.F., 1988. Suppression of specific antibody production by inescapable shock: stability under varying conditions. Brain Behav. Immun. 2, 445 – 452.
Laverty, R., Taylor, K., 1968. The fluorometric assay of catecholamines
and related compounds: improvement and extension to the hydroxyindole technique. Ann. Biochem. 22, 269 – 279.
Lysle, D., Cunnick, J., Rabin, B., 1990. Stressor-induced alteration of
lymphocyte proliferation in mice: evidence for enhancement of mitogenic responsiveness. Brain Behav. Immun. 4, 269 – 277.
Maier, S.F., Watkins, L.R., Fleshner, M., 1994. Psychoneuroimmunology.
The interface between behavior, brain and immunity. Am. Psychol. 49,
1004 – 1017.
McEwen, B.S., 1998. Protective and damaging effects of stress mediators:
allostasis and allostatic load. N. Engl. J. Med. 338, 171 – 179.
Millan, S., Gonzalez-Quijano, M.I., Giordano, M., Soto, L., Martı́n, A.I.,
Lopez-Calderon, A., 1996. Short and long restraint differentially affect
humoral and cellular immune functions. Life Sci. 59, 1431 – 1442.
Mizoguchi, K., Yuzurihara, M., Ishige, A., Sasaki, H., Chui, H., Tabira, T.,
2001. Chronic stress differentially regulates glucocorticoid negative
feedback in rats. Psychoneuroendocrinology 26, 443 – 459.
Monleon, S., D’Aquila, P., Parra, A., Simon, V.M., Brain, P.F., Willner, P.,
1995. Attenuation of sucrose consumption in mice by chronic mild
stress and its restoration by imipramine. Psychopharmacology 117,
453 – 457.
Moynihan, J.A., Karp, J.D., Cohen, N., Cocke, R., 1994. Alterations in
interleukin-4 and antibody production following pheromone exposure:
role of glucocorticoids. J. Neuroimmunol. 54, 51 – 58.
Munck, A., Guyre, P.M., 1991. Glucocorticoids and immune function. In:
Ader, R., Felten, D.L., Cohen, N. (Eds.), Psychoneuroimmunology.
Academic Press, Rochester, pp. 447 – 475.
Murray, S.E., Lallman, H.R., Heard, A.D., Rittenberg, M.B., StenzelPoore, M.P., 2001. A genetic model of stress displays decreased lymphocytes and impaired antibody responses without altered susceptibility
to Streptococcus pneumoniae. J. Immunol. 167, 691 – 698.
Okimura, T., Ogawa, M., Yamauchi, T., Sasakii, Y., 1986. Stress and immune responses IV-adrenal involvement in the alteration of antibody
responses in restraint-stressed mice. Jpn. J. Pharmacol. 41, 237 – 245.
Roszman, T.L., Brooks, W.H., 1997. Interactive signaling pathways of the
neuroendocrine-immune network. Chem. Immunol. 69, 203 – 222.
Silberman, D.M., Wald, M., Genaro, A.M., 2002. Effects of chronic mild
stress on lymphocyte proliferative response. Participation of serum thyroid hormones and corticosterone. Int. Immunopharmacol. 2, 487 – 497.
Tournier, J.N., Mathieu, J., Mailfert, Y., Multon, E., Drouet, C., Jouan, A.,
Drouet, E., 2001. Chronic restraint stress induces severe disruption of
the T-cell specific response to tetanus toxin vaccine. Immunology 102,
87 – 93.
Tuchinda, M., Newcomb, R.W., DeVald, B.I., 1972. Effect of prednisone
treatment on the human immune response to keyhole limpet hemocyanin. Int. Arch. Allergy 42, 533 – 544.
Wilckens, T., De Rijk, R., 1997. Glucocorticoids and immune function:
unknown dimensions and new frontiers. Immunol. Today 18, 418 – 424.
Wood, P.G., Karol, M.H., Kusnecov, A.W., Rabin, B.S., 1993. Enhancement of antigen-specific humoral and cell-mediate immunity by electric
footshock stress in rats. Brain Behav. Immun. 7, 121 – 134.
Zalcman, S., Anisman, H., 1993. Acute and chronic stressor effects on the
antibody response to sheep red blood cells. Pharmacol. Biochem. Behav. 46, 445 – 452.
Zalcman, S., Minkiewicz-Janda, A., Richter, M., Anisman, H., 1988. Critical periods associated with stressor effects on antibody titers and on the
plaque-forming cell response to sheep red blood cells. Brain Behav.
Immun. 2, 254 – 266.
Zhang, D., Kishihara, K., Wang, B., Mizobe, K., Kubo, C., Nomoto, K.,
1998. Restraint stress-induced immunosuppression by inhibiting leukocyte migration and Th1 cytokine expression during intraperitoneal infection of Listeria monocytogenes. J. Neuroimmunol. 92, 139 – 151.