Recognizing the Signs and Symptoms of Dementia in Older Adults
advertisement

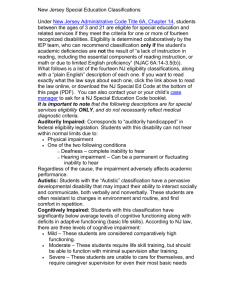
PCA Regional Conference on Aging 2014 Recognizing the Signs and Symptoms of Dementia in Older Adults Joel E. Streim, M.D. Professor of Psychiatry University of Pennsylvania Philadelphia VA Medical Center Disclosures Dr. Streim is on the faculty of the Geriatric Education Center of Greater Philadelphia, which is funded by the Bureau of Health Professions, Health Resources and Services Administration (HRSA), Dept. of Health and Human Services (DHHS). The content of this presentation is solely the responsibility of the presenters and does not necessarily represent the official views or policies of HRSA or the DHHS. Objectives Identify at least 3 signs or symptoms of cognitive impairment in the early, middle and late stages of dementia; Identify at lesat 3 cognitive domains other than memory that may be impaired in older adults with dementia; Understand the potential effects of impairment in various cognitive domains on behavior and everyday function in older adults with dementia; Appreciate the resources needed to care for older adults with behavioral changes, disability and activity limitation. What cognitive changes do we see in persons with dementia? Deficits in one or more cognitive domains: —learning and memory (amnesia) —language (aphasia) —perceptual-motor • visual recognition (agnosia) • performing motor activities (apraxia) —executive function (abulia, apathy) —complex attention (distractability) —social cognition (lack of insight) Consequences of Cognitive Impairment Cognitive impairment can interfere with Communication — Comprehension — Ability to report symptoms, express needs Social awareness, self-monitoring Ability to follow directions Self-care (basic ADLs) Household management (instrumental ADLs) Impairment in Activities of Daily Living (ADLs) Instrumental ADLs (Household Management) Basic ADLs (Personal Care) — Shopping — Bathing — Cooking — Hygiene — Cleaning — Grooming — Laundering — Dressing — Using Telephone — Feeding — Paying Bills — Toileting Other Consequences Cognitive impairment can interfere with Personal safety — Eating (e.g. risk of choking or aspiration) — Walking (e.g. risk of getting lost, falling) — Household tasks (e.g. risk of fires, accidents) Receipt of medical and nursing care — Patient participation — Delivery of care by providers & caregivers Recognition of Cognitive Impairment Suspect a neurocognitive disorder when person has self-care deficits person has difficulty following instructions family has “taken over” responsibilities person doesn’t participate well in medical, nursing care, or rehabilitative care behaviors interfere with safety or care delivery Don’t blame “old age” What are the signs and symptoms of cognitive impairment ? SIGNS are what we observe in these individuals — Objective SYMPTOMS are what the individual experiences — Subjective Impaired Memory and Learning (amnesia) Forgetfulness — Repetitious statements — Misplacing things — Missing appointments — Leaving bills unpaid — Inability to recall recent events Disorientation — Getting lost Impaired Language (aphasia) Trouble comprehending spoken or written language — Inability to follow simple directions Word-finding difficulty — Hesitant speech — Paraphasias (word substitutions) — Anomia (loss of name recall); substitutes general terms and pronouns — Circumlocutions (“talking around”) — Neologisms (non-sense words or sounds) Perseveration (repetitious speech, echolalia, palilalia) Impaired Perceptual-Motor Function Agnosia — Inability to recognize faces, family members — Trouble navigating in familiar environs Apraxia — Difficulty manipulating objects (e.g., opening package, unscrewing lid, buttoning, using zipper) — Inability to assemble objects, perform spatial tasks (e.g., sewing, carpentry, dressing) Impaired Complex Attention Distracted by multiple stimuli Can’t scan and focus on relevant stimuli or objects in environment Can’t register information just given Thinking and processing speed is slower Can’t perform mental calculations Impaired Executive Function Loss of frontal lobe function: Lack of will or initiative (abulia, apathy) Difficulty with reasoning and decisions Inability to organize and plan activities Inability to perform sequential tasks Poor task completion Inability to shift between concepts / tasks Impaired social cognition Loss of insight — Lack of awareness of own situation — Inability to appreciate safety concerns Insensitivity to other persons’ mental state — Inability to recognize social cues or read facial expressions Disinhibition Impaired judgment Common Presentations: Early and Middle Stages of Dementia Visual complaints Trouble following directions Difficulty performing familiar tasks Family members take over usual roles Loss of initiative — Disengagement from usual activities — Self-neglect — Weight loss Diminished social spontaneity — Less conversation Common Psychological Changes: Early and Middle Stages of Dementia Depression — Apathy, withdrawal — Sad or flat affect Anxiety — Fear of being alone Paranoia — Delusions about “imposters” — Accusations of infidelity, theft Personality changes Loss of Cognition and Function in Late-Stage Dementia Aphasia: single words, echolalia, palilalia, mutism Apraxia: —Manual: inability to hold or manipulate objects —Oral: difficulty chewing & swallowing —Gait: instability, loss of ambulatory ability Incontinent of bladder and bowel Terminal stages: inability to sit up, smile, hold up head; bedbound Total dependence in basic ADLs How does memory impairment lead to inability to perform basic ADLs? Example Patient is able to dress himself, but can’t remember where his clothes are kept Walks outside naked How does apraxia lead to difficulty with basic ADLs? Example Patient is continent of bladder, but cannot unzip or unbutton to pull down her pants Wets her clothing How does language impairment (aphasia) interfere with care? Example Patient who can’t verbally communicate that pills are hard to swallow Spits medication at caregiver How does visual agnosia lead to changes in behavior and function? Example Patient can maneuver to pull down his pants, but can’t recognize that a toilet is a receptacle for urination Urinates on living room floor Common Caregiver Misattributions Laziness Dependency Belligerence Depression Misattributions can lead to caregiver distress (frustration, anger, anxiety, depression) and increased risk of elder abuse Initial approach to assessment, management, and prevention Recognize areas of impaired cognitive function and areas of preserved cognitive function Help compensate for impairment Support residual abilities What other factors interact with cognitive deficits, contributing to behavioral changes and functional decline in patients with dementia? Factors that Affect Function and Behavior in the Cognitively Impaired Cognitive deficits reduce a person’s ability to deal with: Unmet needs (e.g., physical or psychological) Environmental or social irritants Acute or chronic illness (medical, psychiatric) Distressing symptoms (e.g., pain, anxiety) Adverse effects of medications Many of these aggravating factors are modifiable or treatable Unmet needs that can lead to functional and behavioral changes Physical needs — Nutrition, hydration, toileting, exercise, rest Psychological needs —Security, autonomy, affection, self-worth Environmental irritants that can lead to functional and behavioral changes Physical — Noise — Confusing visual stimuli — Uncomfortable temperature — Unfamiliar surroundings Social — Changes in routines — Provocative social interactions Adverse drug effects that can cause functional and behavioral changes Nuisance symptoms Anticholinergic effects Antihistaminic effects Paradoxical excitation / disinhibition Intoxication or withdrawal states Akathisia Medical conditions and somatic discomfort can alter function and behavior Medical condition Somatic discomfort — Arthritis — Pain — Dehydration — Constipation — Prostatic hypertrophy — Urinary urgency — COPD — Shortness of breath — Cerebrovascular disease — Dizziness — CHF — Fatigue Psychiatric conditions can cause functional and behavioral problems Depression Delirium Psychosis — delusions — hallucinations Anxiety Sleep disturbance What do we need to learn as caregivers? Understand how the cognitively impaired person experiences situations (the environment, social interactions) Recognize specific factors that cause or contribute to behavioral changes and functional deficits Once understood, interventions and management strategies become apparent Person-centered Care: WHAT? Focus on the elderly person’s experience — Try to imagine being in their world — Consider how things look from their perspective Accept their reality — Their subjective experience is real to them — Doesn’t mean you actually adopt their point of view for yourself Person-centered Care: HOW? Look for meaning in verbal and non-verbal communication — Ask, “what do you want? “how can I help?” — When language comprehension and communication are severely impaired, LOOK AND LISTEN for non-verbal clues to sources of distress or unmet needs Avoid saying “no”, arguing or disagreeing Offer to help in ways that reduce distress or meet needs, without compromising safety QUESTIONS CLINICAL VIGNETTES SIGNS OF IMPAIRMENT IN VARIOUS COGNITIVE DOMAINS Vignette #1 A woman has a doctor’s appointment tomorrow. Her husband tells her it’s on Wed at 9am. 10 minutes later, she asks when she’s going to the doctor’s office. Husband repeats the information. 2 minutes later, she asks the same question. This is repeated more than 15 times in the course of the afternoon. Vignette #2 A man tells his son that his neighbors stole his socks. When his son opens his dresser drawer and shows him the socks, he seems surprised, and states that the neighbors must have come in the middle of the night to return them. Vignette #3 A woman who used to be very social and talkative now speaks only when someone asks her a question, and she usually responds with a single word answer. Sometimes she only nods her head. The caregiver thinks she may be depressed. Vignette #4 A man refers to his belt as “my strap.” When pointing to his watch, he calls it “that thig-a-ma-jig.” Vignette #5 A man has urinary incontinence. His adult daughter, who is his caregiver, notes that prior to episode of incontinence, rather than asking to go to the bathroom, he becomes increasingly agitated, begins pacing, and seems upset. Vignette #6 A man asks his wife of more than 50 years who sent her to his house. When she says she’s his wife, he insists that she doesn’t look anything like his wife. However, when she begins to sing their favorite song, he begins to cry, and asks her how she knows that. Vignette #7 A man who has been very active and always enjoyed hikes in the woods, has been spending more time sitting in a chair over that past 3 months, and now seldom gets up. When he stands, he doesn’t fully extend his knees, and needs coaxing to take a step. He appears fearful, even when his caregiver offers support under his arm. Vignette #8 A woman who was always fastidious and well-mannered at the dinner table has stopped using and knife and fork to cut her food. Vignette #9 A man who loves to eat keeps chewing and chewing without swallowing, and pieces of food sometimes fall from his mouth. Vignette #10 A woman who is continent of urine most of the time, today is wearing pants that button on the side, gets to the bathroom and wets herself before she can pull down her pants. Vignette #11 A man tries to use a butcher knife to open a cardboard milk container. Vignette #12 A woman always baked Christmas cookies every year to bring to her grandchildren. This year she doesn’t. Her daughter observed that on one occasion she added whole egg yolks to a batter without beating them, after first assembling all the other ingredients. Vignette #13 A man used to be very social, and the person at home who always initiated dinner conversations. Now he spends most of the day sitting on the couch. Family is concerned that he is depressed or lacking motivation. Vignette #14 A man writes a check for his electric bill with the correct payee and amount, signs and dates the check, places it in the envelope, and seals the envelope without including the payment stub with the address showing through the envelope window. He then deposits it in a mailbox. Vignette #15 A usually well-mannered elderly man is walking down the sidewalk accompanied by his wife of 60 years. The couple passes a young girl walking the other way, and the man asks her if she wants to have sex with him. His wife is horrified and embarrassed. Vignette #16 A woman sends her husband to buy a quart of milk and a box of tea bags at the local grocery store, 3 blocks away from their house. He returns two hours later without any groceries. Vignette #17 A woman has been living independently for 8 years since her husband died. A daughter from California, who hasn’t seen her in the past six months, is now in town for a visit and notices that her mother has lost so much weight that her clothes are sagging on her. The refrigerator is full of spoiled dairy products and moldy fruit. DISCUSSION: SHARE YOUR CASES THANK YOU !