Efficiency of Class II Division 1 and Class II
Division 2 Treatment in Relation to Different
Treatment Approaches
Julia yon Bremen and Hans Pancherz
The aim of this study was to assess the efficiency of Class II Division 1 and
Class II Division 2 treatment comparing different treatment approaches
(conventional and Herbst). Treatment efficiency was defined as a better
result in a shorter treatment time. One hundred forty-two patients aged 10
to 15 years treated in the late mixed and permanent dentition were examined. The conventional treatment approach used at the University of Giessen (removable and multibracket appliance) was used in 98 subjects (75
Class II Division 1 and 23 Class II Division 2). The Herbst approach (Herbst
appliance followed by a multibracket appliance) was used in 44 subjects (30
Class II Division 1 and 14 Class II Division 2). Pre- and posttreatment dental
casts were evaluated using the PAR Index. Active treatment duration was
recorded. Subjects treated with the Herbst approach had a shorter treatment duration (Class II Division 1 = 21.0 months, Class 11:2 = 30.4 months)
than those treated with the Conventional approach (Class II Division 1 = 32.1
months, Class 11:2 = 38.3 months). The PAR Score reduction (= improvement) was larger in subjects treated with the Herbst approach (Class II
Division 1 = 76%, Class 11:2 = 76%) than in subjects treated with the
Conventional approach (Class II Division 1 = 68%, Class II Division 2 = 65%).
It was concluded that both treatment of Class II Division 1 and Class II
Division 2 malocclusions was more efficient using the Herbst approach than
using the conventional approach. (Semin Orthod 2003;9:87-92.) Copyright
20032003, Elsevier Science (USA). All rights reserved.
ecause of constraints in the public health
care system, the assessment of t r e a t m e n t
success is of increasing importance. In various
studies assessing orthodontic t r e a t m e n t outcome, the influence of patient-related factors
(age, sex, cooperation), l ~6 the qualification of
the operator, l,:<~,v',~7 and the m e t h o d of therapy3,7,S,ll,~U,15 m have been examined.
Many indices have b e e n developed to assess
orthodontic t r e a t m e n t outcome. ~,2° 2~ O f these,
B
From the Department of Orthodontics, (k*ivet:~ily q[ Giessen,
Giessen, Germany
Addre,~ co~responde~tce to Hans Par~che~z, I)DS; OdontDr; Department of Orthodonti(~, University of (;iesse~, Schlangenzahl 14,
1)-35392 Giessen, German)~.
Copyright 2003, Elsevier Science (USA). All rights reserved.
1073-8746/03/0901-0001 $35.00/0
doi: 10.1053/sodo. 2003. 34028
the Peer Assessment Rating (PAR Index)2.~,,~ has
b e c o m e increasingly popular. It is an objective
method, and its reliability and validity have been
certified in m a n y studies.~.l:<17.9>:~4
At the o r t h o d o d o n t i c d e p a r t m e n t in Giessen,
the 2 most c o m m o n t r e a t m e n t a p p r o a c h e s for
Class II malocclusions are the conventional approach and the Herbst approach.
Conventional Approach
In Class II Division 1 subjects treated during
pubertal growth and in the late mixed dentition,
usually an activator is used for m a n d i b u l a r advancement, often p r e c e d e d by a removable plate
for expansion of the u p p e r jaw. Once the patient
is in the p e r m a n e n t dentition, m u h i b r a c k e t appliances in both jaws, often c o m b i n e d with Class
ii elastics, are used for final adjustments.
,Seminars in O~¢hodontics, l))l R No 1 (March), 2003: pp 87-92
87
88
yon Bremen and Pancherz
In Class II Division 2 subjects treated during
pubertal growth and in the late m i x e d dentition
the u p p e r incisors are first proclined using a
removable plate in the u p p e r jaw, thus converting the Class II Division 2 into a Class II Division
1. Thereafter, m a n d i b u l a r a d v a n c e m e n t is perf o r m e d by the use of an activator. Once the
patient is in the p e r m a n e n t dentition, multibracket appliances in b o t h jaws, often c o m b i n e d
with Class II elastics, are used for final adjustments.
Herbst Approach
In Class II Division 1 subjects treated after
pubertal growth and in the p e r m a n e n t dentition, the m e t h o d of j u m p i n g the bite with the
H e r b s t appliance is the a p p r o a c h of choice.
O n c e the Class II occlusion has b e e n corrected,
the H e r b s t appliance is removed, and a multibracket appliance in the u p p e r and lower jaw is
used for final adjustments.
In Class II Division 2 subjects treated after
pubertal growth and in the p e r m a n e n t dentition, the Herbst appliance is also the c o m m o n
a p p r o a c h to correct the Class II malocclusion.
However, to be able to p e r f o r m m a n d i b u l a r advancement, the u p p e r incisors have to be proclined first with a maxillary multibracket appliance. O n c e the Class II occlusion has b e e n
corrected, the H e r b s t appliance is removed, and
a multibracket appliance in the u p p e r and lower
.jaw is used for final adjusunents.
T h e p u r p o s e of this study was to assess the
efficiency of Class II Division 1 and Class II
Division 2 t r e a t m e n t c o m p a r i n g the H e r b s t and
conventional approaches. T r e a t m e n t efficiency
was defined as a shorter t r e a t m e n t duration with
a better outcome. T h e t r e a t m e n t o u t c o m e was
assessed using the PAR I n d e x 2 5,2~
Subjects
All patients with a Class II Division 1 or Class II
Division 2 malocclusion aged 10 to 15 years
whose t r e a t m e n t was c o m p l e t e d between 1990
and 1997 at the orthodontic d e p a r t m e n t of the
University of Giessen were screened. Only those
subjects (n = 142) fulfilling the following req u i r e m e n t s as d e t e r m i n e d f r o m p r e t r e a t m e n t
dental casts were selected for this study:
1. T r e a t m e n t in the late mixed or p e r m a n e n t
dentition.
2. Unilateral or bilateral distal m o l a r relationship >1/~ cusp width when the deciduous
lower second molars still were present.
3. Unilateral or bilateral distal molar relationship ->l/e cusp width when the second premolars had erupted.
With respect to the t r e a t m e n t m e t h o d the
patients were divided into 2 groups: (1) Herbst
a p p r o a c h (n = 44) and (2) conventional approach (n - 98).
Within each of these groups the patients were
subdivided according to their malocclusion:
Herbst approach: Class II Division 1 (n = 30)
and Class II Division 2 (n = 14) and conventional approach: Class II Division 1 (n = 75) and
Class II Division 2 (n = 23).
Methods
T h e duration of active t r e a t m e n t (before retention) was recorded. Pre- and p o s t t r e a t m e n t dental casts were evaluated by using the PAR Index.
Posttreatment means after retention and full
eruption of all p e r m a n e n t teeth, with or without
third molars, were calculated.
In the PAR Index, 95,~6 the deviation f r o m a
normal occlusion and alignment is assessed by
using 5 dental c o m p o n e n t s which are weighted
differently. T h e weighted scores of the components are s u m m e d to obtain a total score (PAR
Index), expressing the severity of the malocclusion. T h e 5 c o m p o n e n t s are anterior alignment
(weighted × 1), buccal occlusion (weighted ×
1), overjet (weighted × 6), overbite (weighted ×
2), and midline discrepancy (weighted × 4). A
total score of 0 means a perfect occlusion and
alignment. The higher the score, the greater the
deviation f r o m normal. To assess t r e a t m e n t success the p o s t t r e a t m e n t score is c o m p a r e d with
the p r e t r e a t m e n t score and the reduction in
PAR score (improvement) is expressed in percent a n d / o r in points. All registrations are perf o r m e d with the PAR ruler, a plastic ruler designed especially for this index. In this study, all
m e a s u r e m e n t s were m a d e twice, and the m e a n
value was used for the final evaluation. All registrations were p e r f o r m e d by one of the authors
(JB) calibrated for the use of this index.
89
(;lass H Diwlsion 1 and 2
Statistical Methods
months
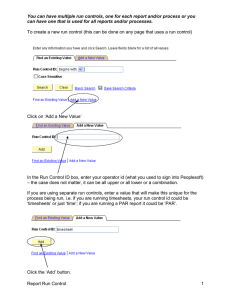
Because the variables showed an asymmetric
distribution, n o n p a r a m e t r i c Kruskal-Wallis H
tests and Hodges L e h m a n n estimates were applied for the statistical analysis. T h e significance
levels used were P < .001, P < .01, and P < .05.
P -> .05 was considered nonsignificant. The
results were expressed by box plot diagrams
(Fig 1).
80
60 ¸
40
20 ¸
Results
Treatment Duration
Class II Division 1 patients had a shorter treatm e n t duration than Class II Division 2 patients
(P < .001) F u r t h e r m o r e , patients treated with
the Herbst a p p r o a c h had a shorter (P < .001)
t r e a t m e n t duration (Class II Division 1, 21.0
months; Class II Division 2, 30.4 months) than
those treated with the conventional a p p r o a c h
(Class II Division 1, 32.1 months; Class II Division 2, 38.3 months) (Fig 2).
PAR Index
T h e p r e t r e a t m e n t PAR score in subjects
treated with the Herbst a p p r o a c h (27.0) and
•
T
maximum value ( • )
95 th percentile
75 th percentile
mean (e)
Herbst
Conventional
Class I1:1
Herbst
Conventional
Class Ih2
Figure 2. Treatment duration (months) in 105 Class
II DMsion 1 and 37 Class II Division 2 patients in
relation to the treatment approach. Herbst approach:
Class II Division 1 (n = 30), Class II Division 2 (11=
14); conventional approach: Class I1 Division 1 (11=
75), Class II Division 2 (n = 23).
snbjects treated with the conventional a p p r o a c h
(26.7) was nearly the same. After treatment, subjects treated with the Herbst a p p r o a c h had a
lower (P < .01) PAR score (5.7) than those
treated with the conventional a p p r o a c h (8.2)
(Fig 3).
PAR Score Reduction in Points
Class II Division 1 patients had a higher PAR
score reduction (P < .001) in points than Class
II Division 2 patients. F u r t h e r m o r e , subjects
treated with the Herbst a p p r o a c h had a higher
PAR Score reduction (P < .01) in points (Class
II Division 1, 24.6; Class II Division 2, 13.7) than
subjects treated with the conventional a p p r o a c h
(Class II Division 1, 20.2; Class II Division 2,
13.5) (Fig 4).
50 th percentile
PAR Score Reduction in Percent
25 th percentile
5 th percentile
•
minimum value ( • )
Figure 1. Explanation of the box plot diagram.
Class II DMsion 1 patients had about the
same PAR score reduction as Class II Division 2
patients. Subjects treated with the Herbst approach had a higher PAR score reduction (P <
.001) in percentage (Class II Division 1, 75.9;
Class II Division 2, 76.4) than subjects treated
with the conventional a p p r o a c h (Class II Division 1, 68.1; Class II Division 2, 65.3) (Fig 5).
90
yon Bremen and Panchevz
%
PAR Score
120 60
100 £
50
8040
60-
30-
4o~
20.
20-
ol
10-
¢
0
-20 ~
,
before
after
before
,
Herbst
Herbst
Conventional
Figure 3. PAR score before and after treatment in
105 Class II Division 1 and 37 Class II Division 2
patients in relation to the treatment approach. Herbst
approach: Class II Division I (n = 30), Class II Division 2 (n = 14); conventional approach: Class II
Division 1 (n = 75), Class II Division 2 (n = 23).
Discussion
I n i n t e r p r e t i n g t h e p r e s e n t findings, it m u s t b e
k e p t in m i n d t h a t all p a t i e n t s w e r e t r e a t e d by
orthodontic postgraduate students. However,
t h e t r e a t m e n t o f t h e p a t i e n t s was s u p e r v i s e d by
points
50-
40-
30-
20-
q
10-
0I
Herbst
I
Conventional
Class Ihl
]'
,
after
1
1
Herbst
Conventional
Class Ih2
Figure 4. PAR score reduction (points) in 105 Class II
Division 1 and 37 Class II Division 2 patients in relation to the treatment approach. Herbst approach:
Class II Division 1 (n = 30), Class lI Division 2 (n =
14); conventional approach: Class II Division 1 (n =
75), Class II Division 2 (n - 23).
Conventional
Class Iht
Herbst
Conventional
Class 11:2
Figure 5. PAR Score reduction (%) in 105 Class II
Division 1 and 37 Class II Division 2 patients in relation to the treatment approach. Herbst approach:
Class II Division 1 (n = 30), Class II Division 2 (n =
14); conventional approach: Class II Division 1 (n =
75), Class II Division 2 (n = 23).
t h e s a m e t e a m o f i n s t r u c t o r s , thus e n s u r i n g unif o r m i t y in t h e r a p e u t i c a l a p p r o a c h e s .
Treatment Duration
T h e d u r a t i o n o f active t r e a t m e n t f o r all 142
p a t i e n t s r a n g e d b e t w e e n 8 a n d 71 m o n t h s , with
a m e d i a n o f 30.6 m o n t h s . U s i n g exclusively f i x e d
a p p l i a n c e s , a s i m i l a r t r e a t m e n t d u r a t i o n (4-91
m o n t h s ) was r e p o r t e d by Vig et al TM with a m e a n
o f 31 m o n t h s . A s h o r t e r m e a n d u r a t i o n was des c r i b e d by A l g e r Is with 22 m o n t h s a n d F i n k a n d
S m i t h y with 23 m o n t h s . T h e p r e s e n t study, however, s h o w e d t h a t t r e a t m e n t t i m e was s h o r t e r
w h e n u s i n g t h e H e r b s t a p p r o a c h (Class II Division 1, 21 m o n t h s ; Class II Division 2, 30
m o n t h s ) t h a n w h e n u s i n g t h e c o n v e n t i o n a l app r o a c h (Class II Division 1, 32 m o n t h s ; Class II,
Division 2, 38 m o n t h s . ) In b o t h t r e a t m e n t app r o a c h g r o u p s , Class II Division 2 p a t i e n t s g e n erally h a d a l o n g e r t r e a t m e n t d u r a t i o n t h a n
Class II Division 1 p a t i e n t s , p r o b a b l y b e c a u s e a
Class II Division 2 h a d to b e c o n v e r t e d into a
Class II Division 1, b e f o r e m a n d i b u l a r a d v a n c e ment could be performed.
PAR Index
T h e a v e r a g e ( m e d i a n ) p r e t r e a t m e n t PAR
s c o r e o f all 142 p a t i e n t s was 26.8 points. S i m i l a r
Class II DivMon 1 and 2
scores (27-31 points) were f o u n d by Turbill et
al -~2,34 w h e n assessing the o r t h o d o n t i c s t a n d a r d
o f the G e n e r a l Dental Services in E n g l a n d a n d
O ' B r i e n et al v' a n d H a m d a n a n d Rock :~' w h e n
e x a m i n i n g patients treated in dental schools.
Lower scores (16-25 points) were f o u n d by Pangrazio-Kulbersh et al p-~a n d Firestone et al. s Pangrazio-Kulbersh et al 1:~ e x a m i n e d 103 consecutively treated cases (average p r e t r e a t m e n t age,
9.8 years), a n d Firestone et al s patients treated at
a dental school. T h e majority were treated with
fixed appliances. T h e low p r e t r e a t m e n t PAR
Score o f Pangrazio-Kulbersh et al ~ m i g h t be
explained by the y o u n g patient material a n d the
fact that d e c i d u o u s teeth are n o t evaluated in
the PAR Index.
After treatment, the average ( m e d i a n ) PAR
score o f all 142 patients was 7.3 points. This
score is in a c c o r d a n c e with that (5-12 points) o f
o t h e r studies. ~,2~'.2~;,-~2,:~4 R i c h m o n d et al 2:~,~ rem a r k e d that a final PAR score below 10 is an
acceptable result a n d scores u n d e r 5 are close to
a perfect occlusion a n d alignment. T h a t m e a n s
that, o n average, an acceptable result was
r e a c h e d in the p r e s e n t patient material.
F u r t h e r m o r e , R i c h m o n d et al ~',2~i p o i n t e d o u t
that a high t r e a t m e n t s t a n d a r d is characterized
by a PAR score r e d u c t i o n o f at least 70%. A high
PAR score r e d u c t i o n is, o f course, r e a c h e d easier
in subjects with a high p r e t r e a t m e n t PAR I n d e x
than in subjects with a low p r e t r e a t m e n t index.
This means, the worse the p r e t r e a t m e n t malocclusion, the greater the possible i m p r o v e m e n t
t h r o u g h treatment. This is in a g r e e m e n t with
Taylor et al, 1~' w h o also f o u n d that a high pret r e a t m e n t PAR Score h a d a positive effect w h e n
assessing the quality o f o r t h o d o n t i c therapy.
Similar results were f o u n d by Kerr et al I~ a n d AI
Yami et al. 2
PAR Score Reduction in Relation to the
Treatment Approach
Patients treated with the H e r b s t a p p r o a c h
had a g r e a t e r PAR score r e d u c t i o n in points a n d
in p e r c e n t than patients treated with the conventional a p p r o a c h . O t h e r a u t h o r s ~',~'.~7 also rep o r t e d a b o u t a correlation b e t w e e n t r e a t m e n t
m e t h o d a n d o u t c o m e . T h e y f o u n d that fixed
appliances in b o t h arches h a d the greatest effect
in i m p r o v i n g a malocclusion. However, n e i t h e r
Pangrazio-Kulbersh et al 1:~ n o r A h l g r e n ~ f o u n d
91
any association between the appliances used a n d
the t r e a t m e n t success.
In the p r e s e n t study Class II Division 1 subjects achieved a greater PAR score r e d u c t i o n in
points than Class II Division 2 subjects. This can
be explained by a h i g h e r p r e t r e a t m e n t PAR
score in Class II Division 1 subjects because o f
the great overjet (weighted × 6). However, the
PAR score r e d u c t i o n in % was a b o u t the same in
Class II Division 1 a n d Class Ii Division 2 subjects. T h a t means, that in relation to the severity
o f the p r e t r e a t m e n t malocclusion, the a m o u n t
o f i m p r o v e m e n t was a b o u t the same in b o t h
malocclusion groups.
Conclusion
Both with respect to t r e a t m e n t d u r a t i o n a n d to
t r e a t m e n t o u t c o m e , Class II Division 1 a n d Class
II Division 2 t r e a t m e n t was m o r e efficient with
the H e r b s t a p p r o a c h than with the conventional
approach.
References
1. Ahlgren .J. A ten-year evaluation of tile quality of orthodontic treatment. Swed D c n t J 1993;17:201-2(19.
2. AI Yami E, KuijpersJagtmann A, V a n ' t H o t M. Occlusal
o u t c o m e o f o r t h o d o n t i c treatment. Angle O r t h o d 1998:
68:439-444.
3. Beckwith FR, A c k e r m a n n R, Cobb C, Tira D. An evahlation ot factors atti'cting duration of orthodontic treatmere. Am J O r t h o d Dentotac O r t h o p 1999:115:439-447.
4. Berg R. Die Bewermng wm kieterorthopfidischen Behandhmgs-ergebnissen, lntorm O r t h o d u n d Kiel(worthop 1990;22:483-487.
5. Birkeland K, Boe O, Wisth P. Evaluation of treatment
a n d post-treatment changes hv the PAR Index. Eur
,1 O r t h o d 1997;19:279-288.
~. Dver G, Harris EF, VadenJ1,. Age etl~ects on orthodontic
lreatmenl: adolescents contrasted with aduhs. Am ,l
Orthlld l)entofac O r t h o p 1991 ; 1(t0:523-530,
7. Fmk DF, Smith R:J. T h e duratilln of orthodontic treab
ment. Am,l O r t h o d Dentol:ac O r t h o p 1992:102:45-51.
8. Firestone A, H/islet R, lngervall B. T r e a t m e n t results in
denial s(hool orthodontic patients in 1983 and 1993.
Angle O r t h o d 1999;69:19-26.
9. Fox N. T h e lirst 109 cases: a personal audit o f o u h o d o n tic treatnlCnt assessed by the PAR (peel- assessment rating) Index. Bri! D c n t J 1993; 174:290-297.
10. (;ianelly AA. One-phase versus two-phase treatment.
Am,] O r t h o d Denmiac O r t h o p 1995;108:556-559.
11. Kerr S,,]ohn W, B u c h a n a n IB, et al. Factors influencing
the outconle and duration of removable appliance treatment. Eur,] O r t h o d 1994;16:181-186.
12. O'Brien K, Shaw WC, Roberts CT. T h e use tlf occlusal
indices in assessing the provisilm ot orthodontic treat-
99
von Bremen and Pancherz
ment by the Hospital Orthodontic Service of England
and Wales. BritJ Orthod 1993;20:25-35.
13. Pangrazio-Kulbersh V, Kaczynski R, Shunock M. Early
treatment outcome assessed by the Peer Assessment Rating Index. AmJ Orthod Dentofac Orthop 1999;115:544550.
14. Shia GJ. Treatment overruns.J Clin Orthod 1986;20:602604.
15. Taylor PJS, Kerr WJS, McCollJH. Factors Associated with
the Standard and Duration of Orthodontic Treatment.
BritJ Orthod 1996;23:335-341.
16. Vig PS, Weintraub JA, Brown C, et al. The duration of
orthodontic treatment with and without extractions: A
pilot study of five selected practices. AmJ Orthod Dentofac Orthop 1990;97:45-51.
17. Richmond S, Shaw WC, Stephens CD, et al. Orthodontics in the General Dental Service of England and Wales:
A critical assessment of standards. Brit DentJ 1993;174:
315-329.
18. Alger DW. Appointment frequency versus treatment
time. Am J Orthod Dentofac Orthop 1988;94:436-439.
19. Vaden JL, Kidser HE. Straight talk about extraction ans
nonextraction: A differential diagnostic decision. Am J
Orthod Dentofac Orthop 1996;109:445-452.
20. Eismann D. A Method of Evaluating the Efficiency of
Orthodontic Treatment. Trans Eur Orthod Soc 1974:
223-232.
21. Gottlieb E. Grading your orthodontic treatment restdts.
J Clin Orthod 1975;9:155-161.
22. Berg R. Post-retention analysis of treatment problems
and tailures in 264 consecutively treated cases. Eur
J Orthod 1979;1:55-68.
23. Berg R, Fredlund A. Evaluation of orthodontic treatment results. EurJ Orthod 1981;3:181-185.
24. Ahlgren J. Tio~rig utv/irdering av ortodontiska behandlingsresultat. Tandl~ikartidningen 1988;80:206-216.
25. Richmond S, Shaw WC, O'Brien KD, et al. The develop-
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
ment of the PAR Index (Peer Assessment Rating): reliability and validity. EurJ Orthod 1992;14:125-139.
Richmond S, Shaw WC, Roberts CT, et al. The PAR
Index (Peer Assessment Rating): methods to determine
outcome of orthodontic treatment in terms of improvement and standards. EurJ Orthod 1992;14:180-187.
Buchanan IB, Shaw WC, Richmond S, et al. A comparison of the reliability and validity of the PAR Index and
Summers' Occlusal Index. EurJ Orthod 1993;15:27-31.
Buchanan IB, Russell JI, Clark JD. Practical application
of the PAR Index: An illustrative comparison of the
outcome of treatment using two fixed appliance techniques. BritJ Orthod 1996;23:351-357.
De Guzman L, Bahiraei D, Vig KWL, et al. The validation
of the Peer Assessment Rating index for malocclusion
severity and treatment difficulty.. AmJ Orthod Dentofac
Orthop 1995;107:172-176.
Fellner U, Schl6mer R. Der PAR-Index--Eine praktikable Metbode der Qualit/itssicherung. Kieferorthop
1996; 10:193-200.
Richmond S, O'Brieu K, Buchanan I, et al. An Introduction to Occlusal Indices. Manchester, Victoria University
of Manchester, 1994.
Turbill E, Richmond S, Wright JL. Assessment of General Dental Set~'ices Orthodontic Standards: the Dental
Practice Board's Gradings Compared to PAR and IOTN.
Brit J Orthod 1996;23:211-220.
Turbill E, Richmond S, Andrews M. A Preliminary Comparison of the DPB's Grading of Completed Orthodontic Cases with the PAR Index. BritJ Orthod 1994;21:279285.
Turbill E, Richmond S, WrightJL. A critical assessment
of orthodontic standards in England and Wales (19901991) in relation to changes in prior approval. Brit
J Orthod 1996;23:221-228.
Hamdan AM, Rock WP. An Appraisal of the Peer Assessment Rating (PAR) Index and a suggested new weighting system. EurJ Orthod 1999;21:181-192.