2016 Billing Guide for
®
REMICADE (infliximab)
Table of Contents
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
Factors That Influence Coverage . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2
REMICADE® (infliximab) Quick Reference Guide . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
Coding for REMICADE® and Drug Administration Services . . . . . . . . . . . . . . . . . . . . . . 4
Indications and Usage . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
REMICADE® Coding Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
ICD-10-CM Diagnosis Codes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
CPT® and HCPCS Codes for Drugs and Drug Administration . . . . . . . . . . . . . . . . . . . . 7
Physician Office Setting . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
Place of Service Codes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
Hospital Outpatient Setting . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
Home Infusion Providers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
Other Coding Considerations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
REMICADE® Billing Units . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Billing With National Drug Codes (NDCs) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Partial Additional Hours of Infusion Time . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Modifiers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Distinct Procedural Service . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
CMS Discarded Drug Policies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
Same Day Evaluation and Management Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
Payment for REMICADE® and Drug Administration Services . . . . . . . . . . . . . . . . . . .
17
Medicare Payment to Physician Offices . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
Medicare Payment to Hospital Outpatient Departments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
Medicare Policy for Other Healthcare Providers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
Medicaid Payment Policies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
Commercial Payers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
Home Infusion Reimbursement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
Medicare Part D . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
i
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
20
Appendices
Appendix A: Sample Claim Forms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
Appendix B: Medical Necessity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26
Appendix C: Appeals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26
Appendix D: Working With Specialty Pharmacy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27
Appendix E: Medicare Quality Programs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28
Appendix F: ICD-10-CM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29
Appendix G: Resources . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 31
Important Safety Information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
Please see Important Safety Information, full Prescribing Information, and Medication
Guide for REMICADE® (infliximab).
The information in this guide is provided to assist you in understanding the reimbursement process. It is intended to
help providers in accurately obtaining reimbursement for healthcare services. It is not intended to increase or maximize
reimbursement by any payer. We strongly suggest that you consult your payer organization with regard to local reimbursement
policies. This document is presented for informational purposes only and is not intended to provide reimbursement or legal
advice. Laws, regulations, and policies concerning reimbursement are complex and updated frequently. While Janssen
Biotech, Inc., has made an effort to be current as of the issue date of this document, the information may not be as current
or comprehensive when you view it. Please consult with your counselor reimbursement specialist for any reimbursement
or billing questions. Similarly, all Current Procedural Terminology (CPT®) & Healthcare Common Procedural Coding System
(HCPCS) billing codes are supplied for informational purposes only and represent no statement, promise or guarantee by
Janssen Biotech, Inc., that these codes will be appropriate or that reimbursement will be made.
CPT © 2015 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS/DFARS
Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, and/or related components are not assigned by the AMA, are
not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The
AMA assumes no liability for the data contained or not contained herein. Current Procedural Terminology (CPT)® 2015. American Medical Association. All
rights reserved.
01ii
Introduction
Janssen Biotech, Inc., has developed this Billing Guide to help healthcare providers and billing staff
understand third-party reimbursement for REMICADE® (infliximab). Specifically, this guide presents
general information on coverage, coding, reimbursement, and claims submission for REMICADE®.
In addition, it provides information on how to manage denied claims and information about other
reimbursement-related topics that are relevant to the sites of care in which REMICADE® is administered.
The information contained in this guide is intended to provide a general understanding of the
reimbursement process and is not intended to assist providers in obtaining reimbursement for any
specific claim. Additional information about coding, billing, and coverage of REMICADE® may be
obtained through AccessOne®, a single source of services designed to simplify access to therapy with
REMICADE®. You may contact AccessOne® at: 1 (888) ACCESS-1 (1-888-222-3771), Monday through Friday,
8 AM to 8 PM, ET, or visit their website at: www.janssenaccessone.com.
1
Factors That Influence Coverage
Most third-party payers (eg, commercial insurers, Medicare, Medicaid) cover REMICADE® (infliximab)
for its approved U.S. Food and Drug Administration indications (see Indications on page 5 of this guide).
However, benefits may vary depending upon a patient’s insurer or specific insurance plan (or “product”)
offered by a payer.
When third-party payers review claims for REMICADE®, first they will determine if the reported service
is covered under their contract or rules. Most payers cover drug infusions as part of their core benefits.
Next, payers will look for evidence supporting the medical necessity of therapy. This evidence
may include:
• Information about the patient’s medical condition and history
• A physician’s statement or letter of medical necessity
• Supporting literature (eg, peer-reviewed studies and compendia monographs)
• Prescribing information
• Availability of other treatment alternatives
Administrative issues may also affect coverage of therapy with REMICADE®. For example, payers may
consider the following:
Does the payer’s contract specifically preclude physician offices from billing for infusion services
or infused drugs?
A small portion of payers have exclusive contracts with designated preferred providers for infusion
services. This may include certain clinics or specialty pharmacies that deliver drugs to healthcare
providers or other infusion centers.
Does the payer cover the therapy only when provided through a specific treatment site?
Payers may have site-specific coverage rules that restrict provision of infused therapies. For example,
currently Medicare does not cover infusions when they are billed by Medicare-certified ambulatory
surgery centers. Medicare and other payers also may restrict coverage for certain infused drugs in the
home or hospital outpatient setting.
Is the billing provider a “participating” member of, or “in-network” provider for, that
particular plan?
Payers contract with providers to deliver services to the plan’s members. Providers are thus
“participating” or within that plan’s network, requiring them to abide by the contract charge structure
when providing care for that plan’s members.
Did the patient obtain the appropriate referral or prior authorization if required by their plan?
Many plans require that non-emergency services be pre-approved or that a primary care physician make
the referral for specialty care. Failing to obtain appropriate referrals or preauthorization can result in
non-payment by the plan.
2
REMICADE® (infliximab) Quick Reference Guide
This section provides general information about the payers and payment mechanisms for the different
sites of care in which REMICADE® is administered (Table 1) and lists the codes commonly associated
with billing for REMICADE® and the related drug administration services (Table 2).
Table 1: REMICADE® Reimbursement Summary by Payer Type and Site of Care
Payer
Hospital Outpatient Department
Physician Office
• Physician Fee Schedule (PFS)
Medicare
Part B*
• Outpatient Prospective Payment
System (OPPS)
• ASP+6%
• Covered incident to physician
services
• Local Coverage Determinations
(LCD) may apply
Medicaid
• Variable reimbursement
methodology
• Coverage policies may apply
• May require preauthorization
• Variable reimbursement
methodology
• Coverage policies may apply
• May require preauthorization
Commercial
Insurance
• Variable reimbursement
methodology
• May require use of specialty
pharmacy
• May require preauthorization
• Variable reimbursement
methodology
• May require use of specialty
pharmacy
• May require preauthorization
• ASP+6%
• Covered incident to physician
services
• Local Coverage Determinations
(LCD) may apply
*Note: While REMICADE® is covered under Medicare Part B some Part D formularies also list REMICADE®. If the physician and
patient conclude that obtaining REMICADE® through Part D (at a Part D retail pharmacy provider or a Part D participating specialty
pharmacy) is clinically better for the patient, that option is available. Under these circumstances providers may not bill Part B for the
drug, only the services for drug administration.
Medicare payment rates may be subject to change based on mandated budget cuts or Congressional legislation.
Please see Important Safety Information, full Prescribing Information, and Medication Guide
for REMICADE®.
3
Coding for REMICADE® (infliximab)
and Drug Administration Services
Indications and Usage
Crohn’s Disease – REMICADE® is indicated for reducing signs and symptoms and inducing and
maintaining clinical remission in adult and pediatric patients 6 years of age and older with moderately to
severely active Crohn’s disease who have had an inadequate response to conventional therapy.
REMICADE® is indicated for reducing the number of draining enterocutaneous and rectovaginal fistulas
and maintaining fistula closure in adult patients with fistulizing Crohn’s disease.
Pediatric Crohn’s Disease – REMICADE® is indicated for reducing signs and symptoms and inducing and
maintaining clinical remission in pediatric patients 6 years of age or older with moderately to severely
active disease who have had an inadequate response to conventional therapy.
Ulcerative Colitis – REMICADE® is indicated for reducing signs and symptoms, inducing and
maintaining clinical remission and mucosal healing, and eliminating corticosteroid use in adult patients
with moderately to severely active disease who have had an inadequate response to conventional
therapy.
Pediatric Ulcerative Colitis – REMICADE® is indicated for reducing signs and symptoms and inducing
and maintaining clinical remission in pediatric patients 6 years of age or older with moderately to
severely active disease who have had an inadequate response to conventional therapy.
Rheumatoid Arthritis in combination with methotrexate – REMICADE® is indicated for reducing
signs and symptoms, inhibiting the progression of structural damage, and improving physical function in
patients with moderately to severely active disease.
Ankylosing Spondylitis – REMICADE® is indicated for reducing signs and symptoms in patients with
active disease.
Psoriatic Arthritis – REMICADE® is indicated for reducing signs and symptoms of active arthritis,
inhibiting the progression of structural damage, and improving physical function.
Plaque Psoriasis – REMICADE® is indicated for treatment of adult patients with chronic severe (ie,
extensive and /or disabling) plaque psoriasis who are candidates for systemic therapy and when other
systemic therapies are medically less appropriate. REMICADE® should only be administered to patients
who will be closely monitored and have regular follow-up visits with a physician.
SELECTED IMPORTANT SAFETY INFORMATION
Serious and sometimes fatal side effects have been reported with REMICADE® (infliximab).
Infections due to bacterial, mycobacterial, invasive fungal, viral, or other opportunistic pathogens
(eg, TB, histoplasmosis) have been reported. Lymphoma, including cases of fatal hepatosplenic
T-cell lymphoma (HSTCL), and other malignancies have been reported, including in children and
young adult patients. Due to the risk of HSTCL, mostly reported in Crohn’s disease and ulcerative
colitis, assess the risk/benefit, especially if the patient is male and is receiving azathioprine
or 6-mercaptopurine treatment. REMICADE® is contraindicated in patients with severe
hypersensitivity reactions to REMICADE® and certain patients with congestive heart failure. Other
serious side effects reported include melanoma and Merkel cell carcinoma, hepatitis B reactivation,
hepatotoxicity, hematological events, hypersensitivity, neurological events, and lupus-like
syndrome. Please see related and other Important Safety Information.
4
REMICADE® (infliximab) Coding Summary
It is important to accurately and fully complete claim forms for the therapy, whether the claim is
submitted by physician offices using the CMS-1500 claim form or by hospital outpatient departments
using the UB-04 claim form. This section identifies procedure and supply codes that are likely to be most
relevant to healthcare provider claims for therapy with REMICADE®. Please note that healthcare providers
are responsible for selecting appropriate codes for any particular claim based on the patient’s condition
and the items and services that are furnished. Contact your local payer with regard to local payment and
policies. Table 2 summarizes the relevant codes for REMICADE® claims. See Appendix A for sample CMS1500 and UB-04 REMICADE® claims, along with tips for successful claims submission.
Table 2: REMICADE® Coding Summary
Type of Claim
Information
Type of
Code
Code
K50.00
K50.10
K50.80
K50.90
K60.3
K63.2
Diagnosis*
ICD-10-CM
Diagnosis1
K51.80
K51.20
K51.30
K51.50
K51.00
K51.90
M06.00
M05.60
M45.9
L40.50
CPT
Procedures,
Services and
Supplies
HCPCS
AHA
Revenue
Codes
L40.8
96413†
96415†
96365†
96366†
99211 to 99215‡,§,II
J7050
0250
0258
0260
0636¶
0510
Description
Crohn’s Disease
Crohn’s disease of small intestine w/o complications
Crohn’s disease of large intestine w/o complications
Crohn’s disease of both small and large intestine w/o
complications
Crohn’s disease, unspecified, w/o complications
Fistula (use in addition to codes for Crohn’s Disease)
Anal fistula
Fistula of intestine
Ulcerative Colitis
Other ulcerative colitis w/o complications
Ulcerative (chronic) proctitis w/o complications
Ulcerative (chronic) rectosigmoiditis w/o complications
Left-sided colitis w/o complications
Ulcerative (chronic) pancolitis w/o complications
Ulcerative colitis, unspecified, w/o complications
Rheumatoid Arthritis (RA)
Rheumatoid arthritis w/o rheumatoid factor, unspecified
Rheumatoid arthritis of unspecified site with involvement
of organs and systems
Ankylosing Spondylitis
Ankylosing spondylitis of unspecified sites in spine
Psoriatic Arthritis
Arthropathic psoriasis, unspecified
Plaque Psoriasis
Other psoriasis
IV infusion, up to 1 hour (chemotherapy)
IV infusion for each additional hour
IV infusion, up to 1 hour (therapeutic)
IV infusion for each additional hour
Evaluation and management services
Infusion, normal saline solution, 250 mL
Pharmacy, no detailed coding
IV solutions
IV therapy
Pharmacy, with detailed coding (requires HCPCS)
Clinic visit
Physician
Office
Hospital
Outpatient
Department
Location on
CMS-1500 Form
Location on
UB-04 Form
Item 21
Form Locator 67
Item 24D
Form Locator 44
N/A
Form Locator 44
N/A
Form
Locator 42
and 43
5
Table 2: REMICADE® Coding Summary (cont’d)
Type of Claim
Information
REMICADE
Type of
Code
Code
Medicare
HCPCS
J1745#
Description
Infliximab, 10 mg (1/10th vial)
Physician
Office
Hospital
Outpatient
Department
Location on
CMS-1500 Form
Location on
UB-04 Form
Item 24D
Form
Locator 44
Shaded area above or Electronic
Item 24D or Item Comment Field
24A or Item 19
®
NDC (11 digit) 57894-0030-01** REMICADE® (infliximab vial, 100 mg)
*The ICD-10-CM codes listed in this table are general and for example only. Actual clinical diagnosis coding should be done to the highest level of
specificity, including complications, lateralization and other considerations, resulting in many more code options. For more information regarding
ICD-10-CM coding, please refer to additional materials located throughout this guide.
† Payer policies for codes used to describe IV therapy may vary. Consult local payers for policies regarding use of 96413 and 96415 or 96365 and 96366.
‡CPT code 99211 is not billable or payable on physician office Medicare claims when used in conjunction with CPT codes 96413, 96415, 96365, or 96366.
§Code all hospital outpatient clinic visits (99201-99205 and 99211-99215) for Medicare claims with G0463.
llUse of evaluation and management codes require documentation of medically appropriate services performed on the same day as the infusion.
¶Medicare suggests use of revenue code 0636 along with HCPCS J1745 to describe REMICADE® on hospital outpatient claim forms.
#10 units = 1 vial of REMICADE®, 100 mg.
**The NDC is not usually listed as a line item. When required in the shaded area above Item 24A-D, it also usually requires a Unit of Measure identifying
the quantity per NDC; the “units of measure” will likely be 1 unit = one 100-mg vial. Please consult with your local payer for additional guidance.
ICD-10-CM Diagnosis Codes1
As of October 1, 2015, all parties covered by HIPAA, not just providers who bill Medicare or Medicaid,
are required to use the International Classification of Diseases, 10th Revision, Clinical Modification (ICD10-CM) codes to document patient diagnoses. ICD-10-CM replaces ICD-9-CM and far exceeds previous
coding systems in the number of concepts and codes provided, allowing for greater specificity when
describing patient conditions. ICD-10-CM uses 3-7 alpha and numeric digits to achieve this level of detail:
ALPHA
(NOT U)
NUMERIC
1st
2nd
DIGIT
DIGIT
CATEGORY
CHARACTERS 3-7 CAN BE ANY COMBINATION OF ALPHA OR NUMERIC
3rd
DIGIT
4th
DIGIT
5th
DIGIT
6th
DIGIT
ETIOLOGY, ANATOMICAL SITE, SEVERITY
7th
DIGIT
EXTENSION
Source: CMS. Road to 10: The Small Physician Practice’s Route to ICD-10, at: http://www.roadto10.org/icd-10-basics; last accessed December 30, 2015.
Codes with three characters are included in ICD-10-CM as the heading of a category of codes that
may be further subdivided by the use of any or all of the 4th, 5th, and 6th characters. Digits 4-6
provide greater detail of etiology, anatomical site, and severity. For example:
K50
K50.0
K50.01
K50.012
Crohn’s disease
Crohn’s disease of small intestine
Crohn’s disease of small intestine with complications
Crohn’s disease of small intestine with intestinal obstruction
The 7th character may be used to provide data about the characteristic of the encounter (eg, initial,
subsequent). It is not necessary to use all seven digits, however coding to the highest level of
specificity is a must.
6
ICD-10-CM Diagnosis Codes1 (continued)
There are many sources for mapping ICD-9-CM codes to ICD-10-CM, including
https://www.janssenaccessone.com/pages/reference/icd10-crosswalks.jsp. Although the guidelines
are helpful, the ultimate responsibility for correct coding lies with the provider of services and must be
supported with detailed documentation in the medical record.
For more information about ICD-10-CM helpful resources, please see Appendix F.
CPT® and HCPCS Codes for Drugs
and Drug Administration
This section discusses appropriate codes for REMICADE® (infliximab) and associated drug administration
services provided in physician offices and hospital outpatient departments.
Physician Office Setting
Drug
Medicare Administrative Contractors (MACs), many private payers, and most Medicaid agencies
require healthcare providers to use Healthcare Common Procedure Coding System (HCPCS) codes to
identify infused drugs on claim forms. HCPCS codes have a 5-character alphanumeric format and are
used to bill for supplies and services not described by the Current Procedural Terminology (CPT), 4th
Edition, coding system. The following HCPCS code may be used to describe REMICADE® on claim forms
submitted from the physician office setting:
• J1745 Infliximab 10 mg
Although the National Drug Code (NDC) is usually reserved for billing by pharmacies, some private
payers and the majority of Medicaid fee-for-service programs require an NDC for billing instead of, or in
addition to, an HCPCS code, for physicians and other service providers as well. Although the FDA uses
a 10-digit format when registering NDCs, payers usually recognize and often require an 11-digit NDC
format on claim forms for billing purposes. It is important to confirm with your payer which NDC format
they require. Guidelines for reporting the NDC in the appropriate format, quantity, and unit of measure
vary by state and by payer, and should be reviewed prior to submitting a claim. The 10-digit NDC and
11-digit alternative NDC formats used for REMICADE® 100 mg are:
• 10-Digit NDC format: 57894-030-01
• 11-Digit NDC format (used by most payers): 57894-0030-01
Place of Service Codes2
The Place of Service (POS) code set provides setting information necessary to appropriately pay
professional service claims. The place of service is the location of the provider’s face-to-face encounter
with the beneficiary. POS codes are required on all claims for professional services (billed on CMS-1500).
Under the Physician Fee Schedule (PFS), some procedures have separate rates for professional services
when provided in facility and non-facility settings, therefore it is important to accurately designate the
POS in order to assure appropriate payment. The physician practice location is considered “non-facility”
(NF), allowing for the practice expenses to be included in the payment under the Physician Fee Schedule
(PFS). When professional services are performed in a facility (eg, hospital outpatient department) the
practice does not incur the same expense (overhead, staff, equipment and supplies, etc.), thus payment
under the PFS is generally lower for facility-based services than for NF.
7
The physician practice setting is indicated with POS code 11. In order to differentiate between on-campus
and off-campus provider-based departments CMS recently created a new POS code (POS 19) and revised
the POS code description for outpatient hospital (POS 22). Professional services delivered in outpatient
hospital settings must now specifically include the off-campus or on-campus POS on the claim form:
POS Code POS Location
Office
Location, other than a hospital, skilled nursing facility, military treatment
facility, community health center, state or local public health clinic,
or intermediate care facility, where the health professional routinely
provides health examinations, diagnosis, and treatment of illness or injury
on an ambulatory basis.
Off Campus Outpatient
Hospital
A portion of an off-campus hospital provider based department which
provides diagnostic, therapeutic (both surgical and nonsurgical), and
rehabilitation services to sick or injured persons who do not require
hospitalization or institutionalization. (Effective January 1, 2016)
On Campus Outpatient
Hospital
A portion of a hospital’s main campus which provides diagnostic,
therapeutic (both surgical and nonsurgical), and rehabilitation services
to sick or injured persons who do not require hospitalization or
institutionalization. (Effective January 1, 2016)
11
19
22
POS Descriptor
Use of the new/revised codes is required as of January 1, 2016. When billing professional services on
the CMS-1500, enter the appropriate POS code in Item 24B, adjacent to each HCPCS code. Claims for
covered services rendered in either on-campus or off-campus outpatient hospital settings will be paid at
the facility rate. Payment policies that currently apply to POS 22 will continue to apply and will also apply
to POS 19.
Drug Administration Services3
Physician services are reported on claim forms using the Current Procedural Terminology (CPT),
4th Edition, coding system. The CPT codes most commonly associated with the administration of
REMICADE® (infliximab) are:
• 96413 Chemotherapy administration, intravenous infusion technique; up to 1 hour, single or initial
substance/drug
• 96415 Each additional hour (Use 96415 in conjunction with 96413; report 96415 for infusion intervals
of greater than 30 minutes beyond 1 hour increments.)
According to the American Medical Association (AMA) and the Centers for Medicare and Medicaid
Services (CMS), these codes also cover certain complex biologic infusions such as monoclonal
antibodies, including infliximab. Non-Medicare payer policies regarding the use of 96413 and 96415 may
vary. Alternatively, some may require the use of CPT codes:
• 96365 Intravenous infusion for therapy, prophylaxis, or diagnosis (specify substance or drug); initial,
up to 1 hour
• 96366 Each additional hour (List separately in addition to code for primary procedure; report 96366
for infusion intervals of greater than 30 minutes beyond 1 hour increments.)
Please contact your local payers for specific coding policies and more information on correct billing and
claims submission, or call AccessOne® for assistance: 1 (888) ACCESS-1 (1-888-222-3771).
8
Hospital Outpatient Setting
Drug
Medicare Administrative Contractors (MACs), many private payers, and most Medicaid agencies require
healthcare providers to use Healthcare Common Procedure Coding System (HCPCS) codes to identify
infused drugs on claim forms. HCPCS codes have a 5-character alphanumeric format and are used to
bill for supplies and services not described by the Current Procedural Terminology (CPT), 4th Edition,
coding system. The following HCPCS code may be used to describe REMICADE® (infliximab) on claim
forms submitted from the hospital outpatient setting:
• J1745 Infliximab 10 mg
Although the National Drug Code (NDC) is usually reserved for billing by pharmacies, some private
payers and the majority of Medicaid fee-for-service programs require an NDC for billing instead of, or in
addition to, an HCPCS code, for physicians and other service providers as well. Although the FDA uses
a 10-digit format when registering NDCs, payers usually recognize and often require an 11-digit NDC
format on claim forms for billing purposes. It is important to confirm with your payer which NDC format
they require. Guidelines for reporting the NDC in the appropriate format, quantity, and unit of measure
vary by state and by payer, and should be reviewed prior to submitting a claim. The 10-digit NDC and
11-digit alternative NDC formats used for REMICADE® 100 mg are:
• 10-Digit NDC format: 57894-030-01
• 11-Digit NDC format (used by most payers): 57894-0030-01
Payers’ policies regarding separate payment for saline used to administer IV drugs vary. Hospitals may
need to record costs on claims even though saline is not separately reimbursed (ie, it is bundled into
the APC payment for infusion services). If billed on the claim form, the following HCPCS code describes
saline used to administer REMICADE®:
• J7050 Infusion, normal saline solution, 250 mL
Drug Administration Services3
Hospital outpatient department services are reported on claim forms using the Current Procedural
Terminology (CPT), 4th Edition, coding system. The CPT codes most commonly associated with the
administration of REMICADE® are:
• 96413 Chemotherapy administration, intravenous infusion technique; up to 1 hour, single or initial
substance/drug
• 96415 Each additional hour (Use 96415 in conjunction with 96413; report 96415 for infusion intervals
of greater than 30 minutes beyond 1 hour increments.)
According to the American Medical Association (AMA) and the Centers for Medicare and Medicaid
Services (CMS), these codes also cover certain complex biologic infusions such as monoclonal
antibodies, including infliximab. Non-Medicare payer policies regarding the use of 96413 and 96415 may
vary. Alternatively, some may require the use of CPT codes:
• 96365 Intravenous infusion for therapy, prophylaxis, or diagnosis (specify substance or drug); initial,
up to 1 hour
• 96366 Each additional hour (List separately in addition to code for primary procedure; report 96366
for infusion intervals of greater than 30 minutes beyond 1 hour increments.)
Please contact your local payers for specific coding policies and more information on correct billing and
claims submission, or call AccessOne® for assistance: 1 (888) ACCESS-1 (1-888-222-3771).
9
Revenue Codes
Many payers require use of American Hospital Association (AHA) revenue codes to bill for services
provided in hospital outpatient departments. Revenue codes consist of a leading zero followed by three
other digits and are used on claim forms to assign costs to broad categories of hospital revenue centers.
The revenue codes that are commonly used with REMICADE® are:
• 0250 Pharmacy, drugs not requiring detailed coding (used for claims to many non-Medicare
payers)
• 0636 Pharmacy, drugs requiring detailed coding with HCPCS code (suggested for Medicare and
sometimes required for other payers)
When AHA revenue code 0636 is used to identify REMICADE®, hospital outpatient departments should
also record HCPCS code J1745.
Home Infusion Providers
The Healthcare Common Procedure Coding System (HCPCS) contains the only Health Insurance
Portability and Accountability Act (HIPAA)-approved, comprehensive code set available to submit
home infusion and ambulatory infusion suite claims that support the typical per diem contracts present
in the marketplace. The S codes are used to report drugs, services, and supplies for which there are no
national codes but for which codes are needed by the private sector to implement policies, programs,
or claims processing. Some combination of the codes may be appropriate for describing therapy with
REMICADE® when it is provided by ambulatory infusion service providers. The following chart illustrates
the codes that may be relevant. Although these codes are used by some private payers, please note
that they are not payable by Medicare or other Federal payers.
Table 3: Home Infusion Codes4
Code
Type
Code Description
PER DIEM SPECIALTY THERAPY SERVICES: HCPCS CODES
S9359*
HCPCS
Home infusion therapy, anti–tumor necrosis factor intravenous therapy
(eg, infliximab); administrative services, professional pharmacy services, care
coordination, and all necessary supplies and equipment (drugs and nursing
visits coded separately), per diem
HOME NURSING: CPT CODES
99601*
CPT
Home infusion/specialty drug administration, per visit (up to 2 hours)
99602*
CPT
Each additional hour (list separately in addition to code for primary procedure)
(use 99602 in conjunction with 99601)
CODES FOR REMICADE®
J1745*
HCPCS
578940030-01
NDC
Injection, infliximab, 10 mg
REMICADE® (infliximab vial, 100 mg)
* If the infusion is performed in an ambulatory infusion suite rather than a patient’s home, modifier SS may be appended to the codes.
10
Table 3: Home Infusion Codes4 (cont’d)
Code
Type
Code Description
OTHER SUPPLIES
J7050*
HCPCS
xxxxxxxxx-xx†
NDC
A4216*
HCPCS
xxxxxxxxx-xx†
NDC
Infusion, normal saline solution, 250 cc
Sodium chloride 0.9% 250 mL bag
Sterile water, sterile saline and/or dextrose, diluent/flush, 10 mL
Sterile water, preservative-free injection, 20 mL vial
* If the infusion is performed in an ambulatory infusion suite rather than a patient’s home, modifier SS may be appended to the codes.
† The NDC will vary by product manufacturer.
Other Coding Considerations
When coding and billing for REMICADE® (infliximab) and drug administration services, providers may
also need to accurately calculate billing units, describe concomitant services or supplies, or account for
modification to a service. This section reviews some of those additional considerations.
REMICADE® Billing Units
The HCPCS code for REMICADE® is J1745, described as: “Injection infliximab, 10 mg.” Thus, each 10-mg
dose equals one billing unit, or 1/10th of a vial. It is important to understand that when billing for
REMICADE®, each 100-mg vial of drug represents 10 units of J1745. The following chart illustrates the
correlation between vials, milligrams, and billing units.
Number of 100-mg vials
of infliximab
Number
of mg
Number of billing units based on J1745
(10 mg infliximab per unit)
1
100
10
2
200
20
3
300
30
4
400
40
5
500
50
Billing With National Drug Codes (NDCs)5
Reporting NDCs is required for Medicaid and Medicare/Medicaid crossover claims to support the
Medicaid drug rebate process. NDCs may also be reported to facilitate claims processing and may be
required by payers. Accurate NDC reporting must include specific elements:
• NDC (11-digit format)
• NDC unit of measure qualifier (eg, UN, ML, GR, etc.)
• NDC qualifier - N4
• NDC units
11
NDC billing information must conform to the HIPAA 5010 standard, thus follow a specific format:
11-DIGIT NDC
NDC UNITS
N4xxxxxxxxxxxUNx
NDC QUALIFIER
QUANTITY QUALIFIER
The corresponding entry for one vial of REMICADE® is: N457894003001UN1. The number of NDC units
to be billed is based on the dose:
Example:
NDC Unit Calculation
X
000-00-1234
Doe, John B.
3914 Spruce Street
Anytown
01010
X
HCPCS code
Doe, John B.
X
07 01 45
Amount of drug to be billed
300 MG
J1745
AS
3914 Spruce Street
Anytown
AS
HCPCS code description
Infliximab injection, 10 mg
Number of HCPCS units
30
203 555-1234
01010
NDC (11-digit billing format)
203 555-1234
57894-0030-01
NDC description
REMICADE® (infliximab vial, 100 mg)
NDC unit of measure
UN
Medicare
To calculate the NDC units:
• the amount to be billed is 300 mg
• the NDC unit of measure is UN (powder for reconstitution)
• mg must be converted to UN
• the
NDC description is 100 mg/vial 123 456 7890
Dr. Jones
• divide the amount to be billed (300-mg) by the number in the NDC description (300/100 = 3)
Below555.1
is an example of the CMS 1500 form entry for a 300-mg dose of REMICADE® (30 units of J1745 or
UN3
of
theHospital
NDC):
Pay-to-name
Anytown
XX-XXXX
1
3a PAT.
CNTL #
b. MED.
REC. #
2
Pay-to-address
Pay-to-city/state
160 Main Street
Anytown, Anystate 01010
N457894003001UN3
a
John B. Doe (ID)
b 01 31
John B.16
Doe01 31 16
8 PATIENT NAME
10 BIRTHDATE
07-01-45
11 SEX
31
OCCURRENCE
CODE
DATE
M
12
DATE
9 PATIENT ADDRESS
J1745b Anytown,
ADMISSION
13 HR 14 TYPE 15 SRC 16 DHR 17 STAT
32
OCCURRENCE
CODE
DATE
33
OCCURRENCE
DATE
CODE
18
19
34
OCCURRENCE
CODE
DATE
4
DOE 1234-97
6
5 FED. TAX NO.
010001010
3914 Spruce St.
A
xxxx
a
20
CONDITION CODES
24
22
23
21
35
CODE
25
STATEMENT COVERS PERIOD
FROM
THROUGH
30 c AS
26
27
36
CODE
OCCURRENCE SPAN
FROM
THROUGH
28
d
TYPE
OF BILL
7
01010
e
29 ACDT 30
STATE
OCCURRENCE SPAN
FROM
THROUGH
US
37
a
a
b
b
38
a
39
CODE
40
CODE
VALUE CODES
AMOUNT
VALUE CODES
AMOUNT
41
CODE
VALUE CODES
AMOUNT
b
The corresponding CMS-1450 form entry for a 300-mgc dose of REMICADE® is:
d
42 REV. CD.
1
2
43 DESCRIPTION
44 HCPCS / RATE / HIPPS CODE
45 SERV. DATE
N457894003001UN3
4
5
6
12
8
9
47 TOTAL CHARGES
3
3
7
46 SERV. UNITS
PLEASE PRINT OR TYPE
48 NON-COVERED CHARGES
49
1
Dr. Jones
4231 Center Road
Anytown, AS 01010
123 456 7890
203 987-6543
APPROVED OMB-0938-1197 FORM 1500 (02-12)
2
3
4
5
6
7
8
9
Partial Additional Hours of Infusion Time6
CMS has a policy for reporting the add-on infusion codes when less than a full hour of service is
provided. CPT code 96415 (for “each additional hour”) is to be used for “infusion intervals of greater than
thirty minutes beyond one hour increments.” If the incremental amount of infusion time is 30 minutes or
less the time is not to be billed separately. Document infusion start and stop times in the medical record.
Some payers may require reporting the actual number of minutes on claims.
Modifiers
Modifiers provide a means to report or indicate that a service or procedure has been altered by some
specific circumstance but not changed in its definition or code. They add more information and help to
eliminate the appearance of duplicate billing and unbundling. Appropriately used, modifiers increase
coding and reimbursement accuracy. The following table summarizes modifiers that may be applicable
to the provision of REMICADE® (infliximab) in physician offices and hospital outpatient departments.
Table 4: Summary of Code Modifiers7
Modifier
25
52
59
Description
Indication and Placement
Significant, separately
• patient requires distinct E/M service in
identifiable evaluation
and management service addition to the infusion procedure
by the same physician or • must be substantiated with relevant
other qualified healthcare documentation
professional on the same • append the modifier to the relevant
day of the procedure or
E/M code
other service
Reduced Services
• last additional hour of service is not a full
60 minutes; may require listing actual
service minutes
• local MAC/other payer requirements
may vary
• append the modifier to the infusion code
Distinct Procedural
Service
• indicates a procedure or service separate
and distinct from another service with which
it would usually be considered bundled
• do not use with E/M codes and use only if
a more descriptive modifier is not available
• may append to an initial drug administration
service code when the patient must
return for a separately identifiable drug
administration service on the same day or
has two IV lines per protocol
UB-04
CMSLocator
1500
Item 24D Box 44
✓
✓
If
If
required required
by payer by payer
✓
✓
13
Table 4: Summary of Code Modifiers7 (cont’d)
Modifier
PO
JW
KX
14
Description
Indication and Placement
• required beginning January 1, 2016
• to be reported with every HCPCS code
Services, procedures,
for all items and services furnished in offand/or surgeries
campus provider-based departments of a
furnished at offhospital
campus provider-based
outpatient departments • should not be reported for remote
locations or satellite facilities of a hospital, or
emergency departments
UB-04
CMSLocator
1500
Item 24D Box 44
N/A
✓
Drug amount
discarded/not
administered to
any patient
• unused drug remains after applicable dose
is administered from single-use vial
• CMS has issued a discarded drug policy;
If
If
local MAC/other payer requirements
required required
may vary
by payer by payer
• append the modifier to the drug code on
a line separate from that reporting the
administered dose
Requirements
specified in the
medical policy have
been met
• represents awareness of/compliance with
payer policies for the use of specific codes
• payer requirements may vary regarding
If
If
use with the chemotherapy/complex
required required
biologic infusion codes
by payer by payer
• append the modifier to codes as required
by the payer
Distinct Procedural Service8
The -59 modifier is the most widely used modifier. Because it is defined for use in a wide variety
of circumstances it has often been implicated for incorrect use and abuse. To better separate the
circumstances in which this modifier is likely to apply from those for which it would be inappropriate,
CMS has defined four new HCPCS modifiers. The new modifiers selectively identify subsets of Distinct
Procedural Services (-59 modifier) and are collectively referred to as the -X {EPSU} modifiers:
Modifier
Title
Description
XE
Separate Encounter
A service that is distinct because it has occurred during a
separate encounter
XS
Separate Structure
A service that is distinct because it was performed on a
separate organ/structure
XP
Separate Practitioner
A service that is distinct because it was performed by a
different practitioner
XU
Unusual Nonoverlapping Service
The use of a service that is distinct because it does not overlap
components of the main service
Although CMS continues to recognize the -59 modifier, it may selectively require a -X {EPSU} modifier,
especially when billing codes are at high risk for incorrect billing. Overall CMS encourages providers to
rapidly migrate to these new, more specific modifiers.
CMS Discarded Drug Policies9
When it is necessary to discard the remainder of a single-use vial or other single-use package after
administering a dose/quantity of the drug or biological to a Medicare patient, the program provides
payment for the amount of drug or biological discarded as well as the dose administered, up to the
amount of the drug or biological as indicated on the vial or package label.
When processing claims for drugs and biologicals local contractors may require the use of the modifier
JW to identify unused drugs or biologicals from single-use vials or packages. This modifier, billed on a
separate line, will provide payment for the amount of discarded drug or biological. For example, a
single-use vial that is labeled to contain 100 units of a drug has 95 units administered to the patient and
5 units discarded. The 95-unit dose is billed on one line, while the discarded 5 units may be billed on
another line by using the JW modifier. Both line items would be processed for payment. The JW modifier
is only applied to the amount of drug or biological that is discarded.
Summary:
• Payment for discarded amounts of drug or biological applies only to single-use vials or packages.
• Multi-use vials are not subject to payment for discarded amounts of drug or biological.
• Medicare contractors may choose to require the JW modifier on claims for discarded drug or
biological. Check with your local contractor for their specific requirements.
• Both the administered and discarded drug amounts should be clearly documented in the medical
record.
15
Same Day Evaluation and Management Services10
It may be necessary to provide evaluation and management (E/M) services on the same day as a drug
administration procedure. Depending on the payer, E/M services that are medically necessary, separate
and distinct from the infusion procedure (CPT codes 99201-99205 and 99211-99215 in the physician office
and HCPCS code G0463 in the hospital outpatient setting), and documented appropriately are generally
covered. Please note that CMS has a specific policy regarding use of CPT code 99211 (level 1 medical visit
for an established patient) in the physician office. The policy states:
For services furnished on or after January 1, 2004, do not allow payment for CPT code 99211,
with or without modifier 25, if it is billed with a nonchemotherapy drug infusion code or a
chemotherapy administration code.
This means that a level 1 medical visit for an established patient (99211) cannot be billed on the same day
as an office-based infusion of REMICADE® (infliximab).
16
Payment for REMICADE® (infliximab)
and Drug Administration Services
There is a demonstrated history of paid claims for REMICADE® for all payers, including Medicare,
Medicaid, and commercial plans. Coverage varies by payer, contracts, treatment setting, and
individual patient case. There are comprehensive published Medicare coverage policies specific to
REMICADE®. Copies of coverage policies are available on your regional Medicare Administrative
Contractor (MAC) website, and are also available from the AccessOne® website under Billing and
Reimbursement: http://www.janssenaccessone.com/pages/remicade. The following section discusses
Medicare, Medicaid, and private insurer payment policies that will usually apply to REMICADE®.
Medicare Payment to Physician Offices
In 2016, Medicare Part B reimburses for REMICADE® administered in Medicare-participating physician
offices based on Average Sales Price plus six percent (ASP+6%). After the patient’s deductible is met,
Medicare pays 80% of these established rates, and the patient or secondary insurance is responsible for
the remaining 20%.
CMS updates the ASP+6% reimbursement amount on a quarterly basis. Current drug pricing files are
accessible from the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-BDrugs/McrPartBDrugAvgSalesPrice/index.html.
Medicare reimburses physicians for drug administration services and procedures associated with
REMICADE® according to the Physician Fee Schedule (PFS). The Medicare fee schedule for professional
services is based on the resource-based relative value scale (RBRVS) methodology, a system in which
considerations are made for physician work, practice expense, and malpractice expense relative to
each code, then adjusted for differences in costs by geographic location. For geographic-specific
rates for any PFS code, please refer to the Physician Fee Schedule Search, available at:
http://www.cms.gov/apps/physician-fee-schedule/overview.aspx.
Medicare Payment to Hospital Outpatient Departments
In 2016, Medicare Part B reimburses for REMICADE® administered in Medicare-participating hospital
outpatient departments based on Average Sales Price plus six percent (ASP+6%). After the patient’s
deductible is met, Medicare pays 80% of these established rates, and the patient or secondary insurance
is responsible for the remaining 20%.
CMS updates the ASP+6% reimbursement amount on a quarterly basis. Current drug pricing files are
accessible from the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-BDrugs/McrPartBDrugAvgSalesPrice/index.html.
Medicare reimburses hospital outpatient departments for drug administration services and procedures
associated with REMICADE® (infliximab) according to the Outpatient Prospective Payment System
(OPPS). Payment is based on ambulatory payment classifications (APC), a system in which services of
similar resource consumption are grouped and paid at the same rate. Adjustments are made for
geographic location. Updates are posted quarterly to the OPPS website at:
http://www.cms.gov/Regulations-and-Guidance/Regulations-and-Policies/QuarterlyProviderUpdates/index.html.
17
Medicare Policy for Other Healthcare Providers
Medicare coverage policies limit provision of drugs to certain treatment settings. Under current rules,
Medicare will not reimburse home health companies, ambulatory surgical centers, or durable medical
equipment companies for REMICADE® (infliximab). If patients have secondary or supplemental insurance
(eg, through a spouse’s employer-sponsored plan or post-retirement health benefits), there may be
coverage and reimbursement that goes beyond what is provided by Medicare. Also, Medicare does not
provide additional payment to rural health clinics for infused drugs like REMICADE®.
Medicaid Payment Policies
Medicaid programs generally provide reimbursement for REMICADE® in one or more ambulatory
treatment settings, but the Medicaid payment policies may vary because each state administers its own
program. Not all Medicaid fee-for-service programs use the same payment formula to reimburse for
REMICADE® provided in physician offices. Providers can check with the state agency for the current
reimbursement method.
States will typically use a fee schedule to reimburse for office-based infusion services. Most Medicaid
programs require prior authorization for office infusions, and some may have specific coverage policies
for infused therapies. Some state Medicaid programs may allow REMICADE® to be billed through
pharmacies. In a few states, Medicaid programs may require REMICADE® to be dispensed to the
physician’s office then billed through the pharmacy benefit. In these cases, the drug is delivered to
the treatment setting and the office or clinic may only bill for the infusion service. In some cases, state
Medicaid programs also may permit REMICADE® to be provided in the home setting by a qualified home
infusion company.
Medicaid reimbursement for drugs provided in hospital outpatient departments is most commonly
determined by an ASP-based formula and may be influenced by whether the facility is located in an urban
or rural area or whether it is a specialty (eg, children’s or rehabilitation hospital) or teaching facility.
If you need assistance understanding Medicaid policies in your area, AccessOne® is available to help you
at 1 (888) ACCESS-1 (1-888-222-3771). In addition, you may contact your local payer.
Commercial Payers
Private payers will generally provide reimbursement for REMICADE® although some may restrict the site
of care in which infusion services will be covered. For example, recently some payers have restricted
coverage in the hospital outpatient setting (POS 19 and 22) to those cases for which medical necessity
for a hospital setting can be established. Some payers may require drug acquisition through a specialty
pharmacy, in which case the provider may only bill for the administration service (please refer to
“Coding for Drugs Purchased From Other Than the Administering Provider”, Appendix D). Payment
for REMICADE® provided in the office setting is commonly based on an ASP-based formula. However,
there will be some cases in which the cost of the drug is included in some type of capitated rate.
Although such rates are often assumed to cover the cost of the therapy, physician offices and clinics
can sometimes obtain separate payment by calling the plan and explaining the medical necessity and
specific circumstances. To the degree that providers are offered capitated or risk contracts, they should
consider attempting to negotiate a separately payable status for drugs like REMICADE®.
18
Private insurance payments for hospital outpatient department services will typically be based on
charges, fee schedules, or outpatient per-diem rates. However, this will vary by plan, the contracts
between plans and hospitals, and by the specific insurance “products” offered by any given payer
(eg, HMO, PPO, etc.). If you need assistance understanding plan payment policies, contact AccessOne®
or your local payer.
Home Infusion Reimbursement
Ambulatory infusion providers are licensed pharmacies that provide a wide range of services ranging
from home infusion and nutritional therapies, to care management services and biologics, including
REMICADE®. Reimbursement for REMICADE® provided through a home infusion pharmacy depends
strictly on individual private payer and state Medicaid policies. It is especially important to note that
Medicare does not currently pay for REMICADE® when provided by a home infusion provider although
other payers may allow or even require this setting. Drug administration services may be provided in
either the patient’s place of residence or within an Ambulatory Infusion Suite (AIS) operated by the home
infusion provider.
Medicare Part D
REMICADE® is covered under Medicare Part B, however some Part D formularies also list REMICADE®.In
circumstances where the physician and patient conclude that obtaining REMICADE® through Part D (eg,
Part D retail pharmacy provider, or Part D participating specialty pharmacy) is clinically preferred for the
patient, this option is available. Under these circumstances physicians may not bill Part B for the drug,
only the services they supply for drug administration.
19
References
1 A
merican Medical Association. (2015). ICD-10-CM Mappings 2016: Linking ICD-9-CM to All Valid
ICD-10-CM Alternatives. Chicago; American Medical Association. (2015). ICD-10-CM: The Complete
Official Codebook. Chicago.
2 CMS. Transmittal 3315. August 6, 2015; CMS Place of Service Codes for Professional Claims Database
(updated August 6, 2015) at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/
PhysicianFeeSched/Downloads/Website-POS-database.pdf. Last accessed Dec. 31, 2015.
3 American Medical Association. (2015). CPT® 2016: Professional Edition. Chicago.
4 N
ational Home Infusion Association. NHIA national coding standard for home infusion claims
under HIPAA, version 1.11.01d.
5 C
MS. Transmittal 1401. December 21, 2007; CMS. Pub. 100-04 Medicare Claims Processing Manual,
Chap. 26, Section 10.4. CMS Pub 100-04 Medicare Claims Processing Manual, Chapter 25,
Section 75.5.
6 CMS. Pub. 100-04 Medicare Claims Processing Manual, Chap. 12, Section 30.5(E).
7 American Medical Association. (2015). CPT® 2016: Professional Edition. Chicago. American Medical Association. (2015). HCPCS 2016 Level II Professional Edition. Chicago.
8 CMS. Transmittal 1422. August 15, 2014.
9 CMS Pub. 100-04 Medicare Claims Processing Manual, Chapter 17, Section 40.
10 CMS Pub. 100-04 Medicare Claims Processing Manual, Chapter 12, Section 30.5(F).
20
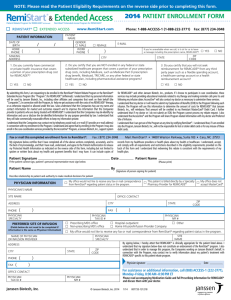
Appendix A: Sample Claim Forms
The Form CMS-1500 is the basic form prescribed by CMS for the Medicare and Medicaid programs for
claims from suppliers and non-institutional providers that qualify for a waiver from the Administrative
Simplification Compliance Act (ASCA) requirement for electronic submission of claims. It has also been
adopted by the TRICARE Program. For detailed guidance on completing the CMS-1500 items, please
see the Medicare Claims Processing Manual, Pub. 100-04, Chap 26, available at:
http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals.
The 837P (Professional) is the standard format used by healthcare professionals and suppliers to transmit
healthcare claims electronically. The American National Standards Institute (ANSI) Accredited Standards
Committee (ASC) X12N 837P (Professional) Version 5010A1 is the current electronic claim version.
Data elements in the CMS uniform electronic billing specifications are consistent with the hard copy data set
to the extent that one processing system can handle both. For more information on electronic claims, please
see the ASC website at: http://www.x12.org/. To view a crosswalk between the electronic and hard copy claim
form, please see: http://www.nucc.org/images/stories/PDF/1500_form_map_to_837p_5010_v2-0_112011.pdf.
The Form CMS-1450, also known as the UB-04, is a uniform institutional provider bill suitable for use in
billing multiple third party payers. It is the basic form prescribed by CMS for the Medicare and Medicaid
programs for claims from hospitals, including hospital outpatient departments. Because it serves many
payers, a particular payer may not need some data elements. For detailed guidance on completing the
CMS-1450 items, please see the Medicare Claims Processing Manual, Pub. 100-04, Chap 25, available at:
http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals.
Please see Checklist for Clean Claims on page 26.
21
REMICADE® (infliximab)
2016 Physician Office Sample Claim Form: CMS-1500
1
Item 19—Some payers may ask providers to specify REMICADE® (infliximab) dosage and NDC, or
insert “patient on concomitant methotrexate therapy” for RA. Do not abbreviate “methotrexate.”
NOTE: Some payers require alternate product codes (eg, Medicaid claims). Please consult with
your local payers or contact AccessOne® at 1-888-ACCESS-1 (1-888-222-3771) to confirm payer-
specific coding requirements.
2 Item 21—Indicate diagnosis/diagnoses using appropriate ICD-10-CM codes. Use diagnosis codes
to the highest level of specificity for the date of service and enter the diagnoses in priority order.
The “ICD Indicator” identifies the ICD code set being reported. For ICD-10-CM diagnoses enter 0
(zero) as a single digit between the vertical, dotted lines.
3 Item 24D—Indicate appropriate CPT and HCPCS codes and modifiers if required. Be sure to
enter the correct CPT codes by payer–Medicare claims for REMICADE® administration will use
codes 96413 and 96415.
NOTE: Individual payer (eg, private, Medicaid) policies may vary regarding the use of codes
96413 and 96415 or 96365 and 96366. Consult local payers for coding policy. Medicaid coding
for REMICADE® may vary. Please consult with your local payer or contact AccessOne® at
1-888-ACCESS-1 (1-888-222-3771) to confirm payer requirements.
4 Use of evaluation and management codes requires documentation of medically appropriate
services performed on the same day as the infusion. Medicare requires the use of modifier 25
when reporting a significant, separately identifiable E/M service by the same physician, on the
same day of the infusion procedure.
5 Item 24E—Refer to the diagnosis for this service (see box 21). Enter only one diagnosis pointer
per line.
6 Item 24G—10-mg units (10 units of J1745 = a single 100-mg vial of infliximab).
22
000-00-1234
X
Doe, John B.
07 01 45
3914 Spruce Street
Doe, John B.
X
3914 Spruce Street
X
AS
Anytown
01010
Anytown
203 555-1234
AS
01010
203 555-1234
Medicare
123 456 7890
Dr. Jones
1
2
0
K50.10
3
01 02 16
01 02 16
11
01 02 16
01 02 16
11
96415
01 02 16
01 02 16
11
J1745
01 02 16
01 02 16
11
4
5
96413
99212
25
PLEASE PRINT OR TYPE
A
6
1
123 456 7890
A
1
123 456 7890
A
40
123 456 7890
A
1
123 456 7890
Dr. Jones
4231 Center Road
Anytown, AS 01010
123 456 7890
203 987-6543
APPROVED OMB-0938-1197 FORM 1500 (02-12)
23
REMICADE® (infliximab)
2016 HOPD Sample Claim Form: UB-04
1
Locator Box 42—List revenue codes in ascending order.
2 Locator Box 43—Describe procedure (eg, IV therapy, clinic visit).
3 Use of E/M codes requires documentation of medically appropriate services performed on the
same day as the infusion. Medicare requires that HCPCS code G0463 be used to represent all
hospital outpatient clinic visits (formerly coded with CPT codes 99201-99205 and 99211-99215).
4 Locator Box 44—Indicate appropriate CPT and HCPCS codes and modifiers if required.
Be sure to enter the correct CPT codes by payer–Medicare claims for REMICADE® (infliximab)
administration will use codes 96413 and 96415.
NOTE: Individual payer (eg, private, Medicaid) policies for codes to describe IV therapy may vary.
Consult local payers or contact AccessOne® at 1-888-ACCESS-1 (1-888-222-3771) for coding policy
regarding use of 96413 and 96415 or 96365 and 96366.
NOTE: Effective January 1, 2016, the -PO modifier is required for all items and services provided in
an off-campus, provider-based department of a hospital.
5 Locator Box 46—10-mg units (10 units of J1745 = a single 100-mg vial of infliximab).
6 Locator Box 47—Indicate total charges.
7 Locator Box 67—Indicate diagnosis using appropriate ICD-10-CM codes. Use diagnosis codes to
the highest level of specificity for the date of service and enter the diagnoses in priority order.
24
1
2
4
3
6
J7050
01-02-16
01-02-15
96413
01-02-16
96415PO
96415
01-02-16
G0463
01-02-16
5
J1745
7
0
01-02-16
K50.10
25
Checklist for Clean Claims
To proactively prevent denials and underpayments, it may be helpful to perform a pre-billing review
prior to submitting any claim to a payer. The following may be considered:
❏ Has insurance been verified?
❏ Is this a covered service?
❏ Were the specific payer requirements followed?
❏ If applicable, is the referral authorized?
❏ Is medical necessity documented?
❏ Is all of the required information included on the claim?
❏ Are the correct codes (diagnosis, CPT, and HCPCS) reported?
❏ Are the billed units accurate and consistent with the J code descriptor?
❏ If reporting any discarded drug, was it properly documented?
❏ If a separate and distinct E/M service was provided, is it identified with modifier 25?
Appendix B: Medical Necessity
Medical necessity refers to a decision by a health plan that a treatment, test, or procedure is necessary
for health or to treat a diagnosed medical problem. Health insurance companies provide coverage only
for health-related services that they define or determine to be medically necessary. Medicare National
Coverage Determinations (NCDs) and Medicare Administrative Contractors’ (MACs) Local Coverage
Determinations (LCDs) define medical necessity requirements. Within these documents covered
diagnoses, documentation requirements, and limitations of coverage for specific services provide
guidance for establishing medical necessity.
You can check your regional MAC website for coverage policies for REMICADE® (infliximab) or
go to http://www.janssenaccessone.com/pages/remicade to access state-specific billing and
reimbursement guidelines for Medicare Administrative Contractors. This website also contains
information on state-specific Commercial Payer and Medicare Part D prior authorization.
For a sample template for a letter of medical necessity, please contact AccessOne® at: 1 (888) ACCESS-1
(1-888-222-3771), Monday through Friday, 8 AM to 8 PM, ET.
Appendix C: Appeals
The most common reasons for denials or underpayment of claims include:
• Omission of any information that clarifies medical necessity (eg, relevant diagnosis codes)
• Inaccurately reporting the billable units of drug; note that REMICADE® (infliximab) is reported in
10-mg units
• Use of incorrect CPT or HCPCS codes
• Lack of proper and complete documentation
• Omission of a physician letter/statement of medical necessity
• Omission of special coding requirements (eg, the NDC number or required modifiers)
• Failure to follow payer-specific requirements for providing this therapy
26
Different payers provide different appeals rights depending upon the level of appeal for the denied
claim (eg, first appeal, second appeal). In the event of a claim denial, be sure to resubmit your claim.
Most well-documented follow-up submissions are successful.
Additional resources for appealing Medicare claims may be found at:
https://www.cms.gov/Medicare/Appeals-and-Grievances/OrgMedFFSAppeals/index.html?redirect=/
orgmedffsappeals/. You may also want to encourage your patients to contact their employer’s benefits
office. Many companies are willing to intervene on behalf of employees when prescribed therapies are
challenged.
For additional information regarding coding, coverage, and reimbursement policies or claim denials
for REMICADE®, see: http://www.janssenaccessone.com/pages/remicade.
For additional assistance, call AccessOne® at: 1 (888) ACCESS-1 (1-888-222-3771),
Monday through Friday, 8 AM to 8 PM, ET.
Appendix D: Working With Specialty Pharmacy
Some patients may obtain REMICADE® through Medicare Part D or another prescription drug benefit,
and thus acquire the drug through a retail or specialty pharmacy. The drug is then brought or sent to the
administering site of care. Providers that do not buy and supply the drug may not bill for the drug itself,
but only for the services associated with drug administration.
Management Tools
Providers that obtain drugs outside the buy-and-bill model for both commercial and Medicare
patients (ie, via some type of pharmacy delivery option) generally find it helpful to develop systems
to help manage this method of drug acquisition and service delivery. Please contact AccessOne® at
1 (888) ACCESS-1 (1-888-222-3771) for tools that may assist you with tracking and coordinating drugs
acquired through specialty pharmacy channels.
Coding for Drugs Purchased From Other Than the Administering Provider
If the drug is brought to the provider by the patient or delivered to the provider by a specialty pharmacy,
the provider may only bill for the administration service. In order to identify and reimburse for the
appropriate administration service, most payers require that the name and dosage of the drug be
documented on the claim. Commonly payers require that the drug be reported in 24D and “billed” with
a charge of $0.00.* Billing systems that do not permit a $0.00 charge entry may require entering $0.01.
Please check with your software vendor.
Because payer policies can vary widely regarding the entry of charges and where the drug detail should
be reported on the claim form, please contact the payer to clarify the billing policies for drugs that are
provider-administered but not provider-purchased. AccessOne® is also available to help research payerspecific policies for documenting non-charged drugs.
*Data on file with Janssen Biotech, Inc.
27
Appendix E: Medicare Quality Programs*
Medicare quality programs apply to both the hospital outpatient department and the physician practice
setting. The programs are designed to reward high quality, efficient performance and support the move
from payment for volume to payment for value. Compliance with the requirements may preserve or
enhance payments and non-compliance may decrease payments across the relevant Medicare payment
systems. The following is a brief overview of programs applicable to the hospital outpatient department and
physician practice sites of care. Please refer to the respective websites for additional detail and resources.
Hospital Outpatient Departments
The Hospital Outpatient Quality Reporting Program (Hospital OQR) is a pay for quality data
reporting program implemented by CMS for outpatient hospital services. This program requires
hospitals that are paid under the Outpatient Prospective Payment System (OPPS) to report quality
measures for care provided in their outpatient settings. There is no upward payment adjustment
available with the Hospital OQR. Hospitals that fail to comply are subject to a two (2) percentage point
reduction in their annual payment update across the OPPS. For more information and resources, please
see the Hospital OQR home page at the CMS website:
http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/
HospitalOutpatientQualityReportingProgram.html.
Physician Practice Settings
The Physician Quality Reporting System (PQRS) is intended to promote reporting of quality
information by eligible professionals (EPs)† practicing in the medical office setting. Under the PQRS EPs
are encouraged to report quality measures for covered professional services furnished to Medicare Part
B Fee-for-Service (FFS) beneficiaries or incur a payment reduction under the Physician Fee Schedule
(PFS). There is no longer an upward payment adjustment available to PQRS participants. Additionally,
successful participation in PQRS is fundamental to successful participation in the Physician Value-Based
Payment Modifier program (see below). The following website serves as the primary and authoritative
source for all publicly available information and CMS-supported educational and implementation
support materials for PQRS:
http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.
html?redirect=/PQRI/01_Overview.asp.
The Physician Value-Based Payment Modifier (VM) is designed to support the transformation of
Medicare from a passive payer to an active purchaser of higher quality, more efficient health care
through the value-based purchasing (VBP) initiative. The VM is designed to provide comparative
performance information to eligible professionals and medical practice groups to improve the
quality and efficiency of medical care. Both cost and quality data are included in calculating the
VM. In 2017, the VM applies to all physicians who bill Medicare for services provided under the PFS, and
in 2018, to all EPs.†‡ Based on quality and cost performance compared to benchmarks, both upward and
downward payment adjustments are possible under the VM program. For a detailed discussion of the
VM and access to resources, please see:
http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/
ValueBasedPaymentModifier.html.
* This summary provides an overview of the prominent Medicare quality programs and is not intended to be all-inclusive. Other factors/programs may
ultimately impact payment in the hospital outpatient department or physician practice settings. Within some programs, under specific circumstances,
hardship exemptions may apply.
† EPs include physicians, nurse practitioners, physician assistants, and others. Disciplines included as EPs may vary between quality programs.
‡ The performance period precedes the payment adjustment period by two years (ie, participation in 2016 impacts payment in 2018).
28
Appendix F: ICD-10-CM
The compliance date for implementation of ICD-10-CM was October 1, 2015, for all Health
Insurance Portability and Accountability Act (HIPAA)-covered entities. ICD-10-CM replaces
International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) Diagnosis
Codes in all healthcare settings for diagnosis reporting with dates of service, or dates of discharge
for inpatients, that occur on or after October 1, 2015.
There is no grace period, however CMS acknowledges that ICD-10 is a significant change and has
implemented some provider supports to help the transition:
• Coding: for the first 12 months after ICD-10 implementation, Medicare review contractors
will not deny PFS claims based solely on the specificity of the ICD-10 diagnosis code, as long
as the claims contain a code from the right family.
• Problem resolution: developed a communication and collaboration center
(ICD10@cms.hhs.gov) responsible for identifying and initiating resolution of issues that arise
as a result of the ICD-10 transition.
• Ombudsman: appointed William Rogers, MD, as the ICD-10 Ombudsman MD
(ICD10_Ombudsman@cms.hhs.gov) to help receive and triage physician and other provider issues1.
Approach to ICD-10
To help providers smooth the transition to ICD-10, CMS recommends the following 3-step process:
Step 1 For general ICD-10 information, access the many resources on the CMS ICD-10 and Road to 10
web pages (see “Resources”, below).
Step 2 Contact your Medicare Administrative Contractor (MAC) for Medicare claims questions. If you
have a Medicaid claim question contact your State Medicaid Agency. If you have a commercial or
private health plan claim question, please contact your health plan directly.
Step 3 Contact the ICD-10 Ombudsman for questions. The ICD-10 Ombudsman is an impartial
advocate with a dedicated team of experts to answer your questions. Send your Ombudsman
inquiries to ICD10_Ombudsman@cms.hhs.gov. Responses typically will be sent within 3 business days
of receipt.
Resources
ICD-10 Code Lookup
Enter a code or keyword to conduct your search for ICD-10 Codes.
https://www.cms.gov/medicare-coverage-database/staticpages/icd-10-code-lookup.aspx
Road to 10: The Small Physician Practice’s Route to ICD-10
The Road to 10 is a no-cost tool intended to familiarize providers with ICD-10; explore the common
codes; review clinical documentation and clinical scenarios; provide additional resources associated
with specialty practice; and help create an action plan.
http://www.roadto10.org
¹ CMS. ICD-10 Letter to Medicare Providers. July 7, 2015, at: https://www.cms.gov/Medicare/Coding/ICD10/Downloads/MedicareProviderICD-10.pdf;
see also the ICD-10 Ombudsman and ICD-10 Coordination Center (ICC) web page, at: https://www.cms.gov/Medicare/Coding/ICD10/
ICD10OmbudsmanandICD10CoordinationCenterICC.html.
29
Appendix F: ICD-10-CM (continued)
ICD-10: Resources for Specialties and Selected Health Conditions and Services
This guide offers links to webcasts, videos, interactive case studies and other resources, by specialty.
Specialty categories include: dermatology, Family Practice and Internal Medicine, Pharmacy and others.
https://www.cms.gov/Medicare/Coding/ICD10/Downloads/ICD10SpecialtyResourcesGuide20151123.pdf
Provider ICD-10 Resource Guide & Contact List
CMS developed this state-by-state list of contacts for Medicare and Medicaid ICD-10 questions;
includes a link to contact the ICD-10 Ombudsman:
https://www.cms.gov/Medicare/Coding/ICD10/ICD-10-Provider-Contact-Table.pdf
ICD-10-CM Official Guidelines for Coding and Reporting FY 2016
These guidelines have been approved by the four organizations that make up the Cooperating Parties
for the ICD-10-CM: the American Hospital Association (AHA), the American Health Information
Management Association (AHIMA), CMS, and the National Center for Health Statistics (NCHS). The
guidelines are a set of rules that have been developed to accompany and complement the official
conventions and instructions provided within the ICD-10-CM itself.
https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2016-ICD-10-CM-Guidelines.pdf
2016 ICD-10-CM and GEMs
This CMS website provides links to 2016 ICD-10-CM coding resources, including the General
Equivalence Mappings (GEMs) for 2016.
https://www.cms.gov/Medicare/Coding/ICD10/2016-ICD-10-CM-and-GEMs.html
ICD-10-CM Coding Basics and Coding for ICD-10-CM: More of the Basics (videos)
This MedLearn Matters video series presents an overview of ICD-10-CM and introduction to coding.
https://www.youtube.com/watch?v=kCV6aFlA-Sc#t=0m0s
https://www.youtube.com/watch?v=s86pXhhOG7c
ICD-10 Post-Implementation: Coding Basics Revisited
In this 33-minute video, Sue Bowman from the American Health Information Management Association
(AHIMA) and Nelly Leon-Chisen from the American Hospital Association (AHA) discuss the unique
characteristics and features of the new coding system: what is a valid code; guidelines for coding
and reporting; coding process and examples: 7th character, unspecified codes, external cause codes,
laterality; how to submit coding questions and resources for coders.
https://www.cms.gov/Outreach-and-Education/Outreach/FFSProvPartProg/Provider-PartnershipEmail-Archive-Items/2015-12-10-eNews.html?DLPage=1&DLEntries=10&DLSort=0&DLSortDir=descendi
ng#ICD-10%20Post-Implementation:%20Coding%20Basics%20Revisited
In addition to CMS, many medical and trade associations offer ICD-10 resources:
American Academy of Professional Coders (AAPC)
https://www.aapc.com/icd-10/
American Health Information Management Association (AHIMA)
http://www.ahima.org
American Medical Association (AMA)
http://www.ama-assn.org/ama/pub/physician-resources/solutions-managing-your-practice/
coding-billing-insurance/hipaahealth-insurance-portability-accountability-act/transaction-code-setstandards/icd10-code-set.page
30
Appendix G: Resources
The following resources are available to you and your patients.
AccessOne®
AccessOne® provides information and assistance regarding coding, coverage, and claim submissions
related to REMICADE® (infliximab). In addition, AccessOne® can also investigate specialty pharmacy
options that may be available to simplify product procurement and billing for healthcare providers.
Finally, AccessOne® can provide coverage information and support directly to patients.
Call 1 (888) ACCESS-1 (1-888-222-3771), Monday through Friday, 8 AM to 8 PM, ET.
Services:
• Benefits investigation to determine patient-specific benefits for REMICADE®
• Alternate coverage research for patients requiring coverage or additional coverage for REMICADE®
• Requirements for the prior authorization process
• Assistance with the appeal process for administrative denials
• Infusion site location assistance through www.2infuse.com
• Personalized care coordination including benefits explanation to your patients
Upon patient request:
• Patient education materials, providing disease-state information and infusion education for all
approved indications for REMICADE®
Patient insurance benefit investigation is provided as a service by The Lash Group, Inc., under contract
for Janssen Biotech, Inc. In this regard, The Lash Group, Inc., assists healthcare professionals in the
determination of whether treatment could be covered by the applicable third-party payer based on
coverage guidelines provided by the payer and patient information provided by the healthcare provider
under appropriate authorization following the provider’s exclusive determination of medical necessity.
This reimbursement support service has no independent value to providers apart from the product and
is included within the cost of the product.
Importantly, insurance verification is the ultimate responsibility of the provider. Third-party
reimbursement is affected by many factors. Therefore, The Lash Group, Inc., and Janssen Biotech, Inc.,
make no representation or guarantee that full or partial insurance reimbursement or any other payment
will be available. This information is provided as an information service only. While The Lash Group, Inc.,
tries to provide correct information, it and Janssen Biotech, Inc., make no representations or warranties,
expressed or implied, as to the accuracy of the information. In no event shall The Lash Group, Inc., or
Janssen Biotech, Inc., or its employees or agents be liable for any damages resulting from, or relating to,
these services. All providers and other users of this information agree that they accept responsibility for
the use of this service.
31
Patient Assistance Programs
Foundations offer assistance with out-of-pocket costs for prescription drugs. Patients that are having
difficulty paying for their medications, and that have federally funded Medicare, Medicaid, TRICARE, or
commercial insurance, may qualify for additional support from foundations. Fund availability can vary
from time to time. If initially there is no funding available it may be helpful to periodically check back
with these sources.
Foundation
Services
Contact Information
HealthWell Foundation
Assistance with cost-sharing
•premiums
•deductibles
•co-payments
•co-insurance
P.O. Box 4133
Gaithersburg, MD 20885
1-800-675-8416
www.healthwellfoundation.org
Patient Access Network
Foundation
Assistance with cost-sharing
•co-payments
•co-insurance
P.O. Box 221858
Charlotte, NC 28222
1-866-316-PANF (7263)
www.panfoundation.org
Patient Advocate
Foundation
• support and referral
services
• Co-Pay Relief
Program
421 Butler Farm Rd.
Hampton, VA 23666
1-800-532-5274
www.patientadvocate.org
Co-Pay Relief Program
1-866-512-3861
www.copays.org
Johnson & Johnson Patient Assistance Foundation, Inc. (JJPAF) is committed to providing access to
medicines for uninsured patients who lack the financial resources to pay for them. If your patient needs
REMICADE® (infliximab), and is uninsured and unable to pay for their medicine, please have them
contact a JJPAF program specialist at 1-800-652-6227 (9 AM to 6 PM, ET) or visit the foundation website
at http://jjpaf.org to see if they might qualify for assistance.
32
Important Safety Information for
REMICADE® (infliximab)
SERIOUS INFECTIONS
Patients treated with REMICADE® (infliximab) are at increased risk for developing serious
infections that may lead to hospitalization or death. Most patients who developed
these infections were taking concomitant immunosuppressants such as methotrexate or
corticosteroids. Discontinue REMICADE® if a patient develops a serious infection or sepsis.
Reported infections include:
- Active tuberculosis (TB), including reactivation of latent TB. Patients frequently presented
with disseminated or extrapulmonary disease. Patients should be tested for latent TB before
and during treatment with REMICADE®.1,2 Treatment for latent infection should be initiated
prior to treatment with REMICADE®.
- Invasive fungal infections, including histoplasmosis, coccidioidomycosis, candidiasis,
aspergillosis, blastomycosis and pneumocystosis. Patients may present with disseminated,
rather than localized, disease. Empiric anti-fungal therapy should be considered in patients at
risk for invasive fungal infections who develop severe systemic illness.
- Bacterial, viral, and other infections due to opportunistic pathogens, including Legionella and
Listeria.
The risks and benefits of treatment with REMICADE® should be carefully considered prior to
initiating therapy in patients with chronic or recurrent infection. Closely monitor patients
for the development of signs and symptoms of infection during and after treatment with
REMICADE®, including the possible development of TB in patients who tested negative for
latent TB infection prior to initiating therapy, who are on treatment for latent TB, or who were
previously treated for TB infection.
Risk of infection may be higher in patients greater than 65 years of age, pediatric patients, patients
with co-morbid conditions and/or patients taking concomitant immunosuppressant therapy.
In clinical trials, other serious infections observed in patients treated with REMICADE® included
pneumonia, cellulitis, abscess, and skin ulceration.
MALIGNANCIES
Lymphoma and other malignancies, some fatal, have been reported in children and adolescent
patients treated with TNF blockers, including REMICADE®. Approximately half of these
cases were lymphomas, including Hodgkin’s and non-Hodgkin’s lymphoma. The other cases
represented a variety of malignancies, including rare malignancies that are usually associated with
immunosuppression and malignancies that are not usually observed in children and adolescents.
The malignancies occurred after a median of 30 months after the first dose of therapy. Most of the
patients were receiving concomitant immunosuppressants.
Postmarketing cases of hepatosplenic T-cell lymphoma, a rare type of T-cell lymphoma, have
been reported in patients treated with TNF blockers, including REMICADE®. These cases have had
a very aggressive disease course and have been fatal. The majority of reported REMICADE® cases
have occurred in patients with Crohn’s disease or ulcerative colitis and most were in adolescent
and young adult males. Almost all of these patients had received treatment with azathioprine or
6-mercaptopurine concomitantly with REMICADE® at or prior to diagnosis. Carefully assess the
risks and benefits of treatment with REMICADE®, especially in these patient types.
(continued)
33
Important Safety Information for
REMICADE® (infliximab)
(continued)
MALIGNANCIES (continued)
In clinical trials of all TNF inhibitors, more cases of lymphoma were observed compared with controls
and the expected rate in the general population. However, patients with Crohn’s disease, rheumatoid
arthritis, or plaque psoriasis may be at higher risk for developing lymphoma. In clinical trials of some
TNF inhibitors, including REMICADE® (infliximab), more cases of other malignancies were observed
compared with controls. The rate of these malignancies among patients treated with REMICADE®
was similar to that expected in the general population whereas the rate in control patients was lower
than expected. Cases of acute and chronic leukemia have been reported with postmarketing TNFblocker use. As the potential role of TNF inhibitors in the development of malignancies is not known,
caution should be exercised when considering treatment of patients with a current or a past history of
malignancy or other risk factors such as chronic obstructive pulmonary disease (COPD).
Melanoma and Merkel cell carcinoma have been reported in patients treated with TNF-blocker therapy,
including REMICADE®. Periodic skin examination is recommended for all patients, particularly those with
risk factors for skin cancer.
CONTRAINDICATIONS
REMICADE® is contraindicated in patients with moderate to severe (NYHA Class III/IV) congestive heart
failure (CHF) at doses greater than 5 mg/kg. Higher mortality rates at the 10 mg/kg dose and higher
rates of cardiovascular events at the 5 mg/kg dose have been observed in these patients. REMICADE®
should be used with caution and only after consideration of other treatment options. Patients should
be monitored closely. Discontinue REMICADE® if new or worsening CHF symptoms appear. REMICADE®
should not be (re)administered to patients who have experienced a severe hypersensitivity reaction or
to patients with hypersensitivity to murine proteins or other components of the product.
HEPATITIS B REACTIVATION
TNF inhibitors, including REMICADE®, have been associated with reactivation of hepatitis B virus (HBV)
in patients who are chronic carriers. Some cases were fatal. Patients should be tested for HBV infection
before initiating REMICADE®. For patients who test positive, consult a physician with expertise in the
treatment of hepatitis B. Exercise caution when prescribing REMICADE® for patients identified as carriers
of HBV and monitor closely for active HBV infection during and following termination of therapy with
REMICADE®. Discontinue REMICADE® in patients who develop HBV reactivation and initiate antiviral
therapy with appropriate supportive treatment. Exercise caution when considering resumption of
REMICADE® and monitor patients closely.
HEPATOTOXICITY
Severe hepatic reactions, including acute liver failure, jaundice, hepatitis, and cholestasis have been reported
rarely in patients receiving REMICADE® postmarketing. Some cases were fatal or required liver transplant.
Aminotransferase elevations were not noted prior to discovery of liver injury in many cases. Patients with
symptoms or signs of liver dysfunction should be evaluated for evidence of liver injury. If jaundice and/or
marked liver enzyme elevations (eg, ≥5 times the upper limit of normal) develop, REMICADE® should be
discontinued, and a thorough investigation of the abnormality should be undertaken.
34
HEMATOLOGIC EVENTS
Cases of leukopenia, neutropenia, thrombocytopenia, and pancytopenia (some fatal) have been
reported. The causal relationship to REMICADE® therapy remains unclear. Exercise caution in patients
who have ongoing or a history of significant hematologic abnormalities. Advise patients to seek
immediate medical attention if they develop signs and symptoms of blood dyscrasias or infection.
Consider discontinuation of REMICADE® in patients who develop significant hematologic abnormalities.
HYPERSENSITIVITY
REMICADE® has been associated with hypersensitivity reactions that differ in their time of onset.
Acute urticaria, dyspnea, and hypotension have occurred in association with infusions of REMICADE®.
Serious infusion reactions including anaphylaxis were infrequent. Medications for the treatment of
hypersensitivity reactions should be available.
NEUROLOGIC EVENTS
TNF inhibitors, including REMICADE®, have been associated in rare cases with CNS manifestation of
systemic vasculitis, seizure, and new onset or exacerbation of CNS demyelinating disorders, including
multiple sclerosis and optic neuritis, and peripheral demyelinating disorders, including Guillain-Barré
syndrome. Exercise caution when considering REMICADE® in patients with these disorders and consider
discontinuation if these disorders develop.
AUTOIMMUNITY
Treatment with REMICADE® may result in the formation of autoantibodies and, rarely, in development of
a lupus-like syndrome. Discontinue treatment if symptoms of a lupus-like syndrome develop.
ADVERSE REACTIONS
In clinical trials, the most common REMICADE® adverse reactions occurring in >10% of patients included
infections (eg, upper respiratory, sinusitis, and pharyngitis), infusion-related reactions, headache, and
abdominal pain.
LIVE VACCINES/THERAPEUTIC INFECTIOUS AGENTS
Live vaccines or therapeutic infectious agents should not be given with REMICADE® due to the possibility
of clinical infections, including disseminated infections.
Bring pediatric patients up to date with all vaccinations prior to initiating REMICADE®. At least a 6-month
waiting period following birth is recommended before the administration of any live vaccine to infants
exposed in utero to REMICADE®.
For more information, please see Important Safety Information, full Prescribing
Information, and Medication Guide for REMICADE®. Provide the Medication Guide to your
patients and encourage discussion.
References: 1. American Thoracic Society, Centers for Disease Control and Prevention. Targeted tuberculin testing and treatment of latent
tuberculosis infection. Am J Respir Crit Care Med. 2000;161:S221-S247. 2. See latest Centers for Disease Control guidelines and recommendations for
tuberculosis testing in immunocompromised patients.
35
039670-150902
USE WITH OTHER DRUGS
Concomitant use of REMICADE® with anakinra, abatacept, tocilizumab, or other biologics used to treat
the same conditions as REMICADE® is not recommended because of the possibility of an increased
risk of infection. Care should be taken when switching from one biologic to another, since overlapping
biological activity may further increase the risk of infection.
Please see full Prescribing Information and Medication Guide for
REMICADE® (infliximab), also available at www.remicade.com.
Extensive resources available at www.janssenaccessone.com.
Janssen Biotech, Inc.
© Janssen Biotech, Inc. 2016
04/16
051454-160415