LAB #16
advertisement

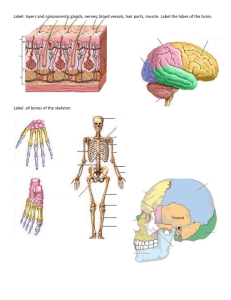
Biology 241 – Lab LAB #16 (16th/21 Lab Sessions for Fall Quarter, 2008) TOPICS TO BE COVERED: »Demonstration/Dissection/Identification of certain Non-Muscular Structures »Introduction to the Nervous System components »Introduction to Cranial Nerves DESIRED OUTCOMES: After completing the activities described for this lab session, students should: »Be able to identify the required non-muscular structures: Tendinous inscriptions Lymph Node(s) Transverse carpal ligament Sciatic Nerve Patellar tendon Calcaneal tendon Thyroid gland Transverse Jugular Vein Parotid salivary gland Parotid gland duct Submaxillary salivary gland MATERIALS NEEDED: »Gloves »Safety Glasses (or your own glasses) »Dissection Trays (large, flat pans) »Preserved cats »Dissection Tools (large forceps, scissors, blunt probes, dissection needles, scalpels) »Photographic Atlas, Ch. 8, 9, 13, 15 »Cat Atlas Activity #1: Demonstration/Dissection/Identification of certain Non-Muscular Structures Up to this point, you have learned most of the bony landmarks on bones of the skeleton and most of the superficial muscles of both the human and the cat, along with several of the deep muscles. Along the way, there have been several structures that have been encountered about which you should be conversant. These are: Tendinous inscriptions: Regarding the rectus abdominis muscles, these are vertically oriented and lie one to either side of the midline. Their vertical fibers are interrupted along their course by three transverse fibrous bands called tendinous inscriptions, believed to be remnants of the myosepta that separated muscle segments, or myotimes, during embryological development. These result in making the rectus abdominis muscles stronger by virtue of allowing for four times the potential shortening in length of the muscle compared to if the muscle did NOT include these “interruptions”. (Also, since the rectus abdominis is 3 times as wide cranially, where fleshy, as it is caudally, where tendinous, these tendinous inscriptions are longer up near the rib cage.) These structures are absent on the cat. Lymph nodes: Lymph nodes (sometimes called “lymph glands”), are small, oval or bean-shaped collections of lymphatic tissue interposed in the course of lymphatic vessels and macroscopically visible along the routes of all blood vessels. They are especially aggregated in large collections in the following regions: cervical, axillary, inguinal, popliteal, intestinal and bronchomediastinal. The tissue of each node is enclosed in a strong fibroelastic capsule from which septa, or trabeculae, push into the substance of the node to partially subdivide it into a number of compartments. There are both superficial and deep lymph nodes; the superficial ones are palpable as firm (but not hard), moveable masses. Among the palpable nodes are those in the neck region, in the axilla, and in the inguinal area. When a lymph node is enlarged, hard, and tender, it is infected (that is, it is actively fighting a local infectious process), and it is known as a “bubo”. This is how the Bubonic Plague was named: the clinical symptoms were numerous, large, swollen lymph nodes, or bubos. Biology 241 – LAB #16 – continued Page Two Transverse carpal ligament: This structure is also called the flexor retinaculum. It unites the 4 marginal carpal bones. (The carpus consists of eight bones arranged in two transverse rows of four each. The proximal row from lateral to medial side is made up of the scaphoid, lunate, triquetrum, and pisiform bones; those of the distal row, in the same order, are called the trapezium, trapezoid, capitates, and hamate bones. The four marginal bones are the scaphoid and pisiform and the trapezium and hamate.) Remember, the carpal bones are small and irregular in shape. Their names are more or less suggestive of their appearance. The smallest is the pisiform which rests on the front of the triquetrum, rather than at its side, and can be easily palpated when the wrist is flexed. The bones are closely fitted together and bound by ligaments but they do have synovial cavities and some movement is allowed between them. The greatest movement, however, is between the proximal an distal rows, at the transverse intercarpal, or midcarpal, joint. The rows of bones are also placed in such a manner as to form a transverse arch with its concavity anterior. In life, this concavity is bridged by a ligament, the flexor retinaculum (transverse carpal ligament), under which pass the numerous flexor tendons to the wrist and fingers. See Figure 8.36 of the Photographic Atlas. (Owing to the irregularity of carpal bones, fractures and other injuries are serious and often may not be restored to 100 percent function.) Sciatic Nerve: The sacral plexus of nerves is formed by ventral rami of L4, L5, S1, S2, S3 and S4 uniting to form a large, flattened band, most of which continues into the thigh as the sciatic nerve. The sciatic nerve is the largest nerve in the body, supplying the skin of the foot and most of the leg, the muscles of the posterior side of the thigh, and all those of the leg and foot. Its terminal branches are the tibial and common peroneal nerves. Together with the lumbar plexus of nerves (L1 – L4), these two great plexuses collectively supply the skin and muscles of the entire lower limb. You will see this large, impressive nervous structure immediately deep to the biceps femoris muscle if you cut its tendinous insertion on the lateral side of the lateral condyle of the tibia and head of the fibula and reflect the biceps femoris muscle upward. Patellar tendon: The quadriceps femoris (actually four muscles: rectus femoris, vastus lateralis, vastus medialis, vastus intermedius) is the great extensor of the leg. Its vasti components cover the anterior, lateral, and medial surfaces of the shaft of the femur, and reach posteriorly to the linea aspera. The rectus femoris lies in front of the vastus intermedius and between the vastus medialis and lateralis; but unlike them, it has a double origin – one head to the anterior inferior spine of the ilium and the other to the posterosupeiror tim of the acetabulum. These four muscles have a common tendon of insertion into the superior border of the patella, which in turn is attached to the tuberosity of the tibia by the ligamentum patellae. Actually, since the patella is a sesamoid bone, which formed in the tendon of the quadriceps femoris muscle, this muscle can be said to have originally inserted into the tibial tuberosity. In all, the structure we refer to as “the patellar tendon” is really two structures (the tendon of the quadriceps femoris muscles together with the patellar ligament) AND it includes the patella itself interposed between the two of these tendinous/ligamentous structures. (See Figures 8.45 – 8.47 and 8.51 – 8.53 of the Photographic Atlas.) The patella, bearing on the condyles of the femur, serves as a lever to improve the angle of pull of the quadriceps on the tibial tuberosity. The quadriceps tendon, by sending fibers over the capsule of the knee joint and by the tension of the muscles helps to strengthen and maintain the integrity of the knee joint. Since the rectus femoris crosses the hip joint as well as the knee joint, it is a flexor of the thigh as well as an extensor of the knee. The whole group functions in walking, running, climbing, jumping, and kicking. Calcaneal tendon: With regard to the posterior crural muscles, their primary function is to extend (plantar flex) the foot at the ankle. The gastrocnemius and soleus together form the “calf of the leg” and they insert by a common tendon, the tendo calcaneus (aka Tendon of Achilles), into the tuberosity of the calcaneus, or heel bone. These two muscles are sometimes referred to as the triceps surae. Because the origins of the gastrocnemius are just above the lateral and medial condyles on the posterior surface of the femur and the muscle crosses the knee joint, it also flexes the knee. Also know that the plantaris is a small muscle between the proximal ends of the gastrocnemius and the soleus and inserts into the calcaneus by a long, slender tendon that follows (and often fuses into) the medial side of the calcaneal tendon (tendo calcaneus.) Biology 241 – LAB #16 – continued Page Three Thyroid gland: The thyroid gland is the largest of the endocrine glands, weighing 20 – 30 grams. It lies in the neck region with one lobe on either side of the lower larynx and upper trachea. The lobes are connected anteriorly across the trachea by the isthmus. (See Figure 10.1 in the Photographic Atlas.) In about a third of all individiauls, a tall, narrow pyramidal lobe extends upward from the isthmus in front of the larynx. Transverse Jugular Vein: This vein is somewhat variable in size from specimen to specimen (cats or humans) and is considered a tributary of the external jugular vein fed by venous drainage from the superior, middle, and inferior thyroid veins. It is a short, but prominent vein that crosses the midline and seems to unite the R and L external jugular veins. Parotid salivary gland: There are three pairs of major salivary glands: the parotid, submandibular (aka: submaxillary), and sublingual. (There are also innumerable minor salivary “glands” in the lingual, labial, and buccal mucosa. These are microscopic aggregates of salivary glandular tissue; but they contribute in a very big way to the total amount of saliva that washes the oral cavity.) The parotid gland lies below and in front of the external ear and within the cervical fascia. Although the parotids (there are two of these: Right and Left) are the largest of the three major salivary glands, they produce less saliva (by volume) than do the submandibular salivary glands. The saliva produced by the parotids is considered to be nearly totally serous (watery) in nature; whereas the submandibular glands produce a mixed serous/mucous saliva, and the sublingual glands produce a nearly totally mucous saliva. Parotid gland duct: Also known as Stensen’s Duct, this large duct crosses the masseter muscle and at its anterior border, bends inward to penetrate the cheek. The open end of the duct is anchored by a mound of buccal mucosa called the parotid papilla, and the it opens at the level of the second maxillary molar tooth. Submaxillary salivary gland: The second largest of the major salivary glands; but the ones (again, these are bilateral) that produce the most saliva by volume! Each submandibular gland lies below the body of the mandible and the mylohyoid muscle. Its duct (Wharton’s duct) arises from a lobe of the land under the floor of the mouth from which it pushes upward and forward dto open on the underside of the tongue in the floor of the mouth. Activity #2: Introduction to the Nervous System Components The cranial and spinal nerves constitute in part the peripheral nervous system. As we have seen, the spinal nerves are paired and form a regular segmental sequence along the spinal cord. They have posterior, or afferent, roots and anterior, or efferent, roots. There is a sensory ganglion on the posterior root containing the cells of origin of the afferent neurons; a nucleus made up of the cells of origin of the efferent neurons is in the anterior gray column of the cord. Here is a list of the structures of the spinal cord that you should be able to identify on anatomical models and/or diagrams: (Refer also to Figures 9.4 – 9.6, 9.21, and 9.22 in the Photographic Atlas) 1. Meninges 2. Spinal gray matter 3. Spinal white matter a. Dura mater a. Anterior (ventral) horn a. Anterior column (aka funiculus) (1) Epidural space b. Lateral horn b. Lateral column (aka funiculus) (2) Subdural space c. Posterior (dorsal) horn c. Posterior column (aka funiculus) b. Arachnoid mater (1) Subarachnoid space 4. Spinal nerve roots: c. Pia mater a. Dorsal root and Dorsal Root Ganglion (1) Denticulate ligaments b. Ventral root Biology 241 – LAB #16 – continued 5. Conus medullaris 6. Filum terminale 7. Cauda equine Page Four 8. Cervical enlargement 9. Lumbar enlargement 10. Central Canal 11. Anterior median fissure 12. Posterior median sulcus Activity #3: Introduction to Cranial Nerves The cranial nerves issue from the brain (except, of course I – Olfactory which issue from the superior nasal mucosa and II – Optic which issue from the nervous tunic (retina) of each eye). From our understanding of the development of the brain and cord from a common neural tube, we have reason to expect that as the brain bears some resemblance to the cord, the cranial nerves should also bear some resemblance to the spinal nerves. This is indeed the case, but as the brain developed its special features, so did the cranial nerves become more specialized. In studying the cranial nerves, the student should be alert to the similarities and differences between these two subdivision of the peripheral nervous system. Twelve pairs of cranial nerves are commonly recognized. Most of these nerves, like the spinal nerves, have efferent and afferent roots (mixed nerves), but a few have only afferent or only efferent roots (pure nerves). The afferent, or sensory, components have their cell bodies in ganglia outside of the brain; the efferent, or motor, components have their cell bodies in gray nuclei within the brain. Except for the first pair of cranial nerves, which is atypical, they all attach to the “old” brain stem. Cranial nerves have been given both names and numbers, and Roman numerals should be used. They are as follows: I II III IV V VI Olfactory Optic Oculomotor Trochlear Trigeminal Abducens VII VIII IX X XI XII Facial Vestibulocochlear Glossopharyngeal Vagus Spinal Accessory Hypoglossal Refer to Figure 9.11 in the Photographic Atlas; and to pages 500 – 514 of the Tortora textbook. Also, several reference sheets follow this exercise.