Cytomegalovirus and Lung Transplantation
advertisement

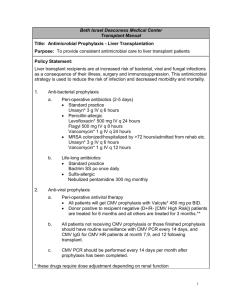
American Journal of Transplantation 2004; 4: 1219–1226 Blackwell Munksgaard C Blackwell Munksgaard 2004 Copyright doi: 10.1111/j.1600-6143.2004.00505.x Minireview Cytomegalovirus and Lung Transplantation Martin R. Zamora∗ Division of Pulmonary Sciences and Critical Care Medicine, and the Lung Transplant Program, University of Colorado Health Sciences Center, Denver, CO ∗ Corresponding author: Martin Zamora, Marty.Zamora@uchsc.edu Cytomegalovirus (CMV) infection remains a serious problem in lung transplant recipients. Development of potent oral antiviral agents, molecular techniques for the detection of infection and its response to therapy and the emergence of isolates with antiviral resistance have had significant impacts on the approach to CMV in these patients. This article discusses the following issues as part of a comprehensive CMV management strategy in lung transplant recipients: (1) Prevention strategies in the era of potent oral antiviral agents, (2) the role of new diagnostic techniques in the management of CMV, (3) treatment regimens for established CMV infection or disease, (4) the potential impact of treatment of CMV on the indirect effects on long-term allograft function, and (5) the incidence, risk factors for and impact of ganciclovir resistance following lung transplantation. Key words: Antiviral resistance, ganciclovir, polymerase chain reaction, valganciclovir Received 7 September 2003, revised and accepted for publication 25 March 2004 seronegative recipients of seropositive organs are at the highest risk of severe disease and require prophylaxis, despite more than a decade of experience with lung transplantation and ganciclovir availability, management of the CMV seropositive recipient remains controversial. Risk of CMV Infection and Disease in Lung Transplant Recipients The incidence of CMV infection and disease following lung transplantation in the postganciclovir era ranges from 30 to 86% with an associated mortality rate of 2–12% (1). Innate host immunity, the type of organ transplanted with its viral burden, viral coinfection and the net state of immunosuppression affect the risk of developing CMV infection. The Papworth group showed that seronegative heart–lung recipients of CMV-positive organs are at the highest risk of developing severe, sometimes fatal, disease (8). Lung transplantation involves the transfer of large amounts of lymphatic tissue harboring greater amounts of latent CMV than other organs, theoretically increasing the risk and severity of CMV infection (9). Therefore, some authors recommend that all lung transplant recipients should be considered high-risk. Coinfection with other betaherpesviruses (HHV-6 and HHV-7) with inherent immunomodulating properties enhances CMV replication (10). Use of antilymphocytic antibodies for induction therapy or treatment of steroid-resistant rejection increases the rate of CMV reactivation (11). CMV and Acute Chronic Allograft Injury Introduction CMV remains the most important pathogen following lung transplantation (1). Its effects on morbidity and mortality can be divided into direct effects of tissue injury and clinical illness and indirect effects leading to long-term adverse sequelae in the lung allograft. Accumulating evidence suggests the indirect effects of CMV may be at least as important as its direct effects. Via mechanisms of enhanced allorecognition, CMV has been associated with, though not causally linked to, the development of acute and chronic rejection (2). Potential immunomodulatory effects of CMV may predispose patients to infection with opportunistic organisms or the development of post-transplant lymphoproliferative disease (3,4). Cytomegalovirus increases the costs associated with solid organ transplants by 40–50% (5–7). These observations have prompted various strategies for the prevention, early diagnosis and treatment of CMV infection. While there is general consensus that The relationship between CMV and allograft injury is bidirectional (12). Cytokines, chemokines and growth factors are induced in response to both CMV infection and rejection, resulting in activation of the vascular endothelium and inflammatory cells. The proinflammatory cytokine, tumor necrosis factor (TNF), is a key signal in reactivating CMV from latency. TNF-induced activation of protein kinase C and nuclear factor-jB (NFjB) leads to expression of CMV immediate early proteins triggering the onset of viral replication. As TNF is released during allograft rejection, it is not surprising that CMV reactivation occurs in response to acute rejection. Intensified immunosuppression to treat rejection can amplify viral replication: following antilymphocyte agents, the incidence of CMV disease increases from 10 to 15–65% (1). Cytomegalovirus infection of the vascular endothelium and smooth muscle cells likely plays an important role in the 1219 Zamora pathogenesis of vascular injury seen in acute and chronic rejection. Cytomegalovirus up-regulates endothelial adhesion molecules such as VCAM, ICAM, LFA-1 and VLA4, which increases the number of inflammatory cells in the graft. Injury may also occur via molecular mimicry: sequence homology and immunologic cross-reactivity between CMV immediate early antigens and the HLA-DR b chain have been demonstrated and CMV induces a glycoprotein homologous to MHC class I antigens (13). Cytomegalovirus also induces antiendothelial cell antibodies, which may participate directly in the development of chronic rejection. While CMV prophylaxis has been shown to decrease the incidence of acute rejection, therapy of established disease with ganciclovir alone may not prevent the long-term sequelae of CMV-induced graft injury (2). Addition of immunoglobulin preparations which have immunomodulatory properties may be required to limit acute inflammatory events and the progression to chronic allograft injury. Similar strategies have shown efficacy in bone marrow transplant recipients to decrease graft vs. host disease (14). In lung transplant recipients, CMV has been associated with chronic allograft injury or bronchiolitis obliterans syndrome (BOS); the major limiting factor to long-term survival after lung transplantation. Cytomegalovirus pneumonitis and positive CMV serology may be risk factors for BOS; however, these associations are still being debated (2,15– 18). Given that BOS is typically progressive despite augmented immunosuppressive therapy, strategies to prevent BOS are paramount in controlling this devastating complication of lung transplantation. Prevention and treatment of CMV infections may therefore be important strategies to limit the development of BOS. Strategies to Prevent CMV Infection Three potential mechanisms of CMV infection have been recognized: transmission by the donor organ, blood products or reactivation of latent virus in the recipient. Presence of antibody to CMV in the recipient, whether endogenous or passively transferred, provides partial protection against the development of serious and sometimes fatal disease. Absent endogenous antibody protection, primary CMV infections, particularly CMV pneumonitis or gastrointestinal disease, may be quite severe with mortality rates of 2–20% (19). Based on these potential mechanisms of infection, four strategies to prevent CMV infection have been utilized: matching the donor–recipient pair by CMV serologic status, use of CMV-negative blood products, antiviral agents to suppress viral replication and immunoglobulin preparations to provide passive immunization. The use of CMV-negative or leukocyte-reduced blood products clearly decreases the incidence of CMV transmission and infection following lung transplantation (17). In CMV-negative bone marrow trans1220 plant recipients, seronegative blood results in an incidence of CMV infection transmission of 1.3% while leukocytereduced CMV-positive blood results in a transmission rate of 2.4% with CMV disease rates of 0% and 2.4%, respectively (20). Therefore, it seems prudent to strictly adhere to use of CMV-negative blood products in seronegative lung transplant recipients. Seromatching recipients and donors may be ideal but is impractical given the current shortage of donor organs. Furthermore, seromatching, while perhaps desirable, is most likely no longer necessary to prevent the direct effects on morbidity and mortality given the efficacy of antivirals and immunoglobulins in decreasing the incidence and severity of primary CMV infections. However, caution may still be warranted when performing CMV-mismatched transplants, as the long-term sequelae of CMV infections on allograft function remains unknown. Many retrospective or case-controlled series have demonstrated the benefit of antivirals or immunoglobulin preparations alone or in combination in decreasing or delaying the onset of CMV infection following lung transplantation. However, to date, primarily owing to the lack of randomized, controlled trials comparing regimens, the ‘ideal’ strategy for the prevention, monitoring and treatment of CMV remains controversial. Monitoring Techniques Rapid and accurate diagnostic tests are critical for the appropriate management of CMV following lung transplantation. Qualitative or quantitative polymerase chain reaction (PCR) [TaqMan (Applied Biosystems, Foster City, CA, USA) CMV quantitative PCR and the COBAS AMPLICOR (Roche Diagnostics, Pleasanton, CA, USA) CMV Monitor] using serum, plasma or circulating peripheral blood leukocytes or the pp65 antigenemia test (CMV-vue kit), are efficacious in solid organ transplant and bone marrow transplant recipients (21–26). The hybrid capture assay, a non-PCR, molecular, quantitative and highly sensitive assay, has been shown to be effective in lung transplant recipients (27,28). Each test has their own advantages and disadvantages. The quantitative PCR and hybrid capture assays are fully quantitative, molecular techniques. Qualitative PCR is much less useful. PCR requires radioactive probes and most centers use ‘homemade primers’ thereby precluding standardization. The pp65 antigenemia assay is only semiquantitative (read as number of positive cells) although their readings can be used in the same ways by clinicians experienced in its interpretation and may be more labor intensive in that the cells need to be spun and placed on slides within 6 h of arrival to the laboratory. The value of a quantitative assay such as viral load is seen by its increased utilization by clinicians for assessing or predicting the severity of illness or impending illness (29). Weinberg et al. (30) evaluated serial CMV blood cultures, antigenemia, and qualitative and quantitative plasma PCR tests for their value in predicting CMV disease and for American Journal of Transplantation 2004; 4: 1219–1226 Cytomegalovirus and Lung Transplantation guiding preemptive therapy after lung transplantation. They found that PCR and antigenemia tests were the most effective predictors of symptomatic CMV infections and the response to therapy. Cytomegalovirus PCR-measured DNA increased 5–10-fold immediately preceding symptoms and PCR and antigenemia levels decreased with anti-CMV therapy. A number of these monitoring tests are commercially available and regardless of which method is chosen the technique should be validated in each individual transplant center. but had limited efficacy in preventing CMV infection or disease (15,31). Studies employing extended prophylactic therapy with ganciclovir for 6–12 weeks suggested that prolonged ganciclovir infusion decreased the incidence of CMV infection and disease (32), however, the benefit was lost when patients were followed more than a year posttransplant (33). These reports point out the importance of long-term follow up when comparing published reports and confirm that ganciclovir monotherapy delays rather than prevents the onset of CMV infection following lung transplantation. Prophylaxis of CMV Infection The largest prospective trial utilizing ganciclovir monotherapy was reported by Hertz et al. (34). Ganciclovir was given intravenously for 3 months post-transplant either daily or thrice-weekly. There were no significant differences between groups with respect to freedom from CMV infection or disease or in the incidence of BOS. Cytomegalovirus disease developed in 18/35 (51%) of the daily patients vs. 11/37 (30%) of the thrice-weekly patients and emerged shortly after termination of prophylaxis. While prolonged thrice-weekly ganciclovir prophylaxis was as effective as daily administration at delaying the onset of CMV infections, it was still associated with patient inconvenience, catheter-related infections and increased costs. Before the development of effective antiviral agents, CMV caused illness in the majority of lung transplant recipients, and primary infection in D+/R– recipients was severe and often life-threatening (8). Following the development of ganciclovir it soon became clear that the acute morbidity and mortality of CMV infections could be controlled with therapeutic courses of intravenous ganciclovir. Investigators then sought to determine whether prophylactic use of ganciclovir or other agents could prevent CMV infection and disease following lung transplantation. Most approaches involved universal prophylaxis in which all patients receive prophylaxis for a predetermined amount of time. This strategy aims for complete viral elimination but is associated with increased costs, toxicities and the possibility of the development of resistance. While it is difficult to summarize and compare the published reports on CMV prophylaxis in lung transplant recipients, as they utilized different lengths of prophylaxis in patients receiving different immunosuppressive strategies based on the year of transplant, the published studies can be categorized as those employing ganciclovir or immunoglobulin monotherapy or combination strategies. An alternative strategy to prolonged infusion of ganciclovir is the use of oral ganciclovir. Bhorade et al. (28) found that 12 weeks of oral ganciclovir (3 g per day) decreased the incidence of CMV to levels similar to those seen with intravenous ganciclovir. Cytomegalovirus disease developed in 10/34(29%) lung transplant recipients with an average onset of 4 months. However, 24% of the patients developed asymptomatic, breakthrough viremia. While none of these patients developed CMV disease, this breakthrough viremia may predispose to or be a marker of the emergence of ganciclovir resistance (35). Ganciclovir monotherapy (Table 1) Early studies found that short courses of prophylactic ganciclovir (2–3 weeks) delayed the onset of CMV infection The availability of valganciclovir, which provides antiviral exposure similar to intravenous ganciclovir (comparable AUCs), obviates the need for prolonged intravenous Table 1: Intravenous ganciclovir for cytomegalovirus prophylaxis following lung or heart–lung transplantation (North American centers) Author/year (ref.) n CMV prophylaxis CMV onset Outcome Duncan et al. 1992 Pittsburgh (32) Duncan et al. 1994 Pittsburgh (15) Kelly et al. 1995 Seattle (33) Soghikian et al. 1996 Stanford (31) Hertz et al. 1998 Minnesota (34) Total 13 72 13 GCV ×3 weeks ACY ×2 months GCV ×90 days 5/13 Inf (38%) 2/13 Dz (15%) 8/13 Inf (58%) 21 GCV ×6 weeks 145 52 (L + HL) 35 37 171 GCV ×5 weeks 85 GCV qd × 90d GCV ×3/week NR 268 17/21 Inf (81%) 8/21 Dz (38%) 42/52 Inf (86%) 27/52 Dz (55%) 18/35 Dz (51%) 11/37 Dz (30%) Inf. 101/171 (59.1%) Dz. 66/158 (41.8%) n = number of patients in series receiving intravenous ganciclovir, L + HL = lung and heart–lung transplants, GCV = ganciclovir, ACY = acyclovir, IVIG = standard intravenous immunoglobulin, NR = not reported, Inf = Infection, Dz = disease. American Journal of Transplantation 2004; 4: 1219–1226 1221 Zamora access and allows prolonged high-level antiviral exposure. Valganciclovir was at least as effective as oral ganciclovir in preventing CMV infections and produced more complete viral suppression without the development of antiviral resistance in solid organ recipients (36). When the published results of intravenous ganciclovir monotherapy are pooled, the incidence of CMV infection and disease remains 59% and 42%, respectively (Table 1). While differing lengths of prophylaxis and types of immunosuppression were employed in these studies, taken in sum, these data suggest that while ganciclovir decreases the incidence of CMV infections compared with placebo or oral acyclovir, there is still a significant incidence of CMV infection following lung transplantation with ganciclovir monotherapy strategies. CMV immune globulin monotherapy An alternative strategy to ganciclovir monotherapy is CMV hyperimmune globulin (CMV-IVIG). Maurer reported an incidence of CMV pneumonitis of 28% in patients receiving CMV-IVIG alone (37). Similarly, Gould et al. (38) reported an incidence of CMV disease of 23%. However, a more recent study found that CMV-IVIG alone did not prevent CMV viremia or pneumonitis (39). While this suggests that a randomized, controlled trial comparing these regimens is warranted, it also begs the question as to whether combination prophylaxis with both agents may be more efficacious in the prevention of CMV following lung transplantation. Preemptive Therapy Some centers advocate preemptive therapy based on detection of CMV antigenemia or DNAemia in routinely collected blood samples. The advantage of this strategy is that only high-risk patients are exposed to therapy, which would be expected to decrease cost and toxicity. Several small studies have suggested that this approach is indeed effective in lung transplant recipients. Egan et al. (22) showed that preemptive treatment of CMV infection as determined by antigenemia prevented progression to CMV disease in heart and lung transplant recipients. Kelly et al. (45) found that preemptive therapy directed by the antigenemia assay was as effective as universal prophylaxis with 6 weeks of intravenous ganciclovir and concluded that it was also more cost-effective. There are several potential disadvantages of preemptive therapy: (1) in large geographic regions, it may be difficult to routinely obtain blood samples from the patients, (2) the cost of surveillance may be high, and (3) some patients escape detection and present with severe CMV disease. The latter was a problem in the report by Kelly et al.: 5/19 patients presented with CMV pneumonitis and the antigenemia test revealed zero positive cells (45,46). Such problems with sensitivity and specificity await clarification in larger cohorts of lung transplant recipients. We and others have found that a high viral load was associated with a high degree of progression to symptomatic disease and that following universal prophylaxis, routine monitoring followed by preemptive therapy was effective in preventing the progression to symptomatic disease (28,29). Therefore, our center advocates a combination of the approaches with routine viral load monitoring at scheduled clinic visits. Treatment Combination prophylaxis Bailey et al. (40) reported an 86% incidence of CMV pneumonitis in D+/R– recipients treated with 2–3 weeks of intravenous ganciclovir and standard IVIG. Maurer et al. (37) reported significant decreases in CMV pneumonitis in patients receiving CMV-IVIG and either ganciclovir or oral acyclovir (41% vs. 67%). Further, survival in the combination therapy group approached that seen when both donor and recipient were seronegative. Similarly, we have reported that CMV-IVIG in combination with ganciclovir decreased the incidence of CMV infection to 21% and disease to 31%, their severity and delayed its onset (41). More recently, Valantine et al. (42,43) reported improved outcomes with fewer infections, decreased acute rejection and BOS at 12 and 24 months in the combined therapy group compared with the ganciclovir-only group. Similarly, Weill et al. (44) found that despite induction therapy with daclizumab, when compared with a historical, casecontrolled group receiving ganciclovir alone, combination prophylaxis decreased the incidence of CMV disease from 33% to 8%. 1222 Standard therapy for CMV disease consists of 2–4 weeks of intravenous ganciclovir at a dose of 5 mg/kg twice daily adjusted for renal insufficiency. Somewhat concerning, Duncan et al. (2) found that treatment with intravenous ganciclovir as monotherapy did not prevent the long-term sequelae of CMV. Although no randomized, controlled treatment trials are available for the use of CMV hyperimmune globulin for therapy in organ transplant recipients, many centers add it to ganciclovir for the treatment of tissue invasive CMV pneumonia or colitis. Studies in bone marrow transplant patients with CMV pneumonitis and murine models of disseminated CMV infection suggest that the combination of ganciclovir and CMV hyperimmune globulin may provide significant benefits for immunosuppressed recipients with invasive disease (1,47). One potential role for immunoglobulin therapy may be as replacement therapy in patients with occult hypogammaglobulinemia (48). In these patients, tissue-invasive CMV as well as other infectious complications were more common in the lowest IgG group. Recently, immunoglobulin American Journal of Transplantation 2004; 4: 1219–1226 Cytomegalovirus and Lung Transplantation replacement has been shown to decrease acute rejection and infection in heart transplant recipients with hypogammaglobulinemia (49). The vast majority of isolates causing first episodes of CMV infections in lung transplant recipients are ganciclovir sensitive. Despite this, oral ganciclovir, owing to its low biovailability, has no role in the treatment of symptomatic infection, as it may select resistant clones of CMV when high viral loads and active viral proliferation are occurring. However, oral ganciclovir may have a role in the prevention of relapsing symptomatic disease. The risk of recurrent disease ranges from 20% in seropositive recipients to 60% in those with primary disease (50). The use of oral ganciclovir for 3 months following a full course of intravenous therapy may decrease the risk of recurrent disease by up to 50% (51,52). Whether the use of combination therapy followed by oral ganciclovir decreases the recurrence risk further is presently unknown. Antiviral Resistance Antiviral-resistant CMV is increasing in all solid organ transplants and is particularly problematic following lung transplantation with an incidence of 3–16% (53). These estimates are imprecise, as much of the data has been collected retrospectively and there is significant variability among centers (54), some of which is owing to the fact that genotypic testing of isolates provides greater sensitivity in detecting resistance than the culture-based methods in use at most centers. It is concerning that antiviral resistance has been associated not only with treatment failure, but poor long-term allograft function and decreased patient survival. Kruger et al. (55) found an incidence of ganciclovir resistance in their lung transplant cohort of 5.2%, which resulted in increased positive viral blood cultures, CMV pneumonia, decreased overall survival and the earlier onset of BOS. The most important risk factors for antiviral resistance are D+/R– status and the intensity of immunosuppression. Suboptimal antiviral prophylaxis, which may occur with oral ganciclovir owing to its poor bioavailability, is another risk factor for resistance. Finally, the intensity of the immunosuppressive regimen, particularly the use of antithymocyte globulin or OKT3 for induction therapy or treatment of rejection episodes, is associated with the development of antiviral resistance (56–58). Resistance should be suspected in patients who fail to respond to intravenous ganciclovir therapy of tissue-invasive CMV infections, who have persistent viremia or recurrent viremia during or after ganciclovir prophylaxis. While neither has been validated, the lack of complete resolution of clinical symptoms or the failure of the viral load (by antigenemia or PCR) to decline after 2–3 weeks of therapy have been postulated to indicate the presence of a resisAmerican Journal of Transplantation 2004; 4: 1219–1226 tant isolate (54). Empiric switch therapy to foscarnet or combination therapy with ganciclovir and foscarnet should be performed while awaiting laboratory confirmation of resistance (59). Genotypic analysis is more sensitive than phenotypic or plaque reduction assays and may provide a more rapid diagnosis of resistance. Ganciclovir resistance occurs by two mechanisms: mutations in the UL97 gene, which codes for a phosphotransferase important in the phosphorylation of ganciclovir to its active form, and mutation in the UL54 gene, which encodes the viral DNA polymerase. Foscarnet and cidofovir do not require phosphorylation for activation; thus the UL97 mutation does not confer cross-resistance to these agents. However, mutations of the DNA polymerase confer crossresistance to ganciclovir and cidofovir but to foscarnet is less predictable (60). The management of antiviral-resistant CMV disease has been to switch therapy to foscarnet, which is typically effective for the treatment of ganciclovir-resistant isolates. With the emergence of cross-resistant strains the use of cidofovir or combination antiviral therapy with or without immunoglobulin preparations may be required. One such approach has been to use intravenous ganciclovir at 50% its typical dose with once-daily foscarnet, which is gradually increased to a maximum of 125 mg/kg. This approach was effective in solid organ transplant recipients in clearing the infection and no recurrence was seen in the 6–30 months of follow up (59). The immunosuppressive agent leflunomide has been shown in vitro to have activity against resistant isolates (61). Two approaches have been advocated for the prevention of ganciclovir resistance. As suboptimal prophylaxis is associated with resistance, more potent agents may be effective. Valganciclovir, which has greater bioavailability than oral ganciclovir, may allow continual exposure to ganciclovir and may prove to be useful in the future. However, careful analysis of breakthrough viremia for resistance genotypes will be necessary. The other approach is preemptive therapy, which limits exposure to antivirals only to those at high risk as documented by active viral replication. Problems associated with this approach are the frequent monitoring which is required and patients who present with invasive CMV disease. While prolonged exposure to intravenous ganciclovir was associated with the development of resistance and it has been asserted that less antiviral for shorter time periods is beneficial, it is still being debated whether prolonged exposure to potent antivirals or intermittent exposure with preemptive therapy will induce similar levels of resistance. Contrary to what is claimed by advocates of the preemptive approach, such a strategy does not always prevent the emergence of ganciclovir resistance (35). Finally, given the association of CMV pneumonia with BOS, this risk must be weighed against that of developing ganciclovir resistance with prolonged therapy. 1223 Zamora Future Directions in CMV Management Most of the lung transplant literature to date has dealt with the prevention and treatment of the direct effects of CMV. Remaining to be answered, is whether the prevention of CMV proliferation, or its treatment in the asymptomatic phase, will limit its indirect effects. It has been suggested that even asymptomatic viral proliferation may be associated with the development of BOS in lung transplant recipients. Therefore, it would seem that prevention of any CMV proliferation, or treatment of asymptomatic infections, would be a desirable goal. Preliminary results from our institution suggest that preemptive treatment of asymptomatic CMV DNAemia is associated with a decrease in the acute and chronic effects of CMV infection following lung transplantation when compared with patients with symptomatic viremia or disease (62). The relationship between preemptive therapy and allograft response to CMV infections and augmented immunosuppression (as measured by opportunistic infections) was also investigated in this study. Preemptive therapy of CMV DNAemia decreased CMV-associated acute rejection, but not infection. This suggests that preemptive therapy of asymptomatic CMV infections attenuates the immune response in the allograft but not the augmented immunosuppressive state induced by CMV. Clearly further studies are necessary to investigate the role of treatment strategies on the indirect effects of CMV infection following lung transplantation. Early clinical investigations with valganciclovir make maintenance therapy more convenient, however, there appear to be potential dose-limiting properties (e.g. bone marrow suppression) (37,62). Frequent monitoring of complete blood counts and serum creatinine will be required to properly dose-adjust valganciclovir. Profound neutropenia may also increase the risk of fungal infection, which may counteract the benefit of preventing CMV. Future studies will be necessary to determine the role of oral valganciclovir in universal or preemptive prophylaxis, as a single prophylactic agent or in combination with immunoglobulin preparations and possibly for treatment of established disease. The development of ganciclovir-resistant isolates necessitates the development of newer drugs that have high oral bioavailability, low toxicity and mechanisms of action that will allow them to be used against ganciclovir-resistant isolates. The recognition that HHV-6 and HHV-7 are conducive to the development of CMV infection and may be additive to the indirect effects of CMV on allograft function suggests that antivirals with an expanded spectrum against these viruses would be desirable. Conclusion Lung transplant programs still need to refine the types of CMV prophylactic strategies that best match individual re1224 cipients of seropositive and seronegative allografts and the type of immunosuppression utilized. It seems clear that universal prophylaxis is warranted for high-risk D+/R– recipients. However, it remains unclear as to whether R+ recipients are also at higher risk than other solid-organ recipients and whether they should receive universal prophylaxis or preemptive therapy. The use of antilymphocyte globulin would also appear to warrant the use of targeted, preemptive therapy with intravenous ganciclovir followed by 2–3 months of an oral agent. The development of high oral bioavailable drugs such as valganciclovir may provide a more convenient method of prophylaxis or treatment of CMV infections. There is a role for prophylactic hyperimmune anti-CMV immunoglobulin, which may offer advantages for specific lung transplant recipients and improve both short-term and long-term morbidity and mortality. However, better definitions for which patients likely benefit from it are needed owing to the lack of pharmacoeconomic analyses of the various strategies. Combination therapy may also provide the opportunity to prevent and treat chronic and progressive allograft injury, particularly in the thoracic organs. Finally, molecular techniques should be employed for the detection of CMV infection, for determining the response to and duration of therapy and for the determination of the emergence of ganciclovirresistant isolates. Ongoing studies should help to answer these issues as well as generating new hypotheses in the role of CMV infection in chronic allograft failure following lung transplantation. References 1. Fishman JA, Rubin RH. Infection in organ-transplant recipients. N Engl J Med 1998; 338: 1741–1751. 2. Duncan SR, Paradis IL, Yousem SA et al. Sequelae of cytomegalovirus pulmonary infections in lung allograft recipients. Am Rev Respir Dis 1992; 146: 1419–1425. 3. Snydman DR. Infection in solid organ transplantation. Transpl Infect Dis 1999; 1: 21–28. 4. Singh N, Arnow PM, Bonham A et al. Invasive aspergillosis in liver transplant recipients in the 1990s. Transplantation 1997; 64: 716–720. 5. McCarthy JM, Karim MA, Krueger H, Keown PA. The cost impact of cytomegalovirus disease in renal transplant recipients. Transplantation 1993; 55: 1277–1282. 6. Falagas ME, Arbo M, Ruthhazer R et al. Cytomegalovirus disease is associated with increased cost and hospital length of stay among orthotopic liver transplant recipients. Transplantation 1997; 63: 1595–1601. 7. Kim WR, Badley AD, Weisner RH et al. The economic impact of cytomegalovirus infection after liver transplantation. Transplantation 2000; 69: 357–361. 8. Wreghitt T. Cytomegalovirus infections in heart and heart-lung transplant recipients. J Antimicrob Chemother 1989; 23: 49–60. 9. Balthesen M, Messerle M, Reddehase MJ. Lungs are a major organ site of cytomegalovirus latency and recurrence. J Virol 1993; 67: 5360–5366. 10. Mendez JC, Dockrell DH, Espy MJ et al. Human betaherpesvirus interactions in solid organ transplant recipients. J Infect Dis 2001; 183: 179–184. American Journal of Transplantation 2004; 4: 1219–1226 Cytomegalovirus and Lung Transplantation 11. Jamil B, Nicholls KM, Becker GJ, Walker RG. Influence of antirejection therapy on the timing of cytomegalovirus disease and other infections in renal transplant recipients. Clin Transplant 2000; 14: 14–18. 12. Tolkhoff-Rubin NE, Fishman JA, Rubin RH. The bidirectional relationship between cytomegalovirus and allograft injury. Transplant Proc 2001; 33: 1773–1775. 13. Beck S, Barrell BG. Human cytomegalovirus encodes a glycoprotein homologous to MHC class-I antigens. Nature 1988; 331: 269–272. 14. Winston DJ, Antin JH, Wolff SN et al. A multicenter, randomized, double-blind comparison of different doses of intravenous immunoglobulin for prevention of graft-versus-host disease and infection after allogeneic bone marrow transplantation. Bone Marrow Transplant 2001; 28: 187–196. 15. Duncan SR, Grgurich WF, Iacono AT et al. A comparison of ganciclovir and acyclovir to prevent cytomegalovirus after lung transplantation. Am Rev Respir Dis 1994; 150: 146–152. 16. Schulman LL, Weinberg AD, McGregor CC, Suciu-Foca NM, Itescu S. Influence of donor and recipient HLA locus mismatching on development of obliterative bronchiolitis after lung transplantation. Am J Respir Crit Care Med 2001; 163: 437–442. 17. Ettinger NA, Bailey TC, Trulock EP et al. Cytomegalovirus infection and pneumonitis. Am Rev Respir Dis 1993; 147: 1017–1023. 18. Sharples LD, Tamm M, McNeil K, Higenbottam TW, Stewart S, Wallwork J. Development of bronchiolitis obliterans syndrome in recipients of heart-lung transplantation – early risk factors. Transplantation 1996; 61: 560–566. 19. Valantine HA. Prevention and treatment of cytomegalovirus disease in thoracic organ transplant patients: evidence for a beneficial effect of hyperimmune globulin. Transplant Proc 1995; 27: 49–57. 20. Bowden RA, Slichter SJ, Sayers M et al. A comparison of filtered leukocyte-reduced and cytomegalovirus (CMV) seronegative blood products for the prevention of transfusion-associated CMV infection after marrow transplant. Blood 1995; 86: 3598– 3603. 21. Baldanti F, Revello MG, Percivalle E, Gerna G. Use of the human cytomegalovirus (HCMV) antigenemia assay for diagnosis and monitoring of HCMV infections and detection of antiviral drug resistance in the immunocompromised. J Clin Virol 1998; 11: 51– 60. 22. Egan JJ, Barber L, Lomax J et al. Detection of human cytomegalovirus antigenemia: a rapid diagnostic technique for predicting cytomegalovirus infection/pneumonitis in lung and heart transplant recipients. Thorax 1995; 50: 9–13. 23. Bewig B, Haacke TC, Tirocke A et al. Detection of CMV pneumonitis after lung transplantation using PCR of DNA from bronchoalveolar lavage cells. Respiration 2000; 67: 166–172. 24. Michaelides A, Liolios L, Glare EM et al. Increased human cytomegalovirus (HCMV) DNA load in peripheral blood leukocytes after lung transplantation correlates with HCMV pneumonia. Transplantation 2001; 72: 141–147. 25. Guiver M, Fox AJ, Mutton K, Mogulkoc N, Egan J. Evaluation of CMV viral load using TaqMan CMV quantitative PCR and comparison with CMV antigenemia in heart and lung transplant recipients. Transplantation 2001; 71: 1609–1615. 26. Masaoka T, Hiraoka A, Ohta K et al. Evaluation of the AMPLICOR CMV, COBAS AMPLICOR CMV monitor, and antigenemia assay for cytomegalovirus disease. Jpn J Infect Dis 2001; 54: 12–16. 27. Mazzulli T. Multicenter comparison of the Digene hybrid capture CMVDNA assay, Version 2.0, the Pp65 antigenemia assay, and cell culture for detection of cytomegalovirus viremia. J Clin Microbiol 1999; 37: 958–63. American Journal of Transplantation 2004; 4: 1219–1226 28. Bhorade SM, Sandesara C, Garrity ER et al. Quantification of cytomegalovirus (CMV) viral load by the hybrid capture assay allows for early detection of CMV disease in lung transplant recipients. J Heart Lung Transplant 2001; 20: 928–934. 29. Humar A, Gregson D, Caliendo AM et al. Clinical utility of quantitative cytomegalovirus viral load determination for predicting cytomegalovirus disease in liver transplant recipients. Transplantation 1999; 68: 1305–1311. 30. Weinberg A, Hodges TN, Li S, Cai G, Zamora MR. Comparison of PCR, antigenemia assay and rapid blood culture for detection and prevention of cytomegalovirus disease after lung transplantation. J Clin Microbiol 2000; 38: 768–772. 31. Soghikian MV, Valentine VG, Berry GJ, Patel HR, Robbins RC, Theodore J. Impact of ganciclovir prophylaxis on heart-lung and lung transplant recipients. J Heart Lung Transplant 1996; 15: 881– 887. 32. Duncan SR, Paradis IL, Dauber JH, Yousem SA, Hardesty RL, Griffith BP. Ganciclovir prophylaxis for cytomegalovirus infections in pulmonary allograft recipients. Am Rev Respir Dis 1992; 146: 1213–1215. 33. Kelly JL, Albert RK, Wood DE, Raghu G. Efficacy of a 6week prophylactic ganciclovir regimen and the role of serial cytomegalovirus antibody testing in lung transplant recipients. Transplantation 1995; 59: 1144–1147. 34. Hertz MI, Jordan C, Savik SK et al. Randomized trial of daily versus three-times-weekly prophylactic ganciclovir after lung and heart-lung transplantation. J Heart Lung Transplant 1998; 17: 913– 920. 35. Limaye AP, Raghu G, Koelle DM, Ferrenberg J, Huang ML, Boeckh M. High incidence of ganciclovir-resistant cytomegalovirus infection among lung transplant recipients receiving preemptive therapy. J Infect Dis 2002; 185: 20–27. 36. Paya CV. A randomized, double-blinded, double-dummy, active comparator controlled multicenter study of the efficacy and safety of valganciclovir vs. oral ganciclovir for prevention of CMV in 372 high-risk (D+/R-) heart, liver and kidney recipients. [Abstract LB-4]. In: Program and Abstracts of the 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy, September, 27-30, 2002, San Diego, California. Washington, D.C.: American Society for Microbiology Press, 2002. 37. Maurer JR, Snell G, deHoyos A, Kesten S, Winton T. Outcomes of lung transplantation using three different cytomegalovirus prophylactic regimens. Transplant Proc 1993; 25: 1434– 1435. 38. Gould FK, Freeman R, Taylor CE, Ashcroft T, Dark JH, Corris PA. Prophylaxis and management of cytomegalovirus pneumonitis after lung transplantation: a review of experience in one center. J Heart Lung Transplant 1993; 12: 695–699. 39. Kruger RM, Paranjothi S, Storch GA, Lynch JP, Trulock EP. Impact of prophylaxis with cytogam alone on the incidence of CMV viremia in CMV-seropositive lung transplant recipients. J Heart Lung Transplant 2003; 22: 754–763. 40. Bailey TC, Trulock EP, Ettinger NA, Storch GA, Cooper JD, Powderly WG. Failure of prophylactic ganciclovir to prevent cytomegalovirus disease in recipients of lung transplants. J Infect Dis 1992; 165: 548–552. 41. Zamora MR. Use of cytomegalovirus immune globulin and ganciclovir for the prevention of cytomegalovirus disease in lung transplantation. Transplant Infect Dis 2001; 3: 49–56. 42. Valantine HA, Luikart H, Doyle R et al. Impact of cytomegalovirus hyoerimmune globulin on outcome after cardiothoracic transplantation: a comparative study of combined prophylaxis with CMV hyperimmune globulin plus ganciclovir versus ganciclovir alone. Transplantation 2001; 72: 1647–1652. 1225 Zamora 43. Poirier CD, Doyle RL, Theodore J, Robbins RC, Reitz BA, Valantine HA. Comparison between CMV Hyperimmune globulin and GCV for CMV prophylaxis in heart-lung and lung transplant recipients. J Heart Lung Transplant 1998; 17: 96. 44. Weill D, Lock BJ, Wewers DL et al. Combination prophylaxis with ganciclovir and cytomegalovirus (CMV) immune globulin after lung transplantation: effective CMV prevention following daclizumab induction. Am J Transplant 2003; 3: 492–496. 45. Kelly J, Hurley D, Raghu G. Comparison of the efficacy and cost effectiveness of pre-emptive therapy as directed by CMV antigenemia and prophylaxis with ganciclovir in lung transplant recipients. J Heart Lung Transplant 2000; 19: 355–359. 46. Weill D, Zamora MR. Comparison of the efficacy and costeffectiveness of pre-emptive therapy as directed by CMV antigenemia and prophylaxis with ganciclovir in lung transplant recipients. J Heart Lung Transplant 2000; 19: 815– 816. 47. Rubin RH, Lynch P, Pasternack MS, Schoenfeld D, Medearis DN JrCombined antibody and ganciclovir treatment of murine cytomegalovirus-infected normals and immunocompromised BALB/c mice. Antimicrob Agents Chemother 1989; 33: 1975– 1979. 48. Goldfarb NS, Avery RK, Goormastic M et al. Hypogammaglobulinemia in lung transplant recipients. Transplantation 2001; 71: 242–246. 49. Yamani MH, Avery R, Mawhorter S et al. Hypogammaglobulinemia following cardiac transplantation: a link between rejection and infection. J Heart Lung Transplant 2001; 20: 425–430. 50. Rubin RH. Prevention and treatment of cytomegalovirus disease in heart transplant patients. J Heart Lung Transplant 2000; 19: 731–735. 51. Turgeon N, Fishman JA, Doran M et al. Prevention of recurrent cytomegalovirus disease in renal and liver transplant recipients: effect of oral ganciclovir. Transpl Infect Dis 2000; 2: 2–10. 52. Nankivell BJ, Malouf MA, Russ GR et al. Maintenance therapy with oral ganciclovir after treatment of cytomegalovirus infection. Clin Transplant 1998; 12: 270–273. 1226 53. Erice A. Resistance of human cytomegalovirus to antiviral drugs. Clin Microbiol Rev 1999; 12: 286–297. 54. Limaye AP, Corey L, Koelle DM, Davis CL, Boeckh M. Emergence of ganciclovir-resistant cytomegalovirus disease among recipients of solid-organ transplants. Lancet 2000; 356: 645–649. 55. Kruger RM, Shannon WD, Arens MQ, Lynch JP, Storch GA, Trulock EP. The impact of ganciclovir-resistant cytomegalovirus infection after lung transplantation. Transplantation 1999; 68: 1272– 1279. 56. Alain S, Honderlick P, Grenet D et al. Failure of ganciclovir treatment associated with selection of a ganciclovir-resistant cytomegalovirus strain in a lung transplant recipient. Transplantation 1997; 62: 1533–1536. 57. Baldanti F, Simoncini L, Sarasini A et al. Ganciclovir resistance as a result of oral ganciclovir in a heart transplant recipient with multiple human cytomegalovirus strains in blood. Transplantation 1998; 66: 324. 58. Lurain N, Ammons H, Kapell K, Yeldandi V, Garrity E, O’Keefe J. Molecular analysis of human cytomegalovirus strains from two lung transplant recipients with the same donor. Transplantation 1996; 62: 497. 59. Chou S, Marousek G, Guentzel S et al. Evolution of mutations conferring multidrug resistance during prophylaxis and therapy of cytomegalovirus disease. J Infect Dis 1998; 176: 786–789. 60. Mylonakis E, Kallas WM, Fishman JA. Combination antiviral therapy for ganciclovir-resistant cytomegalovirus infections in solid organ transplant recipients. Clin Infect Dis 2002; 34: 1337– 1341. 61. Waldman WJ, Knight DA, Lurain NS et al. Novel mechanism of inhibition of cytomegalovirus by the experimental immunosuppressive agent leflunomide. Transplantation 1999; 68: 814–825. 62. Zamora MR, Nicolls M, Weill D et al. Valganciclovir for the prevention of cytomegalovirus following lung transplantation: efficacy and optimal length of therapy. [Abstract 26]. In: Program and abstracts of the American Transplant Congress, May 30– June 4, 2003. Copenhagen, Denmark: Blackwell Munksgaard, 2003. American Journal of Transplantation 2004; 4: 1219–1226